Abstract
Following a slip occurred in the overground walking, a fall can be classified into two exclusive categories: feet-forward fall or split fall. The purposes of this study were to investigate whether the placement of the recovery foot would determine the slip types, the likelihood of fall, and the severity of fall. The fall severity was estimated based on the impact velocity of body segments or trunk orientation upon fall arrest. One hundred ninety-five participants experienced a novel, unannounced slip while walking on a 7-meter walkway. Kinematics of a full-body marker set was collected by a motion capture system which was synchronized with the force plates and loadcell. The results showed that the recovery foot landing position relative to the projected center of mass position at the recovery foot touchdown determined the slip type by 90.8%. Feet-forward slips led to significantly lower rate of falls than did split slips (47.6% vs. 67.8%, p < 0.01). Yet, feet-forward falls were much more dangerous because they were associated with significantly greater estimated maximum hip impact velocity (p < 0.001) and trunk backward leaning angle (p < 0.001) in comparison to split falls.
Keywords: Split fall, feet-forward fall, fracture, obesity, forensic
Introduction
The injuries, particularly hip fractures or traumatic head injuries related slip-induced fall accidents are major health problems in older adults.8, 21, 34 Even without injuries, falls can still lead to self-imposed limitations on independence of daily activities.46 Not all falls are equal, however, at least 10–20% falls result in serious injuries including fractures or require hospitalization.34 Injury severity is affected by many factors, including the location, direction and magnitude of the load applied on the body segments at the moment of impact as well as the tolerance level of the tissue.5, 16, 29 The hip or arm impact velocity are often associated with the respective hip or arm fractures,7, 30 and the trunk angle is indicative of the risk of head impact.29 The first step following the onset of a fall triggered by postural disturbance is likely the most critical reaction that can determine or at the very least, heavily influence the rest of the recovery outcome. Hence, this first step is termed either as compensatory step after postural disturbance in standing,15, 18 recovery step9, 36 or protective step19, 23 in walking.
The recovery foot placement follows a sequence of events. First, soon after the disturbance the recovery foot unloads the ground reaction force (GRF) and lifts off the ground. A rapidly lowering of the foot, landing and reloads followed sequentially.2, 20 In some instances following a slip onset, the recovery (trailing) foot’s unloading was never completed before reloading, which was called an “aborted” step.3 Generally, the slipping foot continues to move forward regardless how much the recovery foot moves forward. If the recovery foot moves in the opposite direction (V ≤ 0) after its landing, it results in a split slip; if it moves forward together with the slipping foot (V > 0), it leads to a feet-forward slip. The ensuing falls are termed correspondingly either split falls or feet-forward falls.42
The possibility of a one-foot or two-foot slip after landing can further complicate the characterization of these events. A one-foot (unilateral) slip always results in a split slip. A two-foot (bilateral) slip does not guarantee a feet-forward slip, though the majority (83.3%) would actually do so.42 The risk of falls is nearly equal regardless of one-foot or two-foot slip.42 Because of such complications, the causation in this chain of events, from postural disturbance to recovery foot liftoff (unloaded) some 200 (± 40) milliseconds later, to its touchdown (reloading) 100 (± 40) milliseconds later, and finally another 500 (± 200) milliseconds later to the fall arrest (terminated by a harness support in the laboratory and monitored by loadcell sensor),41 is far from clear.
At the time of recovery foot touchdown, its position relative to the slipping foot location cannot well predict the subsequent outcome from a split fall to a feet-forward fall.42 It is perceivable, however, its position relative to the vertically projected center of mass (COM) may improve such prediction and hence provide more reliable explanation of the causation of this event. The relative position between the COM and the foot landing position was found to indicate whether the initial step was of sufficient length to allow the body to arrest the posterior perturbation in response to waist pulls.32 Because the foot placement is the primary determinant of the position of the center of pressure (COP),25 the closer the distance between the foot placement and COM, the closer the distance between COP and COM, the lower the horizontal GRF and friction-force requirement,40 the lower the subsequent slip velocity,26 and hence the lower the risk of falls.4 From this perspective, the foot placement may not only determine the type of slips but also directly influences the risk of falls.
Is it possible that the recovery foot placement also plays an essential role that determines the severity of a fall? It has been postulated that the split fall would pose a lesser risk of hip fracture in comparison to the feet-forward fall.33, 42 Many kinematic variables such as the pelvis vertical velocity, slip distance, slip velocity, and trunk angle were used to estimate the fall severity in previous studies.7, 17, 29, 30 Yet, none has ever quantified the risk of injury between feet-forward and split falls with respective to their estimated impact velocity.
The purposes of this study were to investigate whether the recovery foot placement would determine the slip types, the likelihood of fall, and the severity of fall represented using the impact velocity of body parts and trunk orientation upon fall arrest. The greater hip or hand drop velocity prior to fall arrest (on the ground in real-life and by harness support in laboratory reproduction), the greater impact force this body segment will likely experience. These variables along with the loadcell value upon fall arrest were used to quantify the severity of a fall. We hypothesized that an anterior placement of the recovery foot relative to COM would likely cause feet-forward slip, whereas a posterior placement would lead to split slip (Hypothesis 1). Because feet-forward slip appeared less stable, we hypothesized it would lead to higher likelihood of falls in comparison to split slip (Hypothesis 2). Finally, since the spring-like action associated with split falls would likely cushion and slowdown the hip descending, we hypothesized that the split fallers would have slower hip or arm drop vertical velocity than feet-forward fallers at the time of harness arrest (Hypothesis 3).
Methods
Subjects
195 community-dwelling older adults (≥65 years) participated in this study (age: 72.3 ± 5.3 years; height: 165.5 ± 8.8 cm; mass: 75.5 ± 14.1 kg). All participants were screened via questionnaire before their training sessions to exclude neurologic, musculoskeletal, cardiopulmonary, and any other systemic disorders. All participants provided written informed consent, approved by the Institutional Review Board in the University of Illinois at Chicago.
Experimental setup
The slip was induced by releasing a pair of side-by-side, low-friction, movable platforms embedded near the middle of a 7-meter walkway. The platforms were firmly locked in first ten walking trials. During the slip trial, it could slide freely in the anteroposterior (AP) direction for up to 90 cm forward or 58 cm backward. Once a subject’s right (slipping) foot was detected in contact with the right platform by the force plates (AMTI, Newton, MA) installed beneath the platforms,24 a computer controlled triggering mechanism would release the platform. The left platform was automatically released after the left (recovery) foot landed on it. All subjects experienced at least two slips, only the novel (first) slip trial was analyzed in this study.
The subjects wore their own athletic shoes and a full-body safety harness connected with shock-absorbing ropes to a loadcell (Transcell Technology Inc., Buffalo Grove, IL) mounted on an overhead trolley on a track over the walkway, enabled subjects to walk freely while providing protection against body impact with the floor surface. Kinematics of a full body marker set of 28 retro-reflective markers were recorded by an eight-camera motion capture system (Motion Analysis Corporation, Santa Rosa, CA). Kinematic data were sampled at 120 Hz and synchronized with the force plate and loadcell data, which were collected at 600 Hz.
Outcome variables
The foot position relative to COM was calculated by subtracting COM position from the toe (head of 1st metatarsal) position of the recovery foot in AP direction. The toe position was estimated based on the position of heel, ankle, 5th metatarsal, foot length, foot width and heel width using a foot model43. The initial contact area of the recovery foot was always around the toe in this study. The deceleration time of the recovery (left) foot after its touchdown (left touchdown, LTD) was between 50–80 ms, which was consistent with previous study.37 Thus, the foot position relative to COM in landing was taken at 80 ms after LTD. The events of step time used in this study, including left foot liftoff (LLO) and LTD, were all detected from force plate data.
The COM state (that is, its position and velocity relative to base of support (BOS)) was used to measure a person’s instantaneous dynamic stability.22 BOS represents the area beneath a person encircled by the points of contact that the person’s foot or feet make(s) with the supporting surface. First, body COM kinematics were calculated using a 13-segment rigid body model with gender-dependent segmental inertial parameters.6 Then the relative position and velocity of COM/BOS were calculated using the motion state of the rear edge of BOS (the right heel) as reference. The relative COM position was normalized by foot length (FL), and the relative velocity was normalized by the quantity , where g is the gravitational acceleration and BH represents the body height. Finally, the COM state stability was computed as the shortest distance from the COM motion state to the dynamic feasible stability boundary against backward loss of balance under slip conditions.
Fall and recovery were two outcomes of a slip. A fall was identified as if the peak loadcell force during a slip exceeded 30% body weight (BW).44 A recovery was identified as if the moving average loadcell force over any 1-second period did not exceed 4.5% BW. The other condition was labeled as harness-assisted trial and not included in this study. The loadcell force reflected the pull force participants relied on the harness, which prevented the body from contacting the ground. Thus, the peak loadcell force was used to compare the fall severity in this study.
The hip impact velocity was projected based on the height, vertical velocity and acceleration of the mid-point of the left and right greater trochanters measured upon the instant of harness-fall-arrest:
| (1) |
Here v indicated the estimated hip impact velocity when the hip crashed on the ground. v0 and a indicated the measured hip drop vertical velocity and acceleration on the instant of harness-fall-arrest separately. Assuming the hip would keep the same acceleration without the harness arrest, the hip drop duration after harness arrest would be:
| (2) |
Combining equations (1) and (2) above, the estimated hip impact velocity would be:
| (3) |
The wrist (arm) impact velocity was calculated using the same method with hip impact velocity. The wrist (right or left) with lower distance to the ground upon the instant of harness-fall-arrest was used to calculate the wrist impact velocity. Both impact velocities were normalized by the body height. The trunk angle was measured at the same instant as the angle between the trunk segment (the line from the greater trochanter midpoint to shoulder midpoint) and vertical axis in the counterclockwise direction. The peak slip velocity was defined as the maximum velocity of the movable platform in AP direction after LTD.
Slip type identification
The foot distance was calculated by subtracting the heel position of recovery foot from the heel position of slipping foot in AP direction. The maximum foot distance after LTD was used for slip type identification. 0.43 × BH obtained from cluster analysis in our previous study was used as criteria of foot distance to separate slip types.42 The video record was used to verify the result. According to this result, 195 subjects were sorted into 4 groups: split fall group, feet-forward fall group, split recovery group and feet-forward recovery group.
Statistical analysis
Independent t-tests were performed to compare the age, body mass, body height and BMI between feet-forward and split slip groups. Chi-square test was used to examine the difference in gender and fall history (over 12 months before the experiment) between the two groups. To test Hypothesis 1, logistic regression determined the influence of the toe relative position at LTD + 80 ms on the slip types for fallers, recoveries and combination of them separately. Correlation analysis was used to test the relationship between the fall incidence and the maximum foot distance, and r was used to represent the correlation coefficient. To test Hypothesis 2, chi-square test was used to compare the fall incidence between the two slip types and independent t-test was used to compare the stability between the two slip types. To test Hypothesis 3, independent t-test was used to compare the fall severity between the two slip types. All statistical analysis was performed using SPSS 22 (IBM Corp, Armonk, NY). The p-values below 0.05 were considered statistically significant.
Results
All the subjects (N = 195) lost their balance in the backward direction on the novel slip. Among these, 105 (53.8%) subjects experienced feet-forward slips, while 90 (46.2%) subjects experienced split slips (Table 1). There was no slip-type-related difference in age, gender, body height and fall history (p > 0.05 for all). Subjects with feet-forward slips had significantly lower body weight and BMI (p<0.001 for both) in comparison to subjects with split slips (Table 2).
Table 1.
Distribution of slip types in 195 subjects during the gait slip test. If the recovery foot is moving forward together with the slipping foot (V > 0) after its landing, the slip is termed as Feet-forward slip, otherwise, if it is moving in the opposite direction after its landing (V ≦ 0), the slip is termed as split slip.
| Falls | Recoveries | Total | ||
|---|---|---|---|---|
| Feet-forward | Multi-step | 15 | 28 | 105 |
| Single-step | 35 | 27 | ||
| Split | Multi-step | 5 | 14 | 90 |
| Single-step | 56 | 15 |
Table 2.
Comparisons of the demographics and fall history in means ± SD between feet-forward and split slip groups. Independent t-test and chi-square test were used.
| Feet-forward (n=105) | Split (n=90) | P value | |
|---|---|---|---|
| Age (year) | 72.2 ± 5.4 | 72.4 ± 5.3 | >0.05 a |
| Male (%) | 36 | 24 | >0.05 b |
| Body mass (kg) | 72.0 ± 14.0 | 79.7 ± 13.0 | <0.001 a |
| Body height (cm) | 166 ± 9 | 164 ± 13 | >0.05 a |
| BMI (kg m−2) | 26.1 ± 4.7 | 29.4 ± 4.9 | <0.001 a |
| Fall history (%) | 35 | 33 | >0.05 b |
independent t-test
chi-square test
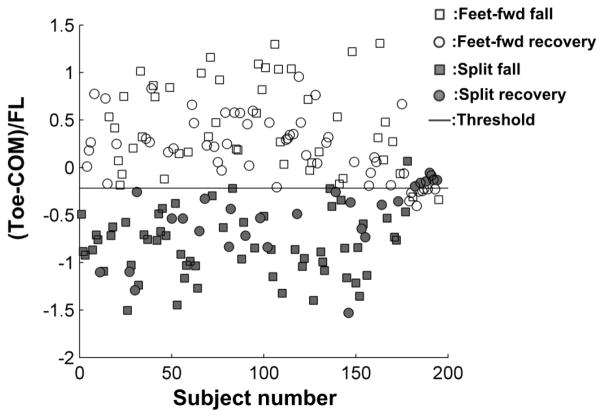
The recovery foot landing position relative to COM did determine the slip type (p < 0.001, Fig. 1). The threshold value that separated these two slips was close to the COM projection on the horizontal plane (0 in y axis, Fig. 1) with the recovery (left) toe landed posterior (negative) to the COM by 22% of the foot length (Fig. 1). If the recovery toe landed anterior to this point, a slip would have a 91.2% of chance to be a feet-forward slip, otherwise with a 90.4% of chance to be a split slip when the toe landed posterior to that point. The overall prediction accuracy was 90.8% (p < 0.001).
Figure 1.
Distribution of the recovery step position relative to COM at 80 ms after the recovery step touchdown for all 4 groups (Split falls: filled circles, feet-forward falls: filled squares, split recoveries: open circles, feet-forward recoveries: open squares). The distance between COM and recovery foot was normalized by the foot length (FL). The solid line indicates the threshold for slip type prediction.
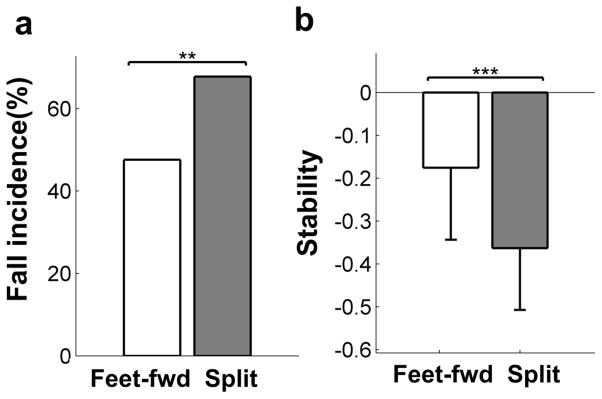
Subjects selected feet-forward slip showed significantly lower fall rate (47.6% vs 67.8%, p < 0.01, Fig. 2a) and higher reactive stability (stability at LLO) (−0.18 ± 0.17 vs −0.36 ± 0.14, p < 0.001, Fig. 2b) in comparison to subjects who made split slip.
Figure 2.
(a) Comparison of the fall incidence between the feet-forward slips and the split slips (included both the fall and recovery outcomes), chi-square test was performed on the fall incidence between the two slip types. (b) Comparison of the stability at LLO between the feet-forward slips and the split slips, an independent t-test was performed on stability between these two slip types. * indicates a significance level of p < 0.05, ** p < 0.01 and *** p < 0.001.
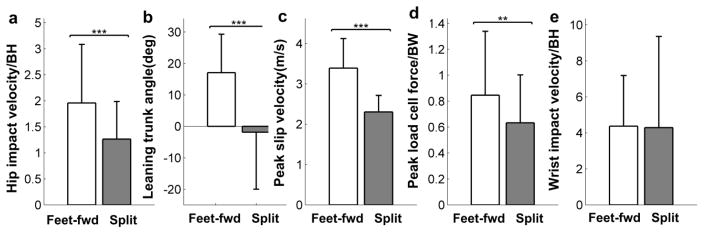
The feet-forward falls had significantly higher estimated hip impact velocity (1.96 ± 1.13 vs 1.26 ± 0.72 × BH, p < 0.001, Fig. 3a), greater backward leaning trunk angle (17.06 ± 12.23 vs −1.85 ± 18.11 degree, p < 0.001, Fig. 3b), higher peak slip velocity (3.45 ± 0.73 vs 2.33 ± 0.71 m s−1, p < 0.001, Fig. 3c), and higher peak loadcell force (87.99 ± 47.31 vs 63.34 ± 36.95 × BW, p < 0.01, Fig. 3d)than split falls. The measured hip height (p < 0.001) and acceleration (p < 0.05) upon the instant of harness-fall-arrest used for hip impact velocity estimation also had significant difference between the two groups (Table 3). No significant difference was found in the estimated wrist impact velocity between the two groups (p > 0.05, Fig. 3e).
Figure 3.
Comparison of (a) estimated hip impact velocity, (b) backward leaning trunk angle at the instant of harness-fall-arrest, (c) peak slip velocity after LTD, (d) peak loadcell force after LTD and (e) estimated wrist impact velocity between the feet-forward falls and the split falls. * p < 0.05, ** p < 0.01 and *** p < 0.001 for the independent t-tests performed.
Table 3.
The measured height, vertical velocity and vertical acceleration of hip and wrist upon the harness-fall-arrest instant used for hip and wrist impact velocity estimation. Independent t tests were performed to examine the difference between feet-forward and split falls.
| Height (m) | Velocity (m s−1) | Acceleration (m s−2) | ||
|---|---|---|---|---|
| Hip | Feet-forward | 0.40 ± 0.04 | −0.34 ± 0.23 | −2.60 ± 4.23 |
| Split | 0.36 ± 0.03 | −0.28 ± 0.20 | −0.94 ± 2.64 | |
| p value | p<0.001 | p>0.05 | P<0.05 | |
|
| ||||
| Wrist | Feet-forward | 0.47 ± 0.16 | −0.95 ± 0.63 | −4.41 ± 4.87 |
| Split | 0.37 ± 0.78 | −1.09 ± 2.41 | −4.02 ± 4.43 | |
| p value | p>0.05 | p>0.05 | p>0.05 | |
Discussion
While all participants in this study experienced the same unannounced, novel slip during their walking, the landing locations of their recovery foot were highly variable. Interestingly, for all participants the odds of landing their foot (toe) anteriorly (relative to their COM) or landing posteriorly was about even. The landing location indeed determined (with 91% accuracy) two types of slip, a feet-forward or a split slip (Hypothesis 1). The feet-forward slips had significantly lower fall risk in comparison to the split slips, because the former tended to be more stable than the latter (Hypothesis 2). Yet, the severity of falls was much higher in the former, because it was associated with significantly higher hip impact velocity, greater trunk backward leaning angle and greater harness support around the time of harness arrest (Hypothesis 3).
Using the COM-COP relationship, the present study was one of the first to quantify the probability of slip types with high certainty. When the subjects took a shorter recovery step, their COP of the trailing foot would still remain posterior to the COM. Based on a bipedal inverted pendulum model during walking,39, 40 such landing would lead to a posterior GRF on the landing foot and add an anterior GRF in the slipping foot. That will accelerate the slipping foot while move the recovery foot in the opposite direction, resulting in a split slip. On the other hand, when the COP of the trailing foot located anterior to the COM, it would require a backward directed friction just as that required in regular walking. When the floor surface cannot meet this demand to brake for forward momentum carried from the landing of the trailing foot, the foot will keep moving forward, resulting in a feet-forward slip.
Still there are approximately 9% of exceptions to this reasoning. In all of those cases, the landing position was very close to the COM. The direction of the impulsive force could be interchangeable as the COP could shift quickly upon the recovery foot landing position, while the magnitudes of the pressure and the friction were very small.10 The signal and noise ratio at the time may be very unfavorable for accurate prediction due to the limitation in the temporal resolution of the measurement systems. While there is evidence that stability has a strong negative correlation with body weight and those with a higher BMI are more likely to fall,13, 27, 45 this is the first evidence that interestingly, higher body mass and BMI also are more likely to result in split slip (p < 0.001, Table 2). It is reasonable to postulate that higher BMI reduces stability which forces this person to have a very quick landing, and leaves foot further behind, hence results in split slip. Given the importance of understanding the causation of obesity, falls and the likelihood of ensuing injuries, this possibility warrants further examination.
To our surprise, in comparison to the feet-forward slip, the split slip was more likely to result in a fall. The split slip was associated with significantly lower stability at LLO in comparison to the feet-forward slip (p < 0.001, Fig. 3a). The higher likelihood of falls in the split slip could be attributable to the less stability at LLO.41 Another factor could be that it is difficult to take multiple recovery steps with the split slip when stability is not fully recovered after the first step. Only 21.1 % of the split slips were multi-step slips versus 41.0 % in the feet-forward slips (Table 1). Effective multiple recovery steps could also contribute to a higher recovery success rate in the feet-forward slips.12 In this connection, our results indicated that 68.4 % of the single-step slips turned out to be falls, while only 32.3 % of the multi-step slips ended up with falls.
The higher hip impact velocity among the feet-forward fallers in comparison to the split fallers can be contributable to their significantly faster slip velocity coupled with greater backward trunk leaning. These differences led to a greater demand for support from the harness to prevent the body from hitting the floor. The moment created by the gravitational force and GRF can be magnified in the feet-forward slips, causing the faster backward rotation of the whole body. In contrast, these external forces were better balanced during the split slips with the COM centered between the GRF from both feet. With less angular momentum, the GRF could better damp the hip impact velocity in the split falls in comparison to the feet-forward falls. In addition, there could be a damping effect resulted from passive elastic joint moment from stretching the hip joints during the split slip.28 While a higher hip impact velocity increases the risk of hip fracture, a greater backward trunk excursion and a high angular momentum are other critical factors affecting the severity of fall.29 In this case, the potential energy loss during a fall can increase the kinetic energy prior to the impact31 and hence increase the risk of traumatic head injury upon impact.29 Apparently, these considerations are essential not only to physical rehabilitation but also to forensic science. For the first time, we now can rather precisely determine from the location of a protective step touchdown, which can be provided by the image or video recording of any kind, to the outcome severity of a fall, if that happens. Our findings could also be applied to assess the success of a fall-reduction training program, following which older adults’ protective stepping landing is expected to reduce the danger of serious injuries. This piece of information could be enormously valuable for forensic biomechanist when his/her role is to determine the causation of injury in a legal dispute.
Finally, it is an intriguing question as to the role of the central nervous system in determining the outcome of slip recovery. Does it have the opportunity to consciously decide the landing location of the recovery foot placement? Or, is the foot placement subconsciously governed in part driven by subconscious, automatic feedback of the COM instability prior to its touchdown? In the latter case, a tight correlation should be expected between the foot placement and the instability. It is quite likely that in this unannounced and novel slip, the feedforward mechanism does not control the recovery foot placement. The reaction (touchdown 300 ms after slip onset) in fact requires the modification of the ongoing feedforward control of the stepping in gait.35, 38 The landing is most likely governed by the reactive control via an automatic postural response, involving various subcortical or even cortical motor centers.14 Training in the reactive placement of the recovery foot, therefore, may require different approaches from those that only involve volitional footwork in feedforward control.1, 11
In summary, this study revealed that the recovery foot placement determines the type of slip following its touch – down either a feet-forward slip or a split slip. Older adults who experienced the feet-forward slip had a greater chance to recover. Yet, those who fell during this type of the slip would have a higher hip impact velocity and greater backward trunk inclination, likely associated with a higher kinetic energy upon impact, and hence a greater risk of fracture or traumatic injury – on the hip or the head.
Acknowledgments
This work was funded by NIH RO1-AG029616 and NIH R01-AG044364.
Footnotes
Conflict of interest
None.
References
- 1.Bastian AJ. Learning to predict the future: the cerebellum adapts feedforward movement control. Current Opinion in Neurobiology. 2006;16:645–649. doi: 10.1016/j.conb.2006.08.016. [DOI] [PubMed] [Google Scholar]
- 2.Bhatt T, Wening JD, Pai YC. Adaptive control of gait stability in reducing slip-related backward loss of balance. Experimental Brain Research. 2006;170:61–73. doi: 10.1007/s00221-005-0189-5. [DOI] [PubMed] [Google Scholar]
- 3.Bhatt T, Wening JD, Pai YC. Influence of gait speed on stability: recovery from anterior slips and compensatory stepping. Gait & Posture. 2005;21:146–156. doi: 10.1016/j.gaitpost.2004.01.008. [DOI] [PubMed] [Google Scholar]
- 4.Cham R, Redfern MS. Changes in gait when anticipating slippery floors. Gait & Posture. 2002;15:159–171. doi: 10.1016/s0966-6362(01)00150-3. [DOI] [PubMed] [Google Scholar]
- 5.Cody DD, Hou FJ, Divine GW, Fyhrie DP. Femoral structure and stiffness in patients with femoral neck fracture. Journal of Orthopaedic Research. 2000;18:443–448. doi: 10.1002/jor.1100180317. [DOI] [PubMed] [Google Scholar]
- 6.de Leva P. Adjustments to Zatsiorsky-Seluyanov’s segment inertia parameters. Journal of Biomechanics. 1996;29:1223–1230. doi: 10.1016/0021-9290(95)00178-6. [DOI] [PubMed] [Google Scholar]
- 7.DeGoede KM, Ashton-Miller JA. Fall arrest strategy affects peak hand impact force in a forward fall. Journal of Biomechanics. 2002;35:843–848. doi: 10.1016/s0021-9290(02)00011-8. [DOI] [PubMed] [Google Scholar]
- 8.Donald IP, Bulpitt CJ. The prognosis of falls in elderly people living at home. Age and Ageing. 1999;28:121–125. doi: 10.1093/ageing/28.2.121. [DOI] [PubMed] [Google Scholar]
- 9.Espy DD, Yang F, Bhatt T, Pai YC. Independent influence of gait speed and step length on stability and fall risk. Gait & Posture. 2010;32:378–382. doi: 10.1016/j.gaitpost.2010.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gruben KG, Boehm WL. Ankle torque control that shifts the center of pressure from heel to toe contributes non-zero sagittal plane angular momentum during human walking. Journal of Biomechanics. 2014;47:1389–1394. doi: 10.1016/j.jbiomech.2014.01.034. [DOI] [PubMed] [Google Scholar]
- 11.Hohne A, Stark C, Bruggemann GP, Arampatzis A. Effects of reduced plantar cutaneous afferent feedback on locomotor adjustments in dynamic stability during perturbed walking. Journal of Biomechanics. 2011;44:2194–2200. doi: 10.1016/j.jbiomech.2011.06.012. [DOI] [PubMed] [Google Scholar]
- 12.Hsiao ET, Robinovitch SN. Elderly subjects’ ability to recover balance with a single backward step associates with body configuration at step contact. Journals of Gerontology Series a-Biological Sciences and Medical Sciences. 2001;56:M42–M47. doi: 10.1093/gerona/56.1.m42. [DOI] [PubMed] [Google Scholar]
- 13.Hue O, Simoneau M, Marcotte J, Berrigan F, Dore J, Marceau P, Marceau S, Tremblay A, Teasdale N. Body weight is a strong predictor of postural stability. Gait & Posture. 2007;26:32–38. doi: 10.1016/j.gaitpost.2006.07.005. [DOI] [PubMed] [Google Scholar]
- 14.Jacobs J, Horak F. Cortical control of postural responses. Journal of neural transmission. 2007;114:1339–1348. doi: 10.1007/s00702-007-0657-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jobges M, Heuschkel G, Pretzel C, Illhardt C, Renner C, Hummelsheim H. Repetitive training of compensatory steps: a therapeutic approach for postural instability in Parkinson’s disease. Journal of Neurology Neurosurgery and Psychiatry. 2004;75:1682–1687. doi: 10.1136/jnnp.2003.016550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Keyak JH, Skinner HB, Fleming JA. Effect of force direction on femoral fracture load for two types of loading conditions. Journal of Orthopaedic Research. 2001;19:539–544. doi: 10.1016/S0736-0266(00)00046-2. [DOI] [PubMed] [Google Scholar]
- 17.Lockhart TE, Smith JL, Woldstad JC. Effects of aging on the biomechanics of slips and falls. Human Factors. 2005;47:708–729. doi: 10.1518/001872005775571014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mcilroy WE, Maki BE. Changes in Early Automatic Postural Responses Associated with the Prior-Planning and Execution of a Compensatory Step. Brain Research. 1993;631:203–211. doi: 10.1016/0006-8993(93)91536-2. [DOI] [PubMed] [Google Scholar]
- 19.Mille ML, Johnson ME, Martinez KM, Rogers MW. Age-dependent differences in lateral balance recovery through protective stepping. Clinical Biomechanics. 2005;20:607–616. doi: 10.1016/j.clinbiomech.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 20.Moyer BE, Redfern MS, Cham R. Biomechanics of trailing leg response to slipping - Evidence of interlimb and intralimb coordination. Gait & Posture. 2009;29:565–570. doi: 10.1016/j.gaitpost.2008.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Norton R, Campbell AJ, LeeJoe T, Robinson E, Butler M. Circumstances of falls resulting in hip fractures among older people. Journal of the American Geriatrics Society. 1997;45:1108–1112. doi: 10.1111/j.1532-5415.1997.tb05975.x. [DOI] [PubMed] [Google Scholar]
- 22.Pai YC, Patton JL. Center of mass velocity-position predictions for balance control. Journal of Biomechanics. 1997;30:347–354. doi: 10.1016/s0021-9290(96)00165-0. [DOI] [PubMed] [Google Scholar]
- 23.Pai YC, Rogers MW, Patton J, Cain TD, Hanke TA. Static versus dynamic predictions of protective stepping following waist-pull perturbations in young and older adults. Journal of Biomechanics. 1998;31:1111–1118. doi: 10.1016/s0021-9290(98)00124-9. [DOI] [PubMed] [Google Scholar]
- 24.Pai YC, Yang F, Bhatt T, Wang E. Learning from laboratory-induced falling: long-term motor retention among older adults. Age. 2014;36:1367–1376. doi: 10.1007/s11357-014-9640-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Patla AE, Adkin A, Ballard T. Online steering: coordination and control of body center of mass, head and body reorientation. Experimental Brain Research. 1999;129:629–634. doi: 10.1007/s002210050932. [DOI] [PubMed] [Google Scholar]
- 26.Redfern MS, Cham R, Gielo-Perczak K, Gronqvist R, Hirvonen M, Lanshammar H, Marpet M, Pai CYC, Powers C. Biomechanics of slips. Ergonomics. 2001;44:1138–1166. doi: 10.1080/00140130110085547. [DOI] [PubMed] [Google Scholar]
- 27.Ren J, Waclawczyk A, Hartfield D, Yu SC, Kuang XY, Zhang HR, Alamgir H. Analysis of Fall Injuries by Body Mass Index. Southern Medical Journal. 2014;107:294–300. doi: 10.1097/SMJ.0000000000000097. [DOI] [PubMed] [Google Scholar]
- 28.Riener R, Edrich T. Identification of passive elastic joint moments in the lower extremities. Journal of Biomechanics. 1999;32:539–544. doi: 10.1016/s0021-9290(99)00009-3. [DOI] [PubMed] [Google Scholar]
- 29.Robinovitch SN, Brumer R, Maurer J. Effect of the “squat protective response” on impact velocity during backward falls. Journal of Biomechanics. 2004;37:1329–1337. doi: 10.1016/j.jbiomech.2003.12.015. [DOI] [PubMed] [Google Scholar]
- 30.Robinovitch SN, Inkster L, Maurer J, Warnick B. Strategies for avoiding hip impact during sideways falls. Journal of Bone and Mineral Research. 2003;18:1267–1273. doi: 10.1359/jbmr.2003.18.7.1267. [DOI] [PubMed] [Google Scholar]
- 31.Sandler R, Robinovitch S. An analysis of the effect of lower extremity strength on impact severity during a backward fall. Journal of Biomechanical Engineering-Transactions of the Asme. 2001;123:590–598. doi: 10.1115/1.1408940. [DOI] [PubMed] [Google Scholar]
- 32.Schulz BW, Ashton-Miller JA, Alexander NB. Compensatory stepping in response to waist pulls in balance-impaired and unimpaired women. Gait & Posture. 2005;22:198–209. doi: 10.1016/j.gaitpost.2004.09.004. [DOI] [PubMed] [Google Scholar]
- 33.Smeesters C, Hayes WC, McMahon TA. Determining fall direction and impact location for various disturbances and gait speeds using the articulated total body model. Journal of Biomechanical Engineering-Transactions of the Asme. 2007;129:393–399. doi: 10.1115/1.2737432. [DOI] [PubMed] [Google Scholar]
- 34.Stevens JA, Sogolow ED. Gender differences for non-fatal unintentional fall related injuries among older adults. Injury Prevention. 2005;11:115–119. doi: 10.1136/ip.2004.005835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tang PF, Woollacott MH, Chong RKY. Control of reactive balance adjustments in perturbed human walking: roles of proximal and distal postural muscle activity. Experimental Brain Research. 1998;119:141–152. doi: 10.1007/s002210050327. [DOI] [PubMed] [Google Scholar]
- 36.van den Bogert AJ, Pavol MJ, Grabiner MD. Response time is more important than walking speed for the ability of older adults to avoid a fall after a trip. Journal of Biomechanics. 2002;35:199–205. doi: 10.1016/s0021-9290(01)00198-1. [DOI] [PubMed] [Google Scholar]
- 37.Winter DA, Patla AE, Frank JS, Walt SE. Biomechanical Walking Pattern Changes in the Fit and Healthy Elderly. Physical Therapy. 1990;70:340–347. doi: 10.1093/ptj/70.6.340. [DOI] [PubMed] [Google Scholar]
- 38.Woollacott MH, Tang PF. Balance control during walking in the older adult: Research and its implications. Physical Therapy. 1997;77:646–660. doi: 10.1093/ptj/77.6.646. [DOI] [PubMed] [Google Scholar]
- 39.Yamaguchi T, Hokkirigawa K. Experimental analysis of slip potential in Normal-style walking and Nanba-style walking. Journal of Biomechanical Science and Engineering. 2009;4:468–479. [Google Scholar]
- 40.Yamaguchi T, Masani K. Contribution of center of mass–center of pressure angle tangent to the required coefficient of friction in the sagittal plane during straight walking. Biotribology. 2016;5:16–22. [Google Scholar]
- 41.Yang F, Bhatt T, Pai YC. Role of stability and limb support in recovery against a fall following a novel slip induced in different daily activities. Journal of Biomechanics. 2009;42:1903–1908. doi: 10.1016/j.jbiomech.2009.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yang F, Espy D, Bhatt T, Pai YC. Two types of slip-induced falls among community dwelling older adults. Journal of Biomechanics. 2012;45:1259–1264. doi: 10.1016/j.jbiomech.2012.01.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yang F, Espy D, Pai YC. Feasible Stability Region in the Frontal Plane During Human Gait. Annals of Biomedical Engineering. 2009;37:2606–2614. doi: 10.1007/s10439-009-9798-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yang F, Pai YC. Automatic recognition of falls in gait-slip training: Harness load cell based criteria. Journal of Biomechanics. 2011;44:2243–2249. doi: 10.1016/j.jbiomech.2011.05.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhang MZ, Yang F, Wang E, Pai YC. Association between Anthropometric Factors and Falls in Community-Dwelling Older Adults during a Simulated Slip While Walking. Journal of the American Geriatrics Society. 2014;62:1808–1810. doi: 10.1111/jgs.13016. [DOI] [PubMed] [Google Scholar]
- 46.Zijlstra GAR, van Haastregt JCM, van Rossum E, van Eijk JTM, Yardley L, Kempen GIJM. Interventions to reduce fear of falling in community-living older people: A systematic review. Journal of the American Geriatrics Society. 2007;55:603–615. doi: 10.1111/j.1532-5415.2007.01148.x. [DOI] [PubMed] [Google Scholar]