ABSTRACT
AxyXY-OprZ is an RND-type efflux system that confers innate aminoglycoside resistance to Achromobacter spp. We investigated here a putative TetR family transcriptional regulator encoded by the axyZ gene located upstream of axyXY-oprZ. An in-frame axyZ gene deletion assay led to increased MICs of antibiotic substrates of the efflux system, including aminoglycosides, cefepime, fluoroquinolones, tetracyclines, and erythromycin, indicating that the product of axyZ negatively regulates expression of axyXY-oprZ. Moreover, we identified an amino acid substitution at position 29 of AxyZ (V29G) in a clinical Achromobacter strain that occurred during the course of chronic respiratory tract colonization in a cystic fibrosis (CF) patient. This substitution, also detected in three other strains exposed in vitro to tobramycin, led to an increase in the axyY transcription level (5- to 17-fold) together with an increase in antibiotic resistance level. This overproduction of AxyXY-OprZ is the first description of antibiotic resistance acquisition due to modification of a chromosomally encoded mechanism in Achromobacter and might have an impact on the management of infected CF patients. Indeed, tobramycin is widely used for aerosol therapy within this population, and we have demonstrated that it easily selects mutants with increased MICs of not only aminoglycosides but also fluoroquinolones, cefepime, and tetracyclines.
KEYWORDS: Achromobacter, AxyZ, AxyXY-OprZ, tobramycin, cystic fibrosis, efflux
INTRODUCTION
Achromobacter spp. belong to the Gram-negative nonfermenters respiratory pathogens that are emerging in cystic fibrosis (CF) patients (1). The Achromobacter genus includes 18 species: A. xylosoxidans (2); A. piechaudii and A. ruhlandii (3); A. denitrificans (4), A. spanius, and A. insolitus (5); A. marplatensis (6); A. animicus, A. mucicolens, and A. pulmonis (7, 8); A. insuavis, A. aegrifaciens, A. anxifer, and A. dolens (9); A. agilis, A. pestifer, A. kerstersii, and A. deleyi (10). The most prevalent species in CF are A. xylosoxidans, A. ruhlandii, and A. insuavis (11, 12). The pathogenic role of Achromobacter in CF remains unclear, but during the course of chronic lung infection, it might cause a level of inflammation similar to caused by Pseudomonas aeruginosa (13). Some guidelines suggest that patients chronically infected with Achromobacter or patients with clinical degradation should be treated (14). Nevertheless, Achromobacter displays not only innate but also frequently acquired multidrug resistance, particularly in the case of chronic colonization, making treatment a real challenge (15). The mechanisms of acquired resistance are unknown; only a few β-lactamase-encoding genes located on mobile genetic elements have been reported thus far (16–20).
Two resistance-nodulation-cell division (RND)-type efflux systems have been described to date in Achromobacter and contribute to its intrinsic antibiotic resistance: AxyABM and AxyXY-OprZ (21, 22). The latter system is encoded by three chromosomal genes: axyX, axyY, and oprZ. The first gene encodes the membrane fusion protein, the second encodes the RND pump, and the third encodes the outer membrane protein. AxyXY-OprZ is responsible for the innate high-level aminoglycoside (AG) resistance of the Achromobacter species that are the most prevalent in CF patient airways (23). The antibiotic substrate range of AxyXY-OprZ is wide and includes, in addition to AG, cefepime, fluoroquinolones, tetracyclines, and, to a lesser extent, carbapenems, ceftazidime, and erythromycin. Several of these antibiotics (ceftazidime, carbapenems, ciprofloxacin, tobramycin, and amikacin) are major compounds commonly used to treat pulmonary infections in CF patients (14).
AxyX and AxyY are orthologs of the well-described MexX and MexY in Pseudomonas aeruginosa (24). AxyXY-OprZ and MexXY/OprM share a similar antibiotic substrate range. It has been demonstrated that MexXY/OprM plays an important role in multidrug resistance acquisition in P. aeruginosa, particularly in CF patients (25, 26). Its expression level is controlled by multiple pathways, including local and global regulatory factors (27, 28). Among these factors the local repressor MexZ that belongs to the TetR family has been widely studied (29). Various mutations have been described within the mexZ gene as well as within the intergenic sequence between mexZ and mexX (25, 30). mexZ mutations lead to overexpression of mexXY and an increase in the MICs of antibiotic substrates (31). It has been demonstrated that mutations in mexZ can be selected by exposure of P. aeruginosa to AG (30). In addition, MexZ activity is downregulated in the presence of ribosome inhibitor antibiotics (32, 33).
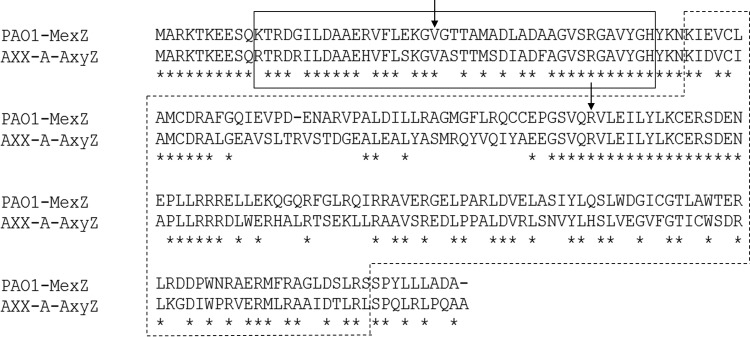
We have previously described upstream of axyXY-oprZ and in an inverted orientation an open reading frame, named axyZ, encoding a putative TetR family transcription repressor (22). AxyZ shares 59% amino acid similarity with MexZ of P. aeruginosa (Fig. 1). In the present study, we examined the role of axyZ in the expression of axyXY-oprZ. Furthermore, we looked for axyZ mutations in CF isolates that acquired antibiotic resistance during chronic colonization and in laboratory mutants selected by tobramycin exposure. Finally, we tested the inducibility of axyXY-oprZ by doxycycline and tobramycin, which are ribosome-targeting antibiotics.
FIG 1.
Alignment of MexZ of Pseudomonas aeruginosa (PAO1 strain) and AxyZ of Achromobacter insuavis (AXX-A strain) (Clustal Omega). The area boxed with the solid line delimits the DNA-binding domain, and the area boxed with the dashed line delimits the C-terminal domain (41). Amino acid sequence similarity was as follows: overall, 59%; DNA-binding domain, 76%; C-terminal domain, 51%. Stars indicate identical residue positions; arrows indicate positions of substitutions detected in laboratory mutants, i.e., valine at position 29 and arginine at position 105.
RESULTS
Consequences of in-frame axyZ gene deletion.
In the AXX-A strain with a deletion of axyZ (AXX-A-ΔZ) the MICs of all antibiotic substrates of AxyXY-OprZ except for carbapenems and ceftazidime were increased (Table 1). MICs of antibiotics were from 1.3-fold to more than 10-fold higher in the AXX-A-ΔZ strain than in AXX-A. In addition, the level of axyY expression was 9.18-fold higher in AXX-A-ΔZ than in AXX-A (mean value from five independent experiments with a coefficient of variation of 0.43) (Table 2).
TABLE 1.
MICs of AxyXY-OprZ antibiotic substrates for Achromobacter isolates and their mutants
| Drug | MIC (μg/ml)a |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| AXX-A | AXX-A-ΔZ | ACH-CF-490 | ACH-CF-911 | CIP-102236 | CIP-102236V29G | CIP-102236R105S | ACH-NCF-39 | ACH-NCF-39V29G | ACH-CF-842 | ACH-CF-842V29G | |
| Tobramycin | 16 | 128 (8) | 32 | 64 (2) | 32 | 256 (8) | >256 (>8) | 24 | 96 (4) | 8 | 32 (4) |
| Amikacin | 256 | >256 | ≥256 | >256 | >256 | >256 | >256 | 192 | >256 (>1.3) | 32 | >256 (>8) |
| Gentamicin | 48 | >256 (>5.3) | 48 | 256 (5.3) | 192 | >256 (>1.3) | >256 (>1.3) | 48 | >256 (>5.3) | 12 | ≥256 (≥21) |
| Netilmicin | 24 | >256 (>10.7) | 64 | ≥256 (≥4) | >256 | >256 | >256 | 64 | >256 (>4) | 16 | >256 (>16) |
| Ceftazidime | 4 | 4 | 4 | 4 | 1.5 | 4 (2.6) | 3 (2) | 1.5 | 3 (2) | 1.5 | 1.5 |
| Cefepime | 16 | 128 (8) | 192 | >256 (>1.3) | 48 | >256 (>5.3) | >256 (>5.3) | 24 | >256 (>10) | 8 | 32 (4) |
| Imipenem | 1 | 1 | 2 | 4 (2) | 2 | 2 | 2 | 6 | 8 (1.3) | 2 | 4 (2) |
| Meropenem | 0.064 | 0.064 | 0.064 | 6 (94) | 0.094 | 0.125 (1.3) | 0.125 (1.3) | 0.094 | 0.125 (1.3) | 0.75 | 0.75 |
| Doripenem | 0.25 | 0.25 | 0.25 | 2 (8) | 0.38 | 0.5 (1.3) | 0.5 (1.3) | 0.25 | 0.38 (1.5) | 1 | 1 |
| Ofloxacin | 2 | 12 (6) | ≥32 | >32 | 16 | >32 (>2) | >32 (>2) | 6 | >32 (>5.3) | 24 | >32 (>1.3) |
| Levofloxacin | 1 | 4 (4) | 3 | >32 (>10) | 3 | 12 (4) | 32 (>10) | 1.5 | 6 (4) | 4 | 8 (2) |
| Ciprofloxacin | 0.75 | 2 (2.6) | 1.5 | >32 (>21) | 2 | 8 (4) | >32 (>16) | 1.5 | 8 (5.3) | 2 | 6 (3) |
| Tetracycline | 48 | 64 (1.3) | 192 | >256 (>1.3) | 96 | 128 (1.3) | >256 (>2.7) | 192 | ≥256 (≥1.3) | 48 | 192 (4) |
| Doxycycline | 8 | 12 (1.5) | 24 | 96 (4) | 12 | 16 (1.3) | 32 (2.7) | 16 | 24 (1.5) | 6 | 8 (1.3) |
| Tigecycline | 4 | 8 (2) | 3 | 3 | 2 | 2 | 3 (1.5) | 1.5 | 2 (1.3) | 0.38 | 0.5 (1.3) |
| Erythromycin | 128 | 256 (2) | 192 | >256 (>1.3) | 96 | >256 (>2.7) | >256 (>2.7) | 32 | 128 (4) | >256 | >256 |
Values in parentheses represent relative MIC increases (ratio of the MIC for the mutant isolate to the MIC for the original isolate).
TABLE 2.
Relative expression levels of axyY genes in mutant versus parental strains
| Parental strain | Mutant | Relative axyY expression (CV)a |
|---|---|---|
| AXX-A | AXX-A-ΔZ | 9.18 (0.43) |
| ACH-CF-490 | ACH-CF-911 | 4.98 (0.39) |
| CIP-102236 | CIP-102236V29G | 5.17 (0.37) |
| CIP-102236 | CIP-102236R105S | 9.16 (0.1) |
| ACH-NCF-39 | ACH-NCF-39V29G | 17.32 (0.44) |
| ACH-CF-842 | ACH-CF-842V29G | 6.44 (0.33) |
Fold increase in the mutant compared to the level in the parental strain. CV, coefficient of variation.
axyZ sequencing in clinical isolates.
Two mutations were detected in strain ACH-CF-911 compared to the sequence of ACH-CF-490. The first one occurred in the axyZ-axyX intergenic sequence (G → A substitution at nucleotide position 169 upstream of the start codon of axyZ). The second one, which occurred within axyZ (86T → G), was a nonsynonymous substitution, exchanging a valine for a glycine at amino acid position 29 of AxyZ (V29G). From 2004 (isolation year of ACH-CF-490) to 2012 (isolation year of ACH-CF-911), we collected successively 13 isogenic isolates from this patient and sequenced the axyZ genes. Substitution V29G has been found in 11 out of the 13 isolates, with the first one being isolated in 2007.
For the other pairs of clinical isolates, we did not detect any mutation in either axyZ or the axyZ-axyX intergenic sequence when we compared the sequence of the second isolate to that of the first.
axyZ mutation assays (laboratory mutants).
One-step mutants were obtained for CIP-102236, ACH-NCF-39, and ACH-CF-842 on medium containing tobramycin concentrations ranging from 2× to 8× the MIC of the parental strains. Mutation frequency was approximately 10−7. axyZ was sequenced in all the mutants that harbored increased resistance to antibiotic substrates of AxyXY-OprZ.
In some mutants for which the antibiotic MICs were increased, no mutation was detected. Nevertheless, in other mutants we detected two amino acid substitutions within AxyZ that were stable after successive subcultures (Fig. 1). The first one, R105S, was encountered in a single mutant, obtained from CIP-102236, and it was named CIP-102236R105S. Interestingly, the second one, V29G (already detected in the clinical isolate ACH-CF-911) was found in several mutants, named CIP-102236V29G, ACH-NCF-39V29G, and ACH-CF-842V29G. MICs of aminoglycosides, cefepime, fluoroquinolones, tetracyclines, and erythromycin were higher in R105S and V29G mutants than in parental strains (Table 1). The increase in the MICs was similar to that observed between the AXX-A and AXX-A-ΔZ strains. MICs of ceftazidime, meropenem, and doripenem were slightly increased in three of the four mutants.
Relative gene expression measurement of axyY.
axyY relative transcript levels in AXX-CF-911, CIP-102236V29G, CIP-102236R105S, ACH-NCF-39V29G, and ACH-CF-842V29G were, respectively, 4.98-, 5.17-, 9.16-, 17.32-, and 6.44-fold higher than in parental strains. Use of either the rpsL or rpoD housekeeping gene led to similar results. Furthermore, interexperiment reproducibility showed that using reverse transcription-quantitative PCR (RT-qPCR) with the present protocol is a robust method for measuring gene expression levels in Achromobacter.
Induction assay by ribosome-targeting antibiotics.
axyY expression was increased (6.52-fold) in AXX-A after exposure to doxycycline (1 μg/ml). Exposure to tobramycin led to increased axyY expression depending on the drug concentration: 1.86-fold for 4 μg/ml, 5.93-fold for 8 μg/ml, and 6.35-fold for 16 μg/ml.
DISCUSSION
In the present work we have confirmed that axyZ encodes a transcriptional repressor of axyXY-oprZ. Indeed, in-frame axyZ gene deletion experiments led to an increased transcript level of axyY as well as increased MICs of antibiotic substrates of AxyXY-OprZ. Two types of mutants of axyZ were obtained by tobramycin exposure. The substitution V29G that resulted in overexpression of axyXY-oprZ is particularly interesting. Indeed, it has been detected in not only a clinical isolate but also three laboratory mutants. On the one hand, these clinical and laboratory mutants displayed an antibiotic resistance evolution similar to that observed between AXX-A and AXX-A-ΔZ. On the other hand, all mutants overexpressed axyY. It is likely that the V29G substitution alters AxyZ, preventing the repression of axyXY-oprZ. It is noteworthy that most of the mutations reported in mexZ of P. aeruginosa occur either in the DNA-binding domain or in the C-terminal domain (28, 34). Position 29 in MexZ belongs to the DNA-binding domain of MexZ (Fig. 1). Furthermore, comparison of amino acid sequences of AxyZ from A. insuavis AXX-A, MexZ from P. aeruginosa PAO1, and AmrR (ortholog of MexZ) from Burkholderia pseudomallei 1026b (35) revealed that valine at position 29 is a conserved residue, suggesting its probable importance in the function of the members of the TetR family.
In some laboratory mutants selected on tobramycin, we did not detect any mutation in either axyZ or the axyZ-axyX intergenic sequence, whereas these genes harbored increased resistance levels to AxyXY-OprZ antibiotic substrates. Moreover, the increase of axyY expression was variable among the V29G mutants (5- to 17-fold higher than in parental strains). These observations strongly suggest that axyXY-oprZ expression depends on not only axyZ but also other regulatory pathways, as previously described in P. aeruginosa (27). Among them, the PA5471 gene indirectly activates mexXY by repressing mexZ when bacteria are exposed to antibiotics that target the ribosome (33). We observed that axyY expression was induced in AXX-A in the presence of subinhibitory concentrations of doxycycline or tobramycin. An ortholog of the PA5471 gene is present in most of the Achromobacter published genomes but, surprisingly, not in that of AXX-A. The adaptation of efflux expression in response to antibiotic exposure probably results from multiple regulatory mechanisms.
As exposure to tobramycin can induce mutations in axyZ, one might wonder about potential consequences of AG therapy among CF patients. Indeed, analysis of medical data of a patient chronically colonized by the resistant mutant ACH-CF-911 revealed that the patient received tobramycin aerosol therapy on two occasions, in 2005 and 2008. Although the first mutant isolate had been detected after the first tobramycin cure, we could not correlate the mutation event with tobramycin treatment because the patient also received other, different, antibiotics. Therefore, further studies should be conducted on a larger number of clinical isolates from patients treated or not by AG. We observed that the V29G substitution is stable in vivo. Indeed, it has been detected in all isolates obtained from 2007 to 2012. In some cases, mutant and nonmutant isogenic subpopulations coexisted in the respiratory airways.
In conclusion, our results strongly suggest that axyZ encodes the local negative regulator of axyXY-oprZ in Achromobacter spp. Some stable mutations in axyZ that can be selected by tobramycin led to overexpression of the efflux system and increased MICs of aminoglycosides, fluoroquinolones, cefepime, and tetracyclines. The prevalence of this mechanism in clinical isolates and the potential role of tobramycin aerosol therapy in selecting resistant mutants have to be studied.
MATERIALS AND METHODS
Bacterial strains.
Achromobacter species strains used in this work are listed and described in Table 3. Species-level identifications were performed by nrdA sequencing (11).
TABLE 3.
Isolates used in the study
| Isolate | Species | Origin | axyZ application |
|---|---|---|---|
| AXX-A | A. insuavis | Ear discharge | Inactivation |
| ACH-CF-490, ACH-CF-911a | A. xylosoxidans | CF sputum | Sequencing |
| CIP-102236 | A. xylosoxidans | Sputum | Mutation assays |
| ACH-NCF-39 | A. xylosoxidans | Catheter insertion site | Mutation assays |
| ACH-CF-842 | A. xylosoxidans | CF sputum | Mutation assays |
Isogenic isolates.
The AXX-A strain, initially assigned to the species A. xylosoxidans, was reclassified as A. insuavis when the multilocus sequence typing (MLST) identification scheme for Achromobacter was published (9, 23, 36). AXX-A has been used in previous studies to characterize AxyABM and AxyXY-OprZ RND-type efflux systems (21, 22). It was used in the present work to examine the role of axyZ in the expression of axyXY-oprZ by gene deletion.
Five pairs of Achromobacter isolates from CF sputum samples (four pairs of A. xylosoxidans and one pair of A. insuavis) from five different patients were included. Each pair of Achromobacter isolates of the CF sputum samples had the following characteristics: both isolates were recovered from the same patient at different periods (interval ranging from 5 to 11 years), they shared the same pulsed-field gel electrophoresis profile (isogenic isolates [data not shown]), and the second isolate of each pair harbored antibiotic resistance levels higher than those of the first one, indicating resistance acquisition during chronic colonization.
Three other A. xylosoxidans strains were included for axyZ mutation assays: CIP-102236 from the Institut Pasteur collection, ACH-NCF-39 recovered from a catheter insertion site skin swab, and ACH-CF-842 from a CF patient sputum sample.
This study was performed in accordance with the principles of good clinical practice and the need for ethics committee approval was waived.
MICs determinations.
MICs of tobramycin, amikacin, gentamicin, netilmicin, ceftazidime, cefepime, imipenem, meropenem, doripenem, ofloxacin, levofloxacin, ciprofloxacin, tetracycline, doxycycline, tigecycline, and erythromycin were measured by the Etest method (bioMérieux) as recommended by the manufacturer and as previously described (21, 22). Mueller-Hinton agar plates (Mueller-Hinton E medium; bioMérieux) were inoculated by swabbing the surfaces of the plates with a bacterial suspension adjusted to a 0.5 McFarland turbidity standard, and MICs were recorded after a 24-h incubation at 37°C.
Bacterial DNA preparation, amplification, and sequencing of axyZ.
Bacterial DNA templates were prepared by heat lysis of cells. A bacterial suspension in 300 μl of distilled water was boiled for 10 min and then centrifuged (10,000 × g for 5 min). The supernatant was used as the DNA template. The axyZ-flanking degenerate primers axyZ-F and axyZ-R (Table 4) were designed for sequencing the whole axyZ gene as well as the axyZ-axyX intergenic sequence. PCR was carried out in reaction mixtures containing deoxynucleoside triphosphates (dNTP; 0.2 mM), axyZ-F and axyZ-R primers (0.25 μM each), Taq polymerase (2.5 U; Fermentas) with the supplied buffer, MgCl2 (1.5 mM), dimethyl sulfoxide (5%, vol/vol), and DNA template (1 μl), adjusted with water to a final volume of 50 μl. The cycling parameters were 94°C for 10 min, followed by 30 cycles of 94°C for 60 s, 60°C for 90 s, and 72°C for 90 s, with a final step at 72°C for 10 min. PCR products were purified with a Millipore centrifugal filter unit (Amicon Microcon PCR kit; Millipore). Double-strand sequencing was performed using BigDye, version 1.1, Terminator chemistry and a 3130XL genetic analyzer (Applied Biosystems).
TABLE 4.
Primers used in this study
| Primer | Nucleotide sequence (5′–3′)a |
|---|---|
| axyZ-F | ATGCGCTTGGACAGYGACGA |
| axyZ-R | CGGATRCGARTGCGAGCGTT |
| Screen-deltaAxyZ-F | TTGGAAGGAATATGGCAACG |
| Screen-deltaAxyZ-R | ACGTAGATCGGGTCGAGTTG |
| Seq-deltaAxyZ-1 | CCCTCAAGCAACTCGAAGC |
| Seq-deltaAxyZ-2 | GCTTCGAGTTGCTTGAGGG |
| Seq-deltaAxyZ-3 | CGCCAGCATACTTTTGAACA |
| Seq-deltaAxyZ-4 | TGTTCAAAAGTATGCTGGCG |
| axyY-qPCR-F3 | TGTATTCGGTCAACGGCTTC |
| axyY-qPCR-R4 | GCGCGAACACCATCAGGTT |
| rpsl-qPCR-1F | ACGCACTTTGGCAACCTTAC |
| rpsl-qPCR-1R | GCGAAGTCAGCATCATCAAA |
| rpoD-qPCR-F1 | AAGGACGGCTACAAGTCGGA |
| rpoD-qPCR-R1 | GCCAGCTTCTCGACCATCTT |
The nucleotide base code for degenerate primers is as follows: Y is C or T; R is A or G.
In-frame axyZ gene deletion.
An in-frame axyZ gene deletion in AXX-A was constructed as previously described (27, 37). A DNA fragment of the 700 nucleotides upstream of the axyZ gene and the 700 nucleotides downstream of axyZ were synthesized (GeneArt; Thermo Fisher Scientific). This fragment was cloned into the pKNG101 vector in Escherichia coli CC118 λpir. The recombinant plasmid pINA-axyZ was transferred into AXX-A by conjugation using the helper strain E. coli HB101 that contains the pRK2013 vector. Recombinant AXX-A strains were selected on Pseudomonas isolation agar containing 5 mg/ml streptomycin and cultivated on Luria-Bertani (LB) agar containing 5% sucrose in order to force the recombination event leading to gene deletion. The deletion was confirmed by sequencing (primers Screen-deltaAxyZ-F, Screen-deltaAxyZ-R, Seq-deltaAxyZ-1, Seq-deltaAxyZ-2, Seq-deltaAxyZ-3, and Seq-deltaAxyZ-4) (Table 4). The knockout clone was named AXX-A-ΔZ.
Selection of one-step mutants.
CIP-102236, ACH-NCF-39, and ACH-CF-842 were grown by plating 100 μl of a bacterial suspension adjusted to a 0.5 McFarland turbidity standard on Mueller-Hinton agar containing tobramycin at concentrations of 2×, 4×, 8×, and 16× the MIC of each strain. Such concentrations were previously chosen by Islam et al. and by Westbrock-Wadman et al. to select Pseudomonas aeruginosa aminoglycoside-resistant mutants that overexpressed mexXY (30, 38). Plates were incubated for 48 to 72 h at 37°C. For each mutant we performed antibiotic susceptibility testing and compared the profile of the mutant to that of the parental strain. In the case of acquired resistance, the whole axyZ gene was sequenced.
Relative gene expression measurement of axyY.
The transcript level of axyY was determined by RT-qPCR as follows.
(i) RNA extraction.
Strains were inoculated into Luria-Bertani broth (10 g/liter tryptone [Difco Laboratories], 5 g/liter yeast extract [Oxoid], and 10 g/liter sodium chloride [VWR]) at 37°C overnight and subcultured in 20 ml of LB broth at 37°C with shaking until mid-exponential phase (optical density at 600 nm [OD600] of 1 to 1.2). Culture (0.5 ml) was added to 1 ml of RNAprotect bacteria reagent (Qiagen), bacterial cells were pelleted (5,000 × g, 10 min), and total RNA was extracted using an RNeasy minikit (Qiagen) according to the manufacturer's instructions and eluted twice in 30 μl of RNase-free water. Residual genomic DNA was removed by 10 units of DNase treatment (RQ1 RNase-Free DNase; Promega) for 30 min at 37°C. RNA was purified by ethanol (2 volumes) and sodium acetate (1/10 volume) precipitation. RNA concentration was determined using a NanoDrop ND-1000 spectrophotometer (Thermo Scientific).
(ii) Reverse transcription.
One microgram of RNA was used for total cDNA synthesis using an ImProm-II reverse transcription system (Promega) with the random hexamer primer protocol. A control without reverse transcriptase was performed and then included in the PCR step to ensure total genomic DNA removal. Aliquots of serial dilutions in DNA-free water (1:10, 1:100, and 1:1,000) of each cDNA were conserved at −20°C until use in the PCR experiment.
(iii) Quantitative PCR.
qPCRs were performed on a LightCycler 2.0 instrument (Roche) in reaction mixtures containing 4 μl of LightCycler FastStart DNA Master Plus SYBR green I master mix (Roche), forward and reverse primers (0.5 μM each), and cDNA (1 μl), adjusted with DNase-free water to a final volume of 20 μl. The cycling parameters were the following: 95°C for 10 min (denaturation); 40 cycles of 95°C for 10 s, 56°C for 10 s, and 72°C for 20 s (amplification, single fluorescence acquisition mode); 64°C to 95°C with a heating slope of 0.1°C per s (melting curve, continuous fluorescence acquisition mode); and a final cooling step at 40°C for 30 s. Primers were designed in conserved sequences of the three targeted genes: axyY and two reference housekeeping genes, rpsL and rpoD. rpsL, which encodes a ribosomal protein, is commonly used for measurement of relative gene expression in P. aeruginosa (25). In the absence of any available data about a gene expression measurement method in Achromobacter, it was necessary to confirm our results by using another housekeeping gene. For this purpose, we chose rpoD, encoding one of the sigma factors that confer promoter-specific transcription initiation on RNA polymerase (39). All the PCRs targeting axyY, rpsL, and rpoD of each mutant and the respective parental strain were performed in duplicate within the same qPCR experiment, and each experiment was repeated at least twice (from two independently RNA extractions). Each qPCR experiment included 1:10, 1:100, and 1:1,000 cDNA dilutions of the parental strain in order to calculate the real-time PCR efficiency of each targeted gene. For calculating relative expression, we used the method described by Pfaffl (40).
Induction assay by ribosome-targeting antibiotics.
We performed induction assays of axyXY-oprZ in AXX-A by cultivating the strain in the presence of subinhibitory concentrations of doxycycline (1 μg/ml) or tobramycin (4, 8, and 16 μg/ml), followed by measurement of the axyY expression level by RT-qPCR.
Accession number(s).
Nucleotide sequences of the axyZ genes in the following strains have been submitted to the GenBank under the indicated accession numbers: ACH-CF-490, KY630178; ACH-CF-911, KY630179; CIP-102236, KY630180; CIP-102236V29G, KY630181; CIP-102236R105S, KY630182; ACH-NCF-39, KY630183; ACH-NCF-39V29G, KY630184; ACH-CF-842, KY630185; ACH-CF-842V29G, KY630186.
REFERENCES
- 1.Parkins MD, Floto RA. 2015. Emerging bacterial pathogens and changing concepts of bacterial pathogenesis in cystic fibrosis. J Cyst Fibros 14:293–304. doi: 10.1016/j.jcf.2015.03.012. [DOI] [PubMed] [Google Scholar]
- 2.Yabuuchi E, Oyama A. 1971. Achromobacter xylosoxidans n. sp. from human ear discharge. Jpn J Microbiol 15:477–481. doi: 10.1111/j.1348-0421.1971.tb00607.x. [DOI] [PubMed] [Google Scholar]
- 3.Yabuuchi E, Kawamura Y, Kosako Y, Ezaki T. 1998. Emendation of genus Achromobacter and Achromobacter xylosoxidans (Yabuuchi and Yano) and proposal of Achromobacter ruhlandii (Packer and Vishniac) comb. nov., Achromobacter piechaudii (Kiredjian et al.) comb. nov., and Achromobacter xylosoxidans subsp. denitrificans (Rüger and Tan) comb. nov. Microbiol Immunol 42:429–438. doi: 10.1111/j.1348-0421.1998.tb02306.x. [DOI] [PubMed] [Google Scholar]
- 4.Coenye T, Vancanneyt M, Cnockaert MC, Falsen E, Swings J, Vandamme P. 2003. Kerstersia gyiorum gen. nov., sp. nov., a novel Alcaligenes faecalis-like organism isolated from human clinical samples, and reclassification of Alcaligenes denitrificans Rüger and Tan 1983 as Achromobacter denitrificans comb. nov. Int J Syst Evol Microbiol 53:1825–1831. doi: 10.1099/ijs.0.02609-0. [DOI] [PubMed] [Google Scholar]
- 5.Coenye T, Vancanneyt M, Falsen E, Swings J, Vandamme P. 2003. Achromobacter insolitus sp. nov. and Achromobacter spanius sp. nov., from human clinical samples. Int J Syst Evol Microbiol 53:1819–1824. doi: 10.1099/ijs.0.02698-0. [DOI] [PubMed] [Google Scholar]
- 6.Gomila M, Tvrzová L, Teshim A, Sedláček I, González-Escalona N, Zdráhal Z, Šedo O, González JF, Bennasar A, Moore ERB, Lalucat J, Murialdo SE. 2011. Achromobacter marplatensis sp. nov., isolated from a pentachlorophenol-contaminated soil. Int J Syst Evol Microbiol 61:2231–2237. doi: 10.1099/ijs.0.025304-0. [DOI] [PubMed] [Google Scholar]
- 7.Vandamme P, Moore ER, Cnockaert M, De Brandt E, Svensson-Stadler L, Houf K, Spilker T, LiPuma JJ. 2013. Achromobacter animicus sp. nov., Achromobacter mucicolens sp. nov., Achromobacter pulmonis sp. nov and Achromobacter spiritinus sp. nov., from human clinical samples. Syst Appl Microbiol 36:1–10. doi: 10.1016/j.syapm.2012.10.003. [DOI] [PubMed] [Google Scholar]
- 8.Vandamme PA, Peeters C, Cnockaert M, Gomila M, Moore ERB, Spilker T, LiPuma JJ. 2016. Reclassification of Achromobacter spiritinus Vandamme et al. 2013 as a later heterotypic synonym of Achromobacter marplatensis Gomila et al. Int J Syst Evol Microbiol 66:1641–1644. doi: 10.1099/ijsem.0.000872. [DOI] [PubMed] [Google Scholar]
- 9.Vandamme P, Moore ER, Cnockaert M, Peeters C, Svensson-Stadler L, Houf K, Spilker T, LiPuma JJ. 2013. Classification of Achromobacter genogroups 2, 5, 7 and 14 as Achromobacter insuavis sp. nov., Achromobacter aegrifaciens sp. nov., Achromobacter anxifer sp. nov. and Achromobacter dolens sp. nov., respectively. Syst Appl Microbiol 36:474–482. doi: 10.1016/j.syapm.2013.06.005. [DOI] [PubMed] [Google Scholar]
- 10.Vandamme PA, Peeters C, Inganäs E, Cnockaert M, Houf K, Spilker T, Moore ER, LiPuma JJ. 2016. Taxonomic dissection of Achromobacter denitrificans Coenye et al. 2003 and proposal of Achromobacter agilis sp. nov., nom. rev., Achromobacter pestifer sp. nov., nom. rev., Achromobacter kerstersii sp. nov and Achromobacter deleyi sp. nov. Int J Syst Evol Microbiol 66:3708–3717. doi: 10.1099/ijsem.0.001254. [DOI] [PubMed] [Google Scholar]
- 11.Spilker T, Vandamme P, LiPuma JJ. 2013. Identification and distribution of Achromobacter species in cystic fibrosis. J Cyst Fibros 12:298–301. doi: 10.1016/j.jcf.2012.10.002. [DOI] [PubMed] [Google Scholar]
- 12.Amoureux L, Bador J, Bounoua Zouak F, Chapuis A, de Curraize C, Neuwirth C. 2016. Distribution of the species of Achromobacter in a French Cystic Fibrosis Centre and multilocus sequence typing analysis reveal the predominance of A. xylosoxidans and clonal relationships between some clinical and environmental isolates. J Cyst Fibros 15:486–494. doi: 10.1016/j.jcf.2015.12.009. [DOI] [PubMed] [Google Scholar]
- 13.Hansen CR, Pressler T, Nielsen KG, Jensen PØ, Bjarnsholt T, Høiby N. 2010. Inflammation in Achromobacter xylosoxidans infected cystic fibrosis patients. J Cyst Fibros 9:51–58. doi: 10.1016/j.jcf.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 14.UK Cystic Fibrosis Trust Antibiotic Working Group. 2009. Antibiotic treatment for cystic fibrosis, 3rd ed Cystic Fibrosis Trust, London, United Kingdom. [Google Scholar]
- 15.Amoureux L, Bador J, Siebor E, Taillefumier N, Fanton A, Neuwirth C. 2013. Epidemiology and resistance of Achromobacter xylosoxidans from cystic fibrosis patients in Dijon, Burgundy: first French data. J Cyst Fibros 12:170–176. doi: 10.1016/j.jcf.2012.08.005. [DOI] [PubMed] [Google Scholar]
- 16.Levesque R, Roy PH. 1982. Mapping of the plasmid (pLQ3) from Achromobacter and cloning of its cephalosporinase gene in Escherichia coli. Gene 18:69–75. doi: 10.1016/0378-1119(82)90057-9. [DOI] [PubMed] [Google Scholar]
- 17.Riccio ML, Pallecchi L, Fontana R, Rossolini GM. 2001. In70 of plasmid pAX22, a blaVIM-1-containing integron carrying a new aminoglycoside phosphotransferase gene cassette. Antimicrob Agents Chemother 45:1249–1253. doi: 10.1128/AAC.45.4.1249-1253.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sofianou D, Markogiannakis A, Metzidie E, Pournaras S, Tsakris A. 2005. VIM-2 metallo-beta-lactamase in Achromobacter xylosoxidans in Europe. Eur J Clin Microbiol Infect Dis 24:854–855. doi: 10.1007/s10096-005-0054-2. [DOI] [PubMed] [Google Scholar]
- 19.Yamamoto M, Nagao M, Hotta G, Matsumura Y, Matsushima A, Ito Y, Takakura S, Ichiyama S. 2012. Molecular characterization of IMP-type metallo-β-lactamases among multidrug-resistant Achromobacter xylosoxidans. J Antimicrob Chemother 67:2110–2113. doi: 10.1093/jac/dks179. [DOI] [PubMed] [Google Scholar]
- 20.Neuwirth C, Freby C, Ogier-Desserrey A, Perez-Martin S, Houzel A, Péchinot A, Duez J-M, Huet F, Siebor E. 2006. VEB-1 in Achromobacter xylosoxidans from cystic fibrosis patient, France. Emerg Infect Dis 12:1737–1739. doi: 10.3201/eid1211.060143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bador J, Amoureux L, Duez J-M, Drabowicz A, Siebor E, Llanes C, Neuwirth C. 2011. First description of an RND-type multidrug efflux pump in Achromobacter xylosoxidans, AxyABM. Antimicrob Agents Chemother 55:4912–4914. doi: 10.1128/AAC.00341-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bador J, Amoureux L, Blanc E, Neuwirth C. 2013. Innate aminoglycoside resistance of Achromobacter xylosoxidans is due to AxyXY-OprZ, an RND-type multidrug efflux pump. Antimicrob Agents Chemother 57:603–605. doi: 10.1128/AAC.01243-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bador J, Neuwirth C, Liszczynski P, Mézier M-C, Chrétiennot M, Grenot E, Chapuis A, de Curraize C, Amoureux L. 2016. Distribution of innate efflux-mediated aminoglycoside resistance among different Achromobacter species. New Microbes New Infect 10:1–5. doi: 10.1016/j.nmni.2015.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Morita Y, Tomida J, Kawamura Y. 2012. MexXY multidrug efflux system of Pseudomonas aeruginosa. Front Microbiol 3:408. doi: 10.3389/fmicb.2012.00408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Llanes C, Hocquet D, Vogne C, Benali-Baitich D, Neuwirth C, Plésiat P. 2004. Clinical strains of Pseudomonas aeruginosa overproducing MexAB-OprM and MexXY efflux pumps simultaneously. Antimicrob Agents Chemother 48:1797–1802. doi: 10.1128/AAC.48.5.1797-1802.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vogne C, Aires JR, Bailly C, Hocquet D, Plesiat P. 2004. Role of the multidrug efflux system MexXY in the emergence of moderate resistance to aminoglycosides among Pseudomonas aeruginosa isolates from patients with cystic fibrosis. Antimicrob Agents Chemother 48:1676–1680. doi: 10.1128/AAC.48.5.1676-1680.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Muller C, Plesiat P, Jeannot K. 2011. A two-component regulatory system interconnects resistance to polymyxins, aminoglycosides, fluoroquinolones, and β-lactams in Pseudomonas aeruginosa. Antimicrob Agents Chemother 55:1211–1221. doi: 10.1128/AAC.01252-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Guénard S, Muller C, Monlezun L, Benas P, Broutin I, Jeannot K, Plésiat P. 2014. Multiple mutations lead to MexXY-OprM-dependent aminoglycoside resistance in clinical strains of Pseudomonas aeruginosa. Antimicrob Agents Chemother 58:221–228. doi: 10.1128/AAC.01252-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Matsuo Y, Eda S, Gotoh N, Yoshihara E, Nakae T. 2004. MexZ-mediated regulation of mexXY multidrug efflux pump expression in Pseudomonas aeruginosa by binding on the mexZ-mexX intergenic DNA. FEMS Microbiol Lett 238:23–28. doi: 10.1111/j.1574-6968.2004.tb09732.x. [DOI] [PubMed] [Google Scholar]
- 30.Islam S, Jalal S, Wretlind B. 2004. Expression of the MexXY efflux pump in amikacin-resistant isolates of Pseudomonas aeruginosa. Clin Microbiol Infect 10:877–883. doi: 10.1111/j.1469-0691.2004.00991.x. [DOI] [PubMed] [Google Scholar]
- 31.Morita Y, Tomida J, Kawamura Y. 2012. Primary mechanisms mediating aminoglycoside resistance in the multidrug-resistant Pseudomonas aeruginosa clinical isolate PA7. Microbiology 158:1071–1083. doi: 10.1099/mic.0.054320-0. [DOI] [PubMed] [Google Scholar]
- 32.Jeannot K, Sobel ML, El Garch F, Poole K, Plésiat P. 2005. Induction of the MexXY efflux pump in Pseudomonas aeruginosa is dependent on drug-ribosome interaction. J Bacteriol 187:5341–5346. doi: 10.1128/JB.187.15.5341-5346.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Morita Y, Sobel ML, Poole K. 2006. Antibiotic inducibility of the MexXY multidrug efflux system of Pseudomonas aeruginosa: involvement of the antibiotic-inducible PA5471 gene product. J Bacteriol 188:1847–1855. doi: 10.1128/JB.188.5.1847-1855.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jahandideh S. 2013. Diversity in structural consequences of MexZ mutations in Pseudomonas aeruginosa. Chem Biol Drug Des 81:600–606. doi: 10.1111/cbdd.12104. [DOI] [PubMed] [Google Scholar]
- 35.Moore RA, DeShazer D, Reckseidler S, Weissman A, Woods DE. 1999. Efflux-mediated aminoglycoside and macrolide resistance in Burkholderia pseudomallei. Antimicrob Agents Chemother 43:465–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Spilker T, Vandamme P, LiPuma JJ. 2012. A multilocus sequence typing scheme implies population structure and reveals several putative novel Achromobacter species. J Clin Microbiol 50:3010–3015. doi: 10.1128/JCM.00814-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kaniga K, Delor I, Cornelis GR. 1991. A wide-host-range suicide vector for improving reverse genetics in Gram-negative bacteria: inactivation of the blaA gene of Yersinia enterocolitica. Gene 109:137–141. doi: 10.1016/0378-1119(91)90599-7. [DOI] [PubMed] [Google Scholar]
- 38.Westbrock-Wadman S, Sherman DR, Hickey MJ, Coulter SN, Zhu YQ, Warrener P, Nguyen LY, Shawar RM, Folger KR, Stover CK. 1999. Characterization of a Pseudomonas aeruginosa efflux pump contributing to aminoglycoside impermeability. Antimicrob Agents Chemother 43:2975–2983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yamamoto S, Kasai H, Arnold DL, Jackson RW, Vivian A, Harayama S. 2000. Phylogeny of the genus Pseudomonas: intrageneric structure reconstructed from the nucleotide sequences of gyrB and rpoD genes. Microbiology 146:2385–2394. doi: 10.1099/00221287-146-10-2385. [DOI] [PubMed] [Google Scholar]
- 40.Pfaffl MW. 2001. A new mathematical model for relative quantification in real-time RT-PCR. Nucleic Acids Res 29:e45. doi: 10.1093/nar/29.9.e45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Alguel Y, Lu D, Quade N, Sauter S, Zhang X. 2010. Crystal structure of MexZ, a key repressor responsible for antibiotic resistance in Pseudomonas aeruginosa. J Struct Biol 172:305–310. doi: 10.1016/j.jsb.2010.07.012. [DOI] [PubMed] [Google Scholar]