Abstract
Messages emphasizing the harms of smoking (loss-framed) or the benefits of not smoking (gain-framed) may be effective for engaging adolescents with tobacco prevention resources. This novel approach could help to close a gap in tobacco prevention intervention delivery in the pediatric primary care setting. To examine the effects of framed messages for engaging adolescents with an evidence-based smoking prevention website, adolescents ages 12 to 17 presenting for primary care well-visits were recruited for a three-arm experiment. Participants completed baseline measures including demographics, smoking behavior, and smoking susceptibility and were randomized to view 1 of 3 messages introducing an evidence-based smoking prevention website: (1) gain-framed communicating the benefits of avoiding smoking, (2) loss-framed communicating the harms of smoking, or (3) neutral. Self-reported website engagement was assessed at 1-month follow-up. Participants (279) (87% of those enrolled) completed a follow-up (M age 14.9 years, 66% female, 32% non-white race, 47% non-susceptible never smokers, 53% susceptible never smokers/ever smokers). Overall, 26% of participants reported website engagement. After adjusting for baseline intentions to visit the website, engagement was significantly greater in response to the loss-framed message than the gain-framed (odds ratio [OR] 3.05, 95% confidence interval [CI] 1.51, 6.15) and neutral (OR 2.31, 95% CI 1.15, 4.63) messages. The message framing effects did not differ by baseline smoking risk. Loss-framed messages emphasizing the harms of smoking may be effective for engaging adolescents with smoking prevention resources.
Electronic supplementary material
The online version of this article (doi:10.1007/s13142-017-0481-5) contains supplementary material, which is available to authorized users.
Keywords: Adolescents, Smoking prevention, Message framing, Primary care
INTRODUCTION
Despite recent declines in cigarette smoking prevalence in the population, smoking remains a leading preventable cause of death in the USA and continues to incur substantial morbidity, mortality, and financial costs each year [1]. Nearly 10% of US adolescents smoke cigarettes [2], a substantial proportion of youth who initiate smoking transition to regular use by young adulthood [3], and a majority of adult smokers initiate smoking during adolescence, making primary prevention of adolescent smoking a public health priority [1]. The pediatric primary care setting is one important context for delivering adolescent tobacco prevention interventions [4]. Clinical guidelines recommend that pediatric primary care providers screen and counsel all adolescent patients for cigarette smoking and other forms of tobacco use [5]. However, setting-, provider-, and patient-level barriers (e.g., brief clinical encounters, competing health priorities) often limit providers’ ability to accomplish this goal [4]. Population data indicate that as few as one of three middle- and high school-aged US adolescents report being asked about tobacco use or counseled on tobacco cessation or avoidance by a healthcare provider [6].
Emerging models (e.g., Ask, Advise, Connect [AAC]) seek to address this gap in tobacco use intervention delivery by positioning providers to screen patients during the clinical encounter and connect them to evidence-based interventions that can be readily accessed outside of the clinical setting [7, 8]. In the AAC model, providers assess smoking and provide brief guidance to patients on smoking behavior change, and then refer patients to supportive interventions, such as smoking cessation quitlines or other counseling, to access following the clinical encounter. The AAC model has been shown to be effective for increasing adult smokers’ uptake of cessation resources such as quitlines in primary care settings [7, 8]. However, there is limited evidence on whether such a model can be adopted for smoking prevention in the pediatric primary care setting.
Evidence-based adolescent smoking prevention interventions are available online, can be freely accessed, and can appeal to adolescents due to their interactivity and game-like features [9, 10]. Research suggests adolescents find such interventions to be engaging, and non-smokers have been shown to be up to three times less likely to initiate smoking as a result of such interventions [9, 10]. Pediatric primary care providers are poised to connect adolescents to such resources by offering them as adjuncts to clinical encounters [4]. However, a critical unanswered question in this intervention model is how to communicate online resources to adolescents in such a way that motivates them and engage with them. This is an important step to investigate because adolescents are traditionally a difficult population to engage with prevention resources online due in part to competing interests and activities within this medium (e.g., web surfing, social media) [11, 12].
Grounded in prospect theory, the concept of message framing suggests that framing messages around the benefits of avoiding a risky behavior (i.e., gain-framed) or the harms of engaging in a risky behavior (i.e., loss-framed) can differentially affect behavioral outcomes [13, 14]. This message framing hypothesis is rooted in prospect theory’s tenets of decision making under circumstances of risk and uncertainty and postulates that health-related messaging can convey information in terms of gains or losses to motivate behavior change [13]. Gain- and loss-framed messages may influence behavioral outcomes through differential cognitive pathways, such as respectively affecting efficacy and risk beliefs related to the target behavior [15]. A longstanding body of research generally indicates that gain-framed messages are more effective for promoting disease prevention behaviors, such as avoiding smoking [16]. However, framing effects consistent with this hypothesis are not always evident and the observed effects are often small [16]. There is also evidence from message framing studies on tobacco use and other behavioral domains that gain- and loss-framed message effects may differ based on factors such as prior involvement with the target behavior or level of behavioral risk [17, 18]. Most message framing studies have focused on adult smoking cessation behavior [16], and research examining the effects of framed messages for adolescent smoking prevention is scarce. Unique factors influencing adolescent smoking initiation (e.g., sensation seeking, social exposures) [19] compared with adult smoking cessation behavior (e.g., nicotine dependence) [20] also suggests the possibility that the effects of framed messages for youth smoking prevention may differ from those observed in studies of adult smoking cessation. No study to date has investigated whether gain- or loss-framed messages are effective for motivating adolescents to take action to avoid smoking by engaging with evidence-based prevention resources online and if message framing effects differ based on adolescents’ risk of smoking in the future.
This study sought to fill this research gap by examining the effects of persuasive, gain- and loss-framed messages for promoting adolescents’ engagement with an evidence-based, interactive online smoking prevention intervention offered as an adjunct to pediatric primary care visits. The study also investigated if the effects of framed messages differed by adolescents’ baseline smoking risk.
METHODS
Setting and participants
The study took place at an adolescent medicine clinic in a large, urban hospital located in Washington, DC. Eligible participants were patients aged 12 to 17 years who were in good health based on parent and adolescent self-report. Participants also had to have access to the Internet and an e-mail address in order to complete study procedures. There were no inclusion or exclusion criteria based on smoking behavior.
Participants were recruited in two ways. Potentially eligible patients within the study age range were identified using clinic records, and a recruitment packet was sent by US postal mail to the address of the parent or guardian. The packet included a letter introducing the study, informed consent and assent forms, and a stamped return envelope. Research staff conducted telephone follow-up to the mailings within 7 days to address any questions about the study, assess interest and eligibility to participate, and administer informed consent and assent. Recruitment also occurred in the clinic setting at predetermined times where research staff approached potentially eligible patients and their parents at the time of their clinic visits, introduced the study, and screened those who were interested for eligibility. Those who were eligible and had a parent present provided signed informed consent and assent forms to complete study enrollment at their clinic visits. Potentially interested and eligible patients who did not complete enrollment at the clinic (e.g., if a parent was not present or they wanted more time to consider participating) were provided with a study packet and research staff followed up by telephone to screen and enroll participants similar to procedures described above.
All study participants provided written parental consent and adolescent assent, and the study procedures were reviewed and approved by an institutional review board.
Procedures
Participants were contacted by e-mail within 7 days of enrollment and provided with a web link to complete a secure, baseline assessment online. The baseline included measures of demographic characteristics, smoking behavior, and other constructs described below. At the conclusion of the baseline, using a simple randomization algorithm, the participants were randomly assigned in approximately equal numbers to one of three message conditions: (1) a gain-framed message emphasizing the benefits of avoiding smoking; (2) a loss-framed message emphasizing the risks of smoking; (3) a neutral message. All messages introduced participants to the online smoking prevention intervention in such a way that was consistent with the framing conditions. The gain- and loss-framed messages included visual imagery consistent with the message frame. Framed message content was developed based on the existing literature on adolescent tobacco prevention communication [21–23] and message framing [16] and with feedback from the study team. Draft messages were pretested through one-on-one interviews with adolescents from the target population and revised according to their feedback. Study messages are available from the corresponding author upon request.
At the conclusion of the baseline assessment after the message exposure, participants were provided with a web link to access the smoking prevention website. The website to which participants were directed is an evidence-based, multimedia online smoking prevention and cessation resource developed for adolescents called “A Smoking Prevention Interactive Experience” (ASPIRE) [9, 10]. ASPIRE is a theory-driven, individually tailored program designed for adolescents that is available online [9, 10]. It is designed as a self-paced game where adolescents enter basic demographic information and their past smoking behavior, and the interactive experience is tailored to their responses. It is designed so adolescents can revisit the site and access the contents as often as they wish. In a school-based randomized trial, at 18-month follow-up, adolescent non-smokers were three times less likely to initiate smoking with ASPIRE relative to usual care [9]. ASPIRE is recognized as a National Cancer Institute Research Tested Intervention Program and is included in the American Academy of Pediatrics recommendation statement for tobacco prevention programs [5].
One month after the baseline assessment, participants were contacted by e-mail using similar procedures to complete an online follow-up assessment.
Measures
Demographics
Adolescent demographics measured at baseline included gender, age, and race/ethnicity. Parents’ marital status and educational attainment were ascertained at eligibility screening from those willing to report this information.
Smoking-related covariates
To characterize the sample and assess the need to control for any smoking-related risk factors in analyses, we measured three well-established risk factors for adolescent smoking: exposure to family and friends who smoke and tobacco advertising exposure [19]. Exposure to family and friends who smoke were measured using five valid items [24, 25]. Items capture exposure to smoking by immediate family members (parents, siblings) and male and female friends and are used to create a dichotomous variable indicating any smoking exposure through these two sources. Tobacco advertising exposure was assessed using four items adapted from a previously validated national adolescent tobacco survey [26]. Items measure adolescents’ exposure to tobacco advertising via television and in movies, the Internet, print media, and the point of sale. Responses are on a five-point scale ranging from “never” to “all the time” and were summed to create a score with higher values indicating greater advertising exposure (Cronbach’s α = 0.70).
Adolescent smoking risk
Adolescent smoking risk was codetermined by two independent variables: (1) lifetime smoking behavior and (2) smoking susceptibility. Lifetime smoking was measured at baseline using valid items from adolescent tobacco surveys [27] and used to categorize participants as either never smokers (never tried smoking, not even a puff) or ever smokers (tried smoking). Among never smokers, baseline susceptibility to smoking was then assessed with a valid four-item measure [28]. This measure evaluates the likelihood of smoking a cigarette soon, in the next year, experimenting in the future, and smoking a cigarette if offered one by a friend. Response options include “definitely yes,” “probably yes,” “probably not,” and “definitely not.” Never smokers were considered susceptible to smoking in the future if they endorsed a response other than definitely not to any of the four items [19, 28, 29]; otherwise, they were considered non-susceptible. Susceptibility has been consistently shown to predict future smoking initiation among adolescents [19, 28, 29]. Our binary variable of adolescent smoking risk indicated whether participants were non-susceptible never smokers or susceptible never smokers/ever smokers. The latter categories were combined due to the low prevalence of ever smokers in the sample (11.6% at follow-up).
Intentions to use prevention website
At baseline, immediately after exposure to the messages presenting the website, participants’ behavioral intentions to visit the smoking prevention website were assessed using a single item adapted from previous research on adolescent Internet use and online tobacco interventions [30–32]. The item asked “Do you think you would visit this website?” with response options for definitely yes, probably yes, probably not, and definitely not.
Website engagement
The primary outcome for the study was participants’ self-reported engagement with the prevention website at follow-up. Similar to the behavioral intentions item, engagement was measured using a single item adapted from previous research [30–32]. The item was preceded by a statement describing the study website and asked participants whether they visited the site in the past 30 days (yes/no). Among those who indicated any engagement with the website, we assessed how often they did so during the follow-up period using a single item with response options for once, twice, three times, and four or more times.
Statistical analysis
A priori power calculations indicated a baseline sample of 300 or more participants would provide adequate power to test the effects of framed messages for website engagement between messaging conditions. Descriptive statistics were used to characterize the baseline and follow-up samples, and bivariate tests (t-tests, χ2 tests) were used to assess whether participants who were lost to follow-up differed from those retained. Similarly, bivariate tests were used to assess whether any participant characteristics differed by message condition.
To assess whether participants’ engagement with the website at follow-up differed by message condition, bivariate χ 2 tests were conducted. Then, a series of logistic regression models were created to assess the effects of message condition on website engagement comparing the loss-framed message to both gain-framed and neutral messages. Models were conducted unadjusted and adjusting for intentions to visit the website measured at baseline. To assess whether message framing effects differed by smoking risk at baseline (non-susceptible, never smokers versus those who were susceptible or had tried smoking previously), χ 2 tests were used to examine whether message framing effects differed by smoking risk at baseline, and an interaction between message condition and baseline smoking risk was introduced into the regression model.
The clinical setting serves families with multiple children, so the sample included the following sibling sets: 204 singletons, 29 dyads, 3 triads, and 2 tetrads. The logistic regression models corrected for variance attributable to clustering of siblings within families using survey procedures in SAS version 9.3 [3].
RESULTS
Participants
In total, 645 patients and their parents were approached about the study (n = 106 by postal mail, n = 539 in clinic), 558 (86.5% of those approached) were screened for eligibility, and 433 (77.6% of those screened) were eligible. Most were ineligible due to the presence of a health condition that parents or patients reported would inhibit participation (89.6% of n = 125 ineligible patients). Of the eligible patients, 375 (86.6%) provided parental consent and adolescent assent, and 319 (85.1% of those consented) completed a baseline survey and were randomized. Additional information on recruitment and enrollment is shown in Supplementary Fig. 1.
A total of 279 participants (87.5% of those enrolled) completed a follow-up and were included in the analytic sample. Those lost to follow-up were more likely to be Black/African American (46.2% to follow-up vs. 23.7% retained, p = .003), to report having friends who smoked cigarettes at baseline (41.0% lost to follow-up vs. 25.0% retained, p = .035), and reported greater baseline tobacco advertising exposure (M 12.4, SD 2.9 lost to follow-up, M 11.2, SD 2.8 retained, p = .013). Characteristics of participants at baseline and follow-up are shown in Table 1.
Table 1.
Participant characteristics at baseline and 1-month follow-up
| Baseline (n = 319) | Follow-up (n = 279) | P value | |
|---|---|---|---|
| Gender | .107 | ||
| Male | 36.0% (105) | 34.4% (96) | |
| Female | 64.0% (204) | 65.6% (183) | |
| Age (M, SD) | 15.0 (1.6) | 14.9 (1.6) | .263 |
| Race | .003 | ||
| Black/African American | 26.4% (84) | 23.7% (66) | |
| White | 57.9% (184) | 58.4% (163) | |
| Other race | 15.7% (51) | 17.9% (50) | |
| Ethnicity | .645 | ||
| Hispanic | 12.2% (39) | 12.5% (35) | |
| Non-Hispanic | 87.8% (280) | 87.5% (244) | |
| Parent’s marital status | – | ||
| Married/partnership | 78.3% (241) | 81.4% (219) | |
| Single, never married | 6.8% (21) | 6.0% (16) | |
| Divorced/separated/widowed | 14.9% (46) | 12.6% (34) | |
| Parent’s educational attainment | – | ||
| Less than college degree | 19.6% (59) | 19.7% (52) | |
| College degree or higher | 80.4% (243) | 80.3% (212) | |
| Smoking risk | .100 | ||
| Never smoker, not susceptible | 46.2% (145) | 47.3% (130) | |
| Never smoker, susceptible/ever smoker | 53.8% (169) | 52.7% (145) | |
| Covariates related to smoking risk | |||
| Exposure to family members’ smoking | 18.7% (59) | 18.1% (50) | .457 |
| Exposure to friends’ smoking | 26.9% (85) | 25.0% (69) | .035 |
| Tobacco advertising exposure (M, SD) | 11.4 (2.8) | 11.6 (3.1) | .013 |
| Message framing conditions | .797 | ||
| Gain-framed | 32.9% (105) | 33.0% (92) | |
| Loss-framed | 33.2% (106) | 32.6% (91) | |
| Neutral | 33.9% (108) | 34.4% (96) |
Data are % (n) unless otherwise indicated. Some ns within categories do not sum to total n due to sporadic missing data (<5% of the sample for any given variable). P values reflect comparison of the sample retained at 1 month versus those lost to follow-up. All participants lost to follow-up were missing data on parental demographics, so p value could not be computed
Bivariate analyses by study condition
There were no statistically significant differences in participant demographic or smoking-related characteristics by study condition, indicating successful randomization. After the message exposure at baseline, participants’ intentions to visit the website differed significantly by study condition (F 2,274 = 5.23, p = .006). Intentions to visit the website were highest for neutral condition (M 2.48, SD 0.75), followed by the loss-frame (M 2.21, SD 0.74) and gain-framed (M 2.15, SD 0.71) conditions.
Website engagement by message condition
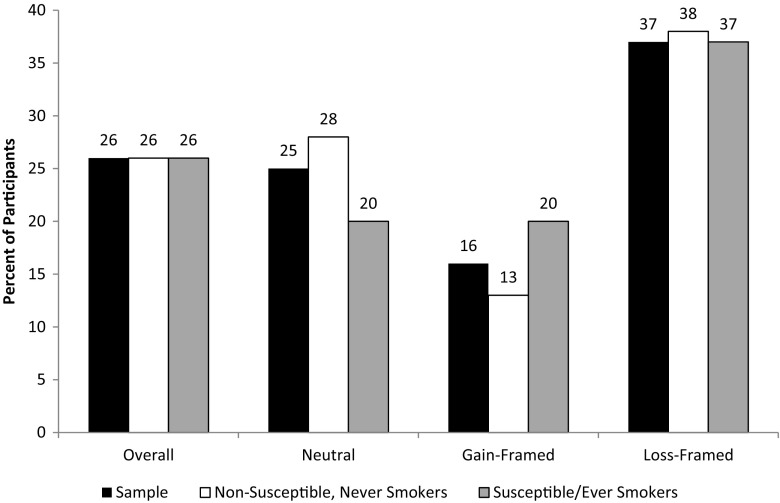
Overall, 25.9% of participants reported engagement with the website. Of participants who reported website engagement, 60.6% visited the site once, 22.5% twice, 4.2% three times, and 12.7% four or more times during the follow-up period. In bivariate analyses website engagement differed significantly by messaging condition (Fig. 1). Engagement was greatest for the loss-framed message (37.1%), followed by the neutral (24.5%) and gain-framed message (16.1%, p = .006).
Fig 1.
Percentage of participants reporting website engagement at follow-up overall and by baseline smoking risk. Note: In bivariate analyses of message framing effects in the study sample χ 2 [2 df] = 10.25, p = .006; among non-susceptible, never smokers χ 2 [2 df] = 6.96, p = .031; and among susceptible never smokers/ever smokers χ 2 [2 df] = 4.96, p = .084. In a multivariable logistic regression model that adjusted for baseline intentions to visit the website, the interaction between message condition and baseline smoking risk was not statistically significant (χ2 [2 df] = 1.53, p = .466)
Results of the logistic regression analyses of message framing effects on website engagement are shown in Table 2. In unadjusted models, participants in the loss-framed message condition reported greater website engagement than the neutral (odds ratio [OR] 1.85, 95% confidence interval [CI], 0.99, 3.46) and gain-framed (OR 3.13, 95% CI 1.56, 6.29) message conditions. In the models adjusting for differences in baseline intentions to visit the website, patterns were similar but all comparisons reached statistical significance: the loss-framed message produced significantly greater website engagement compared with the neutral (OR 2.31, 95% CI 1.15, 4.63) and gain-framed (OR 3.05, 95% CI 1.51, 6.15) messages.
Table 2.
Smoking prevention website utilization by study condition at 1-month follow-up
| Neutral message as comparison | Gain-framed message as comparison | |||
|---|---|---|---|---|
| Unadjusted odds ratio (95% CI) | Adjusted odds ratio (95% CI) | Unadjusted odds ratio (95% CI) | Adjusted odds ratio (95% CI) | |
| Loss-framed message | 1.85 (0.99, 3.46) | 2.31 (1.15, 4.63) | 3.13 (1.56, 6.29) | 3.05 (1.51, 6.15) |
| Gain-framed message | 0.59 (0.28, 1.26) | 0.76 (0.34, 1.69) | Ref. | Ref. |
| Neutral message | Ref. | Ref. | 1.69 (0.80, 3.58) | 1.32 (0.59, 2.95) |
| Baseline intentions | – | 2.17 (1.40, 3.36) | – | 2.17 (1.40, 3.36) |
Models corrected variance attributable to within-family correlated data due to siblings in the dataset using SAS version 9.3 survey data analysis procedures. Odds ratios with 95% confidence intervals that do not include 1 are statistically significant at p < .05
Message framing effects by baseline smoking risk
Figure 1 displays message framing effects for website engagement by baseline smoking risk. In bivariate analyses, there were similar trends in the message framing effect among non-susceptible, never smokers (χ 2 [2 df] = 6.96, p = .031) and among those who were susceptible to smoking or who had tried smoking previously (χ 2 [2 df] = 4.96, p = .084), with the highest proportion of both groups reporting website engagement in response to the loss-framed message (Fig. 1). In the logistic regression model that adjusted for baseline intentions to visit the website, the interaction between message condition and baseline smoking risk was not statistically significant (χ 2 [2 df] = 1.53, p = .466), indicating the message framing effects were robust to baseline smoking risk.
DISCUSSION
This study examined the effects of persuasive gain- and loss-framed messages for motivating adolescents to engage with an evidence-based smoking prevention website offered as an adjunct to pediatric primary care visits. The findings indicate loss-framed messages using text and imagery to convey the risks of smoking were more effective than gain-framed and neutral messages for promoting website engagement, and the effects of loss-framed messages were consistent across participants’ baseline smoking risk. These results have implications for future research and interventions for adolescent smoking prevention in the primary care setting that can address known barriers to smoking prevention intervention delivery [4].
Examining how to effectively communicate evidence-based smoking prevention resources to youth is an important first step to implementing system-based approaches to improve intervention delivery in this clinical context. Such systems-based interventions leverage clinical informatics resources, such as electronic health records, to streamline the clinical workflow and routinize screening and counseling patients for smoking and referral to intervention resources [7]. Recent studies demonstrate such an Ask, Advise, Connect intervention model where primary care providers screen for smoking, provide brief cessation advice, and connect adult smokers with cessation resources such as telephone quitlines is effective for increasing utilization of these cessation resources among smokers [7, 8]. Our findings provide evidence in support of an initial step of this intervention approach in pediatric primary care for adolescent smoking prevention: loss-framed messages conveying the risks of smoking led two to three times as many adolescents to engage with an evidence-based prevention website than gain framed messages conveying the benefits of smoking avoidance or a neutral message introducing them to the website. In both these investigations, however, the effect on engagement with smoking-related interventions was modest overall. This highlights a need for research to continue to investigate ways to design communication strategies to maximize their effect on patients’ intervention engagement within such intervention models, such as messaging targeting other smoking-related constructs beyond the risk-related targets of loss-framed messages (e.g., self-efficacy) [15].
These results are consistent with other evidence indicating messaging that vividly conveys the risks of smoking is effective for adolescent tobacco prevention, such as pictorial warning labels on tobacco products [33, 34]. The study results add uniquely to the evidence on adolescent smoking prevention by indicating that such loss-framed messages are effective not only for shifting adolescents’ perceptions of smoking and other related outcomes [33, 34] but by demonstrating they can promote engagement with smoking prevention resources offered online. Future studies can apply these findings in the process of implementing and testing intervention models such as Ask, Advise, Connect for adolescent smoking prevention in the pediatric primary care setting.
The study also showed the effects of loss-framed messages were similar across levels of baseline smoking risk, including among those who were susceptible to smoking or had ever tried smoking at baseline. However, the prevalence of smoking in the sample was low in comparison with adolescents nationally [2] preventing further analyses of message effects among adolescents who actively smoke. Among adult smokers, research indicates that framed message effects vary based on factors related to smoking intensity, such as nicotine dependence, indicating that gain-framed messages have a stronger effect for promoting cessation among dependent smokers [17]. The observed effects of loss-framed messages may have been due in part to the fact that few adolescents were active smokers and messaging conveying smoking-related risks motivated action [35]. The differences in message framing effects observed here compared with studies of adult smokers may also be due to differences in the recommended behavioral action (i.e., engaging with a website versus quitting smoking) and factors influencing these respective behaviors [19, 20], as previous message framing studies show variation in effects across these types of behaviors [16]. Future studies can build from this investigation by examining the effects of framed messages in higher-risk adolescents, including those who smoke.
The study findings may also have implications for research related to tobacco product warning label regulations. The Family Smoking Prevention and Tobacco Control Act authorized the Food and Drug Administration (FDA) to regulate tobacco products, including requiring pictorial warning labels for cigarette packs that are similar to the loss-framed messages tested here [36]. FDA issued an initial set of pictorial warnings for cigarette packages, but tobacco industry lawsuits prevented their implementation [37]. As part of this court decision, the federal judge criticized the inclusion of smoking cessation resources (i.e., a quitline number) on the warnings [37]. Although this study did not investigate the effects of pictorial warnings, the loss-framed messages tested are similar and the findings suggest they may be effective for motivating adolescents to engage with evidence-based intervention resources. This is an outcome that may be important to investigate in studies of warning labels among adolescents.
The study findings should be interpreted in light of important limitations. All study measures were based on adolescent self-report, website engagement was assessed with a single item measure, and it is unclear how this metric of engagement relates to smoking behavior. Although the study relied on valid measures, they are subject to potential reporting biases. Future studies should implement multiple, objective website engagement measures (e.g., website tracking analytics) and examine smoking behavior as an outcome. The study was conducted in a convenience sample of adolescents recruited from a single clinical site, and the prevalence of smoking in the sample was low relative to adolescents nationally. This limits the generalizability of the findings to broader populations, and future work to replicate the findings in population-based samples is warranted. Finally, the results are based on a single brief exposure to the study messages. It will be important to examine additional strategies to increase adolescents’ engagement with smoking prevention resources, such as message content targeting additional smoking-related constructs, repeated exposures, or booster messages sent through other media (e.g., online, through mobile phones).
Despite these limitations, the study findings have implications for researchers, practitioners, and policymakers. For researchers, it will be important to evaluate the effects of framed messages for motivating preventive behavior change in higher-risk populations not studied here, such as adolescents who currently smoke. For practitioners, our findings suggest that in pediatric primary care settings, presenting evidence-based prevention resources offered as adjuncts to clinical visits by vividly conveying the risks of smoking using text and vivid imagery can optimize adolescents’ engagement with these resources following the clinical encounter. For policymakers, the study findings add to the evidence base in support of risk-based messaging in broader tobacco regulatory contexts, such as pictorial warning labels for cigarette packages to dissuade smoking among adolescents.
Electronic supplementary material
(PDF 13.7 kb).
Compliance with ethical standards
Funding sources
This study was supported in part by the National Institutes of Health (NIH) and the Food and Drug Administration (FDA) Center for Tobacco Products under NIH grant numbers R03CA162839 and K07CA172217. This work was also supported in part by the Georgetown Lombardi Comprehensive Cancer Center Support under NIH grant number P30CA051008. The study sponsors had no role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the FDA.
Conflict of interest
The authors declare that they have no conflicts of interest.
Statement of animal welfare
Not applicable.
Ethical approval
All procedures were conducted were conducted in accordance with the ethical standards of the responsible committee on human subjects and with the 1964 Helsinki Declaration.
Informed consent
Written parental consent and participant assent was obtained from all participants.
IRB approval
The study was reviewed and approved by the Georgetown University Institutional Review Board.
Footnotes
Previous Publication: The findings reported have not been previously published.
Previous Reporting: The findings reported were presented in part at the 2014 Annual Meeting of the Society for Research on Nicotine and Tobacco.
Data Access: The authors have full control of all primary data and agree to allow the journal to review their data if requested.
Implications
Researchers or Research: In the future, it will be important to evaluate the effects of framed messages for motivating preventive behavior change in higher-risk populations not studied here, such as adolescents who currently smoke.
Practitioners or Practice: For practitioners, our findings suggest that in pediatric primary care settings, presenting evidence-based prevention resources offered as adjuncts to clinical visits by conveying the risks of smoking using text and vivid imagery can optimize adolescents’ engagement with these resources following the clinical encounter.
Policymakers or Policy: For policymakers, the study findings add to the evidence base in support of risk-based messaging in broader tobacco regulatory contexts, such as pictorial warning labels for cigarette packages to dissuade smoking among adolescents.
Electronic supplementary material
The online version of this article (doi:10.1007/s13142-017-0481-5) contains supplementary material, which is available to authorized users.
References
- 1.National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health. The Health Consequences of Smoking—50 years of progress: a report of the surgeon general. 2014. Available at http://www.ncbi.nlm.nih.gov/books/NBK179276/. Accessed 11 August 2016.
- 2.Singh T, Arrazola RA, Corey CG, et al. Tobacco use among middle and high school students - United States, 2011-2015. MMWR Morb Mortal Wkly Rep. 2016;65(14):361–367. doi: 10.15585/mmwr.mm6514a1. [DOI] [PubMed] [Google Scholar]
- 3.Mays D, Gilman SE, Rende R, Luta G, Tercyak KP, Niaura RS. Parental smoking exposure and adolescent smoking trajectories. Pediatrics. 2014;133(6):983–991. doi: 10.1542/peds.2013-3003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pbert L, Farber H, Horn K, et al. State-of-the-art office-based interventions to eliminate youth tobacco use: the past decade. Pediatrics. 2015;135(4):734–747. doi: 10.1542/peds.2014-2037. [DOI] [PubMed] [Google Scholar]
- 5.Farber HJ, Walley SC, Groner JA, Nelson KE. Clinical practice policy to protect children from tobacco, nicotine, and tobacco smoke. Pediatrics. 2015;136(5):1008–1017. doi: 10.1542/peds.2015-3110. [DOI] [PubMed] [Google Scholar]
- 6.Schauer GL, Agaku IT, King BA, Malarcher AM. Health care provider advice for adolescent tobacco use: results from the 2011 National Youth Tobacco Survey. Pediatrics. 2014;134(3):446–455. doi: 10.1542/peds.2014-0458. [DOI] [PubMed] [Google Scholar]
- 7.Vidrine JI, Shete S, Cao Y, et al. Ask-advise-connect: a new approach to smoking treatment delivery in health care settings. JAMA Intern Med. 2013;173(6):458–464. doi: 10.1001/jamainternmed.2013.3751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vidrine JI, Shete S, Li Y, et al. The ask-advise-connect approach for smokers in a safety net healthcare system: a group-randomized trial. Am J Prev Med. 2013;45(6):737–741. doi: 10.1016/j.amepre.2013.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Prokhorov AV, Kelder SH, Shegog R, et al. Impact of a smoking prevention interactive experience (ASPIRE), an interactive, multimedia smoking prevention and cessation curriculum for culturally diverse high-school students. Nicotine Tob Res. 2008;10(9):1477–1485. doi: 10.1080/14622200802323183. [DOI] [PubMed] [Google Scholar]
- 10.Prokhorov AV, Kelder SH, Shegog R, et al. Project ASPIRE: an interactive, multimedia smoking prevention and cessation curriculum for culturally diverse high school students. Subst Use Misuse. 2010;45(6):983–1006. doi: 10.3109/10826080903038050. [DOI] [PubMed] [Google Scholar]
- 11.Crutzen R, De NJ, Brouwer W, Oenema A, Brug J, de Vries NK. Internet-delivered interventions aimed at adolescents: a Delphi study on dissemination and exposure. Health Educ Res. 2008;23(3):427–439. doi: 10.1093/her/cym094. [DOI] [PubMed] [Google Scholar]
- 12.Crutzen R, De NJ, Brouwer W, Oenema A, Brug J, de Vries NK. Strategies to facilitate exposure to internet-delivered health behavior change interventions aimed at adolescents or young adults: a systematic review. Health Educ Behav. 2011;38(1):49–62. doi: 10.1177/1090198110372878. [DOI] [PubMed] [Google Scholar]
- 13.Rothman AJ, Salovey P. Shaping perceptions to motivate healthy behavior: the role of message framing. Psychol Bull. 1997;121(1):3–19. doi: 10.1037/0033-2909.121.1.3. [DOI] [PubMed] [Google Scholar]
- 14.Tversky A, Kahneman D. The framing of decisions and the psychology of choice. Science. 1981;211(4481):453–458. doi: 10.1126/science.7455683. [DOI] [PubMed] [Google Scholar]
- 15.Witte K. Fear control and danger control: a test of the extended parallel process model (EPPM) Commun Monogr. 1994;61(2):113–134. doi: 10.1080/03637759409376328. [DOI] [Google Scholar]
- 16.Gallagher KM, Updegraff JA. Health message framing effects on attitudes, intentions, and behavior: a meta-analytic review. Ann Behav Med. 2012;43(1):101–116. doi: 10.1007/s12160-011-9308-7. [DOI] [PubMed] [Google Scholar]
- 17.Fucito LM, Latimer AE, Salovey P, Toll BA. Nicotine dependence as a moderator of message framing effects on smoking cessation outcomes. Ann Behav Med. 2010;39(3):311–317. doi: 10.1007/s12160-010-9187-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gerend MA, Shepherd JE, Monday KA. Behavioral frequency moderates the effects of message framing on HPV vaccine acceptability. Ann Behav Med. 2008;35(2):221–229. doi: 10.1007/s12160-008-9024-0. [DOI] [PubMed] [Google Scholar]
- 19.Wellman RJ, Dugas EN, Dutczak H, et al. Predictors of the onset of cigarette smoking: a systematic review of longitudinal population-based studies in youth. Am J Prev Med. 2016;51(5):767–778. doi: 10.1016/j.amepre.2016.04.003. [DOI] [PubMed] [Google Scholar]
- 20.Vangeli E, Stapleton J, Smit ES, Borland R, West R. Predictors of attempts to stop smoking and their success in adult general population samples: a systematic review. Addiction. 2011;106(12):2110–2121. doi: 10.1111/j.1360-0443.2011.03565.x. [DOI] [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention. Best Practices for Comprehensive Tobacco Control Programs—2014. 2014. Available at http://www.cdc.gov/tobacco/stateandcommunity/best_practices/pdfs/2014/comprehensive.pdf. Accessed 11 August 2016.
- 22.National Cancer Institute. The role of the media in promoting and reducing tobacco use. Tobacco Control Monograph No. 19. 2008. Available at http://cancercontrol.cancer.gov/brp/tcrb/monographs/19/m19_complete.pdf. Accessed 11 August 2016.
- 23.National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health. Preventing tobacco use among youth and young adults: a report of the surgeon general. 2012. Available at http://www.ncbi.nlm.nih.gov/books/NBK99237/. Accessed 11 August 2016.
- 24.Pierce JP, Choi WS, Gilpin EA, Farkas AJ, Berry CC. Tobacco industry promotion of cigarettes and adolescent smoking. JAMA. 1998;279(7):511–515. doi: 10.1001/jama.279.7.511. [DOI] [PubMed] [Google Scholar]
- 25.Pierce JP, Distefan JM, Jackson C, White MM, Gilpin EA. Does tobacco marketing undermine the influence of recommended parenting in discouraging adolescents from smoking? Am J Prev Med. 2002;23(2):73–81. doi: 10.1016/S0749-3797(02)00459-2. [DOI] [PubMed] [Google Scholar]
- 26.Bunnell RE, Agaku IT, Arrazola RA, et al. Intentions to smoke cigarettes among never-smoking US middle and high school electronic cigarette users: National Youth Tobacco Survey, 2011-2013. Nicotine Tob Res. 2015;17(2):228–235. doi: 10.1093/ntr/ntu166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Arrazola RA, Singh T, Corey CG, et al. Tobacco use among middle and high school students—United States, 2011-2014. MMWR Morb Mortal Wkly Rep. 2015;64(14):381–385. [PMC free article] [PubMed] [Google Scholar]
- 28.Pierce JP, Choi WS, Gilpin EA, Farkas AJ, Merritt RK. Validation of susceptibility as a predictor of which adolescents take up smoking in the United States. Health Psychol. 1996;15(5):355–361. doi: 10.1037/0278-6133.15.5.355. [DOI] [PubMed] [Google Scholar]
- 29.Evans N, Farkas A, Gilpin E, Berry C, Pierce JP. Influence of tobacco marketing and exposure to smokers on adolescent susceptibility to smoking. J Natl Cancer Inst. 1995;87(20):1538–1545. doi: 10.1093/jnci/87.20.1538. [DOI] [PubMed] [Google Scholar]
- 30.Escoffery C, McCormick L, Bateman K. Development and process evaluation of a web-based smoking cessation program for college smokers: innovative tool for education. Patient Educ Couns. 2004;53(2):217–225. doi: 10.1016/S0738-3991(03)00163-0. [DOI] [PubMed] [Google Scholar]
- 31.Hunley SA, Evans JH, Delgado-Hachey M, Krise J, Rich T, Schell C. Adolescent computer use and academic achievement. Adolescence. 2005;40(158):307–318. [PubMed] [Google Scholar]
- 32.Patten CA, Croghan IT, Meis TM, et al. Randomized clinical trial of an Internet-based versus brief office intervention for adolescent smoking cessation. Patient Educ Couns. 2006;64(1–3):249–258. doi: 10.1016/j.pec.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 33.Noar SM, Hall MG, Francis DB, Ribisl KM, Pepper JK, Brewer NT. Pictorial cigarette pack warnings: a meta-analysis of experimental studies. Tob Control. 2016;25(3):341–354. doi: 10.1136/tobaccocontrol-2014-051978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Noar SM, Francis DB, Bridges C, Sontag JM, Ribisl KM, Brewer NT. The impact of strengthening cigarette pack warnings: systematic review of longitudinal observational studies. Soc Sci Med. 2016;164:118–129. doi: 10.1016/j.socscimed.2016.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sheeran P, Harris PR, Epton T. Does heightening risk appraisals change people’s intentions and behavior? A meta-analysis of experimental studies. Psychol Bull. 2014;140(2):511–543. doi: 10.1037/a0033065. [DOI] [PubMed] [Google Scholar]
- 36.Husten CG, Deyton LR. Understanding the Tobacco Control Act: efforts by the US Food and Drug Administration to make tobacco-related morbidity and mortality part of the USA’s past, not its future. Lancet. 2013;381(9877):1570–1580. doi: 10.1016/S0140-6736(13)60735-7. [DOI] [PubMed] [Google Scholar]
- 37.Bayer R, Gostin L, Marcus-Toll D. Repackaging cigarettes—will the courts thwart the FDA? N Engl J Med. 2012;367(22):2065–2067. doi: 10.1056/NEJMp1211522. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 13.7 kb).