Abstract
Study Objectives:
Insomnia is a widespread issue among United States adults and rates of insomnia among veterans are even higher than the general population. Prior research examining primary care provider (PCP) perspectives on insomnia treatment found that: sleep hygiene and pharmacotherapy are the primary treatments offered; PCPs tend to focus on perceived causes of insomnia rather than the insomnia itself; and neither patients nor providers are satisfied with insomnia treatment options. Although insomnia complaints are typically first reported to primary care providers, little research has focused on perspectives regarding insomnia treatment among PCPs working in the largest integrated health care system in the United States—the Veterans Affairs (VA) health care system. This study was conducted to examine VA PCP perceptions of the availability of insomnia treatments, identify specific strategies offered by PCPs, and examine perceptions regarding the importance of treating insomnia and the role of comorbid conditions.
Methods:
A survey was conducted within the VA health care system. Primary care providers completed surveys electronically.
Results:
A high percentage of veterans (modal response = 20% to 39%) seen in VA primary care settings report an insomnia complaint to their provider. Almost half of respondents do not consistently document insomnia in the medical record (46% endorsed “sometimes,” “rarely,” or “never”). PCPs routinely advise sleep hygiene recommendations for insomnia (ie, avoid stimulants before bedtime [84.3%], and keep the bedroom environment quiet and dark and comfortable [68.6%]) and many are uncertain if cognitive behavioral therapy for insomnia is available at their facility (43.1%).
Conclusions:
Findings point to the need for systems-level changes within health care systems, including the adoption of evidence-based clinical practice standards for insomnia and PCP education about the processes that maintain insomnia.
Commentary:
A commentary on this article appears in this issue on page 937.
Citation:
Ulmer CS, Bosworth HB, Beckham JC, Germain A, Jeffreys AS, Edelman D, Macy S, Kirby A, Voils CI. Veterans affairs primary care provider perceptions of insomnia treatment. J Clin Sleep Med. 2017;13(8):991–999.
Keywords: insomnia, primary care, provider perspectives
INTRODUCTION
Insomnia is a widespread issue among adults in the United States. An estimated 4% to 22% of United States adults meet diagnostic criteria for insomnia,1–3 and rates of insomnia among veterans are even higher.4 More than half of veterans enrolling in Veterans Affairs (VA) health care at a large Midwestern VA facility endorsed clinically significant levels of insomnia.5 The primary care clinical setting serves as the “hub” for the treatment of insomnia. Thus, understanding primary care provider (PCP) perspectives may be most salient to efforts targeting improved insomnia treatment and management. Three prior studies have focused on PCP perspectives on insomnia treatment and revealed the following themes. First, PCPs tend to use a “stepped” treatment approach for insomnia involving sleep hygiene education followed by pharmacotherapy.6 Second, both patients and providers often view sleep disorders as relatively less important than other medical conditions.7,8 Third, insomnia is often viewed as a symptom of another medical or mental health condition rather than an independent disorder warranting separate treatment.8 Fourth, neither patients nor providers are satisfied with the range of treatment options available to them for the treatment of insomnia,6 and think that resources are inadequate for offering nonpharmacologic approaches to insomnia treatment.9 Finally, providers would like more education and training in the management of insomnia.6
BRIEF SUMMARY
Current Knowledge/Study Rationale: Prior research has not examined primary care provider (PCP) perspectives on treatment within the Veterans Affairs (VA) health care system. This study was conducted to expand the existing literature with data from the VA health care setting.
Study Impact: Despite increased availability of cognitive behavioral therapy for insomnia within the VA, this study reveals the need for additional systems-level changes. Specifically, PCP education and practice standards are needed to increase patient access to evidence-based insomnia treatments.
The primary care clinical setting presents a unique challenge for the assessment and diagnosis of sleep disorders. PCPs are responsible for the prevention and management of an array of medical and mental health conditions. Most physicians (80%) report being overextended or at full capacity,9 and this perspective is occurring in the context of an increasing number of patients presenting to primary care for sleep complaints.10,11 Thus, the PCP experience of limited resources and increasing sleep complaints among their patients sets the stage for under-diagnosis/treatment of insomnia disorder in the medical setting where patients are likely to first report their sleep difficulties.
Prior studies have not specifically examined the perspectives of PCPs working in the VA health care system, which is the largest integrated health care system in the United States. Understanding PCP perspectives in this setting is important for a number of reasons. First, the prevalence of insomnia among veterans is considerably higher than that of the average adult in the United States, and is often comorbid with mental health and medical conditions.12–14 Thus, VA PCP perspectives could differ, reflecting a need for more intensive insomnia treatments. Second, VA PCPs may have been influenced by the presence of behavioral medicine providers embedded into the VA primary care setting pursuant to integrated primary care programs. Third, more than half of physicians trained in the United States (> 65%) had VA clinical training prior to employment.15 Thus, the approach to insomnia adopted within the VA health care system is likely to inform the approach in other settings as well. Finally, the VA health care system has implemented nationwide dissemination of training in cognitive behavioral therapy for insomnia (CBT-I).16 Prior studies were not conducted in systems with this relatively greater access to CBT-I.
To our knowledge, only one published study has focused on perspectives of VA health care providers on insomnia treatment. Epstein and colleagues17 conducted surveys and interviews with both veterans and VA health care providers (not exclusively PCPs) regarding the acceptability of various insomnia treatments. Individual therapy and relaxation therapy were found to be acceptable by both veterans and providers, and veterans also endorsed pharmacotherapy as acceptable. Prior studies have not focused on VA PCPs, and have not provided insight into: provider perceptions of the availability of insomnia treatment options; what specific sleep hygiene strategies are offered by providers; provider perceptions of the relative importance of treating insomnia relative to other medical conditions; and provider perceptions of the role of comorbid conditions (eg, mental health conditions such as posttraumatic stress disorder [PTSD] and depression and medical conditions) in the treatment of insomnia.
The purpose of the current study was to expand the existing literature by examining these questions and to specifically explore the perspectives of VA PCPs on insomnia management and treatment. Although VA PCP perspectives are unlikely to differ considerably from those of non-VA PCPs on many topics, it is unclear how the aforementioned factors (ie, presence of psychologists in the primary care setting and greater access to CBT-I) might affect VA PCP perspectives on insomnia treatment specifically. As such, our analyses are considered exploratory in nature, and a priori hypotheses were not proposed.
METHODS
Setting
Participants were recruited from primary care clinics located at VA facilities in the mid-Atlantic region (VISN 6) of the VA health care system, which includes North Carolina and Virginia. Nine sites participated in the survey. VA facilities provide primary care in both hospitals and community-based outpatient clinics. Within VISN 6, VA hospitals are located in urban areas (eg, Durham, North Carolina; Asheville, North Carolina; Salem, Virginia), whereas community-based outpatient clinics are located in either urban or rural areas (Winston-Salem, North Carolina; Hickory, North Carolina). All full-time PCPs carry approximately 1,200 patients on their panels regardless of facility type or location. Within VISN 6, there are a total of 34 mental health providers who have been trained in CBT-I pursuant to the national training effort, and at least one trained provider is available at each facility surveyed. Only 4 of 9 sites surveyed had CBT-I–trained providers offering CBTI within primary care clinics.
Population
Study participants were VA primary care providers, including physicians (MDs), nurse practitioners (NPs), and physician assistants (PAs). All PCPs were eligible to participate in the survey with the exception of those who were also investigators in the Durham Center for Health Services Research in Primary Care (HSR&D) due to their involvement in survey item development and/or the possibility of prior exposure to survey topics during research talks by the first author. Standard electronic health record templates used in primary care do not include questions regarding sleep. Thus, inquiry about a patient's sleep quality or quantity are left to the discretion of each provider.
Procedures
Before PCP recruitment began, authorization to participate in the survey was sought from the ambulatory care service associate chief of staff within each VA VISN 6 facility. Nine of 10 VA medical facilities provided approval for their staff to participate in the survey. Recruitment emails were then sent to PCPs at facilities whose chief of staff provided approval for their participation. Recruitment emails were sent to 269 MDs and 112 midlevel providers (either NP or PA). This email message informed PCPs that the survey was focused on insomnia treatment practices. The email message also contained a hyperlink to the survey and a statement informing respondents that by clicking on the link, they were providing their consent to participate. To ensure the anonymity of respondents, research staff did not track who had/had not completed the survey. Therefore, reminder emails were again sent to all PCPs at about 1 and 2 weeks after the initial recruitment email to prompt those not yet completing the survey; a final reminder email was sent at about 4 weeks after the initial recruitment email. The survey ended on February 23, 2015. Approval for all studies procedures previously outlined was obtained by the Durham VA Institutional Review Board prior to initiating the study.
Survey Development
The survey was developed using an iterative process of item generation, review, and feedback from VA Behavioral Sleep Medicine providers and coauthors, and item revision. Durham VA PCPs/HSR&D investigators also provided item review and feedback, which led to item revision. As noted previously, PCPs involved in survey development were not eligible for recruitment into the study. The survey was designed to assess topics that are currently missing from the literature and/or those that have not been evaluated in the VA health care system. Specifically, the survey focused on the following key domains of insomnia management: estimates of percentage of veterans reporting insomnia complaint; specific behavioral approaches recommended; familiarity with CBT-I; perceptions of available treatment options; documentation of insomnia in the medical record; perceptions of the cause of insomnia; perceptions of the importance of treating insomnia; and satisfaction with available treatment options and with sleep disorders training. Among the items we included for assessing typical behavioral strategies recommended by PCPs for insomnia were two items that are counter to evidence-based behavioral approaches. These counterintuitive items were included to identify potential random responding patterns because the response set for this survey question was larger than for others and as such, respondents might randomly select responses to conclude the survey more quickly. Two survey items reference documentation forms that are unique to the VA electronic health record system: the Encounter Form and the Computerized Patient Record System (CPRS) Problem List. The Encounter Form is used for documenting the critical elements of the patient contact for billing purposes, including visit type, the complexity level of the visit, and diagnosis. The CPRS Problem List is a summary of active health concerns for each VA patient and serves as a reference for providers during clinical encounters.
The approach developed by Yang and colleagues18 was used to categorize recommended behavioral strategies for insomnia. Behaviors that interfere with homeostatic and/or circadian processes were grouped into the category of “sleep schedule and timing.” Behaviors that enhance arousal by promoting anxiety and/or conditioned arousal were categorized as “arousal-related behaviors.” Maladaptive eating and drinking habits and sleep-interfering environmental factors were grouped accordingly. We also included 2 items on our list of behavioral strategies that have face validity, but are, in fact, counter to recommended strategies for insomnia: (1) extend your time in bed; and (2) stay busy until bedtime.
Statistical Analyses
Means and standard deviation (SD) were used to report continuous variable findings and frequencies and percentages were used to report categorical variable findings.
RESULTS
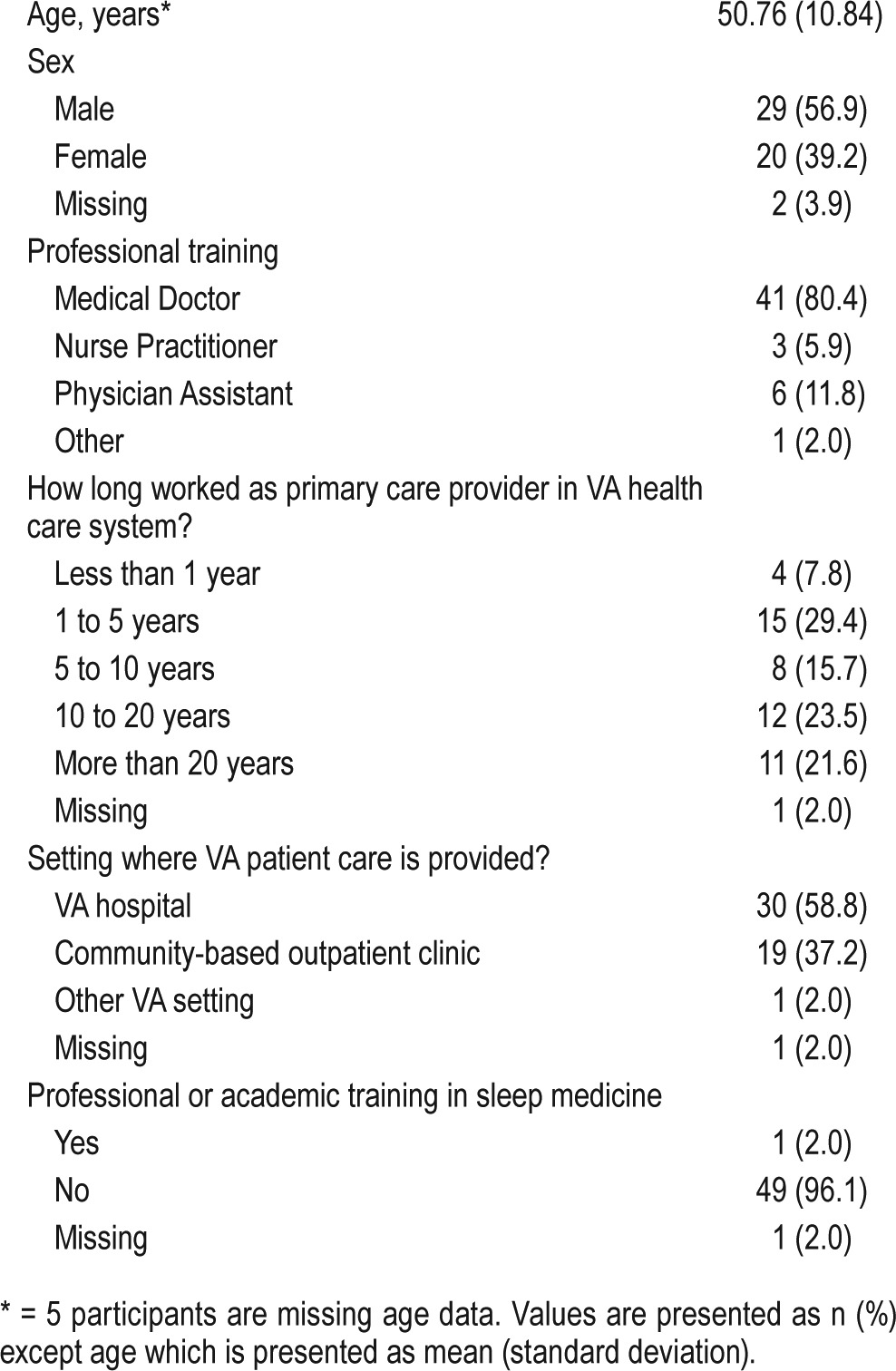
The survey response rate was 13% (51/381). Respondents were 50.76 years of age on average (SD = 10.84), primarily physicians (80.4%), and more than half were male (56.9%) (Table 1). In terms of both VA employee tenure and work history as a VA PCP, responses reflect a bimodal distribution with the greatest percentages having either 1 to 5 years of experience (29.4%) or 10 to 20 years of experience (23.5%). Most PCPs provided care in a VA hospital setting (58.8%) versus other clinical settings (39.2%), and only one respondent (2.0%) reported specialized training in sleep medicine.
Table 1.
Demographic and occupational characteristics of respondents (n = 51).
Survey Questions
What percentage of the veterans on your panel report a complaint of difficulty falling asleep, difficulty staying asleep, or waking too early?
The most frequently endorsed estimate among respondents was 20% to 39% (58.8% of respondents) of veterans reporting insomnia symptoms, whereas other respondents estimated the frequency to be higher (31.4%) or lower (5.9%). A few respondents did not answer this question (3.9%).
When a patient presents to your clinic complaining of difficulty falling asleep or staying asleep for 3 months or longer, and you do not suspect sleep apnea, which of the following treatment options are available to you? (Please check all that apply)
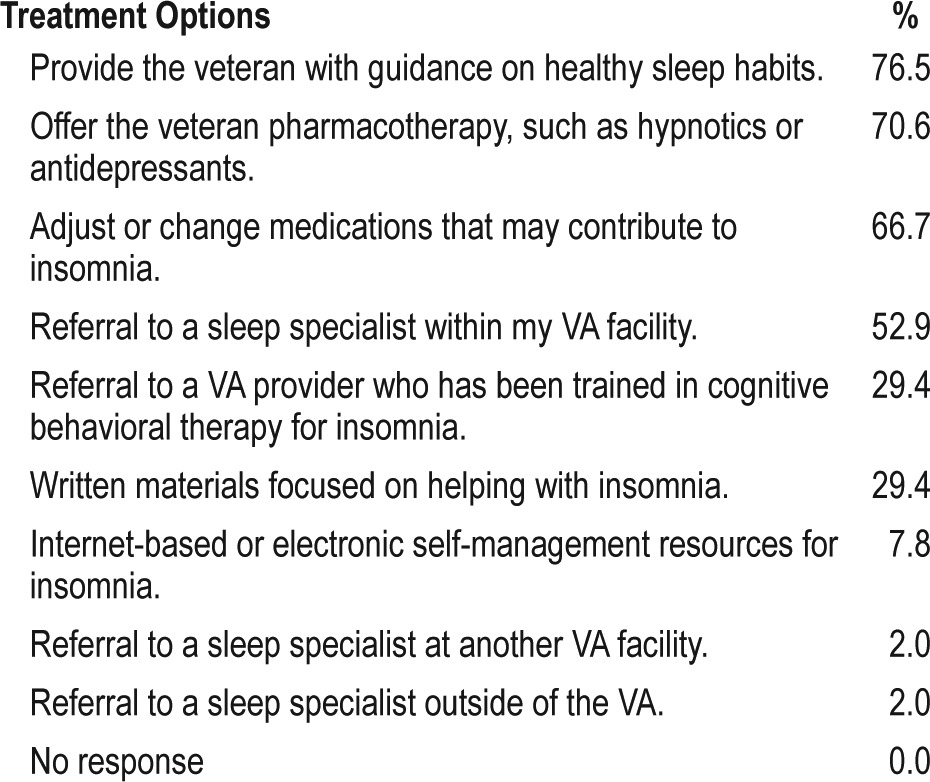
Table 2 summarizes PCP perceptions of available treatment options for addressing the insomnia complaints of veterans on their patient panel. The most frequently endorsed treatment options included: “provide the veteran with guidance on healthy sleep habits” (76.5%); “offer the veteran pharmacotherapy, such as hypnotics or antidepressants” (70.6%); and “adjust or change medications that may contribute to insomnia” (66.7%).
Table 2.
Perceived available insomnia treatment options.
When a patient presents to a primary care clinic complaining of difficulty falling asleep or difficulty staying asleep, primary care providers often suggest that the patient try one of several behavioral strategies to address their sleep complaint.
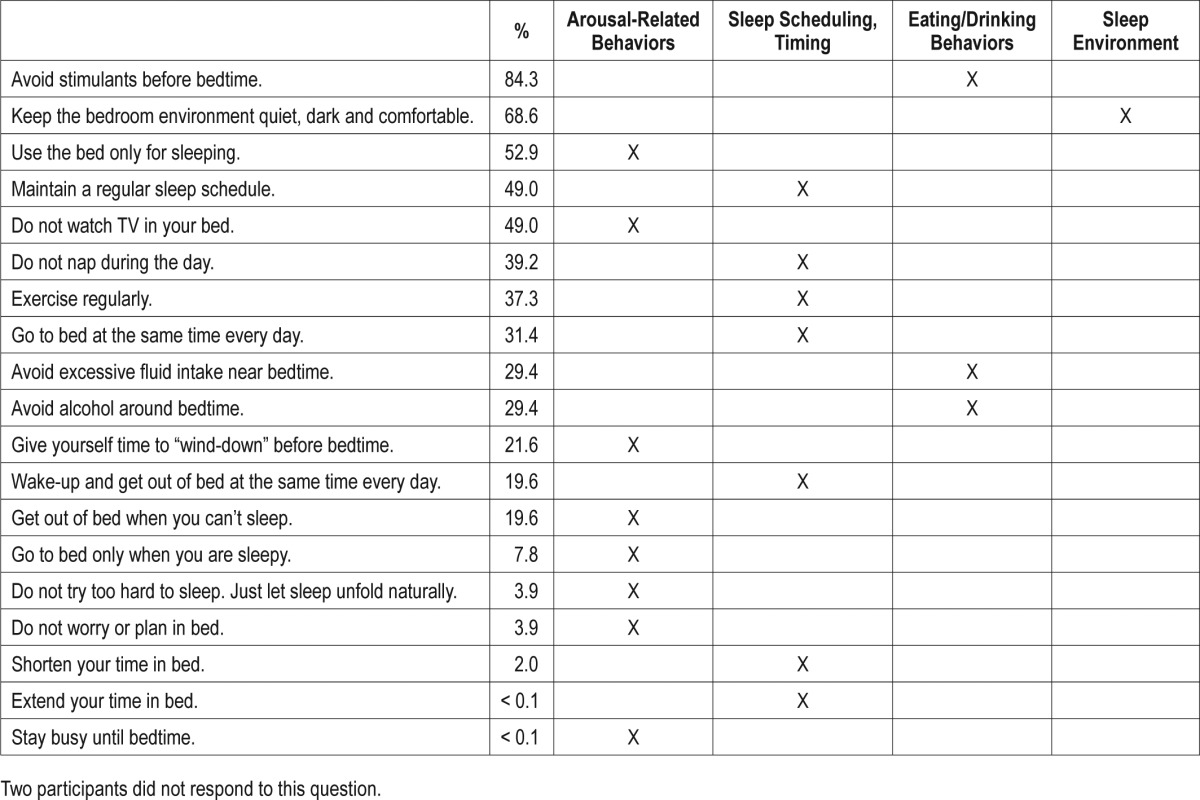
Table 3 summarizes the percentage of PCPs who endorsed each of several commonly recommended strategies for addressing their patients' insomnia complaints. The most common behavioral strategies endorsed by PCPs were: “avoid stimulants before bedtime” (84.3%); “keep the bedroom environment quiet and dark and comfortable” (68.6%); and “use the bed only for sleeping” (52.9%). The behavioral strategies endorsed least often were: “do not try too hard to sleep; just let sleep unfold naturally” (3.9%); “do not worry or plan in bed” (3.9%); and “shorten your time in bed” (2.0%). None of the respondents endorsed the 2 items that had been included to reveal random responding; “extend your time in bed” and “stay busy until bedtime.”
Table 3.
Primary care provider rates of endorsement for recommending strategies to address their patients' insomnia complaints.
When a patient presents to your clinic with a complaint of difficulty falling asleep or staying asleep for 3 months or longer, and you do not suspect sleep apnea, how often do you enter an insomnia diagnosis code into: (A) the encounter form; and (B) the CPRS problem list?
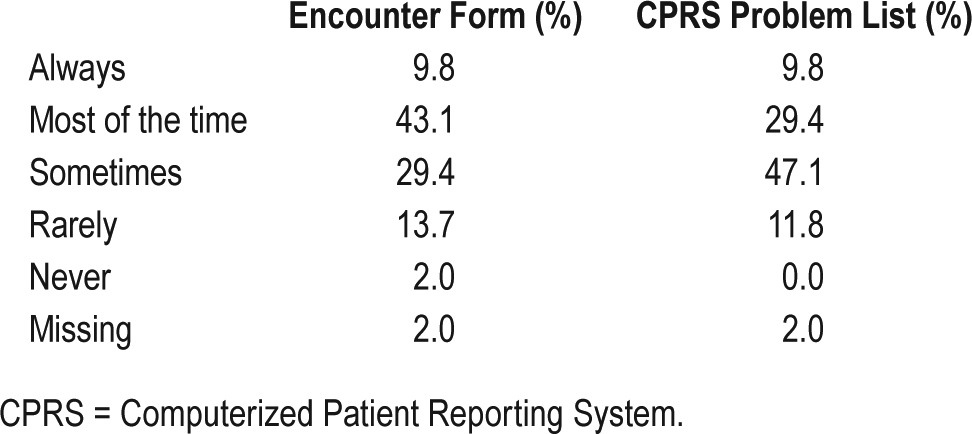
Table 4 summarizes PCP responses regarding documentation of insomnia in the medical record. Slightly more than half of respondents (52.9%) indicated that they document insomnia on the encounter form either “most of the time” or “always,” but less than half of respondents (39.2%) document insomnia in the problem list “most of the time” or “always.” Respondents endorsing “rarely” or “never” on either were asked for an explanation. Respondents endorsing “rarely” (n = 5) provided the following answers to the question, “Briefly state why you rarely diagnose Insomnia Disorder”: “easily missed”; “I did not say that, I said I don't list it”; “Not certain of the diagnostic criteria”; “often a co-existing condition related to…”; and “seems more a symptom than diagnosis.” Respondents endorsing “never” (n = 1) to this question stated: “other diagnoses take up the space.” Respondents endorsing “rarely” (n = 4) provided the following answers to the question, “Briefly state why you rarely add Insomnia Disorder to the problem list”: “competing diagnoses”; “no time”; “seems more a symptom than a diagnosis”; “usually other diagnosis, apnea being one” or have multiple mental health diagnoses as well.”
Table 4.
Insomnia documentation in the medical record.
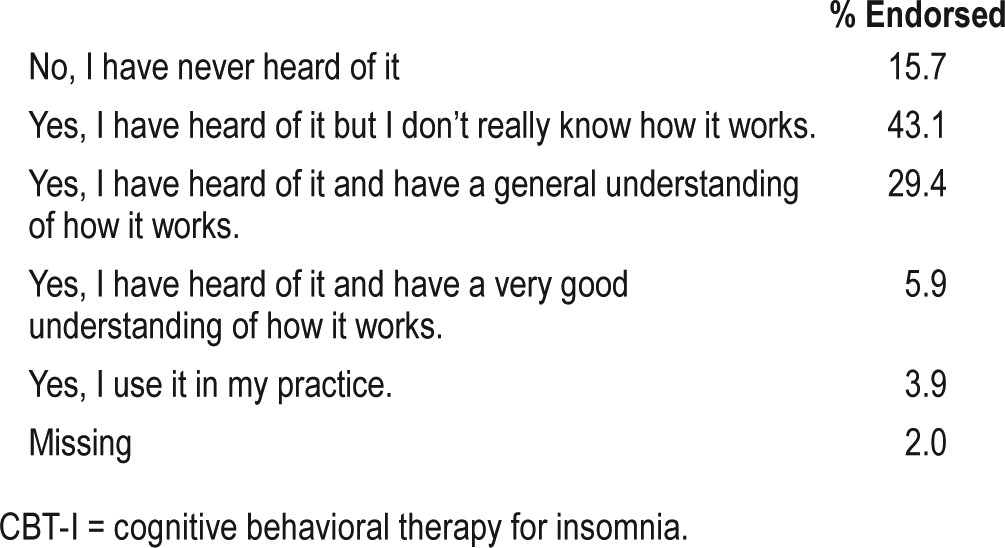
Are you familiar with cognitive behavioral therapy for insomnia (CBT-I)?
As reflected in Table 5, the majority of respondents had some level of familiarity with CBT-I (82.3%). However, a small percentage of respondents (15.7%) had never heard of it. One respondent did not answer this question (2%).
Table 5.
Respondents' familiarity with CBT-I.
Is cognitive behavioral therapy for insomnia (CBT-I) available at your facility?
PCPs responded to this question as follows: Yes (41.2%); No (13.7%); and Don't Know (43.1%). One respondent did not answer this question (2%).
From your perspective, treating insomnia is (more important/ equally important/less important) than treating other health concerns in terms of the overall health of veterans.
The majority of respondents indicated that treating insomnia is equally important (80.4%) as treating other health concerns. Others indicated that treating insomnia is less important (7.8%) or more important (5.9%) than treating other health concerns. Three respondents did not answer this question (5.9%).
From your perspective, treating insomnia is (more important/ equally important/less important) than treating sleep apnea in terms of the overall health of veterans.
The majority of respondents indicated that treating insomnia is equally important (66.7%) as treating sleep apnea. Others indicated that treating insomnia is less important (23.5%) or more important (3.9%) than treating sleep apnea. Three respondents did not answer this question (5.9%).
On a scale of 1 to 10 where 1 = not at all satisfied and 10 = very satisfied, how satisfied are you with the array of treatment options available to you for addressing the insomnia complaints of veterans presenting to your clinic?
The modal response to this question was 5 (23.5% of respondents).
On a scale of 1 to 10 where 1 = not at all satisfied and 10 = very satisfied, How satisfied are you with the opportunities available to you for training in the assessment and diagnosis of sleep disorders?
The modal response to this question was 5 (33.3% of respondents).
After a veteran has been successfully treated for PTSD or depression, their sleep difficulties will (always/often/ sometimes/rarely/never) remit.
All respondents perceive that sleep difficulties will remit either sometimes (49%) or often (45.1%) following successful treatment for PTSD or depression. Three (5.9%) respondents did not answer this question.
DISCUSSION
Our findings are generally consistent with research conducted in non-VA clinical settings. When considered in light of clinically significant insomnia prevalence as high as 50% among veterans,5 and prior research suggesting that only half of patients with probable insomnia discuss their insomnia complaint with their PCP,18,19 it appears from our findings that veterans report insomnia to their VA PCPs at rates similar to the general population (20% to 39%). In prior research, those discussing their insomnia complaint with their providers had more comorbid conditions and poorer self-ratings of overall health.20 Thus, veterans reporting insomnia to their VA PCPs may be those who are the most complex and more difficult to treat whereas those not reporting insomnia to their PCP might be more appropriate for less intensive insomnia interventions. This is an important consideration for disseminating insomnia treatment models focused on tailoring, such as stepped care, which considers matching between the patients' insomnia severity/chronicity and provider expertise/resources.
One of the most noteworthy findings of our survey was that PCPs perceived sleep hygiene as the most available insomnia treatment option, and they provided sleep hygiene education to their patients more often than any other approach. This finding contrasts with guidance that CBT-I should serve as the first-line treatment for insomnia, as recommended by the American Academy of Sleep Medicine,21 the Society of Behavioral Sleep Medicine,22 the National Institutes of Health,23 and most recently, by the American College of Physicians.24 Our findings in favor of the use of sleep hygiene, despite the dissemination of CBT-I, could be explained by a number of factors. First, access to CBT-I may remain insufficient to match the high prevalence of insomnia among veterans. With rates of clinically significant insomnia as high as 50% among veterans enrolling in VA health care,5 this is an entirely plausible explanation. Second, providers trained in CBT-I may devote minimal clinical resources to insomnia treatment. Despite having trained more than 600 mental health providers in CBT-I thus far, most trained providers are assigned to clinics focused on the treatment of other mental health conditions that are similarly prevalent among veterans (eg, PTSD, depression, substance use disorders). Thus, providing CBT-I may represent only a small portion of mental health providers' overall workload. Third, it is also possible that PCPs are unaware of the availability of CBT-I at their facilities, or that providers who have been trained in CBT-I have not “advertised” themselves as such at their facilities. Indeed, we found that only 29% of PCPs perceived CBT-I to be an available treatment option despite the fact that at least one provider at each facility has been trained in CBT-I. Fourth, preferences for sleep hygiene and medication might reflect a belief that treatments other than CBT-I are most effective. In fact, this was a central finding of prior research on physician referral practices.25 Fifth, the disconnect between availability and perception of CBT-I as a treatment option might also reflect a lack of understanding of CBT-I. We found that only 9.8% of respondents had a good understanding of how CBT-I is hypothesized to work or use it in their practice. Finally, because CBT-I is delivered by mental health providers within the VA setting, it may be that VA PCPs defer to mental health providers to manage the insomnia complaints of their patients with comorbid mental health conditions and insomnia disorder. As such, they may be less inclined to assess and diagnose insomnia for these patients who are likely to represent a considerable portion of their patient panels.
No matter the reason for the widespread use of sleep hygiene and limited use of CBT-I, our findings suggest that focused efforts are needed to increase access to CBT-I in VA primary care settings. In contrast with sleep hygiene, CBT-I produces sustained resolution of insomnia with fewer side effects than medications.26–28 Accordingly, the American College of Physicians recently recommended that “all adult patients receive CBT-I as the initial treatment for chronic insomnia disorder.”24 Although initially developed and promoted as an insomnia treatment,29 sleep hygiene is currently recommended only as an adjunct to effective CBT-I.27,30 In addition to small effect sizes and limited empirical support, sleep hygiene guidelines have been inconsistent.31 Although sleep hygiene education may be largely ineffective for insomnia, it may nevertheless have a legitimate role in the primary care setting. In prior research, sleep hygiene was strongly associated with sleep quality among normal sleepers but not in those with insomnia.18
Findings for PCP documentation of insomnia in the medical record were noteworthy as well. In prior research, Hermes and colleagues32 suggested that, more often than not, insomnia is not documented in the medical record by VA health care providers. They found an annual prevalence of 3.4% for diagnosed insomnia within the VA, a rate that is lower than prevalence rates suggested for the general population despite the fact that veterans have shorter sleep durations, longer sleep onset latencies, more wake after sleep onset, and lower sleep efficiencies than non-veterans.5,12,14,16 In fact, the failure to document insomnia in the medical record contrasts with recommendations by the American Academy of Sleep Medicine to document sleep satisfaction or quality in each visit wherein insomnia is discussed.33 Our findings extend prior research by providing insight into possible reasons for inconsistent documentation in the VA medical record. When respondents were asked to explain endorsement of rarely or never documenting insomnia, their explanations revealed three primary themes: insomnia is a symptom of another disorder that, if treated, would resolve the insomnia; other conditions are more important; and documenting secondary conditions is not realistic given the constraints of the clinical setting.
With our increased understanding of the etiology of insomnia over recent years, and concern that the term “secondary insomnia” promotes undertreatment,23 insomnia diagnoses were recently collapsed into a single disorder called “Insomnia Disorder” in revised medical and mental health diagnostic nosologies. In contrast, prior nosologies emphasized causal factors (secondary insomnia). As such, respondent perceptions of insomnia as a secondary condition may reflect adoption of older diagnostic schemes and lesser awareness of recent changes to insomnia diagnostic nosologies.
A subset of respondents did not routinely document insomnia in the medical record because it was perceived as less important than other conditions. Understandably so, acute symptoms representing imminent adverse health risks are prioritized in primary care clinical interactions. Because veterans are known to present to primary care clinics with more chronic conditions and more comorbidities than non-veterans,34 sleep complaints might receive even lesser clinical attention among veterans than non-veterans. Moreover, as reflected in the findings of the 2016 Physician Survey conducted by the Physician's Foundation,10 most PCPs feel challenged to attend to their patients' numerous medical and mental health conditions, and this is likely to be the case among VA PCPs as well.
Future research should be conducted to clarify certain response patterns and understand contradictory findings. For example, it is unclear why 41% of PCPs surveyed report that CBT-I is available at their facility, but only 29% endorsed CBT-I as an available insomnia treatment option. What considerations determine if a PCP documents insomnia in the medical record? How does the perception of insomnia as a symptom of another condition affect PCPs approach to insomnia treatment? In their recent review study, Araújo and colleagues35 recommended qualitative research as a strategy for improving insomnia care in the primary care setting. Qualitative research designed to expound on these topics could serve to increase understanding of PCP insomnia treatment practices and may reveal other relevant topics not previously considered.
In June 2015, the Sleep Research Society convened a work-group of implementation scientists and sleep researchers “to set a research agenda for sleep and circadian sciences in the area of implementation science.” Our study is responsive to the following insomnia research high-priority area recommended by the workgroup: “Assess perceived and actual barriers regarding insomnia treatment delivery, and incentives and disincentives for using various treatment modalities.”36 We identified implementation barriers at both the provider level and the systems level. At the provider level, our findings suggest the need to provide PCPs with education about the processes by which insomnia develops so they understand why, in many cases, treatment of a precipitating condition (eg, depression and PTSD) does not result in successful resolution of comorbid insomnia.37,38 In addition, PCPs should be made aware of the updated insomnia diagnostic criteria (International Classification of Sleep Disorders, Third Edition and the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition) and encouraged to document insomnia in the medical record because an inaccurate accounting of insomnia limits our ability to estimate prevalence and deploy resources. At the systems level, our findings reveal the need for health care systems to disseminate practice standards that align with the existing empirical evidence and to explicitly state that CBT-I is the standard of care for treatment of insomnia. Sleep hygiene can be considered for those with mild insomnia and should include education about how these guidelines relate to sleep regulation processes. In general, however, sleep hygiene should be offered by PCPs primarily as a strategy for maintaining healthy sleep in normal sleepers.31
The Sleep Research Society workgroup outlined a research agenda designed to “accelerate late-stage translation of sleep and circadian rhythms research findings to benefit public health.”36 With its strong evidence base but limited reach, CBT-I is exactly the kind of intervention in need of efforts to accelerate the pace of translation into clinical practice. The workgroup also suggested a need for community-based interventions to increase health literacy and screening for sleep disorders. With rates of insomnia among veterans at 50% or higher, efforts to identify and address insomnia among veterans cannot be limited to the primary care setting alone; community-based public health efforts are needed as well.
Our findings should be considered in light of certain limitations. First, our sample is not representative of all VA PCPs. Our study was conducted within a single region of the VA health care system and in only one part of the United States, so our findings may not generalize to PCPs in other regions or to non-VA providers. Although some evidence suggests that physician survey response rates have been on the decline,39 our response rate was lower than we would have liked and limited our ability to compare responses by provider type. Our response rate was considerably lower than a prior study of VA PCPs (51.8%) conducted by Singh and colleauges.40 However, on the one hand, because the recruitment process is not described in the study by Singh et al., it is unclear how our recruitment process might have differed. On the other hand, our response rate of 13% was higher than a recent study41 designed to examine the effect of incentives on physician response to Internet surveys wherein 11.4% responded to at least one question and only 8.5% completed the entire survey. Offering a nonmonetary incentive (book) did not increase response rates among physicians in this study. We explored the possibility of increasing PCP participation by offering an incentive, but found this to be against VA policy.
Although response rate has long been considered a criterion by which survey quality is assessed, recent empirical evidence suggests that nonresponse bias is a more important concept to consider than response rate.39 Specifically, it may be more important to understand how respondents compare to the recruitment sample as a whole. We compared the percentage of midlevel providers (versus MDs) between respondents and the sample of providers who received our recruitment emails. We found that 20% of survey respondents were midlevel providers as compared to 29% of the recruitment sample. The similarity between respondents and the recruitment sample allays some concern about nonresponse bias because provider training is likely to be relevant to treatment approach. However, due to the anonymous nature of our survey, we were unable to compare responders to the recruitment sample on other characteristics. For example, we could not compare findings by specific facility or the presence/absence of a CBT-I provider at an individual facility or clinic. As such, our study findings should be interpreted with caution due to the possibility that our survey respondents are not similar to the recruitment sample on other important characteristics. Future surveys should be designed to allow a thorough assessment of nonresponse bias as recommended by Johnson and Wislar.39 Larger sample sizes are also recommended to render larger cell sizes, allowing comparisons by provider type, facility type, CBT-I availability, and other provider characteristics.
The findings of our survey of VA PCPs underscore the need for a greater focus on insomnia assessment and treatment in primary care clinics, and may also serve as a starting point for future qualitative and implementation-focused research. In light of the prevalence of insomnia among both veterans and United States adults and an increasing awareness of the adverse health effects of chronic insomnia,42 increasing PCPs' ability to identify and effectively manage insomnia in the primary care setting is essential. Community-based efforts are needed to promote sleep health literacy, and to complement health care provider management of this highly prevalent condition.
DISCLOSURE STATEMENT
Work for this study was performed at Durham VA Medical Center. All authors have seen and approved this article. The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs. The authors have no conflicts related to the research described in this article. The first author was supported by a Veterans Affairs Research (VA) Career Development Award (CDA 09-218). Drs. Beckham, Bosworth and Voils were supported by VA Senior Research Career Scientist Awards (CSR&D #1lK6CX001494, HSR&D #RCS 08-027, and HSR&D #RCS 14-443, respectively) while preparing this manuscript. Preparation of this work was also supported by the Durham Veterans Affairs Medical Center; and the Department of Veterans Affairs Office of Research and Development. None of the other authors received financial support associated with their work on this project.
ACKNOWLEDGMENTS
The authors thank the following individuals for their assistance in developing our survey (listed in alphabetical order): James T. Bridges, PhD; Dana R. Epstein, PhD, RN; Stephen Gearhart, LCSW; Melanie Leggett, PhD, CBSM; Jennifer Martin, PhD, CBSM; Wilfred Pigeon, PhD, CBSM; Rachel Sol, PhD; Victoria Soler-Perez, PhD; Steve Woodward; and William Yancy, Jr, MD.
ABBREVIATIONS
- CBT-I
cognitive behavioral therapy for insomnia
- CPRS
Computerized Patient Record System
- HSR&D
Health Services Research and Development
- MD
medical doctor
- NP
nurse practitioner
- PA
physician assistant
- PCP
primary care provider
- PTSD
posttraumatic stress disorder
- SD
standard deviation
- VA
Veterans Affairs
- VISN
Veterans Integrated Service Network
REFERENCES
- 1.Ohayon MM. Prevalence of DSM-IV diagnostic criteria of insomnia: distinguishing insomnia related to mental disorders from sleep disorders. J Psychiatr Res. 1997;31(3):333–346. doi: 10.1016/s0022-3956(97)00002-2. [DOI] [PubMed] [Google Scholar]
- 2.Ohayon MM, Reynolds CF. Epidemiological and clinical relevance of insomnia diagnosis algorithms according to the DSM-IV and the International Classification of Sleep Disorders (ICSD) Sleep Med. 2009;10(9):952–960. doi: 10.1016/j.sleep.2009.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Roth T, Coulouvrat C, Hajak G, et al. Prevalence and perceived health associated with insomnia based on DSM-IV-TR; International Statistical Classification of Diseases and Related Health Problems, Tenth Revision; and Research Diagnostic Criteria/International Classification of Sleep Disorders, Second Edition criteria: results from the America Insomnia Survey. Biol Psychiatry. 2011;69(6):592–600. doi: 10.1016/j.biopsych.2010.10.023. [DOI] [PubMed] [Google Scholar]
- 4.Troxel WM, Shih RA, Pedersen ER, et al. Sleep in the Military: Promoting Healthy Sleep Among U.S. Servicemembers. Santa Monica, CA: RAND Corporation; 2015. [PMC free article] [PubMed] [Google Scholar]
- 5.Jenkins MM, Colvonen PJ, Norman SB, Afari N, Allard CB, Drummond SP. Prevalence and mental health correlates of insomnia in first-encounter veterans with and without military sexual trauma. Sleep. 2015;38(10):1547–1554. doi: 10.5665/sleep.5044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Davy Z, Middlemass J, Siriwardena AN. Patients' and clinicians' experiences and perceptions of the primary care management of insomnia: qualitative study. Health Expectations. 2013;18(5):1371–1383. doi: 10.1111/hex.12119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bailes S, Baltzan M, Rizzo D, et al. Sleep disorder symptoms are common and unspoken in Canadian general practice. Family Practice. 2009;26(4):294–300. doi: 10.1093/fampra/cmp031. [DOI] [PubMed] [Google Scholar]
- 8.Dyas JV, Apekey TA, Tilling M, Ørner R, Middleton H, Siriwardena AN. Patients' and clinicians' experiences of consultations in primary care for sleep problems and insomnia: a focus group study. Br J Gen Pract. 2010;60(574):e180–e200. doi: 10.3399/bjgp10X484183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cheung JM, Atternas K, Melchior M, Marshall NS, Fois RA, Saini B. Primary health care practitioner perspectives on the management of insomnia: a pilot study. Aust J Prim Health. 2014;20(1):103–112. doi: 10.1071/PY12021. [DOI] [PubMed] [Google Scholar]
- 10.The Physicians Foundation 2016 Physician Survey. The Physicians Foundation website. [Accessed March 9, 2017]. http://www.physiciansfoundation.org/healthcare-research/physician-survey. Published September 21, 2016.
- 11.Ford ES, Wheaton AG, Cunningham TJ, Giles WH, Chapman DP, Croft JB. Trends in outpatient visits for insomnia, sleep apnea, and prescriptions for sleep medication among US adults: findings from the National Ambulatory Medical Survey 1999-2010. Sleep. 2014;37(8):1283–1293. doi: 10.5665/sleep.3914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Faestel PM, Littell CT, Vitiello MV, Forsberg CW, Littman AJ. Perceived insufficient rest or sleep among veterans: Behavioral Risk Factor Surveillance System 2009. J Clin Sleep Med. 2013;9(6):577–584. doi: 10.5664/jcsm.2754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cepeda MS, Stang P, Blacketer C, Kent JM, Wittenberg GM. Clinical relevance of sleep duration: results from a cross-sectional analysis using NHANES. J Clin Sleep Med. 2016;12(6):813–819. doi: 10.5664/jcsm.5876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ulmer CS, Van Voorhees E, Germain AE, et al. A comparison of sleep difficulties among Iraq/Afghanistan theater veterans with and without mental health diagnoses. J Clin Sleep Med. 2015;11(9):995–1005. doi: 10.5664/jcsm.5012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mission of the Office of Academic Affiliations. U.S. Department of Veterans Affairs website. [Accessed June 26, 2017]. https://www.va.gov/oaa/oaa_mission.asp. Updated June 23, 2017.
- 16.Karlin BE, Trockel M, Taylor CB, Gimeno J, Manber R. National dissemination of cognitive behavioral therapy for insomnia in veterans: therapist- and patient-level outcomes. J Cons Clin Psych. 2013;81(5):912–917. doi: 10.1037/a0032554. [DOI] [PubMed] [Google Scholar]
- 17.Epstein DR, Babcock-Parziale JL, Haynes PL, Herb CA. Insomnia treatment acceptability and preferences of male Iraq and Afghanistan combat veterans and their healthcare providers. J Rehabil Res Dev. 2012;49(6):867–878. doi: 10.1682/jrrd.2011.06.0114. [DOI] [PubMed] [Google Scholar]
- 18.Yang CM, Lin SC, Hsu SC, Cheng CP. Maladaptive sleep hygiene practices in good sleepers and patients with insomnia. J Health Psychol. 2010;15(1):147–155. doi: 10.1177/1359105309346342. [DOI] [PubMed] [Google Scholar]
- 19.Shepardson RL, Funderburk JS, Pigeon WR, Maisto SA. Insomnia treatment experience and preferences among veterans affairs primary care patients. Mil Med. 2014;179(10):1072–1076. doi: 10.7205/MILMED-D-14-00011. [DOI] [PubMed] [Google Scholar]
- 20.Aikens JE, Rouse ME. Help-seeking for insomnia among adult patients in primary care. J Am Board Fam Pract. 2005;18(4):257–261. doi: 10.3122/jabfm.18.4.257. [DOI] [PubMed] [Google Scholar]
- 21.Morgenthaler T, Kramer M, Alessi C, et al. Practice parameters for the psychological and behavioral treatment of insomnia: an update. An American Academy of Sleep Medicine report. Sleep. 2006;29(11):1415–1419. [PubMed] [Google Scholar]
- 22.Schmitz MF. The ACP guidelines for treatment of chronic insomnia: the challenge of implementation. Behav Sleep Med. 2016;14(6):699–700. doi: 10.1080/15402002.2016.1220131. [DOI] [PubMed] [Google Scholar]
- 23.NIH state-of-the-science conference statement on manifestations and management of chronic insomnia in adults. NIH Consens State Sci Statements. 2005;22(2):1–30. [PubMed] [Google Scholar]
- 24.Qaseem AD, Kansagara MA, Forciea, et al. Management of chronic insomnia disorder in adults: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2016;165(2):125–133. doi: 10.7326/M15-2175. [DOI] [PubMed] [Google Scholar]
- 25.Conroy DA, Ebben MR. Referral practices for cognitive behavioral therapy for insomnia: a survey study. Behav Neurol. 2015;2015:819402. doi: 10.1155/2015/819402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Edinger JD, Olsen MK, Stechuchak KM, et al. Cognitive behavioral therapy for patients with primary insomnia or insomnia associated predominantly with mixed psychiatric disorders: a randomized clinical trial. Sleep. 2009;32(4):499–510. doi: 10.1093/sleep/32.4.499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Morin C, Bootzin RR, Buysse DJ, Edinger JD, Espie CA, Lichstein KL. Psychological and behavioral treatment of insomnia: update of the recent evidence (1998-2004) Sleep. 2006;29(11):1398–1414. doi: 10.1093/sleep/29.11.1398. [DOI] [PubMed] [Google Scholar]
- 28.Edinger JD, Wohlgemuth WK, Radtke RA, Marsh GR, Quillian RE. Cognitive behavioral therapy for treatment of chronic primary insomnia a randomized controlled trial. JAMA. 2001;285(14):1856–1864. doi: 10.1001/jama.285.14.1856. [DOI] [PubMed] [Google Scholar]
- 29.Hauri P. The Sleep Disorders. Kalamazoo, MI: Upjohn; 1982. [Google Scholar]
- 30.Lacks P, Morin CM. Recent advances in the assessment and treatment of insomnia. J Consult Clin Psychol. 1992;60(4):586–594. doi: 10.1037//0022-006x.60.4.586. [DOI] [PubMed] [Google Scholar]
- 31.Irish LA, Kline CE, Gunn HE, Buysse DJ, Hall MH. The role of sleep hygiene in promoting public health: a review of empirical evidence. Sleep Med Rev. 2015;22:23–36. doi: 10.1016/j.smrv.2014.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hermes E, Rosenheck R. Prevalence, pharmacotherapy and clinical correlates of diagnosed insomnia among Veterans Health Administration service users nationally. Sleep Med. 2014;15(5):508–514. doi: 10.1016/j.sleep.2013.12.010. [DOI] [PubMed] [Google Scholar]
- 33.Edinger JD, Buysse DJ, Deriy L, et al. Quality measures for the care of patients with insomnia. J Clin Sleep Med. 2015;11(3):311–334. doi: 10.5664/jcsm.4552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hoerster KD, Lehavot K, Simpson T, McFall M, Reiber G, Nelson KM. Health and health behavior differences: U.S. Military, veteran, and civilian men. Am J Prev Med. 2012;43(5):483–489. doi: 10.1016/j.amepre.2012.07.029. [DOI] [PubMed] [Google Scholar]
- 35.Araújo T, Jarrin DC, Leanza Y, Vallières A, Morin CM. Qualitative studies of insomnia: current state of knowledge in the field. Sleep Med Rev. 2016;31:58–69. doi: 10.1016/j.smrv.2016.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Parthasarathy S, Carskadon MA, Jean-Louis G, et al. Implementation of sleep and circadian science: recommendations from the Sleep Research Society and National Institutes of Health workshop. Sleep. 2016;39(12):2061–2075. doi: 10.5665/sleep.6300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Carney C, Segal ZV, Edinger JD, Krystal AD. A comparison of rates of residual insomnia symptoms following pharmacotherapy or cognitive-behavioral therapy for major depressive disorder. J Clin Psychiatry. 2007;68(2):254–260. doi: 10.4088/jcp.v68n0211. [DOI] [PubMed] [Google Scholar]
- 38.Belleville G, Guay S, Marchand A. Impact of sleep disturbances on PTSD symptoms and perceived health. J Nerv Mental Dis. 2009;197(2):126–132. doi: 10.1097/NMD.0b013e3181961d8e. [DOI] [PubMed] [Google Scholar]
- 39.Johnson TP, Wislar JS. Response rates and nonresponse errors in surveys. JAMA. 2012;307(17):1805–1806. doi: 10.1001/jama.2012.3532. [DOI] [PubMed] [Google Scholar]
- 40.Singh H, Spitzmueller C, Petersen NJ, et al. Primary care practitioners' views on test result management in EHR-enabled health systems: a national survey. J Am Med Inform Assoc. 2013;20(4):727–735. doi: 10.1136/amiajnl-2012-001267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cook DA, Wittich CM, Daniels WL, West CP, Harris AM, Beebe TJ. Incentive and reminder strategies to improve response rate for internet-based physician surveys: a randomized experiment. J Med Internet Res. 2016;18(9):e244. doi: 10.2196/jmir.6318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Li M, Zhang XW, Hou WS, Tang ZY. Insomnia and risk of cardiovascular disease: a meta-analysis of cohort studies. Int J Cardiol. 2014;176(3):1044–1077. doi: 10.1016/j.ijcard.2014.07.284. [DOI] [PubMed] [Google Scholar]


