SUMMARY
To address uncertainty of whether pathologic stage groupings after neoadjuvant therapy (ypTNM) for esophageal cancer share prognostic implications with pathologic groupings after esophagectomy alone (pTNM), we report data—simple descriptions of patient characteristics, cancer categories, and non–risk-adjusted survival—for pathologically staged cancers after neoadjuvant therapy from the Worldwide Esophageal Cancer Collaboration (WECC). Thirty-three institutions from six continents submitted data using variables with standard definitions: demographics, comorbidities, clinical cancer categories, and all-cause mortality from first management decision. Of 7,773 pathologically staged neoadjuvant patients, 2,045 had squamous cell carcinoma, 5,686 adenocarcinoma, 31 adenosquamous carcinoma, and 11 undifferentiated carcinoma. Patients were older (61 years) men (83%) with normal (40%) or overweight (35%) body mass index, 0–1 Eastern Cooperative Oncology Group performance status (96%), and a history of smoking (69%). Cancers were ypT0 (20%), ypT1 (13%), ypT2 (18%), ypT3 (44%), ypN0 (55%), ypM0 (94%), and G2-G3 (72%); most involved the distal esophagus (80%). Non–risk-adjusted survival for yp categories was unequally depressed, more for earlier categories than later, compared with equivalent categories from prior WECC data for esophagectomy-alone patients. Thus, survival of patients with ypT0-2N0M0 cancers was intermediate and similar regardless of ypT; survival for ypN+ cancers was poor. Because prognoses for ypTNM and pTNM categories are dissimilar, prognostication should be based on separate ypTNM categories and groupings. These data will be the basis for the 8th edition cancer staging manuals following risk adjustment for patient, cancer, and treatment characteristics and should direct 9th edition data collection.
Keywords: cancer staging, chemotherapy, prognostication, radiotherapy, survival
INTRODUCTION
Esophageal cancer staging in the 7th edition AJCC and UICC cancer staging manuals1,2 was based on pathologic stage (pTNM) after esophagectomy alone, derived from Worldwide Esophageal Cancer Collaboration (WECC) data.3 However, today a minority of advanced-stage esophageal cancers are treated by esophagectomy alone; some form of combined modality therapy (neoadjuvant therapy) is nearly always used. Pathologic stage after neoadjuvant therapy (ypTNM), by tradition, shares pathologic stage groupings with pTNM. However, whether the prognostic significance of pTNM staging is shared with ypTNM is uncertain.
To address this uncertainty, a six-continent collaborative effort—WECC—was mounted to collect patient and esophageal cancer characteristics and all-cause mortality following neoadjuvant therapy to (i) test the hypothesis that pathologic classifications after neoadjuvant therapy share the same prognostic implications as those after esophagectomy alone; (ii) facilitate post-treatment prognostication; and (iii) develop the first data-driven ypTNM recommendations for the 8th edition cancer staging manuals after risk adjustment. In this article, we simply report the descriptive data on patient and cancer characteristics of individuals with pathologically staged cancers after neoadjuvant therapy, and non–risk-adjusted survival analyses that begin to address these aims.
PATIENTS AND METHODS
Data
In 2012, institutions worldwide were invited to participate in WECC, aimed at constructing refined data-driven esophageal cancer staging for the 8th edition of the cancer staging manuals.4 Data were requested in completely de-identified form (Health Insurance Portability and Accountability Act research standards) for analysis, using a set of required variables with standard definitions. Local ethics-board approval of the databases and data-use agreements were executed with Cleveland Clinic. Variables included demographics, comorbidities, cancer categories, cancer treatment, and time-related outcomes. The Case Cancer Institutional Review Board of Case Western Reserve University and the Cleveland Clinic Institutional Review Board approved the entire project. This paper reports results of pathologic data of patients receiving neoadjuvant therapy from 33 institutions whose data were submitted by September 30, 2014, and were cleaned and adjudicated (Appendix).
Patients
A total of 7,773 patients with epithelial esophageal cancers had pathologic staging data after neoadjuvant therapy. The majority were older men with normal or overweight body mass index, no weight loss, and 0–1 Eastern Cooperative Oncology Group (ECOG) performance status (Table 1 and Supporting Information Table S1). Comorbidities were present in a minority of patients, with cardiopulmonary comorbidities predominating. Although six continents are represented, most patients were treated in North America or Europe.
Table 1.
Characteristics of patients receiving neoadjuvant therapy for pure squamous cell carcinoma and pure adenocarcinoma of the esophagus
| Squamous Cell Carcinoma (total n = 2,045)
|
Adenocarcinoma (total n = 5,686)
|
|||
|---|---|---|---|---|
| Characteristic | n* | No. (%) or Mean ± SD | n* | No. (%) or Mean ± SD |
| Demographics | ||||
| Age (y) | 2,000 | 61 ± 9.4 | 5,513 | 61 ± 9.8 |
| Female | 2,045 | 678 (33) | 5,686 | 658 (12) |
| Body mass index (mg/kg2) | 1,053 | 23 ± 4.1 | 3,222 | 28 ± 5.2 |
| Weight loss (kg) | 1,067 | 2.6 ± 6.0 | 2,532 | 3.6 ± 7.1 |
| Comorbidities | ||||
| ECOG performance status | 571 | 1,891 | ||
| 0 | 289 (51) | 660 (35) | ||
| 1 | 238 (42) | 1,163 (62) | ||
| 2 | 31 (5.4) | 54 (2.9) | ||
| 3 | 12 (2.1) | 12 (0.63) | ||
| 4 | 1 (0.18) | 2 (0.11) | ||
| Diabetes | 1,798 | 94 (5.2) | 5,091 | 638 (13) |
| IDDM | 1,765 | 16 (0.91) | 4,876 | 67 (1.4) |
| NIDDM | 1,765 | 45 (2.5) | 4,876 | 356 (7.3) |
| Coronary artery disease | 915 | 109 (12) | 3,323 | 486 (15) |
| Arrhythmia | 686 | 23 (3.4) | 1,976 | 43 (2.2) |
| Hypertension | 1,351 | 338 (25) | 3,688 | 1,084 (29) |
| Peripheral arterial disease | 1,102 | 50 (4.5) | 3,363 | 84 (2.5) |
| Smoker | 1,370 | 1038 (76) | 4,324 | 2,902 (67) |
| Past | 1,075 | 444 (41) | 3,527 | 1,552 (44) |
| Current | 1,075 | 299 (28) | 3,527 | 553 (16) |
| FEV1 (% of predicted) | 903 | 90 ± 20 | 2,530 | 95 ± 19 |
| FVC (% of predicted) | 657 | 99 ± 18 | 1,411 | 99 ± 17 |
| Creatinine (μmol/L) | 316 | 73 ± 19 | 667 | 77 ± 20 |
| Bilirubin (μmol/L) | 259 | 12 ± 5.4 | 416 | 9.8 ± 7.5 |
| Decade of treatment | 2,045 | 5,686 | ||
| 1970–1979 | 60 (2.9) | 6 (0.11) | ||
| 1980–1989 | 197 (9.6) | 137 (2.4) | ||
| 1990–1999 | 424 (21) | 826 (15) | ||
| 2000–2009 | 977 (48) | 3,316 (58) | ||
| 2010–2014 | 387 (19) | 1,401 (25) | ||
| Continent | 2,045 | 5,686 | ||
| North America | 973 (48) | 3,880 (68) | ||
| Europe | 568 (28) | 1,367 (24) | ||
| Asia | 408 (20) | 51 (0.9) | ||
| Australia | 94 (4.6) | 379 (6.7) | ||
| South America | 1 (0.049) | 6 (0.11) | ||
| Africa | 1 (0.049) | 3 (0.053) | ||
Patient characteristics of those with adenosquamous and undifferentiated carcinoma are shown in Supporting Information Table S1.
Patients with data available.
ECOG, Eastern Cooperative Oncology Group; FEV1 (%), forced expiratory volume in 1 second (percent of predicted); FVC (%), forced vital capacity (percent of predicted); IDDM, insulin-dependent diabetes mellitus; NIDDM, non–insulin-dependent diabetes mellitus; SD, standard deviation.
Compared to patients with pure squamous cell carcinoma (SCC), those with pure adenocarcinoma were far less likely to be female, but more likely to be larger, have an ECOG performance status of 1 rather than 0, have diabetes, better forced expiratory volume in 1 second, and be from the West (Table 1). Age and cardiovascular morbidity were similar.
Treatment
Chemoradiotherapy was the predominant neoadjuvant therapy (Table 2 and Supporting Information Table S2). Approximately one fifth of patients received neoadjuvant chemotherapy, and one tenth of those with pure SCC received radiotherapy. Less invasive esophagectomy was used in few patients. Number of lymph nodes resected was highly variable. Fifteen percent of patients received postoperative adjuvant therapy.
Table 2.
Treatment received by patients with pure squamous cell carcinoma and pure adenocarcinoma of the esophagus
| Squamous cell carcinoma (n = 2,045) | Adenocarcinoma (n = 5,686) | |
|---|---|---|
| Treatment | No. (%) | No. (%) |
| Neoadjuvant | ||
| Chemoradiotherapy | 1,372 (67) | 4,242 (76) |
| Chemotherapy | 454 (22) | 1,306 (23) |
| Radiotherapy | 211 (10) | 62 (1.1) |
| Unknown | 8 | 76 |
| Resection | ||
| Esophagectomy | 2,045 (100) | 5,686 (100) |
| Less invasive | 56 (2.7) | 350 (6.2) |
| Lymph nodes resected | ||
| 0 | 17 (1.8) | 103 (3.4) |
| 1–5 | 71 (7.4) | 246 (8.1) |
| 6–10 | 147 (15) | 432 (14) |
| 11–20 | 356 (37) | 1,106 (36) |
| 21–30 | 232 (24) | 704 (23) |
| >30 | 131 (14) | 446 (15) |
| Unknown | 1,091 | 2,649 |
| Resection Margin | ||
| R0 | 1,851 (91) | 5,086 (89) |
| R1 | 149 (7.3) | 425 (7.5) |
| R2 | 45 (2.2) | 175 (3.1) |
| Adjuvant | ||
| Chemoradiotherapy | 62 (3.0) | 420 (7.4) |
| Chemotherapy | 210 (10) | 375 (6.6) |
| Radiotherapy | 43 (2.1) | 60 (1.1) |
Treatment received by patients with adenosquamous and undifferentiated carcinoma are shown in Supporting Information Table S2.
Endpoint
The study endpoint was all-cause mortality from first management decision. Median potential follow-up,5 if there were no deaths, was 8.2 years (25% >12.9 years, 10% >17.9 years), but considering deaths in this elderly population with a rapidly lethal cancer, overall median follow-up was 1.6 years; median follow-up for surviving patients was 1.8 years, with 25% followed more than 4.1 years and 10% more than 6.8 years.
Data analysis
For analysis, patients with adenosquamous and undifferentiated carcinoma (Supporting Information Tables S1 and S2) were considered in both SCC and adenocarcinoma data sets. Survival was estimated by the Kaplan–Meier method, and these estimates are accompanied by 68% confidence limits, equivalent to ±1 standard error. The hazard function for death was estimated by a parametric temporal decomposition method6 (for additional details, see http://www.lerner.ccf.org/qhs/software/hazard). Continuous variables are summarized by means and standard deviation and categorical variables by frequency and percentage.
RESULTS
Neoadjuvant pathologic cancer categories
Histopathologic cell type was SCC in 2,045, adenocarcinoma in 5,686, adenosquamous carcinoma in 31, and undifferentiated carcinoma in 11. Upon resection, the majority of SCCs were confined to the esophageal wall (ypT2 or less); there was an equal distribution within (ypT2 or less) and beyond (ypT3-T4) the esophageal wall for adenocarcinomas (Table 3 and Supporting Information Table S3). There was no residual cancer (ypT0N0M0) in 25% of SCCs and 13% of adenocarcinomas. Most cancers were free of regional lymph node metastasis (ypN0). Frequency of number of positive lymph nodes progressively decreased for both histopathologic cell types, with 2.8% of SCCs and 8.9% of adenocarcinomas having seven or more positive nodes. Extracapsular lymph node invasion (ECLNI) was infrequently recorded, but present in 22% of N+ SCCs and 43% of N+ adenocarcinomas. Lymphovascular invasion was discovered in approximately one third of cancers. Few cancers had distant metastases (ypM). The majority of SCCs were G1-2 (74%); adenocarcinomas were less differentiated (77% G2-3). The middle thoracic esophagus was the most common location, followed by the lower thoracic esophagus in SCC, with a minority (16%) in the upper thoracic esophagus. Cancer location was almost exclusively in the lower thoracic esophagus for adenocarcinoma.
Table 3.
Pathologic cancer categories of patients receiving neoadjuvant therapy for pure squamous cell carcinoma and adenocarcinoma of the esophagus
| Squamous cell carcinoma (n = 2,045) | Adenocarcinoma (n = 5,686) | |
|---|---|---|
| Category | No. (%) | No. (%) |
| ypT | ||
| ypT0 | 604 (30) | 896 (17) |
| ypTis | 6 (0.30) | 13 (0.24) |
| ypT1 | 220 (11) | 752 (14) |
| ypT2 | 363 (18) | 990 (19) |
| ypT3 | 699 (35) | 2,542 (48) |
| ypT4a | 99 (4.8) | 121 (2.3) |
| ypTX | 54 | 372 |
| ypN | ||
| ypN0 | 1,349 (65) | 2,900 (51) |
| ypN+ | 696 (34) | 2,757 (49) |
| ypN1 | 375 (64)* | 1,138 (48)† |
| ypN2 | 157 (27)* | 748 (32)† |
| ypN3 | 54 (9.2)* | 466 (20)† |
| ypNX | 6 | 29 |
| Number of positive nodes | ||
| 0 | 1,343 (70) | 2,900 (55) |
| 1 | 252 (13) | 672 (13) |
| 2 | 123 (6.4) | 466 (8.9) |
| 3 | 60 (3.1) | 273 (5.2) |
| 4 | 50 (2.6) | 206 (3.9) |
| 5 | 31 (1.6) | 133 (2.5) |
| 6 | 16 (0.83) | 136 (2.6) |
| 7 or more | 54 (2.8) | 466 (8.9) |
| Unknown | 116 | 434 |
| ECLNI | 48 (22)§ | 174 (43)¶ |
| Lymphovascular invasion | 211 (28)†† | 736 (37)‡‡ |
| ypM | ||
| ypM0 | 1,931 (94) | 5,334 (94) |
| ypM1 | 114 (5.6) | 352 (6.2) |
| Grade‡ | ||
| ypG1 | 692 (42) | 1,012 (23) |
| ypG2 | 523 (32) | 1,476 (33) |
| ypG3 | 431 (26) | 1,960 (44) |
| ypGX | 399 | 1,238 |
| Location | ||
| ypUpper | 297 (16) | 31 (0.70) |
| ypMiddle | 850 (47) | 141 (3.0) |
| ypLower | 676 (37) | 4,526 (96) |
| ypLocationX | 222 | 988 |
Neoadjuvant pathologic cancer categories of those with adenosquamous and undifferentiated carcinoma are shown in Supporting Information Table S3.
Data available for 586 patients.
Data available for 2,352 patients.
G4 carcinomas are reported in Supporting Information Table S3.
Data available for 221 ypN+ patients.
Data available for 402 ypN+ patients.
Data available for 743 patients.
Data available for 1,984 patients. ECLNI, extracapsular lymph node invasion.
Non–risk-adjusted survival
Overall survival was 98%, 75%, 33%, and 21% at 30 days, 1, 5, and 10 years, respectively, and was similar for SCC and adenocarcinoma (Supporting Information Fig. S1). Risk of death peaked within months of the first management decision for SCC and within a year for adenocarcinoma, then gradually decreased and plateaued by about 5 years to a near constant rate of 8% per year for both (Supporting Information Fig. S2).
Neoadjuvant pathologic categories (ypTNM)
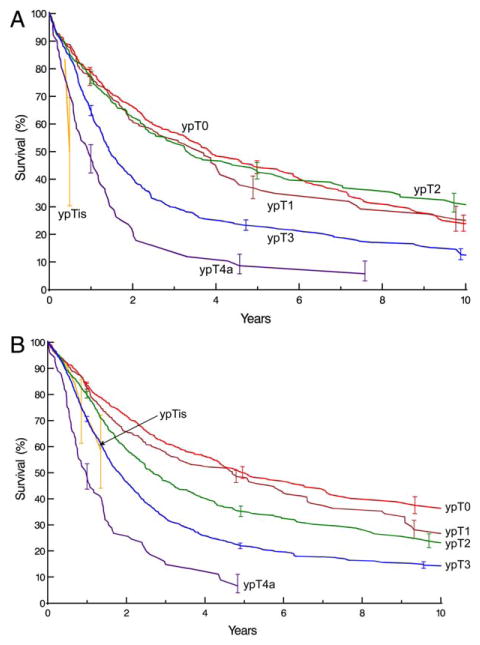
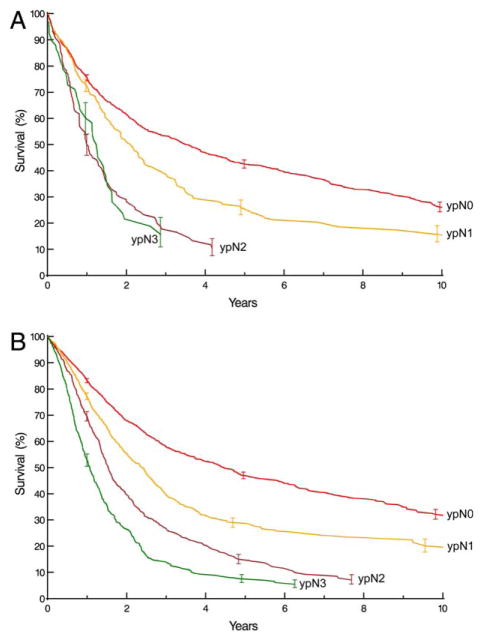
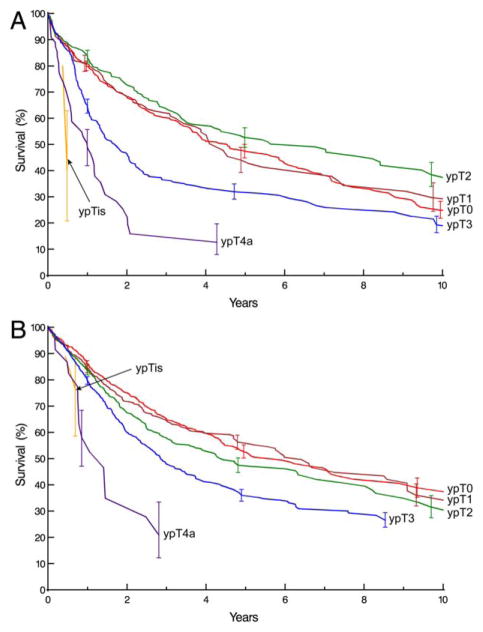
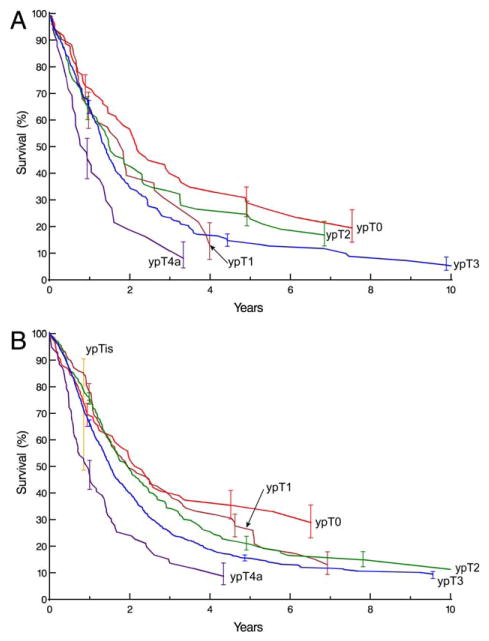
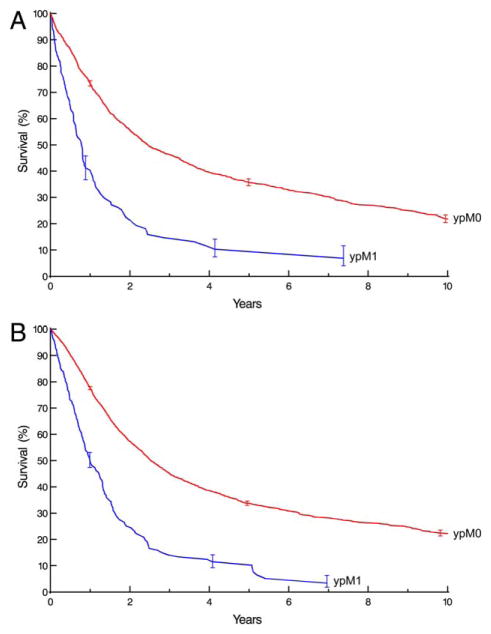
Survival was similar for squamous cell cancers confined to the wall (ypT2 or less), but poor, distinctive, and stratified for ypT3 and ypT4a cancers (Fig. 1A). Survival had a similar pattern for adenocarcinoma, except that ypT2 was distinctive and stratified (Fig. 1B). Survival decreased monotonically and distinctively with presence of regional lymph node metastases (ypN), except for ypN2 and ypN3 SCCs (Fig. 2). Survival diminished markedly with increasing number of regional lymph nodes positive for cancer (Supporting Information Fig. S3). For ypN0 cancers, survival decreased distinctively and monotonically only for ypT3 and ypT4a cancers (Fig. 3). Survival for ypN+ cancers was poor and not well stratified for SCC (Fig. 4A), but was distinctive and stratified for adenocarcinoma (Fig. 4B). Survival decreased with presence of distant metastases (ypM) (Fig. 5).
Fig. 1.
Survival by ypT category. Kaplan-Meier estimates accompanied by vertical bars representing 68% confidence limits, equivalent to ±1 standard error. A. Squamous cell carcinoma. B. Adenocarcinoma.
Fig. 2.
Survival by ypN category. Format is as in Fig. 1. A. Squamous cell carcinoma. B. Adenocarcinoma.
Fig. 3.
Survival by ypT category for ypN0 cancers. Format is as in Fig. 1. A. Squamous cell carcinoma. B. Adenocarcinoma.
Fig. 4.
Survival by ypT category for ypN+ cancers. Format is as in. Fig. 1. A. Squamous cell carcinoma. B. Adenocarcinoma.
Fig. 5.
Survival by ypM category. Format is as in Fig. 1. A. Squamous cell carcinoma. B. Adenocarcinoma.
Other cancer categories
Survival was distinctive for G1 SCC and for G1–3 adenocarcinomas, but generally stratified for both cancers (Supporting Information Fig. S4). Survival was not distinctive or stratified by location in the esophagus (Supporting Information Fig. S5).
Other characteristics
Survival did not stratify well by age, particularly for adenocarcinoma (Supporting Information Fig. S6). Survival was worse for men with SCC than women (Supporting Information Fig. S7A), but similar between the sexes for adenocarcinoma (Supporting Information Fig. S7B).
Treatment
Survival was similar for patients receiving neoadjuvant chemoradiotherapy or chemotherapy, but worse for those receiving radiotherapy (Supporting Information Fig. S8). Patients receiving adjuvant therapy had better early survival, but by 2 years it was slightly worse compared with those who did not (Supporting Information Fig. S9). Survival was not better with increasing number of lymph nodes resected (Supporting Information Fig. S10), and was best for R0 and similar for R1 or R2 resections (Supporting Information Fig. S11).
DISCUSSION
Appropriateness of shared stage groupings
Comparing survival of patients receiving neoadjuvant therapy to that of patients with equivalent pathologic categories receiving surgery alone,3,7 it is evident that prognostic implications for neoadjuvant categories (ypTNM) differ from those of equivalent pathologic categories (pTNM). Survival of node-negative patients receiving neoadjuvant therapy (ypN0) is worse than equivalently pathologically categorized patients receiving esophagectomy alone (pN0); prognosis of node-positive patients receiving neoadjuvant therapy (ypN+) is either worse or no better than equivalent patients receiving esophagectomy alone (pN+). Separate or adjusted stage groupings for patients receiving neoadjuvant therapy based on prognosis would be ideal.
Principal findings
Complete response of the primary cancer (ypT0N0M0) does not ensure good survival. Patients with cancer confined to the wall or less (ypT0-2) and no regional lymph node metastasis (ypN0) have intermediate survival, which is similar across ypT. Persistence of cancer outside the esophageal wall (ypT3/T4a) in node-negative patients and failure to sterilize regional lymph node metastasis (ypN+) is associated with poor survival. In these patients, neoadjuvant therapy has a small survival benefit or may be harmful, depending on the extent of downstaging of cN+ and amount of toxicity. The effect of non-anatomic cancer categories (histologic grade and location) on survival is less evident after neoadjuvant therapy than after esophagectomy alone.
WECC and data assemblage
WECC data for the 7th edition staging manuals was based on pathologic staging of patients undergoing esophagectomy alone.3 This new WECC effort included collecting pathologic staging data for all patients undergoing neoadjuvant therapy and for those who received postoperative adjuvant therapy. This is a unique data set representing the current state of the art in treatment of advanced-stage esophageal cancer, which has replaced esophagectomy alone for such patients. The number of patient characteristics was greater and the data more complete than in the prior WECC effort.3 Thus, this was a global effort of considerable magnitude across geography, institutions, patient characteristics, cancer categories, and treatments. These data will serve as the basis for developing the first data-driven esophageal cancer ypTNM recommendations for the 8th edition cancer staging manuals after risk adjustment for all these variables.
Neoadjuvant patient characteristics
Patients receiving neoadjuvant therapy for esophageal cancer are highly selected. Mean age was less and ECOG performance status better than for the average patient in the WECC database.4 However, comorbidities were numerous, clinically significant, and similar to those in the complete WECC database; collection of these data is essential for risk adjustment of all-cause mortality.
Treatment
Chemoradiotherapy was the principal neoadjuvant therapy. Chemotherapy was administered to approximately a fifth of the patients. Radiotherapy was uncommon, particularly in adenocarcinoma patients. Despite inclusion of many institutions with expertise in less invasive esophagectomy, the vast majority of neoadjuvant patients had a traditional esophagectomy approach. There was significant variability in number of lymph nodes resected, explained in part by the difficulty in performing lymphadenectomy in a pre-treated field. Postoperative adjuvant therapy was administered to approximately 15% of patients.
Neoadjuvant pathologic cancer categories
The majority of primary cancers were sterilized or confined to the esophageal wall (ypT0-2), and the majority of regional lymph nodes were free of cancer (ypN0). However, there was a sufficient number of patients to provide a spectrum of pathologically staged esophageal cancer patients undergoing neoadjuvant therapy. Frequency of histologic grade in decreasing order for SCC was G1, G2, and G3; the inverse was reported for adenocarcinoma. Few patients had G4 cancers, reflecting their rarity. Location was predominately the lower thoracic esophagus in adenocarcinoma patients; there were few patients with adenocarcinoma of the middle thoracic esophagus, and rarely, of the upper thoracic esophagus. The distribution of location for SCC, although predominantly in the middle and lower thoracic esophagus, will be sufficient to permit analysis of the effect of location on risk-adjusted survival. No patients with cervical esophageal cancer were included in the data.
Non–risk-adjusted survival
The endpoint for this study was all-cause mortality.3 This hard endpoint has been shown to provide a truer reflection of death due to cancer than the softer endpoint of disease-specific mortality.8–10
Regardless of histopathologic cell type, survival curves were unequally depressed, more for earlier cancer classifications than for later, compared with pathologic staging after esophagectomy alone.3 Survival was much less distinctive for ypT, grade, and location than seen in pathologically staged cancers treated by esophagectomy alone.3 Survival was substantially different for ypN0 patients versus those with N+. Similarly, survival was substantially different for ypM0 patients versus those with ypM+. The survival benefit of lower histologic grade is less evident in patients with ypTNM cancers than in those with similarly staged pTNM cancers.3
Survival was homogeneous for ypN0 patients for cancer confined to the wall (ypTis-2, ypT1, and ypT2) or those sterilized (ypT0). Survival was poor for ypN+ patients regardless of ypTand number of positive nodes for SCC. Adenocarcinoma patients with ypN1 cancers had better survival compared withypN2-3 patients.
Radiation therapy is less effective than chemoradiotherapy or chemotherapy. Non–risk-adjusted survival was similar for chemotherapy and chemoradiotherapy; however, risk adjustment is necessary to confirm similarity. Further, non–risk-adjusted survival for patients receiving adjuvant therapy was similar to that of patients not receiving it, a finding also requiring risk adjustment to confirm.
Strengths and limitations
Currently, this is the best attempt at providing worldwide pathologic esophageal cancer staging data in patients receiving neoadjuvant therapy. However, patient selection and treatment delivery were not uniform among centers or continents, and these heterogeneities are reflected in heterogeneous survival. Patients treated in North America and Europe predominated. Unlike most registry data, WECC collected more patient and cancer characteristics, specific treatment and start dates were known in all, and follow-up data were available in all. However, not all variables were recorded in all patients.
Limitations include variability of clinical staging, pathologic and staging definitions, and neoadjuvant treatment protocols over time. Where possible, data variables were updated to 7th edition definitions. Stage grouping analyses with risk adjustment will potentially minimize the effect of time. However, changing neoadjuvant treatment over time can only be coarsely corrected for, because there are minimal details about treatment delivered.
An additional limitation of this pure data presentation is that it does not account for patient variables that affect all-cause mortality; the interplay among TNM, histopathologic cell type, histologic grade, and cancer location, in part due to the unique lymphatic anatomy of the esophagus; and the confounding of treatment effects, temporal factors, etiology, diagnosis, and clinical decision making around the world. This analysis does not account for patients’ initial cancer characteristics and variable downstaging.
Clinical implications
These data reinforce the need for improved clinical staging so that fewer cancers are incorrectly staged as advanced (overstaged), needlessly exposing patients to the toxicity of neoadjuvant therapy. If this therapy is to be successful, it is necessary to identify those cancers that will respond to a neoadjuvant approach and spare patients with non-responding cancers (persistent disease invading outside the esophageal wall and persistent nodal metastasis) from neoadjuvant therapy. There is need for targeted, cancer-specific therapy. Hopefully, the shotgun approach of neoadjuvant therapy is temporary and does not represent the future.
CONCLUSIONS
These data demonstrate that patients receiving neoadjuvant therapy do not have equivalent survival to patients with the same pathologic category undergoing esophagectomy alone. For them, separate stage groupings will be used in the 8th edition cancer staging manuals.
Prognostication is possible, but survival is reduced from what has been classically quoted from stage groupings based on esophagectomy alone. Persistent regional lymph node metastases (ypN+) portend poor survival, and sterilization of metastatic regional lymph nodes (ypN0) does not equate with cure. Patients with ypN0 cancers confined to the esophageal wall or those with complete response have an intermediate survival regardless of ypT.
These data will be used to prepare for the 8th edition cancer staging manuals after risk adjustment for many confounding variables. They should direct data collection for the 9th edition. This is a milestone in the pathologic staging of esophageal cancer patients receiving neoadjuvant therapy and provides a direction for future advancements.
Acknowledgments
The authors thank Brian Kohlbacher for assistance with figure annotation and Tess Parry for editorial assistance.
APPENDIX : Worldwide Esophageal Cancer Collaboration: participating institutions and investigators
| Institution | Location | Investigators |
|---|---|---|
| Beijing Cancer Hospital, Peking University | Beijing, China | Ken N. Chen |
| Cleveland Clinic | Cleveland, OH; USA | Thomas W. Rice Eugene H. Blackstone |
| Case Western Reserve University | Cleveland, OH; USA | Carolyn Apperson-Hansen |
| Erasmus Medical Center | Rotterdam, The Netherlands | Bas P.L. Wijnhoven Jan van Lanschot Sjoerd Lagarde |
| Fourth Hospital of Hebei Medical University | Shijiazhuang, Hebei; China | Jun-Feng Liu |
| Fox Chase Cancer Center | Philadelphia, PA; USA | Walter J. Scott Donna Edmondson |
| Groote Schuur Hospital, University of Cape Town | Cape Town; South Africa | Riette Burger |
| Guy’s & St Thomas’ Hospitals | London, UK | Andrew R. Davies Janine Zylstra |
| Helsinki University Hospital | Helsinki; Finland | Jari V. Rasanen Jarmo A. Salo Yvonne Sundstrom |
| Hospital Universitario del Mar | Barcelona; Spain | Manuel Pera |
| Hôpital Nord | Marseille; France | Xavier B. D’Journo |
| Indiana University Medical Center | Indianapolis, IN; USA | Kenneth A. Kesler |
| University of Texas MD Anderson Hospital | Houston, TX; USA | Wayne L. Hofstetter Arlene Correa Stephen G. Swisher |
| Mayo Clinic | Rochester, MN; USA | Mark S. Allen |
| Medical University of South Carolina | Charleston, SC; USA | Chad E. Denlinger |
| Memorial Sloan-Kettering Cancer Center | New York, NY; USA | Valerie W. Rusch |
| University of Queensland, Princess Alexandra Hospital | Brisbane; Australia | B. Mark Smithers David Gotley Andrew Barbour Iain Thomson |
| University of Newcastle upon Tyne | Newcastle upon Tyne; UK | S. Michael Griffin Jon Shenfine |
| Oregon Health & Science University | Portland, OR; USA | Paul H. Schipper John G. Hunter |
| Royal Marsden NHS Foundation Trust | London; UK | William H. Allum |
| Shanghai Chest Hospital | Shanghai; China | Wentao (Vincent) Fang |
| Toronto General Hospital | Toronto, ON; Canada | Gail E. Darling |
| University Zeikenhuizen Leuven | Leuven; Belgium | Tony E.M.R. Lerut Phillipe R. Nafteux |
| University Medical Center Utrecht | Utrecht, The Netherlands | Richard van Hillegersberg |
| University of Alabama at Birmingham | Birmingham, AL; USA | Robert J. Cerfolio |
| Hospital de Clinicas, University of Buenos Aires | Buenos Aires; Argentina | Luis Durand Roberto De Antón |
| The University of Chicago, Department of Surgery | Chicago, IL; USA | Mark K. Ferguson |
| University of Hong Kong Medical Center, Queen Mary Hospital | Hong Kong; China | Simon Law |
| University of Michigan | Ann Arbor, MI; USA | Mark B. Orringer Becky L. Marshall |
| University of Montreal | Montreal, Quebec; Canada | André Duranceau Susan Howson |
| University of Pittsburgh Medical Center | Pittsburgh, PA; USA | James D. Luketich Arjun Pennathur Kathy Lovas |
| University of Rochester | Rochester, NY; USA | Thomas J. Watson |
| University of São Paulo | São Paulo; Brazil | Ivan Cecconello |
| West China Hospital of Sichuan University | Chengdu, Sichuan; China | Long-Qi Chen |
Footnotes
Author contributions: Conception or design of the experiment(s), or collection and analysis or interpretation of data: All authors. Drafting the manuscript or revising its intellectual content: T.W. Rice, C. Apperson-Hansen, and E. H. Blackstone. Approval of the final version of the submitted manuscript: All authors.
SUPPORTING INFORMATION
Additional Supporting Information may be found in online version of this article.
Fig. S1. All-cause mortality of esophageal cancer patients undergoing pathologic staging after receiving neoadjuvant therapy. Vertical bars on Kaplan–Meier estimates represent 68% confidence limits, equivalent to ±1 standard error.
Fig. S2. Instantaneous risk of death (hazard function). Dashed lines represent 68% confidence limits.
Fig. S3. Survival by number of cancer-positive locoregional lymph nodes. Format is as in Fig. 1. A. Squamous cell carcinoma. B. Adenocarcinoma.
Fig. S4. Survival by histologic grade (G1, well differentiated; G2, moderately differentiated; G3, poorly differentiated; G4, undifferentiated). Format is as in Fig. 1. A. Squamous cell carcinoma. B. Adenocarcinoma.
Fig. S5. Survival by upper extent of cancer in the esophagus (location: upper, middle, lower). Format is as in Fig. 1. A. Squamous cell carcinoma. B. Adenocarcinoma.
Fig. S6. Survival by patient age (<60, 60–70, >70 years). Format is as in Fig. 1. A. Squamous cell carcinoma. B. Adenocarcinoma.
Fig. S7. Survival by sex. Format is as in Fig. 1. A. Squamous cell carcinoma. B. Adenocarcinoma.
Fig. S8. Survival by type of neoadjuvant therapy. Format is as in Fig. 1. A. Squamous cell carcinoma. B. Adenocarcinoma.
Fig. S9. Survival by use of adjuvant therapy. Format is as in Fig. 1. A. Squamous cell carcinoma. B. Adenocarcinoma.
Fig. S10. Survival by number of regional lymph nodes resected. Format is as in Fig. 1. A. Squamous cell carcinoma. B. Adenocarcinoma.
Fig. S11. Survival by resection margin (R0, cancer-free; R1, microscopic; R2, macroscopic). Format is as in Fig. 1. A. Squamous cell carcinoma. B. Adenocarcinoma.
Table S1. Characteristics of patients receiving neoadjuvant therapy for adenosquamous and undifferentiated carcinoma of the esophagus
Table S2. Treatment received by patients with adenosquamous and undifferentiated carcinoma of the esophagus
Table S3. Pathologic cancer categories of patients receiving neoadjuvant therapy for adenosquamous and undifferentiated carcinoma of the esophagus
References
- 1.Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A, editors. American Joint Committee on Cancer Staging Manual. 7. New York: Springer-Verlag; 2010. [Google Scholar]
- 2.Sobin LH, Gospodarowicz MK, Wittekind C, editors. International Union against Cancer. 7. Oxford, England: Wiley-Blackwell; 2009. TNM Classification of Malignant Tumours. [Google Scholar]
- 3.Rice TW, Rusch VW, Apperson-Hansen C, et al. Worldwide Esophageal Cancer Collaboration. Dis Esophagus. 2009;22:1–8. doi: 10.1111/j.1442-2050.2008.00901.x. [DOI] [PubMed] [Google Scholar]
- 4.Rice TW, Apperson-Hansen C, DiPaola LM, et al. Worldwide Esophageal Cancer Collaboration: Clinical staging data. Dis Esophagus. 2016 doi: 10.1111/dote.12493. (forthcoming) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goldman AI. Eventcharts: Visualizing survival and other timed-event data. Am Stat. 1992;46:13–8. [Google Scholar]
- 6.Blackstone EH, Naftel DC, Turner ME., Jr The decomposition of time-varying hazard into phases, each incorporating a separate stream of concomitant information. J Am Stat Assoc. 1986;81:615–24. [Google Scholar]
- 7.Rice TW, Rusch VW, Ishwaran H, Blackstone EH. Cancer of the esophagus and esophagogastric junction: data-driven staging for the seventh edition of the American Joint Committee on Cancer/International Union against Cancer Cancer Staging Manuals. Cancer. 2010;116:3763–73. doi: 10.1002/cncr.25146. [DOI] [PubMed] [Google Scholar]
- 8.van Leeuwen PJ, Kranse R, Hakulinen T, et al. Disease-specific mortality may underestimate the total effect of prostate cancer screening. J Med Screen. 2010;17:204–10. doi: 10.1258/jms.2010.010074. [DOI] [PubMed] [Google Scholar]
- 9.Black WC, Haggstrom DA, Welch HG. All-cause mortality in randomized trials of cancer screening. J Natl Cancer Inst. 2002;94:167–73. doi: 10.1093/jnci/94.3.167. [DOI] [PubMed] [Google Scholar]
- 10.Lauer MS, Blackstone EH, Young JB, Topol EJ. Cause of death in clinical research: Time for a reassessment? J Am Coll Cardiol. 1999;34:618–20. doi: 10.1016/s0735-1097(99)00250-8. [DOI] [PubMed] [Google Scholar]