Abstract
PURPOSE
To inform efforts to reduce costly service utilization, the present study examined longitudinal trajectories of mental health-related outpatient and residential service use among at-risk youth with a history of early externalizing problems.
METHODS
809 children in the Fast Track project, a multi-site longitudinal study of children at risk for conduct disorder, were followed prospectively from kindergarten through 12th grade. They resided in high-risk areas with high rates of poverty, crime, and violence. Their outpatient and residential service use was assessed annually between 6th through 12th grades through parent report. Growth mixture modeling (GMM) was applied to model individual differences in trajectories of service use during this period. Teacher, parent, and observer-reported childhood predictors of those trajectories were also examined.
RESULTS
The majority of youths had minimal service use during pre-adolescence into adolescence. However, approximately 31% had moderate probability of using outpatient counseling services, and approximately 8% had elevated probability of seeing a family doctor for mental health needs. For residential services, approximately 6% had moderate to high probability of service use that peaked during transition to high school, whereas close to 5% had service use that dramatically increased during high school. Childhood predictors of these trajectories included earlier externalizing, internalizing, and emotion regulation problems.
CONCLUSIONS
This study is the first to use person-centered analytic methods to examine longitudinal trajectories in mental health-related service use among at-risk adolescents. Timely treatment for severe externalizing problems, comorbid internalizing problems, and emotion dysregulation during childhood may be crucial for preventing chronic service use.
Keywords: mental health services, adolescents, at-risk, externalizing, service utilization
Introduction
Children with early externalizing problems are at high risk for a number of maladaptive and costly outcomes by young adulthood, including antisocial activity, risky health behaviors, poor educational and employment attainment, and increased mental health service use (1, 2, 3). They are also at higher risk for sequelae requiring medical care, including injury (4) and engagement in or exposure to violence (5). If their externalizing problems are unmitigated, they may suffer from continued psychopathology (6) and poorer physical health (7) into adulthood. Prevention of these difficult and costly outcomes require timely intervention. To determine who would benefit from intervention and when intervention needs to be timed, it is important to first understand individual differences in their utilization of mental health services and predictors of chronic or high levels of service use. Toward this goal, the present study used person-centered, longitudinal analysis to identify patterns of mental health service use among adolescents with a history of early externalizing problems.
Children with externalizing problems, which include oppositional, aggressive, and disruptive behaviors, comprise a particularly vulnerable population. They pose increased costs of mental health services and childcare at home based on their increased need for behavior management and supervision (8). Moreover, past research has suggested a higher rate of mental health-related service use in children or adolescents with externalizing disorders than those with internalizing disorders (3). Even among youth with internalizing problems such as depressive disorder, co-morbid externalizing problems have been associated with increased functional impairment, obesity, and a trend towards increased suicidal ideation (9). Consistent with this research, costs of mental health-related services for adolescents and young adults with histories of externalizing problems are quite significant, averaging $2,636 annually (10). In contrast, the estimated cost for the average individual is $1,591 (11).
Furthermore, they may require increased levels of general medical care and pediatric services. For example, a large community-based study in the United States (12) has found that many parents of children with mental health needs seek out care from a general medical care provider rather than a mental health professional. Children with externalizing problems are also at high risk for injury (4) and exposure to violence (5), further increasing their potential need for medical services. Among young children in low-income households, externalizing problems was one of the top ten reasons for pediatric hospitalization (13), suggesting that unmet mental health needs in this population may result in general medical care use. Thus, the present study also examined the use of general medical or pediatric care services for mental health needs.
There are additional questions related to long-term service use in children with externalizing problems that are not yet fully addressed in the existing literature. For one, it is unclear to what extent at-risk adolescents in disadvantaged communities access services. They are less likely to receive necessary mental health services compared to those in more privileged communities (14), possibly due to service-related costs, lack of insurance, and an overall deficit in accessible services (15). Moreover, families may have difficulty accessing available services because of geographical barriers, though having a child with externalizing problems is a strong predictor of mental health service use (14). More research is needed to clarify the extent to which high-risk adolescents residing in low-income, high-risk regions access mental health-related services.
Additionally, there is limited longitudinal research on service utilization. Existing studies have shown that, when service use begins in early childhood, it continues to increase throughout adolescence (16). Moreover, children who experience increased functional impairment due to psychopathology are more likely to continue utilizing services over time (17, 18). However, most existing research has been conducted with epidemiological data that are summarized at the population level. More research is needed to examine whether there are individual differences in the trajectories of service use (e.g., chronic, minimal use, decreasing or increasing across adolescence) and the types of services used among at-risk youth.
In addition to addressing these gaps in the literature by examining individual differences in service use over time, the present study also examined childhood predictors of service use, to help identify children at-risk for chronic and/or high service use. They are important to identify in order to optimize the utilization of effective and timely services and to maximize the clinical, public health, and economic value of services that are sought and received. Childhood predictors examined include earlier internalizing and externalizing psychopathology, poor emotion regulation skills, and lack of positive attention in parenting, as they are known risk factors for later psychopathology (19, 20, 21) and may also predict increased long-term service use.
In summary, although children with externalizing problems are known to utilize mental health services at an increased rate, to our knowledge, individual differences in trajectories of their service use during adolescence have not yet been explored. Examining potential heterogeneity in service use can inform intervention efforts, for instance by identifying adolescents with elevated risk for prolonged or high rates of service use. Furthermore, this line of research may provide insight into which types of mental health or health services are most likely to be used. Based on existing literature, the present study took an exploratory approach to study trajectories of mental health-related service use among adolescents with histories of externalizing problems in low-income, high-crime neighborhoods. We hypothesized that heterogeneity in trajectories of service use would be found among these adolescents, and that earlier psychopathology, emotion regulation problems, and low positive parental attention would be associated with elevated service use over time.
Method
Participants
Participants were 809 children (69.6% male) followed prospectively and annually from kindergarten to late adolescence by the Fast Track project, a multi-site, longitudinal study of children at risk for conduct disorder (http://www.fasttrackproject.org/). These children had adequate data for analysis and comprised 90.8% of the sample originally recruited for the project (N = 891). They were recruited for exhibiting the highest levels of externalizing behaviors at kindergarten on teacher and parent-report screens (for detailed information, see 22). Approximately half of the sample (n = 415; 51.3%) received the Fast Track services for prevention of future conduct disorder, while the rest (n = 394; 48.7%) did not receive any Fast Track prevention services. They attended 27 schools in areas selected for elevated levels of poverty and neighborhood crime, at four study sites (Durham, North Carolina; Nashville, Tennessee; Seattle, Washington; rural central Pennsylvania). These schools were randomized to intervention or control conditions. All procedures were approved by the Institutional Review Board of the Fast Track project’s principal investigators’ home institutions.
Measures
Service use
The child’s use of mental health services was measured using the parent report on the Service Assessment for Children and Adolescents (SACA; 23). Two types of mental health-related service use were assessed: 1. outpatient services (mental health center, day treatment, substance abuse clinic, school counselor, counselor/therapist, family doctor for mental health reasons), and 2. residential services (psychiatric hospital, residential treatment center, group home, foster home, general hospital, emergency shelter, and other residential facility). Annually between 6th and 12th grades, parents indicated how many times their child had used each service in the past year. Because the distribution of responses was highly zero-inflated (i.e., high endorsement of 0 times), and there was not enough meaningful variability in the total number of visits among users, service use was coded dichotomously (0 = not used; 1 = used) to permit analysis. Moreover, as some services had very low rates of use but could be meaningfully combined into a related category, they were combined to represent a larger category (e.g., outpatient mental health clinic to include mental health center, day treatment, and substance abuse clinic; residential mental health services all combined) to obtain adequate variability in the data for analysis.
Childhood predictors
Several psychosocial measures were used to assess potential predictors of the latent trajectories.
Early externalizing problems
Child Behavior Checklist (CBCL; 24) and its teacher version, Teacher Report Form (TRF), were used to assess child internalizing and externalizing behavior problems at kindergarten. Parents (CBCL) and teachers (TRF) rated 113 statements regarding the child’s behaviors on a 3-point scale ranging from 0 (not true) to 2 (very true or often true). High internal consistency has been found for both internalizing (CBCL α = .90; TRF α = .94) and externalizing broadband scales (CBCL α = .90; TRF α = .95).
Early emotion regulation
Social Competence Scale – Parent Version (SCP; 25) was administered at kindergarten to assess child emotion regulation skills. The SCP consists of 12 items completed by the parents, rated using a 5-point Likert scale ranging from 0 (not at all) to 4 (very well). The Emotional Regulation Skills subscale, which has adequate internal consistency (α = .78), was used.
Positive parental attention
Behavioral Coding System (BCS; 26) was used to assess the frequency of positive attention displayed by the parent during the Parent-Child Interaction Task (PCIT). During an annual home visit, each parent-child dyad participated in the PCIT, engaging in four tasks (free play; parent controlled game; challenging Lego task; clean-up). Trained research staff recorded the frequency of observed parental behaviors indicating positive attention towards the child in 30-second intervals. Total number of such behaviors were divided by the total length of the session to calculate the score (α = .70–.71). To obtain a reliable estimate of positive parental attention and minimize missing data, ratings from 1st through 3rd grade, when the BCS was administered, were averaged.
Preadolescent externalizing problems
CBCL and TRF were administered again in grade 5 to assess internalizing and externalizing problems. High internal consistency has been found for both the internalizing (α = .84–.88) and externalizing (α = .91–.92) scales.
Analytic Plan
To examine individual differences in longitudinal trajectories of service use, growth mixture modeling (GMM; 27) was applied. GMM is a person-centered analytic method that identifies subgroups, or latent classes, that differ in the trajectories of the outcome variables. Outcome variables were the dichotomized indicators of annual service use between 6th and 11th grades. Two separate models were estimated, one for outpatient service use with multiple types of service use modeled simultaneously, and the other for residential service use combined. Data from 12th grade were omitted from analyses, as they contained higher rate of missing data compared to prior years, likely reflecting increased attrition from the Fast Track study, and significantly worsened model fit.
GMM requires the number of latent classes fitted to the data to be specified a priori. Models with an increasing number of classes are compared, and the best fitting model is chosen based on indices of model fit and on interpretability. Model fit was compared using the Bayesian Information Criterion (BIC), entropy, the Lo-Mendell-Rubin likelihood ratio test of model fit (LMR; 28), and the Bootstrapped Likelihood Ratio Test (BLRT; 29). Superior model fit is indicated by the low BIC, high entropy, and significant results for LMR and BLRT.
GMM was used in an exploratory manner, to identify the number of distinct trajectories (latent classes) that exist in the sample. To identify potential confounding variables, effects of Fast Track intervention and demographic factors were examined using a Wald test (30). Potential predictors of the latent classes were tested using the 3-step approach that employs multinomial logistic regression (31). Analyses were run in Mplus 7.31, using full information maximum likelihood to accommodate missing data.
Results
Based on model fit (Table 1) and trajectories that emerged, outpatient and residential models with three latent classes were selected for interpretation. These models evidenced the highest entropy, which suggests that individuals were most clearly classified into three classes. Furthermore, the LMR test suggested that the 3-class model had improved model fit compared to the 2-class model, whereas adding another class to the 3-class model did not significantly improve model fit. The 3-class models also had relatively low BIC and good BLRT results.
Table 1.
Model Fit Indicators for the Growth Mixture Models
| Number of Classes | BICa | Entropy | Lo-Mendell- Rubin Testb p-value | Bootstrapped Likelihood Ratio Testb p-value |
|---|---|---|---|---|
| Outpatient Model | ||||
| 2 | 10426.91 | .78 | .00 | .00 |
| 3 | 10362.79 | .81 | .01 | .00 |
| 4 | 10349.17 | .77 | .06 | .00 |
| 5 | 10361.06 | .78 | .07 | .00 |
|
| ||||
| Inpatient Model | ||||
| 2 | 1815.17 | .85 | .00 | .00 |
| 3 | 1806.27 | .91 | .00 | .00 |
| 4 | 1821.51 | .84 | .13 | .00 |
| 5 | 1838.22 | .83 | .05 | .03 |
BIC = Bayesian Information Criterion. Lower BIC and higher entropy values indicate better model fit.
Significant results for the Lo-Mendell-Rubin and the Bootstrapped Likelihood Ratio tests indicate superior model fit compared to the model with one fewer class.
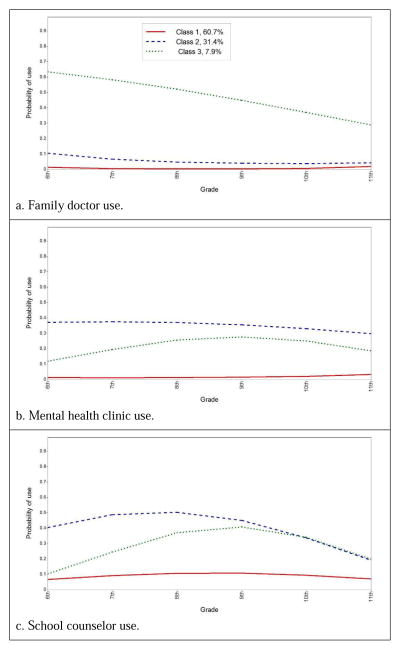
For the outpatient model (Figure 1), a slight majority of the sample (class 1, “minimal use”; 60.7%) evidenced consistently minimal use of all services. Another class (class 2, “moderate outpatient service use”; 31.4%) had moderate probability of service use, though with minimal family doctor visits. Finally, the smallest class (class 3, “family doctor use”; 7.9%) evidenced the highest levels of family doctor use but low to moderate use of other services.
Figure 1.
Latent trajectories of outpatient service use by type. Solid line represents Class 1 (“minimal use”), dashed line represents Class 2 (“moderate outpatient service use”), and dotted line represents Class 3 (“family doctor use”).
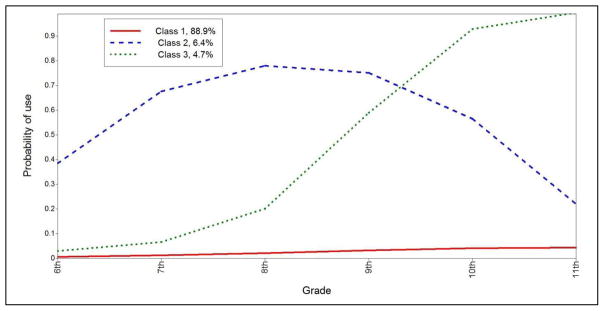
For the residential model (Figure 2), the vast majority of the sample (class 1, “minimal use”; 88.9%) evidenced consistently minimal use of all residential services. Another class (class 2 “early adolescent use”; 6.4%) evidenced elevated use of residential mental health services, with probability of use peaking near 8th grade. Finally, the smallest class (class 3 “increasing use”; 4.7%) evidenced low probability of service use during middle school and a sharply increased probability of use in high school.
Figure 2.
Latent trajectories of residential service use. Solid line represents Class 1 (“minimal use”), dashed line represents Class 2 (“early adolescent use”), and dotted line represents Class 3 (“increasing use”).
When potential covariates were examined for these models, neither demographic factors nor membership in the intervention (as opposed to control) condition of the Fast Track project significantly affected the participants’ latent class membership. However, four childhood variables significantly predicted class membership for the outpatient model (Table 2). Child emotion regulation skills at kindergarten predicted lowered likelihood of membership in class 2 (moderate mental health service use) compared to class 1 (minimal use), whereas teacher-reported externalizing problems at kindergarten predicted increased likelihood of membership in class 2. Interestingly, observer-rated parental positive attention and parent-reported externalizing problems at grade 5 both predicted increased likelihood of membership in class 3 (family doctor use). For the residential model, parent-reported internalizing problems at kindergarten and parent-reported externalizing problems and teacher-reported internalizing problems at grade 5 all predicted increased likelihood of membership in class 2 (early adolescent use) compared to the minimal use class. Parent-reported externalizing problems at grade 5 also predicted increased likelihood of membership in class 3 (increasing use).
Table 2.
Significant Predictors of Latent Classes, Based on Multinomial Logistic Regression
| Predictorsb | Likelihood of class membership
|
|||||
|---|---|---|---|---|---|---|
| Compared to class 1a
|
Compared to class 2a
|
|||||
| Class 2
|
Class 3
|
Class 3
|
||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Outpatient services model | ||||||
| SCP Emotion Regulation T1 | 0.54** | [0.12, 0.95] | 0.43 | [−0.40, 1.27] | 0.81 | [−0.11, 1.72] |
| TRF Externalizing T1 | 1.04*** | [1.02, 1.07] | 1.00 | [0.97, 1.03] | 0.96* | [0.93, 0.99] |
| BCS Parental Positive Attention (T2–T4) | 1.31 | [0.92, 1.71] | 2.25** | [1.75, 2.75] | 1.71* | [1.25, 2.18] |
| CBCL Externalizing T6 | 1.10 | [1.07, 1.13] | 1.08*** | [1.04, 1.11] | 0.98 | [0.94, 1.02] |
| Residential services model | ||||||
| CBCL Internalizing T1 | 1.05* | [1.01, 1.09] | 1.03 | [0.98, 1.07] | 0.98 | [0.92, 1.04] |
| CBCL Externalizing T6 | 1.06** | [1.02, 1.10] | 1.04* | [1.00, 1.08] | 0.98 | [0.93, 1.04] |
| TRF Internalizing T6 | 1.07** | [1.03, 1.12] | 1.02 | [0.97, 1.06] | 0.95 | [0.89, 1.01] |
“Compared to” indicates the reference class against which the odds of class membership in another class was compared.
T1 = kindergarten; T2–T4 = annual scores from grade 1 through grade 3 were averaged; T6 = grade 5.
p < .05.
p < .01.
p < .001.
Discussion
The present study examined longitudinal patterns of mental health-related service use among high-risk adolescents with a history of early externalizing behavior problems. Our findings suggest that children with early externalizing problems who also face high levels of ecological risk (e.g., poverty, violence exposure) develop heterogeneous patterns in service use during adolescence. A majority of the participants (60.7% for outpatient services; 88.9% for residential services) had stably low levels of use between 6th and 11th grades. Approximately one-third of the sample reported modest use of outpatient mental health services but fairly low use of the family doctor for mental health reasons. This group had poorer parent-reported emotion regulation skills and greater teacher-reported externalizing problems at kindergarten, as well as greater parent-reported externalizing problems in grade 5. Thus, these adolescents may have long-standing mental health needs. In contrast, the smallest proportion of the sample (7.9%) had highest levels of family doctor use for mental health needs and modest use of other outpatient services that increased during the transition to high school. These adolescents had higher externalizing problems and parental positive attention during childhood. Future studies are needed to clarify why their use of the family doctor declined over time while their use of other outpatient services increased during early adolescence. They may have experienced increased distress during their transition to adolescence and received referrals to specialty mental health services.
With respect to residential service use, a small proportion (6.4%) of the sample evidenced modest use that peaked between 8th and 9th grades. This group had higher levels of early internalizing problems and of both internalizing and externalizing problems in grade 5, and thus, they were characterized by chronic behavioral and affective dysregulation. Their increased service use during early adolescence is consistent with an increase in internalizing symptoms found during this developmental period, particularly among females (e.g., 32), though our current sample had a higher proportion of males (69.6%). Moreover, this pattern is also consistent with the idea that treatment-seeking behaviors tend to increase when more than one condition is present (33). The smallest (4.7%) proportion of adolescents showed a marked increase in residential service use between grades 8 and 11. Prediction of membership in this group was quite difficult, though this group had higher levels of parent-reported externalizing problems at grade 5 compared to the minimal-use group. These findings suggest that older children and pre-adolescents with high levels of externalizing problems, possibly comorbid with internalizing problems, are at highest risk for increased residential service use during adolescence. While residential service use may be appropriate and necessary in some cases, for some other youths, their service use may have been prevented with earlier access to less costly services, for example treatment in outpatient mental health or primary care settings. Future studies are needed to examine empirically whether these adolescents did not receive timely treatment, or failed to respond to earlier treatment though utilized.
With regard to prediction of membership in the subgroups, most of the findings were as expected, though results should be interpreted with caution and treated as preliminary given the small magnitude of difference in the odds ratios. However, contrary to the literature suggesting that positive regard by parents prevent self-regulation problems in children (34), observed positive parental attention predicted elevated family doctor use and modest use of other outpatient services during adolescence. Reasons for these links need to be investigated in future studies, to clarify whether higher positive parental attention was insufficient to prevent later psychopathology, or rather reflect parenting that is sensitive to children’s difficulties and seeks out for them necessary mental health care.
Another surprising result was the absence of detectable differences in service use between children in the Fast Track intervention group versus those in the control group. Previous research has also found that Fast Track prevention services did not affect rates of residential or outpatient service use in high school years, though they lowered parent-reported health service use and self-reported late adolescent outpatient mental health service use (35). Thus, the effects of intervention may not become apparent until later. Moreover, although the Fast Track intervention reduced the prevalence of externalizing disorders by late adolescence (36) and produced long-term reduction in such symptoms as antisocial behavior, avoidant personality, and alcohol and serious substance use, adolescents receiving Fast Track services may have utilized services for symptoms not addressed by the intervention. Further, the intervention may also have encouraged service use by raising awareness of needs for treatment. Again, further research on reasons for seeking treatment is needed, to clarify whether multimodal preventive services such as those offered by the Fast Track project improve appropriate treatment utilization.
Overall, our findings suggest divergence in long-term outcomes among children with early externalizing problems, predicted somewhat by earlier psychopathology. Interestingly, children with co-morbid internalizing problems were more likely to utilize residential services during adolescence. This is consistent with existing research showing that depression and behavioral problems are the most common clinical reasons for inpatient admission among youth (37). Thus, for prevention of later residential service use, early intervention may be especially indicated for children with greatest levels of co-morbid internalizing and externalizing problems.
Service use peaked during pre-adolescence or early adolescence for many of the services. This may be due to significant developmental transitions and biopsychosocial changes taking place during this time, including onset of puberty, transition to middle and high schools, and increased peer contact and independence (38). The increased stress associated with these types of transitions may lead to increased need for mental health treatment.
The present study had several limitations. As service use was measured using retrospective parent report, it is possible that some service use was not accurately reported. Moreover, utilization of outpatient psychiatric services was not assessed in the study. Furthermore, as the clinical reason for service use was not assessed, whether chronic service use reflected unmitigated symptoms or an emergence of new problems over time could not be assessed. Also, although race did not moderate the results, there may have been ethnic or cultural differences in service utilization among participating families (39) that were not accounted for by the present study. As with any longitudinal study, there was missing data, which were estimated using full-information maximum likelihood. The findings from the present study apply primarily to children with early externalizing problems, which are more prevalent in boys (40), though sex did not moderate the findings. Finally, any investigation of services use patterns is subject to variation in healthcare policy and practice, both regionally and historically. Findings may differ based on changes in circumstances (e.g., major initiatives such as the Affordable Care Act) that could differentially affect sub-populations. We encourage future research examining variations based on key contextual factors.
In conclusion, the findings suggest that many children with early externalizing behavior problems, especially those with the highest levels of chronic externalizing problems, early emotion dysregulation, and/or comorbid internalizing problems, are likely to continue requiring mental health treatment during adolescence. Although it is not possible to prevent all mental health service use among high-risk adolescents, as service use may be unpreventable, appropriate, and needed for some youths, improving access to effective mental health treatment or to universal, selected, or indicated prevention services during childhood may help reduce preventable chronic service use. Further research is needed to clarify individual and contextual factors that affect access and responses to earlier treatment, as well as their impact on service use during adolescence.
Implications and Contribution.
Present study found individual differences in mental health-related outpatient and residential service use among high-risk adolescents with a history of early externalizing problems. To reduce costly, preventable service use, early intervention is indicated for chronic externalizing problems, comorbid internalizing problems during childhood, and distress necessitating residential treatment during pre-adolescence.
Acknowledgments
The data utilized in the study were provided courtesy of Conduct Prevention Problems Research Group (Karen Bierman, PhD, John Coie, PhD, Ken Dodge, PhD, John Lochman, PhD, Robert McMahon, PhD, and Ellen Pinderhughes, PhD). The data were collected as part of the Fast Track project, supported by grants from the National Institute of Mental Health (NIMH) (R18 MH48043, R18 MH50951, R18 MH50952, R18 MH50953, K05MH00797, K05MH01027), the Department of Education (S184U30002), and the National Institute on Drug Abuse (DA16903, DA017589, K05DA015226, P30DA023026). The Center for Substance Abuse Prevention and the National Institute on Drug Abuse also provided support through a memorandum of agreement with NIMH. We thank the Fast Track project staff and participants.
Footnotes
Disclosure of potential conflicts: The authors have no conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Timmermans M, Van Lier PAC, Koot HM. Which forms of child/adolescent externalizing behaviors account for late adolescent risky sexual behavior and substance use? J Child Psychol Psychiatry. 2008;49:386–394. doi: 10.1111/j.1469-7610.2007.01842.x. [DOI] [PubMed] [Google Scholar]
- 2.Zwaanswijk M, Van Der Ende JAN, Verhaak PFM, et al. Factors Associated With Adolescent Mental Health Service Need and Utilization. J Am Acad Child Adolesc Psychiatry. 2003;42:692–700. doi: 10.1097/01.CHI.0000046862.56865.B7. [DOI] [PubMed] [Google Scholar]
- 3.Merikangas KR, He J-p, Burstein M, et al. Service Utilization for Lifetime Mental Disorders in U.S. Adolescents: Results of the National Comorbidity Survey - Adolescent Supplement (NCS-A) J Am Acad Child Adolesc Psychiatry. 2011;50:32–45. doi: 10.1016/j.jaac.2010.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jokela M, Power C, Kivimäki M. Childhood problem behaviors and injury risk over the life course. J Child Psychol Psychiatry. 2009;50:1541–1549. doi: 10.1111/j.1469-7610.2009.02122.x. [DOI] [PubMed] [Google Scholar]
- 5.Liu J. Childhood externalizing behavior: Theory and implications. J Child Adolesc Psychiatr Nurs. 2004;17:93–103. doi: 10.1111/j.1744-6171.2004.tb00003.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Copeland WE, Shanahan L, Costello J, et al. Childhood and adolescent psychiatric disorders as predictors of young adult disorders. Arch Gen Psychiatry. 2009;66:764–772. doi: 10.1001/archgenpsychiatry.2009.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jones DR, Macias C, Barreira PJ, et al. Prevalence, severity, and co-occurrence of chronic physical health problems of persons with serious mental illness. Psychiatr Serv. 2004;55:1250–1257. doi: 10.1176/appi.ps.55.11.1250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Romeo R, Knapp M, Scott S. Economic cost of severe antisocial behaviour in children -- and who pays it. Br J Psychiatry. 2006;188:547–553. doi: 10.1192/bjp.bp.104.007625. [DOI] [PubMed] [Google Scholar]
- 9.Rockhill CM, Katon W, Richards J, et al. What clinical differences distinguish depressed teens with and without comorbid externalizing problems? Gen Hosp Psychiatry. 2013;35:444–447. doi: 10.1016/j.genhosppsych.2013.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pelham WE, Foster EM, Robb JA. The economic impact of Attention-Deficit/Hyperactivity Disorder in children and adolescents. Ambul Pediatr. 2007;7:121–131. doi: 10.1016/j.ambp.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 11.Agency for Healthcare Research and Quality. [Accessed March 7, 2016];Mental healthcare cost data for all americans. Available at: http://www.nimh.nih.gov/health/statistics/cost/mental-healthcare-cost-data-for-all-americans-2006.shtml.
- 12.Briggs-Gowan MJ, Horwitz SM, Schwab-Stone ME, et al. Mental health in pediatric settings: Distribution of disorders and factors related to service use. J Am Acad Child Adolesc Psychiatry. 2000;39:841–849. doi: 10.1097/00004583-200007000-00012. [DOI] [PubMed] [Google Scholar]
- 13.Simpson L, Owens PL, Zodet MW, et al. Health care for children and youth in the United States: Annual report on patterns of coverage, utilization, quality, and expenditures by income. Ambul Pediatr. 2005;5:6–e20. doi: 10.1367/A04-119R.1. [DOI] [PubMed] [Google Scholar]
- 14.Gudiño OG, Lau AS, Hough RL. Immigrant status, mental health need, and mental health service utilization among high-risk Hispanic and Asian Pacific Islander youth. Child Youth Care Forum. 2008;37:139–152. doi: 10.1007/s10566-008-9056-4. [DOI] [Google Scholar]
- 15.Albritton T, Angley M, Gibson C, et al. Mental health utilization among diverse parenting young couples. Am J Community Psychol. 2015;56:89–100. doi: 10.1007/s10464-015-9738-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.John LH, Offord DR, Boyle MH, et al. Factors predicting use of mental health and social services by children 6–16 years old: findings from the Ontario Child Health Study. Am J Orthopsychiatry. 1995;65:76–86. doi: 10.1037/h0079597. [DOI] [PubMed] [Google Scholar]
- 17.Horwitz SM, Storfer-Isser A, Demeter C, et al. Use of outpatient mental health services among children of different ages: Are younger children more seriously ill? Psychiatr Serv. 2014;65:1026–1033. doi: 10.1176/appi.ps.201300209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nelson TD, Smith TR, Pick R, et al. Psychopathology as a predictor of medical service utilization for youth in residential treatment. J Behav Health Serv Res. 2013;40:36–45. doi: 10.1007/s11414-012-9301-3. [DOI] [PubMed] [Google Scholar]
- 19.Fanti KA, Henrich CC. Trajectories of pure and co-occurring internalizing and externalizing problems from age 2 to age 12: Findings from the National Institute of Child Health and Human Development Study of Early Child Care. Dev Psychol. 2010;46:1159–1175. doi: 10.1037/a0020659. [DOI] [PubMed] [Google Scholar]
- 20.Bornstein M, Hahn C, Haynes O. Social competence, externalizing, and internalizing behavioral adjustment from early childhood through early adolescence: Developmental cascades. Dev Psychopathol. 2010;22:717–735. doi: 10.1017/S0954579410000416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zeman J, Cassano M, Perry-Parrish C, et al. Emotion regulation in children and adolescents. J Dev Behav Pediatr. 2006;27:155–168. doi: 10.1097/00004703-200604000-00014. [DOI] [PubMed] [Google Scholar]
- 22.Lochman J. Screening of child behavior problems for prevention programs at school entry: Prediction and prevention of child and adolescent antisocial behavior. J Consult Clin Psychol. 1995;63:549–559. doi: 10.1037//0022-006x.63.4.549. [DOI] [PubMed] [Google Scholar]
- 23.Stiffman AR, Horwitz SM, Hoagwood K, et al. The Service Assessment for Children and Adolescents (SACA): Adult and child reports. J Am Acad Child Adolesc Psychiatry. 2000;39:1032–1039. doi: 10.1097/00004583-200008000-00019. [DOI] [PubMed] [Google Scholar]
- 24.Achenbach TM. Manual for the Child Behavior Checklist/4-18 and 1991 profile. Burlington, VT: University of Vermont, Department of Psychiatry; 1991. [Google Scholar]
- 25.Corrigan A. Social Competence Scale: Parent Version. Fast Track Project Technical Report. 2002 [Google Scholar]
- 26.Forehand R, McMahon R. Helping the noncompliant child: A clinician’s guide to parent training. New York, NY: Guilford Press; 1981. [Google Scholar]
- 27.Muthén BO. Mplus technical appendices. Los Angeles, CA: Muthén & Muthén; 1998–2004. [Google Scholar]
- 28.Lo Y, Mendell NR, Rubin DB. Testing the number of components in a normal mixture. Biometrika. 2001;88:767–778. doi: 10.1093/biomet/88.3.767. [DOI] [Google Scholar]
- 29.McLachlan G, Peel D. Finite mixture models. New York, NY: Wiley; 2000. [Google Scholar]
- 30.Asparouhov T. Wald test of mean equality for potential latent class predictors in mixture modeling. Los Angeles, CA: Mplus; 2007. [Google Scholar]
- 31.Vermunt JK. Latent class modeling with covariates: Two improved three-step approaches. Polit Anal. 2010;18:450–469. [Google Scholar]
- 32.Hankin BL, Abramson LY, Moffitt TE, et al. Development of depression from preadolescence to young adulthood: Emerging gender differences in a 10-year longitudinal study. J Abnorm Psychol. 1998;107:128–140. doi: 10.1037/0021-843X.107.1.128. [DOI] [PubMed] [Google Scholar]
- 33.du Fort GG, Newman SC, Bland RC. Psychiatric comorbidity and treatment seeking: Sources of selection bias in the study of clinical populations. The Journal of Nervous and Mental Disease. 1993;18:467–474. doi: 10.1097/00005053-199308000-00001. [DOI] [PubMed] [Google Scholar]
- 34.Eisenberg N, Zhou Q, Spinrad TL, et al. Relations among positive parenting, children’s effortful control, and externalizing problems: A three-wave longitudinal study. Child Dev. 2005;76:1055–1071. doi: 10.1111/j.1467-8624.2005.00897.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jones D, Godwin J, Dodge KA, et al. Impact of the Fast Track prevention program on health services use by conduct-problem youth. Pediatrics. 2010;125:e130–e136. doi: 10.1542/peds.2009-0322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Conduct Problems Prevention Research Group. The effects of the Fast Track Preventive Intervention on the development of conduct disorder across childhood. Child Dev. 2011;82:331–345. doi: 10.1111/j.1467-8624.2010.01558.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Case BG, Biel MG, Peselow ED, et al. Reliability of personality disorder diagnosis during depression: the contribution of collateral informant reports. Acta Psychiatr Scand. 2007;115:487–491. doi: 10.1111/j.1600-0447.2007.00995.x. [DOI] [PubMed] [Google Scholar]
- 38.Erath SA, Keiley MK, Pettit GS, et al. Behavioral predictors of mental health service utilization in childhood through adolescence. J Dev Behav Pediatr. 2009;30:481–488. doi: 10.1097/DBP.0b013e3181c35938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cauce AM, Domenech-Rodriguez M, Paradise M, et al. Cultural and contextual influences in mental health help seeking: A focus on ethnic minority youth. J Consult Clin Psychol. 2002;70:44–55. doi: 10.1037/0022-006X.70.1.44. [DOI] [PubMed] [Google Scholar]
- 40.Reef J, Diamantopoulou S, van Meurs I, et al. Developmental trajectories of child to adolescent externalizing behavior and adult DSM-IV disorder: results of a 24-year longitudinal study. Soc Psychiatry Psychiatr Epidemiol. 2011;46:1233–1241. doi: 10.1007/s00127-010-0297-9. [DOI] [PMC free article] [PubMed] [Google Scholar]