Abstract
Objectives
Dry socket may occur secondary to the removal of any tooth. However, most dry socket cases develop in the third molar region. Dry socket is multifactorial in nature and has been treated using various modalities with varying success rates. This study assessed the efficacy of platelet rich fibrin (PRF) in established dry socket.
Materials and Methods
Ten patients of either sex aged from 41 to 64 years with established dry socket according to established criteria were treated using PRF. Evaluation was performed by observing the reduction of pain using visual analogue scale, analgesic tablet use over the follow-up period, and healing parameters.
Results
Pain was reduced on the first day in all patients with decreased analgesic use. Pain was drastically reduced during follow-up on the first, second, third, and seventh days with a fall in pain score of 0 to 1 after the first day alone. The pain scores of all patients decreased to 1 by the first day except in one patient, and the scores decreased to 0 in all patients after 48 hours. Total analgesic intake ranged from 2 to 6 tablets (aceclofenac 100 mg per tablet) over the follow-up period of 7 days. Healing was satisfactory in all patients by the end of the seventh day.
Conclusion
PRF showed early pain reduction in established dry socket with minimal analgesic intake. No patients had allergic reactions to PRF as it is derived from the patient's own blood. PRF showed good wound healing. Our study suggests that PRF should be considered as a treatment modality for established dry socket.
Keywords: Osteogenesis, Tooth extraction, Tooth impaction, Wound Healing, Pain reduction
I. Introduction
Dry socket may occur as a complication secondary to the removal of any tooth. However, most dry socket cases develop in the third molar region1,2. Dry socket is multifactorial in nature. In a dry socket, blood clots dissolve2,3. This may result from many factors including surgical trauma, infection, type of extraction, patient factors, and surgeon factors3,4,5. Fibrinolytic activity is postulated to occur through plasminogen-mediated fibrinolysis, non-plasminogen-mediated fibrinolysis, and leucocyte-mediated fibrinolysis4. Other reports have suggested explanations for the differential occurrence of dry socket in females, including menstrual cycle associations and the use of oral contraceptives6,7. Poor oral hygiene and dislodgement of clot due to forceful spitting and sucking through straw have been suggested as predisposing factors4,8,9.
Management of dry socket was initially with anti-bacterial agents4,5,8, lavage, anti-fibrinolytic agents, steroidal anti-inflammatory agents, obtundents, and clot supportive agents1,3,9,10,11,12. The concept of dry socket management is changing toward alternative interventions including plasma rich growth factors, low level laser therapy11,12, and other treatments such as the use of honey. However, none of these modalities have proven 100% successful for prevention or for treatment1. Basic understanding about dry socket and management concepts remain the subject of significant debate1. This study assessed second generation platelet rich growth factors (PRGF)—platelet rich fibrin (PRF) in the management of established dry socket.
II. Materials and Methods
The study included 10 patients with aged from 41 to 64 years of either sex with dry socket diagnosis established according to the criteria of inclusion and were willing to participate in the PRF treatment protocol. Patients were enrolled from July to December 2015, the defined period of study. Patient complaints falling within the criteria of dry socket included major symptoms like continuous throbbing pain radiating to the ear, temple, and neck, start of pain 1 to 3 days post extraction, foul taste, bad breath, pain not relieved even after medication, and signs including devoid of blood clot, infected or retained roots, localized swelling, and lymphadenopathy. Such patients having a minimum of two symptoms and one sign were considered as established dry socket. (Table 1) Patients willing to participate in the treatment protocol using PRF were postoperatively assessed for various parameters like reduction of pain using visual analogue scale, reduction in analgesic use, and reduced symptoms and signs were noted. Those not willing to undergo PRF treatment were excluded from the study and were managed with other conventional modalities. Patients falling under the American Society of Anesthesiology category II, III, and IV, and pregnant women were not included in the study. The procedure and follow-up protocol were explained to both the patient and a relative in their mother tongue and informed written consent was obtained according to the Declaration of Helsinki. The study protocol was approved by the Institutional Ethics Committee.
Table 1. Criteria for diagnosis of dry socket (tick appropriate).
| Feature | Discription |
|---|---|
| Symptom | Continuous throbbing type of pain |
| Radiating to ear, temple and neck | |
| Start of pain 1-3 days post extraction | |
| Foul taste | |
| Bad breath | |
| Pain not relieved even after medication | |
| Sign | Devoid of blood clot |
| Infected or retained roots | |
| Localised swelling | |
| Lymphadenopathy |
1. Preparation of platelet rich fibrin
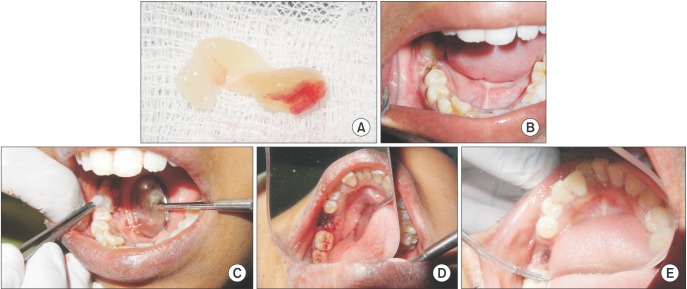
Ten milliliters of venous blood was drawn and centrifuged at 3,000 rpm for 10 minutes. Three layers were isolated after centrifugation with the first layer of red blood cells at the bottom, the second layer of white blood cells in the middle, and platelet rich fibrin on the surface. The standard operating procedure was followed. The wound was irrigated with normal saline. PRF was placed in the socket and sutured using 3.0 mersilk with a figure of eight.(Fig. 1) Clinical parameters were assessed on the first, second, third, seventh, and fifteenth days postoperatively for reduction in pain, analgesic intake, and satisfactory wound healing. Aceclofenac 100 mg tab was prescribed for all patients. Pain measured using a visual analogue scale (0 to 10) and wound healing (0 to 3) were used as modified assessment scales13,14,15.
Fig. 1. A. Photograph Showing Prepared Platelet Rich Fibrin (Prf). B. Intraoral Photograph Showing Dry Socket In Right Mandibular First Molar Region. C. Intraoperative Photograph Showing Placement Of Prf Into Dry Socket. D. Intraoperative Photograph Showing Closure Of Socket With A 3-0 Mersilk Suture. E. Intraoral Photograph Showing Healed Socket After 1 Week.
2. Statistical analysis
Data were tabulated using Microsoft excel (Microsoft, Redmond, WA, USA) and statistical analysis was carried out using the mean, percentage, Mann-Whitney test, Kruskal-Wallis test, and paired t-test. For statistical analysis, IBM SPSS Statistics ver. 20.0 (IBM Co., Armonk, NY, USA) was used. Statistics were considered significant if P<0.05.
III. Results
The study consisted of a total of ten patients (5 males and 5 females).(Table 2) Pain for all patients decreased to 1 by the first day except in one patient and decreased to 0 after 48 hours in all patients.(Tables 3,4,5) Severe pain was experienced by all patients before examination 6.80±0.789 (minimum-maximum pain score, 6-8), but was drastically reduced 3.00±0.000 (minimum-maximum pain score, 3-3) during follow-up (P<0.005).(Tables 4, 5) Analgesic intake ranged from 2 to 6 tablets but decreased to 0.(Table 6)
Table 2. Total number of administered analgesic tablets with patient details.
| Patient no. | Gender | Age (yr)1 | Tablet (n) |
|---|---|---|---|
| 1 | Male | 41 | 3 |
| 2 | Female | 43 | 4 |
| 3 | Male | 42 | 3 |
| 4 | Female | 50 | 4 |
| 5 | Male | 49 | 2 |
| 6 | Female | 48 | 6 |
| 7 | Male | 55 | 2 |
| 8 | Female | 58 | 3 |
| 9 | Male | 58 | 3 |
| 10 | Female | 64 | 3 |
| Total male | 5 | - | 50% |
| Total female | 5 | - | 50% |
1Mean (range) of age=50.8 yr (41-64 yr).
Table 3. Patients and percentage for each score at different time intervals (n=10).
| Time interval | Pain score | ||||||
|---|---|---|---|---|---|---|---|
| 8 | 7 | 6 | 3 | 2 | 1 | 0 | |
| At the time of examination | 2 (20) | 4 (40) | 4 (40) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| At the time of manipulation | 0 (0) | 0 (0) | 0 (0) | 10 (100) | 0 (0) | 0 (0) | 0 (0) |
| On day 1 | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (10) | 9 (90) | 0 (0) |
| On day 2 | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (10) | 9 (90) |
| On day 3 | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 10 (100) |
| On day 7 | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 10 (100) |
Values are presented as number (%).
Table 4. Visual analogue scale results at different intervals using the Mann-Whitney test.
| Time interval | Group | Patient (n) | Mean rank | P-value |
|---|---|---|---|---|
| At the time of examination vs manipulation | Examination | 10 | 15.50 | 0.001* |
| Manipulation | 10 | 5.50 | ||
| At the time of manipulation vs day 1 | Manipulation | 10 | 15.50 | 0.001* |
| Day 1 | 10 | 5.50 | ||
| At the time of manipulation vs day 2 | Manipulation | 10 | 15.50 | 0.001* |
| Day 2 | 10 | 5.50 | ||
| Day 1 vs day 2 | Day 1 | 10 | 15.05 | 0.001* |
| Day 2 | 10 | 5.95 |
*P<0.05 is considered significant.
Table 5. The visual analogue scale results at different interval days using Kruskal-Wallis test.
| Day | Patient (n) | Mean rank | P-value |
|---|---|---|---|
| 1 | 10 | 35.05 | 0.001* |
| 2 | 10 | 16.95 | |
| 3 | 10 | 15.00 | |
| 7 | 10 | 15.00 |
*Statistically significant.
Table 6. Comparison of intake of analgesics using paired t-test.
| Day | Mean | Patient (n) | Standard deviation | P-value |
|---|---|---|---|---|
| Day 1-morning-evening | 1.00 | 10 | 0.000 | 0.168 |
| 0.80 | 10 | 0.422 | ||
| Day 2-morning-evening | 0.30 | 10 | 0.483 | 0.168 |
| 0.10 | 10 | 0.316 | ||
| Day 1-day 2 | 2.80 | 10 | 0.422 | 0.001* |
| 0.50 | 10 | 0.972 |
*Statistically significant.
IV. Discussion
Dry socket is a complication secondary to extraction and the cause is multifactorial1,2,3,4,5. The management of dry socket is varied3,4,5,6,7,8,9,11,12,13,14,15, and strategies have varying rate of success1,9,10,11,12,13,14,15. Kaya et al.11 showed use of alvogyl, Salicept patch, low laser therapy, and curettage with irrigation in dry sockets of 104 patients divided into four groups. They concluded that Salicept patches can be used as an alternative to alvogyl as dressing in dry socket management. Pal et al.13 studied 45 patients divided into three groups (15 each) and showed better healing and reduced symptoms with zinc oxide eugenol (ZOE) and gelatin-soaked sponge with PRGF compared to conventional irrigation with saline. The study also suggested that use of PRGF with gelatin might be an appropriate management choice. Haraji et al.14 studied PRGF application in preventing dry socket in bilateral impactions of 40 patients divided in two groups, and showed good healing with PRGF and significant decrease in incidence of dry socket. The study showed beneficial effects of PRGF and suggested prophylactic use of PRGF after third molar extraction for the prevention of dry socket14. Singh et al.15 studied honey for the treatment of dry socket, which demonstrated a significant reduction of pain, inflammation, hyperemia, and soothing effect in 54 patients. Symptoms decreased with varying time duration, and the authors suggested the use of honey as a medicament in the management of dry socket.
The literature review showed patient response with varying degrees of success using available modalities1,3. Our study used PRF to fill the socket after irrigation, which showed potential pain reduction within 24 hours.(Table 6) This was associated with reduction in analgesic intake. Patients used a maximum of 6 tablets and a minimum of 2 tablets (aceclofenac 100 mg each). Preoperatively, the pain score was 6.80±0.078 and during treatment it was 3. At the first day, pain score was reduced to 1 in all but one patient. Complete reduction of pain was seen in 100% of patients by the third day with no analgesic intake. One patient showed very mild pain on the second day with intake of analgesic, which might be attributed to sociopsychological factors as the patient not having any deleterious habits, such as smoking that might have enhanced the pain condition. The resolution of pain was faster and this may be due to PRF. The kinine released from dry sockets will be antagonized by tissue growth factor, platelet-derived angiogenesis factor, platelet-derived growth factor, platelet-derived endothelial growth factor, interstitial growth factor, and platelet factor 4. These factors increase angiogenesis, chemotaxis, and epithelization with enhanced osteogenesis13,15.
PRF is biocompatible, effective, and safe because it is derived from the patient's own blood16. Recent reports suggested rapid epithelization and faster bone regeneration with PRF17,18,19,20,21,22,23,24. A few reports have noted the use of PRF in the extraction socket showing better healing and reduced incidence of dry socket or prevention of dry socket incidence18,19,21. Our study showed effective pain reduction with patients showing reduced intake of analgesic within 24 hours. Epithelization was prompt in all cases. We were able to appreciate wound closure by the seventh day without any pain or infection. PRF is a potential novel treatment modality for dry socket13,20,21,22,23,24, and the PRF mixture has shown to be a good scaffold for bone regeneration in rats25.
Upon comparing studies with existing treatment modalities, including the use of ZOE, alvogyl, GECB (guaiacol, eugenol, chlorobutanol, balsam Peru mixture), pastille, vitamin C, Salicept patch, PRGF, topical anesthetic gel Oraqix (Dentsply Pharmaceutical, Karlskoga, Sweden) neocone, and low level laser therapy11,13,15,25,26,27,28,29,30, the use of PRGF showed faster and better alveolar mucosal healing and was complete within 7 days of starting the treatment, which is earlier than the ZOE group13,14. Many of these studies did not conclude on the best treatment modality and instead offer suggestions for prevention without any one existing protocol superseding others8,31,32. Dry socket occurs frequently after tooth extraction as a complication and causes discomfort to the patient. Due to its multifactorial etiology, it is necessary to follow preventive methods in daily practice32,33. The published literature shows a disparity in interventions and type of measurement scale, and the published results are difficult to compare31. From the published data, it is not possible to draw any clear conclusions on treatment protocol11,12,13,14,15,25,26,27,28,29,30,31,32,33. Each institution has adopted a different protocol and therefore, despite the many studies and publications, additional investigations are required to establish the best method to treat dry socket31,32,33,34,35,36. Published review and meta-analysis suggests placement of topical antibiotics including tetracycline, lincomycin, or clindamycin foam, whereas systemic antibiotics should be reserved for patients who are immunocompromised5,8.
Within the limitations of our study, PRF showed better results when compared to any other modalities mentioned in the literature1,13,14,31. Our study included only 10 patients in a single center. We have not compared sex differences but the literature shows a higher incidence of dry socket in females6. This study did not have control groups for comparison as this was a preliminary case series with 15 days of follow-up for clinical examination. A randomized, blind, multicenter longterm study with histopathological examination is needed to confirm the nature of new bone formed during implant placement.
V. Conclusion
PRF is a promising agent for the management of dry socket in a cost-effective manner. PRF does not have reactions like analgesics, as it is derived from the patient's own blood without any additives. PRF showed early pain reduction in established dry socket with minimal analgesic intake. Our study suggests PRF as a potential treatment modality in the management of established dry socket.
Footnotes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Daly B, Sharif MO, Newton T, Jones K, Worthington HV. Local interventions for the management of alveolar osteitis (dry socket) Cochrane Database Syst Rev. 2012;12:CD006968. doi: 10.1002/14651858.CD006968.pub2. [DOI] [PubMed] [Google Scholar]
- 2.Fridrich KL, Olson RA. Alveolar osteitis following surgical removal of mandibular third molars. Anesth Prog. 1990;37:32–41. [PMC free article] [PubMed] [Google Scholar]
- 3.Blum IR. Contemporary views on dry socket (alveolar osteitis): a clinical appraisal of standardization, aetiopathogenesis and management: a critical review. Int J Oral Maxillofac Surg. 2002;31:309–317. doi: 10.1054/ijom.2002.0263. [DOI] [PubMed] [Google Scholar]
- 4.Vezeau PJ. Dental extraction wound management: medicating postextraction sockets. J Oral Maxillofac Surg. 2000;58:531–537. doi: 10.1016/s0278-2391(00)90016-8. [DOI] [PubMed] [Google Scholar]
- 5.Caso A, Hung LK, Beirne OR. Prevention of alveolar osteitis with chlorhexidine: a meta-analytic review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99:155–159. doi: 10.1016/j.tripleo.2004.05.009. [DOI] [PubMed] [Google Scholar]
- 6.Garcia AG, Grana PM, Sampedro FG, Diago MP, Rey JM. Does oral contraceptive use affect the incidence of complications after extraction of a mandibular third molar? Br Dent J. 2003;194:453–455. doi: 10.1038/sj.bdj.4810032. discussion 445. [DOI] [PubMed] [Google Scholar]
- 7.Muhonen A, Ventä I, Ylipaavalniemi P. Factors predisposing to postoperative complications related to wisdom tooth surgery among university students. J Am Coll Health. 1997;46:39–42. doi: 10.1080/07448489709595585. [DOI] [PubMed] [Google Scholar]
- 8.Noroozi AR, Philbert RF. Modern concepts in understanding and management of the “dry socket” syndrome: comprehensive review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:30–35. doi: 10.1016/j.tripleo.2008.05.043. [DOI] [PubMed] [Google Scholar]
- 9.Bloomer CR. Straws do not cause dry sockets when third molars are extracted. Tex Dent J. 2012;129:25–32. [PubMed] [Google Scholar]
- 10.Reekie D, Downes P, Devlin CV, Nixon GM, Devlin H. The prevention of ‘dry socket’ with topical metronidazole in general dental practice. Br Dent J. 2006;200:210–213. doi: 10.1038/sj.bdj.4813253. discussion 206; quiz 226. [DOI] [PubMed] [Google Scholar]
- 11.Kaya GŞ, Yapici G, Savaş Z, Güngörmüş M. Comparison of alvogyl, SaliCept patch, and low-level laser therapy in the management of alveolar osteitis. J Oral Maxillofac Surg. 2011;69:1571–1577. doi: 10.1016/j.joms.2010.11.005. [DOI] [PubMed] [Google Scholar]
- 12.Jovanović G, Urić N, Krunić N, Tijanić M, Stojanović S. Assessment of the effectiveness of low level laser in the treatment of alveolar osteitis. Vojnosanit Pregl. 2011;68:506–510. doi: 10.2298/vsp1106506j. [DOI] [PubMed] [Google Scholar]
- 13.Pal US, Singh BP, Verma V. Comparative evaluation of zinc oxide eugenol versus gelatin sponge soaked in plasma rich in growth factor in the treatment of dry socket: an initial study. Contemp Clin Dent. 2013;4:37–41. doi: 10.4103/0976-237X.111592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Haraji A, Lassemi E, Motamedi MH, Alavi M, Adibnejad S. Effect of plasma rich in growth factors on alveolar osteitis. Natl J Maxillofac Surg. 2012;3:38–41. doi: 10.4103/0975-5950.102150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Singh V, Pal US, Singh R, Soni N. Honey a sweet approach to alveolar osteitis: a study. Natl J Maxillofac Surg. 2014;5:31–34. doi: 10.4103/0975-5950.140166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Martínez-Zapata MJ, Martí-Carvajal A, Solà I, Bolibar I, Angel Expósito J, Rodriguez L, et al. Efficacy and safety of the use of autologous plasma rich in platelets for tissue regeneration: a systematic review. Transfusion. 2009;49:44–56. doi: 10.1111/j.1537-2995.2008.01945.x. [DOI] [PubMed] [Google Scholar]
- 17.Anitua E, Orive G. Use of PRGF to accelerate bone and soft tissue regeneration in postextraction sites. Implant Dialogue. 2003;36:3–14. [Google Scholar]
- 18.Alexander RE. Dental extraction wound management: a case against medicating postextraction sockets. J Oral Maxillofac Surg. 2000;58:538–551. doi: 10.1016/s0278-2391(00)90017-x. [DOI] [PubMed] [Google Scholar]
- 19.Plachokova AS, Nikolidakis D, Mulder J, Jansen JA, Creugers NH. Effect of platelet-rich plasma on bone regeneration in dentistry: a systematic review. Clin Oral Implants Res. 2008;19:539–545. doi: 10.1111/j.1600-0501.2008.01525.x. [DOI] [PubMed] [Google Scholar]
- 20.Aldecoa EA, Ortiz IA. A mew approach to bone regeneration: plasma rich in growth factors. Vitoria: Puesta al Dia Publicaciones; 2001. p. 172. [Google Scholar]
- 21.Sammartino G, Tia M, Marenzi G, di Lauro AE, D'Agostino E, Claudio PP. Use of autologous platelet-rich plasma (PRP) in periodontal defect treatment after extraction of impacted mandibular third molars. J Oral Maxillofac Surg. 2005;63:766–770. doi: 10.1016/j.joms.2005.02.010. [DOI] [PubMed] [Google Scholar]
- 22.Simon D, Manuel S, Geetha V, Naik BR. Potential for osseous regeneration of platelet-rich plasma--a comparative study in mandibular third molar sockets. Indian J Dent Res. 2004;15:133–136. [PubMed] [Google Scholar]
- 23.Mozzati M, Martinasso G, Pol R, Polastri C, Cristiano A, Muzio G, et al. The impact of plasma rich in growth factors on clinical and biological factors involved in healing processes after third molar extraction. J Biomed Mater Res A. 2010;95:741–746. doi: 10.1002/jbm.a.32882. [DOI] [PubMed] [Google Scholar]
- 24.Rutkowski JL, Johnson DA, Radio NM, Fennell JW. Platelet rich plasma to facilitate wound healing following tooth extraction. J Oral Implantol. 2010;36:11–23. doi: 10.1563/AAID-JOI-09-00063. [DOI] [PubMed] [Google Scholar]
- 25.Song JY, Kweon H, Kwon KJ, Park YW, Kim SG. The bone regenerative effect of silk fibroin mixed with platelet-rich fibrin (PRF) in the calvaria defect of rabbit. J Korean Assoc Oral Maxillofac Surg. 2010;36:250–254. [Google Scholar]
- 26.Halberstein RA, Abrahmsohn GM. Clinical management and control of alveolalgia (“dry socket”) with vitamin C. Am J Dent. 2003;16:152–154. [PubMed] [Google Scholar]
- 27.Burgoyne CC, Giglio JA, Reese SE, Sima AP, Laskin DM. The efficacy of a topical anesthetic gel in the relief of pain associated with localized alveolar osteitis. J Oral Maxillofac Surg. 2010;68:144–148. doi: 10.1016/j.joms.2009.06.033. [DOI] [PubMed] [Google Scholar]
- 28.Faizel S, Thomas S, Yuvaraj V, Prabhu S, Tripathi G. Comparision between neocone, alvogyl and zinc oxide eugenol packing for the treatment of dry socket: a double blind randomised control trial. J Maxillofac Oral Surg. 2015;14:312–320. doi: 10.1007/s12663-014-0667-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rani A, Mohanty S, Sharma P, Dabas J. Comparative evaluation of Er:Cr:YSGG, diode laser and alvogyl in the management of alveolar osteitis: a prospective randomized clinical study. J Maxillofac Oral Surg. 2016;15:349–354. doi: 10.1007/s12663-015-0848-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Haghighat A, Bahri Najafi R, Bazvand M, Badrian H, Khalighinejad N, Goroohi H. The effectiveness of GECB pastille in reducing complications of dry socket syndrome. Int J Dent. 2012;2012:587461. doi: 10.1155/2012/587461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Taberner-Vallverdú M, Nazir M, Sánchez-Garcés MÁ, Gay-Escoda C. Efficacy of different methods used for dry socket management: a systematic review. Med Oral Patol Oral Cir Bucal. 2015;20:e633–e639. doi: 10.4317/medoral.20589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kolokythas A, Olech E, Miloro M. Alveolar osteitis: a comprehensive review of concepts and controversies. Int J Dent. 2010;2010:249073. doi: 10.1155/2010/249073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sharif MO, Dawoud BE, Tsichlaki A, Yates JM. Interventions for the prevention of dry socket: an evidence-based update. Br Dent J. 2014;217:27–30. doi: 10.1038/sj.bdj.2014.550. [DOI] [PubMed] [Google Scholar]
- 34.Torres-Lagares D, Serrera-Figallo MA, Romero-Ruíz MM, Infante-Cossío P, García-Calderón M, Gutiérrez-Pérez JL. Update on dry socket: a review of the literature. Med Oral Patol Oral Cir Bucal. 2005;10:81–85. [PubMed] [Google Scholar]
- 35.Fazakerley M, Field EA. Dry socket: a painful post-extraction complication (a review) Dent Update. 1991;18:31–34. [PubMed] [Google Scholar]
- 36.Cardoso CL, Rodrigues MT, Ferreira Júnior O, Garlet GP, de Carvalho PS. Clinical concepts of dry socket. J Oral Maxillofac Surg. 2010;68:1922–1932. doi: 10.1016/j.joms.2009.09.085. [DOI] [PubMed] [Google Scholar]