Abstract
Introduction:
Children with cerebral palsy need highly specialized care. This can be very burdensome for families, particularly in large rural states, due to the need for long-distance travel to appointments. In this study, children undergoing the selective percutaneous myofascial lengthening surgery utilized a telephone-based telemedicine evaluation to assess for surgical eligibility. The goal was to avoid a separate preoperative clinic visit weeks before the surgery. If possible, eligibility was determined by telephone, and then, the patient could be scheduled for a clinic visit and possible surgery the next day, saving the family a trip. The purposes of the study were to calculate estimated reductions in miles traveled, in travel expenses, and in carbon emissions and to determine whether the telephone assessment was accurate and effective in determining eligibility for surgery.
Methods:
From 2010 to 2012, 279 patients were retrospectively reviewed, and of those, 161 mailed four-page questionnaire and anteroposterior pelvis X-ray followed by a telephone conference. Geographic information system methods were used to geocode patients by location. Savings in mileage and travel costs were calculated. From 2014 to 2015, 195 patients were additionally studied to determine accuracy and effectiveness.
Results:
The telephone prescreening method saved 106,070 miles in transportation over 3 years, a 38% reduction with US$55,326 in savings. Each family saved an average of 658 (standard deviation = 340) miles of travel and US$343.64 (standard deviation = US$178) in travel expenses. For each increase of 10 miles in distance from the health center, the odds of a patient utilizing telephone screening increased by 10% (odds ratio: 1.101, 95% confidence interval: 1.073–1.129, p < 0.001). After the telephone prescreening, 86% were determined to be likely candidates for the procedure. For 14%, a clinic visit only was scheduled, and they were not scheduled for surgery.
Conclusion:
Families seeking specialized surgical care for their disabled children particularly benefited from this approach.
Keywords: Telemedicine, telehealth, telephone, surgery, cerebral palsy, selective percutaneous myofascial lengthening
Introduction
Selective percutaneous myofascial lengthening surgery
Children with cerebral palsy can often benefit from surgery to lengthen muscle tendon units.1 These surgeries can be through small or large incisions. Selective percutaneous myofascial lengthening (SPML) surgery uses incisions that are so small that sutures are not needed (2–3 mm) possibly making recovery time shorter. Because there are only two major centers that perform the SPML surgery, families often need to travel long distances to get the procedure. The goal of our center is to optimize the entire SPML healthcare experience.
Telemedicine use in pre-surgery evaluation
One of the most important aspects of a surgery is the pre-surgery evaluation. The skill of a surgeon is to do surgery, but also to know which procedures will benefit which patients. Traditionally, telemedicine has been predominantly used for clinical diagnosis and follow-up of non-surgical diseases and processes. Telemedicine as a means for surgical evaluation has been less substantiated. One study found that low-bandwidth Internet-based telemedicine acted as a cost-effective and efficient means for surgical prescreening for adult and pediatric patients undergoing varying general and gynecologic procedures even when located in remote locations.2 Another study analyzing pediatric ear, nose, and throat patients concluded that decisions about need for surgical intervention were equivalent through either videoconferencing or in-clinic observation.3 Postoperative evaluation following laparoscopic procedures through low-bandwidth video, high-resolution images, and voice was also found to be accurate.4
Impact of telemedicine on travel and cost reduction
Some studies exploring the cost-effectiveness and utility of telemedicine have demonstrated prominent reductions in spending, while others have shown no significant statistical difference.5–8 The lack of definitive economic evaluation of telehealth has contributed to impediment in global adoption of telemedicine across medical specialties.9
There is a large body of research on telehealth efficacy and cost-effectiveness.6–8 However, there are fewer papers discussing the direct benefits that patients receive in terms of reduction in travel expenditures. A systematic review from 2011 on teledermatology indicated that roughly 43% of overall travel could be eliminated by adherence to telemedicine protocols.10 Furthermore, a study published in 2015 showed that in a mental health department of a veterans’ hospital in Vermont, telemedicine use minimized patient travel by 145 miles/visit, with total savings of US$63,000 or 3.5% of the total travel pay disbursement for the year.11 Another study in rural Kansas showed that a pediatric psychology telemedicine service could save patients an average of US$138 per consult in travel expenses using the conservative metric of US$0.35/mile.12
Telephone-based telemedicine for surgical evaluation
Telephone-based telemedicine involves a conversation between a physician and a patient or parent discussing the patient’s history and X-ray findings. A family may send in a questionnaire and X-rays, but this would be insufficient to make a decision for surgery. Additionally, an in-depth discussion of the family’s goals and expectations is necessary prior to a decision on surgical intervention. This can only be done as a conversation, and the use of a telephone allows this critical conversation to take place. Telephone-based telemedicine interventions have often been used for delivery of healthcare information to patients with chronic conditions and with those in need of behavioral-based therapy, with satisfactory results.13–15 Ovid and PubMed searches for telephone-based preoperative surgical assessments find a paucity of literature on the topic. Several articles focus on assessing patient preparedness for elective surgery, especially in terms of medical clearance to undergo anesthesia and as a method for reducing patient cancelations, rather than as a focal diagnostic and evaluation strategy for the surgery itself. More commonly, surgical evaluations by telemedicine utilize telephone consultation as a component of the assessment, supplemented with high-resolution imaging and/or videoconferencing.11
Telemedicine use in patients with cerebral palsy
Cerebral palsy is a central nervous system disorder occurring in the first 3 years of life causing physical dysfunction. Cerebral palsy patients present with a variety of medical problems and require continuous follow-up among specialists throughout their care. For example, a single patient may see neurology for seizures, orthopedics for contractures and joint dislocations, wheelchair experts for custom seating, orthotists for braces, and therapists for movement and speech therapy. A retrospective audit looking at pediatric orthopedic patients referred to a telepediatric service found that there was a role for telehealth consultation. There was a role for all patients, but a more substantial benefit for patients with a disability, where the cost and inconvenience of patient transport is considerably higher.16 Additional research on the role of telemedicine in the care of cerebral palsy patients looked at miles traveled by cerebral palsy patients and their families. They concluded that traditional care for cerebral palsy was insufficient and that telemedicine may be a feasible alternative for improving care. They noted that current access to telehealth options was limited.17
Study purpose
The purposes of the study were to calculate estimated reductions in miles traveled, in travel expenses, and in carbon emissions. Another purpose was to determine whether the telephone assessment was equivalent to assessment in the clinic in terms of determining eligibility for surgery.
Methods
SPML procedure and patient evaluation
The setting was a university-based tertiary referral center. The patient population consisted of those from the state of Texas who contacted the center with an interest in the surgery. Patients were not recruited for the study. Patients who lived outside of Texas were excluded to simplify data analysis. The use of the telephone interview was optional. The families who contacted the clinic could be appointed for a pre-surgery evaluation visit without a telephone interview. Those who contacted the surgeon’s office were directed to send in a questionnaire (see Appendix 1) and an X-ray and were subsequently contacted by phone.
We obtained the names of all children with cerebral palsy who underwent surgery utilizing the SPML procedure from January 2010 to December 2012. Children of all gross motor function classification system levels are represented in the study. The goals of this surgery were to increase ambulatory ability in the more functional groups and to aid in comfort and ease of care for the more severely involved children. Of those undergoing the SPML procedure, some had a clinic evaluation followed by surgery weeks in the future. Others had a telehealth evaluation to assess surgical eligibility and then a clinic visit with possible surgery the next day, allowing the clinic visit and the surgery to be done in one trip. The telehealth preoperative interview was used to determine whether these patients would be possible surgical candidates. All patients must undergo a physical examination in person in order to determine the extent of muscle lengthening and specific muscle groups to be targeted. One of the goals of the center is to minimize the impact of travel on families. Pre-surgery screening involved the use of a four-page questionnaire, an anteroposterior pelvis X-ray that families mail, and then a telephone interview with the surgeon. It was usually not necessary to schedule these calls. The surgeon was able to call when he had a break in his schedule. The purpose of the telephone interview was to find out whether there were contractures at the hips, knees, or ankles, and if so, whether they were a significant issue. The telephone interview also addressed any ambiguities in the medication history and prior surgical history. Details of the child’s strategies for mobility were also elicited. The process of studying the X-rays, reviewing the questionnaire, and calling the family took the surgeon 45 min to 1 h. One surgeon with more than 20 years of experience performed all surgeries and all telephone interviews. A video component was not used. The advantage of this was the convenience of reaching families on their home or cellular phones.
Because not all families utilized telephone screening, we were able to compare the distance traveled by the families that utilized or did not utilize the screening.
The year from September 2014 to August 2015 was additionally studied to determine how often the telephone evaluation was successful at eliminating a separate clinic visit and to determine the accuracy of the telephone evaluations in predicting the need for surgery.
To ensure the study was performed ethically, it was approved by our center’s Institutional Review Board (07-166, 01/2010-12/2015) and written consent was obtained from legally authorized representatives of the pediatric patients.
Data analysis
A Microsoft Excel database was constructed that noted whether telephone screening occurred. If an office visit was scheduled with surgery the following day, this was evidence that a trip for evaluation was eliminated with the family staying in a nearby hotel. The patient’s home address and ZIP code were noted.
Geographic information systems (GIS) methods were used, and all geographic analyses were calculated using ArcGIS 10.2.18 Address geocoding was utilized to compare their home address to a database of known addresses and corresponding latitude and longitude coordinates. Euclidian distance between the home address (or centroid of patient ZIP code) and the health center was calculated using the GIS software’s near tool.
Furthermore, the research team collected socioeconomic characteristics of the patient’s home ZIP code (median household income) using data from the 2014 American Community Survey 5-year estimates.19 This was converted into a dichotomous variable based on the ZIP code’s median household income. Incomes were determined to be either above or equal to or below the US median household income of US$53,482.20 When analyzing cost reductions in terms of employment earnings, a number representing the potential cost from lost wages (due to driving to a preoperative visit) also utilized the median household income for this patient population (US$53,482). For this calculation, we used an average of one wage-earning parent present at each clinical assessment, with the assumption that they would miss 1 day of work.
Data were then imported into Stata 14. The GIS software produced distance between patients and the health center. To estimate cost burdens due to mileage, the distance was multiplied by 2 (representing a round-trip visit) and then by US$0.5216 (the average Internal Revenue Service (IRS) mileage rate for business miles driven from 2010 to 2012).20–22 Savings in mileage and costs were calculated by totaling the round-trip mileage distance and cost for those utilizing the telephone screening (equating to one saved visit).
To determine estimated reduction in carbon emissions, the amount of mileage reduction was multiplied by the reference amount of 411 g of CO2 emissions per mile for automobile travel.23
Univariate statistics (proportions for binary variables and means and standard deviations (SDs) for continuous variables) were calculated. To determine whether distance was statistically associated with the odds of utilizing the telephone preoperative assessment, we conducted a logistic regression. Distance served as the independent variable.
Results
Patient population demographics
A total of 317 patients had SPML surgery during this period. Of them, 38 patients were excluded since they lived outside of Texas, leaving 279 patients. Of these patients, 161 or 58% participated in the telemedicine preoperative evaluation. The median age at the time of surgery was approximately 8 years, and 40% of patients were female. Of the 279 patients, 232 patients’ addresses (83%) were successfully geocoded to their exact location. The remaining 47 patient addresses were geocoded to the geographic center (centroid) of their home ZIP code.
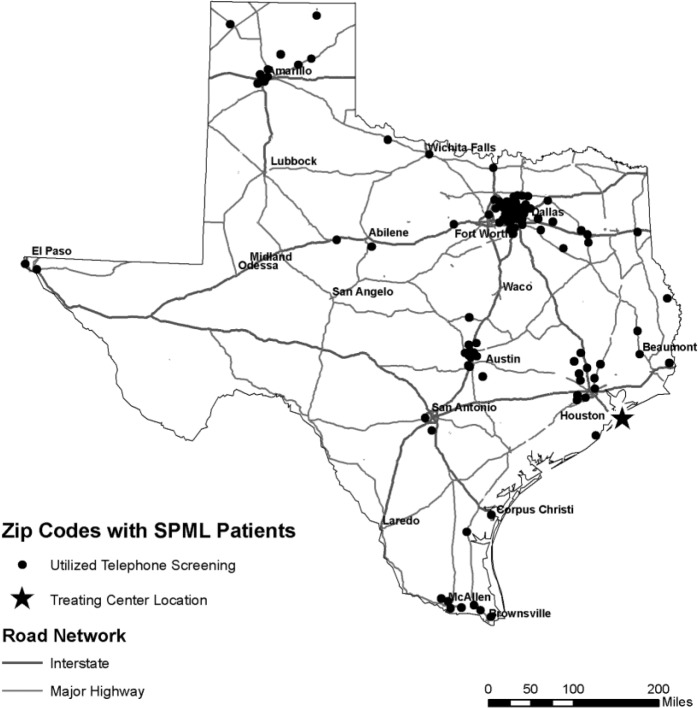
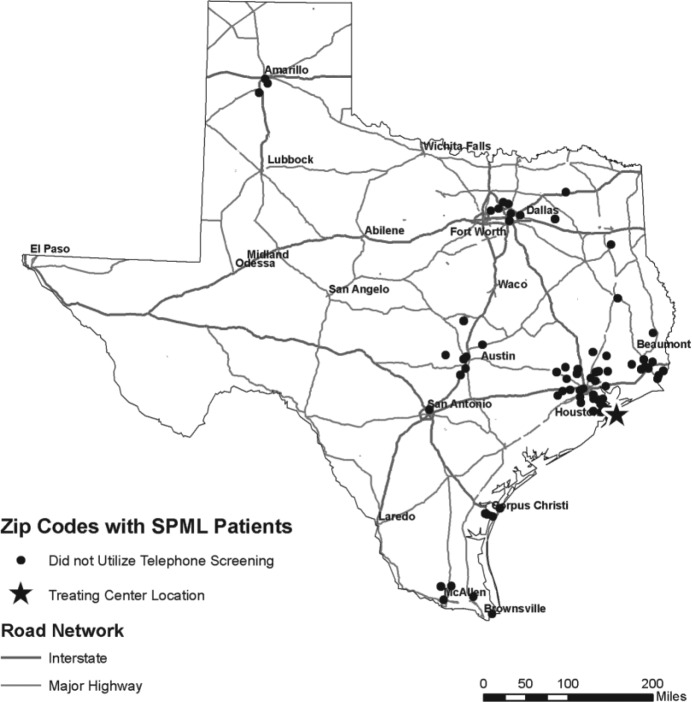
Patients tended to live in or around the major metropolitan areas in the State (Figure 1). Roughly half (50.2%) of the patients lived in ZIP codes where the median household income is below the US median, making travel savings even more beneficial to this patient cohort. Patients’ mean distance from the health center averaged 249 miles (SD = 179) or 498 miles round trip. Those utilizing the telephone-based preoperative screening lived a mean of 329.1 miles (SD = 170) or 659 miles round trip from the health center (Figure 1), compared to 140 miles (SD = 125) or 280 miles round trip for those not utilizing the screening (Figure 2). It appears that distance may play a role in the utilization of telephone-based prescreening. For each increase of 10 miles in distance from the health center, the odds of a patient utilizing telephone screening increased by 10% (odds ratio (OR): 1.101, 95% confidence interval (CI): 1.073–1.129, p < 0.001).
Figure 1.
Those utilizing telephone screening were often from regions distant to the treating center.
Figure 2.
Those not utilizing telephone screening were often from the region of the treating center.
Pre-surgery evaluation
To give more perspective on how the prescreening works in clinical practice, an additional year was examined in more detail. From September 2014 to August 2015, 195 children were screened. Of those, 168 (86%) were determined to be likely candidates for the procedure. However, for the remaining 27, it was unclear whether they were candidates for surgery or not. For those 27, it was recommended to schedule a clinic visit for evaluation. During that same year, 184 SPML surgeries were performed. Zero patients who were initially deemed possibly eligible for surgery from the telehealth screening were then deemed not eligible for surgery during the evaluation the day before the scheduled procedure. In every telehealth case, the patient was seen and a physical examination was done prior to surgery. Therefore, the approach using telehealth to determine surgical suitability is as safe as seeing patients in clinic to determine surgical suitability without telehealth. If during their clinic visit a muscle that was targeted for lengthening by telehealth was not found to be suitable for surgery, then that muscle tendon unit was not lengthened.
Reductions in travel miles, travel expenses, and carbon emissions
The average round-trip distance for all patients was 498 miles and the average cost was US$260 (SD = US$187). By participating in the telephone-based preoperative screening, patients were able to reduce their travel by one round-trip visit. This allowed these patients, who were also located further than average, to save an average of 659 (SD = 340) miles in additional travel distance, saving on average US$344 (SD = US$178). Overall, the telephone prescreening appointment saved 106,070 miles in transportation for this cohort of 161 patients (161 × 659). This equates to US$55,326 in savings from mileage costs alone at the IRS rate of US$0.5216/mile or US$18,442 per year in this 3-year study. Across this cohort, the telephone prescreening reduced miles traveled and mileage costs by 38% (106,070/(279 × 498 × 2)). Additionally, when looking at carbon emissions, at 106,070 miles, there was a total reduction in 43,595 kg of CO2 emissions or 14,532 kg per year in this 3-year study.23
Reductions in lost wages
Estimated cost reductions from lost wages through use of the telephone prescreening were US$205 per patient. The range of savings may vary between US$0 (no wage-earning parents) and US$820 (two wage-earning parents missing 2 days of work each) or more.
Discussion
Telemedicine use in pre-surgery evaluation
Our findings coincide with some evidence that telehealth may be useful for pre-surgical evaluation and postoperative follow-ups for pediatric patients and those with special care needs.2–4,24 This preoperative assessment’s success at determining patient eligibility was reviewed from 2014 to 2015, with 100% of the patients identified as possible surgical candidates (168) subsequently continuing through with surgery the day after their clinic visit. However, this may vary with other diagnoses. Similarly, other studies have shown high accuracy in making appropriate preoperative diagnoses (100% and 99%).2,3 In these situations, telemedicine also eliminated a separate visit for in-clinic evaluation.
Impact of telemedicine on travel and cost reduction
A systematic review on teledermatology indicated that roughly 43% of travel could be eliminated by adherence to telemedicine protocols, compared to 38% found in this study.10 Furthermore, the cost and travel reductions appreciated by cerebral palsy patients and their families (not including calculated lost wages) in our study were actually found to be more drastic compared to other studies cited in the literature. Our study demonstrated reductions of 659 miles per patient compared to 391 miles per consult in the Kansas pediatric psychology telemedicine service study and 147 miles per visit in the Vermont mental health department study.11,12
A unique aspect of the study is the highly specialized nature of SPML surgery. Only a handful of surgeons routinely perform SPML surgery. Therefore, most patients travel a significant distance. Similar savings might also occur when looking at other highly specialized fields. For medical services that are more locally and readily available, travel costs are less encumbering as treatment can generally be performed near the patient.
About 50% of the patients in this study received Medicaid as their form of insurance. Medicaid will reimburse patients for travel costs, lodging, and food expenditures at specific rates. Thus, Medicaid is significantly benefiting through use of telephone evaluations in regards to allocation of its finances. One study wrote that The Centers for Medicare and Medicaid Services have incentivized the use of telemedicine as it has “shown its ability to facilitate meaningful use through technological innovation with savings.”25
Telephone-based telemedicine for surgical evaluation
In this study, the use of telephones made it extremely convenient to contact patients and share information. A telephone conversation was an excellent complement to the additional components of a mailed questionnaire and X-ray images. Other surgical telemedicine studies more frequently relied on videoconference to evaluate their patients.3,4
Telemedicine use in patients with cerebral palsy
Several studies have illustrated the important role that telehealth can play in improving care received by pediatric and disabled patient populations.16,17 Specifically, patients living in more remote areas may be challenged to receive the healthcare they need and thus be more likely to benefit from telehealth services.17 When looking at our study, this may be appreciated by the OR of patients utilizing the preoperative telephone evaluation the farther they were located from the health center (p < 0.001).
Children with cerebral palsy frequently have complicated histories. There is a further advantage to the system of a mailed four-page questionnaire and X-ray followed by telephone conference by the physician. This process results in a comprehensive note in the electronic medical record. On the day of the clinic visit, the surgeon can review the previously obtained history and then concentrate on physical examination and counseling about surgery. It is also beneficial for the surgeon to do an examination of a complicated child with cerebral palsy including gait evaluation the day before the surgery, instead of weeks or months before. That way, the surgeon has recent memory of the child and their examination findings.
Environmental impact
Telemedicine is a climate-friendly strategy for reductions in carbon emissions.26–28 Use of videoconferencing and other communication technology has been shown to reduce carbon emissions by 40–70 times that of physical visits.26 This was similarly noted in our carbon emission analysis.
Limitations
The analysis assumes that all travel was by personal automobile and that their transportation costs equate to the US IRS’s US$0.5216/mile rate. Some patients may have traveled by other means (bus, air, or a mix of other modes). Additionally, only patients residing in Texas were analyzed. Out-of-state and out-of-country patients were not addressed; however, it is likely that they would benefit even more. This report details the experience of one surgeon with over 20 years of experience. It is unknown whether similar results could be obtained by less-experienced physicians.
Conclusion
The use of telemedicine prescreening for the SPML procedure created a patient-centered system focused on minimizing the burden of travel for children with cerebral palsy and their families in order to reduce costs, improve accessibility, and improve the quality of the patient’s overall medical experience. Utilizing software such as GIS is essential to create more patient-centered healthcare networks. Our study adds premise to the role of telephone-based telemedicine in pre-surgical evaluation of pediatric patients with cerebral palsy, especially for those located from further away.
Appendix
Appendix 1.
Patient Questionnaire.
| Name: | |
| Date of Birth: | |
| Home Phone: | |
| Cell Phone: | |
| Other Phone: | |
| Grandparent phone: | |
| E-mail address: | |
| City, State: | |
| Referred by: | |
| Pediatrician: | Phone: |
| Physical Therapist: | Phone: |
| Physiatrist: | Phone: |
| Neurologist: | Phone: |
| Is the child able to walk? If so, can the child walk 20 feet or more in a clinic with or without equipment? | |
| Can the child stand for one minute without assistance? | |
| Does the child use a wheelchair for mobility? NoYes (circle) | |
| Today’s Date: | |
| What name does child go by? What is the child’s overall condition? (example: cerebral palsy, anoxic brain injury) | |
| Reason for seeing Dr. Yngve (example: “tight hamstrings,” “walking on toes”) | |
| History of Present Illness (Provide a brief description of the child’s current problem you are seeking medical attention for): | |
| Are there any current issues the child is experiencing? | |
| Child’s favorite thing (What does he/she like to play with, what interests them?) | |
| Birth history (How many weeks was the baby born at? Was there any problem when the baby was in the womb?) | |
| Brain history (Does the child have cerebral palsy or some other brain disorder? Was this diagnosed with an MRI?): | |
| Any history of Botox injections? (if so, how long have they been getting them and what part of the body was injected?) | |
| Does the child have Ankle Foot Orthoses (AFO’s)? If so, who provides the Orthoses? Assistive devices (example walker; crutches; wheelchair; gait trainer?) Physical Therapy (how many times per week?) | |
| Language ability (Is the child able to communicate fully with you? Are they able to understand what you say? Are they able to show you when they are in pain?) | |
| Pain Questions: Rate your child’s pain in the last week on a scale of 0–10. Where was the pain? Child’s rating? (put n/a if not possible) | |
| PODCI Pain questions:29 (For the following questions put today’s date before the correct response) -During the last week how much of the time did your child feel sick and tired? ________ most ________some ________a little ________ none -During the last week how much of the time did pain or discomfort interfere with your child’s activities? ________ most ________some ________a little ________ none -How much pain has your child had during the last week? _______ none _______ very mild _______ mild _______ moderate _______ severe _______ very severe -During the last week how much did pain interfere with your child’s normal activities including at home, outside of the home and at school? ______ not at all ______ a little bit ______ moderately ______ quite a bit ______ extremely | |
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Ethical approval for this study was obtained from the center’s Institutional Review Board (07-166, 01/2010-12/2015).
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Written informed consent was obtained from all subjects before the study. Written informed consent was obtained from legally authorized representatives of the pediatric patients. Verbal informed consent was obtained from legally authorized representatives before the study.
References
- 1. Mitsiokapa EA, Mavrogenis AF, Skouteli H, et al. Selective percutaneous myofascial lengthening of the lower extremities in children with spastic cerebral palsy. Clin Podiatr Med Surg 2010; 27: 335–343. [DOI] [PubMed] [Google Scholar]
- 2. Lee S, Broderick TJ, Haynes J, et al. The role of low-bandwidth telemedicine in surgical prescreening. J Pediatr Surg 2003; 38: 1281–1283. [DOI] [PubMed] [Google Scholar]
- 3. Smith AC, Dowthwaite S, Agnew J, et al. Concordance between real-time telemedicine assessments and face-to-face consultations in paediatric otolaryngology. Med J Aust 2008; 188: 457–460. [DOI] [PubMed] [Google Scholar]
- 4. Rosser JC, Jr, Prosst RL, Rodas EB, et al. Evaluation of the effectiveness of portable low-bandwidth telemedical applications for postoperative followup: initial results. J Am Coll Surg 2000; 191: 196–203. [DOI] [PubMed] [Google Scholar]
- 5. Currell R, Urquhart C, Wainwright P, et al. Telemedicine versus face to face patient care: effects on professional practice and health care outcomes. Cochrane Database Syst Rev 2000; 2: CD002098. [DOI] [PubMed] [Google Scholar]
- 6. De la Torre-Diez I, Lopez-Coronado M, Vaca C, et al. Cost-utility and cost-effectiveness studies of telemedicine, electronic, and mobile health systems in the literature: a systematic review. Telemed J E Health 2015; 21: 81–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kairy D, Lehoux P, Vincent C, et al. A systematic review of clinical outcomes, clinical process, healthcare utilization and costs associated with telerehabilitation. Disabil Rehabil 2009; 31: 427–447. [DOI] [PubMed] [Google Scholar]
- 8. Mistry H. Systematic review of studies of the cost-effectiveness of telemedicine and telecare. Changes in the economic evidence over twenty years. J Telemed Telecare 2012; 18: 1–6. [DOI] [PubMed] [Google Scholar]
- 9. Miller EA. Telemedicine and doctor-patient communication: an analytical survey of the literature. J Telemed Telecare 2001; 7: 1–17. [DOI] [PubMed] [Google Scholar]
- 10. Wootton R, Bahaadinbeigy K, Hailey D. Estimating travel reduction associated with the use of telemedicine by patients and healthcare professionals: proposal for quantitative synthesis in a systematic review. BMC Health Serv Res 2011; 11: 185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Russo JE, McCool RR, Davies L. VA telemedicine: an analysis of cost and time savings. Telemed J E Health 2016; 22: 209–215. [DOI] [PubMed] [Google Scholar]
- 12. Spaulding R, Belz N, DeLurgio S, et al. Cost savings of telemedicine utilization for child psychiatry in a rural Kansas community. Telemed J E Health 2010; 16: 867–871. [DOI] [PubMed] [Google Scholar]
- 13. Bidargaddi N, Bastiampillai T, Allison S, et al. Telephone-based low intensity therapy after crisis presentations to the emergency department is associated with improved outcomes. J Telemed Telecare 2015; 21: 385–391. [DOI] [PubMed] [Google Scholar]
- 14. Davis AM, Sampilo M, Gallagher KS, et al. Treating rural paediatric obesity through telemedicine vs. telephone: outcomes from a cluster randomized controlled trial. J Telemed Telecare 2016; 22: 86–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Raphael D, Waterworth S, Gott M. Telephone communication between practice nurses and older patients with long term conditions—a systematic review. J Telemed Telecare 2016; 23: 142–148. [DOI] [PubMed] [Google Scholar]
- 16. Rowell PD, Pincus P, White M, et al. Telehealth in paediatric orthopaedic surgery in Queensland: a 10-year review. ANZ J Surg 2014; 84: 955–959. [DOI] [PubMed] [Google Scholar]
- 17. Edirippulige S, Reyno J, Armfield NR, et al. Availability, spatial accessibility, utilisation and the role of telehealth for multi-disciplinary paediatric cerebral palsy services in Queensland. J Telemed Telecare 2016; 22: 391–396. [DOI] [PubMed] [Google Scholar]
- 18. Environmental Systems Research Institute (ESRI). ArcGIS desktop: release 10.2. Redlands, CA: ESRI, http://www.esri.com (2013, accessed 15 January 2016). [Google Scholar]
- 19. U.S. Census Bureau; American Community Survey, 2014 American Community Survey 5-year estimates; using American FactFinder, http://factfinder2.census.gov (2014, accessed 15 January 2016).
- 20. IRS announces 2010 standard mileage rates. IRS, 3 December, https://www.irs.gov/uac/IRS-Announces-2010-Standard-Mileage-Rates (2009, accessed 13 May 2016).
- 21. IRS announces 2011 standard mileage rates. IRS, 3 December, https://www.irs.gov/uac/IRS-Announces-2011-Standard-Mileage-Rates (2010, accessed 13 May 2016).
- 22. IRS announces 2012 standard mileage rates, most rates are the same as in July. IRS, 9 December, https://www.irs.gov/uac/IRS-Announces-2012-Standard-Mileage-Rates,-Most-Rates-Are-the-Same-as-in-July (2011, accessed 13 May 2016).
- 23. EPA. Greenhouse gas emissions from a typical passenger vehicle. The United States Environment Protection Agency: Office of Transportation and Air Quality, https://www.epa.gov/sites/production/files/2016-02/documents/420f14040a.pdf (2014, accessed 13 May 2016). [Google Scholar]
- 24. Hilty DM, Ingraham RL, Yang SP, et al. Multispecialty telephone and e-mail consultation for patients with developmental disabilities in rural California. Telemed J E Health 2004; 10: 413–421. [DOI] [PubMed] [Google Scholar]
- 25. Vo A, Shore J, Waugh M, et al. Meaningful use: a national framework for integrated telemedicine. Telemed J E Health 2015; 21: 355–363. [DOI] [PubMed] [Google Scholar]
- 26. Holmner A, Ebi KL, Lazuardi L, et al. Carbon footprint of telemedicine solutions—unexplored opportunity for reducing carbon emissions in the health sector. PLoS ONE 2014; 9: e105040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lewis D, Tranter G, Axford AT. Use of videoconferencing in Wales to reduce carbon dioxide emissions, travel costs and time. J Telemed Telecare 2009; 15: 137–138. [DOI] [PubMed] [Google Scholar]
- 28. Yellowlees PM, Chorba K, Parish MB, et al. Telemedicine can make healthcare greener. Telemed J E Health 2010; 16: 230–233. [DOI] [PubMed] [Google Scholar]
- 29. Daltroy LH, Liang MH, Fossel AH, et al. The POSNA pediatric musculoskeletal functional health questionnaire: report on reliability, validity, and sensitivity to change. Pediatric Outcomes Instrument Development Group. Pediatric Orthopaedic Society of North America. J Pediatr Orthop. 1998; 18(5): 561–571. [DOI] [PubMed] [Google Scholar]
- 30. Hunt A, Goldman A, Seers K, et al. Clinical validation of the paediatric pain profile. Dev Med Child Neurol. 2004; 46(1): 9–18. [DOI] [PubMed] [Google Scholar]
- 31. Novacheck TF, Stout JL, Tervo R. Reliability and validity of the Gillette Functional Assessment Questionnaire as an outcome measure in children with walking disabilities. J Pediatr Orthop. 2000; 20(1): 75–81. [PubMed] [Google Scholar]
- 32. Graham HK, Harvey A, Rodda J, et al. The Functional Mobility Scale (FMS). J Pediatr Orthop. 2004; 24(5): 514–520. [DOI] [PubMed] [Google Scholar]