Abstract
Background:
In tibial tubercle transfer (TTT) procedures, the osteotomized and transferred tibial tubercle is usually fixed into the host bone using metal screws.
Purpose:
To compare the strength of fixation provided by a single bioabsorbable screw versus a metal screw for TTT.
Study Design:
Controlled laboratory study.
Methods:
Twenty-two pairs of human cadaveric tibiae were used to compare the fixation strength of a single 4.5-mm bicortical bioabsorbable or metal screw for TTT. In our 2-phase biomechanical testing protocol, the specimens were first subjected to a cyclic-loading test (1500 loading cycles between 50 and 300 N at 0.5 Hz frequency), after which they were loaded to failure (single-cycle load-to-failure test). To control for possible differences in bone quality, volumetric bone mineral density was determined using peripheral quantitative computed tomography.
Results:
No significant displacement differences were observed between the 2 groups for the cyclic-loading test. In the subsequent single-cycle load-to-failure test, the mean yield load was 566 ± 234 N in the bioabsorbable screw group and 984 ± 630 N in the metal screw group (P = .002). The failure mode of bioabsorbable screws was breakage and/or bending, and that of metal screws was bending and/or pull-out. Bone density was similar in the 2 groups.
Conclusion:
A metal screw seems to provide greater fixation strength than a biodegradable screw in the TTT of a human cadaveric knee. However, considering the maximum quadriceps pull in vivo, the strength of fixation provided by a biodegradable screw seems clinically sufficient.
Clinical Relevance:
Bioabsorbable screws, particularly if used in duplicate, could provide a viable option for metal screws in TTT fixation.
Keywords: tibial tubercle transfer, screw fixation, osteotomy, cadaver study, biomechanical study
Patellar dislocation is a relatively common knee complaint, especially in physically active young adult populations. In addition to patellar dislocation, various patellofemoral disorders may require surgery to correct abnormalities in the extensor mechanism of the knee.7 Tibial tubercle transfer (TTT) is among the most popular of these surgical procedures. TTT according to Fulkerson et al8 involves osteotomy and transfer of the tibial tubercle toward the anteromedial direction in an attempt to correct the extensor mechanism malalignment and stabilize the patella. TTT has also been used as an unloading procedure in patellofemoral pain and osteoarthritis (OA)8,12 and may be combined with patellofemoral cartilage repair procedures such as autologous cartilage implanting.10
In clinical practice, metal screws are the gold standard for TTT fixation. Although the strength of fixation per se rarely causes a clinical problem, the heads of the screws are occasionally palpable/symptomatic and may thus require removal.15 Ideally, screws manufactured of bioabsorbable material could provide sufficient fixation strength for TTT, possibly eliminating the need for hardware removal and also minimizing the risk of soft tissue irritation.18 To our knowledge, the literature describing the use of bioabsorbable screws in TTT fixation is limited to case reports of fractured tibial tubercle fixation.1,22
Accordingly, the objective of this biomechanical study was to evaluate whether bioabsorbable screws could provide sufficient strength for TTT fixation in comparison with metal screws in a cadaveric tibia model.
Methods
Specimens
The tibiae (with intact patellar tendon and patella) of both limbs were harvested from 22 human cadavers (mean ± SD age, 41 ± 11 years; range, 17-54 years). The harvesting procedure and the use of human cadaveric tissues were approved by a national authority for medicolegal affairs. Seven of the cadavers were female (mean age, 39 ± 11 years; range, 17-49 years) and 15 were male (mean age, 41 ± 11 years; range, 23-54 years). The tibiae were cleansed of adherent muscles and surrounding soft tissues, wrapped in saline-soaked gauze, and stored frozen in −20°C in sealed plastic bags. This preservation procedure has been recommended for knee specimens intended for in vitro testing protocols of the cruciate ligaments and ligament reconstructions2 and has been shown not to affect the mechanical properties of bone tissue.16
Study Groups and Implants Used
The 22 pairs of tibiae were randomized pairwise to the metal and bioabsorbable screw groups, so that the left and right specimens of each cadaver went into a different group (equal number of left and right specimens in both groups).
In the metal screw group, the TTT was fixed with a single standard noncannulated self-tapping fully threaded cortical 4.5-mm stainless steel screw (Smith & Nephew) (metal screw group). In the bioabsorbable screw group, the TTT was fixed with a single bioabsorbable noncannulated fully threaded 4.5-mm self-reinforced polylactide (SR-PLLA) screw (Bionx Implants Ltd) (Figure 1).
Figure 1.

The implants used in the study: a 4.5-mm bioabsorbable fully threaded bone screw (left) and a 4.5-mm metal cortical bone screw (right).
Peripheral Quantitative Computed Tomography Measurements
Peripheral quantitative computed tomography (XCT 3000, Stratec Medizintechnik GmbH) was used to determine trabecular bone density (in mg/cm3) and total bone density (including the cortex surrounding the trabecular bone) at the proximal tibia before specimen preparation and testing. A cross-section of the proximal tibia approximately 2 cm distal from the articular surface was scanned. The trabecular density was determined from the entire cross-section of the proximal tibia to increase the repeatability of the measurement. According to a standardized measurement protocol described by Sievänen et al,20 a constant threshold of 0.420 cm−1 was used to separate soft tissues from the bone tissue, and then the trabecular density was determined by concentrically peeling off 20% of the bone voxels to define a core area consisting exclusively of trabecular bone.
Specimen Preparation
On the day of testing, the specimens were thawed to room temperature. They were kept moist with physiologic saline solution during the preparation, fixation procedures, and biomechanical testing. Each tibia was first cut transversely at the tibial midshaft, approximately 20 cm below the tibial plateau. An osteotomy was then made with an oscillating saw at the level of the tibial tubercle. The length of the osteotomy was approximately 7 cm, with a maximum thickness of 15 mm at the level of the most prominent location of the patellar tendon insertion. The osteotomy was performed in a bevel-cut shape; the osteotomy was oriented straight in the coronal plane and straight or slightly curved in the sagittal plane as viewed from the lateral or medial aspects of the proximal tibia. Accordingly, the protective proximal step-off described by Fulkerson et al8 was not performed, as our intention was to test the fixation without any additional mechanical support (worst-case scenario). The free osteotomized fragment, which included the patellar tendon insertion, was secured back to its original position with a single, fully threaded bicortical 4.5-mm metal or bioabsorbable screw. The screw was centrally placed in the osteotomized fragment and was oriented parallel to the long axis of the tibia and the axis of distraction. To obtain bicortical fixation, the lengths of both the metal (50 mm) and bioabsorbable (60 mm) screws were chosen to exceed the anteroposterior diameter of the proximal tibia. The bicortical fixation of the tuberosity fragment was confirmed visually. To further standardize the specimen preparation, a single surgeon (J.T.N.) performed the osteotomy and fragment fixation.
Biomechanical Testing and Data Analysis
The biomechanical tests were performed using a computer-controlled Lloyd LR 5K mechanical testing machine (J J Lloyd Instruments). For the testing, the specimens were mounted to the machine by specially designed clamps and 8-mm steel bars passed through two 9-mm drill holes made in the tibia and patella: one through the tibia 15 cm below the tibial plateau in a mediolateral direction and another through the patella in an anteroposterior direction. The direction of loading was parallel with the TTT osteotomy and perpendicular to the screw (Figure 2).
Figure 2.

The biomechanical test setup used in the study. The dotted line indicates the osteotomy site.
The biomechanical testing protocol consisted of the cyclic-loading test followed by the single-cycle load-to-failure test. In the cyclic-loading test, the specimens underwent 1500 cycles of loading between 50 and 300 N at a frequency of 0.5 Hz. The response to loading was automatically recorded as a load-displacement curve with a sample rate of 4 Hz. The fixation was evaluated by determining automatically (by the computer connected to the mechanical testing machine) the initial stiffness (determined as the slope of the linear region of the load-displacement curve corresponding to the steepest straight-line tangent to the loading curve of the first loading cycle during the cyclic loading test) and the loading-induced increase in the displacement from the preload level after 1, 10, 50, 100, 250, 500, 1000, and 1500 cycles of loading, respectively. After 1500 loading cycles, the specimens that survived the cyclic loading were tested using a single-cycle load-to-failure test.
In the single-cycle load-to-failure test, a vertical tensile loading parallel with the axis of the TTT osteotomy was performed at a rate of 1.0 m/min until failure of fixation. The specimen’s response to the loading was automatically recorded as a load-displacement curve, and the stiffness (determined as the slope of the linear region of the load-displacement curve corresponding to the steepest straight-line tangent to the loading curve), yield load (described as the load at the point where the slope of the load-displacement curve first clearly decreased), and maximum failure load were determined. The mode of failure was determined visually.
Statistical Analysis
Data are shown as mean ± SD unless otherwise stated. Differences between the groups were determined using a paired t test. A P value less than .05 was considered statistically significant. Statistical analysis was performed using SPSS (version 22.0; IBM Corp).
Results
Volumetric Bone Density
Bone density at the proximal tibia was similar in both groups. In the bioabsorbable screw group the total density was 215 ± 30 mg/cm3 (P = .71) and the trabecular density 174 ± 31 mg/cm3 (P = .30), and in the metal screw group the total density was 217 ± 34 mg/cm3 and the trabecular density 178 ± 40 mg/cm3.
Biomechanical Testing
In the cyclic-loading test, no significant displacement differences were observed between the two groups after 1, 10, 50, 100, 250, 500, 1000, and 1500 loading cycles (Figure 3). However, the initial stiffness was significantly higher in the metal screw group (182 ± 87 N/mm; range, 31-298 N/mm) than in the bioabsorbable screw group (95 ± 60 N/mm; range, 20-193 N/mm; P < .0001). The only failure of fixation during the cyclic-loading test occurred in the bioabsorbable screw group (n = 1), thus total number of specimens for the single-cycle load-to-failure test was 21 and 22 in the bioabsorbable and metal screw groups, respectively. The failed specimen and its pair were excluded from the statistical analysis.
Figure 3.
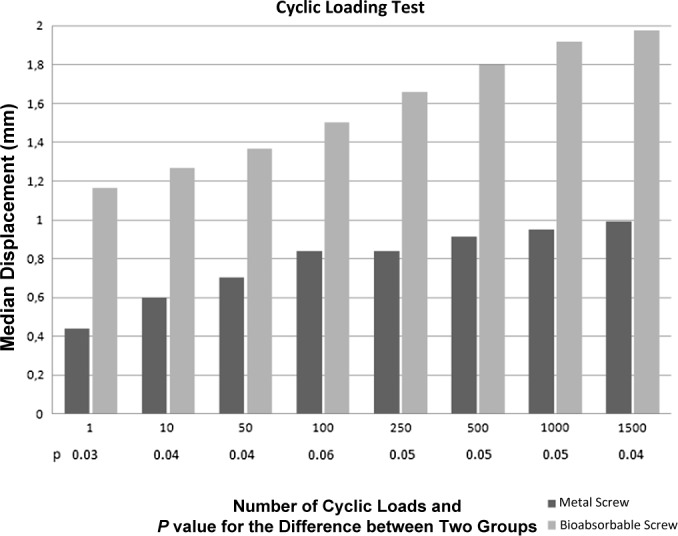
Loading-induced displacement (mean ± SD) observed in the bioabsorbable and metal groups during the cyclic-loading test.
In the single-cycle load-to-failure test made after the cyclic-loading test, the mean yield load was 566 ± 234 N (range, 325-1047 N) in the bioabsorbable screw group and 984 ± 630 N (range, 342-2400 N) in the metal screw group (P = .002). The respective values for the stiffness of the fixation were 125 ± 28 N/mm (range, 62-162 N/mm) and 138 ± 32 N/mm (range, 84-214 N/mm) for the bioabsorbable and metal groups (P = .189). The mean maximum failure loads were 724 ± 172 N (range, 415-1047 N) and 1163 ± 524 N (range, 553-2400 N), respectively (P = .001). The failure modes of the bioabsorbable screws were breakage and/or bending of the screw. For the metal screws, the failure modes were bending and/or pull-out of the screw.
Discussion
The principal finding of the present study was that no significant displacement differences were observed between the metal and bioabsorbable screw groups in the cyclic-loading test, while the single cycle-to-failure test showed higher mean yield load with the metal screw. Although the metal screw provided higher fixation strength, the fixation strength, provided by the bioabsorbable screw exceeded the estimated maximum force required to resist extensor mechanism pull against gravity, and accordingly, we consider that both screws provide clinically sufficient strength for TTT fixation. According to the prevailing understanding on knee biomechanics,11,19 the average maximum quadriceps force subjected to the tibial tubercle is estimated to be approximately 350-390 N during the extension phase of the knee in ordinary walking. We considered this value a rough estimate of fixation strength required for safe fixation of the transferred tibial tubercle to the altered position.3,5,13
To our knowledge, this study is the first to compare the performance of bioabsorbable and metal screw fixation in the TTT procedure. Bioabsorbable fixation implants have several clinical advantages in comparison with conventional metal implants. Most important, the use of bioabsorbable implants eliminates the need for secondary surgery for hardware removal. Also, in contrast to metal implants, bioabsorbable implants do not interfere with imaging or cause stress shielding, growth restriction, or accumulation of metals in tissues. The main disadvantage of bioabsorbable implants is the difficulty in controlling the degradation process. The increased rate of degradation has particularly been associated with adverse biological and chemical reactions, that is, allergic or foreign body reactions, cyst formation, and delayed migration of the screw.17
On the other hand, bioabsorbable materials currently approved for clinical use are not as strong as stainless steel or titanium, and therefore implants made out of these materials are usually mechanically weaker than conventional metal fixation devices and always need to be tested specifically according to indication.23,24
While the strength provided by a fixation implant is undoubtedly one of the most important issues (along with tissue compatibility) in terms of the safety of a novel orthopaedic implant, it has to be kept in mind that conventional metal implants have also been proven to sometimes represent an “overkill”—that is, a stronger fixation or a more rigid construct than what is actually required for many applications.14,18 In this context, the study results showed that the stiffness of the constructs with metal or bioabsorbable screw fixation behaved differently during consecutive tests of cyclic loading and single cycle-to-failure. In the metal screw group, the initial stiffness was 182 ± 87 N/mm, obviously reflecting the high elastic modulus of the metal screw, but it decreased to 125 ± 28 N/mm during the final cycle-to-failure test. Theoretically, the large difference in elastic modulus between metal screw and host bone might cause micromotion and gap formation at interface, decreasing the stiffness of the fixation construct while retaining its strength.21 In contrast, in TTT with bioabsorbable screw fixation, the initial stiffness was 95 ± 60 N/mm during cyclic loading but increased to 138 ± 32 N/mm during the final cycle-to-failure test. This might reflect the lower yield strength of bioabsorbable screws. The initial cyclic loading resulted in plastic deformation of the construct and thus greater force was needed during final cycle-to-failure testing to deflect the fixation construct. The concept of biological fracture fixation with elastic properties of fixation material close to the host bone has been noted previously.9
The only failure of TTT fixation observed during biomechanical testing took place in the bioabsorbable screw group during the cyclic-loading test. Based on the macroscopic analysis of the failed specimen, it seemed that the failure was related to a local defect in the quality of trabecular bone, as no detectable macroscopic surface damage or bending of the screw could be detected. This hypothesis is further supported by the fact that the contralateral specimen failed at 395 N in the load-to-failure test (specimen excluded due to failure of the bioresorbable specimen), a fixation strength far below the average of 984 N found in the rest of the specimens in the metal group.
In this study, TTT fixation with even a single bioabsorbable screw exceeded the normal estimated maximum quadriceps pull-out forces at the tibial tubercle. From a biomechanical point of view, we decided to test TTT fixation with a single screw only to avoid an extensively strong fixation method unable to detect any clinically relevant failure loads near to the previously reported thresholds6,11,19 for tibial tubercle fixation failure. Furthermore, TTT fixation is usually performed with 2 screws, and based on a minimal4,8 number of studies reporting problems associated with the procedure, fixation strength does not seem to be a serious clinical problem. In contrast, the typical complications are usually related to surgical technique, fracture risk in the early postoperative period, and the need for hardware removal in the later phase due to tissue irritation.
Some limitations in our study design require consideration. First, the clinical relevance of findings obtained in cadaveric experiments needs to be assessed with caution. The obvious limitation of our biomechanical testing model is the inability to incorporate all possible forces imposed on the osteotomy site during early postoperative mobilization after TTT. To circumvent this apparent concern, we used a construct that could be considered a worst-case scenario: a TTT without the proximal step-cut, fixed with only 1 screw and loaded parallel to the osteotomy line. Also, from the point of standardizing the biomechanical testing, the use of a drill jig (to control the exact position of fixation screws) would have been preferable for our study setup.
A short period of immobilization of the knee joint with or without restricted weightbearing (eg, because of the use of crutches) is sometimes advocated after a TTT procedure. In this biomechanical cadaveric study, no bone healing or tissue integration occurred at the site of the osteotomy, and therefore, the testing situation simulated early mobilization after surgery and the ability of the sole fixation to resist extensor tensile forces during the immediate postoperative phase. Based on the study data, sufficient TTT fixation strength for early mobilization after surgery can be achieved with both the bioabsorbable and the metal screw. However, we suggest that in clinical practice the fixation of the TTT be performed with 2 screws, and meticulous surgical technique should always be used when performing TTT osteotomy.
In conclusion, considering the typical maximum quadriceps pull in humans,19 even a single bioabsorbable bicortical screw seems to provide sufficient fixation strength for the TTT procedure. Although the results of this biomechanical experiment suggest that bioabsorbable screw(s) could provide a viable option for metal screw(s) in the fixation of anteromedial TTT, the external validity of this notion needs to be assessed in a prospective, randomized clinical trial.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
Ethical approval was not sought for the present study.
References
- 1. Benz G, Kallieris D, Seebock T, McIntosh A, Daum R. Bioresorbable pins and screws in paediatric traumatology. Eur J Pediatr Surg. 1994;4:103–107. [DOI] [PubMed] [Google Scholar]
- 2. Beynnon BD, Amis AA. In vitro testing protocols for the cruciate ligaments and ligament reconstructions. Knee Surg Sports Traumatol Arthrosc. 1998;6(suppl 1):S70–S76. [DOI] [PubMed] [Google Scholar]
- 3. Caldwell PE, Bohlen BA, Owen JR, et al. Dynamic confirmation of fixation techniques of the tibial tubercle osteotomy. Clin Orthop Relat Res. 2004;424:173–179. [DOI] [PubMed] [Google Scholar]
- 4. Cosgarea AJ, Freedman JA, McFarland EG. Nonunion of the tibial tubercle shingle following Fulkerson osteotomy. Am J Knee Surg. 2001;14:51–54. [PubMed] [Google Scholar]
- 5. Cosgarea AJ, Schatzke MD, Seth AK, Litsky AS. Biomechanical analysis of flat and oblique tibial tubercle osteotomy for recurrent patellar instability. Am J Sports Med. 1999;27:507–512. [DOI] [PubMed] [Google Scholar]
- 6. Davis K, Caldwell P, Wayne J, Jiranek WA. Mechanical comparison of fixation techniques for the tibial tubercle osteotomy. Clin Orthop Relat Res. 2000;380:241–249. [DOI] [PubMed] [Google Scholar]
- 7. Dejour D, Le Coultre B. Osteotomies in patello-femoral instabilities. Sports Med Arthrosc. 2007;15:39–46. [DOI] [PubMed] [Google Scholar]
- 8. Fulkerson JP, Becker GJ, Meaney JA, Miranda M, Folcik MA. Anteromedial tibial tubercle transfer without bone graft. Am J Sports Med. 1990;18:490–496. [DOI] [PubMed] [Google Scholar]
- 9. Giannoudis PV, Einhorn TA, Marsh D. Fracture healing: the diamond concept. Injury. 2007;38(suppl 4):S3–S6. [DOI] [PubMed] [Google Scholar]
- 10. Gigante A, Enea D, Greco F, et al. Distal realignment and patellar autologous chondrocyte implantation: mid-term results in a selected population. Knee Surg Sports Traumatol Arthrosc. 2009;17:2–10. [DOI] [PubMed] [Google Scholar]
- 11. Grood ES, Suntay WJ, Noyes FR, Butler DL. Biomechanics of the knee-extension exercise. Effect of cutting the anterior cruciate ligament. J Bone Joint Surg Am. 1984;66:725–734. [PubMed] [Google Scholar]
- 12. Hall MJ, Mandalia VI. Tibial tubercle osteotomy for patello-femoral joint disorders. Knee Surg Sports Traumatol Arthrosc. 2016;24:855–861. [DOI] [PubMed] [Google Scholar]
- 13. Mani S, Kirkpatrick MS, Saranathan A, Smith LG, Cosgarea AJ, Elias JJ. Tibial tuberosity osteotomy for patellofemoral realignment alters tibiofemoral kinematics. Am J Sports Med. 2011;39:1024–1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Miller DL, Goswami T. A review of locking compression plate biomechanics and their advantages as internal fixators in fracture healing. Clin Biomech (Bristol, Avon). 2007;22:1049–1062. [DOI] [PubMed] [Google Scholar]
- 15. Morshuis WJ, Pavlov PW, de Rooy KP. Anteromedialization of the tibial tuberosity in the treatment of patellofemoral pain and malalignment. Clin Orthop Relat Res. 1990;255:242–250. [PubMed] [Google Scholar]
- 16. Pelker RR, Friedlaender GE, Markham TC, Panjabi MM, Moen CJ. Effects of freezing and freeze-drying on the biomechanical properties of rat bone. J Orthop Res. 1984;1:405–411. [DOI] [PubMed] [Google Scholar]
- 17. Pereira H, Correlo VM, Silva-Correia J, Oliveira JM, Reis RL, Espregueira-Mendes J. Migration of “bioabsorbable” screws in ACL repair. How much do we know? A systematic review. Knee Surg Sports Traumatol Arthrosc. 2013;21:986–994. [DOI] [PubMed] [Google Scholar]
- 18. Post WR, Fulkerson JP. Distal realignment of the patellofemoral joint. Indications, effects, results, and recommendations. Orthop Clin North Am. 1992;23:631–643. [PubMed] [Google Scholar]
- 19. Rupp S, Hopf T, Hess T, Seil R, Kohn DM. Resulting tensile forces in the human bone-patellar tendon-bone graft: direct force measurement in vitro. Arthroscopy. 1999;15:179–184. [DOI] [PubMed] [Google Scholar]
- 20. Sievänen H, Koskue V, Rauhio A, Kannus P, Heinonen A, Vuori I. Peripheral quantitative computed tomography in human long bones: evaluation of in vitro and in vivo precision. J Bone Miner Res. 1998;13:871–882. [DOI] [PubMed] [Google Scholar]
- 21. Tencer AF. Biomechanis of fixation and fractures In: Rockwood CA, Green DP, Bucholz RW, eds. Rockwood and Green’s Fractures in Adults. 6th ed Philadelphia, PA: Lippincott Williams & Wilkins; 2006. 1–42. [Google Scholar]
- 22. Tuompo P, Partio E, Rokkanen P. Bioabsorbable fixation in the treatment of proximal tibial osteotomies and fractures. A clinical study. Ann Chir Gynaecol. 1999;88:66–72. [PubMed] [Google Scholar]
- 23. Väänänen P, Koistinen A, Nurmi J, Lappalainen R. Biomechanical in vitro evaluation of the effect of cyclic loading on the postoperative fixation stability and degradation of a biodegradable ankle plate. J Orthop Res. 2008;26:1485–1488. [DOI] [PubMed] [Google Scholar]
- 24. Väänänen P, Nurmi JT, Lappalainen R, Jank S. Fixation properties of a biodegradable “free-form” osteosynthesis plate with screws with cut-off screw heads: biomechanical evaluation over 26 weeks. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:462–468. [DOI] [PubMed] [Google Scholar]


