Abstract
OBJECTIVES
To determine associations between use of three different modes of social contact (in person, telephone, written or e-mail), contact with different types of people, and risk of depressive symptoms in a nationally representative, longitudinal sample of older adults.
DESIGN
Population-based observational cohort.
SETTING
Urban and suburban communities throughout the contiguous United States.
PARTICIPANTS
Individuals aged 50 and older who participated in the Health and Retirement Survey between 2004 and 2010 (N = 11,065).
MEASUREMENTS
Frequency of participant use of the three modes of social contact with children, other family members, and friends at baseline were used to predict depressive symptoms (measured using the eight-item Center for Epidemiologic Studies Depression Scale) 2 years later using multivariable logistic regression models.
RESULTS
Probability of having depressive symptoms steadily increased as frequency of in-person—but not telephone or written or e-mail contact—decreased. After controlling for demographic, clinical, and social variables, individuals with in-person social contact every few months or less with children, other family, and friends had a significantly higher probability of clinically significant depressive symptoms 2 years later (11.5%) than those having in-person contact once or twice per month (8.1%; P < .001) or once or twice per week (7.3%; P < .001). Older age, interpersonal conflict, and depression at baseline moderated some of the effects of social contact on depressive symptoms.
CONCLUSION
Frequency of in-person social contact with friends and family independently predicts risk of subsequent depression in older adults. Clinicians should consider encouraging face-to-face social interactions as a preventive strategy for depression.
Keywords: social isolation, telephone, written, e-mail, in-person, face-to-face
For decades, researchers have been interested in the influence of social relationships on health, with research showing significant and meaningful associations between social relationships and a multitude of mental health and other outcomes.1–5 Lack of social contact is an objective measure of social isolation,6 has been implicated in risk of depression,7 and is particularly troubling in elderly populations.8 Loneliness, a subjective sense of inadequacy or dissatisfaction with one’s social relationships,9 is often conceptualized as perceived social isolation10 and is common in older adults.11 Social isolation may contribute to development of depression.12 At the same time, more social contact itself may not be healthy if the interactions are characterized by interpersonal conflict and lack of social support.7
One of the important matters that has not been addressed is the effect of frequency of particular modes of social contact on depression. People interact in many ways—whether meeting in person, talking on the telephone, or having written or e-mail communication, but it is unclear to what extent older adults use each mode of social contact, who the contacts are with, and whether the association between social contacts and depression varies according to mode of social contact. Surveys that assess social contact have almost invariably lumped various means of contact and types of social relationships together or simply not distinguished between them.6,13–15 In addition, past studies of social isolation and mental health outcomes have typically examined cross-sectional data, limiting any consideration of the longitudinal effects.14,15 Increases in the popularity of various modes of social contact that do not occur in person16 add to the importance of determining the effects of how people have contact with others.
Berkman et al. comprehensive conceptual model of how social networks influence health outcomes such as depression provides additional theoretical grounding to the research gaps highlighted above. Their model showcases a cascading set of causal processes that include upstream social network characteristics and downstream interpersonal behaviors. Moreover, this model highlights characteristics including frequency of contact by different modalities (specifically noting face-to-face vs telephone vs mail), as well as type of social relationship (described as boundedness of social groups).17
To address these knowledge gaps, the frequency of in-person, telephone, and written or e-mail social contact between adults aged 50 and older and their children, other family members, and friends was assessed. Subsequent depressive symptoms of respondents was focused on as the outcome. The research questions (RQs) were as follows. RQ1: Are different modes of social contact (in-person, telephone, and written or e-mail) associated with differential risk of depressive symptoms? RQ2: Is social contact with different types of people associated with different risk of depressive symptoms? RQ3: Does age, baseline social support, interpersonal conflict, or depression moderate any effect of frequency of contact on future depressive symptoms?
METHODS
Sample and Data Source
Data were obtained from a nationally representative cohort of adults aged 50 and older who participated in the Health and Retirement Survey (HRS) between 2004 and 2010. Health and Retirement Survey is a longitudinal survey of a nationally representative cohort of older adults in the United States, with survey waves every 2 years.18–21 Since 2004, a random subsample of participants has completed the self-administered psychosocial Leave-Behind Questionnaire (LBQ), which contains measures of social contact. In 2004, the response rate for the overall HRS sample was 68.7% for individuals and 71.4% for households; the cooperation rate for the LBQ (which takes into account whether an individual was asked to complete it) was 78.2%, and the response rate was 69.9% (available at http://hrsonline.isr.umich.edu/).
The analyses were limited to HRS participants who completed the in-person interview in 2004, 2006, 2008, or 2010 and were eligible for and completed the psychosocial LBQ in 2004, 2006, or 2008. Of these 16,800 individuals, 241 lacked a baseline depressive symptoms score, 3,758 lacked a follow-up depressive symptoms score (because of death or missing response), and 1,736 were missing values in at least one baseline covariate, leaving 11,065 respondents for the main analyses. Respondents lacking at least one follow-up depressive symptoms score or missing baseline covariates were significantly more likely at baseline to be older, male, nonwhite, less educated, unmarried, and depressed; to differ in household size; and to have lower net worth, impairment in activities of daily living (ADLs), less social support, and less social contact than the final sample. The difference in proportions of these characteristics between excluded and included groups was less than 20% for all variables and in most cases less than 10%. For the purpose of this study, baseline was defined as the first survey wave in which the participant completed the LBQ. Sample size for particular analyses varies depending on the group of interest specific to the analysis (e.g., participants with children for analyses of social contact with children).
Dependent Variable
Depressive symptoms were measured using the eight-item Center for Epidemiologic Studies Depression Scale (CES-D 8), administered during the in-person interview with participants. The CES-D 8 measures eight depressive symptoms over the past week (e.g., “I felt depressed”; “My sleep was restless”) with response choices of yes or no. The total number of symptoms was summed to create a score ranging from 0 to 8. This variable was dichotomized, with participants with four or more depressive symptoms, a frequently used cut-off producing results similar to the full 20-item CES-D, classified as having clinically significant depressive symptoms.22,23
Independent Variables
Mode of Social Contact Variables
The primary predictor was frequency of use of three modes of social contact: in-person, telephone, and written (including e-mail). Participants were asked about their use of each mode of social contact with each of three social relationship types: their children, their family (other than children), and their friends. The combination of these three modes of contact and three types of people resulted in a total of nine variables. For example, the three survey items addressing social contact with children participants were as follows:
“On average, how often do you do each of the following with any of your children, not counting any who live with you?”
“Meet up (include arranged and chance meetings)” (hereafter, in-person contact)
“Speak on the telephone” (hereafter, telephone contact)
“Write or e-mail” (hereafter, written or e-mail contact)
Six response choices were available for each of these nine variables: three or more times per week (1), once or twice per week (2), once or twice per month (3), every few months (4), once or twice per year (5), less than once per year or never (6). For the primary analyses, each variable was collapsed into four levels (1, 2, 3, 4–6), based on frequency of response and distribution of the data.
Composite Social Contact Variable
A composite variable was constructed consisting of all nine mode of social contact variables described above. The variable value was an average frequency of all written or e-mail, telephone, and in-person contact between the respondent and their children, other family, and friends. This scale had adequate internal consistency (Cronbach alpha = 0.70) and ranged from 1 to 6.
Additional covariates were incorporated into the models to help adjust for potential confounding. These covariates were selected for their known associations with depression or social contact6,24,25 and were maintained if they significantly altered the relationship between the primary predictors and depressive symptoms. Continuous variables were age, wealth (net worth), impairment in ADLs, household size, social support, and interpersonal conflict. Impairment in ADLs was coded as a variable ranging from 0 to 5, which represented how many of the following activities the participant reported at least some difficulty with: bathing, dressing, eating, getting in and out of bed, and walking across a room. Social support and interpersonal conflict were measured using brief scales assessing relationships with family members and friends; scales were similar to those used in prior analyses of quality of social relationships.25 Social support was defined as endorsing, on average, at least some on three items asking how much others “really understand the way you feel about things,” “you (can) rely on them if you have a serious problem,” and “you (can) open up to them if you need to talk about your worries.” Interpersonal conflict was defined as endorsing, on average, at least some on four items asking how much others: “get on your nerves,” “criticize you,” “let you down when you are counting on them,” and “make too many demands on you.” In 2004, only the first three items for interpersonal conflict were included. Cronbach alpha was 0.76 for interitem reliability in the scales of social support and 0.86 in interpersonal conflict. Categorical variables were sex, race and ethnicity, marital status, educational attainment, presence of at least one child living within 10 miles, and presence of baseline depressive symptoms (CES-D 8 ≥ 4).
Data Analysis
All analyses were conducted using HRS survey weights. The respondent weight for the LBQ adjusts for nonresponse to the psychosocial questionnaire in 2004 and selection into the face-to-face interview sample from which LBQ respondents were drawn.26 To help ensure that data are nationally representative, the weight is scaled to yield weighted sums that correspond to the number of individuals in the U.S. population as measured using the March Current Population Survey for the year of data collection. Robust standard errors were obtained by clustering error structure at the household level.
For the analytical approach, first, descriptive statistics of all variables used in the multivariable analyses were examined. Second, Pearson chi-square tests of independence and linear regression were performed to assess bivariate associations between categorical variables and continuous variables, respectively. Third, multivariable logistic regression analyses were used to examine the adjusted associations between frequency of social contact and depressive symptom status. Regression diagnostic procedures were used to examine the models for multicollinearity and assess goodness of fit. Four primary multivariable models were computed that differed according to which predictor of subsequent depressive symptoms was used: composite social contact and frequency of each mode of social contact with respondents’ children, other family members, and friends.
In the multivariable models, three sequential sets of covariates were used; Model 1 contains adjustments for respondents’ sociodemographic characteristics (age, sex, race, education, marital status, net worth, household size, children living within 10 miles), Model 2 contains adjustments for Model 1 sociodemographic characteristics plus clinical characteristics (number of impaired ADLs and baseline depressive symptoms), and Model 3 contains adjustments for Model 2 sociodemographic and clinical characteristics plus social support and interpersonal conflict. Fourth, predicted probabilities were generated using the average marginal effect and graphed to facilitate interpretation. For moderator analyses, interaction terms were created and tested separately within Model 3.
Two sensitivity analyses were conducted to address missing data. First, multiple imputation was performed using the fully conditional specification of the Markov chain Monte Carlo method. Five imputed data sets were created, and all variables available (including baseline CES-D 8 score and all covariates) were included in the imputation model. Pooled estimates were computed using Rubin’s combination rules.27 Second, to account for respondents without follow-up CES-D 8 data, a competing risk model was used in which death and missing were included as an outcome in the multinomial logistic regression (0 = no depressive symptoms, 1 = depressive symptoms, 2 = missing or death).
Statistical significance was established at P < .05 for main effects and P < .10 for interaction effects. All statistical analyses were performed using survey procedures in Stata version 12.0 (Stata Corp., College Station, TX). The institutional review board at the University of Michigan approved HRS, all participants provided informed consent, and the data specifically used for this study contained no unique identifiers.
RESULTS
Sample Characteristics and Correlates
Approximately one-third each of the 11,065 participants were in their 50s, 60s, and 70s or older (Table 1); 88.4% were white, 50.8% had at least some college education, and 54.1% lived in two-person households. The rate of significant depressive symptoms was 13.5% at baseline and 13.1% at 2-year follow-up. Participants used telephone contact the most, closely followed by in-person contact. Written or e-mail contact was least used, with mean frequency less than every few months for all social relationships.
Table 1.
Baseline Characteristics of Participants in the Analytical Sample (N = 11,065)
| Characteristic | Value |
|---|---|
| Age, n (%) | |
| 50–59 | 2,634 (37.8) |
| 60–69 | 3,960 (32.8) |
| 70–79 | 3,093 (19.5) |
| ≥80 | 1,378 (9.9) |
| Female, n (%) | 6,716 (56.5) |
| Race, n (%) | |
| White | 9,396 (88.4) |
| Black | 1,392 (9.1) |
| Other | 277 (2.5) |
| Education, n (%) | |
| <High school graduate | 1,935 (14.9) |
| High school graduate or General Educational Development | 4,088 (34.3) |
| ≥Some college | 5,041 (50.8) |
| Marital status, n (%) | |
| Married or partnered | 7,561 (67.8) |
| Separated, divorced, or widowed | 3,195 (28.4) |
| Never married | 307 (4.8) |
| Wealth, $, n (%) | |
| ≤50,000 | 2,493 (22.6) |
| 50,001–200,000 | 2,759 (25.2) |
| 200,001–500,000 | 2,785 (24.7) |
| ≥500,001 | 3,028 (27.4) |
| Number of people in household, n (%) | |
| 1 | 2,466 (21.8) |
| 2 | 6,234 (54.1) |
| 3 | 1,392 (13.9) |
| ≥4 | 973 (10.1) |
| ≥1 Children living within 10 miles, n (%) | 5,551 (46.7) |
| Number of activities of daily living impaired in, n (%) | |
| 0 | 9,658 (8.8) |
| 1, 2 | 1,127 (9.5) |
| ≥3 | 280 (2.6) |
| Number of cohabitating children, n (%) | |
| 0 | 8,701 (75.6) |
| 1 | 1,813 (18.1) |
| ≥2 | 551 (6.3) |
| Number of living children, n (%) | |
| 0 | 656 (7.9) |
| 1, 2 | 3,931 (39.5) |
| 3–6 | 5,512 (46.9) |
| ≥7 | 752 (5.6) |
| Frequency of in-person contact with, mean ± SD | |
| Children | 2.87 ± 0.02 |
| Other family | 3.59 ± 0.02 |
| Friends | 2.74 ± 0.02 |
| Frequency of telephone contact with, mean ± SD | |
| Children | 1.88 ± 0.01 |
| Other family | 2.61 ± 0.02 |
| Friends | 2.45 ± 0.01 |
| Frequency of written contact with, mean ± SD | |
| Children | 4.14 ± 0.03 |
| Other family | 4.53 ± 0.02 |
| Friends | 4.34 ± 0.02 |
| Socially supported by, n (%) | |
| Spouse | 6,653 (60.2) |
| Children | 7,963 (69.5) |
| Other family | 6,673 (60.7) |
| Friends | 7,266 (65.8) |
| Interpersonal conflict with, n (%) | |
| Spouse | 873 (7.5) |
| Children | 623 (6.1) |
| Other family | 629 (6.8) |
| Friends | 234 (2.5) |
| Depressive symptoms, n (%) | 1,391 (13.5) |
Percentages are weighted and adjusted for clustering. Social support was defined as endorsing an average of some or more on three items asking how much one can open up to, rely on, and be understood by a person (Cronbach alphas between 0.81 and 0.86). Frequency of contact was a mean of 1 = ≥3 d/wk, 2 = 1–2 d/wk, 3 = 1–2 d/month, 4 = every few months, 5 = couple times per year, 6 = once per year or less. Interpersonal conflict was defined as endorsing an average of some or more on four items asking how much others criticize, let one down, get on one’s nerves, and make too many demands (Cronbach alphas between 0.74 and 0.78). In 2004, only the first three items were included. Depression symptoms were defined as an eight-item Center for Epidemiologic Studies Depression Scale score ≥4.
SD = standard deviation.
RQ1: Are Different Modes of Social Contact Associated with Different Risk of Depressive Symptoms?
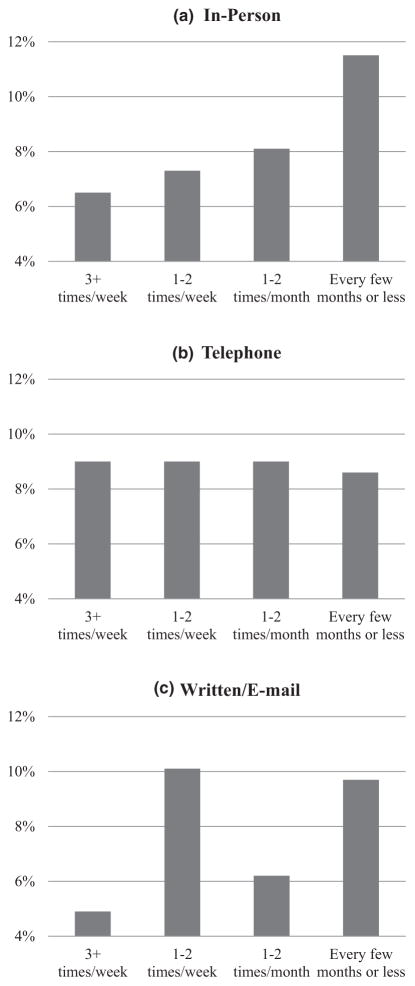
To address the primary aim, whether frequency of each of three modes of social contact (in-person, telephone, written or e-mail) at baseline was associated with depressive symptoms 2 years later was examined. The probability of an individual having clinically significant depressive symptoms as a function of the frequency of social contacts with all people at baseline (children, other family, friends) was estimated. Multivariable models that included all potential confounders were used for these predicted probabilities (Model 3), with covariates held at mean values. Individuals who had in-person social contact on average every few months or less had an 11.5% (95% confidence interval (CI) = 0.09–0.136) chance of depressive symptoms 2 years later, which was significantly higher than those having in-person contact once or twice per week (7.3%, 95% CI = 0.05–0.09, P < .001) or once or twice per month (8.1%, 95% CI = 0.07–0.09, P < .001) (Figure 1). Individuals with the most-frequent in-person contact (≥ 3 times/wk) had the lowest probability of depressive symptoms (6.5%, 95% CI = 0.01–12.3). Individuals who had written or e-mail contact on average every few months or less had a 9.7% (95% CI = 0.08–0.11) chance of depressive symptoms 2 years later, which was significantly higher than those having written contact once or twice per month (6.2%, 95% CI = 0.04–0.08, P = .001). There were no significant differences based on frequency of telephone social contact.
Figure 1.
Estimated probability of depressive symptoms at 2-year follow-up based on frequency of (A) in-person, (B) telephone, and (C) written or e-mail social contact. Probability estimated after adjusting for 12 variables measured at baseline: age, sex, race and ethnicity, educational attainment, wealth (net worth), impairment in activities of daily living, depressive symptoms, marital status, household size, presence of at least one child living within 10 miles, social support, and interpersonal conflict. Depression symptoms were defined as an eight-item Center for Epidemiologic Studies Depression Scale score ≥4. Frequency of social contact was an average of contact with children, other family, and friends.
RQ2: Is Social Contact with Different Types of People Associated with Different Risk of Depressive Symptoms?
Next, social contact with each type of person was analyzed separately. For social contact with children, there were no associations with depression that maintained significance after controlling for all covariates in Model 3 (Table 2). A similar pattern emerged for the effect of frequency of social contact with other family members on subsequent depressive symptoms. No associations for the overall sample were significant in the final model (Table 3).
Table 2.
Multivariable Logistic Regression Models of Frequency of Three Modes of Social Contact with Children Predicting Presence of Depressive Symptoms at 2-Year Follow-Up in Older Adults
| Type of Contact | Model 1, n = 8,998 | Model 2, n = 8,998 | Model 3, n = 8,996 |
|---|---|---|---|
| Odds Ratio (95% Confidence Interval) P-Value | |||
| In-person | |||
| 1–2 times/month | 0.99 (0.78–1.27) .96 | 1.14 (0.88–1.48) .32 | 1.14 (0.87–1.48) .35 |
| 1–2 times/wk | 0.81 (0.63–1.03) .09 | 0.87 (0.67–1.14) .31 | 0.85 (0.64–1.12) .25 |
| ≥3 times/wk | 0.71 (0.53–0.96) .02 | 0.75 (0.54–1.03) .07 | 0.74 (0.52–1.04) .08 |
| Telephone | |||
| 1–2 times/month | 0.73 (0.50–1.07) .11 | 0.83 (0.55–1.25) .37 | 0.89 (0.59–1.33) .63 |
| 1–2 times/wk | 0.66 (0.45–0.95) .02 | 0.65 (0.43–0.98) .04 | 0.73 (0.49–1.09) .13 |
| ≥3 times/wk | 0.80 (0.55–1.17) .25 | 0.77 (0.51–1.17) .22 | 0.90 (0.59–1.37) .56 |
| Written or e-mail | |||
| 1–2 times/month | 0.78 (0.60–1.02) .06 | 0.88 (0.67–1.16) .36 | 0.70 (0.45–1.08) .37 |
| 1–2 times/wk | 0.73 (0.55–0.97) .03 | 0.90 (0.67–1.21) .49 | 0.91 (0.67–1.22) .52 |
| ≥3 times/wk | 0.52 (0.35–0.77) .001 | 0.67 (0.44–1.04) .07 | 0.88 (0.67–1.16) .11 |
All models included adjustment for population weight and clustering. Model 1 also adjusted for age, sex, race, education, and net worth. Model 2 adjusted for all Model 1 covariates plus impairment in activities of daily living and baseline depression. Model 3 adjusted for all Model 2 covariates plus marital status, household size, children living within 10 miles, social support, and interpersonal conflict. All frequency-of-social-contact variables were examined in the same logistic regression model. Depression symptoms were defined as an eight-item Center for Epidemiologic Studies Depression Scale score ≥4. Reference was every few months or less.
Table 3.
Multivariable Logistic Regression Models of Frequency of Three Modes of Social Contact with Other Family Predicting Presence of Depressive Symptoms at 2-Year Follow-Up in Older Adults
| Type of Contact | Model 1, n = 10,057 | Model 2, n = 10,057 | Model 3, n = 10,055 |
|---|---|---|---|
| Odds Ratio (95% Confidence Interval) P-Value | |||
| In-person | |||
| 1–2 times/month | 0.80 (0.64–1.01) .06 | 0.87 (0.68–1.12) .28 | 0.86 (0.67–1.11) .26 |
| 1–2 times/wk | 0.88 (0.68–1.13) .31 | 0.97 (0.73–1.29) .85 | 0.99 (0.74–1.31) .93 |
| ≥3 times/wk | 0.74 (0.53–1.03) .08 | 0.78 (0.54–1.14) .20 | 0.78 (0.54–1.12) .18 |
| Telephone | |||
| 1–2 times/month | 0.94 (0.74–1.19) .60 | 0.95 (0.73–1.22) .67 | 1.06 (0.80–1.39) .69 |
| 1–2 times/wk | 1.00 (0.78–1.30) .97 | 0.91 (0.68–1.21) .50 | 1.01 (0.75–1.38) .92 |
| ≥3 times/wk | 1.12 (0.84–1.49) .45 | 0.96 (0.69–1.33) .80 | 1.11 (0.78–1.57) .57 |
| Written or e-mail | |||
| 1–2 times/month | 0.66 (0.50–0.87) .003 | 0.72 (0.53–0.98) .03 | 0.75 (0.55–1.02) .06 |
| 1–2 times/wk | 0.73 (0.53–1.00) .048 | 0.87 (0.64–1.18) .37 | 0.94 (0.68–1.28) .69 |
| ≥3 times/wk | 0.60 (0.38–0.92) .02 | 0.66 (0.40–1.08) .10 | 0.74 (0.46–1.17) .20 |
All models included adjustment for population weight and clustering. Model 1 also adjusted for age, sex, race, education, and net worth. Model 2 adjusted for all Model 1 covariates plus impairment in activities of daily living and baseline depression. Model 3 adjusted for all Model 2 covariates plus marital status, household size, children living within 10 miles, social support, and interpersonal conflict. All frequency-of-social-contact variables were examined in the same logistic regression model. Depression symptoms were defined as an eight-item Center for Epidemiologic Studies Depression Scale score ≥4. Reference was every few months or less.
For relationships with friends, mode of social contact was significantly associated with odds of developing depressive symptoms 2 years later even after adjusting for all demographic, clinical, and social covariates (Table 4). More-frequent in-person contact with friends was associated with lower odds of subsequent depressive symptoms than contact every few months or less (OR = 0.57, 95% CI = 0.44–0.76, P < .001 for 1–2 times/wk; OR = 0.60, 95% CI = 0.42–0.86, P = .005 for ≥3 times/wk).
Table 4.
Multivariable Logistic Regression Models of Frequency of Three Modes of Social Contact with Friends Predicting Presence of Depressive Symptoms at 2-Year Follow-Up in Older Adults
| Type of Contact | Model 1, n = 9,908 | Model 2, n = 9,908 | Model 3, n = 9,907 |
|---|---|---|---|
| Odds Ratio (95% Confidence Interval) P-Value | |||
| In-person | |||
| 1–2 times/month | 0.81 (0.64–1.01) .07 | 0.78 (0.61–1.01) .06 | 0.77 (0.60–1.00) .05 |
| 1–2 times/wk | 0.55 (0.43–0.70) <.001 | 0.58 (0.45–0.76) <.001 | 0.57 (0.44–0.76) <.001 |
| ≥3 times/wk | 0.56 (0.40–0.76) <.001 | 0.62 (0.44–0.88) .008 | 0.60 (0.42–0.86) .005 |
| Telephone | |||
| 1–2 times/month | 0.93 (0.71–1.22) .62 | 0.91 (0.68–1.21) .52 | 0.95 (0.71–1.28) .76 |
| 1–2 times/wk | 0.89 (0.68–1.15) .36 | 0.81 (0.61–1.08) .14 | 0.80 (0.60–1.07) .14 |
| ≥3 times/wk | 1.19 (0.89–1.61) .24 | 0.96 (0.69–1.35) .83 | 0.95 (0.67–1.36) .80 |
| Written or e-mail | |||
| 1–2 times/month | 0.74 (0.56–0.98) .03 | 0.86 (0.64–1.16) .32 | 0.84 (0.62–1.13) .25 |
| 1–2 times/wk | 0.64 (0.47–0.87) .005 | 0.71 (0.52–0.98) .04 | 0.73 (0.53–1.00) .05 |
| ≥3 times/wk | 0.61 (0.41–0.90) .01 | 0.72 (0.46–1.13) .15 | 0.67 (0.44–1.07) .10 |
All models included adjustment for population weight and clustering. Model 1 also adjusted for age, sex, race, education, and net worth. Model 2 adjusted for all Model 1 covariates plus impairment in activities of daily living and baseline depression. Model 3 adjusted for all Model 2 covariates plus marital status, household size, children living within 10 miles, social support, and interpersonal conflict. All frequency-of-social-contact variables were examined in the same logistic regression model. Depression symptoms were defined as an eight-item Center for Epidemiologic Studies Depression Scale score ≥4. Reference was every few months or less.
To determine whether social contact with one relationship might substitute for another, posterior probability of depressive symptoms across varying levels of social contact was examined, adjusting for multiple comparisons. Increasing the frequency of contact with children or other family members did not result in significantly different probabilities of depression, regardless of frequency of contact with friends (results not shown).
RQ3: Does Baseline Age, Social Support, Interpersonal Conflict, or Depression Moderate the Effect of Frequency of Contact on Future Depressive Symptoms?
First, whether results from the analyses using Model 3 (Tables 2–4) differed between individuals younger than 70 and those aged 70 and above was explored. For older individuals, in-person contact with children (OR = 0.47, 95% CI = 0.28–0.78, P = .004) and other family (OR = 0.52, 95% CI = 0.29–0.93, P = .03) at least three times per week predicted a significantly lower risk of depressive symptoms 2 years later. In contrast, for individuals aged 50 to 69, only frequent in-person contact with friends was significant (OR = 0.55, 95% CI = 0.38–0.78, P = .001 for 1–2 times/wk; OR = 0.59, 95% CI = 0.38–0.93, P = .02 for ≥3 times/wk).
Next, whether self-rated quality of participants’ social relationships interacted with their frequency of social contact to influence depressive symptoms was examined. For participants’ relationships with their children, interpersonal conflict moderated the association between frequency of in-person contact and depressive symptoms such that risk of depressive symptoms was higher as interpersonal conflict and contact rose (OR = 1.16 for the interaction term, 95% CI = 1.03–1.30, P = .01). A similar relationship was observed for participants’ relationships with other family and frequency of written or e-mail contact (OR = 1.17 for the interaction term, 95% CI = 0.99, 1.38, P = .07). No other significant interactions between mode of contact and social support or interpersonal conflict were detected.
Then, to determine whether the association between social contact and depressive symptoms at follow-up differed according to participant baseline depression status, an analysis was conducted using Model 3, with participants stratified according to baseline depressive symptoms. More-frequent in-person contact with friends was associated with lower risk of depression only in participants not depressed at baseline (OR = 0.53 for 1–2 times/wk, 95% CI = 0.38–0.74, P < .001; OR = 0.54 for ≥3 times/wk, 95% CI = 0.35–0.83, P = .005). In contrast, telephone contact with friends was associated with lower risk of depressive symptoms only in participants who were depressed at baseline (OR = 0.51, 95% CI = 0.30–0.86, P = .01 for 1–2 times/wk; OR = 0.55, 95% CI = 0.31–1.00, P = .049 for ≥3 times/wk). Written or e-mail contact with friends once or twice per week was associated with lower risk of future depressive symptoms only in those without depression at baseline (OR = 0.61, 95% CI = 0.41–0.91, P = .01).
Sensitivity Analyses
For both of the sensitivity analyses (multiple imputation, competing risk model), results yielded coefficients similar to those obtained in the sample, and all significant results in the primary analyses were maintained, which suggests that there was minimal bias due to missing data.
DISCUSSION
These results support the claim that how and with whom a person has social contact affects future risk of depressive symptoms. The most important finding is that more-frequent in-person contact at baseline was associated with lower probability of depressive symptoms 2 years later and was in a dose-dependent fashion. In-person social contact involving more activation or being perceived as a more-supportive interaction could explain this. Telephone contact was the most-common mode of social contact, but rates of depressive symptoms remained static across varying levels of telephone contact, and variable rates of depressive symptoms across levels of written or e-mail contact prevent conclusions about it having an effect. An important caveat regarding the effect of in-person contact—at least in older adults’ relationships with their children —is that if frequent contact is also characterized by interpersonal conflict, risk of depressive symptoms is greater rather than less.
These data also emphasize that with whom a person has social contact may affect risk of depression and that the degree of influence may depend on how old an individual is. For those in their 50s and 60s, social contact with friends may be particularly important in preventing future depressive symptoms. In contrast, results in those aged 70 and older suggest that frequent contact with children or other family members is protective against depression. In addition, an earlier study that examined mostly middle-aged adults younger than 50 found that the quality of relationships with spouses and family members, but not friends, predicted development of depression 10 years later.25 These complex and varying results suggest that future studies should more closely examine whether different social relationships serve different mental health functions across the age spectrum. Perhaps relationships with family members are most relevant when many people are focused on raising families (often aged <50) and in retirement (often aged ≥70), whereas relationships with friends are most relevant between those ages.
This study has several implications for depression prevention, risk reduction, and intervention design. Some researchers have recently postulated that indirect modes of contact such as Facebook and other online venues may not influence health in the same way or to the same degree as direct, in-person contact.28 If these types of social contact are substituted for in-person interactions, there could be greater population-level risk for depression. Public health strategies that promote or facilitate in-person social contact may be particularly helpful for primary prevention of depression. Primary care clinicians can emphasize and educate people on the value of face-to-face social contact with close supports. In contrast, for an individual with a known history of depression, telephone-based social support interventions may be effective. This is a noteworthy distinction and one that supports the current trend toward delivery of telephone-based mental health services.29,30 Other intervention options that draw on the present study’s results include trying to expand the social network of individuals with depression with a small number of individuals they might come to identify as a “friends.” Prior research indicates that having as few as two close friends is associated with better psychological well-being.31 Peer support specialists may be especially suitable for this approach.32
As far as the authors are aware, this is the first study to examine the effect of mode of social contact on risk of clinically significant depressive symptoms. Moreover, because of the broad array of covariates, including those addressing geographical proximity to others, household size, and social support in the models, the results indicate the unique effect of mode of social contact on depressive symptoms. When mode of contact has previously been examined, it has almost invariably been mode of contact in an intervention with a healthcare provider rather than with members of an individual’s natural social network.33 The current study also included contact over e-mail, which has rarely been investigated in depression studies. Additional study strengths include large sample size, national representativeness, longitudinal follow-up, and adjustments for cluster effects and survey nonresponse.
Several limitations of this study bear consideration in interpreting the findings. First, a large number of individuals from the HRS could not be included in the primary analyses because of lack of available data on social contact or lack of follow-up depressive symptom scores (due to death, nonresponse, or other reasons), but this was unlikely to bias the sample toward participants with a systematically different pattern of social contact based on the results of a sensitivity analysis with multiple imputation. Multiple imputation provided replacement of these missing values for social contact (and other variables), and its strength is as a flexible, advanced approach that works well at removing such biases in simulation experiments.34 Regarding missing follow-up depression data, the sensitivity analysis using a competing risk model included all individuals missing longitudinal depression data and still found similar estimates of depression risk. This statistical technique helps provide reassurance about the validity of the outcome estimates,35 although because base-year weighting does not correct for attrition, generalization of the results is probably limited to those with less-severe depressive symptoms. Second, the outcome measure, the CES-D 8, is based on depressive symptoms rather than clinical diagnosis of depression. Third, the measure of social contact was limited to social contact with non-co-residing individuals. Finally, although the longitudinal analyses provided stronger evidence than cross-sectional studies that social contact affects subsequent depressive symptoms, experimental evidence, such as that from a randomized intervention, would provide stronger support for causality.
In summary, the findings in a large, nationally representative sample of Americans aged 50 and older suggest that more-frequent in-person social contact predicts lower risk of depressive symptoms 2 years later, and of different social relationships, in-person contact with one’s friends is specifically associated with lower risk of depression. Clinicians and researchers should consider by what means and with whom people have social contact when considering promotion of social support for older adults at risk of depression.
Acknowledgments
This material is the result of work supported in part by a grant from the Robert Wood Johnson Foundation and the Department of Veterans Affairs (IIR 10–176), as well as the use of facilities at the Veterans Affairs Portland Health Care System. The HRS is sponsored by National Institute on Aging Grant U01AG009740 and is conducted by the University of Michigan.
Conflict of Interest: The authors have no financial or any other kind of personal conflicts with this paper.
Author Contributions: Conception and design: Teo. Provided study materials (HRS cohort): Teo, Choi. Statistical analysis: Andrea, Teo, Choi. Interpretation of data: all authors. Drafting article: Teo, Andrea. Critical intellectual revisions: all authors. Final approval: all authors.
Sponsor’s Role: The sponsor had no role in the design, methods, subject recruitment, data collections, analysis, or preparation of paper. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the U.S. government.
References
- 1.Cohen S. Social relationships and health. Am Psychol. 2004;59:676–684. doi: 10.1037/0003-066X.59.8.676. [DOI] [PubMed] [Google Scholar]
- 2.House JS, Landis KR, Umberson D. Social relationships and health. Science. 1988;241:540–545. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- 3.Galea S, Tracy M, Hoggatt KJ, et al. Estimated deaths attributable to social factors in the United States. Am J Public Health. 2011;101:1456–1465. doi: 10.2105/AJPH.2010.300086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Perissinotto CM, Stijacic Cenzer I, Covinsky KE. Loneliness in older persons: a predictor of functional decline and death. Arch Intern Med. 2012;172:1078–1083. doi: 10.1001/archinternmed.2012.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pietrzak RH, Russo AR, Ling Q, et al. Suicidal ideation in treatment-seeking veterans of Operations Enduring Freedom and Iraqi Freedom: The role of coping strategies, resilience, and social support. J Psychiatr Res. 2011;45:720–726. doi: 10.1016/j.jpsychires.2010.11.015. [DOI] [PubMed] [Google Scholar]
- 6.Coyle CE, Dugan E. Social isolation, loneliness and health among older adults. J Aging Health. 2012;24:1346–1363. doi: 10.1177/0898264312460275. [DOI] [PubMed] [Google Scholar]
- 7.Kawachi I, Berkman LF. Social ties and mental health. J Urban Health. 2001;78:458–467. doi: 10.1093/jurban/78.3.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Golden J, Conroy RM, Bruce I, et al. Loneliness, social support networks, mood and wellbeing in community-dwelling elderly. Int J Geriatr Psychiatry. 2009;24:694–700. doi: 10.1002/gps.2181. [DOI] [PubMed] [Google Scholar]
- 9.Heinrich LM, Gullone E. The clinical significance of loneliness: A literature review. Clin Psychol Rev. 2006;26:695–718. doi: 10.1016/j.cpr.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 10.Cacioppo JT, Hawkley LC, Norman GJ, et al. Social isolation. Ann N Y Acad Sci. 2011;1231:17–22. doi: 10.1111/j.1749-6632.2011.06028.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Savikko N, Routasalo P, Tilvis RS, et al. Predictors and subjective causes of loneliness in an aged population. Arch Gerontol Geriatr. 2005;41:223–233. doi: 10.1016/j.archger.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 12.Ciechanowski P, Wagner E, Schmaling K, et al. Community-integrated home-based depression treatment in older adults: A randomized controlled trial. JAMA. 2004;291:1569–1577. doi: 10.1001/jama.291.13.1569. [DOI] [PubMed] [Google Scholar]
- 13.Berkman LF, Syme SL. Social networks, host resistance, and mortality: A nine-year follow-up study of Alameda County residents. Am J Epidemiol. 1979;109:186–204. doi: 10.1093/oxfordjournals.aje.a112674. [DOI] [PubMed] [Google Scholar]
- 14.Cornwell EY, Waite LJ. Social disconnectedness, perceived isolation, and health among older adults. J Health Soc Behav. 2009;50:31–48. doi: 10.1177/002214650905000103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chou KL, Liang K, Sareen J. The association between social isolation and DSM-IV mood, anxiety, and substance use disorders: Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2011;72:1468–1476. doi: 10.4088/JCP.10m06019gry. [DOI] [PubMed] [Google Scholar]
- 16.Hampton KN, Sessions LF, Her EJ, et al. Social Isolation and New Technology. Washington, DC: Pew Internet & American Life Project; 2009. [Google Scholar]
- 17.Berkman LF, Glass T, Brissette I, et al. From social integration to health: Durkheim in the new millennium. Soc Sci Med. 2000;51:843–857. doi: 10.1016/s0277-9536(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 18.Juster F, Suzman R. An overview of the Health and Retirement Study. J Hum Resources. 1995;30:S7–S56. [Google Scholar]
- 19.Health and Retirement Study. Public Use Dataset. Ann Arbor, MI: University of Michigan; 2008. [Google Scholar]
- 20.National Institute on Aging. The Health and Retirement Study: Growing Older in America. Bethesda, MD: National Institutes of Health; 2007. [Google Scholar]
- 21.RAND HRS. Data, Version H. Santa Monica, CA: RAND Center for the Study of Aging; 2008. [Google Scholar]
- 22.Mezuk B, Bohnert ASB, Ratliff S, et al. Job strain, depressive symptoms, and drinking behavior among older adults: results from the Health and Retirement Study. J Gerontol B Psychol Sci Soc Sci. 2011;66B:426–434. doi: 10.1093/geronb/gbr021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Steffick DE HRS Health Working Group. HRS/AHEAD Documentation Report. Ann Arbor, MI: University of Michigan; 2000. Documentation of Affective Functioning Measures in the Health and Retirement Study. [Google Scholar]
- 24.Cacioppo JT, Hawkley LC, Thisted RA. Perceived social isolation makes me sad: 5-year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago Health, Aging, and Social Relations Study. Psychol Aging. 2010;25:453–463. doi: 10.1037/a0017216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Teo AR, Choi H, Valenstein M. Social relationships and depression: Ten-year follow-up from a nationally representative study. PLoS ONE. 2013;8:e62396. doi: 10.1371/journal.pone.0062396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Health and Retirement Study. [Accessed July 22, 2015];Sample weights, sample selection indicators and response rates for the psychosocial and disability leave-behind questionnaires in HRS 2004 [on-line] Available at http://hrson-line.isr.umich.edu/index.php?p=weightinfo.
- 27.Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York: John Wiley and Sons; 1987. [Google Scholar]
- 28.Hamilton J. Maybe isolation, not loneliness, shortens life. [Accessed July 22, 2015];Shots: Health news from NPR [on-line] Available at http://www.npr.org/sections/health-shots/2013/03/26/175283008/maybe-isolation-not-loneliness-shortens-life.
- 29.Mohr DC, Ho J, Duffecy J, et al. Effect of telephone-administered vs face-to-face cognitive behavioral therapy on adherence to therapy and depression outcomes among primary care patients: A randomized trial. JAMA. 2012;307:2278–2285. doi: 10.1001/jama.2012.5588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Choi NG, Marti CN, Bruce ML, et al. Six-month post-intervention depression and disability outcomes of in-home telehealth problem-solving therapy for depressed, low-income homebound older adults. Depress Anxiety. 2014;31:653–661. doi: 10.1002/da.22242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Birditt KS, Antonucci TC. Relationship quality profiles and well-being among married adults. J Fam Psychol. 2007;21:595–604. doi: 10.1037/0893-3200.21.4.595. [DOI] [PubMed] [Google Scholar]
- 32.Pfeiffer PN, Heisler M, Piette JD, et al. Efficacy of peer support interventions for depression: A meta-analysis. Gen Hosp Psychiatry. 2011;33:29–36. doi: 10.1016/j.genhosppsych.2010.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hammond GC, Croudace TJ, Radhakrishnan M, et al. Comparative effectiveness of cognitive therapies delivered face-to-face or over the telephone: An observational study using propensity methods. PLoS ONE. 2012;7:e42916. doi: 10.1371/journal.pone.0042916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cole SR, Chu H, Greenland S. Multiple-imputation for measurement-error correction. Int J Epidemiol. 2006;35:1074–1081. doi: 10.1093/ije/dyl097. [DOI] [PubMed] [Google Scholar]
- 35.Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94:496–509. [Google Scholar]