Abstract
Cetuximab and panitumumab are anti‐epidermal growth factor receptor (anti‐EGFR) monoclonal antibodies used as therapies for metastatic colorectal cancer patients. Intrinsic mechanisms of resistance, such as RAS mutations, can prevent patients from having a response with clinical benefit. The clinical efficacy of EGFR targeted antibodies is limited by the development of acquired (secondary) resistance, which typically occurs within 3–12 months from the start of therapy. Preclinical models and analyses of clinical samples have uncovered some of the alterations that confer a selective advantage to tumor cells when under the pressure of anti‐EGFR therapy. Molecular profiling of clinical specimens confirmed that genetic alterations of genes in the EGFR‐RAS‐RAF‐MEK signaling pathway and of receptor tyrosine kinases are mechanisms of acquired resistance to anti‐EGFR antibodies. The escape from anti‐EGFR blockade appears to converge on the (re)activation of MEK‐ERK or AKT as revealed in preclinical studies. Circulating tumor DNA and patient derived xenografts have proven useful tools to monitor patients for resistance to anti‐EGFR therapy and test combination therapies to overcome or reverse resistance.
Keywords: Anti-EGFR therapy, Cetuximab, Panitumumab, Colorectal cancer, Acquired resistance, RAS, MET
Highlights
Metastatic colorectal cancer patients can acquire resistance to anti‐EGFR therapy.
Acquired resistance is driven by alterations in the EGFR‐RAS‐MEK pathway.
Resistance mechanisms converge at activation of MEK‐ERK or AKT.
Abbreviations
- BEAMing
beads, emulsions, amplification, and magnetics
- CRC
colorectal cancer
- ctDNA
circulating tumor DNA
- EGFR
epidermal growth factor receptor
- FOLFIRI
leucovorin, 5‐fluorouracil, and irinotecan
- FOLFOX
leucovorin, 5‐fluorouracil, and oxaliplatin
- HGF
hepatocyte growth factor
- mCRC
metastatic colorectal cancer
- NSCLC
non‐small cell lung cancer
- OS
overall survival
- PDX
patient derived xenograft
- PFS
progression free survival
- RTK
receptor tyrosine kinase
- TKI
tyrosine kinase inhibitor
- VEGF
vascular endothelial growth factor
- VEGFR
vascular endothelial growth factor receptor
1. Introduction
Colorectal cancer (CRC) is a worldwide health burden with nearly 1.2 million new cases expected each year globally (Brenner et al., 2013). CRC is the third leading cause of cancer related deaths among men and women in the United States (Siegel et al., 2013) and second and third among European men and women, respectively (Malvezzi et al., 2013). The stage at diagnosis determines the treatment. At stage IV when distant metastases are present, combination chemotherapy regimens such as FOLFOX (leucovorin, 5‐fluorouracil, and oxaliplatin) or FOLFIRI (leucovorin, 5‐fluorouracil, and irinotecan) associated with anti‐Epidermal Growth Factor Receptor (EGFR) agents (cetuximab or panitumumab) or antiangiogenic drugs (bevacizumab or aflibercept) are used with the aim of prolongation of survival or even cure if resection of liver‐limited metastases is achieved (Adam et al., 2009). When colorectal cancer is localized, there is a five‐year survival rate of about 90% but it drops to near 12% once there are distant metastases (Siegel et al., 2012). It is due to poor outcomes like these, along with our increased knowledge on genetic and biochemical alterations in colorectal cancer, that there has been a surge in research on targeted therapies with the hope of improving overall survival.
There is much evidence suggesting that the presence of aberrant signaling by the EGFR, a member of the ErbB tyrosine kinase receptors (TKRs) is implicated in the progression of colorectal cancers. EGFR can activate the RAS‐RAF‐MEK as well as the AKT‐PI3K pathways leading to cell proliferation and survival making it a suitable target for inhibition. Anti‐EGFR therapies have been developed including monoclonal antibodies as well as small molecule tyrosine kinase inhibitors. The monoclonal antibodies cetuximab and panitumumab, which bind the EGFR receptor, are approved for treatment of colorectal cancer. These antibodies bind to the EGF receptor on the cell surface preventing ligand binding and dimerization, which inhibits its activation (Li et al., 2005). Consequently, this blocks the signal transduction pathway (Mendelsohn and Baselga, 2000).
The use of cetuximab and panitumumab in mCRC patients has been shown to be successful (Cunningham et al., 2004; Jonker et al., 2007; Van Cutsem et al., 2009; Van Cutsem et al., 2007). However, treatment with cetuximab or panitumumab as single agents were only effective in a minority of patients, as low as 10% in some instances (Cunningham et al., 2004; Van Cutsem et al., 2007), which implied that there was intrinsic resistance to this targeted therapy. Further analyses revealed that activating mutations in the KRAS gene, which is downstream from EGFR in the RAS‐MEK‐ERK signaling pathway, prevents both anti‐EGFR antibodies from working effectively (Amado et al., 2008; Benvenuti et al., 2007; Karapetis et al., 2008; Lièvre et al., 2006). Mutations in codons 12 and 13 of KRAS were the first recognized mechanisms of primary resistance to anti‐EGFR therapy. Rightly so, all patients are now screened for KRAS mutations prior to administration of these targeted therapies (Schmoll et al., 2012). More recently, mutations affecting other codons of KRAS (61, 117 and 146) as well as mutations in the related oncogene NRAS have been recognized (De Roock et al., 2010) then validated as biomarkers of resistance to cetuximab or panitumumab (Douillard et al., 2013; Stintzing et al., 2013). However, even RAS wild type patients can be non‐responders to anti‐EGFR therapy. Additional mechanisms of intrinsic resistance have been attributed to mutations in BRAF and PIK3CA (De Roock et al., 2010; Sartore‐Bianchi et al., 2009); amplification of HER2 (Bertotti et al., 2011), MET (Bardelli et al., 2013), and KRAS (Smith et al., 2010; Valtorta et al., 2013); and loss of PTEN expression (Frattini et al., 2007), all of which are components of or interact with the EGFR signal transduction pathway. In addition to these negative predictive molecular alterations, the copy number of the EGFR gene has been also proposed as a positive candidate biomarker for predicting response of CRC to anti‐EGFR therapy (Laurent‐Puig et al., 2009; Moroni et al., 2005; Sartore‐Bianchi et al., 2007). Signal enumeration in solid tumor sections by FISH is challenging to interpret, and it has been shown that molecular diagnosis of EGFR gene copy number by FISH largely diverge among pathology centers with fluctuations covering the whole range of proposed cut‐offs of predictive usefulness from literature (Sartore‐Bianchi et al., 2012). Overexpression of HER3 (Scartozzi et al., 2011) and IGF1 (Scartozzi et al., 2010) may also contribute to resistance.
Even for patients who do respond to anti‐EGFR therapy, the outlook is poor as most only demonstrate measurable results for 3–12 months before eventually progressing (Cunningham et al., 2004; Van Cutsem et al., 2007). This progression upon therapy is termed acquired resistance. In this review, we explore recent discoveries on the mechanisms of acquired resistance to anti‐EGFR therapy in metastatic colorectal cancer. We further propose strategies to rationally overcome this secondary resistance.
2. Preclinical models of acquired resistance to EGFR blockade
Colorectal cancer (CRC) cell lines are a useful resource for analyzing the mechanisms of acquired resistance to targeted therapies and have been used extensively to clarify this unsettling problem. Long term exposure of drug sensitive cell lines to either acute or incremental treatment with anti‐EGFR agents results in the emergence of resistant cell populations. These can then be analyzed biochemically, genetically, and clonally in vitro as well as in vivo to determine how and why they no longer respond.
2.1. Genetic alterations in the RAS‐RAF‐MEK signal transduction pathway
The colorectal cancer cell lines LIM1215 and DiFi were two of the cell lines used for modeling acquired resistance to cetuximab as both are sensitive to inhibition of EGFR (Misale et al., 2012) especially DiFi as they display amplification and overexpression of wild type EGFR. These cell lines function as good models for metastatic colorectal cancer patients (mCRC) that would receive cetuximab treatment as neither have the genetic alterations that are known to be associated with intrinsic resistance (KRAS, BRAF, and PIK3CA). Genetic analyses of the resistant populations revealed that LIM1215 acquired G13D or G12R mutations in KRAS (Misale et al., 2012), which, notably, is also the most well characterized mediator of primary resistance to cetuximab (Amado et al., 2008; Karapetis et al., 2008; Lièvre et al., 2006). The resistant DiFi, on the other hand, no longer had amplification/overexpression of EGFR and instead exhibited amplification of wild type KRAS (Misale et al., 2012). Given that KRAS mutations are the predominant form of primary resistance, it should come as no surprise that they would be involved in acquired resistance as well. To confirm that these alterations could actually cause resistance, they were experimentally introduced in parental DiFi and LIM1215. Both mutations and amplification of KRAS triggered loss of sensitivity to cetuximab. In the presence of cetuximab, KRAS activity was not depleted for both resistant cell lines, and this was concomitant with maintained phosphorylation of MEK and ERK, particularly in the LIM1215 resistant cells. Pharmacological inhibition of MEK but not PI3K when combined with cetuximab also sensitized the resistant cells to anti‐EGFR therapy. This was in concordance with the absence of altered AKT phosphorylation in the resistant cells (Misale et al., 2012).
Further analyses in additional CRC cell lines sensitive to anti‐EGFR antibodies (including HCA‐46, NCI‐H508, and OXCO‐2) unveiled additional mechanisms of acquired resistance to either cetuximab or panitumumab (Misale et al., 2014). In the resistant populations, KRAS, BRAF, and NRAS mutations were found, and some cell lines exhibited multiple mutations. These results reinforce the notion that intratumor heterogeneity contributes to resistance as multiple mechanisms were found within the same cell line. KRAS amplification was exhibited in cetuximab resistant DiFi, HCA‐46, and NCI‐H508 and also in panitumumab resistant NCI‐H508. Once again, this demonstrates that mechanisms that can cause primary resistance can also cause acquired resistance (Smith et al., 2010; Valtorta et al., 2013). Resistant populations containing KRAS mutations or amplification were analyzed for downstream activation revealing that they have active KRAS, as well as phosphorylated MEK and ERK. However, siRNA knockdown of MEK as well as pharmacologic inhibition with the MEK1/2 inhibitor pimasertib did not attenuate the resistant cells. Notably, only when MEK and EGFR were concomitantly inhibited did the resistant cells start to respond, and this was confirmed in mouse xenografts regardless of the mechanism of resistance (Misale et al., 2014). This implies that there is a convergent evolution of resistance at MEK and ERK activation. In these resistant cells, MEK inhibition only transiently inhibits ERK phosphorylation, but is reactivated following phosphorylation of EGFR. This is why the MEK inhibitor must be given simultaneously with the anti‐EGFR agent in the experimental models and possibly also in clinical protocols.
2.2. Alteration of the receptor tyrosine kinase VEGFR signaling
Additional studies for mechanisms of acquired resistance to anti‐EGFR therapy in colorectal cancer were completed using GEO cells (Bianco et al., 2008; Ciardiello et al., 2004). Analogous to mCRC patients, GEO cell mouse xenografts began progressing after 12 weeks of treatment with either cetuximab or the small molecule EGFR inhibitor gefitinib (Ciardiello et al., 2004). Using these resistant xenografts to generate cell lines allowed for more in‐depth analysis. GEO cells, however, have been shown to have a mutation in KRAS (G12A) (Paranavitana, 1998), which may explain why they are less sensitive to anti‐EGFR therapy than some cells with wild type KRAS (Liska et al., 2011). Compared to parental cells, vascular endothelial growth factor (VEGF) was secreted at higher levels by the resistant cells (Ciardiello et al., 2004), and they had increased levels of VEGFR1 but not VEGFR2 (Bianco et al., 2008). Pharmacological inhibition of the VEGF receptor (VEGFR) using vandetanib inhibited the growth of the resistant xenografts and could deplete phosphorylated AKT in resistant cells (Bianco et al., 2008; Ciardiello et al., 2004). It appears that the inability to inhibit the phosphorylation of AKT, possibly mediated by VEGFR1, contributed to the resistance to anti‐EGFR therapy (Bianco et al., 2008).
2.3. Amplification of the tyrosine kinase receptor HER2
Yonesaka et al. (2011) also used a CRC cell line (GEO) along with the non‐small cell lung cancer (NSCLC) HCC827 cells in their analysis of the mechanisms of acquired resistance to cetuximab. GEO cells were exposed to increasing amounts of cetuximab and several resistant clones were isolated. Three of the seven clones that were isolated demonstrated HER2 amplification that corresponded with increased protein expression. As was shown with the KRAS, NRAS, BRAF mutant resistant cells (Misale et al., 2014), treatment with cetuximab was ineffective at depleting ERK1/2 phosphorylation in the GEO resistant cells. Unlike in the studies described in Section 2.1 (Misale et al., 2014, 2012), the effects of silencing or ectopic expression of HER2 were not explored in the GEO cells; however, shRNA silencing and overexpression of HER2 in the HCC827 cells restored sensitivity and conferred resistance to cetuximab, respectively. There was a synergistic response of the GEO resistant cells when treated with a combination of cetuximab and the HER2 inhibitor trastuzumab reinforcing the importance of HER2 in resistance. Further analyses in the NSCLC cell line suggested that it was ERK1/2 phosphorylation that was critical to the HER2 amplification mediated resistance to cetuximab, which was shown to remain phosphorylated in the presence of cetuximab in the GEO resistant cells. Cetuximab could not inhibit growth of HCC827 xenografts overexpressing HER2, and HER2 co‐precipitated with EGFR suggesting that HER2/EGFR heterodimers form in resistant cells.
The influence of HER2 in cetuximab resistance is not limited to the receptor alone but also to the HER3/4 ligand heregulin (Yonesaka et al., 2011). GEO and DiFi CRC cell lines demonstrated a decrease in sensitivity to cetuximab in the presence of heregulin. Heregulin treatment also partially prevented a decrease in the phosphorylation of ERK1/2, HER2, and HER3 in the presence of cetuximab suggesting these receptors can vicariously activate ERK1/2.
2.4. S492R EGFR mutation preventing binding of cetuximab
As with HER2, alterations to the receptor tyrosine kinase (RTK) EGFR can also contribute to acquired anti‐EGFR resistance. Montagut and colleagues used DiFi as a model for monitoring anti‐EGFR resistance mechanisms (Montagut et al., 2012). Cetuximab could not block ERK or AKT phosphorylation in their resistant clones. However, these clones did respond to gefitinib and panitumumab implying their continued dependence on EGFR. Sequencing analysis of the EGFR gene revealed a missense mutation yielding a serine to arginine at codon 492 (S492R), which was shown to hinder cetuximab binding. Expressing this mutant form of EGFR in NIH3T3 cells resulted in retention of EGFR activity in the presence of cetuximab but not panitumumab. The clinical relevance of these findings is that panitumumab may be effective in mCRC cases in which resistance to cetuximab is due to the S492R mutation.
2.5. Altered regulation of EGFR by ubiquitination and Src
The influence of EGFR on resistance to anti‐EGFR therapies is not limited to genetic alterations. Lu and colleagues derived a cetuximab resistant DiFi line following long term increasing exposure to the antibody (Lu et al., 2007). These resistant DiFi did show not only a decrease in EGFR expression, but also a slower migration when analyzed by Western blot. The altered migration was attributed to an increased association with the Cbl‐protein and ubiquitination. Ubiquitin targeting of EGFR was explained to be the reason for decreased amounts of EGFR, which differed from what Misale and colleagues found previously (Misale et al., 2012). Gene amplification was not analyzed in the current study (Lu et al., 2007). It could be indicative of two independent mechanisms of EGFR down‐regulation in DiFi cells.
Biochemical analysis of EGFR phosphorylation revealed that the resistant cells responded to EGF stimulation with increased tyrosine phosphorylation of the Src‐dependent Y845 (Lu et al., 2007). Src too had higher basal levels of phosphorylation at the positive regulatory site, Y416, in the resistant cells. Combining the Src inhibitor PP2 with cetuximab increased apoptosis in the resistant cells compared to the Src inhibitor alone. This drug combination also reduced phosphorylation of AKT to a level similar to cetuximab treated parental cells, but this was not recapitulated with ERK phosphorylation. This suggests that AKT phosphorylation is more likely mediating cetuximab induced apoptosis in these cells and shows potential for combining anti‐EGFR with anti‐Src therapy. Similar results were seen in the NSCLC cell line NCI–H226 as cetuximab resistant cells were dependent on Src activity. Treatment of these cells with Src‐family kinase inhibitor dasatinib reduced active AKT and could resensitize the cells to cetuximab (Wheeler et al., 2009).
Several of these studies involved the same cell lines, which resulted in differing mechanisms of resistance. Due to heterogeneity it is not surprising to find that within one cell line there could be multiple mechanisms. It is possible that differences in the generation of the resistant lines contributed to the differences in resistance. This was observed in lung cancer cell lines given stepwise and high exposure to gefitinib. For example, the HCC827 cells given the stepwise increase in drug acquired MET amplification, but this was not observed in the high dose resistant cells. Rather, these resistant cells exhibited epithelial to mesenchymal transition and a more stem like phenotype (Shien et al., 2013). Differences were noted in other cell lines as well. It could be that the mechanisms of resistance may be dependent on the microenvironment exerting the pressure (Shien et al., 2013).
3. Acquired resistance to EGFR blockade in patients
The development of preclinical models of acquired resistance allows detailed biochemical analysis of the signaling pathways and provides experimental tools to overcome resistance. For the preclinical models to be of relevance, it is, however, necessary to determine if these mechanisms also occur in clinical samples. As mentioned previously, one feature of colorectal cancer or cancer in general is genetic heterogeneity, and it is very likely that this feature contributes greatly to the mechanisms of resistance to anti‐EGFR as well as other therapies. It also makes it difficult to analyze pre‐ and post treatment tissue as there can be both inter‐ and intratumor heterogeneity if there are multiple metastases. In light of the high level of intratumor heterogeneity, definition of the mechanisms of resistance would in principle require access to multiple regional biopsies. This procedure is invasive and often cannot be performed in the clinical setting. To tackle these issues, multiple groups have started to exploit circulating tumor DNA (ctDNA), an approach often termed “liquid biopsy”. to assess the genotype of the tumor during treatment with targeted agents. Although not without limitations, the molecular profiling of ctDNA has proven useful in analyzing anti‐EGFR refractory patients.
3.1. Genetic alterations acquired in the RAS‐RAF‐MEK signal transduction pathway
The role of the RAS‐RAF‐MEK pathway in colorectal cancer patients has been highlighted by studying tumor tissue from patients that became refractory to cetuximab or panitumumab treatment (Misale et al., 2012). The molecular profiles of relapsed tumors from a cohort of 10 patients who had received anti‐ EGFR antibodies revealed KRAS amplification in one case and KRAS mutations in 6 cases. On the contrary, KRAS alterations were not detected in patients given chemotherapy alone. Analysis of ctDNA in serially collected plasma samples allowed detection of mutant KRAS as early as 10 months before progression was radiologically assessed. A similar approach was simultaneously exploited by Diaz et al. (2012) who analyzed serially collected serum samples from 28 patients for mutations in KRAS and BRAF (in 23). Nine of the 24 patients that were KRAS wild type prior to panitumumab treatment showed mutations in KRAS in their blood while undergoing therapy; three patients had more than one mutation. Three of these patients demonstrated KRAS mutations before it was confirmed by radiologic evaluation that their tumor had progressed. Both of these studies support the use of liquid biopsy not only to find mechanisms of resistance but, more importantly, to monitor patients for disease progression which will be useful for prevention or reversal of resistance. Further analyses of plasma samples from patients who relapsed upon anti‐EGFR treatment revealed that in addition to KRAS, NRAS and BRAF mutations can also be detected in plasma (Bettegowda et al., 2014; Misale et al., 2014). Notably, more than one mutation was often observed in the same patient again indicating that multiple clones can be selected for during treatment (Bettegowda et al., 2014; Misale et al., 2014).
3.2. Amplification of the receptor tyrosine kinase HER2
In their study of in vitro resistance to cetuximab, described in Section 2.2, Yonesaka et al. (2011) included analyses of CRC patients as well. The effects of HER2 amplification were demonstrated both as an intrinsic mechanism of resistance as well as acquired. They determined that both progression free survival (median PFS 149 days vs. 89 days) and overall survival (median OS 515 days vs. 307 days) were longer for patients without HER2 amplification and receiving cetuximab. Two of the patients that developed clinical resistance to cetuximab demonstrated increased amplification of HER2 in their post treatment tissue compared to pretreatment. An additional analysis of 9 patients with pre‐ and post treatment serum found that 2 of the patients had higher levels of the HER2 extracellular domain in their serum when they progressed on cetuximab treatment. An additional cohort of 70 patients also demonstrated that patients with lower levels of the HER3/4 ligand heregulin in plasma prior to treatment with cetuximab were more likely to have a partial response. Findings in plasma were supported by measurement of heregulin mRNA expression in the tumor tissue from 44 patients. In 7 patients that acquired resistance, the levels of heregulin were generally higher post treatment compared to pretreatment. These results again support the notion that a mechanism of acquired resistance may also be a mechanism of intrinsic resistance. As a matter of fact, HER2 amplification as a mechanism of intrinsic resistance was also reported in a large mCRC patient derived xenograft study. Bertotti and colleagues discovered that a subset of these non‐responding xenopatients that were wild type for other genes associated with cetuximab resistance (KRAS, NRAS, BRAF, and PIK3CA) harbored HER2 amplification (Bertotti et al., 2011). Interestingly, in a cohort of patients with colorectal cancer, it was found that 5.05% indeed had HER2 amplified tumors (Marsoni et al., 2013); thus providing together with the xenopatient data (Bertotti et al., 2011) the rationale for an ongoing clinical study with HER2‐targeted therapy in mCRC patients after failure of standard therapies including cetuximab or panitumumab (Marsoni et al., 2013).
Lung cancer, like colorectal, also responds to anti‐EGFR inhibitors. However, the small molecule tyrosine kinase inhibitors (TKIs) are the primary anti‐EGFR agents used in the clinic. Lung cancer patients also relapse during anti‐EGFR treatment, but the majority has a mutation in EGFR (T790M) that prevents binding of the drug (Kobayashi et al., 2005; Pao et al., 2005). As described in colorectal cancer, HER2 amplification was also found in the tissue of patients that acquired resistance to the TKIs gefitinib and erlotinib (Takezawa et al., 2012). Interestingly, it did not coexist with the EGFR T790M mutation. Ectopic expression of HER2 in the NSCLC preclinical models confirmed the capability of HER2 to mediate resistance to erlotinib (Takezawa et al., 2012).
3.3. S492R EGFR mutation preventing binding of cetuximab
The S492R EGFR mutation described in Section 2.3 was confirmed clinically (Montagut et al., 2012). In 2 out of 10 patients that progressed following initial response to cetuximab, the S492R mutation was detected in post treatment tissue. One of these two patients also had a BRAF V600E mutation in their pre‐ and post treatment tissue even though there was an initial response to treatment. Interestingly, both patients had EGFR amplification in pre‐ and post treatment samples. EGFR amplification is also present in the DiFi parental cells (Misale et al., 2012), which were the cells that generated the resistant clones with the S492R mutation (Montagut et al., 2012). The in vitro findings with the cetuximab resistant S492R mutant DiFi cells, described in Section 2.4, prompted the administration of panitumumab to one of the two patients with the S492R EGFR mutation. There was an initial objective response and subsequent progression after 5 months from beginning of treatment. No further analyses were possible to determine the additional mechanism of resistance. Montagut and colleagues did not detect the S492R EGFR mutation in the tumors of 156 treatment naive mCRC patients. This was confirmed recently by Esposito et al. (2013) who also did not detect the mutation in a cohort of 505 patients indicating that this mutation may be unique to acquired resistance and is not related to primary resistance.
3.4. Amplification of the tyrosine kinase receptor MET
Clinical and preclinical evidences indicate that amplification or constitutive activation of the MET gene confers resistance to cetuximab and panitumumab. Stimulation of the MET receptor by its ligand hepatocyte growth factor (HGF) could confer resistance to cetuximab and panitumumab in CRC cells and xenografts (Bardelli et al., 2013; Liska et al., 2011; Troiani et al., 2013), but this could be overcome both by pharmacological inhibition and expression silencing of MET (Bardelli et al., 2013; Liska et al., 2011). HGF mediated resistance may function by preventing anti‐EGFR inhibition of ERK and AKT phosphorylation (Bardelli et al., 2013; Liska et al., 2011). A recent study on 7 CRC patients that progressed following initial response to cetuximab found that three harbored KRAS mutations and three had amplification of MET in post treatment tissue (Bardelli et al., 2013). Overexpression of MET in preclinical CRC models could confer resistance to anti‐EGFR therapy (Bardelli et al., 2013), and pharmacological inhibition and silencing of MET in cetuximab resistant cells could restore sensitivity (Troiani et al., 2013). Careful analysis of the pretreatment tumor demonstrated that in two of the post treatment MET amplified patients there was no amplification, but in the third patient there was a rare occurrence of MET amplification (Bardelli et al., 2013). Amplification in these patients correlated with increased expression of the MET protein. A PCR based approach was devised to detect MET amplification in circulating tumor DNA. Using this approach, MET amplification was reportedly present prior to computed tomography scan detection of disease progression. In untreated patient derived CRC xenograft samples, MET amplification appears to be an infrequent event being present in 2 of the 196 cases (Bardelli et al., 2013). Cetuximab treatment was ineffective on these xenopatients. Notably, MET amplification was found in samples that were KRAS, NRAS, BRAF, PIK3CA, and HER2 wild type adding another mechanism of intrinsic resistance to cetuximab.
As was demonstrated for HER2 in lung cancer, MET was also identified as a tyrosine kinase inhibitor resistance mechanism. Amplification of MET and the EGFR T790M mutation were found in the tumor tissue sample of NSCLC patients post relapse on TKI and they were not mutually exclusive (Engelman et al., 2007). Preclinical models showed that MET amplification mediated resistance by sustaining PI3K/AKT activation through HER3 (Engelman et al., 2007).
4. Selection of pre‐existing resistant clones or therapy‐induced resistant clones
One important issue regarding acquired resistance to any targeted therapy is if the resistant clone was present before therapy was given and selected for under drug pressure or was it truly “acquired”. Misale and colleagues used deep sequencing and high precision BEAMing (beads, emulsions, amplification, and magnetics) on the parental cell lines LIM1215 and DiFi, which were used to generate resistant clones, to determine if the mutations that were selected for in the resistant population were present (Misale et al., 2012). They could detect the KRAS G13D mutation in the LIM1215 parental cells at a rate of 0.2% but not the G12R mutation that was also present at the onset of resistance. Also, the KRAS amplification in the DiFi resistant cells was detected in the parental population with a prevalence of 1:40,000 cells (Misale et al., 2012). This is in support of the theory that acquired resistance very well could be a selection of clones that give a preferential advantage while under the pressure of cetuximab.
Diaz et al. (2012) also addressed this topic. They used the ctDNA from the serum samples that they had collected from CRC patients to calculate the tumor growth rate in order to mathematically model the evolution of tumor progression during treatment. Using this model, they determined that it is unlikely that the resistant clone is absent at the initiation of treatment. There is some evidence, though, that mutations that lead to resistance can be acquired during drug treatment. For example, Misale et al. (2012) were unable to detect the LIM1215 cetuximab resistant KRAS G12R mutation in the LIM1215 parental cells implying that this mutation was acquired during treatment (or that the current technology was unable to detect the low number of mutant cells). However, using single cell cloning of KRAS wild type LIM1215 cells, the same authors demonstrated that following prolonged exposure to cetuximab this clonal population did eventually develop resistance and presented a KRAS A146T mutation. Interestingly, LIM1215 is a cell line displaying microsatellite instability (MSI) and, therefore, the acquisition of a KRAS mutation (Misale et al., 2012) could be a consequence of the higher mutation rate in this model. MET amplification was also not always observed pretreatment (Bardelli et al., 2013). Using deep sequencing, Montagut et al. (2012) were unable to detect the EGFR S492R mutation in the pretreatment tumor samples from patients who had this mutation in their post treatment tumor sample. Given inter‐ and intratumor heterogeneity it is possible that the ability to detect the mutation was limited by the region of the tumor biopsied. In conclusion, secondary resistance most likely arises as an expansion of pre‐existent clones under the pressure of EGFR‐targeted monoclonal antibodies; however, it cannot be ruled out that mutations can be also acquired during therapy.
5. Acquired resistance and convergent evolution
We have discussed at this point seven different mechanisms of acquired resistance to EGFR blockade in colorectal cancer (Table 1). So the question is how many roads can lead to acquired resistance? Based on the clinical characteristics and ctDNA analyses of patients that relapse on panitumumab therapy, Diaz and colleagues estimated the number of mutations that can generate resistance by mathematical modeling. Given the high number of patients that acquire KRAS mutations post treatment, they concluded that the number of mutations that can give rise to a resistant clone is quite small, about 42 nucleotide changes (approximately 10 genes if similar to mutations in KRAS) (Diaz et al., 2012). Not all of the mechanisms that have been described, however, are directly related to a known mutation. Three involve amplification of a gene and two are due to altered regulation or altered protein expression. Remarkably, all the mechanisms appear to converge at very few signaling nodes: MEK‐ERK and AKT (Figure 1). Convergent evolution of mutations in cancer samples has been demonstrated in analyses of intra‐ and inter‐tumor heterogeneity in renal cell carcinoma patients (Gerlinger et al., 2012). Phylogenetic analysis of the mutations found in multiple regions of the primary tumor as well as the metastasis of one patient revealed a convergent evolution of loss of function of SETD2 histone methyltransferase and KDM5C demethylase. Three distinct mutations in SETD2 were found in three independent regions of the tumor/metastases and three in KDM5C found in two regions (not mutually exclusive). A second patient also exhibited convergent evolution of SETD2 and PTEN mutations (Gerlinger et al., 2012). This suggests that loss of function of these genes (or the pathways they control), no matter what the mechanism, confers a selective advantage in these tumors. When comparing to convergent evolution of acquired resistance, regardless of the resistance mechanism, there appear to be two nodes whose deregulation allow the tumor to survive in the presence of the drug: active MEK‐ERK or AKT. Cells that are capable of keeping these nodes active in spite of EGFR inhibition will be selected for under the pressure of the drugs. Even if there are multiple roads to resistance, if all of the roads lead to the same intersection, this may give us a strategy to reverse resistance.
Table 1.
Mechanisms of acquired resistance.
| Resistance mechanism | Clinically validated | Putative strategy to overcome resistance | References |
|---|---|---|---|
| KRAS/NRAS mutations | Yes | Anti‐EGFR with MEK inhibitor | Misale et al. (2012, 2014); Diaz et al., (2012) |
| KRAS amplification | Yes | Anti‐EGFR with MEK inhibitor | Misale et al. (2012, 2014) |
| HER2 amplification | Yes | Anti‐EGFR with anti‐HER2 | Yonesaka et al. (2011) |
| EGFR S492R mutation | Yes | Panitumumab | Montagut et al. (2012) |
| Altered regulation of EGFR (ubiquitination and Src) | No | Anti‐EGFR and Src inhibitor | Lu et al. (2007) |
| Altered VEGF/VEGFR | No | Anti‐VEGFR | Ciardiello et al. (2004); Bianco et al. (2008) |
| Altered/amplification of MET | Yes | Anti‐EGFR with MET inhibitor | Troiani et al. (2013); Bardelli et al. (2013) |
Figure 1.
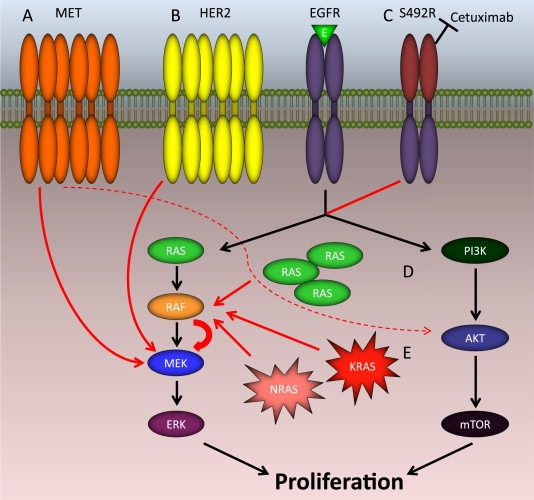
Diagram of clinically detected mechanisms of acquired resistance to anti‐EGFR antibody therapy in colorectal cancers. (A) Amplification/activation of MET bypasses the blockade of the EGFR pathway. (B) Amplification/activation of HER2 bypasses the blockade of the EGFR pathway. (C) The S492 EGFR mutation prevents cetuximab from binding to the receptor. (D) Amplification of KRAS activates the RAS‐RAF‐MEK pathway. (E) Mutations in RAS constitutively activate the RAS‐RAF‐MEK pathway. E: EGFR ligands.
6. Overcoming acquired resistance to anti‐EGFR therapy
We have touched on the mechanisms of acquired resistance to anti‐EGFR therapy that have so far been discovered in CRCs. Given the high molecular heterogeneity associated with this disease, it is likely that more will be found. Several tumor samples or cell lines that do not fit any of the already described mechanisms are available. It is promising that for most of the pathways/genes that are altered, there is already a targeted therapy under study offering hope for combination or secondary therapy.
CRC patient derived xenograft (PDX) models are a great resource for testing combination therapies for overcoming resistance and have already been put to good use. The advantage of using PDXs is that they recapitulate better the heterogeneity of a patient than cell lines and also can provide indications of toxicity, which can hamper combination therapies. Essentially PDX can represent the best preclinical proxy of the disease. For example, a PDX was generated from the tumor of a patient that acquired resistance to cetuximab, which was found to harbor an A146T KRAS mutation (Misale et al., 2014). Treating the expanded transplants of this PDX with cetuximab and the MEK inhibitor pimasertib slowed tumor growth and reduced the size when compared to the monotherapy arms. PDX studies were also designed using the tissue from two patients: one with MET amplification pretreatment (intrinsic) and the other with MET amplification post treatment (acquired) (Bardelli et al., 2013). Both xenopatients were treated with cetuximab and the MET inhibitors crizotinib and JNJ‐38877605. The intrinsic resistant sample demonstrated an initial response to crizotinib followed by progression. Progression was slower when combined with cetuximab. There was a more effective response in those treated with JNJ‐38877605 with or without cetuximab. In the acquired resistance sample, however, there was no enhancement of response when crizotinib was combined with cetuximab. The JNJ‐38877605 combination with cetuximab was much more effective in producing control of disease progression; however, JNJ‐38877605 is a laboratory tool and is not used clinically. Both of these studies provide proof‐of‐principle that combination treatments can be effective at restoring sensitivity to resistant tumors.
The one advantage in these PDX examples is that the mechanism of resistance was known prior to initiating treatment. This information in a clinical setting will allow the clinicians to make an informed decision when assigning a patient to a therapeutic regimen. Depending on how specific the drug is for its target, not knowing the resistance mechanism can doom the combination treatment for failure.
In addition to the valuable preclinical models that can assist in defining the efficacy of agents capable of targeting resistant tumors, a recently developed technology can assist with real‐time monitoring of the mechanisms of resistance in patients' blood. This approach is commonly referred to as liquid biopsy and is based on the detection of resistant alleles in circulating tumor DNA. Independent laboratories reported that genetic alterations connected to acquired resistance in colorectal cancer patients can be detected in blood prior to radiological documentation of progression (Bardelli et al., 2013; Diaz et al., 2012; Misale et al., 2012). Liquid biopsies have even been used effectively for exome sequencing in order to the monitor the evolution of resistance (Murtaza et al., 2013). This approach opens up the possibility of monitoring patients for resistance to the drug during their treatment. This information can allow the clinicians to decide whether to continue treatment or combine the treatment with another therapy to prevent or reverse the progression.
An alternative to overcoming resistance is to prevent it from emerging by using combination treatments as first line targeted therapy rather than after the patient has progressed on therapy. But, it is not that simple. The combination of chemotherapy and anti‐VEGF bevacizumab with or without anti‐EGFR antibodies in the CAIRO2 and PACCE clinical trials showed that combining the two antibodies had higher toxicity and did not improve the outcome (Hecht et al., 2009; Tol et al., 2009). Toxicity will have to be carefully considered when combining therapy. Recently though, in BRAF mutated melanoma there was a tremendous breakthrough with combination targeted therapy. After one year of treatment with the combination of the BRAF inhibitor dabrafenib with the MEK inhibitor trametinib, 41% of the metastatic melanoma patients were alive and progression free which was significantly higher than the 9% of patients that had received monotherapy (Flaherty et al., 2012). As with colorectal cancer, melanoma patients receiving BRAF inhibitors also progress on therapy in less than one year (Sosman et al., 2012). This combination has now been FDA approved for use in the clinic giving promise to the possibility of delaying resistance by using the right combination of targeted therapy first (www.fda.gov/newsevents/newsroom/pressannouncements/ucm381159.htm). Given what we have stated about the convergent evolution of acquired resistance at MEK/ERK in colorectal cancer, this positive outcome in melanoma gives hope that combining the anti‐EGFR antibodies with MEK inhibitors can also delay the onset of resistance.
7. Conclusions
Cancer cells are amazing examples of Darwinian evolution as those with advantageous alterations can survive selection in stressful conditions such as exposure to targeted agents directed against key oncogenic alterations. It is likely that the heterogeneity of colorectal cancer contributes to the multiple mechanisms of resistance. The mechanisms of acquired resistance to EGFR blockade that have been confirmed clinically range from genetic alterations in members of the EGFR‐RAS‐RAF‐MEK pathway to amplification of receptor tyrosine kinases. Most of these mechanisms such as genetic alterations in the RAS‐RAF‐MEK pathway, HER2 amplification, and MET amplification have already been demonstrated as mechanisms of primary resistance, but other mechanisms such as the EGFR mutation S492R appear unique to the acquired resistance setting. With the advances in sequencing technology, such as exome sequencing of ctDNA, it is likely that more genetic alterations will be discovered. Whether they are pre‐existing or acquired during treatment, it appears that there are a limited number of mutations that contribute to resistance, which is good news. We can see, though, that the mechanisms may not always be due to genetics but altered protein regulation as well, which will be more difficult to identify clinically. It is interesting that even though these mechanisms are so different, they all appear to converge at very few nodes: MEK‐ERK or AKT. It may also be true that even if a genetic identifier cannot be found, there is a similar evolutionary convergence in these resistant cells. This holds a great deal of promise for future treatment strategies as we can hopefully exploit these nodes to ideally prevent resistance or reverse it.
Notes added in proof
After acceptance of our manuscript Mohan and colleagues reported the emergence of secondary KRAS, MET and HER2 gene copy amplification in the plasma of 7/10 mCRC patients undergoing anti‐EGFR therapy: Mohan, S et al. PLoS Genet (2014) http://dx.doi.org/10.1371/journal.pgen.1004271
Acknowledgments
Supported by the European Community's Seventh Framework Programme under grant agreement no. 259015COLTHERES (A.B. and S.S.); AIRC IG grant no. 12812 (A.B.); AIRC MFAG n. 11349 (F.D.N.); “Farmacogenomica” –5 per mille 2009 MIUR – Fondazione Piemontese per la Ricerca sul Cancro – ONLUS (F.D.N.); AIRC 2010 Special Program Molecular Clinical Oncology 5 per mille, Project n. 9970 (A.B. and S.S.); FPRC 5 per mille 2010 Ministero della Salute (A.B.); Ministero dell'Istruzione, dell'Università e della Ricerca, progetto PRIN (A.B.); Progetti di Ateneo‐2011, Università di Torino (codice ORTO11RKTW to A.B.); Oncologia Ca' Granda ONLUS (OCGO) Fondazione (S.S.); Grant Terapia Molecolare dei Tumori from Oncologia Ca' Granda Onlus (OCGO) Fondazione.
Van Emburgh Beth O., Andrea Sartore-Bianchi, Federica Di Nicolantonio, Salvatore Siena, Alberto Bardelli, (2014), Acquired resistance to EGFR‐targeted therapies in colorectal cancer, Molecular Oncolog. 8, doi: 10.1016/j.molonc.2014.05.003.
References
- Adam, R. , Wicherts, D.A. , de Haas, R.J. , Ciacio, O. , Lévi, F. , Paule, B. , Ducreux, M. , Azoulay, D. , Bismuth, H. , Castaing, D. , 2009. Patients with initially unresectable colorectal liver metastases: is there a possibility of cure?. J. Clin. Oncol. 27, 1829–1835. [DOI] [PubMed] [Google Scholar]
- Amado, R.G. , Wolf, M. , Peeters, M. , Van Cutsem, E. , Siena, S. , Freeman, D.J. , Juan, T. , Sikorski, R. , Suggs, S. , Radinsky, R. , Patterson, S.D. , Chang, D.D. , 2008. Wild-type KRAS is required for panitumumab efficacy in patients with metastatic colorectal cancer. J. Clin. Oncol. 26, 1626–1634. [DOI] [PubMed] [Google Scholar]
- Bardelli, A. , Corso, S. , Bertotti, A. , Hobor, S. , Valtorta, E. , Siravegna, G. , Sartore-Bianchi, A. , Scala, E. , Cassingena, A. , Zecchin, D. , Apicella, M. , Migliardi, G. , Galimi, F. , Lauricella, C. , Zanon, C. , Perera, T. , Veronese, S. , Corti, G. , Amatu, A. , Gambacorta, M. , Diaz, L.A. , Sausen, M. , Velculescu, V.E. , Comoglio, P. , Trusolino, L. , Di Nicolantonio, F. , Giordano, S. , Siena, S. , 2013. Amplification of the MET receptor drives resistance to anti-EGFR therapies in colorectal cancer. Cancer Discov. 3, 658–673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benvenuti, S. , Sartore-Bianchi, A. , Di Nicolantonio, F. , Zanon, C. , Moroni, M. , Veronese, S. , Siena, S. , Bardelli, A. , 2007. Oncogenic activation of the RAS/RAF signaling pathway impairs the response of metastatic colorectal cancers to anti-epidermal growth factor receptor antibody therapies. Cancer Res. 67, 2643–2648. [DOI] [PubMed] [Google Scholar]
- Bertotti, A. , Migliardi, G. , Galimi, F. , Sassi, F. , Torti, D. , Isella, C. , Corà, D. , Di Nicolantonio, F. , Buscarino, M. , Petti, C. , Ribero, D. , Russolillo, N. , Muratore, A. , Massucco, P. , Pisacane, A. , Molinaro, L. , Valtorta, E. , Sartore-Bianchi, A. , Risio, M. , Capussotti, L. , Gambacorta, M. , Siena, S. , Medico, E. , Sapino, A. , Marsoni, S. , Comoglio, P.M. , Bardelli, A. , Trusolino, L. , 2011. A molecularly annotated platform of patient-derived xenografts (“xenopatients”) identifies HER2 as an effective therapeutic target in cetuximab-resistant colorectal cancer. Cancer Discov. 1, 508–523. [DOI] [PubMed] [Google Scholar]
- Bettegowda, C. , Sausen, M. , Leary, R.J. , Kinde, I. , Wang, Y. , Agrawal, N. , Bartlett, B.R. , Wang, H. , Luber, B. , Alani, R.M. , Antonarakis, E.S. , Azad, N.S. , Bardelli, A. , Brem, H. , Cameron, J.L. , Lee, C.C. , Fecher, L.A. , Gallia, G.L. , Gibbs, P. , Le, D. , Giuntoli, R.L. , Goggins, M. , Hogarty, M.D. , Holdhoff, M. , Hong, S.M. , Jiao, Y. , Juhl, H.H. , Kim, J.J. , Siravegna, G. , Laheru, D.A. , Lauricella, C. , Lim, M. , Lipson, E.J. , Marie, S.K. , Netto, G.J. , Oliner, K.S. , Olivi, A. , Olsson, L. , Riggins, G.J. , Sartore-Bianchi, A. , Schmidt, K. , Shih, l , Oba-Shinjo, S.M. , Siena, S. , Theodorescu, D. , Tie, J. , Harkins, T.T. , Veronese, S. , Wang, T.L. , Weingart, J.D. , Wolfgang, C.L. , Wood, L.D. , Xing, D. , Hruban, R.H. , Wu, J. , Allen, P.J. , Schmidt, C.M. , Choti, M.A. , Velculescu, V.E. , Kinzler, K.W. , Vogelstein, B. , Papadopoulos, N. , Diaz, L.A. , 2014. Detection of circulating tumor DNA in early- and late-stage human malignancies. Sci. Transl Med. 6, 224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bianco, R. , Rosa, R. , Damiano, V. , Daniele, G. , Gelardi, T. , Garofalo, S. , Tarallo, V. , De Falco, S. , Melisi, D. , Benelli, R. , Albini, A. , Ryan, A. , Ciardiello, F. , Tortora, G. , 2008. Vascular endothelial growth factor receptor-1 contributes to resistance to anti-epidermal growth factor receptor drugs in human cancer cells. Clin. Cancer Res. 14, 5069–5080. [DOI] [PubMed] [Google Scholar]
- Brenner, H. , Kloor, M. , Pox, C.P. , 2014. Colorectal cancer. Lance. 383, 1490–1502. [DOI] [PubMed] [Google Scholar]
- Ciardiello, F. , Bianco, R. , Caputo, R. , Damiano, V. , Troiani, T. , Melisi, D. , De Vita, F. , De Placido, S. , Bianco, A.R. , Tortora, G. , 2004. Antitumor activity of ZD6474, a vascular endothelial growth factor receptor tyrosine kinase inhibitor, in human cancer cells with acquired resistance to antiepidermal growth factor receptor therapy. Clin. Cancer Res. 10, 784–793. [DOI] [PubMed] [Google Scholar]
- Cunningham, D. , Humblet, Y. , Siena, S. , Khayat, D. , Bleiberg, H. , Santoro, A. , Bets, D. , Mueser, M. , Harstrick, A. , Verslype, C. , Chau, I. , Van Cutsem, E. , 2004. Cetuximab monotherapy and cetuximab plus irinotecan in irinotecan-refractory metastatic colorectal cancer. N. Engl. J. Med. 351, 337–345. [DOI] [PubMed] [Google Scholar]
- De Roock, W. , Claes, B. , Bernasconi, D. , De Schutter, J. , Biesmans, B. , Fountzilas, G. , Kalogeras, K.T. , Kotoula, V. , Papamichael, D. , Laurent-Puig, P. , Penault-Llorca, F. , Rougier, P. , Vincenzi, B. , Santini, D. , Tonini, G. , Cappuzzo, F. , Frattini, M. , Molinari, F. , Saletti, P. , De Dosso, S. , Martini, M. , Bardelli, A. , Siena, S. , Sartore-Bianchi, A. , Tabernero, J. , Macarulla, T. , Di Fiore, F. , Gangloff, A.O. , Ciardiello, F. , Pfeiffer, P. , Qvortrup, C. , Hansen, T.P. , Van Cutsem, E. , Piessevaux, H. , Lambrechts, D. , Delorenzi, M. , Tejpar, S. , 2010. Effects of KRAS, BRAF, NRAS, and PIK3CA mutations on the efficacy of cetuximab plus chemotherapy in chemotherapy-refractory metastatic colorectal cancer: a retrospective consortium analysis. Lancet Oncol. 11, 753–762. [DOI] [PubMed] [Google Scholar]
- Diaz, L.A. , Williams, R.T. , Wu, J. , Kinde, I. , Hecht, J.R. , Berlin, J. , Allen, B. , Bozic, I. , Reiter, J.G. , Nowak, M.A. , Kinzler, K.W. , Oliner, K.S. , Vogelstein, B. , 2012. The molecular evolution of acquired resistance to targeted EGFR blockade in colorectal cancers. Natur. 486, 537–540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Douillard, J.Y. , Oliner, K.S. , Siena, S. , Tabernero, J. , Burkes, R. , Barugel, M. , Humblet, Y. , Bodoky, G. , Cunningham, D. , Jassem, J. , Rivera, F. , Kocákova, I. , Ruff, P. , Błasińska-Morawiec, M. , Šmakal, M. , Canon, J.L. , Rother, M. , Williams, R. , Rong, A. , Wiezorek, J. , Sidhu, R. , Patterson, S.D. , 2013. Panitumumab-FOLFOX4 treatment and RAS mutations in colorectal cancer. N. Engl. J. Med. 369, 1023–1034. [DOI] [PubMed] [Google Scholar]
- Engelman, J.A. , Zejnullahu, K. , Mitsudomi, T. , Song, Y. , Hyland, C. , Park, J.O. , Lindeman, N. , Gale, C.M. , Zhao, X. , Christensen, J. , Kosaka, T. , Holmes, A.J. , Rogers, A.M. , Cappuzzo, F. , Mok, T. , Lee, C. , Johnson, B.E. , Cantley, L.C. , Jänne, P.A. , 2007. MET amplification leads to gefitinib resistance in lung cancer by activating ERBB3 signaling. Scienc. 316, 1039–1043. [DOI] [PubMed] [Google Scholar]
- Esposito, C. , Rachiglio, A.M. , La Porta, M.L. , Sacco, A. , Roma, C. , Iannaccone, A. , Tatangelo, F. , Forgione, L. , Pasquale, R. , Barbaro, A. , Botti, G. , Ciardiello, F. , Normanno, N. , 2013. The S492R EGFR ectodomain mutation is never detected in KRAS wild type colorectal carcinoma before exposure to EGFR monoclonal antibodies. Cancer Biol. Ther. 14, 1143–1146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flaherty, K.T. , Infante, J.R. , Daud, A. , Gonzalez, R. , Kefford, R.F. , Sosman, J. , Hamid, O. , Schuchter, L. , Cebon, J. , Ibrahim, N. , Kudchadkar, R. , Burris, H.A. , Falchook, G. , Algazi, A. , Lewis, K. , Long, G.V. , Puzanov, I. , Lebowitz, P. , Singh, A. , Little, S. , Sun, P. , Allred, A. , Ouellet, D. , Kim, K.B. , Patel, K. , Weber, J. , 2012. Combined BRAF and MEK inhibition in melanoma with BRAF V600 mutations. N. Engl. J. Med. 367, 1694–1703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frattini, M. , Saletti, P. , Romagnani, E. , Martin, V. , Molinari, F. , Ghisletta, M. , Camponovo, A. , Etienne, L.L. , Cavalli, F. , Mazzucchelli, L. , 2007. PTEN loss of expression predicts cetuximab efficacy in metastatic colorectal cancer patients. Br. J. Cance. 97, 1139–1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerlinger, M. , Rowan, A.J. , Horswell, S. , Larkin, J. , Endesfelder, D. , Gronroos, E. , Martinez, P. , Matthews, N. , Stewart, A. , Tarpey, P. , Varela, I. , Phillimore, B. , Begum, S. , McDonald, N.Q. , Butler, A. , Jones, D. , Raine, K. , Latimer, C. , Santos, C.R. , Nohadani, M. , Eklund, A.C. , Spencer-Dene, B. , Clark, G. , Pickering, L. , Stamp, G. , Gore, M. , Szallasi, Z. , Downward, J. , Futreal, P.A. , Swanton, C. , 2012. Intratumor heterogeneity and branched evolution revealed by multiregion sequencing. N. Engl. J. Med. 366, 883–892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hecht, J.R. , Mitchell, E. , Chidiac, T. , Scroggin, C. , Hagenstad, C. , Spigel, D. , Marshall, J. , Cohn, A. , McCollum, D. , Stella, P. , Deeter, R. , Shahin, S. , Amado, R.G. , 2009. A randomized phase IIIB trial of chemotherapy, bevacizumab, and panitumumab compared with chemotherapy and bevacizumab alone for metastatic colorectal cancer. J. Clin. Oncol. 27, 672–680. [DOI] [PubMed] [Google Scholar]
- Jonker, D.J. , O'Callaghan, C.J. , Karapetis, C.S. , Zalcberg, J.R. , Tu, D. , Au, H.J. , Berry, S.R. , Krahn, M. , Price, T. , Simes, R.J. , Tebbutt, N.C. , van Hazel, G. , Wierzbicki, R. , Langer, C. , Moore, M.J. , 2007. Cetuximab for the treatment of colorectal cancer. N. Engl. J. Med. 357, 2040–2048. [DOI] [PubMed] [Google Scholar]
- Karapetis, C.S. , Khambata-Ford, S. , Jonker, D.J. , O'Callaghan, C.J. , Tu, D. , Tebbutt, N.C. , Simes, R.J. , Chalchal, H. , Shapiro, J.D. , Robitaille, S. , Price, T.J. , Shepherd, L. , Au, H.J. , Langer, C. , Moore, M.J. , Zalcberg, J.R. , 2008. K-ras mutations and benefit from cetuximab in advanced colorectal cancer. N. Engl. J. Med. 359, 1757–1765. [DOI] [PubMed] [Google Scholar]
- Kobayashi, S. , Boggon, T.J. , Dayaram, T. , Janne, P.A. , Kocher, O. , Meyerson, M. , Johnson, B.E. , Eck, M.J. , Tenen, D.G. , Halmos, B. , 2005. EGFR mutation and resistance of non-small-cell lung cancer to gefitinib. N. Engl. J. Med. 352, 786–792. [DOI] [PubMed] [Google Scholar]
- Laurent-Puig, P. , Cayre, A. , Manceau, G. , Buc, E. , Bachet, J.B. , Lecomte, T. , Rougier, P. , Lievre, A. , Landi, B. , Boige, V. , Ducreux, M. , Ychou, M. , Bibeau, F. , Bouché, O. , Reid, J. , Stone, S. , Penault-Llorca, F. , 2009. Analysis of PTEN, BRAF, and EGFR status in determining benefit from cetuximab therapy in wild-type KRAS metastatic colon cancer. J. Clin. Oncol. 27, 5924–5930. [DOI] [PubMed] [Google Scholar]
- Li, S. , Schmitz, K.R. , Jeffrey, P.D. , Wiltzius, J.J. , Kussie, P. , Ferguson, K.M. , 2005. Structural basis for inhibition of the epidermal growth factor receptor by cetuximab. Cancer Cel. 7, 301–311. [DOI] [PubMed] [Google Scholar]
- Liska, D. , Chen, C.T. , Bachleitner-Hofmann, T. , Christensen, J.G. , Weiser, M.R. , 2011. HGF rescues colorectal cancer cells from EGFR inhibition via MET activation. Clin. Cancer Res. 17, 472–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lièvre, A. , Bachet, J.B. , Le Corre, D. , Boige, V. , Landi, B. , Emile, J.F. , Côté, J.F. , Tomasic, G. , Penna, C. , Ducreux, M. , Rougier, P. , Penault-Llorca, F. , Laurent-Puig, P. , 2006. KRAS mutation status is predictive of response to cetuximab therapy in colorectal cancer. Cancer Res. 66, 3992–3995. [DOI] [PubMed] [Google Scholar]
- Lu, Y. , Li, X. , Liang, K. , Luwor, R. , Siddik, Z.H. , Mills, G.B. , Mendelsohn, J. , Fan, Z. , 2007. Epidermal growth factor receptor (EGFR) ubiquitination as a mechanism of acquired resistance escaping treatment by the anti-EGFR monoclonal antibody cetuximab. Cancer Res. 67, 8240–8247. [DOI] [PubMed] [Google Scholar]
- Malvezzi, M. , Bertuccio, P. , Levi, F. , La Vecchia, C. , Negri, E. , 2013. European cancer mortality predictions for the year 2013. Ann. Oncol. 24, 792–800. [DOI] [PubMed] [Google Scholar]
- Marsoni, S. , Bertotti, A. , Sartore-Bianchi, A. , Leone, F. , Lonardi, S. , Ciardiello, F. , Pinto, C. , Aglietta, M. , Zagonel, V. , Gambacorta, M. , Grigioni, W.F. , Rugge, M. , Risio, M. , Martino, C. , Valtorta, E. , Bardelli, A. , Trusolino, L. , Comoglio, P.M. , Siena, S. , 2013. Dual anti-HER2 treatment of patients with HER2-positive metastatic colorectal cancer: the HERACLES trial (HER2 Amplification for Colo-rectaL Cancer Enhanced Stratification). J. Clin. Oncol. 31, [Google Scholar]
- Mendelsohn, J. , Baselga, J. , 2000. The EGF receptor family as targets for cancer therapy. Oncogen. 19, 6550–6565. [DOI] [PubMed] [Google Scholar]
- Misale, S. , Arena, S. , Lamba, S. , Siravegna, G. , Lallo, A. , Hobor, S. , Russo, M. , Buscarino, M. , Lazzari, L. , Sartore-Bianchi, A. , Bencardino, K. , Amatu, A. , Lauricella, C. , Valtorta, E. , Siena, S. , Di Nicolantonio, F. , Bardelli, A. , 2014. Blockade of EGFR and MEK intercepts heterogeneous mechanisms of acquired resistance to anti-EGFR therapies in colorectal cancer. Sci. Transl Med. 6, 224–226. [DOI] [PubMed] [Google Scholar]
- Misale, S. , Yaeger, R. , Hobor, S. , Scala, E. , Janakiraman, M. , Liska, D. , Valtorta, E. , Schiavo, R. , Buscarino, M. , Siravegna, G. , Bencardino, K. , Cercek, A. , Chen, C.T. , Veronese, S. , Zanon, C. , Sartore-Bianchi, A. , Gambacorta, M. , Gallicchio, M. , Vakiani, E. , Boscaro, V. , Medico, E. , Weiser, M. , Siena, S. , Di Nicolantonio, F. , Solit, D. , Bardelli, A. , 2012. Emergence of KRAS mutations and acquired resistance to anti-EGFR therapy in colorectal cancer. Natur. 486, 532–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montagut, C. , Dalmases, A. , Bellosillo, B. , Crespo, M. , Pairet, S. , Iglesias, M. , Salido, M. , Gallen, M. , Marsters, S. , Tsai, S.P. , Minoche, A. , Seshagiri, S. , Somasekar, S. , Serrano, S. , Himmelbauer, H. , Bellmunt, J. , Rovira, A. , Settleman, J. , Bosch, F. , Albanell, J. , 2012. Identification of a mutation in the extracellular domain of the epidermal growth factor receptor conferring cetuximab resistance in colorectal cancer. Nat. Med. 18, 221–223. [DOI] [PubMed] [Google Scholar]
- Moroni, M. , Veronese, S. , Benvenuti, S. , Marrapese, G. , Sartore-Bianchi, A. , Di Nicolantonio, F. , Gambacorta, M. , Siena, S. , Bardelli, A. , 2005. Gene copy number for epidermal growth factor receptor (EGFR) and clinical response to antiEGFR treatment in colorectal cancer: a cohort study. Lancet Oncol. 6, 279–286. [DOI] [PubMed] [Google Scholar]
- Murtaza, M. , Dawson, S.J. , Tsui, D.W. , Gale, D. , Forshew, T. , Piskorz, A.M. , Parkinson, C. , Chin, S.F. , Kingsbury, Z. , Wong, A.S. , Marass, F. , Humphray, S. , Hadfield, J. , Bentley, D. , Chin, T.M. , Brenton, J.D. , Caldas, C. , Rosenfeld, N. , 2013. Non-invasive analysis of acquired resistance to cancer therapy by sequencing of plasma DNA. Natur. 497, 108–112. [DOI] [PubMed] [Google Scholar]
- Pao, W. , Miller, V.A. , Politi, K.A. , Riely, G.J. , Somwar, R. , Zakowski, M.F. , Kris, M.G. , Varmus, H. , 2005. Acquired resistance of lung adenocarcinomas to gefitinib or erlotinib is associated with a second mutation in the EGFR kinase domain. Plos Med. 2, e73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paranavitana, C.M. , 1998. Non-radioactive detection of K-ras mutations by nested allele specific PCR and oligonucleotide hybridization. Mol. Cell Probe. 12, 309–315. [DOI] [PubMed] [Google Scholar]
- Sartore-Bianchi, A. , Fieuws, S. , Veronese, S. , Moroni, M. , Personeni, N. , Frattini, M. , Torri, V. , Cappuzzo, F. , Vander Borght, S. , Martin, V. , Skokan, M. , Santoro, A. , Gambacorta, M. , Tejpar, S. , Varella-Garcia, M. , Siena, S. , 2012. Standardisation of EGFR FISH in colorectal cancer: results of an international interlaboratory reproducibility ring study. J. Clin. Pathol. 65, 218–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sartore-Bianchi, A. , Martini, M. , Molinari, F. , Veronese, S. , Nichelatti, M. , Artale, S. , Di Nicolantonio, F. , Saletti, P. , De Dosso, S. , Mazzucchelli, L. , Frattini, M. , Siena, S. , Bardelli, A. , 2009. PIK3CA mutations in colorectal cancer are associated with clinical resistance to EGFR-targeted monoclonal antibodies. Cancer Res. 69, 1851–1857. [DOI] [PubMed] [Google Scholar]
- Sartore-Bianchi, A. , Moroni, M. , Veronese, S. , Carnaghi, C. , Bajetta, E. , Luppi, G. , Sobrero, A. , Barone, C. , Cascinu, S. , Colucci, G. , Cortesi, E. , Nichelatti, M. , Gambacorta, M. , Siena, S. , 2007. Epidermal growth factor receptor gene copy number and clinical outcome of metastatic colorectal cancer treated with panitumumab. J. Clin. Oncol. 25, 3238–3245. [DOI] [PubMed] [Google Scholar]
- Scartozzi, M. , Mandolesi, A. , Giampieri, R. , Bittoni, A. , Pierantoni, C. , Zaniboni, A. , Galizia, E. , Giustini, L. , Silva, R.R. , Bisonni, R. , Berardi, R. , Biscotti, T. , Biagetti, S. , Bearzi, I. , Cascinu, S. , 2011. The role of HER-3 expression in the prediction of clinical outcome for advanced colorectal cancer patients receiving irinotecan and cetuximab. Oncologis. 16, 53–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scartozzi, M. , Mandolesi, A. , Giampieri, R. , Pierantoni, C. , Loupakis, F. , Zaniboni, A. , Galizia, E. , Giustini, L. , Silva, R.R. , Bisonni, R. , Berardi, R. , Biagetti, S. , Menzo, S. , Falcone, A. , Bearzi, I. , Cascinu, S. , 2010. Insulin-like growth factor 1 expression correlates with clinical outcome in K-RAS wild type colorectal cancer patients treated with cetuximab and irinotecan. Int. J. Cance. 127, 1941–1947. [DOI] [PubMed] [Google Scholar]
- Schmoll, H.J. , Van Cutsem, E. , Stein, A. , Valentini, V. , Glimelius, B. , Haustermans, K. , Nordlinger, B. , van de Velde, C.J. , Balmana, J. , Regula, J. , Nagtegaal, I.D. , Beets-Tan, R.G. , Arnold, D. , Ciardiello, F. , Hoff, P. , Kerr, D. , Köhne, C.H. , Labianca, R. , Price, T. , Scheithauer, W. , Sobrero, A. , Tabernero, J. , Aderka, D. , Barroso, S. , Bodoky, G. , Douillard, J.Y. , El Ghazaly, H. , Gallardo, J. , Garin, A. , Glynne-Jones, R. , Jordan, K. , Meshcheryakov, A. , Papamichail, D. , Pfeiffer, P. , Souglakos, I. , Turhal, S. , Cervantes, A. , 2012. ESMO consensus guidelines for management of patients with colon and rectal cancer. a personalized approach to clinical decision making. Ann. Oncol. 23, 2479–2516. [DOI] [PubMed] [Google Scholar]
- Shien, K. , Toyooka, S. , Yamamoto, H. , Soh, J. , Jida, M. , Thu, K.L. , Hashida, S. , Maki, Y. , Ichihara, E. , Asano, H. , Tsukuda, K. , Takigawa, N. , Kiura, K. , Gazdar, A.F. , Lam, W.L. , Miyoshi, S. , 2013. Acquired resistance to EGFR inhibitors is associated with a manifestation of stem cell-like properties in cancer cells. Cancer Res. 73, 3051–3061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegel, R. , DeSantis, C. , Virgo, K. , Stein, K. , Mariotto, A. , Smith, T. , Cooper, D. , Gansler, T. , Lerro, C. , Fedewa, S. , Lin, C. , Leach, C. , Cannady, R.S. , Cho, H. , Scoppa, S. , Hachey, M. , Kirch, R. , Jemal, A. , Ward, E. , 2012. Cancer treatment and survivorship statistics, 2012. CA Cancer J. Clin. 62, 220–241. [DOI] [PubMed] [Google Scholar]
- Siegel, R. , Naishadham, D. , Jemal, A. , 2013. Cancer statistics, 2013. CA Cancer J. Clin. 63, 11–30. [DOI] [PubMed] [Google Scholar]
- Smith, G. , Bounds, R. , Wolf, H. , Steele, R.J. , Carey, F.A. , Wolf, C.R. , 2010. Activating K-Ras mutations outwith 'hotspot' codons in sporadic colorectal tumours - implications for personalised cancer medicine. Br. J. Cance. 102, 693–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sosman, J.A. , Kim, K.B. , Schuchter, L. , Gonzalez, R. , Pavlick, A.C. , Weber, J.S. , McArthur, G.A. , Hutson, T.E. , Moschos, S.J. , Flaherty, K.T. , Hersey, P. , Kefford, R. , Lawrence, D. , Puzanov, I. , Lewis, K.D. , Amaravadi, R.K. , Chmielowski, B. , Lawrence, H.J. , Shyr, Y. , Ye, F. , Li, J. , Nolop, K.B. , Lee, R.J. , Joe, A.K. , Ribas, A. , 2012. Survival in BRAF V600-mutant advanced melanoma treated with vemurafenib. N. Engl. J. Med. 366, 707–714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stintzing, S. , Jung, A. , Rossius, L. , Modest, D.P. , Fischer von Weikersthal, L. , Decker, T. , Mohler, M. , Scheithauer, W. , Kirchner, T. , Heinemann, V. , 2013. Analysis of KRAS/NRAS and BRAF mutations in FIRE-3: a randomized phase III study of FOLFIRI plus cetuximab or bevacizumab as first-line treatment for wild-type (WT) KRAS (exon 2) metastatic colorectal cancer (mCRC) patients. Eur. J. Cance. 49, LBA 17 [Google Scholar]
- Takezawa, K. , Pirazzoli, V. , Arcila, M.E. , Nebhan, C.A. , Song, X. , de Stanchina, E. , Ohashi, K. , Janjigian, Y.Y. , Spitzler, P.J. , Melnick, M.A. , Riely, G.J. , Kris, M.G. , Miller, V.A. , Ladanyi, M. , Politi, K. , Pao, W. , 2012. HER2 amplification: a potential mechanism of acquired resistance to EGFR inhibition in EGFR-mutant lung cancers that lack the second-site EGFRT790M mutation. Cancer Discov. 2, 922–933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tol, J. , Koopman, M. , Cats, A. , Rodenburg, C.J. , Creemers, G.J. , Schrama, J.G. , Erdkamp, F.L. , Vos, A.H. , van Groeningen, C.J. , Sinnige, H.A. , Richel, D.J. , Voest, E.E. , Dijkstra, J.R. , Vink-Borger, M.E. , Antonini, N.F. , Mol, L. , van Krieken, J.H. , Dalesio, O. , Punt, C.J. , 2009. Chemotherapy, bevacizumab, and cetuximab in metastatic colorectal cancer. N. Engl. J. Med. 360, 563–572. [DOI] [PubMed] [Google Scholar]
- Troiani, T. , Martinelli, E. , Napolitano, S. , Vitagliano, D. , Ciuffreda, L.P. , Costantino, S. , Morgillo, F. , Capasso, A. , Sforza, V. , Nappi, A. , De Palma, R. , D'Aiuto, E. , Berrino, L. , Bianco, R. , Ciardiello, F. , 2013. Increased TGF-α as a mechanism of acquired resistance to the anti-EGFR inhibitor cetuximab through EGFR–MET interaction and activation of MET signaling in colon cancer cells. Clin. Cancer Res. 19, 6751–6765. [DOI] [PubMed] [Google Scholar]
- Valtorta, E. , Misale, S. , Sartore-Bianchi, A. , Nagtegaal, I.D. , Paraf, F. , Lauricella, C. , Dimartino, V. , Hobor, S. , Jacobs, B. , Ercolani, C. , Lamba, S. , Scala, E. , Veronese, S. , Laurent-Puig, P. , Siena, S. , Tejpar, S. , Mottolese, M. , Punt, C.J. , Gambacorta, M. , Bardelli, A. , Di Nicolantonio, F. , 2013. KRAS gene amplification in colorectal cancer and impact on response to EGFR-targeted therapy. Int. J. Cance. 133, 1259–1265. [DOI] [PubMed] [Google Scholar]
- Van Cutsem, E. , Kohne, C.H. , Hitre, E. , Zaluski, J. , Chang Chien, C.R. , Makhson, A. , D'Haens, G. , Pinter, T. , Lim, R. , Bodoky, G. , Roh, J.K. , Folprecht, G. , Ruff, P. , Stroh, C. , Tejpar, S. , Schlichting, M. , Nippgen, J. , Rougier, P. , 2009. Cetuximab and chemotherapy as initial treatment for metastatic colorectal cancer. N. Engl. J. Med. 360, 1408–1417. [DOI] [PubMed] [Google Scholar]
- Van Cutsem, E. , Peeters, M. , Siena, S. , Humblet, Y. , Hendlisz, A. , Neyns, B. , Canon, J.L. , Van Laethem, J.L. , Maurel, J. , Richardson, G. , Wolf, M. , Amado, R.G. , 2007. Open-label phase III trial of panitumumab plus best supportive care compared with best supportive care alone in patients with chemotherapy-refractory metastatic colorectal cancer. J. Clin. Oncol. 25, 1658–1664. [DOI] [PubMed] [Google Scholar]
- Wheeler, D.L. , Iida, M. , Kruser, T.J. , Nechrebecki, M.M. , Dunn, E.F. , Armstrong, E.A. , Huang, S. , Harari, P.M. , 2009. Epidermal growth factor receptor cooperates with Src family kinases in acquired resistance to cetuximab. Cancer Biol. Ther. 8, 696–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yonesaka, K. , Zejnullahu, K. , Okamoto, I. , Satoh, T. , Cappuzzo, F. , Souglakos, J. , Ercan, D. , Rogers, A. , Roncalli, M. , Takeda, M. , Fujisaka, Y. , Philips, J. , Shimizu, T. , Maenishi, O. , Cho, Y. , Sun, J. , Destro, A. , Taira, K. , Takeda, K. , Okabe, T. , Swanson, J. , Itoh, H. , Takada, M. , Lifshits, E. , Okuno, K. , Engelman, J.A. , Shivdasani, R.A. , Nishio, K. , Fukuoka, M. , Varella-Garcia, M. , Nakagawa, K. , Jänne, P.A. , 2011. Activation of ERBB2 signaling causes resistance to the EGFR-directed therapeutic antibody cetuximab. Sci. Transl Med. 3, 99–186. [DOI] [PMC free article] [PubMed] [Google Scholar]


