Abstract
Many pathology departments are introducing subspecialty sign-out in surgical pathology. In 2014, the University of Vermont Medical Center transitioned from general sign-out to partial subspecialty sign-out to include gastrointestinal and breast/cervix subspecialty benches; other specimens remained on general benches. Our experiences with the transition are described, including attending pathologist, trainee, support staff, and clinician satisfaction. A survey was e-mailed to all University of Vermont Medical Center anatomic pathology attendings, pathology trainees, pathologist assistants and grossing technicians, and clinicians who send surgical pathology specimens, immediately before and 1 year after transitioning to partial subspecialty sign-out. Quality assurance metrics were obtained for the 18 months prior to and following the transition. Gastrointestinal and breast/cervix attendings were more satisfied with partial subspecialty sign-out compared to those on the general benches. Overall, trainees were more satisfied with general sign-out because of the rotation schedule but preferred partial subspecialty sign-out due to improved teaching and more focused learning while on subspecialty benches. Clinicians remained very satisfied with our department and our reports; no differences were observed. Turnaround time was unchanged. After switching to partial subspecialty sign-out, there were significantly fewer discrepancies following multidisciplinary conference review for gastrointestinal and breast/cervix cases but remained the same for general cases. Fewer formal internal consults were performed after transitioning to partial subspecialty sign-out across all areas, but more notable for gastrointestinal and breast/cervix cases. Our data show improved quality assurance metrics and trainee education in a subspecialty sign-out setting compared to general sign-out setting.
Keywords: quality, resident education, subspecialization, surgical pathology
An increasing number of pathology departments are introducing subspecialty sign-out in surgical pathology (SP). Potential benefits include increased efficiency, shorter turnaround time (TAT), decreased use of immunohistochemical (IHC) stains, and the fact that the amount of information and knowledge needed to stay current on best practices and new research can be overwhelming across a wide spectrum of anatomic and clinical pathology. Since many of our clinical colleagues are subspecialized, we should also have the corresponding subspecialty knowledge and expertise. Additionally, learning for residents may be improved if their education comes from the experts in their knowledge areas.
However, there is also concern that becoming more specialized means that over time, pathologists lose touch with their “generalist” approach and knowledge, and some pathologists prefer to remain generalists. Additionally, there is concern that the change may have impact on resident education. Several editorials have been written on this topic,1-5 but there has been very little published on how other pathology departments have made the transition from general to subspecialty sign-out nor on the impact of this transition on education, workload, and satisfaction.6-8 A recent study published by Liu et al9 supports the transition to subspecialty. Their focus was primarily on how subspecialization affects the utilization of external consults. We aim to add to the limited number of published data and include additional quality assurance (QA) parameters as well as satisfaction reports from attending pathologists, pathology residents, and clinicians. On January 1, 2014, the University of Vermont Medical Center (UVMMC) Pathology and Laboratory Medicine Department transitioned from general sign-out (GSO) in SP to partial subspecialty sign-out (PSSO). Here, we describe our experiences with the transition and evaluate the satisfaction of clinicians, attending pathologists, pathology trainees, pathologist assistants (PAs), and grossing technicians (GTs) with SP before and after the switch to PSSO. Additionally, QA metrics such as TAT, formal and informal intradepartmental consults, discrepancy rate following external review, and discrepancy rate following review for multidisciplinary conference (MDC) are compared and discussed.
Institutional Environment
UVMMC is Vermont’s only nonprofit academic medical center and provides care for approximately 1 million people in Vermont, New Hampshire, and northern New York. It is the regional referral center with the region’s only level 1 trauma center, Vermont’s only neonatal intensive care unit, and also is the center for the University of Vermont Children’s Hospital and the University of Vermont Cancer Center. The medical center has 447 active inpatient beds.
The division of SP processed approximately 38 500 cases per year during the study time frame. In December 2013, there were 25 surgical pathologists, and in December 2014, there were 23 surgical pathologists. At both time intervals, 2 of those attending pathologists signed out dermatopathology specimens and 4 were only rarely signing out in SP (cross coverage pathologists). Dermatopathology had already been subspecialized and no changes were made to the service.
There are, on average, 16 residents enrolled in the program, 4 residents in each class, and 3 fellows: 1 SP fellow, 1 cytopathology fellow, and 1 dermatopathology fellow. Additionally, the department had 2 pathology student fellows each year, who spent a year in the department between their third and fourth year of medical school. In December 2013, there were 4 PAs and 1 GT; in December 2014, there were 5 PAs and 1 GT. The addition of 1 PA was to address the demand of an increase in volume at our institution.
In June 2013, barcoding of specimens, cassettes, and slides was introduced. Anecdotally, this slowed down productivity in the gross room as it took extra time to scan cassettes and add and delete blocks as needed. Not long after, in September 2013, a transition was made from an in-house transcription service to a voice dictation system. The software system used in the voice dictation system was complex and it took some time for individuals to adapt to using the system.
General Surgical Pathology System
Under the general SP system, cases were divided among 4 benches (A, B, C1, and C2), and 1 attending covered each bench. The A and B benches were resident benches, while the C1 and C2 benches were attending-only benches. The larger, more complex specimens were assigned to be grossed in by the resident benches, while the smaller, more routine nonbiopsy specimens were assigned to the C benches. All specimens that were grossed in by a resident were previewed by that resident for continuity. Pathologist assistants and GTs grossed in the C bench specimens and all biopsies. All dermatopathology specimens were grossed in by a PA or a GT and signed out by a dermatopathologist, which was a separate rotation for the residents. Surgical pathologists signed out lymph nodes, but hematopathologists were always available as consultants.
Three residents covered SP 1 month at a time and the SP fellow or a senior resident covered the hot seat rotation. Hot seat previewed and triaged all large specimens on the resident benches and divvied up the biopsies among the 4 benches. Resident benches were on a 3-day cycle with different daily rotation schedules (Table 1). The 2 C benches were on a 2-day cycle. Senior residents were able to rotate through these benches as a senior elective and they previewed and dictated the cases in the morning, functioning as a junior attending, and passed them on to the attending to be signed out.
Table 1.
Sample General SP Rotation for Resident Benches.
| Day 1 | Day 2 | Day 3 | |
|---|---|---|---|
| Resident 1 | am: sign-out A pm: preview B | am: sign-out B pm: gross A | am: frozen pm: gross B/preview A |
| Resident 2 | am: sign-out B pm: gross A | am: frozen pm: gross B/preview A | am: sign-out A pm: preview B |
| Resident 3 | am: frozen pm: gross B/preview A | am: sign-out A pm: preview B | am: sign-out B pm: gross A |
Abbreviation: SP, surgical pathology.
On a frozen section (FS) day, the pathologist would cover all FS cases that came in that day; the FS resident was responsible for assisting with performing and interpreting FS until noon. In the afternoons, the hot seat covered FS and functioned as a junior attending for FS, with attending backup and support as needed. The FS pathologist also reviewed gross-only specimens, at least 10 gastrointestinal (GI) biopsies, and outside review of slides (ROS).
Each afternoon, there was an intradepartmental consensus conference (IDCC) where pathologists gathered together to discuss and review interesting and challenging cases. Generally, all pathologists on service attended, and often others who were in-house would also attend. Anecdotally, on average approximately 5 individuals attend IDCC on any given day.
Partial Subspecialty System
Under the partial subspecialty system, cases were allocated to 1 of 4 benches, with 1 attending pathologist covering each bench: GI, breast/cervix (BR), general 1, and general 2. Both GI and BR cases were chosen as the subspecialties due to volume of specimens, number of available subspecialists, and following conversations with clinical specialists in these areas. Three residents covered SP for a 4-week block (Table 2); GI, BR, and general 1 benches were covered by residents, while general 2 bench was an attending-only bench. More complex cases were often assigned to general 1 bench, but cases were also divvied up based on each pathologist’s expertise and interests and daily volume on the 2 general benches. For example, if an attending with expertise in pulmonary pathology and an attending with expertise in genitourinary pathology were on the 2 general benches, the pulmonary cases were assigned to the first pathologist and vice versa.
Table 2.
Sample Subspecialty SP Rotation for Resident Benches.
| Week 1-2 | Week 3-4 | |
|---|---|---|
| Resident 1 | am: sign-out BR pm: gross/preview BR | am: sign-out general 1 pm: gross/preview general 1 |
| Resident 2 | am: sign-out GI pm: gross/preview GI | am: sign-out BR pm: gross/preview BR |
| Resident 3 | am: sign-out general 1 pm: gross/preview general 1 | am: sign-out GI pm: gross/preview GI |
Abbreviations: BR, breast/cervix; GI, gastrointestinal; SP, surgical pathology.
Resident benches signed out in the morning and grossed and previewed in the afternoon and evening; cases remained on a 3-day cycle. General 2 (attending-only) bench remained on a 2-day cycle. Again, senior residents were able to rotate through this bench as a senior elective and function as junior attendings. No changes to the handling of dermatopathology specimens were made. Neuropathology cases remained on the general benches. Rather than having hematopathologists consult on cases, lymph nodes were signed out by a hematopathologist unless they were submitted for workup of metastatic disease, in which case they were assigned to the appropriate bench.
FS were covered by a fifth pathologist. The FS pathologist also reviewed all gross-only specimens, at least 10 GI biopsies (mostly polyps), and non-GI and BR ROS; GI and BR ROS were reviewed by the appropriate subspecialty benches. Residents started assisting with performing and interpreting FS on their fourth block on SP. One morning each week, they predictated their cases and handed them to their attending pathologist, who signed out the cases alone and provided feedback to the trainee at a later time. In lieu of signing out cases, the resident assisted with any FS that came in that morning. Every afternoon, the trainee on hot seat functioned as a junior attending for FS, similar to the GSO system.
Each specialty (GI, BR, and general) held their own separate IDCC each afternoon. Generally, most GI and BR pathologists attend their own IDCCs, regardless of whether or not they were on service. For the general IDCC, it was often the 2 pathologists on the general benches, the FS attending, and the trainee on hot seat who attended. Sometimes, additional general pathologists attended if they were in-house. Anecdotally, an average of 2 to 3 individuals attended the general IDCC on any given day.
Materials and Methods
In December 2013, prior to implementing PSSO, a survey was e-mailed to all UVMMC anatomic pathology attending pathologists, all current UVMMC pathology trainees (residents, fellows, and student fellows), all UVMMC PAs and GTs, and all clinicians who send SP specimens to UVMMC (Appendices A to D, General). Participation in the study and completion of the survey were entirely voluntary and completely anonymous.
The same survey was sent out to the same distribution (current UVMMC pathologists, trainees, and PAs/GTs, as well as to clinicians who send SP specimens to UVMMC) in December 2014, 1 year after implementing PSSO. Additional questions focusing on subspecialty sign-out were included following completion of the main survey (Appendices A to D, Partial Subspecialty).
The responses for each of the questions in the survey, GSO system (first survey) versus PSSO system (second survey), were compared. For the second survey, attending pathologist responses were also compared based on whether the respondent signed out subspecialty benches (GI and BR) or general benches. For the clinician surveys, responses were evaluated overall. Additionally, individuals who regularly utilize SP services often discuss cases with the pathologists were evaluated separately. These clinicians include those who stated they were in colon and rectal surgery, dermatology, gastroenterology and hepatology, general surgery, gynecologic oncology, hematology and medical oncology, nephrology, neurosurgery, obstetrics and gynecology, otolaryngology, pulmonology, radiation oncology, transplant surgery, and urology. While some respondents may have completed surveys both before and after the implementation of the subspecialty sign-out system, it was impossible to match pre- and postsurveys. Thus, results across time as well as between attendings who signed out subspecialty versus general benches were compared using the Wilcoxon rank sum test.
Quality assurance measures including TAT, cases shown at IDCC, formal internal consult requests, and discrepancies after MDC were already being tracked for the department’s monthly QA review. The results were tabulated for the 18 months prior to subspecialization (July 2012 to December 2013) and the 18 months after subspecialization (January 2014 to June 2015). The differences in percentage of cases shown at IDCC, formal internal consult requests, and discrepancies after MDC were compared using the χ2 test of independence or Fisher’s exact test. The types of discrepancies were also noted: level 1—little or no clinical impact, level 2—potential clinical impact, and level 3—definite clinical impact.
Utilization of several IHC stains, which are specific to GI and BR, was also reviewed for the 18 months before and after the transition to PSSO. These stains were P16 and MIB-1 in cervix specimens to differentiate high-grade dysplasia from reactive atypia, E-cadherin in breast specimens to differentiate lobular from ductal carcinoma, P63 and heavy chain myosin (HCM) in breast specimens for identification of invasion, and Helicobacter pylori (HP) stain in GI biopsies. The differences in utilization were compared using χ2 test of independence.
Results
Attending Pathologist Satisfaction
Seventeen of 25 surgical pathologists (68.0%) completed the first survey and 15 of 23 surgical pathologists (65.2%) completed the second survey. Two of these 15 did not answer the additional questions focusing on subspecialty sign-out, and it is suspected that these 2 were dermatopathologists, as those questions did not pertain to them. Of the 13 who completed the entire second survey (56.5%), 3 were subspecialists—1 (33.3%) of 3 GI pathologists and 2 (50.0%) of 4 BR pathologists—and 10 signed out other benches (of 16, 62.5%).
Pathologists were significantly more satisfied with the mix of cases they saw with the GSO system compared to the subspecialty system (P = .022). Otherwise, no differences were identified, including overall satisfaction with the sign-out systems (Figure 1), feeling more efficient with either system, being satisfied with the ability to teach residents, number of hours worked, nor feeling the number of hours worked was appropriate. Overall, when specifically asked which type of sign-out they preferred, pathologists were split between preferring general versus subspecialty sign-out (46% vs 53%, respectively).
Figure 1.
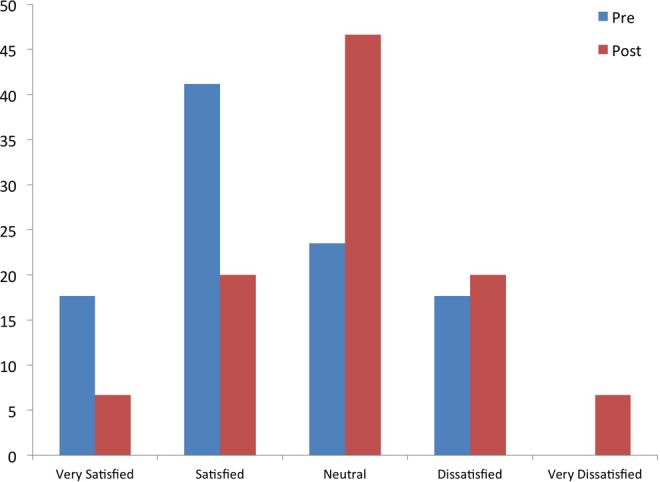
Overall satisfaction of attending with sign-out presubspecialization (blue) and postsubspecialization (red).
In comparing the 3 subspecialty pathologists (GI and BR) to the 10 general pathologists, subspecialty pathologists were more satisfied with the mix of cases they see (P = .032). There was a trend toward the subspecialty pathologists feeling more satisfied with their ability to teach residents (P = .088) and overall satisfaction with the sign-out system (P = .084; Figure 2). When asked in the additional subspecialty questions in the second survey, subspecialists felt better able to teach residents (P = .046) and there was a trend toward feeling more comfortable signing out their cases than the generalists (P = .084).
Figure 2.
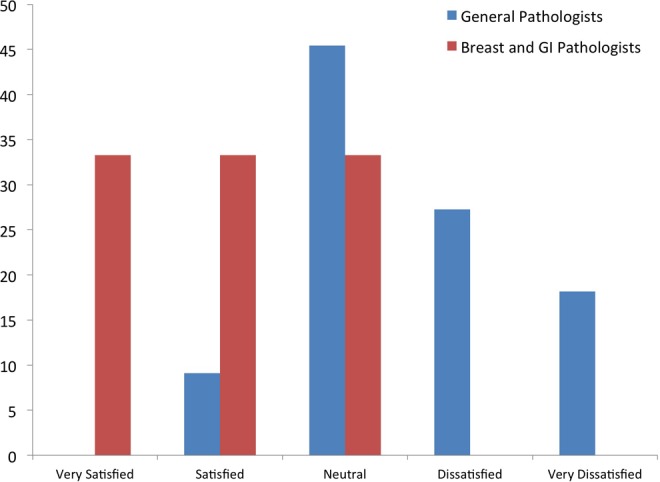
Satisfaction with subspecialty sign-out by pathologist type, general pathologists (blue) and subspecialty (breast and GI) pathologists (red).
Trainee Satisfaction
At the time that both surveys were sent out, there were 22 trainees in the program—17 residents, 3 fellows, and 2 student fellows. One resident did not complete either of the surveys due to being involved in the study. Twelve (54.5%) trainees completed the first survey and 16 (72.7%) completed the second survey. There was no difference between the 2 surveys in the number of months of SP completed or in the number of hours worked.
Overall, trainees were significantly more satisfied with the GSO system compared to the subspecialty sign-out system (P = .043; Figure 3). However, when residents were specifically asked in the second survey, 9 of 10 trainees stated that they preferred subspecialty sign-out (Figure 4). In the second survey, when asked about teaching and learning, 80% of trainees agreed or strongly agreed that they were able to better focus their learning with PSSO and 90% agreed or strongly agreed that there was better teaching from attending pathologists with PSSO. There was a trend toward feeling more satisfied with teaching from pathologists with the subspecialty system (P = .094). The trainees were significantly more satisfied with the time available to preview under the GSO format compared to the partial subspecialty format (P = .002). Otherwise, there was no difference in response between the 2 surveys on any other questions (including satisfaction with time to gross, support from PAs/GTs and attending pathologists, and the mixtures of cases seen).
Figure 3.
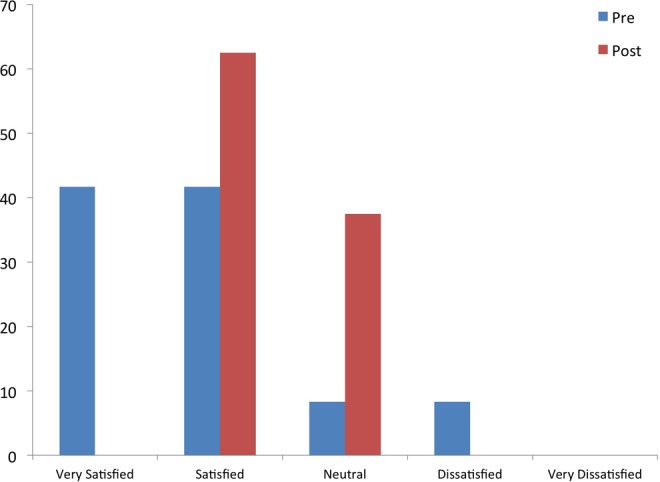
Overall satisfaction of residents with sign-out presubspecialization (blue) and postsubspecialization (red).
Figure 4.
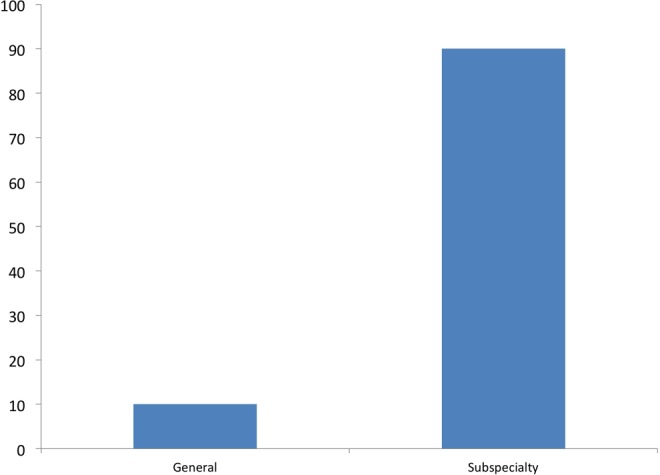
Resident preference for general or subspecialty sign-out.
Pathologist Assistant/Grossing Technician Satisfaction
One hundred percent of PAs and GTs completed both surveys. There was no significant difference in the satisfaction with the GSO system versus the PSSO system. Four (66.7%) of six PAs and GTs preferred the subspecialty sign-out system over the general system.
Clinician Satisfaction
The first survey was e-mailed to 1048 clinicians and 96 completed it (9.16% response rate). The second survey was e-mailed to 1168 individuals and 73 completed it (6.25% response rate). However, many of the recipients of the e-mail do not regularly utilize our services. When looking at only the high utilization group, 52 of 199 completed the first survey (26.1% response rate) and 35 of 195 completed the second survey (17.9% response rate).
For all clinician responses, there was no difference between the first and second surveys and the majority of clinicians were satisfied or very satisfied overall (Figure 5). In looking at the additional subspecialty questions in the second survey, many clinicians strongly agreed or agreed that pathology reports were more consistent (40.8%), were more confident in the accuracy of the reports (42.3%), and felt it was easier to obtain a pathology consult after making the switch to subspecialty sign-out (27.8%). Additionally, a high percentage of clinicians were neutral in feeling that the pathology reports were more consistent (46.5%), in their confidence in the accuracy of reports (45.1%), and in feeling it was easier to obtain a pathology consult after making the switch to subspecialty sign-out (52.8%). The majority of respondents (67.7%) stated that they did not notice a difference in the overall quality of pathology reports and consults.
Figure 5.
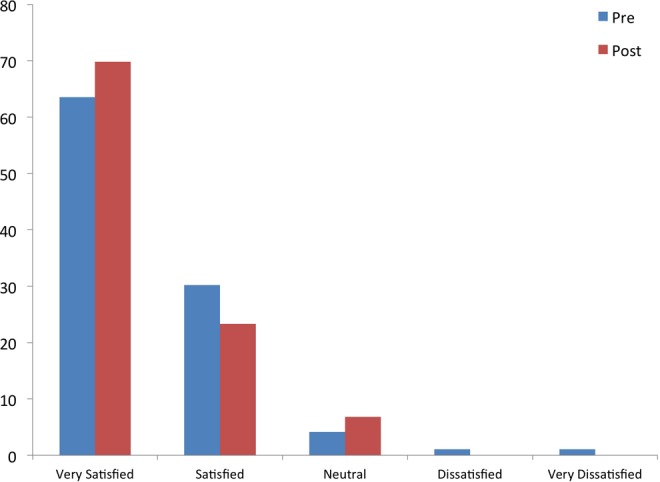
Overall satisfaction of clinicians with our surgical pathology department presubspecialization (blue) and postsubspecialization (red).
There was also no significant difference in responses between the first and second surveys when looking at the high utilization subset of clinicians. However, there was a trend toward increased satisfaction with pathologist accessibility for consultation after subspecialization (P = .079) and with the consultation itself (P = .075). In looking at the additional subspecialty questions, many respondents strongly agreed or agreed that pathology reports were more consistent (67.7%), were more confident in the accuracy of reports (67.7%), and felt it was easier to obtain a pathology consult after making the switch to subspecialty sign-out (45.2%). Additionally, many clinicians were neutral in feeling that pathology reports were more consistent (32.3%), in their confidence in the accuracy of the reports (32.3%), and in feeling it was easier to obtain a pathology consult after making the switch to subspecialty sign-out (45.2%). In this group, 50% of respondents stated that they noticed a difference in the overall quality of the pathology reports and consults, while 50% did not.
Quality Assurance Measures
See Tables 3 to 5 for a summary of data. A total of 49 260 cases were signed out for the 18 months prior to switching to partial subspecialization and 57 294 cases were signed out in the 18 months after the switch, which represents a 6.9% increase in cases.
Table 3.
Quality Assurance Measures.
| Before Partial Subspecialty | After Partial Subspecialty | P Value | |
|---|---|---|---|
| Total number of cases | 49 260 | 57 294 | Not applicable |
| Shown at IDCC | 4900 (9.95%) | 4679 (8.17%) | <.0001 |
| Internal consult | 2931 (5.95%) | 2294 (4.00%) | <.0001 |
| External consult | 1043 (2.12%) | 1106 (1.93%) | .0322 |
| Discrepancy after external consult | 20 (1.91%) | 7 (0.63%) | .008 |
| Level 1 errors | 18 (90.00%) | 5 (71.43%) | .27 |
| Level 2/3 errors | 2 (10.00%) | 2 (28.57%) |
Abbreviation: IDCC, intradepartmental consensus conference.
Table 4.
Formal Internal Consults by Subspecialty.
| Before Partial Subspecialty | After Partial Subspecialty | P Value | |
|---|---|---|---|
| Gastrointestinal | 451 of 14 825 (3.04%) | 203 of 15 751 (1.29%) | <.0001 |
| Breast/cervix | 394 of 3616 (10.90%) | 204 of 5841 (3.49%) | <.0001 |
| General | 1571 of 14 227 (11.04%) | 1159 of 15 553 (10.02%) | <.0001 |
| Dermatopathology | 515 of 16 592 (3.10%) | 728 of 20 149 (3.61%) | .007 |
Table 5.
Discrepancy After Multidisciplinary Clinic Review.
| Before Partial Subspecialty | After Partial Subspecialty | P Value | |
|---|---|---|---|
| Shown at MDC | 4017 (8.15%) | 3841 (6.70%) | <.0001 |
| Gastrointestinal | 1432 (35.65%) | 1116 (29.05%) | <.0001 |
| Breast/cervix | 1089 (27.11%) | 1164 (30.30%) | |
| General | 921 (22.93%) | 1016 (26.45%) | |
| Dermatopathology | 575 (14.31) | 545 (14.19) | |
| Discrepancy after MDC review | 88 (2.19%) | 23 (0.60%) | <.0001 |
| Total GI discrepancies | 41 (2.86%) | 8 (0.72%) | <.0001 |
| Total breast/cervix discrepancies | 34 (3.12%) | 5 (0.43%) | <.0001 |
| Total general discrepancies | 13 (1.41%) | 10 (0.98%) | .41 |
| Total dermatopathology discrepancies | 0 (0.0%) | 0 (0.0%) | .99 |
Abbreviations: GI, gastrointestinal; MDC, multidisciplinary conference.
Turnaround time
Prior to subspecialization, the average TAT for all cases was 51.81 hours. After subspecialization, the average TAT for all cases was 52.15 hours. Standard deviation or standard error information was not available to perform statistical analysis.
Intradepartmental consensus conferences (IDCC)
Overall, significantly fewer cases were shown at IDCC and had formal consults in the 18 months after transitioning to PSSO (P < .0001 for both GI and BR; Table 4). For GI cases, 451 (3.04%) of 14 825 cases had formal internal consults prior to the transition and 203 (1.29%) of 15 751 had formal internal consults following the transition to PSSO (P < .0001). For BR cases, 10.90% (394 of 3616 cases) and 3.49% (204 of 5841) had formal internal consults before and after the transition, respectively (P < .0001). For cases that fall into the general benches, these numbers were 11.04% (1571 of 14 227 cases) and 7.45% (1159 of 15 553 cases; P < .0001), respectively. Finally in dermatopathology, 515 (3.10%) of 16 592 and 728 (3.61%) of 20 149 had formal internal consults (P = .007).
Multidisciplinary conference reviews
Overall, significantly fewer cases were shown at MDC under the PSSO system (P < .0001; Table 5). The distribution of cases under the 2 sign-out systems was significantly different (P < .0001): GI made up a greater portion of the cases shown at MDC prior to subspecialization, whereas it made up a lower proportion of cases shown at MDC after transitioning to PSSO, with a higher proportion of BR and general cases. While there were significantly more discrepancies identified overall with GSO compared to PSSO (P < .0001), there was no difference in the type of errors (P = .73, Fisher’s exact test). The MDC discrepancies were then evaluated based on subspecialty benches. Both GI and BR discrepancies following MDC review decreased significantly after transitioning to partial subspecialty (P < .0001 for both). However, discrepancies did not change for cases on the general bench (P = .41).
External reviews
While the number of cases sent for external review did not change (P = .095), there were significantly fewer discrepancies, between our diagnosis and the diagnosis on external review, after transitioning to partial subspecialty (P = .008). However, there was no difference in the types of errors (P = .27, Fisher’s exact test).
Immunohistochemical stains
See Table 6 for a summary of data. There was no change in the utilization of IHC stains in cervical specimens. Similarly, the utilization of HCM and P63 in breast specimens remained the same. Utilization of E-cadherin on breast specimens significantly decreased (P = .0018). Interestingly, staining for HP in gastric specimens significantly increased (P < .0001).
Table 6.
Immunohistochemical Stain Utilization.
| Antibody | Organ | Before Partial Subspecialty | After Partial Subspecialty | P Value | ||
|---|---|---|---|---|---|---|
| Total Cases | Stained | Total Cases | Stained | |||
| P16 | Cervix | 1825 | 226 (12.38%) | 1972 | 229 (11.61%) | .46 |
| MIB-1 | Cervix | 1825 | 58 (3.18%) | 1972 | 54 (2.74%) | .42 |
| E-cadherin | Breast | 2359 | 139 (5.89%) | 2368 | 93 (3.93%) | .0018 |
| P63 | Breast | 2359 | 195 (8.27%) | 2368 | 163 (6.88%) | .07 |
| HCM | Breast | 2359 | 159 (6.74%) | 2368 | 163 (6.88%) | .85 |
| HP | Stomach | 3463 | 1718 (49.61%) | 3603 | 2260 (62.73%) | <.0001 |
Abbreviations: HCM, heavy chain myosin; HP, Helicobacter pylori.
Discussion
The transition from GSO to PSSO was a difficult process, and at the time of publication, one that continues to be adjusted. Overall, the switch was positive, with most trainees and PAs/GTs preferring PSSO and the attending pathologists being relatively evenly split between the 2 systems. The satisfaction of our clinicians with our department was very high before the transition to PSSO and continued to remain high after the transition. There was no change in clinician satisfaction with our department or our reports. For clinicians who are likely to review more pathology reports, there was a trend toward increased satisfaction with pathology consultations and pathologist accessibility for the consults, but they did not notice a difference in the overall quality of pathology reports and consults.
Pathologists and trainees liked the mix of cases that they saw and the education and learning that came with a more focused range of topics while on subspecialty benches. However, pulling out only a few subspecialty areas meant that the majority of pathologists were still general pathologists but without being able to evaluate the full spectrum of cases that go through SP. When compared to the subspecialty benches, the education in the general benches felt more disjointed and dispersed, which went with the high variability and complexity of types of specimens seen. Based on anecdotal evidence and the responses in this survey, the subspecialty pathologists (those signing out the GI and BR benches) were more satisfied with the transition to partial subspecialization, while many of those signing out the general benches were dissatisfied with being caught in the middle—no longer being true generalists, but also not being able to fully subspecialize. Comments from pathologists signing out the general benches state that there is a need to subspecialize even more, as cases on the general benches are often very complex and diverse, resulting in more consults, as evidenced by similar rates of formal internal consults requested by general pathologists before and after the transition to PSSO (further discussed below).
The dichotomy between the overall satisfaction for GSO and the preference for subspecialty sign-out by trainees is likely because the dissatisfaction with subspecialty sign-out was mostly due to dissatisfaction with the overall system, particularly in losing a dedicated preview afternoon and needing to sign-out, gross, and preview every day. Anecdotally, there also seemed to be less frozen section exposure for trainees. However, trainees preferred the directed teaching and learning while on the subspecialty benches.
In general, there was no difference in PA/GT satisfaction identified before or after the switch to partial subspecialty. Concerns about adequate space in the gross room were prevalent at both time points; all respondents stating they were neutral or disagreed that there was adequate space in the gross room. This is particularly true after making the switch to partial subspecialty: Under the GSO system, 2 of the 3 residents were grossing on any given day while under the partial subspecialty system and all 3 residents were in the gross room every day. The trend toward feeling as though there was less ability to complete their work in the allotted time may have been impacted, in part, by the introduction of barcoding and voice dictation software, rather than as a result of switching to partial subspecialty. The respondents noted that they enjoyed the opportunity to gross more complex specimens under the subspecialty system.
Quality assurance measures remained the same or improved following the transition to PSSO. Turnaround time was not affected (51.81 vs 52.15 h, respectively) and fewer discrepancies were identified after both MDC and external review. Significantly fewer cases were being shown at MDC overall. Cases for MDC are selected by the respective clinical team. Most cases are selected for discussion regarding multidisciplinary management approaches. However, some cases are selected for review to clarify pathology diagnostic reports. With the introduction of subspecialty sign-out, pathology reports became more consistent, which we believe eliminated some uncertainties in the eyes of the clinicians, and therefore contributed to the decrease in the number of cases shown at MDC. There were also fewer discrepancies after MDC review. When separated by subspecialty bench, the decrease in discrepancies holds true for both the GI and BR benches. However, there was no change in the number of discrepancies for specimens signed out on the general bench. As expected, dermatopathology remained relatively stable during both time periods. These findings suggest that when cases are signed out by specialists, fewer discrepant results occur.
The number of formal internal consults decreased overall. However, when these consults were broken down by subspecialty bench for the 18 months after making the switch, there was a noticeable difference in the number of formal consults obtained: The percentage of cases for both the GI and BR benches decreased by over 50% (3.04% to 1.29% for GI and 10.90% to 3.49% for BR), while the percentage of cases for the general benches decreased from 11.04% to 7.45% (Table 4). Where these decreases were all statistically significant, there was a much more noticeable decrease in the subspecialty benches. While the GI and BR pathologists can reliably show difficult and interesting cases to other subspecialists at IDCC, the likelihood of a particular general pathologist with a certain expertise (lung or soft tissue, for example) being at IDCC can be variable and depends on who is on service. In these instances, a formal consult request is made instead of showing the case at IDCC.
The percentage of E-cadherin stains ordered on breast specimens decreased after implementing PSSO. The smaller group of breast pathologists have agreed that performing E-cadherin on core needle biopsies (the majority of E-cadherin stains) which show both ductal and lobular features does not have significant clinical utility and therefore are not ordering as many E-cadherin stains compared to the GSO period. The utilization of other IHC stains for cervical and breast specimens (P16 and MIB-1, and P63 and HCM, respectively) remained the same because these stains do continue to have clinical significance and utility.
Interestingly, this study identified increased use of HP in gastric biopsies following the transition to PSSO. Like using P16 and MIB-1 in cervical specimens and P63 and HCM in breast specimens, HP has clinical utility and therefore a decrease was not expected. We noted a difference in IHC stain ordering practices of SP fellows during this time, with one fellow tending to have a lower threshold to order HP (data not included); this might have contributed to the difference. Further investigation into the reasons and impact of increased HP utilization is also currently being reviewed.
These findings support transitioning to subspecialization. It may be preferable to transition to full subspecialization due to decreased discrepancies following review of cases at MDC or external reviews, overall decreased utilization of IHC stains, and improved trainee education. However, this would not be feasible at our institution due to volume considerations and the number of subspecialty pathologists in certain subspecialties.
We are currently working on revamping our SP system to address concerns that were elucidated through this project as well as in discussions within the department. At the time of this publication, a LEAN process is in progress to reevaluate our system. There is no immediate plan to finalize subspecialization at our institution. However, we are evaluating the general bench, which may lead to further subspecialization. Specific goals include improving general bench workflow, efficiency, and satisfaction and restructuring FS duties to improve workflow and efficiency and to improve trainee education—especially on general benches—to enhance resident experiences in grossing, previewing, and signing out.
One goal of the transition was to ensure that trainees had more exposure to ancillary prognostic and molecular testing (such as estrogen receptor, progesterone receptor, and human epidermal growth factor receptor 2 testing in breast specimens, and mismatch repair protein expression in GI cases). These tests have been incorporated into sign-out and residents now review breast prognostic markers and mismatch repair protein expression for their cases.
Of note, clinician satisfaction with both systems was very high, and the transition from GSO to PSSO did not have a significant effect on the quality of services our department provides. Ultimately, regardless of whether or not a department chooses to subspecialize, it is necessary to remember that maintaining patient safety and having a good relationship with clinicians is of paramount importance.
Acknowledgments
We would like to thank Timothy St John for his assistance in running searches in our laboratory information system to obtain laboratory data related to QA.
Appendix A
Attending Pathologist Survey (General)
-
How satisfied are you with the current mix of cases you see on surgical pathology when on service?
○ Very satisfied ○ Satisfied ○ Neutral ○ Dissatisfied ○ Very dissatisfied
-
How efficient are you with the current surgical pathology sign-out pattern?
○ Very efficient ○ Efficient ○ Neutral ○ Inefficient ○ Very inefficient
-
How satisfied are you with the ability to teach residents while on service?
○ Very satisfied ○ Satisfied ○ Neutral ○ Dissatisfied ○ Very dissatisfied
-
I feel that the number of hours I work while on service is appropriate.
○ Strongly agree ○ Agree ○ Neutral ○ Disagree ○ Strongly disagree
-
On average, how many hours per week do you work while on surgical pathology?
○ <40 ○ 40-50 ○ 51-60 ○ 61-70 ○ >70
-
Overall, how satisfied are you with the current surgical pathology sign-out rotation?
○ Very satisfied ○ Satisfied ○ Neutral ○ Dissatisfied ○ Very dissatisfied
Comments
Attending Pathologist Survey Additional Questions (Partial Subspecialty)
In January 2014, we transitioned from a general surgical pathology sign-out to a partial subspecialty sign-out. All gastrointestinal (GI) specimens are now signed out by GI pathologists, breast and cervical specimens are now signed out by breast pathologists, and all remaining specimens are signed out by general pathologists. With this in mind, please respond to the following statements/questions.
-
8. I feel more comfortable signing out my cases now with partial subspecialty sign-out than in the past.
○ Strongly agree ○ Agree ○ Neutral ○ Disagree ○ Strongly agree ○ N/A
-
9. I feel I am better able to teach residents now than in the past.
○ Strongly agree ○ Agree ○ Neutral ○ Disagree ○ Strongly agree ○ N/A
-
10. Which bench do you sign-out?
○ Breast/cervix ○ Gastrointestinal ○ General
-
11. Do you prefer partial subspecialty or general sign-out?
○ Subspecialty ○ General
12. Comments
Appendix B
Trainee Survey (General)
-
How satisfied are you with the amount of time you have to preview your cases?
○ Very satisfied ○ Satisfied ○ Neutral ○ Dissatisfied ○ Very dissatisfied
-
How satisfied are you with the amount of time you have to gross in your specimens?
○ Very satisfied ○ Satisfied ○ Neutral ○ Dissatisfied ○ Very dissatisfied
-
How satisfied are you with the current mix of cases you see on surgical pathology?
○ Very satisfied ○ Satisfied ○ Neutral ○ Dissatisfied ○ Very dissatisfied
-
How satisfied are you with the teaching you get from attendings on surgical pathology?
○ Very satisfied ○ Satisfied ○ Neutral ○ Dissatisfied ○ Very dissatisfied
-
How satisfied are you with the amount of support you have in the gross room from attendings?
○ Very satisfied ○ Satisfied ○ Neutral ○ Dissatisfied ○ Very dissatisfied
-
How satisfied are you with the PAs’ availability for teaching?
○ Very satisfied ○ Satisfied ○ Neutral ○ Dissatisfied ○ Very dissatisfied
-
How satisfied are you with the teamwork between residents and PAs in the gross room?
○ Very satisfied ○ Satisfied ○ Neutral ○ Dissatisfied ○ Very dissatisfied
-
How satisfied are you with the amount of support you have from the LAs?
○ Very satisfied ○ Satisfied ○ Neutral ○ Dissatisfied ○ Very dissatisfied
-
How many months of surgical pathology (including bridge month) have you completed?
○ 1-2 ○ 3-4 ○ 5-7 ○ 8-11 ○ At least 1 hot seat or C-bench
-
On average, how many hours per week do you work while on surgical pathology?
○ <40 ○ 40-50 ○ 51-60 ○ 61-70 ○ >70
-
Overall, how satisfied are you with the current surgical pathology sign-out rotation?
○ Very satisfied ○ Satisfied ○ Neutral ○ Dissatisfied ○ Very dissatisfied
Comments
Resident Survey Additional Questions (Partial Subspecialty)
In January 2014, we transitioned from a general surgical pathology sign-out to a partial subspecialty sign-out. All gastrointestinal (GI) specimens are now signed out by GI pathologists, breast and cervical specimens are now signed out by breast pathologists, and all remaining specimens are signed out by general pathologists. With this in mind, please respond to the following statements/questions.
-
I feel I am able to focus my learning more with partial subspecialty sign-out than in the past.
○ Strongly agree ○ Agree ○ Neutral ○ Disagree ○ Strongly agree ○ N/A
- I feel I get better teaching from attendings now with partial subspecialty sign-out than in the past.
- ○ Strongly agree ○ Agree ○ Neutral ○ Disagree ○ Strongly agree ○ N/A
- Do you prefer partial subspecialty or general sign-out?
- ○ Subspecialty ○ General
Comments
Appendix C
Pathologist Assistant/Grossing Technician Survey (General)
-
There is adequate work space to accommodate everyone in the gross room.
○ Strongly agree ○ Agree ○ Neutral ○ Disagree ○ Strongly disagree
-
How satisfied are you with your availability to teach residents?
○ Very satisfied ○ Satisfied ○ Neutral ○ Dissatisfied ○ Very dissatisfied
-
How satisfied are you with the teamwork between residents and PAs in the gross room?
○ Very satisfied ○ Satisfied ○ Neutral ○ Dissatisfied ○ Very dissatisfied
-
I am able to finish my work within the daily allotted work hours.
○ Strongly agree ○ Agree ○ Neutral ○ Disagree ○ Strongly disagree
-
Overall, how satisfied are you with the current surgical pathology rotation in the gross room?
○ Very satisfied ○ Satisfied ○ Neutral ○ Dissatisfied ○ Very dissatisfied
Comments
Pathologist Assistant/Grossing Technician Survey Additional Questions (Partial Subspecialty)
In January 2014, we transitioned from a general surgical pathology sign-out to a partial subspecialty sign-out. All gastrointestinal (GI) specimens are now signed out by GI pathologists, breast and cervical specimens are now signed out by breast pathologists, and all remaining specimens are signed out by general pathologists. With this in mind, please respond to the following statements/questions.
-
7. I enjoy the scope and type of specimens I’m grossing in now with partial subspecialty sign-out than in the past.
○ Strongly agree ○ Agree ○ Neutral ○ Disagree ○ Strongly disagree
-
8. Do you prefer partial subspecialty benches or general benches?
○ Subspecialty ○ General
9. Comments
Appendix D
Clinician Survey (General)
What is your specialty?
-
What is your provider level?
○ MD/DO ○ PA ○ NP ○ RN ○ Other—please specify
-
How satisfied are you with pathologist accessibility for consultation?
○ Very satisfied ○ Satisfied ○ Neutral ○ Dissatisfied ○ Very dissatisfied ○ N/A
-
How satisfied are you with the pathologist consultations?
○ Very satisfied ○ Satisfied ○ Neutral ○ Dissatisfied ○ Very dissatisfied ○ N/A
-
The pathology reports I receive are complete.
○ Strongly agree ○ Agree ○ Neutral ○ Disagree ○ Strongly agree ○ N/A
-
The pathology reports I receive are clear.
○ Strongly agree ○ Agree ○ Neutral ○ Disagree ○ Strongly agree ○ N/A
-
The pathology reports I receive are readable.
○ Strongly agree ○ Agree ○ Neutral ○ Disagree ○ Strongly agree ○ N/A
-
The pathology reports I receive are accurate.
○ Strongly agree ○ Agree ○ Neutral ○ Disagree ○ Strongly agree ○ N/A
-
Overall, how satisfied are you with the surgical pathology department?
○ Very satisfied ○ Satisfied ○ Neutral ○ Dissatisfied ○ Very dissatisfied ○ N/A
Comments
Clinician Survey Additional Questions (Partial Subspecialty)
In January 2014, we transitioned from a general surgical pathology sign-out to a partial subspecialty sign-out. All gastrointestinal (GI) specimens are now signed out by GI pathologists, breast and cervical specimens are now signed out by breast pathologists, and all remaining specimens are signed out by general pathologists. With this in mind, please respond to the following statements/questions.
-
11. The pathology reports I receive are more consistent now than they were in the past.
○ Strongly agree ○ Agree ○ Neutral ○ Disagree ○ Strongly agree ○ N/A
-
12. I feel more confident in the accuracy of the pathology reports I receive.
○ Strongly agree ○ Agree ○ Neutral ○ Disagree ○ Strongly agree ○ N/A
-
13. It is easier for me to obtain a pathology consult now than in the past.
○ Strongly agree ○ Agree ○ Neutral ○ Disagree ○ Strongly agree ○ N/A
-
14. Have you noticed an overall difference in the quality of pathology report or pathology consult since we implemented partial subspecialty sign-out?
○ Yes ○ No
15. Comments
Footnotes
Declaration of Conflicting Interests: The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Sarewitz SJ. Subspecialization in community pathology practice. Arch Pathol Lab Med. 2014;138:871–872. [DOI] [PubMed] [Google Scholar]
- 2. Heatley MK. Subspecialisation and despecialisation in anatomical pathology. J Clin Pathol. 2010;63:761–767. [DOI] [PubMed] [Google Scholar]
- 3. Murphy WM. Anatomical pathology in the 21st century: the great paradigm shift. Hum Pathol. 2007;38:957–962. [DOI] [PubMed] [Google Scholar]
- 4. Kirkham N. The pathologist in the 21st century—generalist or specialist? J Clin Pathol. 2000;53:7–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Watts JC. Is there still a need for the general surgical pathologist? Am J Clin Pathol. 1996;106(4 suppl 1):S74–S76. [PubMed] [Google Scholar]
- 6. Groppi DE, Alexis CE, Sugrue CF, Bevis CC, Bhuiya TA, Crawford JM. Consolidation of the North Shore-LIJ Health System anatomic pathology services: the challenge of subspecialization, operations, quality management, staffing, and education. Am J Clin Pathol. 2013;140:20–30. [DOI] [PubMed] [Google Scholar]
- 7. Sanders DS, Carr RA, Stores OP, Chachlani N, Simon J. Subspecialisation in cellular pathology in the DGH setting: the Warwick experience. J Clin Pathol. 2006;59:884–886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Black-schaffer WS, Young RH, Harris NL. Subspecialization of surgical pathology at the Massachusetts General Hospital. Am J Clin Pathol. 1996;106(4 suppl 1):S33–S42. [PubMed] [Google Scholar]
- 9. Liu YJ, Kessler M, Zander DS, Karamchandani DM. Trends in extramural consultation: comparison between subspecialized and general surgical pathology service models. Ann Diagn Pathol. 2016;24:20–24. [DOI] [PubMed] [Google Scholar]


