Abstract
Background
Hypertension and type 2 diabetes mellitus are major modifiable risk factors for cardiac, cerebrovascular, and kidney diseases. Reasons for poor disease control include nonadherence, lack of patient engagement, and therapeutic inertia.
Objective
The aim of this study was to assess the impact on clinic-measured blood pressure (BP) and glycated hemoglobin (HbA1c) using a digital medicine offering (DMO) that measures medication ingestion adherence, physical activity, and rest using digital medicines (medication taken with ingestible sensor), wearable sensor patches, and a mobile device app.
Methods
Participants with elevated systolic BP (SBP ≥140 mm Hg) and HbA1c (≥7%) failing antihypertensive (≥2 medications) and oral diabetes therapy were enrolled in this three-arm, 12-week, cluster-randomized study. Participants used DMO (includes digital medicines, the wearable sensor patch, and the mobile device app) for 4 or 12 weeks or received usual care based on site randomization. Providers in the DMO arms could review the DMO data via a Web portal. In all three arms, providers were instructed to make medical decisions (medication titration, adherence counseling, education, and lifestyle coaching) on all available clinical information at each visit. Primary outcome was change in SBP at week 4. Other outcomes included change in SBP and HbA1c at week 12, and low-density lipoprotein cholesterol (LDL-C) and diastolic blood pressure (DBP) at weeks 4 and 12, as well as proportion of patients at BP goal (<140/90 mm Hg) at weeks 4 and 12, medical decisions, and medication adherence patterns.
Results
Final analysis included 109 participants (12 sites; age: mean 58.7, SD years; female: 49.5%, 54/109; Hispanic: 45.9%, 50/109; income ≤ US $20,000: 56.9%, 62/109; and ≤ high school education: 52.3%, 57/109). The DMO groups had 80 participants (7 sites) and usual care had 29 participants (5 sites). At week 4, DMO resulted in a statistically greater SBP reduction than usual care (mean –21.8, SE 1.5 mm Hg vs mean –12.7, SE 2.8 mmHg; mean difference –9.1, 95% CI –14.0 to –3.3 mm Hg) and maintained a greater reduction at week 12. The DMO groups had greater reductions in HbA1c, DBP, and LDL-C, and a greater proportion of participants at BP goal at weeks 4 and 12 compared with usual care. The DMO groups also received more therapeutic interventions than usual care. Medication adherence was ≥80% while using the DMO. The most common adverse event was a self-limited rash at the wearable sensor site (12%, 10/82).
Conclusions
For patients failing hypertension and diabetes oral therapy, this DMO, which provides dose-by-dose feedback on medication ingestion adherence, can help lower BP, HbA1c, and LDL-C, and promote patient engagement and provider decision making.
Trial Registration
Clinicaltrials.gov NCT02827630; https://clinicaltrials.gov/show/NCT02827630 (Archived by WebCite at http://www.webcitation.org/6rL8dW2VF)
Keywords: digital medicine; hypertension; type 2 diabetes; patient engagement, medication adherence; therapeutic inertia
Introduction
Hypertension (HTN) and diabetes mellitus are major risk factors for cardiac diseases, stroke, and kidney diseases [1-5]. Despite the widespread availability of effective treatments, approximately half of treated patients do not have adequate blood pressure (BP) or glycemic control [4,6,7]. Poor medication adherence, lack of patient engagement, and therapeutic inertia are major contributors to patients not reaching their therapeutic targets [8-12]. Medication nonadherence alone costs US $290 billion annually in the United States and is difficult to assess and improve [13,14].
The psychology literature suggests that human beings in general are poor intuitive statisticians in that they cannot estimate their risk for consequences related to nonadherence and poor disease control [15]. Proteus Digital Health (Redwood City, CA, USA) hypothesized that this problem might be addressed by a common solution: detailed feedback to patients and physicians of actual dosing behavior. This would present patients with a clear adherence target while allowing physicians to discern lack-of-response calling for dosage or medication changes from patient nonadherence.
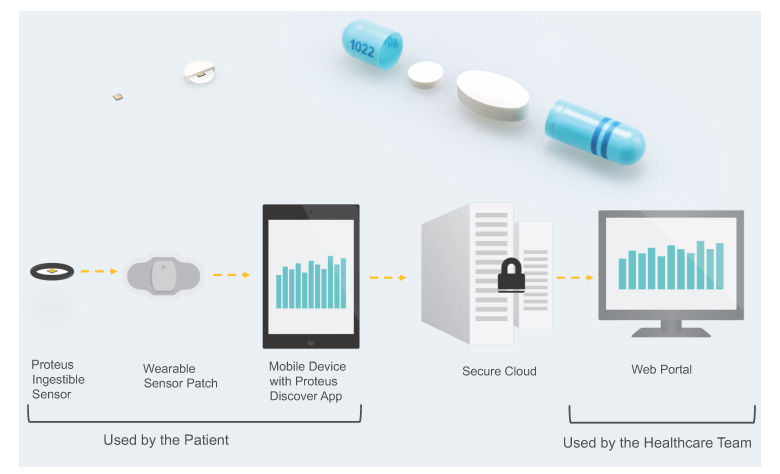
Proteus Discover, a digital medicine offering (DMO) from Proteus Digital Health, was designed specifically to provide feedback for medication taking and other health behaviors to both patients and providers. It consists of an ingestible sensor (contained inside a placebo pill), an adhesive wearable sensor patch, a patient mobile app, and a provider Web portal. After being swallowed, the ingestible sensor is activated and sends a signal with a specific code that is detected by the patch. When the ingestible sensor pill is taken with medication (now a digital medicine), the DMO can measure medication ingestion adherence. To ensure that the ingestible sensor and medication are taken simultaneously, the two can be co-encapsulated by a pharmacist (as was done during this study). The patch also measures activity, body angle, heart rate, and step count. Data from the patch are transmitted to a mobile device (eg, mobile phone) and then to the cloud. Patients can visualize the DMO data on their mobile device via an app and providers can view summaries of the DMO data for their patients on the Web portal. The mobile device app also prompts the patient to take their medication doses as scheduled. The goal of the DMO is to improve clinical outcomes through better patient self-care, enhanced patient-provider dialog, and data-driven optimization of therapy. (See Figure 1 for an overview of the DMO.)
Figure 1.
Top left: ingestible sensor and ingestible sensor pill. Top right: coencapsulation of a medication with an ingestible sensor pill. Bottom: components of the DMO and data flow.
Prior clinical studies demonstrated the accuracy, safety, and feasibility of using the DMO in patients across a range of medical conditions, including HTN and type 2 diabetes mellitus (T2DM), and suggested this DMO can identify reasons for uncontrolled HTN and help patients achieve BP control [16-21]. However, these uncontrolled studies did not focus on disease control. A prior hypertension registry study conducted in several primary care centers in the United Kingdom demonstrated the ability of a prior version of the DMO with no patient feedback (ie, digital medicines plus patch) to uncover a root cause for uncontrolled HTN in all participants after 2 weeks of use. Additionally, 37% of participants achieved BP control after 2 weeks with no adjustments to their antihypertensive medications [20].
In this study, patients with uncontrolled T2DM and HTN with current therapy were offered the DMO or usual care (to compare with the current standard that patients receive today). The design of the HTN registry was used to determine the duration of DMO use in this study; the first 2 weeks of DMO use allowed providers to understand the root cause for elevated BP (nonadherence, inadequate medication, or both) and the subsequent 2 weeks allowed the provider to see the effect of the medical decision on BP after the first 2 weeks [20]. The primary objective was to study the effect of the DMO on BP. Additional objectives were to assess the effect on glycemic and lipid control, engagement, and provider decision making.
Methods
Study Design and Participants
This 12-week, open-label, prospective, cluster-randomized, controlled, three-arm pilot study was executed at 13 outpatient primary care sites across California and Colorado. There were three additional sites that did not enroll any patients. Sites were selected based on the size of their HTN and T2DM population. Use of a cluster-randomized design mitigated the risk of investigator bias by ensuring providers cared for participants assigned to only one arm. Sites were randomized to the treatment arms: DMO use for 4 weeks (4-week DMO), DMO use for 12 weeks (12-week DMO), or usual care. Enrolled participants were assigned to the treatment arm of their clinical site.
Adults with uncontrolled HTN (systolic BP [SBP] ≥140 mm Hg) and T2DM (glycated hemoglobin A1c [HbA1c] ≥7%) who failed treatment with two or more antihypertensive medications available as part of the DMO medicine panel (Table 1) or dose-equivalent medicines from the same classes, and metformin and/or a sulfonylurea were eligible for enrollment. Participants either needed to be able to use a mobile phone or tablet or the investigator determined the participant could learn to use a smart mobile device. Investigators also assessed whether their participants could be treated for HTN during the study period using the DMO medication panel exclusively; if medically necessary, participants could be prescribed off-panel antihypertensive medicines. Exclusion criteria included body mass index (BMI) >40 kg/m2, skin sensitivity to adhesive medical tape or metals, active or chronic dermatitis, secondary causes for uncontrolled HTN or T2DM, evidence of hypertensive emergency, and use of insulin or other injectables to treat T2DM within the past year.
Table 1.
Digital medicine offering panel.a
| Therapeutic area and class | Medication | Doses | |
| Hypertension | |||
| Angiotensin-converting enzyme inhibitor | Lisinopril | 10 mg, 20 mg, 40 mg | |
| Angiotensin receptor blocker | Losartan | 100 mg | |
| Thiazide diuretic | HCTZ | 12.5 mg, 25 mg | |
| Dihydropyridine calcium channel blocker | Amlodipine | 5 mg | |
| Hypercholesterolemia | |||
| Statin | Atorvastatin | 20 mg | |
| Diabetes | |||
| Biguanide | Metformin | 500 mg | |
| Sulfonylurea | Glipizide | 5 mg | |
aParticipants could take more than one medication dose at any one time (eg, ingesting two atorvastatin 20 mg capsules to get a total dose of 40 mg).
Copernicus Group Independent Review Board, a central institutional review board, approved and monitored the study. Participants provided written informed consent prior to screening and were compensated (US $150 to US $525 based on study arm and site-specific guidelines for participant compensation) for participation.
During the study, changes were made to make the inclusion and exclusion criteria less restrictive to promote recruitment. Notably, we included a Spanish version of the consent form and removed an exclusion of non-English speakers.
Interventions
Investigators were instructed to make medication changes and to provide patient education and counseling as clinically appropriate (versus using specific dose-escalation protocols) to ensure the decisions were similar to those in a real clinical practice setting. Blood pressure recorded at each visit was the mean of two or more BP measurements obtained using the recommended measurement guidelines from the American Heart Association [22]. Participants had their BP measured after 5 or more minutes of rest, comfortably seated in a quiet room with their feet touching the floor. Each BP measurement was taken at least 1 minute apart. If the first two BP readings were more than 5 mm Hg different, then the BP was measured at least two more times; the mean of all BP values from one visit were used as the final reading. Laboratory test results were drawn at screening, and at weeks 4 and 12, for HbA1c (screening and week 12), fasting plasma glucose (FPG), total cholesterol, and directly measured low-density lipoprotein cholesterol (LDL-C). Participants also completed the 10-question Patient Activation Measure (PAM), a validated measure of patient activation that includes person’s beliefs, motivation, and actions for self-care at these visits [9,23,24]. During each visit, participants and investigators jointly reviewed the data and collaboratively set goals for medication adherence, physical activity, and rest.
Participants in the DMO arms were prescribed DMO for either 4 or 12 weeks and medicines co-encapsulated with ingestible sensors (see digital medicine panel in Table 1). Participants were allowed to switch to medications on the digital medicine panel in a dose-equivalent manner from the same drug classes. The DMO investigators were instructed to review DMO reports on the Web portal during study visits.
All investigators could titrate medications, provide patient education, and/or counseling at any time during the study as per usual care based on all available clinical data, with the exception that investigators in the DMO arms were instructed to await the DMO report from the first 2 weeks of DMO use before making changes to the antihypertensive medications (or other medical decision) to try to ensure this decision was made using the DMO data.
Providers trained participants on use of the DMO and, along with customer support provided by the sponsor, assisted participants in troubleshooting issues with the DMO.
Study Outcomes
The primary endpoint was change in SBP from baseline to week 4. Secondary endpoints included changes from baseline in SBP and HbA1c at week 12, changes in diastolic BP (DBP) and FPG at weeks 4 and 12, proportion of participants at BP goal (SBP <140 mm Hg and DBP <90 mm Hg) at weeks 4 and 12, medication adherence rate, and mean daily step count and duration of physical activity and rest (DMO only), and medical decisions. Exploratory outcomes included change in LDL-C from baseline at weeks 4 and 12 in patients using digital atorvastatin (DMO arms) or any statin (usual care) and change in PAM score.
Statistical Analysis
Target enrollment in this pilot study was 120 participants to ensure at least 90 evaluable participants at the end of the study. This study was primarily performed to understand the effect size of the DMO intervention. Although there was prior data from the hypertension registry study, the product and study design were different: participants in the hypertension registry study used a DMO without feedback for 2 weeks. It was hypothesized that with feedback to the participant and provider and a longer intervention, the effect size would be larger. Due to the pilot nature of the study, there were no a priori hypotheses for this study; P values are not reported on study outcome data. P values were only calculated for baseline differences between groups.
Values and change for continuous variables were summarized descriptively (mean and SE) and 95% confidence intervals (95% CI) were calculated for all changes. Differences between groups were calculated using a mixed-effects regression model that incorporated covariates found to be significant in the model: baseline value, gender, age (<65 years vs ≥65 years), and race (African American vs other). Proportions as well as differences between groups were summarized descriptively.
The SE was adjusted for cluster (study site) effects as well as the intracluster correlation coefficient (ICC) calculated using a one-way analysis of variance to adjust for any imbalances between and within clusters. Confidence intervals were calculated for differences between groups.
Participants with at least one follow-up BP were included in this modified intention-to-treat (ITT) analysis, which represented the minimal data needed for a pre/post comparison for each participant. Missing data were handled using last observation carried forward. Safety assessments were performed on all enrolled participants. Analyses were performed for 4-week DMO, 12-week DMO, and combined DMO (both DMO arms combined). Because both DMO groups had the same intervention for the first 4 weeks, the two groups were combined for all week 4 endpoints and measures (eg, mean medication adherence).
Medication adherence data and medical decisions (provider treatment decisions in response to DMO data) were summarized descriptively. Medication adherence was calculated only for the DMO users because measurement of medication adherence was an intrinsic aspect of the intervention.
Analyses of efficacy variables were performed on R version 3.2.2 with lme4 version 1.1.11 for building generalized linear mixed models. An interim analysis was performed in October 2015 to get preliminary data on the primary outcome.
Results
Between June and October 2015, 118 participants were enrolled across the 13 sites; 107 participants completed the week 4 visit and 105 completed the week 12 visit by December 30, 2015. Three usual care participants missed the week 4 visit, but were included in the analysis because they returned for the week 12 visit. One usual care site with five participants was not included in the final analysis over concern about violation of the cluster randomization. This usual care site was activated in September and was joined by the lead study coordinator from a 4-week DMO site previously activated in May; this study coordinator had intervened with both DMO and usual care participants. The final modified-ITT group included 109 participants (40 in 4-week DMO, 40 in 12-week DMO, and 29 in usual care) (Figure 2).
Figure 2.
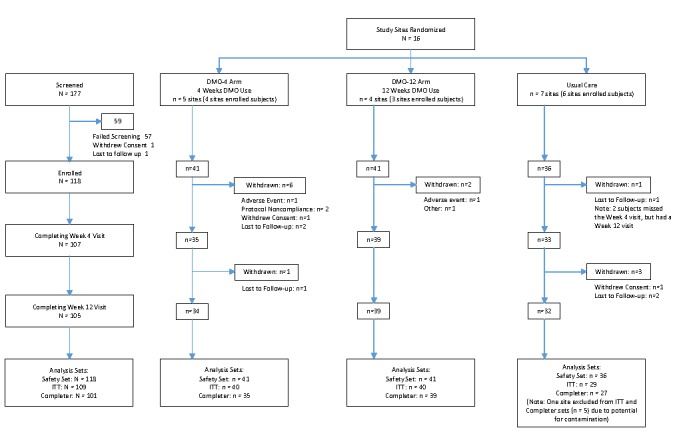
CONSORT flow diagram of participants.
The study included a large portion of low-income participants (56.9%, 62/109 earned ≤ US $20,000 per year) and minorities (52.3%, 57/109 Hispanics) (Table 2). In addition, 22.0% (24/109; 25%, [20/80] in DMO and 14%, [4/29] in usual care) had psychiatric comorbidities.
Table 2.
Demographics and baseline characteristics of participants (N=109).
| Parameter | 4-week DMO (n=40) | 12-week DMO (n=40) | Combined DMO (n=80) | Usual care (n=29) |
| Age (years), mean (SE) | 58.8 (1.4) | 56.7 (1.8) | 57.8 (1.1) | 61.6 (1.7) |
| Female, n (%) | 21 (53) | 24 (60) | 45 (56) | 10 (35) |
| African American, n (%) | 11 (28) | 3 (8) | 14 (18) | 3 (10) |
| Caucasian, n (%) | 29 (73) | 24 (60) | 53 (66) | 19 (66) |
| Asian, n (%) | 0 (0) | 13 (33) | 13 (16) | 2 (7) |
| Hispanic ethnicity (includes all races), n (%) | 22 (55) | 15 (38) | 37 (46) | 14 (45) |
| Income ≤ US$20,000, n (%) | 23 (58) | 21 (53) | 44 (55) | 18 (62) |
| Education <high school, n (%) | 18 (45) | 6 (15) | 24 (30) | 10 (34) |
| Employed, n (%) | 18 (45) | 24 (60) | 42 (53) | 9 (31) |
| Weight (kg), mean (SE) | 91.5 (5.9) | 85.7 (3.4) | 88.6 (3.3) | 89.7 (4.7) |
| BMI (kg/m2), mean (SE) | 32.8 (1.4) | 30.7 (0.9) | 31.8 (0.9) | 31.3 (1.0) |
| Systolic BP (mm Hg), mean (SE) | 152.2 (1.6) | 146.5 (0.8)a | 149.3 (1.5)a | 155.4 (3.0) |
| Diastolic BP (mm Hg), mean (SE) | 90.5 (2.8) | 82.0 (5.1) | 86.2 (3.2) | 83.9 (2.9) |
| HbA1c (%), mean (SE) | 8.8 (0.3) | 8.5 (0.2) | 8.7 (0.2) | 8.3 (0.4) |
| FPG (mg/dL), mean (SE) | 174.2 (13.6) | 191.4 (16.2) | 182.8 (9.9) | 165.0 (8.5) |
| LDL-C (mg/dL), mean (SE) | 110.7 (5.3) | 107.1 (6.6) | 108.9 (3.9) | 99.1 (6.2) |
| HDL-C (mg/dL), mean (SE) | 47.8 (2.6) | 45.2 (1.5) | 46.5 (1.4) | 40.6 (2.5) |
| Triglycerides (mg/dL), mean (SE) | 211.2 (28.1) | 195.7 (17.3) | 203.4 (16.2) | 226.1 (36.2) |
| Total cholesterol (mg/dL), mean (SE) | 190.2 (6.5) | 175.3 (6.0) | 182.8 (4.5) | 174.4 (13.2) |
aDifference compared to usual care was statistically significant (P<.05).
Primary Outcome
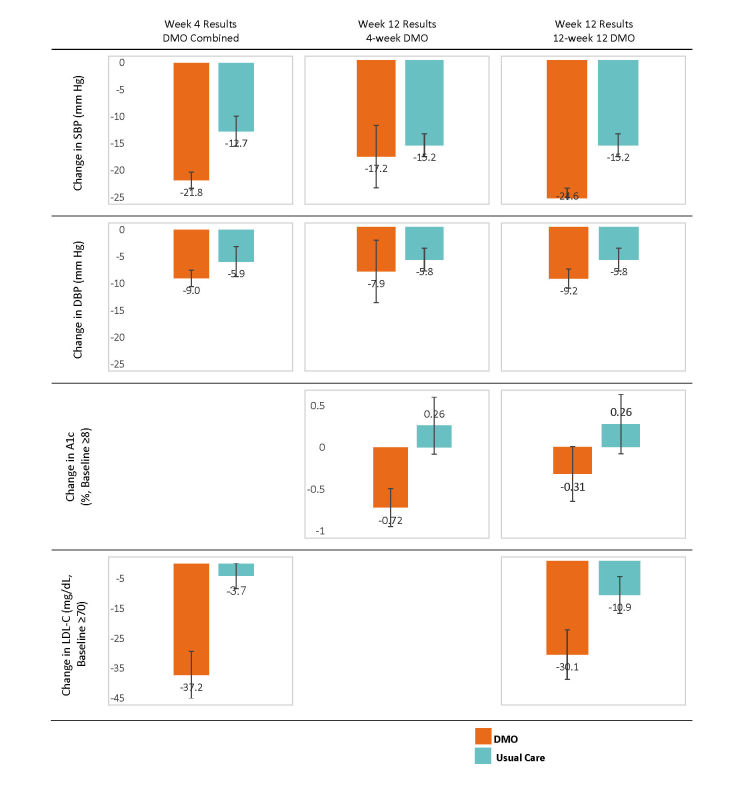
At week 4, combined DMO had a mean change in SBP from baseline of –21.8 (SE 1.5) mm Hg compared to –12.7 (SE 2.8) mm Hg for usual care (combined DMO–usual care: mean –9.1, SE 2.9, 95% CI –14.8 to –3.3 mm Hg; ICC=0; adjusted difference: mean –10.0, SE 3.1, 95% CI –16.1 to –3.9 mm Hg; effect size=0.69) (Figure 3). A sensitivity analysis showed that excluding the one usual care site did not impact the primary outcome; the change in SBP for usual care with the excluded site was mean –14.0 (SE 2.7; difference from combined DMO: –7.8, SE 2.8, 95% CI –13.3 to –2.3 mm Hg).
Figure 3.
Highlighted clinical results for changes in systolic and diastolic blood pressure (SBP and DPB), glycated hemoglobin (HbA1c), and low-density lipoprotein cholesterol (LDL-C) for the combined digital medicine offering (DMO) groups at week 4, week-4 DMO, and 12-week DMO. Error bars represent SE.
Secondary Outcomes
Hypertension
At week 4, a greater proportion of DMO participants achieved their BP goal (81%, 65/80) compared with usual care (33.3%, 9/27; mean difference 47.9%, SE 15.0%, 95% CI 18.5%-77.3%) (Table 3). DMO participants also had a greater reduction in DBP compared with usual care, but the results were not significant. The 12-week DMO group continued to show larger reductions in SBP from baseline (mean –24.6, SE 1.7 mm Hg), which was statistically larger compared to usual care (mean –15.2, SE 2.0 mm Hg; mean difference –9.4, SE 2.7, 95% CI –14.6 to –4.2 mm Hg). At week 12, 98% (39/40) of 12-week DMO participants achieved their BP goal compared with 51.7% of usual care participants (mean difference 45.8%, 95% CI 7.1% to 84.5%). The 4-week DMO group also had greater reductions in SBP and DBP at week 12 than usual care, but the results were not statistically significantly different (Table 4).
Table 3.
Summary of systolic and diastolic blood pressure (SBP and DBP), fasting plasma glucose (FPG), and glycated hemoglobin A1c (HbA1c) results for usual care and combined digital medicine offering (DMO).
| Outcome | Usual care | DMO (combined) | |||
| Value | Value | Difference,a
(95% CI) |
Adjusted difference,a
(95% CI) |
||
| SBP (mm Hg) | |||||
| Baseline, mean (SE) | 155.4 (3.0) | 149.3 (1.5) | |||
| Week 4, mean change (SE) | –12.7 (2.8) | –21.8 (1.5) | –9.1 (2.9); (–14.0, –3.3) |
–10.0 (3.1); (–16.1, –3.9) |
|
| Week 12, mean change (SE) | –15.2 (2.0) | –20.9 (3.4) | –4.6 (4.9); (–14.3, 5.1) |
–4.8 (5.6); (–15.8, 6.3) |
|
| DBP (mm Hg) | |||||
| Baseline, mean (SE) | 83.9 (2.9) | 86.2 (3.2) | |||
| Week 4, mean change (SE) | –5.9 (3.0) | –9.0 (1.6) | –3.4 (3.1); (–9.4, 2.7) |
–2.4 (1.9); (–6.2, 1.3) |
|
| Week 12, mean change (SE) | –5.8 (2.2) | –8.6 (2.2) | –2.4 (3.4); (–9.1, 4.4) |
–1.2 (3.4); (–7.2, 4.8) |
|
| Proportion at BP goal (%) | |||||
| Week 4, mean (SE) | 33.3 (9.7) | 81.2 (5.1) | 47.9 (15.0); (18.5, 77.3) |
N/Ab | |
| Week 12, mean (SE) | 51.7 (15.6) | 80.0 (9.3) | 28.3 (24.6); (–19.9, 76.5) |
N/Ab | |
| FPG (mg/dL) | |||||
| Baseline, mean (SE) | 165.0 (13.6) | 182.8 (9.9) | |||
| Week 4, mean change (SE) | 13.4 (15.8) | –9.4 (14.3) | –22.7 (22.0); (–66.7, 21.4) |
–14.4 (21.7); (–57.0, 28.3) |
|
| Week 12, mean change (SE) | 14.9 (12.0) | –4.9 (14.9) | –16.2 (22.1); (–59.5, 27.1) |
–12.6 (20.1); (–52.0, 26.9) |
|
| HbA1c (%) | |||||
| Baseline, mean (SE) | 8.28 (0.38) | 8.66 (0.18) | |||
| Week 12, mean change (SE) | 0.26 (0.35) | –0.19 (0.14) | –0.48 (0.29); (–1.04, 0.09) |
–0.54 (0.41); (–1.3, 0.3) |
|
| HbA1c baseline ≥8% (%)c | |||||
| Baseline, mean (SE) | 9.25 (0.31) | 9.54 (0.19) | |||
| Week 12, mean change (SE) | 0.26 (0.34) | –0.50 (0.20) | –0.77 (0.40); (–1.6, 0.02) |
–0.94 (0.45); (–1.8, –0.1) |
|
aDifference from usual care.
bN/A: Adjusted analysis was not performed.
cUsual care: n=15; DMO: n=50.
Table 4.
Summary of systolic and diastolic blood pressure (SBP and DBP), fasting plasma glucose (FPG), and glycated hemoglobin A1c (HbA1c) results for 4-week and 12-week digital medicine offering (DMO) groups.
| Outcome | 4-week DMO | 12-week DMO | |||||
| Value | Difference,a
(95% CI) |
Adjusted difference,a
(95% CI) |
Value | Difference,a
(95% CI) |
Adjusted difference,a
(95% CI) |
||
| SBP (mm Hg) | |||||||
| Baseline mean (SE) | 152.2 (1.6) | 146.4 (0.8) | |||||
| Week 4 mean change (SE) | –21.5 (2.5) | –8.8 (3.5); (–15.7, –1.9) |
–8.5 (3.8); (–15.8, –1.1) |
–22.1 (1.8) | –9.4 (2.9); (–15.1, –3.6) |
–11.3 (3.3); (–17.6, –4.9) |
|
| Week 12 mean change (SE) | –17.2 (5.6) | –1.1 (5.9); (–12.6, 10.4) |
–0.3 (6.2); (–12.5, 11.9) |
–24.6 (1.7) | –9.4 (2.7); (–14.6, –4.2) |
–11.0 (3.1); (–17.1, –4.9) |
|
| DBP (mm Hg) | |||||||
| Baseline mean (SE) | 90.5 (2.8) | 82.0 (5.1) | |||||
| Week 4 mean change (SE) | –10.1 (1.6) | –4.3 (3.1); (–10.5, 1.8) |
–1.6 (2.4); (–6.2, 3.0) |
–7.8 (3.9) | –2.1 (5.2); (–12.2, 8.0) |
–4.4 (2.5); (–9.4, 0.5) |
|
| Week 12 mean change (SE) | –7.9 (3.3) | –1.8 (4.0); (–9.7, 6.1) | 2.0 (4.0); (–4.6, 8.6) | –9.2 (3.6) | –3.1 (4.1); (–11.2, 4.9) | –5.9 (4.1); (–13.3, 1.5) | |
| Proportion at BP goal (%) | |||||||
| Week 4 mean (SE) | 72.5 (7.3) | 39.2 (12.5); (14.7, 63.7) |
N/Ab | 90.0 (6.7) | 56.7 (16.4); (24.6, 88.7) |
N/Ab | |
| Week 12 mean (SE) | 62.5 (9.3) | 10.8 (23.4); (–35.1, 56.6) |
N/Ab | 97.5 (2.5) | 45.8 (19.8); (7.1, 84.5) |
N/Ab | |
| FPG (mg/dL) | |||||||
| Baseline mean (SE) | 174.2 (13.6) | 191.4 (16.2) | |||||
| Week 4 mean change (SE) | 4.7 (9.6) | –10.3 (19.9); (–49.2, 28.6) |
–9.8 (23.5); (–56.0, 36.3) |
–22.8 (31.1) | –38.7 (32.0); (–101.4, 24.1) |
–15.9 (30.7); (–76.1, 44.3) |
|
| Week 12 mean change (SE) | 20.9 (9.2) | 6.8 (15.4); (–23.4, 37.0) |
–0.5 (17.3); (–34.4, 33.4) |
–28.9 (18.9) | –44.6 (21.8); (–87.4, –1.8) |
–26.3 (22.9); (–71.2, 18.7) |
|
| HbA1c(%) | |||||||
| Baseline mean (SE) | 8.79 (0.29) | 8.53 (0.20) | |||||
| Week 12 mean change (SE) | –0.32 (0.22) | –0.65 (0.44); (–1.52, 0.23) |
–0.63 (0.54); (–1.69, 0.43) |
–0.08 (0.22) | –0.35 (0.40); (–1.13, 0.42) |
–0.50 (0.67); (–1.81, 0.81) |
|
| HbA1cbaseline ≥8% (%)c | |||||||
| Baseline mean (SE) | 9.78 (0.30) | 9.29 (0.23) | |||||
| Week 12 mean change (SE) | –0.72 (0.23) | –0.98 (0.38); (–1.72, –0.24) |
–0.98 (0.45); (–1.86, –0.10) |
–0.31 (0.31) | –0.57 (0.49); (–1.53, 0.39) |
–0.98 (0.58); (–2.12, 0.16) |
|
aDifference from usual care.
bN/A: Adjusted analysis was not performed.
c4-week DMO: n=26; 12-week DMO: n=24.
Diabetes
At week 12, DMO had a nonsignificant difference in HbA1c reduction compared to usual care (4-week DMO: mean –0.32%, SE 0.22%; 12-week DMO: mean –0.08%, SE 0.22%; usual care: mean 0.28%, SE 0.35%). For participants with a baseline HbA1c of 8% of more (n=65; 4-week DMO: n=26, 12-week DMO: n=24, usual care group: n=15), both DMO groups showed larger HbA1c decreases (4-week DMO: mean –0.72%, SE 0.23%; 12-week DMO: mean –0.31%, SE 0.31%) compared to an increase in the HbA1c seen in the usual care group (mean 0.26%, SE 0.34%; difference from 4-week DMO 0.98%, 95% CI –1.72 to –0.24; difference from 12-week DMO –0.57%, 95% CI –1.53 to 0.39) (See Figure 3 and Table 3). Adjusted differences for the change in HbA1c between each DMO group and usual care were almost 1%. There were no significant differences in change in FPG between the DMO and usual care groups.
Medical Decisions
The DMO providers made approximately 3 times more medical decisions per participant (mean 6.5, SD 5.3 DMO vs mean 2.7, SD 3.3 usual care). The DMO participants received more counseling, patient education, and lifestyle coaching than usual care. The frequency of medication changes per participant was similar for DMO (mean 0.83, SD 1.49) and usual care (mean 1.00, SD 1.58). At week 4, DMO participants with uncontrolled BP, who were medication adherent (≥80%), appeared to be 4 times more likely than usual care participants to receive an antihypertensive titration. Although this suggests that greater targeting of therapy adjustments may occur in patients who utilize DMO, this finding should be interpreted with caution because the actual number of medication changes that occurred was small and the difference was not statistically significant.
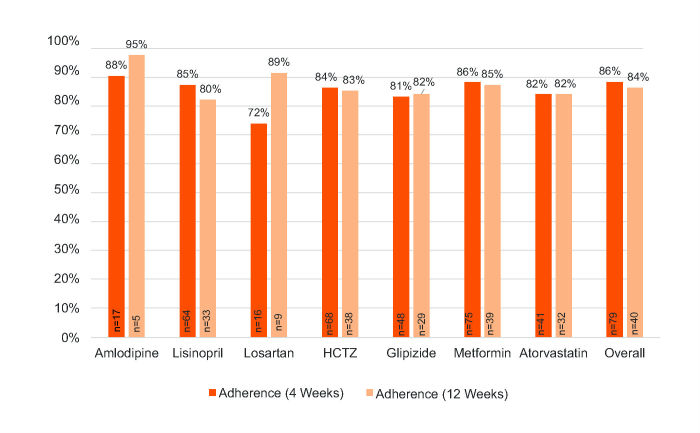
Digital Medicine Offering Measurements
The mean ingestion adherence was 86% during the first 4 weeks (combined DMO) and 84% for the entire 12 weeks (12-week DMO) (see Figure 4).
Figure 4.
Ingestion adherence for DMO subjects measured by DMO. Note adherence for the first 4 weeks includes both 4-week DMO and 12-week DMO; adherence for 12 weeks includes only 12-week DMO.
Exploratory Outcomes
Among statin users, reductions in LDL-C were larger for DMO compared with usual care. These differences were even greater in participants with a baseline LDL-C of 70 mg/dL or higher. In participants with baseline LDL-C of 70 mg/dL or higher (n=54; 4-week DMO: n=6, 12-week DMO: n=28, usual care group: n=20), changes in LDL-C were mean –37.2 (SE 7.9) mg/dL at week 4 and mean –30.1 (SE 8.0) mg/dL at week 12 for DMO and mean –4.0 (4.3) mg/dL at week 4 and mean –10.9 (SE 5.9) mg/dL at week 12 for usual care. The differences in change in LDL-C between DMO and the usual care group were –33.2 (95% CI –50.6 to –15.8) at week 4 and –19.2 (95% CI –36.4 to –2.0) at week 12. These differences were statistically significant (see Table 5 for complete results).
Table 5.
Summary of total cholesterol and low-density lipoprotein cholesterol (LDL-C) outcomes for the combined digital medicine offering (DMO) group only.a
| Outcome | Usual care | DMO (combined) | |||
| Value | Value | Difference,b
(95% CI) |
Adjusted difference,b
(95% CI) |
||
| Total cholesterol (mg/dL)c | |||||
| Baseline, mean (SE) | 174.4 (13.1) | 177.4 (9.5) | |||
| Week 4, mean change (SE) | –9.2 (7.1) | –34.8 (7.1) | –25.7 (9.7); (–44.6, –6.7) |
–23.0 (7.8); (–38.2, –7.8) |
|
| Week 12, mean change (SE) | –21.9 (10.2) | –29.5 (7.4) | –7.9 (11.3); (–30.1, 14.3) |
–8.1 (7.9); (–23, 7) |
|
| LDL-C (mg/dL)c | |||||
| Baseline, mean (SE) | 99.3 (6.7) | 103.9 (10.1) | |||
| Week 4, mean change (SE) | –3.7 (3.8) | –29.7 (9.4) | –25.6 (9.4); (–44.1, –7.1) |
–22.7 (6.1); (–34.6, –10.8) |
|
| Week 12, mean change (SE) | –9.5 (5.6) | –21.3 (10.0) | –11.0 (13); (–37.4, 15.4) |
–10.8 (6.3); (–23.1, 1.5) |
|
| Total cholesterol with baseline LDL ≥70 mg/dL (mg/dL)d | |||||
| Baseline, mean (SE) | 174.1 (11.6) | 185.1 (8.4) | |||
| Week 4, mean change (SE) | –7.0 (6.9) | –39.8 (7.9) | –32.9 (10.2); (–52.9, –12.9) |
–26.5 (9.1); (–44.4, –8.6) |
|
| Week 12, mean change (SE) | –18.9 (9.4) | –37.7 ± 7.5 | –18.8 ± 10.6; (–39.6, 2.0) |
–13.9 ± 8.8; (–31.2, 3.3) |
|
| LDL-C with baseline LDL ≥70 mg/dL (mg/dL)d | |||||
| Baseline, mean (SE) | 104.2 (7.0) | 114.0 (7.1) | |||
| Week 4, mean change (SE) | –4.0 (4.3) | –37.2 (7.9) | –33.2 (8.9); (–50.6, –15.8) |
–25.3 (7.0); (–39.1, –11.6) |
|
| Week 12, mean change (SE) | –10.9 (5.9) | –30.1 (8.0) | –19.2 (8.9); (–36.4, –2.0) |
–13.4 (7.1); (–27.4, 0.5) |
|
aDue to small sample sizes for DMO groups, results are summarized.
bDifference from usual care.
cIncludes participants on any statin therapy in usual care (n=23) and on digital atorvastatin in the DMO group (n=41).
dIncludes participants on statin therapy in usual care (n=20) and on digital atorvastatin in the DMO group (n=34).
The DMO participants had a nonsignificantly greater increase in PAM score compared with usual care; the changes were mean 7.9 (SE 3.8) for 4-week DMO, mean 7.9 (SE 3.0) for 12-week DMO, and mean 1.7 (SE 3.3) for usual care at week 12 (see Table 6).
Table 6.
Summary of Patient Activation Measure (PAM) outcomes.
| Outcome | Usual care | DMO (combined) | 4-week DMO | 12-week DMO | |||
| Value | Value | Difference,a
(95% CI) |
Value | Difference,a
(95% CI) |
Value | Difference,a
(95% CI) |
|
| Baseline, mean (SE) | 70.3 (5.1) | 70.6 (2.8) | 73.4 (4.7) | 68.0 (2.8) | |||
| Week 4, mean change (SE) | –0.9 (1.6) | 2.2 (1.9) | 3.2 (3.6); (–3.9, 10.2) |
2.1 (3.1) | 3.0 (4.0); (–5, 11) |
2.3 (2.4) | 3.3 (3.4); (–3.4, 9.9) |
| Week 12, mean change (SE) | 1.7 (3.3) | 7.9 (2.4) | 6.2 (4.6); (–2.8, 15.2) |
7.9 (3.8) | 6.2 (5.3); (–4, 17) |
7.9 (3.0) | 6.3 (4.7); (–2.9, 15.4) |
aDifference from usual care.
Participant Satisfaction With Digital Medicine Offering
In general, participants agreed the DMO was easy to learn (92%, 69/75) and to incorporate in their daily routine (91%, 68/75), and that using the data was useful to manage (91%, 68/75) and improved their health (93%, 70/75) and that sharing their data with their provider helped them to understand their care plan (91%, 68/75). Most (81%, 61/75) did not mind wearing the patch (see Table 7).
Table 7.
Satisfaction survey results (N=75).
| Survey question | Answered agree or strongly agree, n (%) |
| It was easy to use Proteus in my daily routine | 68 (91) |
| It was easy to learn how to use Proteus | 69 (92) |
| Seeing my data showed me how well I’m managing my health | 68 (91) |
| Seeing my data motivated me to improve my health | 70 (93) |
| Proteus helped me have more helpful conversations with my health care professionals | 64 (85) |
| Sharing my data with my health care professionals helped me understand my care plan | 68 (91) |
| Using Proteus improved my experience of health care service for my condition(s) | 66 (88) |
| Proteus helped me to see how I use my medication(s) from day-to-day | 66 (88) |
| Proteus helped me take my medication(s) more regularly | 68 (91) |
| It was easy to use the iPad | 67 (89) |
| It was easy to use the Proteus app | 64 (85) |
| In general, I did not mind wearing the patch | 61 (81) |
| Connecting and applying each new patch was easy for me to do | 68 (91) |
Safety
There were 32 of 82 DMO participants (39%) who reported 59 adverse events (AEs), of which 33 were unrelated to the DMO; 8 of 36 usual care participants (22%) reported 17 AEs. There were no serious AEs related to the DMO or the study. There were 14 device-related AEs in 11 participants, most commonly mild skin reactions to the wearable sensor (13 events in 10 participants, 12%). Additionally, 12 participants reported study medication-related AEs (14 events total) with gastrointestinal AEs (9 events in 8 participants; 7 mild, 2 moderate, 1 moderate event led to study withdrawal, 10%) being the most common. Another AE, fatigue (mild intensity), unrelated to the device or study medication, led to study withdrawal.
Discussion
In this study, participants with uncontrolled HTN and T2DM who used the DMO had significantly greater reductions in SBP within 4 weeks than the usual care group (9 mm Hg greater reduction), which was maintained at 12 weeks with a significantly greater proportion of patients achieving their BP goal. Participants using the DMO also showed lower trends in HbA1c (as much as a 1% greater reduction), and LDL-C (33 mg/dL greater reduction) compared to participants who received usual clinical care. These clinical findings were maintained in analyses adjusting for age, gender, race, and baseline clinical parameters. Use of the DMO was also safe; the frequency of skin reactions is generally lower than published research on adhesive tape and patches [25-28].
These findings are relevant in the care of T2DM patients who have an increased risk of serious cardiovascular and microvascular complications. Each 2 mm Hg reduction in SBP or 1 mm Hg reduction in DBP has been associated with lowering mortality from stroke and ischemic heart disease by 10% and 7%, respectively [29]. A reduction in HbA1c of 0.5% or more is considered clinically significant to reduce the risk of microvascular complications [30,31]. Statin adherence, as evidenced by LDL-C reduction, has also been associated with improved outcomes in diabetes patients [29,32,33]. However, given the short duration of this pilot study, additional longer-term evidence will be necessary to demonstrate that the changes in BP, HbA1c, and LDL are durable.
We hypothesize that improved clinical outcomes with the DMO were related in part to improved self-care (medication adherence and patient activation). In the literature, average adherence to chronic medicines is approximately 50%; participants using DMO achieved a mean adherence of 86% during the first 4 weeks. The DMO also had a greater increase in PAM scores; a 1-point increase in PAM score is associated with a 1.8% increased likelihood of decreasing HbA1c to less than 8% [9].
Providers could make more targeted and timely therapy optimization decisions using the objective behavioral data reported by the DMO. We found that at week 4, for participants with uncontrolled BP, investigators in the DMO arm were more likely to make therapy adjustments or give adherence counseling and/or education guided by the DMO data compared to usual care participants.
Other digital health solutions have failed to demonstrate benefit. Bloss et al [34] failed to demonstrate benefits of digital health interventions (telemonitoring devices for BP, blood glucose, or electrocardiogram rhythm) compared to usual care in a large controlled study. In that study, no instructions were given to providers on use of the device data; this has been shown to make blood glucose monitoring less effective in non-insulin-using diabetes patients [30,34]. There were also confounders. For example, many participants with diabetes in the control arm used insulin and likely made insulin-titration decisions based on blood glucose results. Finally, the inclusion criteria were based on cost versus level of disease control and may have enrolled participants not needing additional interventions.
In contrast, a recent study demonstrated benefits of a pharmacist case management intervention to reduce BP using a telemonitoring BP device [35]. Participants in the intervention arm spoke with pharmacists (via the phone) who reviewed BP data, provided coaching, and titrated medications. The intervention group had a statistically greater reduction in SBP at 6 months than usual care (mean difference –10.7, 95% CI –14.3 to –7.3 mm Hg), similar to the reductions in SBP observed in our pilot study on the DMO, except the pharmacist case management study only addressed hypertension, whereas this DMO study evaluated patients with both uncontrolled HTN and T2DM.
There were several limitations to this study. This study had a small sample size and included only 13 sites, which likely contributed to discrepancies noted in participant demographic and baseline characteristics. As mentioned in the Methods, this was a pilot study to measure the effect size of the DMO on SBP. The adjusted analyses suggested that these baseline differences did not affect the outcomes. However, they may have still affected the results for BP at goal. The small sample size may have also contributed to lack of power to detect differences between groups for some of the secondary and exploratory outcomes. In order to demonstrate use of the DMO in the real-world primary care clinic workflow, ambulatory BP monitoring was not used; therefore, BP fluctuations may be potentially related to the context of in-clinic measurement (outside of the participant’s natural context). A comparison of adherence to treatment was not included among the goals of this study. No objective assessment of adherence to treatment was attempted in the usual care arm because there are only indirect methods of measuring adherence as an alternative to DMO and none of these methods have been established to be inherently reliable or accurate. Therefore, we cannot conclude that DMO led to higher levels of medication adherence. However, measuring an improvement in adherence was not an objective of the study.
Despite these limitations, this study demonstrates positive evidence that a digital health offering that measures and promotes medication adherence, patient self-care, and provider engagement can help patients improve their level of BP and diabetes control. The results should be generalizable given the diversity of the study population. Reducing BP, HbA1c, and LDL-C in a consistent manner over a longer term through the use of DMO-like approaches may help patients decrease their overall risk for complications. Future real-world evidence can build on these results to further elucidate longer-term outcomes.
Acknowledgments
We thank all the study participants, study coordinators, and site investigators involved in this study. We are also gratefully acknowledge INC Research (Raleigh, NC) who was compensated for their efforts for management and coordination of the study, protocol and statistical analysis plan development, creation of the case report forms, data management, and part of the statistical analysis. Finally, we thank Penjit Moorhead, MS, and Maxsim Gibiansky, PhD, employees of Proteus Digital Health, for providing the bulk of the statistical analysis. This study was funded and supported by the sponsor, Proteus Digital Health.
Abbreviations
- AE
adverse event
- BP
blood pressure
- DBP
diastolic blood pressure
- DMO
digital medicine offering
- FPG
fasting plasma glucose
- HbA1c
glycated hemoglobin A1c
- HTN
hypertension
- ICC
intracluster correlation coefficient
- ITT
intention-to-treat
- LDL-C
low-density lipoprotein cholesterol
- PAM
Patient Activation Measure
- T2DM
type 2 diabetes mellitus
Footnotes
Authors' Contributions: NV and YK had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. All authors contributed to the study concept and design, critically revised the manuscript for important intellectual content, and supervised the conduct of the study. JF, NV, PR, and YK contributed to the acquisition, analysis, or interpretation of the data. JF, NV, and PR drafted the manuscript. YK oversaw the statistical analysis. NV, PR, YK, and GS obtained funding. NV and PR provided administrative, technical, or material support.
Conflicts of Interest: The sponsor, Proteus Digital Health, had a role in the design and conduct of the study; analysis and interpretation of the data; preparation, review, and approval of the manuscript; and decision to submit the manuscript for publication. The sponsor had no role in the collection or management of the study. JF reports consulting relationship with Proteus Digital Health, Johnson & Johnson, AstraZeneca, CeQur, and Sanofi. He also reports receiving study grants from Abbvie, Amgen, AstraZeneca, Boehringer Ingelheim, Bristol-Myers Squibb, Eli Lilly, Johnson & Johnson, Merck, Novo Nordisk, Pfizer, and Sanofi. NV, PR, YK, and GS are employed by Proteus Digital Health. GS is also a cofounder, officer, and stock owner of Proteus Digital Health. LO reports a consulting relationship with Proteus Digital Health; his contribution to this publication was as a paid consultant and was not part of his Stanford University duties or responsibilities.
References
- 1.Centers for Disease Control and Prevention (CDC) Vital signs: prevalence, treatment, and control of hypertension--United States, 1999-2002 and 2005-2008. MMWR Morb Mortal Wkly Rep. 2011 Feb 04;60(4):103–108. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6004a4.htm. [PubMed] [Google Scholar]
- 2.Menke A, Casagrande S, Geiss L, Cowie CC. Prevalence of and trends in diabetes among adults in the United States, 1988-2012. JAMA. 2015 Sep 08;314(10):1021–1029. doi: 10.1001/jama.2015.10029. [DOI] [PubMed] [Google Scholar]
- 3.American Diabetes Association Cardiovascular disease and risk management. Diabetes Care. 2017 Jan;40(Suppl 1):S75–S87. doi: 10.2337/dc17-S012. [DOI] [PubMed] [Google Scholar]
- 4.Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, de Ferranti SD, Floyd J, Fornage M, Gillespie C, Isasi CR, Jiménez MC, Jordan LC, Judd SE, Lackland D, Lichtman JH, Lisabeth L, Liu S, Longenecker CT, Mackey RH, Matsushita K, Mozaffarian D, Mussolino ME, Nasir K, Neumar RW, Palaniappan L, Pandey DK, Thiagarajan RR, Reeves MJ, Ritchey M, Rodriguez CJ, Roth GA, Rosamond WD, Sasson C, Towfighi A, Tsao CW, Turner MB, Virani SS, Voeks JH, Willey JZ, Wilkins JT, Wu JH, Alger HM, Wong SS, Muntner P, American Heart Association Statistics Committee Stroke Statistics Subcommittee Heart disease and stroke statistics-2017 update: a report from the American Heart Association. Circulation. 2017 Mar 07;135(10):e146–e603. doi: 10.1161/CIR.0000000000000485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup K, Ezekowitz MD, Finkelstein EA, Hong Y, Johnston SC, Khera A, Lloyd-Jones DM, Nelson SA, Nichol G, Orenstein D, Wilson PW, Woo YJ, American Heart Association Advocacy Coordinating Committee. Stroke C, Council on Cardiovascular Radiology and Intervention. Council on Clinical Cardiology. Council OE, Council OA, Thrombosis and Vascular Biology. Council OC, Critical C, Perioperative and Resuscitation. Council on Cardiovascular Nursing. Council on the Kidney in Cardiovascular Disease. Council on Cardiovascular Surgery and Anesthesia. Interdisciplinary Council on Quality of Care and Outcomes Research Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011 Mar 1;123(8):933–944. doi: 10.1161/CIR.0b013e31820a55f5. http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=21262990. [DOI] [PubMed] [Google Scholar]
- 6.Egan BM, Li J, Qanungo S, Wolfman TE. Blood pressure and cholesterol control in hypertensive hypercholesterolemic patients: national health and nutrition examination surveys 1988-2010. Circulation. 2013 Jul 02;128(1):29–41. doi: 10.1161/CIRCULATIONAHA.112.000500. http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=23817481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Selvin E, Parrinello CM, Sacks DB, Coresh J. Trends in prevalence and control of diabetes in the United States, 1988-1994 and 1999-2010. Ann Intern Med. 2014 Apr 15;160(8):517–525. doi: 10.7326/M13-2411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sabaté E. Adherence to Long-Term Therapies: Evidence for Action. Geneva: World Health Organization; 2003. http://apps.who.int/iris/bitstream/10665/42682/1/9241545992.pdf . [Google Scholar]
- 9.Remmers C, Hibbard J, Mosen DM, Wagenfield M, Hoye RE, Jones C. Is patient activation associated with future health outcomes and healthcare utilization among patients with diabetes? J Ambul Care Manage. 2009;32(4):320–327. doi: 10.1097/JAC.0b013e3181ba6e77. [DOI] [PubMed] [Google Scholar]
- 10.Lebeau J, Cadwallader J, Aubin-Auger I, Mercier A, Pasquet T, Rusch E, Hendrickx K, Vermeire E. The concept and definition of therapeutic inertia in hypertension in primary care: a qualitative systematic review. BMC Fam Pract. 2014 Jul 02;15:130. doi: 10.1186/1471-2296-15-130. https://bmcfampract.biomedcentral.com/articles/10.1186/1471-2296-15-130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee WC, Balu S, Cobden D, Joshi AV, Pashos CL. Prevalence and economic consequences of medication adherence in diabetes: a systematic literature review. Manag Care Interface. 2006 Jul;19(7):31–41. [PubMed] [Google Scholar]
- 12.Balkrishnan R, Rajagopalan R, Camacho FT, Huston SA, Murray FT, Anderson RT. Predictors of medication adherence and associated health care costs in an older population with type 2 diabetes mellitus: a longitudinal cohort study. Clin Ther. 2003 Nov;25(11):2958–2971. doi: 10.1016/s0149-2918(03)80347-8. [DOI] [PubMed] [Google Scholar]
- 13.New England Healthcare Institute Thinking Outside the Pillbox: A System-Wide Approach to Improving Patient Medication Adherence for Chronic Disease. 2009. Aug, http://www.nehi.net/writable/publication_files/file/pa_issue_brief_final.pdf .
- 14.Zullig LL, Peterson ED, Bosworth HB. Ingredients of successful interventions to improve medication adherence. JAMA. 2013 Dec 25;310(24):2611–2612. doi: 10.1001/jama.2013.282818. [DOI] [PubMed] [Google Scholar]
- 15.Kahneman D. Thinking Fast And Slow. New York: Farrar, Straus, and Giroux; 2011. [Google Scholar]
- 16.Au-Yeung KY, Moon GD, Robertson TL, Dicarlo LA, Epstein MS, Weis SE, Reves RR, Engel G. Early clinical experience with networked system for promoting patient self-management. Am J Manag Care. 2011;17(7):e277–e287. http://www.ajmc.com/pubMed.php?pii=50238. [PubMed] [Google Scholar]
- 17.Belknap R, Weis S, Brookens A, Au-Yeung KY, Moon G, DiCarlo L, Reves R. Feasibility of an ingestible sensor-based system for monitoring adherence to tuberculosis therapy. PLoS One. 2013;8(1):e53373. doi: 10.1371/journal.pone.0053373. http://dx.plos.org/10.1371/journal.pone.0053373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Eisenberger U, Wüthrich RP, Bock A, Ambühl P, Steiger J, Intondi A, Kuranoff S, Maier T, Green D, DiCarlo L, Feutren G, De GS. Medication adherence assessment: high accuracy of the new Ingestible Sensor System in kidney transplants. Transplantation. 2013 Aug 15;96(3):245–250. doi: 10.1097/TP.0b013e31829b7571. http://europepmc.org/abstract/MED/23823651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kane JM, Perlis RH, DiCarlo LA, Au-Yeung K, Duong J, Petrides G. First experience with a wireless system incorporating physiologic assessments and direct confirmation of digital tablet ingestions in ambulatory patients with schizophrenia or bipolar disorder. J Clin Psychiatry. 2013 Jun;74(6):e533–e540. doi: 10.4088/JCP.12m08222. [DOI] [PubMed] [Google Scholar]
- 20.Naik R, Macey N, West RJ, Godbehere P, Thurston SC, Fox R, Xiang W, Kim Y, Singh I, Leadley S, DiCarlo L. First use of an ingestible sensor to manage uncontrolled blood pressure in primary practice: the UK Hypertension Registry. J Community Med Health Educ. 2017;7(1):1–5. doi: 10.4172/2161-0711.1000506. [DOI] [Google Scholar]
- 21.Godbehere P, Wareing P. Hypertension assessment and management: role for digital medicine. J Clin Hypertens (Greenwich) 2014 Mar;16(3):235. doi: 10.1111/jch.12246. doi: 10.1111/jch.12246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, Jones DW, Kurtz T, Sheps SG, Roccella EJ, Subcommittee of ProfessionalPublic Education of the American Heart Association Council on High Blood Pressure Research Recommendations for blood pressure measurement in humans and experimental animals: Part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Hypertension. 2005 Jan;45(1):142–161. doi: 10.1161/01.HYP.0000150859.47929.8e. http://hyper.ahajournals.org/cgi/pmidlookup?view=long&pmid=15611362. [DOI] [PubMed] [Google Scholar]
- 23.Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res. 2004 Aug;39(4 Pt 1):1005–1026. doi: 10.1111/j.1475-6773.2004.00269.x. http://europepmc.org/abstract/MED/15230939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hibbard JH, Greene J, Overton V. Patients with lower activation associated with higher costs; delivery systems should know their patients' 'scores'. Health Aff (Millwood) 2013 Feb;32(2):216–222. doi: 10.1377/hlthaff.2012.1064. [DOI] [PubMed] [Google Scholar]
- 25.Heinemann L, Krinelke L. Insulin infusion set: the Achilles heel of continuous subcutaneous insulin infusion. J Diabetes Sci Technol. 2012 Jul 01;6(4):954–964. doi: 10.1177/193229681200600429. http://europepmc.org/abstract/MED/22920824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hurt RD, Lauger GG, Offord KP, Kottke TE, Dale LC. Nicotine-replacement therapy with use of a transdermal nicotine patch--a randomized double-blind placebo-controlled trial. Mayo Clin Proc. 1990 Dec;65(12):1529–1537. doi: 10.1016/s0025-6196(12)62186-7. [DOI] [PubMed] [Google Scholar]
- 27.Lindley EM, Milligan K, Farmer R, Burger EL, Patel VV. Patient-controlled transdermal fentanyl versus intravenous morphine pump after spine surgery. Orthopedics. 2015 Sep;38(9):e819–e824. doi: 10.3928/01477447-20150902-61. [DOI] [PubMed] [Google Scholar]
- 28.Suwanmalee O, Taneepanichskul S. A clinical study of transdermal contraceptive patch in Thai women. J Med Assoc Thai. 2006 Oct;89 Suppl 4:S1–S4. [PubMed] [Google Scholar]
- 29.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R, Prospective SC. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002 Dec 14;360(9349):1903–1913. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 30.Clar C, Barnard K, Cummins E, Royle P, Waugh N, Aberdeen Health Technology Assessment Group Self-monitoring of blood glucose in type 2 diabetes: systematic review. Health Technol Assess. 2010 Mar;14(12):1–140. doi: 10.3310/hta14120. doi: 10.3310/hta14120. [DOI] [PubMed] [Google Scholar]
- 31.Chrvala CA, Sherr D, Lipman RD. Diabetes self-management education for adults with type 2 diabetes mellitus: A systematic review of the effect on glycemic control. Patient Educ Couns. 2016 Dec;99(6):926–943. doi: 10.1016/j.pec.2015.11.003. https://linkinghub.elsevier.com/retrieve/pii/S0738-3991(15)30116-6. [DOI] [PubMed] [Google Scholar]
- 32.Farsaei S, Sabzghabaee AM, Amini M, Zargarzadeh AH. Adherence to statin therapy in patients with type 2 diabetes: An important dilemma. J Res Med Sci. 2015 Feb;20(2):109–114. http://www.jmsjournal.net/article.asp?issn=1735-1995;year=2015;volume=20;issue=2;spage=109;epage=114;aulast=Farsaei. [PMC free article] [PubMed] [Google Scholar]
- 33.Writing Committee. Lloyd-Jones DM, Morris PB, Ballantyne CM, Birtcher KK, Daly DD, DePalma SM, Minissian MB, Orringer CE, Smith SC. 2016 ACC expert consensus decision pathway on the role of non-statin therapies for LDL-cholesterol lowering in the management of atherosclerotic cardiovascular disease risk: a report of the American College of Cardiology Task Force on Clinical Expert Consensus Documents. J Am Coll Cardiol. 2016 Jul 05;68(1):92–125. doi: 10.1016/j.jacc.2016.03.519. [DOI] [PubMed] [Google Scholar]
- 34.Bloss CS, Wineinger NE, Peters M, Boeldt DL, Ariniello L, Kim JY, Sheard J, Komatireddy R, Barrett P, Topol EJ. A prospective randomized trial examining health care utilization in individuals using multiple smartphone-enabled biosensors. PeerJ. 2016;4:e1554. doi: 10.7717/peerj.1554. doi: 10.7717/peerj.1554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Margolis KL, Asche SE, Bergdall AR, Dehmer SP, Groen SE, Kadrmas HM, Kerby TJ, Klotzle KJ, Maciosek MV, Michels RD, O'Connor PJ, Pritchard RA, Sekenski JL, Sperl-Hillen JM, Trower NK. Effect of home blood pressure telemonitoring and pharmacist management on blood pressure control: a cluster randomized clinical trial. JAMA. 2013 Jul 3;310(1):46–56. doi: 10.1001/jama.2013.6549. http://europepmc.org/abstract/MED/23821088. [DOI] [PMC free article] [PubMed] [Google Scholar]