Abstract
Temperamental negative affect and insufficient sleep have been independently associated with behavior problems during early childhood. However, it unknown whether these factors interact to contribute to behavioral difficulties in young children. The current study examined the interactions between temperamental negative affect and both sleep onset time and sleep midpoint, assessed by actigraphy, in predicting externalizing and internalizing behaviors in a sample of 117 children (34 to 69 months of age). Children with high temperamental negative affect and either later sleep onset time or later sleep midpoint were more likely to exhibit externalizing and internalizing behaviors. These results emphasize the association between temperamental negative affect and behavioral difficulties, particularly for children with insufficient sleep.
Keywords: temperamental negative affect, sleep, externalizing, internalizing, early childhood
Temperamental negative affect is a distinct temperament dimension commonly associated with heightened rates of externalizing and internalizing problems (Garstein, Putnam, & Rothbart, 2012). Marked by the propensity to react to stressors with high levels of negative emotionality, temperamental negative affect is characterized by a constellation of high discomfort, fear, anger/frustration, aggression, sadness, and low soothability (Rothbart, Ahadi, Hershey, & Fisher, 2001). Because assessments of temperamental negative affect focus on negative affectivity and probe elements that are related to both approach and avoidance motivation systems (Gray, 1991), this broad dimension of temperament uniquely poses risks for maladaptive behavior problems across development (Henderson & Wachs, 2007).
Importantly, a growing body of research suggests that the association between temperamental negative affect and behavioral problems may be exacerbated or ameliorated, depending on salient factors early in development. Sleep, which undergoes rapid changes in early childhood, may be particularly relevant to understanding the rise and persistence of poor behavioral outcomes. During this developmental period, from 2 to 5 years of age, preschool enrollment typically motivates the institution of regimented sleep and wake schedules to prepare for the often early (7-8 a.m.) start of the preschool day. Additionally, sleep onset time is particularly irregular during early childhood (Beltramini & Hertzig, 1983; Fisher & McGuire, 1990). Like temperamental negative affect, insufficient sleep has been associated with externalizing and internalizing problems (Yokomaku et al., 2008; LeBourgeois et al., 2013a). Insufficient sleep is measured by late sleep onset time and late sleep midpoint (which is the point in time halfway between sleep onset and sleep offset). As the preschool years are a time in which behavior problems are common (e.g., Gillion & Shaw, 2004), it is particularly important to evaluate the prevalence and consequence of insufficient sleep in this population and determine whether sleep parameters and temperament interact to moderate risk for maladaptive outcomes.
Temperamental Negative Affect and Behavioral Outcomes
A substantial body of research has linked high levels of temperamental negative affect with maladaptive outcomes such as externalizing and internalizing behaviors. Externalizing problems are prevalent in early childhood and generally manifest in the form of attention problems or aggression issues. Also commonly occurring in childhood, but less frequently reported as problematic in young children, are internalizing problems that reflect internal distress such as anxiety or depression (Achenbach & Ruffle, 2000; Tandon, Cardeli & Luby, 2009). Although multiple factors may influence risk for maladaptive outcomes among children, longitudinal work suggests that children high in negative affectivity during infancy and toddlerhood have an increased risk of externalizing and internalizing problems during the preschool years (Garstein et al., 2012). Concurrent connections between negative affectivity and maladaptive outcomes have also been found among young children (Gilliom & Shaw, 2004) as well as heightened risk for externalizing and/or internalizing problems throughout development (Lipscomb et al., 2012; Vitaro, Barker, Boivin, Bredgen, & Tremblay, 2006).
Theoretical work further suggests that early negative affectivity can foreshadow later forms of psychopathology (Frick & Morris, 2004) and evidence of this association has emerged in respect to both externalizing (Eisenberg et al., 2009) and internalizing problems (Leve, Kim, & Pears, 2005). Recently, Olino and colleagues (2014) have explored the structure of psychopathology in preschool-aged children and found a common latent vulnerability to both internalizing and externalizing problems. Similarly, a cross-sectional study of psychopathology in a broader age range of children (2 to 18 years of age) supports the proposal that combined aspects of emotional and behavioral regulation, both of which are associated with temperamental negative affect, contribute to the co-occurrence of internalizing and externalizing symptoms in childhood and adolescence (Slobodskaya, 2014). This work is consistent with other studies that have shown that high levels of temperamental negative affect can correspond to a wide range of developmental trajectories that include externalizing and internalizing outcomes.
However, not all children who display high levels of temperamental negative affect develop maladaptive outcomes. Accumulating evidence suggests that during early childhood, negative affectivity interacts with environmental factors to shape vulnerability to externalizing and internalizing behaviors (Rothbart & Bates, 2006; Shaw, Owens, Giovannelli, & Winslow, 2001). Parenting quality is one moderator of risk for externalizing and internalizing outcomes, particularly among children high in temperamental negative affect (e.g., Putnam, Sanson, & Rothbart, 2002). However, less is known of how other aspects of the child's experience may interact with temperamental characteristics to impact risk for behavior problems. Previous work examining increased vulnerability to behavior problems among children highlights insufficient sleep as a key risk factor (see Dahl, 1996 for review). Specifically, children with shorter sleep duration and later sleep onset times display more maladaptive behaviors (e.g., externalizing and internalizing problems) relative to those with longer sleep duration and earlier sleep onset times (Nixon et al., 2008; Yokomaku et al., 2008). Moreover, a number of studies show that insufficient sleep is associated with dampening of cognitive functions involved in self-regulation (Kurdziel, Duclos, & Spencer, 2013; Miller, Seifer, Crossin, & LeBourgeois, 2015). As sleep problems are common during early childhood (Beltramini & Hertzig, 1983; Fisher & McGuire, 1990), the presence and severity of sleep deficits may underlie behavior problems that emerge at critical stages of early development. Moreover, given the pervasive nature of early childhood behavior problems, along with the developmental changes in sleep patterns during this period, it is essential to better understand how sleep contributes to outcomes for young children with temperamental vulnerabilities to behavioral issues. A more thorough understanding of these factors has important implications for development of targeted interventions.
Sleep as a Moderator of Behavioral Outcomes
Emerging work suggests that insufficient sleep during early childhood may have a lasting impact on trajectories of behavioral outcomes throughout development. For instance, among infants characterized as high in resistance to control (a temperament dimension that incorporates aspects of negative affectivity), higher rates of sleep problems were predictive of growth in externalizing behaviors from early to middle childhood (5-9 years of age; Goodnight, Bates, Staples, Pettit, & Dodge, 2007). Though this study suggests a positive association between insufficient sleep and externalizing behaviors for children of specific temperaments, it is unclear how concurrent associations between temperament, sleep, and behavior interact, particularly during early childhood, when externalizing and internalizing behaviors are prevalent (e.g., Gilliom & Shaw, 2004). Additionally, Goodnight's (2007) measure of sleep sufficiency was based on a broad assessment of sleep difficulties (“overtired,” “trouble sleeping,” and “sleeps less than most children”) through caregiver reports, which are not as accurate as objective sleep measures such as actigraphy (Dayyat, Spruyt, Molfese, & Gozal, 2011; Gregory & Sadeh, 2012).
Counter to the limitations of subjective assessment of sleep, actigraphy enables accurate estimation of sleep parameters such as sleep duration, sleep onset time, and sleep midpoint (Acebo et al., 2005; LeBourgeois et al., 2013a). Late sleep onset time, or the transition from wakefulness to sleep, has been associated with short sleep duration (Kohyama, Shiiki, & Hasegawa, 2000), which, in turn, has been linked to a variety of externalizing and internalizing problems throughout early childhood. Among school-aged children (approximately 7 years of age), sleep duration was significantly shorter when bedtime was after 9:00 PM (Nixon et al., 2008). Moreover, short sleep duration was associated with high emotional lability according to caregiver report. Bedtime has also been positively correlated with aggressive, withdrawn, and anxious/depressed behaviors as well as internalizing behaviors in children 4 to 6 years of age (Yokomaku et al., 2008). Similarly, late sleep midpoint, a marker of circadian phase, has been linked to internalizing behaviors (i.e., anxiety) in young adults (Pace-Schott et al., 2015). Taken together, these studies suggest that sleep parameters indicative of sleep timing (i.e., sleep onset time and sleep midpoint) may be related to the emergence of behavior problems throughout development. Whether or not associations between sleep timing and behavior vary between children with distinct temperament characteristics warrants further research as sleep difficulties may exacerbate temperamental vulnerabilities to behavioral problems.
Current Study
Given the associations between sleep and behavioral outcomes throughout development, the purpose of this study was to evaluate the relations between temperamental negative affect, sleep timing (i.e., sleep onset and sleep midpoint), and their potential interactive contributions to behavioral outcomes during early childhood. If sleep onset and midpoint interact with negative affectivity to predict such outcomes, these variables can be targeted (e.g., via behavioral intervention) to reduce the risk of maladaptive behaviors in temperamentally vulnerable children.
In conjunction with parent-reported measures of temperament and behavior, we used an objective measure of sleep (actigraphy) to evaluate measures of sleep timing, sleep onset time and sleep midpoint, as well as sleep duration. We posited that sleep onset time is an important environmental factor that moderates the relation between temperamental negative affect and behavior problems during early childhood, a developmental period during which sleep onset time is particularly irregular (Beltramini & Hertzig, 1983; Fisher & McGuire, 1990). Likewise, we hypothesized that sleep midpoint, an index of circadian phase, would moderate the association between temperamental negative affect and behavior problems in young children. Finally, as research in adults suggests that disruption to the circadian phase (reflected in measures of sleep timing) confers risk for maladaptive outcomes that is not ameliorated by sleep length (e.g., Genzel et al., 2013; Haus & Smolensky, 2006), we hypothesized that sleep duration would not influence associations between temperament and behavior.
Regarding specific behaviors within the externalizing and internalizing domains, we hypothesized the association between temperamental negative affect and sleep onset time would be strongest for externalizing behaviors previously associated with negative emotionality (Garstein et al., 2012). Alternatively, delayed sleep onset may confer greater risk for internalizing behaviors among children high in temperamental negative affect, as young children with later bedtimes have been reported to have more internalizing problems than those with earlier bedtimes (Yokomaku et al., 2008). Consistent with work in young adults, we predicted the association between temperamental negative affect and sleep midpoint would be strongest for internalizing behaviors (Pace-Schott et al., 2015).
Methods
Participants
Children were recruited from preschools in western Massachusetts as part of a larger study. Children were eligible to participate if they were 33 to 71 months of age and had normal or corrected-to-normal vision. Exclusion criteria included caregiver reported diagnosis of parasomnias or other sleep disorders, developmental disabilities, or use of medications affecting sleep or arousal. Data were collected between October 2012 and July 2014.
Caregivers of 185 children (96 females, M age = 52.44 months, SD = 9.49 months) completed questionnaires on child behavior and temperament. Of these, 127 children (62 females, M age = 53.49 months, SD = 9.01 months) had usable actigraphy data for at least three weekdays. A subset of children had available information pertaining to household income. Thus, the final sample included 117 children (58 females, M age = 52.96 months, SD = 8.85 months). Caregiver report indicated that 51.3% of children were white/Caucasian, 11.1% black/African American, 1.7% American Indian/Alaskan Native, 0.9% Asian Indian, 1.7% Chinese, 2.6% Vietnamese, 0.9% Other, Pacific Islander, 16.2% multiracial, and 2.6% identified as ‘other’.
Of the caregivers who completed questionnaires included in our analyses, 55.6% of caregivers were white/Caucasian, 8.5% were black/African American, 2.6% American Indian/Alaskan Native, 2.6% Asian Indian, 0.9% Chinese, 3.4% Vietnamese, 10.3% were multiracial, and 2.6% identified as ‘other’. For household income, 4.3% reported an annual household income of $5,000 or less, 8.5% between $5,001 to $10,000/year, 16.2% $10,001 to $20,000/year, 26.5% $20,001 to $40,000/year, 9.4% $40,001 to $70,000/year, 12.8% $70,001 to $100,000/year, 13.7% $100,001 to $150,000/year, and 8.5% reported more than $150,000/year. Of these caregivers, 2.6% reported education less than 12th grade, 10.3% completed high school (or received a GED), 23.1% enrolled in college, 13.7% earned an Associate's Degree, 17.1% earned a Bachelor's Degree, and 33.3% earned either a Master's Degree or Doctorate.
The number of weeknights (maximum possible = 9) with usable actigraphy data for children in the final sample ranged from 3-9 nights and averaged 7 nights (M = 7.23, SD = 1.75). Specifically, 28.2% had 9 nights of usable data, 27.4% had 8 nights, 17.9% had 7 nights, 8.5% had 6 nights, 6.0% had 5 nights, 7.7% had 4 nights, and 4.3% had 3 nights.
Measures
Children's Behavior Questionnaire (CBQ)
The CBQ assesses of emotional reactivity in young children and provides reliable measures of temperament on three broad scales: surgency, negative affect, and effortful control (α = 0.75, 0.72, and 0.74, respectively; Putnam & Rothbart, 2006). We used an abbreviated form of the CBQ (i.e., CBQ-Very Short Form), comprised of 36 questions. For each question, caregivers rated the level of reactivity his or her child would have in a particular situation on a 7-point likert scale (Extremely Not True (1), Quite Not True (2), Slightly Not True (3), Neither True Nor False (4), Slightly True (5), Quite True (6), Extremely True (7), or Not Applicable (NA)). The CBQ Very Short Form subscales have been significantly correlated with those reported by the full CBQ (r = 0.83, 0.75, and 0.83 for surgency, negative affect, and effortful control, respectively; Putnam & Rothbart, 2006).
Child Behavior Checklist for Ages 1.5-5 (CBCL)
The CBCL is an assessment of a child's emotional and behavioral problems (Achenbach & Ruffle, 2000). Caregivers rated the degree to which 100 statements reflected his or her child's typical behavior on a 3-point likert scale (Not True (0), Somewhat or Sometimes True (1), and Very True or Often True (2)). The CBCL has been demonstrated to be a reliable assessment (test-retest, α = 0.90) of emotional and behavioral problems in children 1.5 to 5 years of age (Achenbach & Rescorla, 2001).
Sleep Diary
During the 16-day testing protocol, caregivers recorded their child's sleep habits in a daily sleep diary logging naps, overnight sleep latency, sleep onset time, and morning awakening time each day. These logs were used to validate scoring of actigraphy data.
Actigraphy
An Actiwatch Spectrum (Spectrum 2; Philips Respironics, Bend, OR), a wrist-worn device with off-wrist detection and triaxial accelerometer, was used to estimate sleep (Acebo et al., 2005). Enrolled children were instructed to wear the Actiwatch on their non-dominant wrist continuously for the 16-day testing period. The Actiwatch sampled activity at 32 Hz, with a sensitivity of <0.01g and activity was stored in 15 second epochs. Actigraphy has been shown to be a reliable measure of sleep and wakefulness among developmental populations, with 94% agreement with videosomnography and exceptional sleep detection (sensitivity = 97%; Sitnick, Goodlin-Jones, & Anders, 2008). Moreover, the Philips Actiwatch used in this study has been demonstrated to be particularly sensitive to the detection of sleep onset time among preschool-aged children (Meltzer, Wash, & Peightal, 2015).
Procedure
All procedures were approved by the Institutional Review Board at the University of Massachusetts Amherst. Caregivers provided consent for their child's (wearing the Actiwatch) and their own (completing questionnaires) participation. Child assent was obtained before fitting the Actiwatch. On the first day of the protocol, the Actiwatch was placed on the child's non-dominant wrist. The caregiver and child were instructed to press an event marker on the Actiwatch to mark the ‘lights-out’ and ‘lights-on’ at the beginning and end of each sleep bout during the 16-day testing period. Caregivers were also provided instructions on Actiwatch use (e.g., wear continuously during the 16-day testing period, document times during which the Actiwatch was taken off-wrist). At the same time, caregivers were given the CBCL, CBQ, Sleep Diary, and an in-house demographic questionnaire to complete at any time during the 16-day period. Experimenters returned to the preschool frequently (approximately every other day) to check Actiwatches and answer questions regarding testing procedures. At the end of the 16-day period, the Actiwatches and questionnaires were retrieved and parents received monetary compensation for their time completing the surveys and children were given an age-appropriate book for their participation.
Data Analysis
Questionnaires
Items from the CBQ and CBCL were collapsed into subscales following standardized scoring procedures (Achenbach & Ruffle, 2000; Putnam & Rothbart, 2006, respectively). In creating these subscales, averages (across items used in each scale) were used in place of sum scores to account for item-missing data. In accordance with standard use of the CBCL in developmental research, raw scores were used in all statistical analyses (Achenbach & Rescorla, 2001). Higher scores on the negative affect scale (CBQ) represent greater child negative emotionality (e.g. fear, frustration, distress, and sadness), whereas higher scores on the CBCL scales (i.e., externalizing and internalizing broad scales as well as all subscales) represent a greater number of caregiver-reported child behavior problems.
Actigraphy
Segments of time when the Actiwatch was not worn (indicated either in the sleep diary or identified as off-wrist by the Actiwatch sensor) were excluded from analysis. If an excluded interval interfered with the scoring of an overnight sleep bout, data from that day was not included in analyses. Data from children with less than 3 weekdays of usable actigraphy data were not included in analyses based on previous work using the same, or less stringent, criteria (Nixon et al., 2008; Penpraze et al., 2006).
Actiware software (Philips Respironics, Bend, OR) was used to score actigraphy data. The overnight rest interval (i.e., the period of time the child was in bed) was defined as the longest sleep bout centered around midnight. Rest intervals were scored with reference to the event markers and caregiver sleep logs. Sleep onset time was set at the first of three consecutive minutes of sleep, and sleep offset (wake onset) was set at the last of five consecutive minutes of sleep (Acebo et al., 2005; LeBourgeois et al., 2013a,b). Sleep midpoint was defined as the point in time halfway between sleep onset and sleep offset (LeBourgeois et al., 2013a). Sleep duration was defined as the total minutes of sleep between night sleep onset and sleep offset.
As accumulating evidence highlights the importance of maintaining a consistent sleep schedule in order to promote efficient cognitive functioning throughout the school day (National Sleep Foundation, 2014), weekday data were of primary interest in the current study. Consistent with previous studies, weekend data (Friday-Sunday) were excluded, as weekend sleep schedules are potentially irregular and may not be representative of children's typical sleep patterns (e.g., Ward, Gay, Anders, Alkon, & Lee, 2008). Sunday was considered a weekend variable as sleep duration on Sunday evenings has been reported to be significantly longer than sleep durations reported on weekdays (e.g., Basner et al., 2007).
Statistical Analyses
Analyses were conducted in SPSS Version 21.0 (Armonk, NY, USA: IBM Corp). Only children with complete datasets (usable actigraphy data, completed CBQ, CBCL, and information regarding child age, gender, and household income) were included (N = 117). In preliminary analyses we screened for missing data patterns and univariate distributions of the variables were assessed to determine whether any model assumptions were violated (for the multilevel model and separate hierarchical linear regressions). We also examined partial correlations (controlling for child age and gender) between predictor and outcome variables.
Both sleep patterns and prevalence of behavior problems differ between males and females across development (e.g., Deater-Deckard, Dodge, Bates, & Pettit, 1998; El-Sheikh, Kelly, Buckhalt, & Hinnant, 2010). Accumulating evidence also suggests that sleep parameters differ between children of high and low socioeconomic status (Acebo et al., 2005; Biggs, Lushington, van den Heuvel, Martin, & Kennedy, 2011). As such, child age and gender (dichotomous variable, where 0 = male and 1 = female), household income, average sleep duration (in models when sleep onset and midpoint were moderating variables), average sleep onset time (in models when sleep duration and midpoint were moderating variables), and average sleep midpoint (in models when sleep duration and onset were moderating variables), were used as control variables in preliminary hierarchical regression models. Control variables that were significantly associated with the outcome variables of interest were included in final models, while control variables that were not associated with the outcome were removed from subsequent analyses.
Primary analyses included multilevel models with multivariate outcome variables used to determine whether temperamental negative affect and the sleep variables of interest (sleep onset, midpoint, and duration) were related to externalizing and internalizing behaviors, while accounting for the covariance of these outcomes. Although we expected that these sleep variables would be strongly linked to one another, sleep onset assesses effects of timing related to the initiation of nocturnal sleep whereas sleep midpoint evaluates the effects of both sleep onset and offset (i.e. wake onset). Thus, the moderating effects of sleep onset and midpoint were evaluated independently to determine if sleep timing factors (i.e. onset and midpoint) and sleep length (i.e. sleep duration) had similar effects on behavioral outcomes in temperamentally vulnerable children.
Next, a series of hierarchical linear regressions were run to determine whether temperamental negative affect and each of the moderating sleep timing variables (sleep onset and sleep midpoint) were differentially related to distinct behaviors within each of these domains. Specifically, we examined the subscales of attention problems and aggressive behaviors in the externalizing domain and emotional reactivity, anxiety/depression, withdrawal, and somatic complaints in the internalizing domain. As sleep duration did not interact with temperamental negative affect in the primary multilevel model, relations with distinct behaviors within the externalizing and internalizing domains were not assessed for this sleep parameter.
Control variables that were significantly associated with the outcome of interest in preliminary models were entered as control variables in the first block of final models. Predictor variables were entered simultaneously in the second block. The interaction product of these predictor variables was entered in the third block to explore whether associations between negative affect and behavioral outcomes (externalizing behaviors and internalizing behaviors) were moderated by sleep onset time or sleep midpoint. In all models, continuous variables (i.e., child age, household income, average sleep duration, average sleep onset time, average sleep midpoint, and temperamental negative affect) were centered at their respective sample means in order to facilitate detection and interpretation of interaction effects. The interaction term was calculated as the product of the two centered predictor variables.
Significant interactions were then plotted at low (-1 SD) and high (+1 SD) levels of the predictor (temperamental negative affect) and moderator (sleep onset time or sleep midpoint), following Aiken and West's (1991) guidelines. Slopes representing the association between the predictor and outcome variables at each level of the moderator were evaluated to determine if they were significantly different from zero. For all models, unstandardized residuals were plotted against the adjusted predicted values for each outcome variable to ensure there were no violations of (1) normality, (2) linearity, or (3) homoscedasticity. Multivariate outliers were identified using Cook's distance (Cook, 1977) and removed to confirm that results were not sensitive to influential data points.
Results
Preliminary Analyses
The internal consistency (Cronbach's alpha) for the negative affect scale (CBQ) was 0.747. Internal consistencies for the CBCL scales (and subscales) ranged from 0.403 to 0.908. Descriptive statistics and partial correlations between predictor and outcome variables are presented in Table 1. Controlling for child age and gender, children of lower income households had higher scores on temperamental negative affect and internalizing problems (r's ≤ -0.35, p's ≤ 0.001) as well as later sleep onset times (r = -0.40, p < 0.001), less night sleep duration (r = 0.35, p < 0.001), and later sleep midpoint (r = -0.33, p < 0.001).
Table 1. Partial Correlations and Descriptive Statistics for Predictor and Outcome Variables, Controlling for Child Age and Gender.
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Household Income | - | ||||||||||||
| 2. Negative Affect | -0.338*** | - | |||||||||||
| 3. Externalizing Behaviors | -0.101 | 0.412*** | - | ||||||||||
| 4. Aggressive Behaviors | -0.076 | 0.418*** | 0.978*** | - | |||||||||
| 5. Attention Problems | -0.147 | 0.269** | 0.761*** | 0.607*** | - | ||||||||
| 6. Internalizing Behaviors | -0.335*** | 0.554*** | 0.633*** | 0.592 *** | 0.564*** | - | |||||||
| 7. Emotional Reactivity | -0.244** | 0.479*** | 0.73*** | 0.698*** | 0.604*** | 0.836*** | - | ||||||
| 8. Anxiety/Depression | -0.401*** | 0.611*** | 0.4*** | 0.413*** | 0.238** | 0.806*** | 0.563*** | - | |||||
| 9. Withdrawn | -0.197* | 0.415*** | 0.515*** | 0.477*** | 0.475*** | 0.762*** | 0.529*** | 0.487*** | - | ||||
| 10. Somatic Complaints | -0.185* | 0.215* | 0.368*** | 0.286** | 0.507*** | 0.766*** | 0.528*** | 0.422*** | 0.512*** | - | |||
| 11. Average WD Sleep Onset Time (decimalized Time) | -0.403*** | 0.264** | 0.133 | 0.103 | 0.187* | 0.154 | 0.069 | 0.296*** | 0.117 | -0.021 | - | ||
| 12. Average WD Sleep Duration (minutes) | 0.353*** | -0.085 | -0.134 | -0.095 | -0.215* | -0.103 | -0.136 | -0.086 | -0.084 | -0.015 | -0.594*** | - | |
| 13. Average WD Sleep Midpoint (decimalized time) | -0.326*** | 0.277** | 0.096 | 0.078 | 0.121 | 0.126 | 0.008 | 0.312*** | 0.091 | -0.046 | 0.916 *** | -0.238** | - |
| Mean (SD) | 4.64 (1.93) | 3.74 (1.00) | 9.19 (7.52) | 7.32 (6.15) | 1.87 (2.03) | 6.48 (5.48) | 1.91 (1.86) | 1.75 (2.02) | 1.23 (1.37) | 1.59 (l.68) | 21.66 (0.88) | 562.59 (43.00) | 2.36 (0.74) |
| Range | 1-8 | 1.5-6.45 | 0-31 | 0-26 | 0-10 | 0-28 | 0-8 | 0-8 | 0-5 | 0-9 | 19.15-23.77 | 443.89-672 | 0.35-4.09 |
Caregiver Reported Questionnaire Data;
Actigraphy Data
p ≤ 0.05:
p ≤ 0.01;
p ≤ 0.001
Children with higher levels of temperamental negative affect had significantly higher rates of externalizing and internalizing behaviors (r's ≥ 0.41, p's < 0.001). This pattern was consistent for subscales within the externalizing and internalizing domains (r's ≥ 0.22, p's ≤ 0.05). Higher temperamental negative affect was also positively correlated with later sleep onset time (r = 0.26, p = 0.004) and later sleep midpoint (r = 0.28, p = 0.03). Sleep onset time was not associated with either externalizing or internalizing behaviors (r's ≥ 0.13, p's ≥ 0.1). However, children with later sleep onset time also had less night sleep duration (r = -0.594, p < 0.001) and later sleep midpoint (r = 0.92, p < 0.001).
Primary Analyses
Sleep Onset Time, Externalizing, and Internalizing Behaviors
Results of the multilevel model simultaneously predicting externalizing and internalizing behaviors are outlined in Table 2. This multilevel model did not violate any model assumptions. There was a strong correlation between these outcome variables (r = 0.864), which was accounted for in this model. For externalizing behaviors, the interaction between temperamental negative affect and sleep onset time was significant (B = 1.42, p = 0.039), suggesting that the association between temperamental negative affect and externalizing behaviors was strongest among children with later sleep onset time. There was also an interaction between temperamental negative affect and sleep onset in predicting internalizing behaviors (B = 1.44, p = 0.003), again indicating that the association between temperamental negative affect and internalizing behaviors was strongest among children with later sleep onset time.
Table 2. Summary of Multilevel Model Predicting Externalizing and Internalizing Behaviors Simultaneously (Sleep Onset Time).
| Externalizing Behaviors a | Internalizing Behaviors a | |||
|---|---|---|---|---|
|
| ||||
| Variable | B (S.E.) | β | B (S.E.) | β |
| Fixed Effects | ||||
| Constant | 8.88 (0.62)*** | - | 6.16 (0.44)*** | - |
| Temperamental Negative Affect a | 2.92 (0.63)*** | 0.53 | 2.89 (0.44)*** | 0.92 |
| Sleep Onset Time (decimalized time) b | 0.21 (0.71) | 0.03 | 0.08 (0.50) | 0.02 |
| Temperamental Negative Affect * Sleep Onset Time | 1.42 (0.68)* | 0.23 | 1.44 (0.48)** | 0.41 |
| Variance Components | ||||
| Externalizing Residual Variance | 30.85 | |||
| Internalizing Residual Variance | 9.82 | |||
| Within Person Residual Variance | 11.28 | |||
| Model Fit | 1414.12 | |||
| Estimate Parameters | 12 | |||
Note: B = Unstandardized Regression Coefficient; S.E. = Standard Error; β = Standardized Regression Coefficient.
Caregiver Reported Questionnaire Data;
Actigraphy Data
p < 0.05;
p < 0.01;
p < 0.001
Associations between temperamental negative affect and sleep onset time in predicting externalizing and internalizing behaviors are plotted in Figure 1. Fitted regression lines are plotted at low (-1 SD) and high (+1 SD) levels of sleep onset time. Simple slope analysis was used to determine if the slopes of these regression lines were significantly different from zero. The association between temperamental negative affect and externalizing behaviors was marginally significant among children with earlier sleep onset times (B = 1.67, p = 0.080). This association was significant among children with later sleep onset times (B = 4.17, p < 0.001; Figure 1a). Similarly, the association between temperamental negative affect and internalizing behaviors was significant among children with earlier sleep onset time (B = 1.63, p = 0.009) but stronger among children with later sleep onset times (B = 4.16, p < 0.001; Figure 1b).
Figure 1.
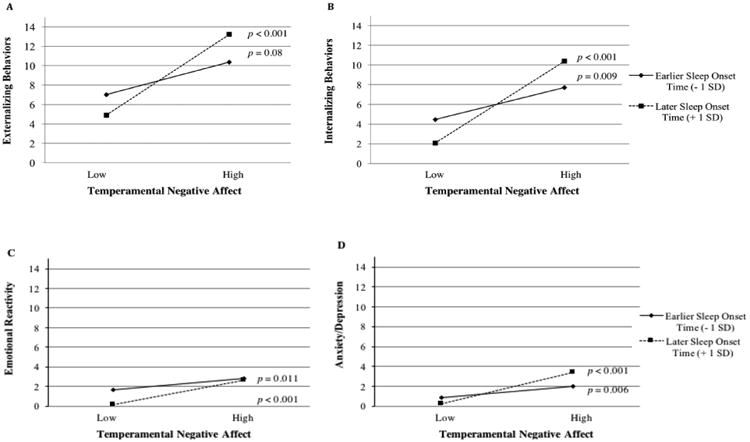
Associations between temperamental negative affect and sleep onset time (plotted at ± 1 SD of the mean) in predicting (a) externalizing behaviors, (b) internalizing behaviors, (c) emotional reactivity, and (d) anxiety/depression.
Sleep Onset Time and Subscales of Externalizing Behaviors
Results of the final models predicting specific behaviors within the externalizing domain are outlined in Table 3. In the model predicting attention problems, the interaction between temperamental negative affect and sleep onset time was not significant (B = 0.25, p = 0.213). These variables accounted for 13% of the variability in attention problems (R2 = 0.13, p = 0.003). For aggressive behaviors, the interaction between temperamental negative affect and sleep onset time was significant (B = 1.16, p = 0.048), suggesting that the association between temperamental negative affect and aggressive behaviors is strongest among children with later sleep onset time. The variables in this model accounted for 18% of the variability in aggressive behaviors (R2 = 0.18, p < 0.001).
Table 3. Summary of Regression Analyses with Subscales of Externalizing and Internalizing Behaviors (Sleep Onset Time).
| Attention Problems a | Aggressive Behaviors a | Emotional Reactivity a | Anxiety / Depression a | Withdrawal a | Somatic Complaints a | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Variable | B (S.E.) | β | B (S.E.) | β | B (S.E.) | β | B (S.E.) | β | B (S.E.) | β | B (S.E.) | β |
| Constant | 2.25 (0.26)*** | - | 7.06 (0.53)*** | - | 1.82 (0.16)*** | - | 1.63 (0.14)*** | - | 1.17 (0.12)*** | - | 1.55 (0.16)*** | - |
| Gender | -0.87 (0.36)* | -0.21 | - | - | - | - | - | - | - | - | - | - |
| Household Income a | - | - | - | - | - | - | -0.11 (0.08) | -0.10 | - | - | - | - |
| Temperamental Negative Affect a | 0.47 (0.19)* | 0.23 | 2.51 (0.54)*** | 0.41 | 0.87 (0.16)*** | 0.46 | 1.08 (0.15)*** | 0.53 | 0.54 (0.12)*** | 0.39 | 0.37 (0.16)* | 0.22 |
| Sleep Onset Time (decimalized time) b | 0.25 (0.21) | 0.11 | -0.07 (0.61) | -0.01 | -0.14 (0.18) | -0.07 | 0.25 (0.17) | 0.11 | 0.03 (0.14) | 0.02 | -0.13 (0.18) | -0.07 |
| Temperamental Negative Affect * Sleep Onset Time | 0.25 (0.20) | 0.11 | 1.16 (0.58)* | 0.17 | 0.39 (0.17)* | 0.18 | 0.58 (0.16)*** | 0.25 | 0.26 (0.13)* | 0.17 | 0.17 (0.17) | 0.09 |
| R2 | 0.13** | 0.20*** | 0.25*** | 0.48*** | 0.20*** | 0.06 | ||||||
| ΔR2 | 0.01 | 0.03* | 0.03* | 0.06*** | 0.03* | 0.008 | ||||||
Note: Results presented from final model. B = Unstandardized Regression Coefficient; S.E. = Standard Error; β = Standardized Regression Coefficient; R2 = Model Fit; ΔR2 = Change in Model Fit
Caregiver Reported Questionnaire Data;
Actigraphy Data
p < 0.05;
p < 0.01;
p < 0.001
Simple slopes analysis indicated that temperamental negative affect and aggressive behaviors were marginally associated among children with earlier sleep onset time (B = 1.49, p = 0.056). However, this association was stronger among children with later sleep onset time (B = 3.54, p < 0.001). After removing potential multivariate outliers from the model (identified using Cook's distance), the interaction term was marginally significant (B = 1.07, p = 0.083).
Sleep Onset Time and Subscales of Internalizing Behaviors
Results of the final models predicting specific behaviors within the internalizing domain are outlined in Table 3. In a model predicting emotional reactivity, the interaction between temperamental negative affect and sleep onset time was significant (B = 0.39, p = 0.026), suggesting that the association between temperamental negative affect and emotional reactivity is strongest among children with later sleep onset time. The variables in this model accounted for 25% of the variability in emotional reactivity (R2 = 0.25, p < 0.001). For the model predicting anxiety/depression, the interaction between temperamental negative affect and sleep onset time was also significant (B = 0.58, p < 0.001), suggesting that the link between temperamental negative affect and anxiety/depression is strongest among children with later sleep onset time. This model accounted for 48% of the variability in anxiety/depression (R2 = 0.48, p < 0.001).
Similarly for withdrawal, the interaction between temperamental negative affect and sleep onset time was significant (B = 0.26, p = 0.048), again suggesting that the association between temperamental negative affect and withdrawal is strongest among children with later sleep onset time. Variables in this model accounted for 20% of the variability in withdrawn behavior (R2 = 0.20, p < 0.001). In the model predicting somatic complaints, the interaction between temperamental negative affect and sleep onset time was not significant (B = 0.17, p = 0.325). The variables in this model accounted for 6% of the variability in somatic complaints (R2 = 0.06, p = 0.089).
Simple slopes analysis indicated that associations between temperamental negative affect and both emotional reactivity (Figure 1c) and anxiety/depression (Figure 1d) were significant among children with earlier (B's ≥ 0.57, p's ≤ 0.011) and later (B's ≥ 1.24, p's ≤ 0.001) sleep onset times, but strongest among children with later sleep onset times. In the model predicting withdrawal, the interaction term was no longer significant after removing influential multivariate outliers (B = 0.11, p = 0.475).
Sleep Midpoint, Externalizing, and Internalizing Behaviors
Results of the multilevel model simultaneously predicting externalizing and internalizing behaviors are outlined in Table 4. This multilevel model did not violate any model assumptions. There was a strong correlation between these outcome variables (r = 0.865), which was accounted for in this model. For externalizing behaviors, the interaction between temperamental negative affect and sleep midpoint was marginally significant (B = 1.40, p = 0.072), suggesting that the association between temperamental negative affect and externalizing behaviors was strongest among children with later sleep midpoint. There was also a significant interaction between temperamental negative affect and sleep midpoint in predicting internalizing behaviors (B = 1.73, p = 0.002), indicating that the association between temperamental negative affect and internalizing behaviors was strongest among children with later sleep midpoint.
Table 4. Summary of Multilevel Model Predicting Externalizing and Internalizing Behaviors Simultaneously (Sleep Midpoint).
| Externalizing Behaviors a | Internalizing Behaviors a | |||
|---|---|---|---|---|
|
| ||||
| Variable | B (S.E.) | β | B (S.E.) | β |
| Fixed Effects | ||||
| Constant | 8.91 (0.62)*** | - | 6.13 (0.44)*** | - |
| Temperamental Negative Affect a | 3.04 (0.63)*** | 0.54 | 2.96 (0.44)*** | 0.95 |
| Sleep Midpoint (decimalized time) b | -0.32 (0.86) | -0.04 | -0.28 (0.60) | -0.07 |
| Temperamental Negative Affect * Sleep Midpoint | 1.40 (0.77)† | 0.20 | 1.73 (0.54)** | 0.44 |
| Variance Components | ||||
| Externalizing Residual Variance | 31.44 | |||
| Internalizing Residual Variance | 9.73 | |||
| Within Person Residual Variance | 11.11 | |||
| Model Fit | 1412.94 | |||
| Estimate Parameters | 12 | |||
Note: B = Unstandardized Regression Coefficient; S.E. = Standard Error; β = Standardized Regression Coefficient.
Caregiver Reported Questionnaire Data;
Actigraphy Data
p < 0.08;
p < 0.01;
p < 0.001
The simple slopes analysis showed that the association between temperamental negative affect and externalizing behaviors was significant among children with earlier sleep midpoint (B = 2.01, p = 0.033) but strongest for children with later sleep midpoint (B = 4.08, p < 0.001; Figure 2a). Similarly, the association between temperamental negative affect and internalizing behaviors was significant among children with earlier sleep point (B = 1.68, p = 0.006) but stronger among children with later sleep midpoint (B = 4.24, p < 0.001; Figure 2b).
Figure 2.
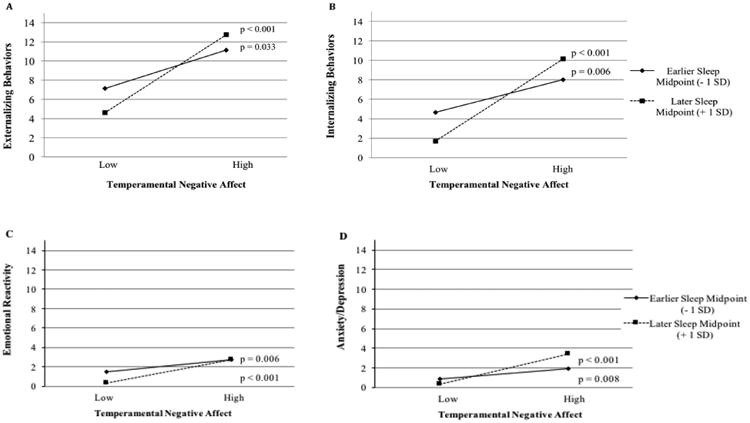
Associations between temperamental negative affect and sleep midpoint (plotted at ± 1 SD of the mean) in predicting (a) externalizing behaviors, (b) internalizing behaviors, (c) emotional reactivity, and (d) anxiety/depression.
Sleep Midpoint and Subscales of Externalizing Behaviors
Results of the final models predicting specific behaviors within the externalizing domain are outlined in Table 5. For attention problems, the interaction between temperamental negative affect and sleep midpoint was not significant (B = 0.27, p = 0.242). The variables in this model accounted for 12% of the variability in attention problems (R2 = 0.12, p = 0.006). Likewise, the interaction term was not significant for aggressive behaviors (B = 1.13, p = 0.091). The variables in this model accounted for 19% of the variability in aggressive behaviors (R2 = 0.19, p < 0.001).
Table 5. Summary of Regression Analyses with Subscales of Externalizing and Internalizing Behaviors (Sleep Midpoint).
| Attention Problems a | Aggressive Behaviors a | Emotional Reactivity a | Anxiety / Depression a | Withdrawal a | Somatic Complaints a | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Variable | B (S.E.) | β | B (S.E.) | β | B (S.E.) | β | B (S.E.) | β | B (S.E.) | β | B (S.E.) | β |
| Constant | 2.26 (0.26)*** | - | 7.09 (0.53)*** | - | 1.82 (0.15)*** | - | 1.61 (0.14)*** | - | 1.17 (0.12)*** | - | 1.54 (0.16)*** | - |
| Gender | -0.90 (0.36)* | -0.22 | - | - | - | - | - | - | - | - | - | - |
| Household Income a | - | - | - | - | - | - | -0.12 (0.08) | -0.11 | - | - | - | - |
| Temperamental Negative Affect a | 0.50 (0.19)** | 0.25 | 2.59 (0.54)*** | 0.42 | 0.92 (0.16)*** | 0.49 | 1.05 (0.15)*** | 0.52 | 0.55 (0.12)*** | 0.40 | 0.38 (0.16)* | 0.23 |
| Sleep Midpoint (decimalized time) b | 0.10 (0.25) | 0.04 | -0.39 (0.73) | -0.05 | -0.40 (0.21)† | -0.16 | 0.34 (0.20)† | 0.13 | -0.04 (0.16) | -0.02 | -0.25 (0.22) | -0.11 |
| Temperamental Negative Affect * Sleep Midpoint | 0.27 (0.23) | 0.11 | 1.13 (0.66) | 0.14 | 0.41 (0.19)* | 0.17 | 0.70 (0.18)*** | 0.27 | 0.32 (0.15)* | 0.19 | 0.26 (0.20) | 0.12 |
| R2 | 0.12** | 0.20*** | 0.27*** | 0.50*** | 0.20*** | 0.07* | ||||||
| ΔR2 | 0.01 | 0.02 | 0.03* | 0.07*** | 0.03* | 0.02 | ||||||
Note: Results presented from final model. B = Unstandardized Regression Coefficient; S.E. = Standard Error; β = Standardized Regression Coefficient; R2 = Model Fit; ΔR2 = Change in Model Fit
Caregiver Reported Questionnaire Data;
Actigraphy Data
p < 0.08;
p < 0.05;
p < 0.01;
p < 0.001
Sleep Midpoint and Subscales of Internalizing Behaviors
Results of the final models predicting specific behaviors within the internalizing domain are outlined in Table 5. In the model predicting emotional reactivity, the interaction between temperamental negative affect and sleep midpoint was significant (B = 0.41, p = 0.036), suggesting that the association between temperamental negative affect and emotional reactivity is strongest among children with later sleep midpoint. The variables in this model accounted for 27% of the variability in emotional reactivity (R2 = 0.27, p < 0.001). In the model predicting anxiety/depression, there was a significant interaction between sleep midpoint and temperamental negative affect (B = 0.70, p < 0.001) showing that the association between temperamental negative affect and anxiety/depression is strongest among children with a later sleep midpoint. Variables in this model accounted for 50% of the variability in anxiety/depression (R2 = 0.50, p < 0.001).
In the model predicting withdrawal, the interaction between temperamental negative affect and sleep midpoint was significant (B = 0.32, p = 0.030), again indicating that the association between temperamental negative affect and withdrawal was strongest among children with later sleep midpoint. The variables in this model accounted for 20% of the variability in withdrawn behavior (R2 = 0.20, p < 0.001). In the model predicting somatic complaints, the interaction between temperamental negative affect and sleep midpoint was not significant (B = 0.26, p = 0.186). These variables accounted for 7% of the variability in somatic complaints (R2 = 0.07, p = 0.047).
Simple slope analysis showed that slopes were significantly different from zero among children with both early (B's ≥ 0.54, p's ≤ 0.006) and late (B's ≥ 1.22, p's ≤ 0.001) sleep midpoints. However, the associations between temperamental negative affect and both emotional reactivity (Figure 2c) and anxiety/depression (Figure 2d) were strongest among children with later sleep midpoints. In the model predicting withdrawal, the interaction term was no longer significant after removing influential multivariate outliers, (B = 0.27, p = 0.181).
Sleep Duration, Externalizing, and Internalizing Behaviors
A separate multilevel model evaluating the moderating role of sleep duration was run to assess the specificity of the sleep timing variables discussed above. The results of this model are outlined in Table 6. This multilevel model did not violate any model assumptions. There was a strong correlation between the outcome variables (r = 0.872), which was accounted for in this model. For externalizing and internalizing behaviors, the interaction between temperamental negative affect and sleep duration was not significant (B = -0.02, p = 0.200 and B = -0.003, p = 0.809, respectively). Taken together, the results indicate that the associations between temperamental negative affect and behavior outcomes are dependent upon sleep timing variables but not sleep duration.
Table 6. Summary of Multilevel Model Predicting Externalizing and Internalizing Behaviors Simultaneously (Sleep Duration).
| Externalizing Behaviors a | Internalizing Behaviors a | |||
|---|---|---|---|---|
|
| ||||
| Variable | B (S.E.) | β | B (S.E.) | β |
| Fixed Effects | ||||
| Constant | 9.14 (0.60)*** | - | 6.47 (0.44)*** | - |
| Temperamental Negative Affect a | 3.03 (0.61)*** | 0.54 | 3.00 (0.44)*** | 0.90 |
| Sleep Duration (minutes) b | -0.02 (0.01) | -0.15 | -0.01 (0.01) | -0.13 |
| Temperamental Negative Affect * Sleep Duration | -0.02 (0.02) | -0.14 | -0.003 (0.01) | -0.03 |
| Variance Components | ||||
| Externalizing Residual Variance | 31.02 | |||
| Internalizing Residual Variance | 11.20 | |||
| Within Person Residual Variance | 11.39 | |||
| Model Fit | 1420.32 | |||
| Estimate Parameters | 12 | |||
Note: B = Unstandardized Regression Coefficient; S.E. = Standard Error; β = Standardized Regression Coefficient.
Caregiver Reported Questionnaire Data;
Actigraphy Data
p < 0.001
Discussion
A growing body of literature suggests that young children with high levels of temperamental negative affect are at heightened risk to concurrently experience, or eventually develop, a greater number of behavior problems, compared to children with low levels of negative affectivity. Consistent with these patterns, the results of the current study show positive associations between temperamental negative affect and both externalizing and internalizing behaviors. Moreover, these results extend the prior literature by demonstrating that associations between temperamental negative affect and behavioral problems are moderated by distinct facets of sleep timing: sleep onset and midpoint. Whereas sleep onset reflects the initiation of nocturnal sleep, sleep midpoint also accounts for constraints on sleep offset or morning wake time. Importantly, relations between temperament and behavior were not moderated by sleep duration, highlighting the specificity of sleep timing (i.e., sleep onset and midpoint) in modulating child outcomes. Provided the culmination of sleep parameters assessed in this study, a number of interventions can be staged to improve sleep timing in order to reduce risk of maladaptive outcomes associated with negative affectivity. For example, sleep onset time and sleep midpoint may be advanced by instituting earlier bedtimes (National Sleep Foundation, 2014). Additionally, reducing misalignment between the child's bedtime and circadian phase (LeBourgeois, Wright, LeBourgeois, & Jenni, 2013b) may reduce the risk of behavior problems among temperamentally vulnerable children.
Temperamental negative affect was strongly associated with both internalizing and externalizing outcomes, although externalizing behaviors were more prevalent in our sample. Importantly, the association between temperament and both domains of behavior problems was moderated by sleep. As delayed sleep onset time is strongly associated with shorter sleep duration and later sleep midpoint in this study and others (Kohyama, Shiiki, & Hasegawa, 2000; Nixon et al., 2008; LeBourgeois et al., 2013a), this finding corresponds to Dahl's proposal (1996) that insufficient sleep exacerbates, or facilitates the emergence of, emotional and behavioral control problems in children with pre-existing difficulties regulating affect. Indeed, recent work demonstrates that insufficient sleep impairs self-regulation in young children (Miller et al., 2015). Importantly, although sleep onset time and sleep midpoint (both early and late) moderated vulnerability to maladaptive outcomes, risk was greater among children with later sleep onset or sleep midpoint. Moreover, sleep duration did not moderate relations between temperamental negative affect and the behavioral outcomes assessed. Consistent with studies in adults (e.g., Genzel et al., 2013; Haus & Smolensky, 2006), this finding suggests that regardless of sleep length, initiating sleep outside of the optimal circadian phase confers risk for maladaptive outcomes. This risk is likely because circadian phase shifts alter the proportion of time spent in distinct sleep stages (e.g., REM sleep) and reduces overall sleep quality (Akerstedt, Kecklund, & Knutsson, 1991). Additional studies assessing sleep physiology and circadian processes are needed to better understand such affects in young children.
Altogether, the current findings suggest that sleep onset time and sleep midpoint moderate risk for adverse behavioral outcomes among temperamentally vulnerable children. However, it is important to note that it is difficult to determine whether the initial origin of risk lies in individual differences in temperament or in the physiological effects of delayed sleep onset and midpoint, which represent aspects of circadian entrainment and may ultimately cause emotional dysregulation and behavior problems (Borbély, Achermann, Trachsel, & Tobler, 1989; Monk, Petrie, Hayes, & Kupfer, 1994). Although the cross-sectional nature of this design prevents us from determining directionality, the results of our study and others (e.g., Bates, Viken, Alexander, Beyers, & Stockton, 2002; Biggs et al., 2011; Goodnight et al., 2007) suggest that children who inherently experience heightened affect may be more susceptible to the effects of insufficient sleep associated with late sleep onset and midpoint. Moreover, differences in maladaptive behavioral outcomes have previously been documented as products of altered sleep onset (e.g., Vriend et al., 2012 and 2013) and sleep midpoint (Pace-Schott et al., 2015).
Interestingly, although sleep onset time and sleep midpoint predicted externalizing and internalizing behaviors in children with high levels of temperamental negative affect, these findings were not consistent across all subscales within each of these domains. In the externalizing domain, sleep onset time moderated risk for aggressive behaviors but not attention issues among children high in temperamental negative affect. This finding aligns with the notions of Frick and Morris (2004), who propose two pathways through which negative affectivity may impede development of emotional regulatory skills and increase risk of conduct problems during early childhood. In the first pathway, children who with heightened negative affectivity may lack the regulatory skills needed to deter expression of aggressive behaviors in emotionally arousing contexts. Alternatively, the second pathway suggests that children with high levels of negative affectivity may be less behaviorally inhibited and, thus, more likely to engage in risk-taking behaviors associated with aggression and conduct problems. Based on our results, we posit that the interaction between temperamental negative affect and sleep onset time in predicting aggressive behaviors emerges via the first proposed pathway involving poor emotion regulation skills. Since children with temperamental negative affect are already prone to heightened affect, those who also have later sleep onset times may experience exacerbated emotional dysregulation, a common consequence of insufficient sleep (e.g., Williams, Berthelsen, Walker, & Nicholson, 2015). In turn, these children likely have more difficulty regulating behavior across various socioemotional situations and may act out in an aggressive manner more frequently. Likewise, insufficient sleep may also contribute to ego depletion: a state in which cognitive resources needed to effectively regulate affective responses are depleted (Baumeister, Bratslavsky, Muraven, & Tice, 1998). Thus, children with later sleep onset may have less cognitive resources available to effectively process and respond to affective demands. Among children who are already prone to negative reactivity, ego depletion may be exacerbated when these children experience later sleep onset.
In the internalizing domain, both sleep onset time and sleep midpoint moderated risk for emotional reactivity and anxiety/depression but not withdrawal or somatic complaints among children high in temperamental negative affect. Analogous to the proposed pathway underlying the emergence of externalizing behaviors, internalizing behaviors that rely on regulatory processes may also be greater among children with insufficient sleep. Whereas externalizing problems may be a consequence of lack of emotional regulation, children who exhibit internalizing behaviors may experience overregulation or ‘overcontrol’ of emotional processes, which may tightly constrain behavior and manifest in the form of anxiety and depression (Eisenberg et al., 2001). Although children with high temperamental negative affect and later sleep onset or later sleep midpoint displayed greater emotional reactivity than those with earlier sleep onset times or earlier sleep midpoint, the magnitude of change in behavior between these groups was not profound. This finding is consistent with the notion that children with low temperamental negative affect may be less reactive (e.g., Fox, Henderson, Rubin, Calkins, & Schmidt, 2001). Thus, among those children, emotional reactivity and regulation may not be impaired by insufficient sleep. Similarly, although temperamental negative affect was predictive of withdrawal and somatic complaints, these outcomes were not associated with, or moderated by, sleep onset time or sleep midpoint. As such, the current results suggest that insufficient sleep assessed via later sleep onset time and sleep midpoint may confer greatest risk for symptoms of anxiety and depression in preschool-aged children with high levels of negative affectivity.
Limitations & Future Directions
Though the present study underscores the importance of sleep timing among young children with heightened temperamental negative affect, there are several limitations to be addressed in future research. One limitation of the current study is the lack of assessments of bedtime routine and sleep hygiene in the sample. It is possible that delayed sleep onset time and later sleep midpoint are a product of bedtime resistance in children with negative emotionality. Having assessed sleep and behavior outcomes at one time point we are unable to infer directionality of these associations and change in such interactions overtime. However, longitudinal studies indicate that insufficient sleep during infancy corresponds to difficulties with emotional regulation and reduced self-regulation later in development (Sadeh et al., 2015; Williams et al., 2015) and suggests that connections between negative emotionality and insufficient sleep may emerge early and precede potential bedtime resistance issues that can arise in early childhood.
Additionally, the results of a recent study by LeBourgeois and colleagues (2013b) indicate that children are more likely to experience greater bedtime resistance and delayed sleep onset if bedtime does not align with their physiological circadian phase (as measured by dim light melatonin onset; LeBourgeois et al., 2013b). Since circadian processes and child temperament are thought to be innate, both bedtime resistance and sleep onset delay may emerge as a consequence of biological mechanisms. Although we were unable to assess circadian phase directly in our sample, both sleep onset and sleep midpoint have been strongly linked to melatonin onset, a biological index of circadian phase (e.g., LeBourgeois et al., 2013a,b). As such, our findings suggest that differences in sleep timing drive relations between temperamental negative affect and maladaptive behaviors in young children. However, future studies should evaluate the effects of bedtime routine and circadian processes (e.g., melatonin onset) to better understand their impact on behavioral outcomes in temperamentally vulnerable children.
Future work should also incorporate longitudinal designs to assess directionality of these interactions and potential changes overtime. To address the possibility of a bidirectional association between sleep and behavior problems, experimental manipulations of sleep schedules may be incorporated to empirically assess the mechanisms by which sleep onset time and sleep midpoint alter behavioral outcomes. For example, daytime sleepiness was reduced and emotionality scores improved among school-aged children when overnight sleep was extended, and stabilized, by one hour across 5 nights (Gruber, Cassoff, Frenette, Wiebe, & Carrier, 2012). Future studies may stage interventions that target sleep hygiene (i.e., consistent bedtime, avoiding stimulation, bedtime routines) which may alleviate bedtime resistance and ultimately advance sleep onset times and sleep midpoint in children with high levels of temperamental negative affect to facilitate more adaptive behavioral outcomes (Wilson et al., 2014).
Distal factors, such as parenting style and cultural influences, may also contribute to bedtime resistance, child bedtime, and sleep onset, as well as the severity of behavior problems (Bates et al., 2002). Although previous work highlights strong associations between parenting style and behavioral outcomes for children of various temperaments (see Putnam et al., 2002 for review), future studies are needed to examine the interplay between parenting, child sleep patterns, and behavioral outcomes in children with different temperaments across key developmental time points. This distinction is particularly important as both excessive parental involvement and low parental sensitivity have been linked to insufficient sleep and greater sleep problems among young children (Erath & Tu, 2011).
Finally, having used the CBQ Very Short Form, we were unable to parse apart distinct facets of temperamental negative affect (e.g., anger, fear, sadness) related to the behavioral outcomes assessed in our sample. As this is one of the first studies exploring the associations between temperament, sleep, and behavior problems in this age range, we used this abbreviated form to assess associations globally and in their simplest form. However, components of temperament may uniquely contribute risk for behavioral outcomes as emerging evidence links the facets of anger and frustration to externalizing and fear and sadness to internalizing outcomes (e.g. Eisenberg et al., 2009; Garstein et al., 2012; Olino et al., 2014). Thus, future studies should employ more comprehensive measures of temperament components to better understand moderating effects of sleep on behavior of children high on temperamental negative affect.
Conclusion
Throughout development, children with high levels of temperamental negative affect experience behavioral problems. This study provides novel and converging evidence highlighting the interplay between temperamental negative affect and sleep in conferring distinct risk for maladaptive outcomes within the externalizing and internalizing domains. As such, interventions designed to inform parents about the importance of sleep timing and teach strategies for good sleep hygiene may reduce the risk of developing behavior problems during early childhood for temperamentally vulnerable children.
Acknowledgments
This work was supported by NIH R01 HL111695-01A1 (R.M.C. Spencer).
References
- Acebo C, Sadeh A, Seifer R, Tzischinsky O, Hafer A, Carskadon MA. Sleep/wake patterns derived from activity monitoring and maternal report for healthy 1-to 5-year-old children. Sleep. 2005;28:1568. doi: 10.1093/sleep/28.12.1568. [DOI] [PubMed] [Google Scholar]
- Achenbach TM, Rescorla L. Manual for the ASEBA school-age forms & profiles. Burlington, VT: Aseba. Univ. of Vermont, Research Center for Children, Youth, & Families; 2001. [Google Scholar]
- Achenbach TM, Ruffle TM. The Child Behavior Checklist and related forms for assessing behavioral/emotional problems and competencies. Pediatrics in Review. 2000;21:265–271. doi: 10.1542/pir.21-8-265. [DOI] [PubMed] [Google Scholar]
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- Akerstedt T, Kecklund G, Knutsson A. Spectral analysis of sleep electroencephalography in rotating three-shift work. Scandinavian Journal of Work, Environment & Health. 1991;17:330–336. doi: 10.5271/sjweh.1694. [DOI] [PubMed] [Google Scholar]
- Basner M, Fomberstein KM, Razavi FM, Banks S, William JH, Rosa RR, Dinges DF. American time use survey: sleep time and its relationship to waking activities. Sleep. 2007;30:1085. doi: 10.1093/sleep/30.9.1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bates JE, Viken RJ, Alexander DB, Beyers J, Stockton L. Sleep and adjustment in preschool children: sleep diary reports by mothers relate to behavior reports by teachers. Child Development. 2002;73:62–75. doi: 10.1111/1467-8624.00392. [DOI] [PubMed] [Google Scholar]
- Baumeister RF, Bratslavsky E, Muraven M, Tice DM. Ego depletion: is the active self a limited resource? Journal of Personality and Social Psychology. 1998;74:1252. doi: 10.1037/0022-3514.74.5.1252. [DOI] [PubMed] [Google Scholar]
- Beltramini AU, Hertzig ME. Sleep and bedtime behavior in preschool-aged children. Pediatrics. 1983;71:153–158. [PubMed] [Google Scholar]
- Biggs SN, Lushington K, van den Heuvel CJ, Martin AJ, Kennedy JD. Inconsistent sleep schedules and daytime behavioral difficulties in school-aged children. Sleep Medicine. 2011;12:780–786. doi: 10.1016/j.sleep.2011.03.017. [DOI] [PubMed] [Google Scholar]
- Borbély AA, Achermann P, Trachsel L, Tobler I. Sleep initiation and initial sleep intensity: interactions of homeostatic and circadian mechanisms. Journal of Biological Rhythms. 1989;4:37–48. [PubMed] [Google Scholar]
- Cook RD. Detection of influential observation in linear regression. Technometrics. 1977;19:15–18. doi: 10.1111/j.0006-341X.2001.01166.x. [DOI] [Google Scholar]
- Dahl RE. Seminars in Pediatric Neurology. Vol. 3. WB Saunders; 1996. The impact of inadequate sleep on children's daytime cognitive function; pp. 44–50. [DOI] [PubMed] [Google Scholar]
- Dayyat EA, Spruyt K, Molfese DL, Gozal D. Sleep estimates in children: Parental versus actigraphic assessments. Nature and Science of Sleep. 2011;3:115–123. doi: 10.2147/NSS.S25676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deater–Deckard K, Dodge KA, Bates JE, Pettit GS. Multiple risk factors in the development of externalizing behavior problems: Group and individual differences. Development and Psychopathology. 1998;10:469–493. doi: 10.1017/s0954579498001709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg N, Cumberland A, Spinrad TL, Fabes RA, Shepard SA, Reiser M, Murphy BC, Losoya SH, Guthrie IK. The relations of regulation and emotionality to children's externalizing and internalizing problem behavior. Child Development. 2001;72:1112–1134. doi: 10.1111/1467-8624.00337. [DOI] [PubMed] [Google Scholar]
- Eisenberg N, Valente C, Spinrad TL, Cumberland A, Liew J, Reiser M, Zhou Q, Losoya SH. Longitudinal relations of children's effortful control, impulsivity and negative emotionality to their externalizing, internalizing, and co-occurring behavior problems. Developmental Psychology. 2009;45:988–1008. doi: 10.1037/a0016213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Sheikh M, Kelly RJ, Buckhalt JA, Hinnant BJ. Children's sleep and adjustment over time: the role of socioeconomic context. Child Development. 2010;81:870–883. doi: 10.1111/j.1467-8624.2010.01439.x. [DOI] [PubMed] [Google Scholar]
- Erath SA, Tu KM. The parenting context of children's sleep. Sleep and development: Familial and socio-cultural considerations. 2011:29–47. [Google Scholar]
- Fox NA, Henderson HA, Rubin KH, Calkins SD, Schmidt LA. Continuity and discontinuity of behavioral inhibition and exuberance: Psychophysiological and behavioral influences across the first four years of life. Child Development. 2001;72:1–21. doi: 10.1111/1467-8624.00262. [DOI] [PubMed] [Google Scholar]
- Frick PJ, Morris AS. Temperament and developmental pathways to conduct problems. Journal of Clinical Child & Adolescent Psychology. 2004;33:54–68. doi: 10.1207/S15374424JCCP3301_6. [DOI] [PubMed] [Google Scholar]
- Fisher BE, McGuire K. Do diagnostic patterns exist in the sleep behaviors of normal children? Journal of Abnormal Child Psychology. 1990;18:179–186. doi: 10.1007/BF00910729. [DOI] [PubMed] [Google Scholar]
- Gartstein MA, Putnam SP, Rothbart MK. Etiology of preschool behavior problems: Contributions of temperament attributes in early childhood. Infant Mental Health Journal. 2012;33:197–211. doi: 10.1002/imhj.21312. [DOI] [PubMed] [Google Scholar]
- Genzel L, Ahrberg K, Roselli C, Niedermaier S, Steiger A, Dresler M, Roenneberg T. Sleep timing is more important than sleep length or quality for medical school performance. Chronobiology International. 2013;30:766–771. doi: 10.3109/07420528.2012.763132. [DOI] [PubMed] [Google Scholar]
- Gilliom M, Shaw DS. Codevelopment of externalizing and internalizing problems in early childhood. Developmental Psychopathology. 2004;16:313–333. doi: 10.1017/s0954579404044530. doi:10.10170S0954579404044530. [DOI] [PubMed] [Google Scholar]
- Goodnight JA, Bates JE, Staples AD, Pettit GS, Dodge KA. Temperamental resistance to control increases the association between sleep problems and externalizing behavior development. Journal of Family Psychology. 2007;21:39–48. doi: 10.1037/0893-3200.21.1.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray JA. The neuropsychology of temperament. In: Strelau J, Angleitner A, editors. Explorations in Temperament: International Perspectives on Theory and Measurement. New York: Plenum Press; 1991. pp. 105–128. [Google Scholar]
- Gregory AM, Sadeh A. Sleep, emotional and behavioral difficulties in children and adolescents. Sleep Medicine Reviews. 2012;16:129–136. doi: 10.1016/j.smrv.2011.03.007. [DOI] [PubMed] [Google Scholar]
- Gruber R, Cassoff J, Frenette S, Wiebe S, Carrier J. Impact of sleep extension and restriction on children's emotional lability and impulsivity. Pediatrics. 2012;130:e1155–e1161. doi: 10.1542/peds.2012-0564. [DOI] [PubMed] [Google Scholar]
- Haus E, Smolensky M. Biological clocks and shift work: Circadian dysregulation and potential long-term effects. Cancer Causes & Control. 2006;17:489–500. doi: 10.1007/s10552-005-9015-4. [DOI] [PubMed] [Google Scholar]
- Henderson HA, Wachs TD. Temperament theory and the study of cognition-emotion interactions across development. Developmental Review. 2007;27:396–427. doi: 10.1016/j.dr.2007.06.004. [DOI] [Google Scholar]
- Kohyama J, Shiiki T, Hasegawa T. Sleep duration of young children is affected by nocturnal sleep onset time. Pediatrics International. 2000;42:589–91. doi: 10.1046/j.1442-200x.2000.01304.x. [DOI] [PubMed] [Google Scholar]
- Kurdziel L, Duclos K, Spencer RMC. Sleep spindles in midday naps enhance learning in preschool children. Proceedings of the National Academy of Sciences. 2013;110:17267–17272. doi: 10.1073/pnas.1306418110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LeBourgeois MK, Carskadon MA, Akacem LD, Simpkin CT, Wright KP, Achermann P, Jenni OG. Circadian phase and its relationship to nighttime sleep in toddlers. Journal of Biological Rhythms. 2013a;28:322–331. doi: 10.1177/0748730413506543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LeBourgeois MK, Wright KP, LeBourgeois HB, Jenni OG. Dissonance between parent-selected bedtimes and young children's circadian physiology influences nighttime settling difficulties. Mind, Brain, and Education. 2013b;7:234–242. doi: 10.1111/mbe.12032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leve LD, Kim HK, Pears KC. Childhood temperament and family environment as predictors of internalizing and externalizing trajectories from ages 5 to 17. Journal of Abnormal Child Psychology. 2005;33:505–520. doi: 10.1007/s10802-005-6734-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipscomb ST, Leve LD, Shaw D, Neiderhiser JM, Scaramella LV, Ge X, Conger RD, Reid JB, Reiss D. Negative emotionality and externalizing problems in toddlerhood: Overreactive parenting as a moderator of genetic influences. Development and Psychopathology. 2012;24:167–179. doi: 10.1017/S0954579411000757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meltzer LJ, Walsh CM, Peightal AA. Comparison of actigraphy immobility rules with polysomnographic sleep onset latency in children and adolescents. Sleep and Breathing. 2015;19:1415–1423. doi: 10.1007/s11325-015-1138-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller AL, Seifer R, Crossin R, LeBourgeois MK. Toddler's self-regulation strategies in a challenge context are nap-dependent. Journal of Sleep Research. 2015;24:241–358. doi: 10.1111/jsr.12260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monk TH, Petrie SR, Hayes AJ, Kupfer DJ. Regularity of daily life in relation to personality, age, gender, sleep quality and circadian rhythms. Journal of Sleep Research. 1994;3:196–205. doi: 10.1111/j.1365-2869.1994.tb00132.x. [DOI] [PubMed] [Google Scholar]
- National Sleep Foundation. 2014 Retrieved from http://sleepfoundation.org/sleep-topics/children-and-sleep/page/0%2C2/
- Nixon GM, Thompson JM, Han DY, Becroft DM, Clark PM, Robinson E, Waldie KE, Wild CJ, Black PN, Mitchell EA. Short sleep duration in middle childhood: risk factors and consequences. Sleep. 2008;31:71. doi: 10.1093/sleep/31.1.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olino TM, Dougherty LR, Bufferd S, Carlson GA, Klein DN. Testing models of psychopathology in preschool-aged children using a structure interview-based assessment. Journal of Abnormal Child Psychology. 2014;42:1201–1211. doi: 10.1007/s10802-014-9865-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pace-Schott EF, Rubin ZS, Tracy LE, Spencer RMC, Orr SP, Verga PW. Emotional trait and memory associates of sleep timing and quality. Psychiatry Research. 2015;229:999–1010. doi: 10.1016/j.psychres.2015.05.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penpraze V, Reilly JJ, MacLean CM, Montgomery C, Kelly LA, Paton JY, Aitchison T, Grant S. Monitoring of physical activity in young children: how much is enough? Pediatric Exercise Science. 2006;18:483. doi: 10.1123/pes.18.4.483. [DOI] [PubMed] [Google Scholar]
- Putnam SP, Rothbart MK. Development of short and very short forms of the Children's Behavior Questionnaire. Journal of Personality Assessment. 2006;87:102–112. doi: 10.1207/s15327752jpa8701_09. [DOI] [PubMed] [Google Scholar]
- Putnam SP, Sanson AV, Rothbart MK. Child temperament and parenting. Handbook of Parenting. 2002;1:255–277. [Google Scholar]
- Rothbart MK, Ahadi SA, Hershey KL, Fischer P. Investigations of temperament at three and seven years: The Children's Behavior Questionnaire. Child Development. 2001;72:1394–1408. doi: 10.1111/1467-8624.00355. [DOI] [PubMed] [Google Scholar]
- Rothbart M, Bates J. Temperament. In: Eisenberg N, Damon W, Richard LM, editors. Handbook of child psychology: Vol 3, Social, emotional, and personality development. 6th. Hoboken, NJ US: John Wiley & Sons Inc; 2006. pp. 99–166. [Google Scholar]
- Sadeh A, De Marcas G, Guri Y, Berger A, Tikotzky L, Bar-Haim Y. Infant Sleep Predicts Attention Regulation and Behavior Problems at 3–4 Years of Age. Developmental Neuropsychology. 2015;40:122–137. doi: 10.1080/87565641.2014.973498. [DOI] [PubMed] [Google Scholar]
- Shaw DS, Owens EB, Giovannelli J, Winslow EB. Infant and toddler pathways leading to early externalizing disorders. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40:36–43. doi: 10.1097/00004583-200101000-00014. [DOI] [PubMed] [Google Scholar]
- Sitnick SL, Goodlin-Jones BL, Anders TF. The use of actigraphy to study sleep disorders in preschoolers: some concerns about detection of nighttime awakenings. Sleep. 2008;31:395. doi: 10.1093/sleep/31.3.395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slobodskaya HR. The hierarchical structure of personality and common psychopathology in childhood. Journal of Research in Personality. 2014;53:36–46. doi: 10.1016/j.jrp.2014.08.005. [DOI] [Google Scholar]
- Tandon M, Cardeli E, Luby J. Internalizing disorders in early childhood: A review of depressive and anxiety disorders. Child & Adolescent Psychiatry Clinics. 2009;18:593–610. doi: 10.1016/j.chc.2009.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vitaro F, Barker ED, Boivin M, Brendgen M, Tremblay RE. Do early difficult temperament and harsh parenting differentially predict reactive and proactive aggression? Journal of Abnormal Child Psychology. 2006;34:685–695. doi: 10.1007/s10802-006-9055-6. [DOI] [PubMed] [Google Scholar]
- Vriend JL, Davidson FD, Corkum PV, Rusak B, Chambers CT, McLaughlin EN. Manipulating sleep duration alters emotional functioning and cognitive performance in Children. Journal of Pediatric Psychology. 2013;38:1058–1069. doi: 10.1093/jpepsy/jst033. [DOI] [PubMed] [Google Scholar]
- Vriend JL, Davidson FD, Corkum PV, Rusak B, McLaughlin EN, Chambers CT. Sleep quantity and quality in relation to daytime functioning in children. Children's Health Care. 2012;41:204–222. doi: 10.1080/02739615.2012.685039. [DOI] [Google Scholar]
- Ward TM, Gay C, Anders TF, Alkon A, Lee KA. Sleep and napping patterns in 3-to-5-year old children attending full-day childcare centers. Journal of Pediatric Psychology. 2008;33:666–672. doi: 10.1093/jpepsy/jsm102. [DOI] [PubMed] [Google Scholar]
- Williams KE, Berthelsen DC, Walker S, Nicholson JM. A developmental cascade model of behavioral sleep problems, emotional and attentional self-regulation across early childhood. Behavioral Sleep Medicine. 2015:1–21. doi: 10.1080/15402002.2015.1065410. [DOI] [PubMed] [Google Scholar]
- Wilson KE, Lumeng JC, Kaciroti N, Chen SYP, LeBourgeois MK, Chervin RD, Miller AL. Sleep hygiene practices and bedtime resistance in low-income preschoolers: Does temperament matter? Behavioral Sleep Medicine. 2014:1–12. doi: 10.1080/15402002.2014.940104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yokomaku A, Misao K, Omoto F, Yamagishi R, Tanaka K, Takada K, Kohyama J. A study of the association between sleep habits and problematic behaviors in preschool children. Chronobiology International. 2008;25:549–564. doi: 10.1080/07420520802261705. [DOI] [PubMed] [Google Scholar]


