Abstract
Study Objectives:
To determine the associations of self-reported sleep quality and duration with health-related quality of life (HRQOL) in older Chinese.
Methods:
We analyzed community-based cross-sectional data of 5,539 individuals aged 60 years and older in the Weitang Geriatric Disease Study. Information of sleep quality and duration were self-reported through participants' responses to predefined questions; HRQOL data were collected by using the European Quality of Life-5 Dimensions (EQ-5D). We estimated the associations of sleep quality and duration with the EQ-5D index and visual analog scale (VAS) scores using linear regression models. The associations between sleep quality and duration and EQ-5D–detected health problems were modeled using logistic regression.
Results:
In multiple linear models adjusting sociodemographic factors, health conditions, and lifestyle habits, both EQ-5D index and VAS scores declined with deterioration of sleep quality. The coefficients for poor and intermediate sleep quality were −0.053 (95% confidence interval [CI]:−0.065, −0.042) and −0.022 (95% CI: −0.030, −0.013), respectively, in relation to EQ-5D index score. They were −5.2 (95% CI: −6.7, −2.4) and − 3.8 (95% CI: −4.9, −2.7) in modeling the EQ-5D VAS score. HRQOL declined as sleep duration decreased below 7.01 hours or exceeded 8.01 hours, though most of the associations did not reach statistical significance. In multiple logistic models, poor sleep quality was associated with problems of mobility, pain/discomfort, and anxiety/ depression; short sleep duration was associated with mobility problems.
Conclusions:
Poor sleep quality and extreme sleep durations appeared to be negatively associated with HRQOL in older Chinese adults.
Citation:
Pan CW, Cong X, Zhou HJ, Li J, Sun HP, Xu Y, Wang P. Self-reported sleep quality, duration, and health-related quality of life in older Chinese: evidence from a rural town in Suzhou, China. J Clin Sleep Med. 2017;13(8):967–974.
Keywords: China, EQ-5D, health-related quality of life, older adults, sleep duration, sleep quality
INTRODUCTION
Sleep disturbances such as insomnia, sleep apnea, and restless legs syndrome are increasingly common health issues when people grow old.1–4 Extensive evidence has shown that sleep disturbance is an independent risk factor of increased overall mortality,5 increased psychiatric and medical morbidity,6,7 decreased physical and cognitive function,8,9 and decreased health-related quality of life (HRQOL)10,11 among older adults.
Sleep disturbances generally manifest declined sleep quality and abnormal sleep duration. Sleep quality and duration are interlinked concepts12 and can be assessed objectively or subjectively. Empirical evidence has shown that subjective assessment of sleep is more sensitive to difference in sleep patterns13 and had stronger correlation with clinical conditions14 (eg, depression) than objective measurements such as polysomnography and actigraphy.15
It has been well documented that self-reported poor sleep quality or extreme sleep durations (either too short or too long) are related to a wide spectrum of health outcomes of older people, including cognitive impairment, depressive symptoms, physical functioning, mobility disorder, pain, and vitality.14,16–20 As a result, the multidimensional health outcome measure HRQOL was clinically required and has been adopted to holistically assess the sleep-health relationships in the population.21,22 One study in Spain found that extreme sleep durations were an indicator of worse HRQOL in a representative cohort of 3,834 older adults.21 Another Hong Kong (HK) study of 310 older community-dwelling adults showed that poor sleep quality and short sleep duration were negatively associated with HRQOL.22
BRIEF SUMMARY
Current Knowledge/Study Rationale: To date, only two studies have assessed the sleep-HRQOL relationships in an older population. More investigations are needed to understand the nature of this association. The current study is aimed to explore the cross-sectional associations of sleep quality and duration with HRQOL in older Chinese based on data from a large community-based survey.
Study Impact: We found that self-reported poor sleep quality and extreme sleep durations were associated with worse HRQOL among older community-dwelling Chinese. Given the ever-growing aging population in China, sleep quality/duration thus should be taken into consideration as important factors when inquiring about HRQOL of older Chinese.
Although the two studies have contributed to the understanding of the sleep-health relationship in older adults, there are some issues that have not been fully addressed by these two studies. The Spanish study did not measure sleep quality, a known significant factor without which the effect of sleep duration on HRQOL could be overestimated or even biased; the HK sample seemed to have an overpresentation of women (84.4%). Additionally, arbitrary dichotomization of sleep duration in this study may pose a weakness to evaluate its association with HRQOL. In mainland China, a nationwide prospective cohort study of adults aged 65 years and older provided similar results by showing that poor sleep quality and extreme sleep durations were associated with increased risk of death and decreased odds of being in a healthy state.23 However, researchers used the cumulative health deficit index, which is not a measure of HRQOL and thus did not reflect individuals' perceptions on their overall health status and specific health domains. Hence, we design this study aiming to investigate the associations of self-reported sleep quality and duration with HRQOL in older Chinese from a large, community-based cross-sectional survey.
METHODS
Study Population
The Weitang Geriatric Diseases Study is a community-based survey conducted in Weitang town, a rural area of Suzhou, which is a metropolis located in East China. The survey aimed to estimate the patterns, risk factors, and burden of prevalent health conditions of community-dwelling people aged 60 years or older. The study invited 6,030 residents aged 60 years or older who were initially detected according to official records. Before the study recruitment, each family received an invitation letter explaining the nature of the study. After applying the following exclusion criteria—(1) younger than 60 years; (2) moved away from the residing address; (3) residence in Weitang shorter than 6 months; and (4) death—a total of 5,613 people were considered eligible. Subsequently 2,872 women and 2,683 men were interviewed face-to-face by trained interviewers from August 2014 to February 2015.
The Weitang Geriatric Diseases Study was conducted in conformity with the tenets of the Helsinki Declaration and approved by the Institutional Review Board of Soochow University. All participants gave informed consent in writing at the recruitment.
Sleep Variables
Several questions were designed to assess participants' sleep status. First, participants were asked to rate their sleep quality by three severity categories (good, intermediate, and poor). Accordingly, a categorical variable was created to represent different sleep quality (good versus intermediate versus poor). Second, sleep duration at night was inquired with the question: “What time do you usually go to sleep at night and wake up in the morning?” Third, daytime napping was queried through the question: “Do you habitually take a nap? If yes, for how many hours and minutes?” The sum of sleep time at night and during napping gave the measure of 24-hour sleep duration. Sleep duration was categorized into 6 levels: ≤ 6, 6.01–7, 7.01– 8, 8.01–9, 9.01–10, and > 10 hours with the category 7.01–8 being defined as the reference group for comparison. Participants who slept too short (< 3 hours, n = 8) or too long (> 15 hours, n = 8) were excluded.
Health-Related Quality of Life Measure
The European Quality of Life-5 Dimensions questionnaire (EQ-5D),24 one of the most widely used generic health status instruments,25 was used to assess respondents' HRQOL. EQ-5D consists of two parts. The first part is a health state classification system defining health status in five dimensions: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. The respondent is required to choose one of three alternatives (ie, “no problem” [level 1], “some problem” [level 2], and “extreme problems” [level 3]) for the five dimensions each that best describes his/her health status on the day of interview. Responses to the dimensions collectively form a multiattribute health state that can be assigned a utility score (ie, EQ-5D index score) to indicate the value of the health state to Chinese general population.26 The index score ranges from −0.149 (worst health state) to 1.0 (full health), with a higher score indicating higher utility or better HRQOL.26 The second part is a visual analog scale (VAS), which is a vertical 0 to 100 point rating scale, for respondents to rate their overall health. The best and worst health states carry a score of 100 and 0, respectively. The EQ-5D has showed satisfactory validity and reliability in both general and patient populations in mainland China.27–30
Assessment of Covariates
Height without shoes was measured in centimeters using a wall-mounted measurement tape while weight after removing heavy clothing was measured in kilograms using a digital scale. Systolic and diastolic blood pressure and pulse rate were recorded using the automated blood pressure monitor (Dinamap model Pro Series DP110X-RW, 100V2; GE Medical Systems Information Technologies, Inc., Milwaukee, Wisconsin, United States).
The survey collected information about respondents' sociodemographic characteristics (ie, age, sex, education level, working status, marriage status, dwelling space, and monthly income), lifestyle habits (ie, smoking, alcohol use, dietary, tea consumption, outdoor activities), and health conditions.
A total of eight health conditions were included in the analysis (ie, obesity, hypertension, hyperlipidemia, diabetes, history of heart disease, history of stroke, cataracts, and cognitive impairment). We defined obesity as body mass index of 30 kg/m2 or higher, hypertension as either systolic/diastolic blood pressure ≥ 140/90 mmHg or use of antihypertensive medications, hyperlipidemia as either a total cholesterol level ≥ 6.2 mmol/L or use of lipid-lowering drugs, diabetes as either fasting blood-glucose ≥ 7.0 mmol/L or use of diabetic medications, and medical history of heart disease and stroke as self-reported physician diagnosis. Cognitive function was assessed by the Abbreviated Mental Test, which is defined as a score of 6 or less according to the clinical recommended value.31 Age-related cataract was graded clinically according to the Lens Opacities Classification System III.32
Statistical Analysis
The characteristics of participants were summarized in percentage for categorical variables and mean ± standard deviation for numerical variables. The differences in characteristics according to sleep quality and duration were analyzed using the chi-square test for categorical variables and the analysis of variance for continuous variables.
To assess the associations between perceived sleep quality and HRQOL, a series of multiple linear regression models were fitted for the EQ-5D scores (both index and VAS scores) controlling for measured covariates. Three types of models with increasing number of variables were constructed. The first model (model 1) adjusted for sociodemographic characteristics only: age, sex, education level (no formal education versus formal education), living with a spouse (with versus without), working status (working versus retired), dwelling space (≤ 60 m2 versus 61–120 m2 versus > 120 m2), and monthly income (≤ 1000 Chinese Yuan [CNY] versus 1001– 3000 CNY versus > 3000 CNY). The second model (model 2) further adjusted for lifestyle parameters: smoking (never versus former versus current), alcohol consumption (never versus former versus current), dietary (normal versus vegetarian), habitual tea consumption (nonhabitual versus habitual) and outdoor activities (with versus without). The third model (model 3) included all covariates in model 2 plus health conditions (presence versus absence): obesity, hypertension, hyperlipidemia, diabetes, cataract, history of heart disease, and history of stroke. Because the EQ-5D index and VAS scores followed skewed distributions, the coefficients were estimated using statistical procedures for robust standard error. Likewise, the relationships of sleep duration with EQ-5D scores were analyzed by repeating multiple linear models as previously described.
Multiple logistic regression was used to model the associations of sleep quality and duration with self-reported EQ-5D health problems. In the analysis, a binary variable (with problems or without problems) was created to indicate the existence of any health problem in each EQ-5D dimension, and was analyzed as dependent variable in separate logistic models. All covariates in model 3 were included in the logistic models.
As relationships of sleep duration and quality with HRQOL may be systematically different between males and females,21 we tested the modifying effect of sex on these associations. An F test of variance was adopted to compare model 3 with interaction terms (sex × sleep quality or duration) with the same model without such terms.
All analyses were performed using SAS (version 9.3, 2011, SAS Inc., Cary, North Carolina, United States) at a significance level of .05.
RESULTS
Overall, the participants reported good HRQOL with a mean EQ-5D index score of 0.954 ± 0.081 and a mean VAS score of 79.2 ± 11.8. Also, most participants rated their sleep quality as good (77.3%). The average sleep duration per 24 hours and per night were 8.98 ± 1.53 and 8.74 ± 1.47 hours, respectively; 23.1% of participants had napping habits with a mean napping time of 1.06 hours.
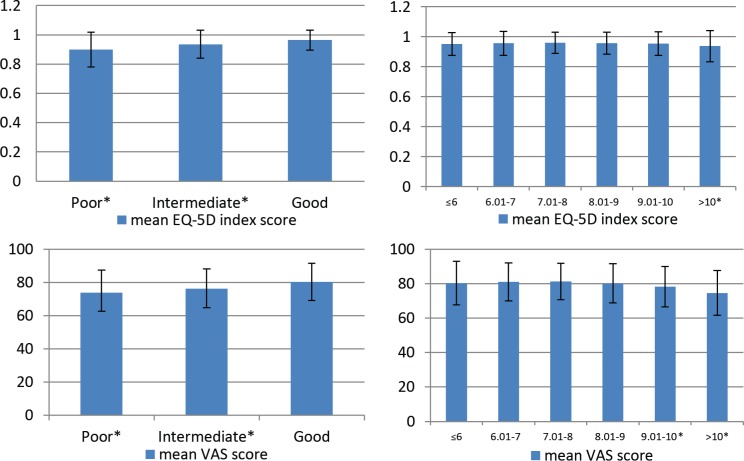
The mean EQ-5D index and VAS scores for older adults who rated themselves as having good sleep quality were higher than those with poor or intermediate sleep quality, and the differences were statistically significant (Table 1). With regard to sleep duration, people who slept 7 to 8 hours per 24-hour period achieved higher EQ-5D scores than those with either shorter (< 7 hours) or longer (> 8 hours) sleep duration (Figure 1). The comparison between categories 7.01–8 hours and > 10 hours reached statistical significance (Table 1).
Table 1.
Characteristics of study participants according to sleep quality and duration.
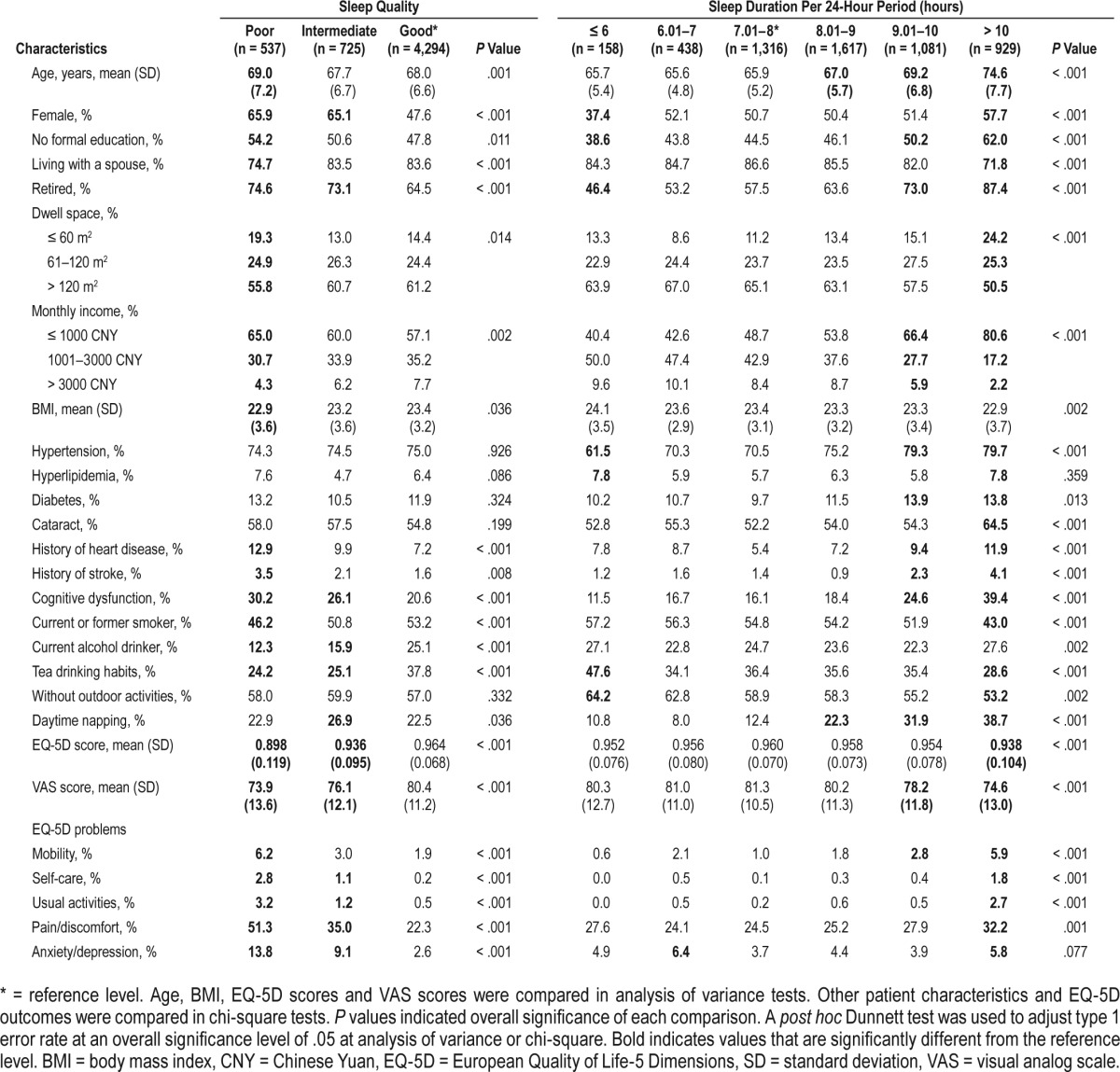
Figure 1. Mean European Quality of Life-5 Dimensions index and visual analog scale scores and their standard deviations according to sleep quality and duration.
Sleep quality was classified into 3 levels: good sleep quality, intermediate sleep quality, and poor sleep quality. 24-hour sleep duration (including napping) was categorized into 6 levels: ≤ 6, 6.01–7, 7.01–8, 8.01–9, 9.01–10, and > 10 hours. * = the level of variable is significantly different from the reference level, which was good sleep quality or sleep duration between 7.01–8 hours. EQ-5D = European Quality of Life-5 Dimensions, VAS = visual analogue scale.
Characteristics of the sample are presented according to sleep quality and duration in Table 1. The percentage of female sex, retirement, low socioeconomic status (eg, smaller dwelling space), the prevalence of history of heart disease and stroke, and cognitive dysfunction were significantly higher among those with poor sleep quality. Conversely, an older adult with good or intermediate sleep quality was more likely to have higher body mass index, tea consumption habits, ever have smoked, and current drinking habits. For sleep duration, older adults who had 7.01–8 hours of sleep duration per 24-hour period were less likely to have chronic conditions and drinking habits, compared with those who had extreme sleep durations.
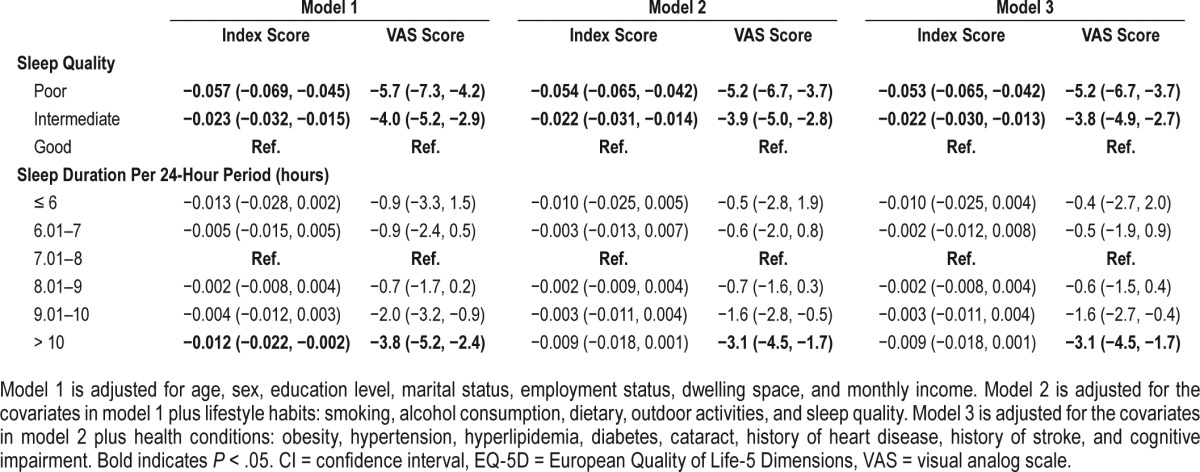
The associations between sleep quality, duration, and HRQOL after controlling for covariates are displayed in Table 2. In general, both EQ-5D index and VAS scores declined when sleep quality worsened from good to poor, though the decline of HRQOL slightly attenuated when more covariates were adjusted. According to the full model of the EQ-5D index score encompassing all covariates (model 3), the coefficients for poor and intermediate sleep quality were −0.053 (95% confidence interval [CI]: −0.065, −0.042) and −0.022 (95% CI: −0.030, −0.013), respectively, when compared to the reference category of good sleep quality. Similarly, the corresponding coefficients were −5.2 (95% CI: −6.7, −2.4), −3.8 (95% CI: −4.9, −2.7) for the EQ-5D VAS score according to the full model. There seemed to be a curvilinear association between sleep duration and HRQOL outcomes. Namely, the coefficients of strata for sleep duration grew negatively when sleep duration declined or increased from the 7.01- to 8-hour category. Although most coefficients did not reach statistical significance, the reduction in VAS score for sleeping more than 10 hours was statistically significant.
Table 2.
Association between sleep quality, duration and the European Quality of Life-5 Dimensions index and visual analog scale scores (linear regression analysis).
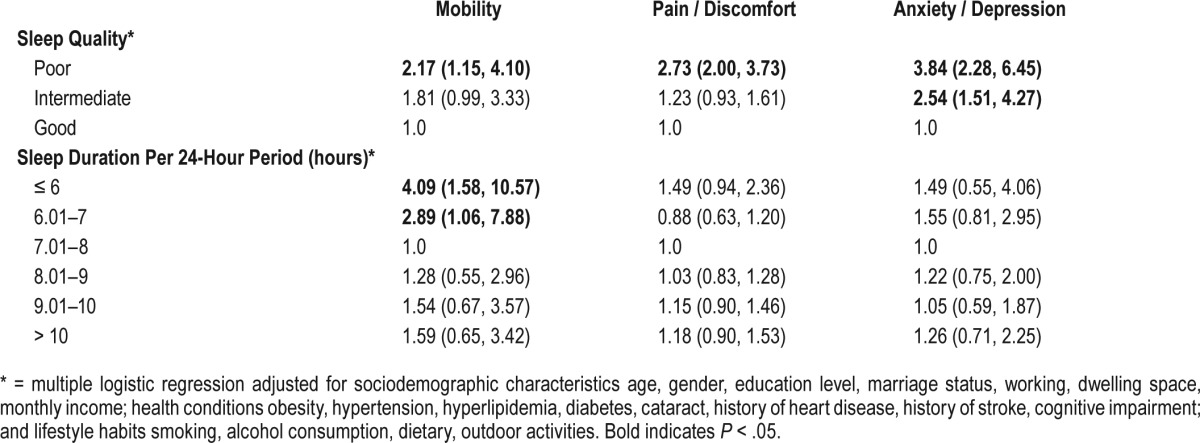
The relationships between sleep quality, duration, and the risk of experiencing EQ-5D problems in mobility, pain/discomfort, and anxiety/depression are shown in Table 3. Problems with self-care and performing usual activities were not analyzed because of their low occurrence (0.54% for self-care and 0.83% for usual activities). Poor sleep quality was significantly associated with self-reported problems in the three dimensions, whereas intermediate sleep quality was related to problems in anxiety/depression. Sleep duration was not significantly associated with self-reported problems in pain/ discomfort anxiety/depression in multiple logistic models. But sleeping shorter than 7 hours was found to be associated with problems with mobility (ie, the shorter the sleep duration, the higher risk of mobility problems).
Table 3.
Odds ratios (95% confidence interval) of sleep quality and duration in predicting European Quality of Life-5 Dimensions health problems.
There was no significant sex difference in associations of sleep quality and duration with HRQOL according to the F test of variance. The interaction terms were not significant in the models yet (P > .05 for both). The coefficients estimated by model 3 for women and men were also similar (see Appendix 1 in the supplemental material).
DISCUSSION
In a sample of Chinese older adults dwelling in communities, we found strong associations between sleep quality and HRQOL. People who perceived themselves with poor sleep quality were associated with worse HRQOL. The associations between sleep duration and HRQOL were also indicated, though not as significant as those for sleep quality. To the best of our knowledge, this was the first study assessing the sleep-HRQOL association in older adults in mainland China. Our study simultaneously examined five EQ-5D dimensions whereas other similar epidemiological studies mostly assessed one health dimension at a time. Additionally, the EQ-5D index score estimated can be used to calculate quality-adjusted life-years in economic evaluations on the effect of sleep problems on population health. Hence, our study not only conformed to prior findings, but also expanded the knowledge of the sleep-health relationship.
In our study, most participants rated their HRQOL favorably. This is consistent with previous studies in mainland China.27–30 Two facts may account for this finding. First, the survey participants lived a normal life at home, which implies better HRQOL than those who live in medical institutions for professional care. Second, the EQ-5D is constrained by significant ceiling effects in measuring HRQOL in the general population.27,29
We also found a high prevalence of good sleep quality in our sample, which is supported by prior studies in mainland China.23,33 This can be explained by reports suggesting that most generally healthy older adults experience satisfactory sleep quality.34 The contrasting finding has been reported by the HK study, which found a prevalence of only 22% good sleep quality. This was partially due to the oversampling of women who appear more likely to report experiences of sleep disturbances compared to men. Indeed, even in our study, women accounted for a bigger proportion (65.9%) of participants who reported poor sleep quality. The average duration of sleep in our study was longer than that reported previously in mainland China,23 HK,22 and Taiwan.35 This discrepancy may be attributed to lifestyle of rural population who tend to sleep longer than urban residents.23
The associations between sleep quality, duration and HRQOL discovered in our study are consistent with previous findings. First, sleep deprivation (ie, poor quality or short duration) has been found to be negatively associated with HRQOL in HK22 and the Spain.21 Second, health problems in HRQOL dimensions such as physical functioning,16,18,19 mental health,14,17 and pain18,20 are correlated with extreme sleep duration and poor sleep quality, which may also have negative effect on self-rated health.36 Third, sleep problems (eg, insomnia)10,37 or sleep complaints38 that normally accompany sleep disturbances are reported to have a negative relationship with HRQOL. Our findings that sleep quality has stronger association with HRQOL than sleep duration also align with the existing evidence.12,22
The mechanisms for negative effects of extreme sleep durations and poor sleep quality on HRQOL have been explored. First, fatigue resulting from poor sleep quality or long sleep duration39 is able to influence people's subjective well-being and HRQOL. Second, sleep restriction leads to a series of adverse neurobehavioral consequences and physiological changes such as lapses of attention, depressive mood, reduced glucose tolerance, and activation of the sympathetic nervous system.40 These sleep-induced changes may manifest as reduced daily function, which is reflected by HRQOL measure. With that said, it should be borne in mind that our findings based on cross-sectional data were limited to confirm a cause-effect relationship between sleep disturbance and HRQOL. Indeed, evidence has suggested a reciprocal relationship between sleep and health,41 and even an inverse cause-effect relationship of sleep to HRQOL.42
However, our findings were slightly different from those of the Spanish study. First, our study found that extremely long sleep duration was significantly correlated with lower EQVAS score measuring overall health, not just the dimension of physical role as reported by the Spanish study. The inconsistency may be linked to differences in sleep patterns between Western and Asian populations,43,44 and reasons for either short or long sleep duration. Because both studies did not collect relevant information, future studies are warranted to address this issue. Second, our study did not find the modifying effect of sex on associations between sleep and HRQOL as did the Spanish study. The inconsistency may be partially attributed to HRQOL instruments chosen. The Spanish study adopted a comprehensive HRQOL instrument, Medical Outcomes Study 36-Item Short Form (SF-36), comprising 36 questions.45 The utility score46 generated from SF-36 scores was found to be more discriminative than the EQ-5D.47,48 Nevertheless, there was no evidence showing that the SF-36 derived utility score was better than the EQ-5D in measuring HRQOL.
It should be noted that sleep quality of our sample was assessed with a single question rather than the validated instrument Pittsburgh Sleep Quality Index (PSQI) in other studies.14,17,20,22 This was determined by the education level of study participants of whom nearly half did not receive formal education. A pilot study with a small sample showed that our participants had difficulties in understanding or completing PSQI in a face-to-face interview setting. So we were concerned with the testability of PSQI and decided to use simple questions considering trade-off between validity and academic authority. Actually, self-reported sleep quality is acceptable and has been used in peer studies.16,18,33,39 Nevertheless, future studies using the PSQI are still warranted.
It should also be noted that the prevalence of health conditions was normally higher for poorer sleep quality and extreme sleep durations (Table 1). Hence, we conducted separate multiple logistic regression analyses and found that both sleep quality and duration were significant predictors for several conditions (Appendix 2 in the supplemental material). Future comprehensive analyses and studies are warranted to further explore the detected associations.
The study had several limitations. First, because of the nature of cross-sectional design, our study was unable to establish a causal relationship between perceived sleep quality, duration, and HRQOL. Future studies adopting a longitudinal design are warranted. Second, the information on sleep quality and duration was collected in a self-reported approach, which may be overestimated as evidence has shown.14 Third, we only examined basic sleep patterns. Detailed questions inquiring about a variety of common sleep problems in older adults, the reasons for poor sleep quality and extreme sleep durations, and the use of sleep medication, which could influence HRQOL differently, would be informative. Fourth, results from our specific sample of Weitang town residents may not be generalizable to a larger population base of older Chinese adults, such as those living in a city or medical institutions.
In conclusion, self-perceived poor sleep quality and extreme sleep durations are associated with worse HRQOL in older Chinese adults. As China faces challenges from its ever-growing aging population, it has become an important goal to maintain favorable HRQOL or relieve HRQOL deterioration of older adults for policy makers in health care. Therefore, sleep quality/duration naturally should be viewed as important issues to address in China. However, our findings should be interpreted with caution because of the lack of follow-up and the minimalistic manner in which sleep patterns were assesssed.
DISCLOSURE STATEMENT
This study was funded by Introduction of talent to start funding of Fudan University, China (NO. JIF201005 and SXF201002). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The authors report no conflicts of interest.
ACKNOWLEDGMENTS
Author contributions: W.P. had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. W.P. and P.C. designed the study. W.P. obtained funding. P.C. collected data for the study. W.P. did statistical analysis and prepared all tables. W.P. and C.X. wrote the main manuscript text. All authors reviewed the manuscript.
ABBREVIATIONS
- EQ-5D
European Quality of Life-5 Dimensions
- HRQOL
health-related quality of life
- HK
Hong Kong
- PSQI
Pittsburgh Sleep Quality Index
- SD
standard deviation
- VAS
visual analog scale
REFERENCES
- 1.LeBlanc M, Merette C, Savard J, Ivers H, Baillargeon L, Morin CM. Incidence and risk factors of insomnia in a population-based sample. Sleep. 2009;32(8):1027–1037. doi: 10.1093/sleep/32.8.1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liu X, Liu L. Sleep habits and insomnia in a sample of elderly persons in China. Sleep. 2005;28(12):1579–1587. [PubMed] [Google Scholar]
- 3.Allen RP, Walters AS, Montplaisir J, et al. Restless legs syndrome prevalence and impact: REST general population study. Arch Intern Med. 2005;165(11):1286–1292. doi: 10.1001/archinte.165.11.1286. [DOI] [PubMed] [Google Scholar]
- 4.Chen YL, Weng SF, Shen YC, et al. Obstructive sleep apnea and risk of osteoporosis: a population-based cohort study in Taiwan. J Clin Endocrinol Metab. 2014;99(7):2441–2447. doi: 10.1210/jc.2014-1718. [DOI] [PubMed] [Google Scholar]
- 5.Dew MA, Hoch CC, Buysse DJ, et al. Healthy older adults' sleep predicts all-cause mortality at 4 to 19 years of follow-up. Psychosom Med. 2003;65(1):63–73. doi: 10.1097/01.psy.0000039756.23250.7c. [DOI] [PubMed] [Google Scholar]
- 6.Ford DE, Kanerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? JAMA. 1989;262(11):1479–1484. doi: 10.1001/jama.262.11.1479. [DOI] [PubMed] [Google Scholar]
- 7.Katz DA, McHorney CA. Clinical correlates of insomnia in patients with chronic illness. Arch Intern Med. 1998;158(10):1099–1107. doi: 10.1001/archinte.158.10.1099. [DOI] [PubMed] [Google Scholar]
- 8.Ohayon MM, Vecchierini MF. Normative sleep data, cognitive function and daily living activities in older adults in the community. Sleep. 2005;28(8):981–989. [PubMed] [Google Scholar]
- 9.Dam TT, Ewing S, Ancoli-Israel S, et al. Association between sleep and physical function in older men: the Osteoporotic Fractures in Men Sleep Study. J Am Geriatr Soc. 2008;56(9):1665–1673. doi: 10.1111/j.1532-5415.2008.01846.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zammit GK, Weiner J, Damato N, Sillup GP, McMillan CA. Quality of life in people with insomnia. Sleep. 1999;22(Suppl 2):S379–S385. [PubMed] [Google Scholar]
- 11.Lee M, Choh AC, Demerath EW, et al. Sleep disturbance in relation to health-related quality of life in adults: the Fels Longitudinal Study. J Nutr Health Aging. 2009;13(6):576–583. doi: 10.1007/s12603-009-0110-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pilcher JJ, Ginter DR, Sadowsky B. Sleep quality versus quantity: relationships between sleep and measures of health, well-being and sleepiness in college students. J Psychosom Res. 1997;42(6):583–596. doi: 10.1016/s0022-3999(97)00004-4. [DOI] [PubMed] [Google Scholar]
- 13.Palermo TM, Toliver-Sokol M, Fonareva I, Koh JL. Objective and subjective assessment of sleep in adolescents with chronic pain compared to healthy adolescents. Clin J Pain. 2007;23(9):812–820. doi: 10.1097/AJP.0b013e318156ca63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Paudel ML, Taylor BC, Diem SJ, et al. Association between depressive symptoms and sleep disturbances in community-dwelling older men. J Am Geriatr Soc. 2008;56(7):1228–1235. doi: 10.1111/j.1532-5415.2008.01753.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Baker FC, Maloney S, Driver HS. A comparison of subjective estimates of sleep with objective polysomnographic data in healthy men and women. J Psychosom Res. 1999;47(4):335–341. doi: 10.1016/s0022-3999(99)00017-3. [DOI] [PubMed] [Google Scholar]
- 16.Malinowska KB, Okura M, Oqita M, et al. Effect of self-reported quality of sleep on mobility in older adults. Geriatr Gerontol Int. 2016;16(2):266–271. doi: 10.1111/ggi.12468. [DOI] [PubMed] [Google Scholar]
- 17.Chang KJ, Son SJ, Lee Y. Perceived sleep quality is associated with depression in a Korean elderly population. Arch Gerontol Geriatr. 2014;59(2):468–473. doi: 10.1016/j.archger.2014.04.007. [DOI] [PubMed] [Google Scholar]
- 18.Sampaio RA, Sewo Sampaio PY, Yamada M, Tsuboyama T, Arai H. Self-reported quality of sleep is associated with bodily pain, vitality and cognitive impairment in Japanese older adults. Geriatr Gerontol Int. 2014;14(3):628–635. doi: 10.1111/ggi.12149. [DOI] [PubMed] [Google Scholar]
- 19.Sapira AP, Covinsky K, Rebok GW, et al. Poor sleep quality and functional decline in older women. J Am Geriatr Soc. 2012;60(6):1092–1098. doi: 10.1111/j.1532-5415.2012.03968.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Park JH, Yoo MS, Bae SH. Prevalence and predictors of poor sleep quality in Korean older adults. Int J Nurs Pract. 2013;19(2):116–123. doi: 10.1111/ijn.12047. [DOI] [PubMed] [Google Scholar]
- 21.Faubel R, Lopez-Garcia E, Guallar-Castillón P, et al. Sleep duration and health-related quality of life among older adults: a population-based cohort in Spain. Sleep. 2009;32(8):1059–1068. [PMC free article] [PubMed] [Google Scholar]
- 22.Lo CM, Lee PH. Prevalence and impacts of poor sleep on quality of life and associated factors of good sleepers in a sample of older Chinese adults. Health Qual Life Outcomes. 2012;10:72. doi: 10.1186/1477-7525-10-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gu D, Sautter J, Pipkin R, Zeng Y. Sociodemographic and health correlates of sleep quality and duration among very old Chinese. Sleep. 2010;33(5):601–610. doi: 10.1093/sleep/33.5.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brooks R. EuroQol: the current state of play. Health Policy. 1996;37(1):1303–1307. doi: 10.1016/0168-8510(96)00822-6. [DOI] [PubMed] [Google Scholar]
- 25.Gusi N, Olivares PR, Rajendram R. The EQ-5D Health-Related Quality of Life Questionnaire. In: Preedy VR, Watson RR, editors. Handbook of Disease Burdens and Quality of Life Measures. New York, NY: Springer; 2010. pp. 87–99. [Google Scholar]
- 26.Liu G, Wu H, Li M, et al. Chinese time trade-off values for EQ-5D health states. Value Health. 2014;17(5):597–603. doi: 10.1016/j.jval.2014.05.007. [DOI] [PubMed] [Google Scholar]
- 27.Wang H, Kindig DA, Mullahy J. Variation in Chinese population health related quality of life: results from a EuroQol study in Beijing, China. Qual Life Res. 2005;14(1):119–132. doi: 10.1007/s11136-004-0612-6. [DOI] [PubMed] [Google Scholar]
- 28.Zhao FL, Yue M, Yang H, Wang T, Wu JH, Li SC. Validation and comparison of EuroQol and short form 6D in chronic prostatitis patients. Value Health. 2010;13(5):649–656. doi: 10.1111/j.1524-4733.2010.00728.x. [DOI] [PubMed] [Google Scholar]
- 29.Wang HM, Patrick DL, Edwards TC, Skalicky AM, Zeng HY, Gu WW. Validation of the EQ-5D in a general population sample in urban China. Qual Life Res. 2012;21(1):155–160. doi: 10.1007/s11136-011-9915-6. [DOI] [PubMed] [Google Scholar]
- 30.Wu J, Han Y, Zhao FL, Zhou J, Chen Z, Sun H. Validation and comparison of EuroQol-5 dimension (EQ-5D) and short form-6 (SF-6D) among stable angina patients. Health Qual Life Outcomes. 2014;12:156. doi: 10.1186/s12955-014-0156-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sahadevan S, Tan JL, Tan T, Tan S. Cognitive testing of elderly Chinese people in Singapore: influence of education and age on normative scores. Age Ageing. 1997;26(6):481–486. doi: 10.1093/ageing/26.6.481. [DOI] [PubMed] [Google Scholar]
- 32.Chylack LT, Jr., Wolfe JK, Singer DM, et al. The Lens Opacities Classification System III. The Longitudinal Study of Cataract Study Group. Arch Ophthalmol. 1993;111(6):831–836. doi: 10.1001/archopht.1993.01090060119035. [DOI] [PubMed] [Google Scholar]
- 33.Gildner TE, Liebert MA, Kowal P, Chatterji S, Snodgrass JJ. Associations between sleep duration, sleep quality, and cognitive test performance among older adults from six middle income countries: results from the Study on Global Ageing and Adult Health (SAGE) J Clin Sleep Med. 2014;10(6):613–621. doi: 10.5664/jcsm.3782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Driscoll HC, Serody L, Patrick S, et al. Sleeping well, aging well: a descriptive and cross-sectional study of sleep in “successful agers” 75 and older. Am J Geriatr Psychiatry. 2008;16(1):74–82. doi: 10.1097/JGP.0b013e3181557b69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chen YY, Kawachi I, Subramanian SV, Acevedo-Garcia D, Lee YJ. Can social factors explain sex differences in insomnia? Findings from a national survey in Taiwan. J Epidemiol Community Health. 2005;59(6):488–494. doi: 10.1136/jech.2004.020511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Frange C, de Queiroz SS, da Silva Prado JM, Tufik S, de Mello MT. The impact of sleep duration on self-rated health. Sleep Sci. 2014;7(2):107–113. doi: 10.1016/j.slsci.2014.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schubert CR, Cruickshanks KJ, Dalton DS, Klein BE, Klein R, Nondahl DM. Prevalence of sleep problems and quality of life in an older population. Sleep. 2002;25(8):889–893. [PubMed] [Google Scholar]
- 38.Fagerström C, Hellström A. Sleep complaints and their association with comorbidity and health-related quality of life in an older population in Sweden. Aging Ment Health. 2011;15(2):204–213. doi: 10.1080/13607863.2010.513039. [DOI] [PubMed] [Google Scholar]
- 39.Mesas AE, López-García E, León-Muñoz LM, Graciani A, Guallar-Castillón P, Rodríguez-Artalejo F. The association between habitual sleep duration and sleep quality in older adults according to health status. Age Ageing. 2011;40(3):318–323. doi: 10.1093/ageing/afr004. [DOI] [PubMed] [Google Scholar]
- 40.Banks S, Dinges DF. Behavioral and physiological consequences of sleep restriction. J Clin Sleep Med. 2007;3(5):519–528. [PMC free article] [PubMed] [Google Scholar]
- 41.Qiu L, Sautter J, Liu YZ, Gu D. Age and gender differences in linkages of sleep with subsequent mortality and health among very old Chinese. Sleep Med. 2011;12(10):1008–1017. doi: 10.1016/j.sleep.2011.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Patel SR, Malhotra A, Gottlieb DJ, White DP, Hu FB. Correlates of long sleep duration. Sleep. 2006;29(7):881–889. doi: 10.1093/sleep/29.7.881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Poland RE, Rao U, Lutchmansingh P, et al. REM sleep in depression is influenced by ethnicity. Psychiatry Res. 1999;88(2):95–105. doi: 10.1016/s0165-1781(99)00080-3. [DOI] [PubMed] [Google Scholar]
- 44.Hale L, Do P. Racial differences in self-reports of sleep duration in a population-based study. Sleep. 2007;30(9):1096–1103. doi: 10.1093/sleep/30.9.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ware JE, Snow KK, Kosinski M, et al. SF-36 Health Survey: Manual & Interpretation Guide. Boston, MA: The Health Institute, New England Medical Centre; 1993. [Google Scholar]
- 46.Brazier JE, Roberts J, Deverill MD. The estimation of a preference-based measure of health from the SF-36. J Health Econ. 2002;21(2):271–292. doi: 10.1016/s0167-6296(01)00130-8. [DOI] [PubMed] [Google Scholar]
- 47.Petrou S, Hockley C. An investigation into the empirical validity of the EQ-5D and SF-6D based on hypothetical preferences in a general population. Health Econ. 2005;14(11):1169–1189. doi: 10.1002/hec.1006. [DOI] [PubMed] [Google Scholar]
- 48.Macran S, Weatherly H, Kind P. Measuring population health? A comparison of three generic health status measures. Med Care. 2003;41(2):218–231. doi: 10.1097/01.MLR.0000044901.57067.19. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.