Abstract
UNINTENTIONAL WEIGHT LOSS, or the involuntary decline in total body weight over time, is common among elderly people who live at home. Weight loss in elderly people can have a deleterious effect on the ability to function and on quality of life and is associated with an increase in mortality over a 12-month period. A variety of physical, psychological and social conditions, along with age-related changes, can lead to weight loss, but there may be no identifiable cause in up to one-quarter of patients. We review the incidence and prevalence of weight loss in elderly patients, its impact on morbidity and mortality, the common causes of unintentional weight loss and a clinical approach to diagnosis. Screening tools to detect malnutrition are highlighted, and nonpharmacologic and pharmacologic strategies to minimize or reverse weight loss in older adults are discussed.
Unintentional weight loss is the involuntary decline in total body weight over time. In clinical practice, it is encountered in up to 8% of all adult outpatients1 and 27% of frail people 65 years and older.2 Weight loss is an important risk factor in elderly patients. It is associated with increased mortality, which can range from 9% to as high as 38% within 1 to 2.5 years after weight loss has occurred.1,3,4 Frail elderly people,5 people with low baseline body weight,5,6,7 and elderly patients recently admitted to hospital are particularly susceptible to increased mortality.8,9 Weight loss is also associated with an increased risk of in-hospital complications,10,11 a decline in activities of daily living or physical function,12,13 higher rates of admission to an institution2,8 and poorer quality of life.14
When is weight loss clinically important?
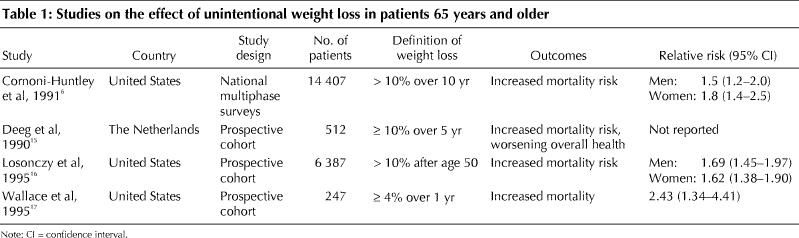
Unintentional weight loss may reflect disease severity (e.g., in patients with advanced heart disease, lung disease or malignant disease) or undiagnosed illness. Weight loss of 4%–5% or more of body weight within 1 year, or 10% or more over 5–10 years or longer, is associated with increased mortality or morbidity or both (Table 1). This association has also been seen in a number of epidemiologic and clinical studies that adjusted for comorbidity,5,7,13 disability,5,13 smoking,5,7 alcohol use5 or level of physical activity13 and that excluded deaths within the first few years of weight loss to exclude undiagnosed illness.7 In frail elderly populations, even small weight loss (e.g., 1 kg,5 or 3% of body weight18) may be significant. Voluntary weight loss among elderly patients is also associated with increased risk of death17 and of hip fracture,19 which highlights the importance of maintaining weight with age.
Table 1
How common is weight loss?
Prevalence estimates of weight loss among elderly people vary tremendously. The results of epidemiologic studies have shown that most elderly patients maintain weight over a reasonably long period of 5–10 years.13,20,21 Nevertheless, about 15%–20% experience weight loss — defined in these studies as a loss of either 5 kg or more or 5% of usual body weight over 5–10 years — with little difference between sexes.13,15,20 This prevalence estimate rises to 27% in high-risk populations, such as free-living frail elderly people receiving community services.2 Increasing age,13,22 disability,9,13 coexisting medical illnesses,19,22 previous admission to hospital,13 low education level,22 presence of cognitive impairment,23 smoking,13,19,22 loss of a spouse13,22 and low baseline body weight9,22 have been associated with a higher likelihood of weight loss. The proportion of elderly people who experience rapid (within 6 months), severe (≥ 7.5% of baseline body weight) and unexplained weight loss is only 0.45%.24
The incidence of unintentional weight loss in clinical studies involving adults seeking health care varies from 1.3% to 8%, depending on the setting and definition of weight loss.1,3,4,25 There is also a difference in rates between clinical and epidemiologic studies, probably because most patients with weight loss present within a year of onset of their clinical symptoms.
Causes and mechanisms
In general, causes of weight loss in elderly people are similar to those in middle-aged people and can be classified as organic (e.g., neoplastic, nonneoplastic and age-related changes), psychological (e.g., depression, dementia, anxiety disorders) or nonmedical (e.g., socioeconomic conditions) (Box 1). Up to one-quarter of all cases have no identifiable cause, despite extensive investigation.1,3,24 People with no known cause of weight loss generally have a better prognosis than people with known causes, particularly when the cause is neoplastic.1,29
Box 1.
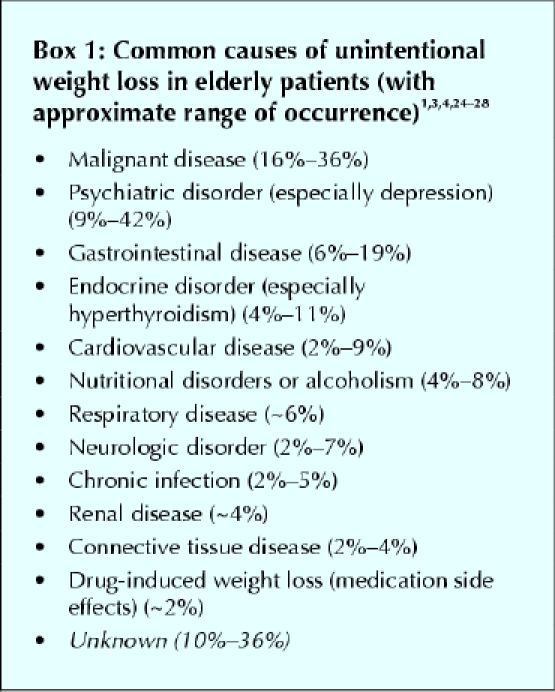
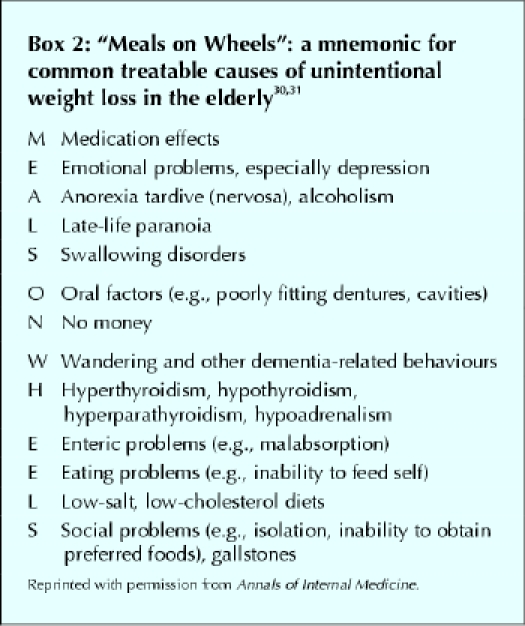
Often a combination of factors will lead to weight loss in elderly people, particularly frail people 75 years or older. Many of these factors are not traditional medical diseases (Box 2). For example, patients with dementia or late-life psychotic disorders may become paranoid and suspicious that the food being served to them is poisoned.32 Elderly people with dementia and habitual wandering expend significant energy in pacing. As well, some common illnesses may cause weight loss (e.g., gallstones may lead to chronic nausea and decreased appetite or avoidance of high-energy, fatty foods).
Box 2.
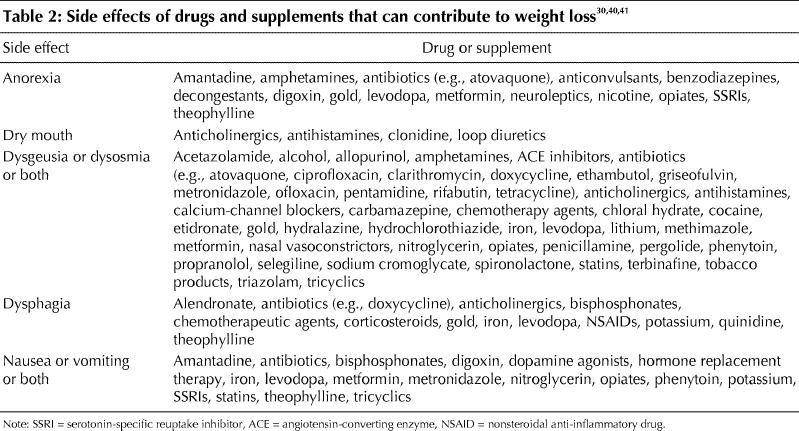
Several important age-associated physiologic changes predispose the elderly person to weight loss, such as declining chemosensory function (smell and taste),33,34 reduced efficiency of chewing,35 slowed gastric emptying36 and alterations to the neuroendocrine axis (including changes in levels of leptin, cholecystokinin, neuropeptide Y and other hormones and peptides).37,38 These changes are associated with early satiety and a decline in both appetite and the hedonistic appreciation of food, and collectively they contribute to the “anorexia of aging.” Other evidence also suggests that, compared with healthy younger adults, elderly people are less able to adapt to periods of over- and undereating and less likely to return to their usual body weight after such periods,39 which makes them more susceptible to weight change. The importance of medications in contributing to weight loss cannot be overstated, since many elderly people take medications, mostly for chronic conditions (Table 2).
Table 2
Various mechanisms have been suggested to explain the association between weight loss and adverse outcomes. Weight loss exacerbates the loss of fat-free mass (sarcopenia) associated with aging,42 which leads to functional decline and fractures.43,44 Many elderly patients with unintentional weight loss are experiencing concomitant malnutrition45 and thereby have cachexia.46 Cachexia is associated with a disproportionate loss of skeletal muscle rather than of body fat and is generally defined as a profound and marked state of constitutional disorder, general ill health and malnutrition. A decline of even 10% of skeletal muscle mass may be associated with a decline in physical function (e.g., decreased exercise tolerance or difficulty performing activities of daily living).47 In addition, cachexia is associated with a systemic inflammatory response, increased cytokine concentrations and impaired immunity, all of which are thought to contribute to adverse outcomes, including early death.48
Optimal clinical approach to weight loss
It is important to establish up front the presence of weight loss. A significant proportion of elderly people with documented weight loss may not complain about losing weight or, less commonly, may mistakenly attribute weight loss to successful diet or lifestyle modifications.1,24 Furthermore, disturbed eating behaviours and body image (e.g., anorexia tardive)32 among some elderly people may lead them to regard weight loss as desirable and therefore nonreportable. Conversely, up to half of people who claim to have lost weight have no documented evidence of weight loss.1 If it is not possible to measure weight directly, a change in clothing size, corroboration of weight loss by a relative or friend, or a numerical estimate of weight loss provided by the patient are suggestive enough of true weight loss.1,3,29 A careful history may elicit localizing symptoms (e.g., changes in defecation frequently imply involvement of the gastrointestinal tract) that may guide further investigations in almost half of patients.4,29 All elderly patients with weight loss should undergo screening for dementia and depression30 by using instruments such as the Mini-Mental Status Examination49 and the Geriatric Depression Scale50 respectively. Specific features on physical examination, such as cachexia, lymphadenopathy or palpable masses, may suggest a physical cause of weight loss (e.g., malignant disease).1,4 However, the diagnostic utility of the medical history and physical examination in identifying the cause of weight loss have not been adequately evaluated.
Although few studies have systematically evaluated the utility of screening investigations for weight loss, the most useful noninvasive procedures appear to include a complete blood count, tests of liver enzyme levels (including alkaline phosphatase and bilirubin), measurement of lactate dehydrogenase level, and chest radiography.1,4,25,29 Patients with iron-deficiency anemia or symptoms likely to originate in the gastrointestinal tract, and patients with elevated liver enzyme levels on initial screening, should undergo investigation of their gastrointestinal tract (either endoscopy or upper gastrointestinal series) or an abdominal ultrasound, respectively.1,4,24,29
Three scoring systems have been developed to help clinicians identify which patient with weight loss is likely to have a physical1,4 or malignant51 cause as opposed to a psychological or unknown cause. None of these scoring systems has been validated in independent populations presenting with weight loss.1,4,51
When weight loss is apparent in the elderly patient with no evidence of an organic disorder, primary malnutrition (i.e., resulting from inadequate food intake) must be considered as a contributor.
In general, elderly people are at increased risk of malnutrition because of insufficient food intake (quantity) rather than inappropriate selection of food (quality). Two screening tools, ENS52,53 (www.dietitians.ca/seniors/content/other/clsc_overview.asp) and SCREEN54,55 (www.dietitians.ca/seniors/index.asp), have been developed and validated in Canada to identify community-dwelling elderly people who are at risk of malnutrition. Two other assessment tools, the Mini Nutritional Assessment (www.mna-elderly.com) and the Nutrition Screening Initiative (www.aafp.org/x16081.xml), which was created by the American Academy of Family Physicians with the American Dietetic Association, are also freely available to be used for nutritional assessment of elderly patients.
How should weight loss be managed?
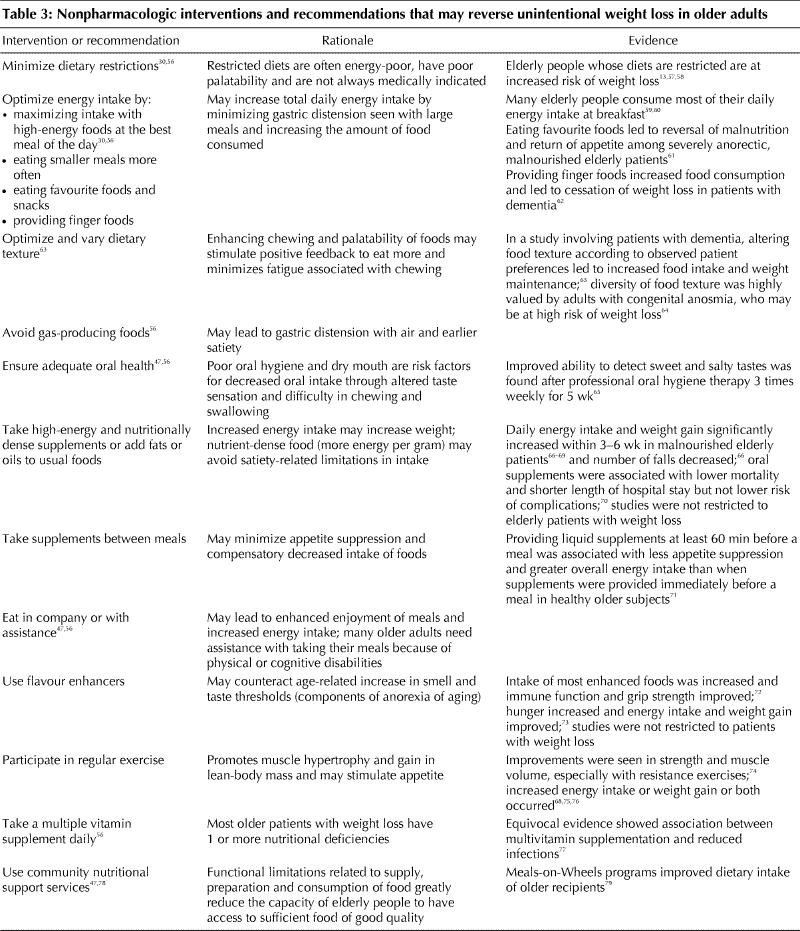
The first priority in managing weight loss is to systematically identify and treat the underlying causes (Fig. 1). Treatment of unintentional weight loss often requires enabling access to good nutrition, and several important nonpharmacologic strategies can be implemented to prevent or treat malnutrition and enhance food intake (Table 3). Factors such as poverty, poor dental health, difficulty in chewing or swallowing, vision or hearing loss, arthritis, stress (e.g., illness or death of a loved one) and unhappiness, which are associated with poor diet quality, should be targeted.52,80 It is therefore prudent to involve a dietitian and a social worker to assist with assessment and management, particularly in cases where an obvious organic cause has not been identified. A physiotherapist may help patients increase their amount of exercise, to thereby stimulate appetite and increase energy intake and muscle mass.68,74,75,76
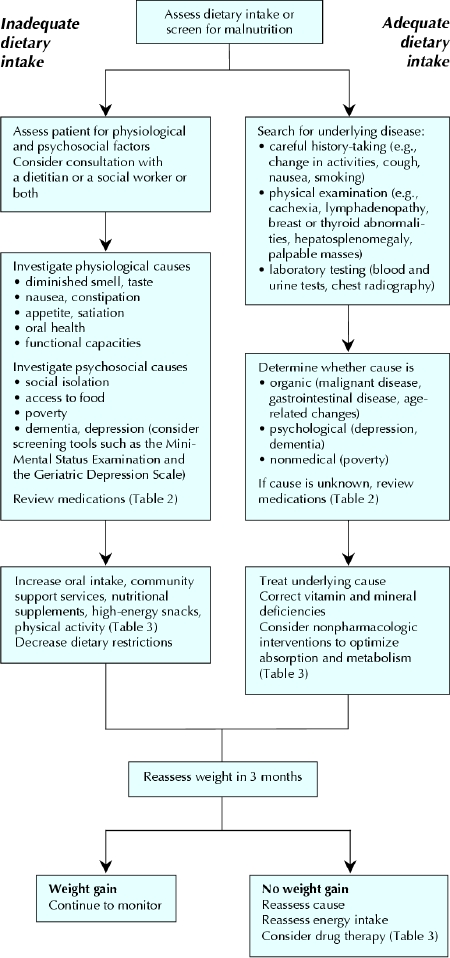
Fig. 1: Strategies for treating weight loss in elderly patients.
Table 3
The use of oral nutritional supplements, such as high-energy drinks, as a means of reversing weight loss and increasing food intake may sometimes, but not always, reverse weight loss.66,69,81,82 Counselling and encouraging patients to consume supplements in addition to their usual food intake rather than as a replacement of that intake is essential, since weight gain is confined to those who actually increase their energy intake.69,82 Advising patients to consume supplements between meals, rather than with the meal, may help minimize appetite suppression and facilitate increased overall intake.71 Although supplement use has been associated with short-term weight gain and improvements in biochemical, anthropometric and quality-of-life parameters in a number of trials, long-term beneficial effects on health, ability to function and survival in undernourished elderly people are yet to be consistently demonstrated.66,83 A systematic review showed a reduction in mortality among elderly patients who received protein-energy supplements, irrespective of whether they had weight loss.70
Many elderly people consume too little food to meet their nutritional needs,84,85 which puts them at risk of vitamin and mineral deficiency. A broad-spectrum vitamin and mineral supplement should be considered for people at risk of malnutrition or where improvements in food intake are not observed.85
Pharmacologic therapy to reverse weight loss
In our experience, the evidence supporting any pharmacologic agent for the treatment of weight loss is limited to mostly small, uncontrolled studies, and benefits are generally restricted to a small gain in weight without evidence of decreased morbidity and mortality or improved function and quality of life. Most of these agents have significant side effects, particularly in frail elderly people, which limits their usefulness. Various pharmacologic agents, including orexigenic (appetite-stimulating) and anabolic medications, have been used to improve appetite or cause weight gain in subjects with weight loss. Only 4 have been studied in randomized trials (Table 4).
Table 4
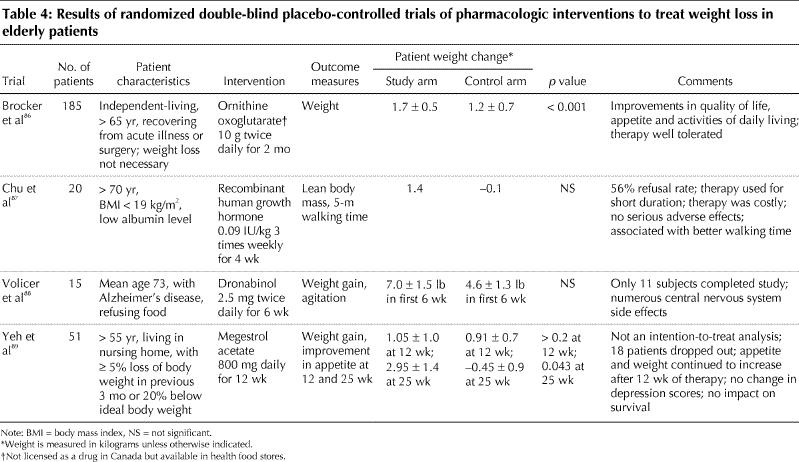
The synthetic progestational agent megestrol acetate is best associated with weight gain in well-designed, randomized trials in populations of patients with malignant disease or HIV infection.90,91 Evidence for its use with elderly people is limited.89,91,92,93 Ornithine oxoglutarate led to weight gain in one randomized trial but has not been studied in other trials.86 There are no randomized trials of either cyproheptadine or dronabinol in elderly people with weight loss, although dronabinol has been studied in one trial involving patients with dementia who were refusing food.88 Both medications are associated with significant side effects, particularly central nervous system toxicity.88,94,95
Among anabolic agents, a 4-week randomized trial of human growth hormone in 20 undernourished elderly people demonstrated slightly faster weight gain and improved walking time in those receiving the hormone. After 4 weeks, between-group differences in weight were no longer statistically significant.87 Use of human growth hormone in other settings has been associated with increased mortality.96 Several small clinical studies or cross-over trials of androgenic agents have not shown that they lead to weight gain.95,97 Other pharmacologic approaches, such as anticytokine therapies, antileptin therapies and anti-inflammatory medications, are being investigated.95,98
Conclusion
Unintentional weight loss is common in elderly people and is associated with significant adverse health outcomes, increased mortality and progressive disability. The differential diagnosis is broad, ranging from reduced food intake to organic causes to psychological disorders. Medications may also contribute to weight loss, as may social or economic factors. Up to 1 in 4 elderly people with unintentional weight loss will have no obvious medical cause. In others, a limited set of initial symptom-oriented investigations may reveal the underlying causes. A variety of nonpharmacologic interventions may improve energy intake and lead to weight gain, whereas the role for pharmacotherapy remains limited.
Footnotes
This article has been peer reviewed.
Contributors: Shabbir Alibhai contributed to the article design, performed the primary systematic literature review, summarized the key studies, drafted significant portions of the paper and revised the article. Carol Greenwood and Hélène Payette contributed to the article design, performed supplementary literature reviews, drafted significant portions of the paper and critically revised the article for important intellectual content. All of the authors approved the final version of the paper.
Competing interests: None declared.
Correspondence to: Dr. Shabbir M.H. Alibhai, University Health Network, Rm. ES 9–407, 200 Elizabeth St., Toronto ON M5G 2C4; fax 416 595-5826; shabbir.alibhai@uhn.on.ca
References
- 1.Marton KI, Sox HC, Jr., Krupp JR. Involuntary weight loss: diagnostic and prognostic significance. Ann Intern Med 1981;95(5):568-74. [DOI] [PubMed]
- 2.Payette H, Coulombe C, Boutier V, Gray-Donald K. Nutrition risk factors for institutionalization in a free-living functionally dependent elderly population. J Clin Epidemiol 2000;53(6):579-87. [DOI] [PubMed]
- 3.Rabinovitz M, Pitlik SD, Leifer M, Garty M, Rosenfeld JB. Unintentional weight loss. A retrospective analysis of 154 cases. Arch Intern Med 1986;146(1):186-7. [DOI] [PubMed]
- 4.Bilbao-Garay J, Barba R, Losa-Garcia JE, Martin H, Garcia de Casasola G, Castilla V. Assessing clinical probability of organic disease in patients with involuntary weight loss: a simple score. Eur J Intern Med 2002;13(4):240-5. [DOI] [PubMed]
- 5.Payette H, Coulombe C, Boutier V, Gray-Donald K. Weight loss and mortality among free-living frail elders: a prospective study. J Gerontol A Biol Sci Med Sci 1999;54(9):M440-5. [DOI] [PubMed]
- 6.Cornoni-Huntley JC, Harris TB, Everett DF, Albanes D, Micozzi MS, Miles TP, et al. An overview of body weight of older persons, including the impact on mortality. The National Health and Nutrition Examination Survey I — Epidemiologic Follow-up Study. J Clin Epidemiol 1991;44(8):743-53. [DOI] [PubMed]
- 7.Somes GW, Kritchevsky SB, Shorr RI, Pahor M, Applegate WB. Body mass index, weight change, and death in older adults: the systolic hypertension in the elderly program. Am J Epidemiol 2002;156(2):132-8. [DOI] [PubMed]
- 8.Satish S, Winograd CH, Chavez C, Bloch DA. Geriatric targeting criteria as predictors of survival and health care utilization. J Am Geriatr Soc 1996;44(8):914-21. [DOI] [PubMed]
- 9.Verdery R, Levy K, Roberts N, Howell W. Natural history of failure to thrive, weight loss, and functional disability in elderly people after hospitalization. Age Nutr 1996;7(2):70-4.
- 10.Seltzer MH, Slocum BA, Cataldi-Betcher EL, Fileti C, Gerson N. Instant nutritional assessment: absolute weight loss and surgical mortality. JPENJ Parenter Enteral Nutr 1982;6(3):218-21. [DOI] [PubMed]
- 11.Sullivan DH, Patch GA, Walls RC, Lipschitz DA. Impact of nutrition status on morbidity and mortality in a select population of geriatric rehabilitation patients. Am J Clin Nutr 1990;51(5):749-58. [DOI] [PubMed]
- 12.Launer LJ, Harris T, Rumpel C, Madans J. Body mass index, weight change, and risk of mobility disability in middle-aged and older women. The epidemiologic follow-up study of NHANES I. JAMA 1994;271(14):1093-8. [PubMed]
- 13.Newman AB, Yanez D, Harris T, Duxbury A, Enright PL, Fried LP. Weight change in old age and its association with mortality. J Am Geriatr Soc 2001;49(10):1309-18. [DOI] [PubMed]
- 14.Fine JT, Colditz GA, Coakley EH, Moseley G, Manson JE, Willett WC, et al. A prospective study of weight change and health-related quality of life in women. JAMA 1999;282(22):2136-42. [DOI] [PubMed]
- 15.Deeg DJ, Miles TP, Van Zonneveld RJ, Curb JD. Weight change, survival time and cause of death in Dutch elderly. Arch Gerontol Geriatr 1990;10(1):97-111. [DOI] [PubMed]
- 16.Losonczy KG, Harris TB, Cornoni-Huntley J, Simonsick EM, Wallace RB, Cook NR, et al. Does weight loss from middle age to old age explain the inverse weight mortality relation in old age? Am J Epidemiol 1995;141(4):312-21. [DOI] [PubMed]
- 17.Wallace JI, Schwartz RS, LaCroix AZ, Uhlmann RF, Pearlman RA. Involuntary weight loss in older outpatients: incidence and clinical significance. J Am Geriatr Soc 1995;43(4):329-37. [DOI] [PubMed]
- 18.Tully CL, Snowdon DA. Weight change and physical function in older women: findings from the Nun Study. J Am Geriatr Soc 1995;43(12):1394-7. [DOI] [PubMed]
- 19.Ensrud KE, Ewing SK, Stone KL, Cauley JA, Bowman PJ, Cummings SR. Intentional and unintentional weight loss increase bone loss and hip fracture risk in older women. J Am Geriatr Soc 2003;51(12):1740-7. [DOI] [PubMed]
- 20.De Groot CP, Perdigao AL, Deurenberg P. Longitudinal changes in anthropometric characteristics of elderly Europeans. SENECA Investigators. Eur J Clin Nutr 1996;50(Suppl 2):S9-15. [PubMed]
- 21.Shatenstein B, Kergoat MJ, Nadon S. Weight change, nutritional risk and its determinants among cognitively intact and demented elderly Canadians. Can J Public Health 2001;92(2):143-9. [DOI] [PMC free article] [PubMed]
- 22.Meltzer AA, Everhart JE. Unintentional weight loss in the United States. Am J Epidemiol 1995;142(10):1039-46. [DOI] [PubMed]
- 23.Barrett-Connor E, Edelstein SL, Corey-Bloom J, Wiederholt WC. Weight loss precedes dementia in community-dwelling older adults. J Am Geriatr Soc 1996;44(10):1147-52. [DOI] [PubMed]
- 24.Thompson MP, Morris LK. Unexplained weight loss in the ambulatory elderly. J Am Geriatr Soc 1991;39(5):497-500. [DOI] [PubMed]
- 25.Lankisch P, Gerzmann M, Gerzmann JF, Lehnick D. Unintentional weight loss: diagnosis and prognosis. The first prospective follow-up study from a secondary referral centre. J Intern Med 2001;249(1):41-6. [DOI] [PubMed]
- 26.Huerta G, Viniegra L. Involuntary weight loss as a clinical problem. Rev Invest Clin 1989;41(1):5-9. [PubMed]
- 27.Levine MA. Unintentional weight loss in the ambulatory setting: etiologies and outcomes [abstract]. Clin Res 1991;39(2):580A.
- 28.Lin HW, Li CM, Lee YC, Lee LT, Leung KK. Differences in diagnostic approach between family physicians and other specialists in patients with unintentional body weight loss. Fam Pract 1999;16(6):586-90. [DOI] [PubMed]
- 29.Hernandez JL, Riancho JA, Matorras P, Gonzalez-Macias J. Clinical evaluation for cancer in patients with involuntary weight loss without specific symptoms. Am J Med 2003;114(8):631-7. [DOI] [PubMed]
- 30.Huffman GB. Evaluating and treating unintentional weight loss in the elderly. Am Fam Physician 2002;65(4):640-50. [PubMed]
- 31.Morley JE, Silver AJ. Nutritional issues in nursing home care. Ann Intern Med 1995;123(11):850-9. [DOI] [PubMed]
- 32.Morley JE. Anorexia in older patients: its meaning and management. Geriatrics 1990;45(12):59-62, 65-6. [PubMed]
- 33.Schiffman SS. Taste and smell in disease (first of two parts). N Engl J Med 1983;308(21):1275-9. [DOI] [PubMed]
- 34.Shay K, Ship JA. The importance of oral health in the older patient. J Am Geriatr Soc 1995;43(12):1414-22. [DOI] [PubMed]
- 35.Ship JA, Duffy V, Jones JA, Langmore S. Geriatric oral health and its impact on eating. J Am Geriatr Soc 1996;44(4):456-64. [DOI] [PubMed]
- 36.Clarkston WK, Pantano MM, Morley JE, Horowitz M, Littlefield JM, Burton FR. Evidence for the anorexia of aging: gastrointestinal transit and hunger in healthy elderly vs. young adults. Am J Physiol 1997;272(1 Pt 2):R243-8. [DOI] [PubMed]
- 37.Schwartz MW, Seeley RJ. Seminars in medicine of the Beth Israel Deaconess Medical Center. Neuroendocrine responses to starvation and weight loss. N Engl J Med 1997;336(25):1802-11. [DOI] [PubMed]
- 38.Morley JE. Decreased food intake with aging. J Gerontol A Biol Sci Med Sci 2001; 56 Spec No 2:81-8. [DOI] [PubMed]
- 39.Roberts SB, Fuss P, Heyman MB, Evans WJ, Tsay R, Rasmussen H, et al. Control of food intake in older men. JAMA 1994;272(20):1601-6. [DOI] [PubMed]
- 40.Carr-Lopez SM, Phillips SL. The role of medications in geriatric failure to thrive. Drugs Aging 1996;9(4):221-5. [DOI] [PubMed]
- 41.Ackerman BH, Kasbekar N. Disturbances of taste and smell induced by drugs. Pharmacotherapy 1997;17(3):482-96. [PubMed]
- 42.Payette H, Roubenoff R, Jacques PF, Dinarello CA, Wilson PW, Abad LW, et al. Insulin-like growth factor-1 and interleukin 6 predict sarcopenia in very old community-living men and women: the Framingham Heart Study. J Am Geriatr Soc 2003;51(9):1237-43. [DOI] [PubMed]
- 43.Baumgartner RN, Koehler KM, Gallagher D, Romero L, Heymsfield SB, Ross RR, et al. Epidemiology of sarcopenia among the elderly in New Mexico. Am J Epidemiol 1998;147(8):755-63. [DOI] [PubMed]
- 44.Melton LJ 3rd, Khosla S, Crowson CS, O'Connor MK, O'Fallon WM, Riggs BL. Epidemiology of sarcopenia. J Am Geriatr Soc 2000;48(6):625-30. [PubMed]
- 45.Hardy C, Wallace C, Khansur T, Vance RB, Thigpen JT, Balducci L. Nutrition, cancer, and aging: an annotated review. II. Cancer cachexia and aging. J Am Geriatr Soc 1986;34(3):219-28. [DOI] [PubMed]
- 46.Roubenoff R, Heymsfield SB, Kehayias JJ, Cannon JG, Rosenberg IH. Standardization of nomenclature of body composition in weight loss. Am J Clin Nutr 1997;66(1):192-6. [DOI] [PubMed]
- 47.Reife CM. Involuntary weight loss. Med Clin North Am 1995;79(2):299-313. [DOI] [PubMed]
- 48.Roubenoff R, Parise H, Payette HA, Abad LW, D'Agostino R, Jacques PF, et al. Cytokines, insulin-like growth factor 1, sarcopenia, and mortality in very old community-dwelling men and women: the Framingham Heart Study. Am J Med 2003;115(6):429-35. [DOI] [PubMed]
- 49.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;12:189-98. [DOI] [PubMed]
- 50.Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res 1983;17(1):37-49. [DOI] [PubMed]
- 51.Hernandez JL, Matorras P, Riancho JA, Gonzalez-Macias J. Involuntary weight loss without specific symptoms: a clinical prediction score for malignant neoplasm. QJM 2003;96(9):649-55. [DOI] [PubMed]
- 52.Payette H, Gray-Donald K, Cyr R, Boutier V. Predictors of dietary intake in a functionally dependent elderly population in the community. Am J Public Health 1995;85(5):677-83. [DOI] [PMC free article] [PubMed]
- 53.Payette H, Guigoz Y, Vellas BJ. Study design for nutritional assessments in the elderly. In: Yu BP, editor. Methods in aging research. Boca Raton (FL): CRC Press LLC; 1999. p. 301-20.
- 54.Keller HH, Hedley MR, Wong Brownlee S. The Development of Seniors in the Community: Risk Evaluation for Eating and Nutrition (SCREEN). Can J Diet Pract Res 2000;61(2):67-72. [PubMed]
- 55.Keller HH, McKenzie JD, Goy RE. Construct validation and test-retest reliability of the seniors in the community: risk evaluation for eating and nutrition questionnaire. J Gerontol A Biol Sci Med Sci 2001;56(9):M552-8. [DOI] [PubMed]
- 56.Bouras EP, Lange SM, Scolapio JS. Rational approach to patients with unintentional weight loss. Mayo Clin Proc 2001;76(9):923-9. [DOI] [PubMed]
- 57.Buckler DA, Kelber ST, Goodwin JS. The use of dietary restrictions in malnourished nursing home patients. J Am Geriatr Soc 1994;42(10):1100-2. [DOI] [PubMed]
- 58.Kayser-Jones J, Schell ES, Porter C, Barbaccia JC, Steinbach C, Bird WF, et al. A prospective study of the use of liquid oral dietary supplements in nursing homes. J Am Geriatr Soc 1998;46(11):1378-86. [DOI] [PubMed]
- 59.Young KW, Binns MA, Greenwood CE. Meal delivery practices do not meet needs of Alzheimer patients with increased cognitive and behavioral difficulties in a long-term care facility. J Gerontol A Biol Sci Med Sci 2001;56(10):M656-61. [DOI] [PubMed]
- 60.Young KW, Greenwood CE. Shift in diurnal feeding patterns in nursing home residents with Alzheimer's disease. J Gerontol A Biol Sci Med Sci 2001;56(11):M700-6. [DOI] [PubMed]
- 61.Winograd CH, Brown EM. Aggressive oral refeeding in hospitalized patients. Am J Clin Nutr 1990;52(6):967-8. [DOI] [PubMed]
- 62.Soltesz KS, Dayton JH. The effects of menu modification to increase dietary intake and maintain the weight of Alzheimer residents. Am J Alzheimer's Dis 1995;10:20-3.
- 63.Boylston E, Ryan C, Brown C, Westfall B. Increasing oral intake in dementia patients by altering food texture. Am J Alzheimer's Dis 1995;10:37-9.
- 64.Doty R. Food preference ratings of congenitally anosmic humans. In: Kare M, Maller O, eds. Chemical senses and nutrition. New York: Academic Press; 1977. p. 315-25.
- 65.Langan MJ, Yearick ES. The effects of improved oral hygiene on taste perception and nutrition of the elderly. J Gerontol 1976;31(4):413-8. [DOI] [PubMed]
- 66.Gray-Donald K, Payette H, Boutier V. Randomized clinical trial of nutritional supplementation shows little effect on functional status among free-living frail elderly. J Nutr 1995;125(12):2965-71. [DOI] [PubMed]
- 67.Olin AO, Osterberg P, Hadell K, Armyr I, Jerstrom S, Ljungqvist O. Energy-enriched hospital food to improve energy intake in elderly patients. JPEN J Parenter Enteral Nutr 1996;20(2):93-7. [DOI] [PubMed]
- 68.De Jong N, Chin APMJ, de Graaf C, van Staveren WA. Effect of dietary supplements and physical exercise on sensory perception, appetite, dietary intake and body weight in frail elderly subjects. Br J Nutr 2000;83(6):605-13. [DOI] [PubMed]
- 69.Payette H, Boutier V, Coulombe C, Gray-Donald K. Benefits of nutritional supplementation in free-living, frail, undernourished elderly people: a prospective randomized community trial. J Am Diet Assoc 2002;102(8):1088-95. [PubMed]
- 70.Milne AC, Potter J, Avenell A. Protein and energy supplementation in elderly people at risk from malnutrition [Cochrane review]. In: The Cochrane Library; Issue 3, 2002. Oxford: Update Software. [DOI] [PubMed]
- 71.Wilson MM, Purushothaman R, Morley JE. Effect of liquid dietary supplements on energy intake in the elderly. Am J Clin Nutr 2002;75(5):944-7. [DOI] [PubMed]
- 72.Schiffman SS, Warwick ZS. Effect of flavor enhancement of foods for the elderly on nutritional status: food intake, biochemical indices, and anthropometric measures. Physiol Behav 1993;53(2):395-402. [DOI] [PubMed]
- 73.Mathey MF, Siebelink E, de Graaf C, Van Staveren WA. Flavor enhancement of food improves dietary intake and nutritional status of elderly nursing home residents. J Gerontol A Biol Sci Med Sci 2001;56(4):M200-5. [DOI] [PubMed]
- 74.Borst SE. Interventions for sarcopenia and muscle weakness in older people. Age Ageing 2004;33(6):548-55. [DOI] [PubMed]
- 75.Meredith CN, Frontera WR, O'Reilly KP, Evans WJ. Body composition in elderly men: effect of dietary modification during strength training. J Am Geriatr Soc 1992;40(2):155-62. [DOI] [PubMed]
- 76.Fiatarone MA, O'Neill EF, Ryan ND, et al. Exercise training and nutritional supplementation for physical frailty in very elderly people. N Engl J Med 1994; 330(25):1769-75. [DOI] [PubMed]
- 77.Dangour AD, Sibson VL, Fletcher AE. Micronutrient supplementation in later life: limited evidence for benefit. J Gerontol A Biol Sci Med Sci 2004;59(7):659-73. [DOI] [PubMed]
- 78.Position of the American Dietetic Association: nutrition, aging, and the continuum of care. J Am Diet Assoc 2000;100(5):580-95. [DOI] [PubMed]
- 79.Roy MA, Payette H. Meals-on-Wheels improves energy and nutrient intake in a frail free-living elderly population. J Nutr Health Aging. In press. [PubMed]
- 80.Keller HH, Ostbye T, Bright-See E. Predictors of dietary intake in Ontario seniors. Can J Public Health 1997;88(5):305-9. [DOI] [PMC free article] [PubMed]
- 81.Lipschitz DA, Mitchell CO, Steele RW, Milton KY. Nutritional evaluation and supplementation of elderly subjects participating in a “meals on wheels” program. JPEN J Parenter Enteral Nutr 1985;9(3):343-7. [DOI] [PubMed]
- 82.Krondl M, Coleman PH, Bradley CL, Lau D, Ryan N. Subjectively healthy elderly consuming a liquid nutrition supplement maintained body mass index and improved some nutritional parameters and perceived well-being. J Am Diet Assoc 1999;99(12):1542-8. [DOI] [PubMed]
- 83.Volkert D, Hubsch S, Oster P, Schlierf G. Nutritional support and functional status in undernourished geriatric patients during hospitalization and 6-month follow-up. Aging (Milano) 1996;8(6):386-95. [DOI] [PubMed]
- 84.Gray-Donald K, Payette H, Boutier V, Page S. Evaluation of the dietary intake of homebound elderly and the feasibility of dietary supplementation. J Am Coll Nutr 1994;13(3):277-84. [DOI] [PubMed]
- 85.Wendland BE, Greenwood CE, Weinberg I, Young KW. Malnutrition in institutionalized seniors: the iatrogenic component. J Am Geriatr Soc 2003;51(1):85-90. [DOI] [PubMed]
- 86.Brocker P, Vellas B, Albarede JL, Poynard T. A two-centre, randomized, double-blind trial of ornithine oxoglutarate in 194 elderly, ambulatory, convalescent subjects. Age Ageing 1994;23(4):303-6. [DOI] [PubMed]
- 87.Chu LW, Lam KS, Tam SC, Hu WJ, Hui SL, Chiu A, et al. A randomized controlled trial of low-dose recombinant human growth hormone in the treatment of malnourished elderly medical patients. J Clin Endocrinol Metab 2001;86(5):1913-20. [DOI] [PubMed]
- 88.Volicer L, Stelly M, Morris J, McLaughlin J, Volicer BJ. Effects of dronabinol on anorexia and disturbed behavior in patients with Alzheimer's disease. Int J Geriatr Psychiatry 1997;12(9):913-9. [PubMed]
- 89.Yeh SS, Wu SY, Lee TP, Olson JS, Stevens MR, Dixon T, et al. Improvement in quality-of-life measures and stimulation of weight gain after treatment with megestrol acetate oral suspension in geriatric cachexia: results of a double-blind, placebo-controlled study. J Am Geriatr Soc 2000;48(5):485-92. [DOI] [PubMed]
- 90.Ottery FD, Walsh D, Strawford A. Pharmacologic management of anorexia/cachexia. Semin Oncol 1998;25(2 Suppl 6):35-44. [PubMed]
- 91.Karcic E, Philpot C, Morley JE. Treating malnutrition with megestrol acetate: literature review and review of our experience. J Nutr Health Aging 2002;6(3):191-200. [PubMed]
- 92.Castle S, Nguyen C, Joaquin A, Coyne B, Heuston C, Chan A, et al. Megestrol acetate suspension therapy in the treatment of geriatric anorexia/cachexia in nursing home patients. J Am Geriatr Soc 1995;43(7):835-6. [DOI] [PubMed]
- 93.Jackobs MK. Megestrol acetate: a medical nutrition therapy tool to affect positive weight outcomes in the elderly [abstract]. J Am Diet Assoc 1999;99(Suppl 9):A-119.
- 94.Kardinal CG, Loprinzi CL, Schaid DJ, Hass AC, Dose AM, Athmann LM, et al. A controlled trial of cyproheptadine in cancer patients with anorexia and/or cachexia. Cancer 1990;65(12):2657-62. [DOI] [PubMed]
- 95.Morley JE. Orexigenic and anabolic agents. Clin Geriatr Med 2002;18(4):853-66. [DOI] [PubMed]
- 96.Takala J, Ruokonen E, Webster NR, Nielsen MS, Zandstra DF, Vundelickx G, et al. Increased mortality associated with growth hormone treatment in critically ill adults. N Engl J Med 1999;341(11):785-92. [DOI] [PubMed]
- 97.Gherondache CN, Dowling WJ, Pincus G. Metabolic changes induced in elderly patients with an anabolic steroid (oxandrolone). J Gerontol 1967;22(3):290-300. [DOI] [PubMed]
- 98.Hamerman D. Molecular-based therapeutic approaches in treatment of anorexia of aging and cancer cachexia. J Gerontol A Biol Sci Med Sci 2002;57(8):M511-8. [DOI] [PubMed]


