Abstract
It has been shown that epigenetic regulation plays an important role in skin wound healing. We previously found that histone H3K27me3 demethylase JMJD3 regulates inflammation and cell migration in keratinocyte wound healing. In this study, we identified Notch1 as a direct target of JMJD3 and NF-κB in wounded keratinocytes using in vitro cell and in vivo animal models. We found that Notch1 is up-regulated in the wound edge and its expression is dependent on JMJD3 and NF-κB in wounded keratinocytes. We also found that Notch1 activates the expression of RhoU and PLAU gene, which are critical regulators of cell migration. Consistently, depletion or inactivation of Notch1 resulted in decreased filopodia formation, increased focal adhesion and actin stress fiber, leading to reduced keratinocyte migration and skin wound healing. Thus, our findings provide the molecular mechanism involving JMJD3/NF-κB-Notch pathway in keratinocyte wound healing.
Introduction
The skin forms physical and immunological barriers from the external environment to maintain water balance, body temperature, insulation, sensation, and immunity1, 2. When the skin barrier is disturbed, wound healing begins immediately after injury. The skin wound healing process occurs in four overlapping stages: haemostasis, inflammation, migration and proliferation, and remodeling3, 4. Within an hour after injury, blood coagulation and platelet activation at the injury site form a fibrin clot, which stops the bleeding and fills the discontinuity in the skin. The activated platelets provide various growth factors required for inflammation, angiogenesis, and migration of keratinocytes and fibroblasts5. During the inflammation stage, bacteria and cell debris are cleaned by activated neutrophils from injured blood vessels. In the migration and proliferation stage that follows, keratinocytes at the wound edge migrate into the wound via the changing of cell-cell and cell-matrix interaction through up-regulation of matrix metalloproteinases (MMPs). In addition, keratinocytes distant from the wound edge actively proliferate, resulting in the filling of the wound gap. Accumulating evidence indicates that stem cells from the bulge of hair follicles contribute to re-epithelialization6, 7. Once the wound gap is filled, the basement membrane is re-established, and keratinocytes are differentiated. Concurrently, tissue granulation and angiogenesis take place. During wound contraction, myofibroblasts help to decrease the size of the wound. In the maturation and remodeling stage, the replacement of collagen and rearrangement of collagen fibers occur, forming a tension line that increases the tensile strength of the wound.
Accumulation evidences have revealed that Notch signaling plays an important role in skin development, homeostasis, and wound healing by the regulation of differentiation, proliferation, and apoptosis8–11. Mammals have four Notch receptors (Notch1~4) and five ligands such as Delta-like 1, 3, and 4, and Jagged 1 and 2. To activate Notch signaling, the interaction between a transmembrane Notch receptor and a transmembrane ligand is required on two adjacent cells. Ligand binding to Notch receptor results in successive proteolytic cleavage of Notch at extracellular and transmembrane domain, producing Notch intracellular domain (NICD). Translocated NICD to the nucleus form a complex with RBP-J transcription factor and regulates target gene expression including HES and Hey family. In fact, Notch family genes and their ligands are expressed in various epidermal layers during development12–16. Consistently, abnormal Notch signaling results in impaired epidermal differentiation, proliferation, and inflammation, leading to a variety of skin diseases including skin cancer, psoriasis, and atopic dermatitis10, 11, 17.
Recently, epigenetic regulation, such as DNA methylation and histone modification, has been investigated in skin wound healing18, 19. DNA methylation mediated by DNA methyltransferases (DNMTs) has an important role in the maintenance of epidermal progenitor self-renewal during embryonic development20. However, very few reports demonstrated that DNA methylation is implicated on skin wound healing. For example, decreased level of global DNA methylation is observed in rat skin wound healing21. In contrast to DNA methylation, several reports demonstrated the importance of histone modification or histone-modifying enzymes in skin wound healing. Reduction of histone H3K27 trimethylation is observed in the murine skin wound epidermis22. Consistently, Polycomb group protein (PcG) such as Eed, Ezh2, and Suz12 are down-regulated while H3K27 demethylases such as JMJD3 and UTX are up-regulated, resulting in Myc and Egfr gene activation22. Up-regulated JMJD3 at wound edge is required for the inflammatory, MMP, and growth factor gene activation in keratinocytes after wounding23. In addition, double knock out mice for Ezh1 and Ezh2 histone methyltransferase clearly show defective cell proliferation and wound healing6. Regulation of histone acetylation also is shown to be crucial for skin wound healing. Expression of HDAC2 (histone deacetylase 2) increases at the wound margin in early phase and in the wound bed at later stages24. Interestingly, class I-IIa HDAC inhibition by trichostatin A (TSA) results in accelerated wound healing through displacement of HDAC2 from gene promoters and up-regulation of IGF-I, FGF-10, and EGF gene expression25. However, this effect is suppressed by class III HDAC (SIRTs) inhibitor, indicating that SIRT may be an upstream negative regulator of class I HDAC in wound healing25. The level of histone H3K9 acetylation is increased in the wound area and the application of p300/PCAF activator on wounded skin induces accelerated wound healing26. In contrast, the deletion of Setd8 histone methyltransferase, which is essential for epidermal progenitor cells, is not altered in the wound healing process27.
In this study, we demonstrated that JMJD3 and NF-κB-dependent Notch1 activation is required for the regulation of focal adhesion, filopodia, and stress fiber formation though RhoU and uPA gene expressions, leading to keratinocyte migration during the early phase of skin wound healing.
Results
Up-regulation of Notch expression in wounded keratinocytes
Although Notch signaling plays an important role in epidermal differentiation and skin maintenance, the molecular mechanism underlying Notch-mediated keratinocyte wound healing has not been fully elucidated. Thus, we first examined the expression of Notch genes in the scratch-wounded HaCaT keratinocytes. Quantitative PCR analysis revealed that the expression of Notch1 and Notch4 genes increased acutely at 2~6 hr after scratching and then slowly decreased (Fig. 1a). Since Notch1 is expressed more abundantly than Notch4 (Supplementary Fig. S1) and a primary Notch receptor in epidermal differentiation, proliferation, and inflammation12, 15, 28–30, we further examined expression of NICD (Notch intracellular domain) of Notch1 at protein level. Similarly, Western blot analysis showed the acute up-regulation of NICD expression (Fig. 1b). We also observed increased nuclear expression of NICD in the region of the leading wound edge, while no elevated expression were detected in the region far from the wound edge as well as in confluent monolayer HaCaT keratinocytes (Figs 1c and S2). In addition, the promoter activity of Hes1 gene, a direct target of Notch, was up-regulated acutely at 2~6 hr after scratching (Fig. 1d). Mutation of RBP-J binding sites on the Hes1 gene promoter abolished the scratch-induced activation of the promoter activity.
Figure 1.
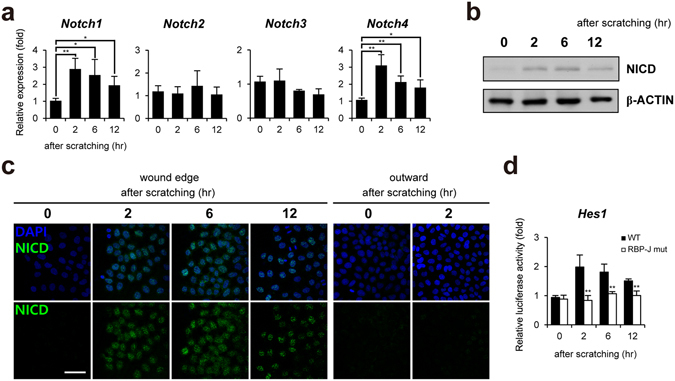
Up-regulation of Notch1 expression in scratch-wounded keratinocytes. (a) After HaCaT keratinocytes were scratched, transcripts of Notch1~4 and GAPDH were determined by quantitative PCR. (b) Lysates from scratch-wounded HaCaT keratinocytes were immunoblotted with anti-NICD and anti-β-ACTIN antibodies, respectively. (c) Increased nuclear NICD expression in the region of the wound edge compared to the region far from the wound edge (outward) (>1 mm). HaCaT keratinocytes after scratching were immunostained with anti-NICD antibody. Nuclei were identified using DAPI staining. Scale bar, 25 μm. (d) Up-regulation of Hes1 promoter reporter activity after scratching. However, activity of promoter reporter containing mutated RBP-J binding sites is not up-regulated by scratching.
JMJD3 activates expression of Notch1 gene in wounded keratinocytes
Since the spatiotemporal expression pattern of Notch1 is similar with that of JMJD3 in the early phase of wounded HaCaT keratinocytes23, we next tested whether JMJD3 regulates the Notch1 gene expression. When the transcript of JMJD3 was depleted by RNA interference, the expression of Notch1 decreased in the scratch-wounded keratinocytes at RNA and protein level (Fig. 2a). Decreased expression of nuclear NICD was observed in the region of the leading wound edge (Supplementary Fig. S3a). We also utilized GSK-J4 to inhibit the histone demethylase activity of JMJD331. GSK-J4 treatment reduced Notch1 expression (Figs 2b and S3b). JMJD3 has been shown to interact with NF-κB and up-regulate gene expression of MMP, inflammatory, and growth factor during keratinocytes wound healing23. Thus, we also tested the dependency of NF-κB for the Notch1 gene activation. Depletion of NF-κB p65 suppressed Notch1 gene activation and nuclear expression of NICD in wounded keratinocytes (Figs 2c and S3c). Consistently, BAY11–7085, which inhibits IκBα phosphorylation, showed same effects of NF-κB p65 depletion (Figs 2d and S3d). We also found suppression of promoter activity of Notch1 gene by depletion or inactivation of NF-κB p65 (Supplementary Fig. S4).
Figure 2.
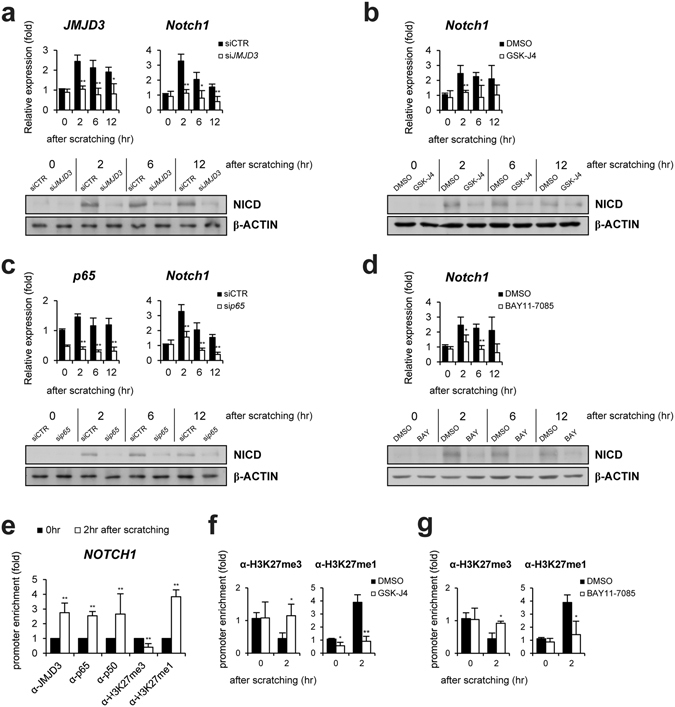
JMJD3 and NF-κB are required for up-regulation of Notch1 expression in scratch-wounded keratinocytes. (a,b) Following the depletion (siJMJD3) or inactivation (GSK-J4) of JMJD3, HaCaT keratinocytes were scratched and expression level was determined by quantitative PCR and Western blotting. (c,d) Following depletion (sip65) or inactivation (BAY11-7085) of NF-κB, HaCaT keratinocytes were scratched and expression level was determined by quantitative PCR and Western blotting. (e) ChIP assay was performed in scratch-wounded HaCaT keratinocytes. The occupancy of each protein was determined with quantitative PCR at the Notch1 gene encompassing the NF-κB binding sites. ChIP using normal IgG was performed as a negative control. (f,g) The methylation level of H3K27 was measured by ChIP assay in scratch-wounded HaCaT keratinocytes treated with GSK-J4 or BAY11-7085.
To investigate whether JMJD3 and NF-κB directly activates Notch1 gene expression, we identified NF-κB binding sites on the upstream region of Notch1 gene (Supplementary Fig. S7a)32. The recruitment of JMJD3 and NF-κB p65 to the upstream region of Notch1 gene was investigated in HaCaT keratinocytes after scratching by a ChIP assay. Chromatin from HaCaT keratinocytes at 0 and 2 hr after scratching were immunoprecipitated. Quantitative PCR showed that JMJD3, p50, and p65 are significantly bound to the NF-κB binding sites of the Notch1 gene (Fig. 2e). Consistent with the recruitment of JMJD3, we detected a decreased level of tri-methylated H3K27 (H3K27me3) as well as an increased level of mono-methylated H3K27 (H3K27me1) at the promoter (Fig. 2e). Inactivation of JMJD3 or NF-κB consistently showed the maintenance of the tri-methylation level of H3K27 in the upstream region of Notch1 gene (Fig. 2f,g).
Notch1 regulates keratinocyte wound healing via cell migration
We investigated the effect of Notch1 depletion or inactivation on the keratinocytes migration in response to scratching. As shown in Fig. 3, wound closure was significantly delayed in Notch1-depleted HaCaT keratinocytes as compared to control siRNA-transfected keratinocytes (Fig. 3a). Transwell migration assay also showed significantly fewer migrating keratinocytes in Notch1-depleted keratinocytes (Fig. 3b). Inhibition of Notch signaling by DAPT, a γ-secretase inhibitor, resulted in delayed wound closure and suppressed keratinocyte migration (Fig. 3c,d). In contrast, over-expression of NICD in HaCaT keratinocytes accelerated wound closure as compare to control empty vector-transfected keratinocytes (Supplementary Fig. S5).
Figure 3.
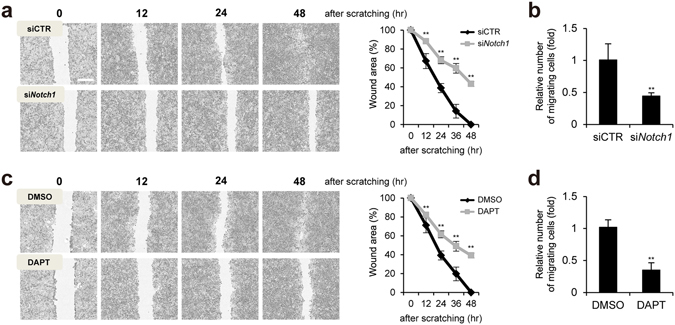
Notch1 regulates keratinocyte migration in scratch-wounded keratinocytes. (a,b) Depletion of Notch1 (siNotch1) attenuates HaCaT keratinocyte migration after scratching. HaCaT keratinocytes were scratched and photographed. Scale bar, 400 μm. Transwell assay was performed. (c,d) Inactivation of Notch1 (DAPT) attenuates HaCaT keratinocyte migration after scratching. Transwell assay was performed.
Notch regulates keratinocytes migration via formation of filopodia, focal adhesion, and actin stress fibers
We first conducted a literature search to identify Notch1 target genes, which affect directly cell migration33–39. Among them, we found that expression of RhoU Rho GTPase (also known as Wrch1) and PLAU (plasminogen activator, urokinase) genes are dependent on Notch1 in scratch-wounded HaCaT keratinocytes (Fig. 4a). Consistently, JMJD3 depletion or inhibition suppressed RhoU and PLAU gene activation (Fig. 4b). NF-κB p65 depletion or inhibition showed the same effect on the RhoU and PLAU gene expression (Fig. 4c).
Figure 4.
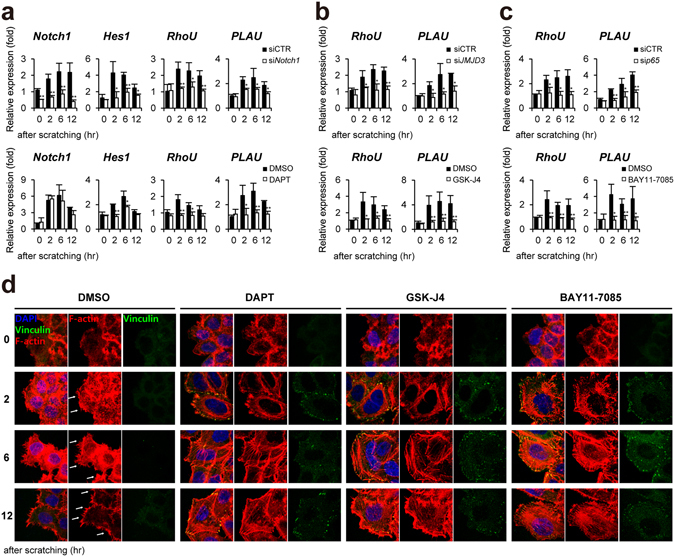
Notch1 regulates keratinocytes migration via RhoU and PLAU gene expression in scratch-wounded keratinocytes. (a) Depletion (siNotch1) or inactivation (DAPT) of Notch1 (b) Depletion (siJMJD3) or inactivation (GSK-J4) of JMJD3 (c) Depletion (sip65) or inactivation (BAY 11-7082) of NF-κB suppresses RhoU and PLAU gene activation in scratch-wounded HaCaT keratinocytes. Transcripts of Notch1, Hes1, RhoU, PLAU, and GAPDH were determined by quantitative PCR. (d) Inactivation of Notch1 or JMJD3 or NF-κB results in decreased filopodia-like protrusions (white arrows), increased focal adhesion and actin stress fibers in scratch-wounded HaCaT keratinocytes. To detect filopodia and actin stress fibers, cells were stained with phalloidin (red). Focal adhesion was identified by cell immunostaining with anti-vinculin antibody (green). Nuclei were identified using DAPI staining. Scale bar, 25 μm.
RhoU has been shown to regulate cell migration through formation of filopodia, focal adhesion, and dissolution of stress fiber in diverse cell types40–42. In addition, PLAU converts plasminogen to plasmin, which regulates cell adhesion and migration though cleavage of ECM and MMPs43. Therefore, we investigated whether Notch regulates formation of filopodia, focal adhesion, and actin stress fibers in the scratch-wounded HaCaT keratinocytes using cell staining with anti-vinculin antibody and phalloidin. As shown in Fig. 4d, we observed that control HaCaT keratinocytes show well developed filopodia-like protrusion, which is stained by phalloidin, at the leading edge. However, fewer filopodia were observed in DAPT, GSK-J4, and BAY11–7085-treated keratinocytes, respectively (Fig. 4d). In addition, DAPT, GSK-J4, and BAY11–7085 treatment significantly increased the number of focal adhesion stained with anti-vinculin antibody (Fig. 4d). Similarly, increased bundles of stress actin filaments were observed in DAPT, GSK-J4, and BAY11-7085-treated keratinocytes compared with control HaCaT keratinocytes after scratching (Fig. 4d). We found consistently that depletion of RhoU or PLAU results in delayed wound closure as compared to control siRNA-transfected HaCaT keratinocytes (Supplementary Fig. S6).
Recruitment of NICD to the RhoU and PLAU gene promoters in wounded keratinocytes
Since our results demonstrated Notch1-dependent RhoU and PLAU gene activations, we next examined the recruitment of NICD to the genes in HaCaT keratinocytes after scratching by ChIP assay. Chromatin from HaCaT keratinocytes at 0~12 hr after scratching was immunoprecipitated with anti-NICD, and anti-acetylated histone H3, respectively. Quantitative PCR was performed to determine the occupancy of proteins using oligonucleotide primers encompassing RBP-J binding site (Supplementary Fig. S7b). Upon scratch wound, NICD significantly bound to the RBP-J binding site of RhoU and PLAU genes (Fig. 5a). We also detected an increased level of histone H3 acetylation (Fig. 5a). As expected, DAPT treatment resulted in a reduced level of NICD and acetylated H3 (Fig. 5b). In addition, the inactivation of JMJD3 and NF-κB also showed the same effects of DAPT on the level of NICD and H3 acetylation at the genes (Fig. 5c,d).
Figure 5.
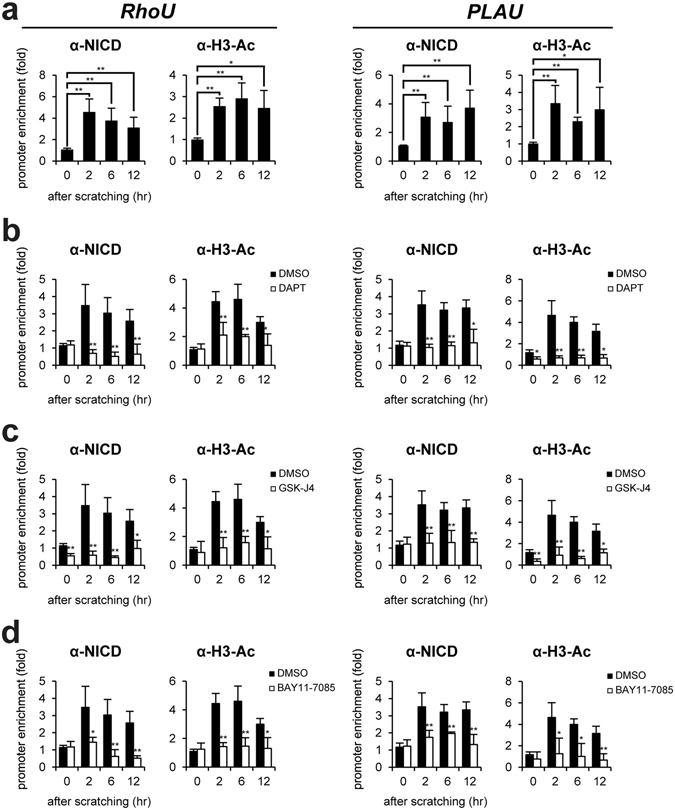
Notch1 activates RhoU and PLAU gene expression in scratch-wounded keratinocytes. (a) ChIP assay was performed in scratch-wounded HaCaT keratinocytes using the anti-NICD and anti-acetylated H3 antibodies, respectively. The occupancy of each protein was determined with quantitative PCR at the RhoU and PLAU gene promoter region encompassing the RBP-J binding site. ChIP using normal IgG was performed as a negative control. (b~d) Inactivation of Notch1 (DAPT) or JMJD3 (GSK-J4) or NF-κB (BAY 11–7082) results in decreased recruitment of NICD to the RhoU and PLAU gene promoters. Following DAPT, GSK-J4, or BAY11–7085 treatment, HaCaT keratinocytes were scratched and ChIP assay was performed.
Effect of JMJD3 and NF-κB on the Notch in skin wound healing
We further investigated the dependency of JMJD3 and NF-κB in Notch1-mediated wound healing using an in vivo mouse skin wound model. We first determined the expression of Notch1~4, RhoU, and PLAU in the skin after wounding. Quantitative PCR analysis revealed that the expression of the Notch1 and 4 genes increased at 1~2 days after scratching and then decreased slowly (Figs 6a and S8a). Consistent to scratch-wounded HaCaT keratinocytes, Notch1 is expressed more abundantly than Notch4 in skin wounds (Supplementary Fig. S8b). The expression pattern of RhoU and PLAU genes is correlated with that of Notch1 (Fig. 6a). Immunohistochemical results further showed that NICD is up-regulated and localized in the nucleus of wound edge keratinocytes, which are immunostained with anti-keratin14 (KRT14) antibody, at 1~7 days after wounding (Supplementary Fig. S9a).
Figure 6.
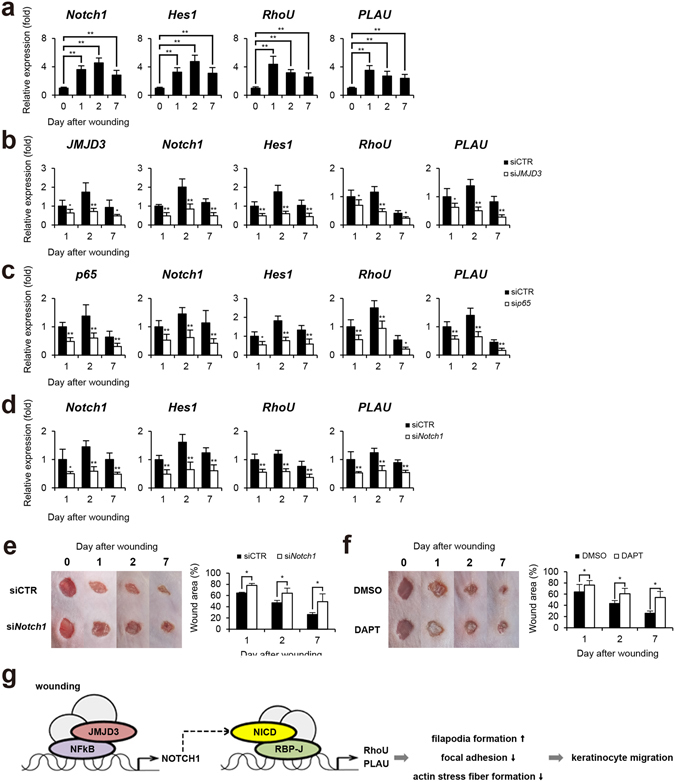
Delayed wound healing in Notch1-depleted mouse skin. (a) Transcripts of Notch1, Hes1, RhoU, PLAU, and GAPDH were determined in mouse skin wound by quantitative PCR (n = 6/group). (b~d) Following topical application of JMJD3 siRNA or NF-κB p65 siRNA or Notch1 siRNA in 30% Pluronic F-127 gel, wound tissue was harvested and transcripts of Notch1, Hes1, RhoU, PLAU, and GAPDH were determined by quantitative PCR (n = 6/group). (e,f) Depletion (siNotch1) or inactivation (DAPT) of Notch1 results in delayed skin wound closure. Following the application of Notch1 siRNA or DAPT, the wounded skins were photographed and a percentage of the wound area was measured quantitatively (n = 6/group). (g) A proposed model. Upon wounding, NF-κB p65 and JMJD3 binds to Notch 1 gene promoter to activate Notch 1 gene expression through demethylation of H3K27me3. The cleaved intracellular domain of Notch1 (NICD) binds to RhoU and PLAU gene promoters and activates RhoU and PLAU gene expression. These events result in enhanced filopodia formation, decreased focal adhesion and actin stress fiber formation in keratinocytes, leading to keratinocyte migration.
To evaluate the necessity of JMJD3 and NF-κB for the up-regulation of Notch1 expression in skin wound healing, JMJD3 or NF-κB p65 siRNA was applied topically to the skin wound. JMJD3 or p65 depletion attenuated the up-regulation of Notch1, RhoU, and PLAU expressions in wounded skin (Fig. 6b,c). We further found a decreased nuclear NICD expression in the wound edge after wounding (Supplementary Fig. S9b,c). Notch1 depletion also resulted in decreased RhoU and PLAU gene activations (Fig. 6d). Finally, we investigated the effects of Notch1 on skin wound healing processes. Although the wound was nearly closed by 7 days after wounding in a control siRNA or DMSO-applied skin wound, we found a significantly delayed wound closure in Notch1 siRNA or DAPT-applied skin wound (Fig. 6e,f).
Discussion
Notch pathway plays an important role in epidermal development in embryo and epidermal homeostasis in adult8–11. Notch family genes and its ligands are expressed in various epidermal layers during development12–16. Notch1 activates expression of keratin 1 and involucrin genes, which are early keratinocyte differentiation markers44. Deficiency of Notch1 further showed epidermal hyperplasia by reducing p21WAF/Cip1 expression in keratinocytes44. Notch signaling also regulates the proliferation and differentiation of keratinocyte stem cells located in basal layer of the epidermis45. However, a few reports have been reported the role of Notch signaling in keratinocyte wound healing.
In this study, we found that JMJD3 and NF-κB activate Notch1 expression at the wound edge in wounded keratinocytes. Although the expression pattern of Notch 4 was similar to that of JMJD3, Notch1 is expressed more abundantly than Notch4 in wounded keratinocytes and skin (Figs 1A and S1 and S6). Similarly, Notch1 has been considered as a primary Notch receptor in epidermal differentiation, proliferation, and inflammation12, 15, 28–30. Notch1 and its ligand Jagged1 are up-regulated at the wound edge in grafted human skin on the nude mouse16. Consistent to our findings, Notch1 is up-regulated in the epidermis including suprabasal and basal laminal keratinocytes at 1~4 days after wounding in the mouse skin30, 46. Up-regulated Notch1 activates TNFα expression, which can induce CCL20 and CXCL13 chemokine expression, leading to the recruitment of RORγ+ group3 innate lymphoid cells in wounded skin30. The inhibition of Notch by antisense RNA or γ-secretase inhibitor DAPT showed impaired skin wound healing due to inhibition of leukocyte infiltration, angiogenesis, and keratinocyte migration47, 48. DAPT-treated wound also showed incomplete wound closure46, 49.
Similar spatiotemporal expression of Notch1 and JMJD3 led us to investigate whether JMJD3 is required for Notch1 gene activation in wounded keratinocytes. In fact, depletion or inhibition of JMJD3 and NF-κB attenuated up-regulation of Notch1 gene expression. Consistently, JMJD3 and NF-κB were recruited to NF-κB binding sites on the Notch1 gene upon wounding as well as demethylation of H3K27me3. Our results are supported by requirement of NF-κB for the Notch1 gene activation32, 50.
At the wound edge, keratinocytes begin to rearrange their cytoplasmic and membrane structures, leading to disassembly of cell-extracellular matrix and cell-cell interaction for cell migration. These events include the actin cytoskeleton-mediated regulation of lamellipodia, filopodia, and focal adhesions during the early phase of wound healing51, 52. We found that depletion or inhibition of Notch1 results in decreased filopodia formation, increased focal adhesion and actin stress fibers, leading to delayed keratinocyte migration and wound closure. Our results further demonstrated that Notch1 directly up-regulates the expression of RhoU and PLAU gene, which are important regulators for cell migration (see below). Consistently, RhoU and PLAU have been identified as the target gene of Notch signaling33, 35, 37. RhoU is considered atypical Rho GTPase because it is likely to be predominately GTP-bound53. In fact, RhoU activates cell migration through formation of filopodia, loss of focal adhesion, and dissolution of stress fiber in several cell types40–42, 53–56. In particular, RhoU prominently localizes to focal adhesion, as indicated by vinculin expression40. Depletion of RhoU results in increased number of focal adhesion and decreased cell migration in response to wounding40. Filopodia formation by RhoU requires interaction with Pyk2 non-receptor tyrosine kinase in the presence of Src41. Pyk2 plays important role in cell adhesion and focal adhesion assembly through regulation of cytoskeleton dynamics57–59. PLAU converts plasminogen to plasmin, which cleaves ECM and MMPs for cell adhesion and migration43. Interestingly, PLAU is shown to be expressed in leading edge of migration keratinocytes60–63. In addition, PLAU colocalizes with vinculin at focal adhesion sites in various cell types64–66. Stimulation of uPA by Endo180, which is 180-kD transmembrane glycoprotein and complex with uPA and uPAR, leads to increased filopodia production in breast cancer cells67. Inhibition of uPA further decreases cell migration68–72. Interestingly, the expression and activity of MMPs are regulated transcriptionally and post-transcriptionally in wounded keratinocytes since we identified MMP-1, MMP-2, MMP-3, MMP-9, MMP-13, and MMP-14 as direct target of JMJD3 and NF-κB23 and PLAU-converted plasmin is shown to activate these MMPs73–83.
In conclusion, our study supports the important role of Notch1 as well as JMJD3 and NF-κB in keratinocytes wound healing. Specifically, JMJD3 and NF-κB-mediated Notch1 activation is required for the regulation of focal adhesion, filopodia, and stress fiber formation though RhoU and PLAU gene expression, leading to keratinocyte migration during the early phase of skin wound healing (Fig. 6g). Given that some genes related to Notch signaling are down-regulated in keratinocyte of venous ulcers and activation of Notch signaling in epidermal stem cells accelerate diabetic wound healing84, 85, our study may provide a new therapeutic intervention for the chronic skin wound.
Materials and Methods
Cell culture, animals, and chemicals
Human HaCaT keratinocytes were maintained in DMEM supplemented with 10% fetal bovine serum and antibiotics. Adult male ICR mice (8 weeks old; Samtako) were held in a temperature-controlled room (22 °C) at 55% humidity. The Committee for Experimental Animal Research at Sogang University approved the animal experiments and all methods were performed in accordance with guidelines and regulations relevant to the study. HaCaT keratinocytes were treated with 30 μM GSK-J4 (Tocris) and 10 μM BAY 11–7085 (Cayman) to inhibit JMJD3 and NF-κB, respectively. To inactivate Notch signaling, 10 μM DAPT (N-[N-(3,5-difluorophenacetyl)-l-alanyl]-S-phenylglycine t-butyl ester, Sigma-Aldrich) was used as a γ-secretase inhibitor.
In vivo mouse skin wound healing
Mice were anesthetized by intraperitoneal injection of 300 μl of 1.25% Avertin (2,2,2-tribromoethanol, Sigma,-Aldrich), and full-thickness excision wounds using 4 mm biopsy punch (Kai) were made in the shaved dorsal skin. Wound tissue was harvested with 6 mm biopsy punch at the indicated time points (0, 1, 2, 7 days post wounding). After wounding, siRNA and DAPT were topically administered to the wound site. For the delivery of siRNA, 20 μl of 10 μM siRNA against mouse JMJD3 (m-063799-01-0005, Dharmacon), p65 (m-040776-01-0005, Dharmacon), Notch1 (18128, Bioneer) or control siRNA (d-001206-14-05, Dharmacon) mixed with 30% pluronic F127 gel (Sigma-Aldrich) was chilled on ice and applied to the wound cavity86. The efficiency of knock down of the specific gene was confirmed with real-time PCR. In addition, 20 μl of 100 μM DAPT was applied directly to the wound once daily until skin tissues were harvested47, 49. DMSO was applied as a control. The wounds were photographed and wound sizes were analyzed using ImageJ software (NIH, Bethesda, USA). Control and experimental wound were done on the same animal. Experiments were performed with two biological repeats (n = 3/group). Data were pooled (total n = 6/group).
RNA interference
HaCaT keratinocytes were transfected with siRNA against human JMJD3 (m-023013-01-0005, Dharmacon), p65 (m-003533-02-0005, Dharmacon), Notch1 (4851, Bioneer), RhoU (58480, Bioneer), PLAU (5328, Bioneer), or control siRNA (d-001206-14-05, Dharmacon) using the X-treamGENE siRNA transfection reagent (Roche). The efficiency of knock down of the specific gene was confirmed with real-time PCR.
RT-PCR
Total RNA was extracted from HaCaT keratinocytes and mouse skin using RNAiso Plus (Takara). First-strand cDNA synthesis from the total RNA template was performed with PrimeScriptTM RT master mix (Takara). The resulting cDNAs were subjected to real-time PCR using qPCR 2x PreMIX SYBR (Enzynomics) with a Stratagen Mx3000p (Agilent Technologies). PCR conditions used to amplify all genes were 10 min at 95 °C and 40 cycles of 95 °C for 15 s, 60 °C for 40 s. Expression data were calculated from the cycle threshold (Ct) value using the ΔCt method of quantification. GAPDH was used for normalization. Oligonucleotides used for real-time PCR are listed in Supplementary Table S1.
Standard curve method for mRNA quantification
Plasmids containing each of Notch1 and 4 cDNA were used as standards for the absolute quantification. The concentration of each plasmid was measured by spectrophotometer or Ct value of real-time PCR using specific oligonucleotides for plasmid backbone. After concentration of plasmids were determined (same copies per 1 μl), plasmids were diluted (1:1, 1:10, 1:100, 1:1000, 1:10000). The diluted plasmids were amplified by specific oligonucleotides for each gene by real-time PCR. Using Ct value of each of plasmids, Notch1 and 4 standard curve were determined as according to the manufacturer’s instructions of Stratagene Mx3000 P (Agilent Technologies, Germany). The absolute amount of mRNA was calculated by each trendline equations [hNotch1: Y = −2.630*LOG(X) + 8.85, hNotch4: Y = −2.627*LOG(X) + 10.25; mNotch1: Y = −2.239*LOG(X) + 7.56, mNotch4: Y = −1.885*LOG(X) + 10.64].
Over-expression of NICD
Intracellular domain of Notch1 was amplified using oligonucleotides: forward (EcoRI) 5′-CCGGAATTCGGTGCTGCTGTCCCGCAA-3′; reverse (XhoI) 5′-CCGCTCGAGCGTTTACTTGAAGGCCTCCGG-3′ and cloned into the pCS4 expression vector containing HA epitope. HaCaT keratinocytes were transfected transiently with jetPRIME reagent (Polyplus).
Immunocytochemistry, immunohistochemistry, and histology
HaCaT keratinocytes were fixed for 15 min with 4% paraformaldehyde in PBS and permeabilized with PBST solution (0.5% Triton X-100 in PBS) for 30 min. After blocking of cells with 5% BSA in PBST solution for 1 h, cells were incubated with the anti-NICD (ab8925, Abcam) or anti-vinculin antibodies (V9131, Sigma-Aldrich) overnight at 4 °C. Antigens were detected with the secondary antibodies conjugated to TR or FITC (Sigma-Aldrich). To detect F-actin, cells were labelled with Alexa 546-phalloidin (Sigma-Aldrich). The wounded skins were immediately fixed with 4% paraformaldehyde in PBS and left overnight at 4 °C. The samples were dehydrated, embedded in paraffin and sectioned at 6 μm. The sections were de-paraffinized and boiled in Tris-EDTA buffer (pH 9.0) for 30 min, and then they were cooled at room temperature. The sections were incubated with 5% normal serum for 30 min. Subsequently, the sections were incubated with anti-NICD (ab8925, Abcam) or anti-KRT14 antibodies (ab7800, Abcam) overnight at 4 °C. After three washings with PBST, the sections were then incubated with a secondary antibody conjugated to FITC or TRITC. For histology, the sections were stained with hematoxylin and eosin (DAKO).
Promoter reporter assay
HaCaT keratinocytes were transfected transiently with Hes1 or Notch1 gene luciferase construct in conjunction with a control thymidine kinase promoter-driven renilla luciferase. For mutation of RBP-J binding sites (TGTGGGAA → TGACGCTA and TTCACACG → TAGAGTCG) on Hes1 gene promoter, PCR was performed87. After transfection of luciferase reporter containing gene and control renilla luciferase expression vector, cells were scratched and reporter activity was determined as described previously88.
Western blot analysis
Cell extracts were prepared as described previously89. Western blotting was carried out using anti-NICD (4147, Cell Signaling) and anti-β-ACTIN antibodies (3G4-F9; AbFrontier), respectively.
Scratch wound assay
HaCaT keratinocytes were plated on 6-well or 12-well culture plates and grown in 10% FBS containing a DMEM medium until they reached confluence. After cells were starved in the serum-free medium for 24 hr, the cell cultures were scratched using a sterile 10 μL tip. Cells were washed with serum-free medium and allowed to grow in 2% FBS containing DMEM. Cell cultures were recorded after scratching at the indicated times using the IncuCyte imaging system (Essen BioScience).
Transwell assay
HaCaT keratinocyte migration was assessed quantitatively using Transwell (Corning Costar). After keratinocytes were starved in a serum free medium for 24 hr, keratinocytes (1 × 105) were plated on the upper chamber of a 24-well Transwell plate with an 8μm pore size. After keratinocytes were incubated for 24 hr in a medium containing 10% FBS, the migrated keratinocytes were counted using the IncuCyte imaging system.
Chromatin immunoprecipitation (ChIP)
ChIP was performed as described previously89. Anti-JMJD3 antibody (AP1022a, Abgent), anti-NICD (4147, Cell Signaling), anti-trimethyl H3K27 antibody (07–449, Millipore), anti-monomethyl H3K27 antibody (07–448, Millipore), anti-phosphorylated RNA polymerase II antibody (ab5131, Abcam), anti-p50 antibody (ab7971, Abcam), anti-p65 antibody (ab7970, Abcam), or normal IgG (SC-2027, Santa Cruz Biotechnology) were used. Real-time PCR was performed with a Stratagene Mx3000P using primers (see Supplementary Table S2).
Statistical analyses
All quantitative data are presented as mean ± S.E.M. for three independent experiments. The differences between two groups were evaluated by a paired t-test. Analysis of variance (ANOVA) was used for multiple comparisons. Significance values were *P ≤ 0.05 and **P ≤ 0.01.
Electronic supplementary material
Acknowledgements
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (2009–0093822).
Author Contributions
B.J., T.Y.Y., B.J.K., and J.N. designed research; J.N., J.Y.S., H.J., and J.Y.L. conducted research; B.J., J.N., T.Y.Y., J.Y.S., J.Y.L., B.J.K., and W.S.K. analyzed data; B.J., J.N., and J.Y.S. prepared figures and Tables; B.J. and T.Y.Y. wrote the paper. T.Y.Y. and B.J. had primary responsibility for final content. All authors read and approved the final manuscript.
Competing Interests
The authors declare that they have no competing interests.
Footnotes
Jungtae Na and Jee Yoon Shin contributed equally to this work.
Electronic supplementary material
Supplementary information accompanies this paper at doi:10.1038/s41598-017-06750-7
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Tae Young Yune, Email: tyune@khu.ac.kr.
Bong-Gun Ju, Email: bgju@sogang.ac.kr.
References
- 1.Madison KC. Barrier function of the skin: “la raison d’etre” of the epidermis. The Journal of investigative dermatology. 2003;121:231–241. doi: 10.1046/j.1523-1747.2003.12359.x. [DOI] [PubMed] [Google Scholar]
- 2.Proksch E, Brandner JM, Jensen JM. The skin: an indispensable barrier. Experimental dermatology. 2008;17:1063–1072. doi: 10.1111/j.1600-0625.2008.00786.x. [DOI] [PubMed] [Google Scholar]
- 3.Braiman-Wiksman L, Solomonik I, Spira R, Tennenbaum T. Novel insights into wound healing sequence of events. Toxicologic pathology. 2007;35:767–779. doi: 10.1080/01926230701584189. [DOI] [PubMed] [Google Scholar]
- 4.Eming SA, Krieg T, Davidson JM. Inflammation in wound repair: molecular and cellular mechanisms. The Journal of investigative dermatology. 2007;127:514–525. doi: 10.1038/sj.jid.5700701. [DOI] [PubMed] [Google Scholar]
- 5.Pierce GF, et al. In vivo incisional wound healing augmented by platelet-derived growth factor and recombinant c-sis gene homodimeric proteins. The Journal of experimental medicine. 1988;167:974–987. doi: 10.1084/jem.167.3.974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ezhkova E, et al. EZH1 and EZH2 cogovern histone H3K27 trimethylation and are essential for hair follicle homeostasis and wound repair. Genes & development. 2011;25:485–498. doi: 10.1101/gad.2019811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ito M, et al. Wnt-dependent de novo hair follicle regeneration in adult mouse skin after wounding. Nature. 2007;447:316–320. doi: 10.1038/nature05766. [DOI] [PubMed] [Google Scholar]
- 8.Bielefeld KA, Amini-Nik S, Alman BA. Cutaneous wound healing: recruiting developmental pathways for regeneration. Cellular and molecular life sciences: CMLS. 2013;70:2059–2081. doi: 10.1007/s00018-012-1152-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Massi D, Panelos J. Notch signaling and the developing skin epidermis. Advances in experimental medicine and biology. 2012;727:131–141. doi: 10.1007/978-1-4614-0899-4_10. [DOI] [PubMed] [Google Scholar]
- 10.Nowell C, Radtke F. Cutaneous Notch signaling in health and disease. Cold Spring Harbor perspectives in medicine. 2013;3:a017772. doi: 10.1101/cshperspect.a017772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Okuyama R, Tagami H, Aiba S. Notch signaling: its role in epidermal homeostasis and in the pathogenesis of skin diseases. Journal of dermatological science. 2008;49:187–194. doi: 10.1016/j.jdermsci.2007.05.017. [DOI] [PubMed] [Google Scholar]
- 12.Ambler CA, Watt FM. Expression of Notch pathway genes in mammalian epidermis and modulation by β‐Catenin. Developmental Dynamics. 2007;236:1595–1601. doi: 10.1002/dvdy.21151. [DOI] [PubMed] [Google Scholar]
- 13.Blanpain C, Lowry WE, Pasolli HA, Fuchs E. Canonical notch signaling functions as a commitment switch in the epidermal lineage. Genes & development. 2006;20:3022–3035. doi: 10.1101/gad.1477606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nickoloff B, et al. Jagged-1 mediated activation of notch signaling induces complete maturation of human keratinocytes through NF-[kappa] B and PPAR [gamma] Cell death and differentiation. 2002;9:842. doi: 10.1038/sj.cdd.4401036. [DOI] [PubMed] [Google Scholar]
- 15.Pan Y, et al. γ-Secretase functions through Notch signaling to maintain skin appendages but is not required for their patterning or initial morphogenesis. Developmental cell. 2004;7:731–743. doi: 10.1016/j.devcel.2004.09.014. [DOI] [PubMed] [Google Scholar]
- 16.Thélu J, Rossio P, Favier B. Notch signalling is linked to epidermal cell differentiation level in basal cell carcinoma, psoriasis and wound healing. BMC dermatology. 2002;2:7. doi: 10.1186/1471-5945-2-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Melnik BC. The potential role of impaired Notch signalling in atopic dermatitis. Acta dermato-venereologica. 2015;95:5–11. doi: 10.2340/00015555-1898. [DOI] [PubMed] [Google Scholar]
- 18.Fahs F, Bi X, Yu FS, Zhou L, Mi QS. New insights into microRNAs in skin wound healing. IUBMB life. 2015;67:889–896. doi: 10.1002/iub.1449. [DOI] [PubMed] [Google Scholar]
- 19.Lewis CJ, Mardaryev AN, Sharov AA, Fessing MY, Botchkarev VA. The Epigenetic Regulation of Wound Healing. Advances in wound care. 2014;3:468–475. doi: 10.1089/wound.2014.0522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sen GL, Reuter JA, Webster DE, Zhu L, Khavari PA. DNMT1 maintains progenitor function in self-renewing somatic tissue. Nature. 2010;463:563–567. doi: 10.1038/nature08683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gomes MV, et al. Effects of the led therapy on the global DNA methylation and the expression of Dnmt1 and Dnmt3a genes in a rat model of skin wound healing. Lasers in medical science. 2016;31:1521–1526. doi: 10.1007/s10103-016-2007-7. [DOI] [PubMed] [Google Scholar]
- 22.Shaw T, Martin P. Epigenetic reprogramming during wound healing: loss of polycomb-mediated silencing may enable upregulation of repair genes. EMBO reports. 2009;10:881–886. doi: 10.1038/embor.2009.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Na J, et al. Histone H3K27 Demethylase JMJD3 in Cooperation with NF-kappaB Regulates Keratinocyte Wound Healing. The Journal of investigative dermatology. 2016;136:847–858. doi: 10.1016/j.jid.2015.11.029. [DOI] [PubMed] [Google Scholar]
- 24.Fitzgerald O’Connor EJ, et al. Histone deacetylase 2 is upregulated in normal and keloid scars. The Journal of investigative dermatology. 2012;132:1293–1296. doi: 10.1038/jid.2011.432. [DOI] [PubMed] [Google Scholar]
- 25.Spallotta F, et al. A nitric oxide-dependent cross-talk between class I and III histone deacetylases accelerates skin repair. The Journal of biological chemistry. 2013;288:11004–11012. doi: 10.1074/jbc.M112.441816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Spallotta F, et al. Enhancement of lysine acetylation accelerates wound repair. Communicative & integrative biology. 2013;6:e25466. doi: 10.4161/cib.25466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Driskell I, Oeztuerk-Winder F, Humphreys P, Frye M. Genetically induced cell death in bulge stem cells reveals their redundancy for hair and epidermal regeneration. Stem Cells. 2015;33:988–998. doi: 10.1002/stem.1910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ambler CA, Watt FM. Adult epidermal Notch activity induces dermal accumulation of T cells and neural crest derivatives through upregulation of jagged 1. Development. 2010;137:3569–3579. doi: 10.1242/dev.050310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Estrach S, Ambler CA, Celso CLL, Hozumi K, Watt FM. Jagged 1 is a β-catenin target gene required for ectopic hair follicle formation in adult epidermis. Development. 2006;133:4427–4438. doi: 10.1242/dev.02644. [DOI] [PubMed] [Google Scholar]
- 30.Li, Z. et al. Epidermal Notch1 recruits ROR [gamma]+ group 3 innate lymphoid cells to orchestrate normal skin repair. Nature communications7 (2016). [DOI] [PMC free article] [PubMed]
- 31.Kruidenier L, et al. A selective jumonji H3K27 demethylase inhibitor modulates the proinflammatory macrophage response. Nature. 2012;488:404–408. doi: 10.1038/nature11262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhou W, et al. The AKT1/NF-kappaB/Notch1/PTEN axis has an important role in chemoresistance of gastric cancer cells. Cell death & disease. 2013;4:e847. doi: 10.1038/cddis.2013.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bhavsar PJ, Infante E, Khwaja A, Ridley AJ. Analysis of Rho GTPase expression in T-ALL identifies RhoU as a target for Notch involved in T-ALL cell migration. Oncogene. 2013;32:198–208. doi: 10.1038/onc.2012.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dai MY, et al. Downregulation of Notch1 induces apoptosis and inhibits cell proliferation and metastasis in laryngeal squamous cell carcinoma. Oncology reports. 2015;34:3111–3119. doi: 10.3892/or.2015.4274. [DOI] [PubMed] [Google Scholar]
- 35.Hafeez BB, et al. Targeted knockdown of Notch1 inhibits invasion of human prostate cancer cells concomitant with inhibition of matrix metalloproteinase-9 and urokinase plasminogen activator. Clinical Cancer Research. 2009;15:452–459. doi: 10.1158/1078-0432.CCR-08-1631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Niessen K, et al. Slug is a direct Notch target required for initiation of cardiac cushion cellularization. The Journal of cell biology. 2008;182:315–325. doi: 10.1083/jcb.200710067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shimizu M, et al. Plasminogen activator uPA is a direct transcriptional target of the JAG1-Notch receptor signaling pathway in breast cancer. Cancer research. 2011;71:277–286. doi: 10.1158/0008-5472.CAN-10-2523. [DOI] [PubMed] [Google Scholar]
- 38.Sivasankaran B, et al. Tenascin-C is a novel RBPJκ-induced target gene for Notch signaling in gliomas. Cancer research. 2009;69:458–465. doi: 10.1158/0008-5472.CAN-08-2610. [DOI] [PubMed] [Google Scholar]
- 39.Zhou L, et al. The significance of Notch1 compared with Notch3 in high metastasis and poor overall survival in hepatocellular carcinoma. PloS one. 2013;8:e57382. doi: 10.1371/journal.pone.0057382. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 40.Chuang YY, Valster A, Coniglio SJ, Backer JM, Symons M. The atypical Rho family GTPase Wrch-1 regulates focal adhesion formation and cell migration. Journal of cell science. 2007;120:1927–1934. doi: 10.1242/jcs.03456. [DOI] [PubMed] [Google Scholar]
- 41.Ruusala A, Aspenstrom P. The atypical Rho GTPase Wrch1 collaborates with the nonreceptor tyrosine kinases Pyk2 and Src in regulating cytoskeletal dynamics. Molecular and cellular biology. 2008;28:1802–1814. doi: 10.1128/MCB.00201-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tao W, Pennica D, Xu L, Kalejta RF, Levine AJ. Wrch-1, a novel member of the Rho gene family that is regulated by Wnt-1. Genes & development. 2001;15:1796–1807. doi: 10.1101/gad.894301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Smith HW, Marshall CJ. Regulation of cell signalling by uPAR. Nature reviews. Molecular cell biology. 2010;11:23–36. doi: 10.1038/nrm2821. [DOI] [PubMed] [Google Scholar]
- 44.Rangarajan A, et al. Notch signaling is a direct determinant of keratinocyte growth arrest and entry into differentiation. The EMBO journal. 2001;20:3427–3436. doi: 10.1093/emboj/20.13.3427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nakamura T, et al. Epiprofin orchestrates epidermal keratinocyte proliferation and differentiation. Journal of cell science. 2014;127:5261–5272. doi: 10.1242/jcs.156778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shu B, Yang R, Shi Y, Xu Y, Liu J. Notch1 Signaling Regulates Wound Healing via Changing the Characteristics of Epidermal Stem Cells. J Stem Cell Res Ther. 2016;6:2. doi: 10.4172/2157-7633.1000348. [DOI] [Google Scholar]
- 47.Chigurupati S, et al. Involvement of notch signaling in wound healing. PloS one. 2007;2:e1167. doi: 10.1371/journal.pone.0001167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Roy M, et al. Notch 1 regulates keratinocyte migration via integrin beta1 activation during wound healing. Journal of the American College of Surgeons. 2012;215:S27. doi: 10.1016/j.jamcollsurg.2012.06.091. [DOI] [Google Scholar]
- 49.Shi Y, et al. Wnt and Notch signaling pathway involved in wound healing by targeting c-Myc and Hes1 separately. Stem cell research & therapy. 2015;6:120. doi: 10.1186/s13287-015-0103-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bedogni B, Warneke JA, Nickoloff BJ, Giaccia AJ, Powell MB. Notch1 is an effector of Akt and hypoxia in melanoma development. The Journal of clinical investigation. 2008;118:3660–3670. doi: 10.1172/JCI36157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hopkinson SB, et al. Focal Contact and Hemidesmosomal Proteins in Keratinocyte Migration and Wound Repair. Advances in wound care. 2014;3:247–263. doi: 10.1089/wound.2013.0489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tsuruta D, Hashimoto T, Hamill KJ, Jones JC. Hemidesmosomes and focal contact proteins: functions and cross-talk in keratinocytes, bullous diseases and wound healing. Journal of dermatological science. 2011;62:1–7. doi: 10.1016/j.jdermsci.2011.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Saras J, Wollberg P, Aspenstrom P. Wrch1 is a GTPase-deficient Cdc42-like protein with unusual binding characteristics and cellular effects. Experimental cell research. 2004;299:356–369. doi: 10.1016/j.yexcr.2004.05.029. [DOI] [PubMed] [Google Scholar]
- 54.Fort P, et al. Activity of the RhoU/Wrch1 GTPase is critical for cranial neural crest cell migration. Developmental biology. 2011;350:451–463. doi: 10.1016/j.ydbio.2010.12.011. [DOI] [PubMed] [Google Scholar]
- 55.Ory S, Brazier H, Blangy A. Identification of a bipartite focal adhesion localization signal in RhoU/Wrch-1, a Rho family GTPase that regulates cell adhesion and migration. Biology of the cell. 2007;99:701–716. doi: 10.1042/BC20070058. [DOI] [PubMed] [Google Scholar]
- 56.Shutes A, Berzat AC, Chenette EJ, Cox AD, Der CJ. Biochemical analyses of the Wrch atypical Rho family GTPases. Methods in enzymology. 2006;406:11–26. doi: 10.1016/S0076-6879(06)06002-2. [DOI] [PubMed] [Google Scholar]
- 57.Avraham H, Park SY, Schinkmann K, Avraham S. RAFTK/Pyk2-mediated cellular signalling. Cellular signalling. 2000;12:123–133. doi: 10.1016/S0898-6568(99)00076-5. [DOI] [PubMed] [Google Scholar]
- 58.Park SY, Li H, Avraham S. RAFTK/Pyk2 regulates EGF-induced PC12 cell spreading and movement. Cellular signalling. 2007;19:289–300. doi: 10.1016/j.cellsig.2006.07.005. [DOI] [PubMed] [Google Scholar]
- 59.Wozniak MA, Modzelewska K, Kwong L, Keely PJ. Focal adhesion regulation of cell behavior. Bba-Mol Cell Res. 2004;1692:103–119. doi: 10.1016/j.bbamcr.2004.04.007. [DOI] [PubMed] [Google Scholar]
- 60.Lian X, Yang L, Gao Q, Yang T. IL-1alpha is a potent stimulator of keratinocyte tissue plasminogen activator expression and regulated by TGF-beta1. Archives of dermatological research. 2008;300:185–193. doi: 10.1007/s00403-007-0828-8. [DOI] [PubMed] [Google Scholar]
- 61.Morioka S, Lazarus GS, Baird JL, Jensen PJ. Migrating keratinocytes express urokinase-type plasminogen activator. The Journal of investigative dermatology. 1987;88:418–423. doi: 10.1111/1523-1747.ep12469754. [DOI] [PubMed] [Google Scholar]
- 62.Planus E, et al. Binding of urokinase to plasminogen activator inhibitor type-1 mediates cell adhesion and spreading. Journal of cell science. 1997;110(Pt 9):1091–1098. doi: 10.1242/jcs.110.9.1091. [DOI] [PubMed] [Google Scholar]
- 63.Romer J, et al. The receptor for urokinase-type plasminogen activator is expressed by keratinocytes at the leading edge during re-epithelialization of mouse skin wounds. The Journal of investigative dermatology. 1994;102:519–522. doi: 10.1111/1523-1747.ep12373187. [DOI] [PubMed] [Google Scholar]
- 64.Hebert CA, Baker JB. Linkage of extracellular plasminogen activator to the fibroblast cytoskeleton: colocalization of cell surface urokinase with vinculin. The Journal of cell biology. 1988;106:1241–1247. doi: 10.1083/jcb.106.4.1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Pollanen J, Hedman K, Nielsen LS, Dano K, Vaheri A. Ultrastructural localization of plasma membrane-associated urokinase-type plasminogen activator at focal contacts. The Journal of cell biology. 1988;106:87–95. doi: 10.1083/jcb.106.1.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wilcox-Adelman SA, Wilkins-Port CE, McKeown-Longo PJ. Localization of urokinase type plasminogen activator to focal adhesions requires ligation of vitronectin integrin receptors. Cell adhesion and communication. 2000;7:477–490. doi: 10.3109/15419060009040305. [DOI] [PubMed] [Google Scholar]
- 67.Sturge J, Wienke D, East L, Jones GE, Isacke CM. GPI-anchored uPAR requires Endo180 for rapid directional sensing during chemotaxis. The Journal of cell biology. 2003;162:789–794. doi: 10.1083/jcb.200302124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Chandrasekar N, et al. Downregulation of uPA inhibits migration and PI3k/Akt signaling in glioblastoma cells. Oncogene. 2003;22:392–400. doi: 10.1038/sj.onc.1206164. [DOI] [PubMed] [Google Scholar]
- 69.Mohanam S, et al. Stable transfection of urokinase-type plasminogen activator antisense construct modulates invasion of human glioblastoma cells. Clinical cancer research: an official journal of the American Association for Cancer Research. 2001;7:2519–2526. [PubMed] [Google Scholar]
- 70.Pulukuri SM, et al. RNA interference-directed knockdown of urokinase plasminogen activator and urokinase plasminogen activator receptor inhibits prostate cancer cell invasion, survival, and tumorigenicity in vivo. The Journal of biological chemistry. 2005;280:36529–36540. doi: 10.1074/jbc.M503111200. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 71.Shen Y, et al. Mice deficient in urokinase-type plasminogen activator have delayed healing of tympanic membrane perforations. PloS one. 2012;7:e51303. doi: 10.1371/journal.pone.0051303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zong H, Wang F, Fan QX, Wang LX. Curcumin inhibits metastatic progression of breast cancer cell through suppression of urokinase-type plasminogen activator by NF-kappa B signaling pathways. Molecular biology reports. 2012;39:4803–4808. doi: 10.1007/s11033-011-1273-5. [DOI] [PubMed] [Google Scholar]
- 73.Carmeliet P, et al. Urokinase-generated plasmin activates matrix metalloproteinases during aneurysm formation. Nature genetics. 1997;17:439–444. doi: 10.1038/ng1297-439. [DOI] [PubMed] [Google Scholar]
- 74.Grant GA, Eisen AZ, Marmer BL, Roswit WT, Goldberg GI. The activation of human skin fibroblast procollagenase. Sequence identification of the major conversion products. The Journal of biological chemistry. 1987;262:5886–5889. [PubMed] [Google Scholar]
- 75.Ishida T, Tsukada H, Hasegawa T, Yoshizawa H, Gejyo F. Matrix metalloproteinase-1 activation via plasmin generated on alveolar epithelial cell surfaces. Lung. 2006;184:15–19. doi: 10.1007/s00408-005-2557-0. [DOI] [PubMed] [Google Scholar]
- 76.Knauper V, et al. Cellular mechanisms for human procollagenase-3 (MMP-13) activation. Evidence that MT1-MMP (MMP-14) and gelatinase a (MMP-2) are able to generate active enzyme. The Journal of biological chemistry. 1996;271:17124–17131. doi: 10.1074/jbc.271.29.17124. [DOI] [PubMed] [Google Scholar]
- 77.Legrand C, et al. uPA/plasmin system-mediated MMP-9 activation is implicated in bronchial epithelial cell migration. Experimental cell research. 2001;264:326–336. doi: 10.1006/excr.2000.5125. [DOI] [PubMed] [Google Scholar]
- 78.Liu Z, et al. Synergy between a plasminogen cascade and MMP-9 in autoimmune disease. The Journal of clinical investigation. 2005;115:879–887. doi: 10.1172/JCI23977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Mazzieri R, et al. Control of type IV collagenase activity by components of the urokinase-plasmin system: a regulatory mechanism with cell-bound reactants. The EMBO journal. 1997;16:2319–2332. doi: 10.1093/emboj/16.9.2319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Monea S, Lehti K, Keski-Oja J, Mignatti P. Plasmin activates pro-matrix metalloproteinase-2 with a membrane-type 1 matrix metalloproteinase-dependent mechanism. Journal of cellular physiology. 2002;192:160–170. doi: 10.1002/jcp.10126. [DOI] [PubMed] [Google Scholar]
- 81.Murphy G, et al. Mechanisms for pro matrix metalloproteinase activation. APMIS: acta pathologica, microbiologica, et immunologica Scandinavica. 1999;107:38–44. doi: 10.1111/j.1699-0463.1999.tb01524.x. [DOI] [PubMed] [Google Scholar]
- 82.Ramos-DeSimone N, et al. Activation of matrix metalloproteinase-9 (MMP-9) via a converging plasmin/stromelysin-1 cascade enhances tumor cell invasion. The Journal of biological chemistry. 1999;274:13066–13076. doi: 10.1074/jbc.274.19.13066. [DOI] [PubMed] [Google Scholar]
- 83.Santala A, Saarinen J, Kovanen P, Kuusela P. Activation of interstitial collagenase, MMP-1, by Staphylococcus aureus cells having surface-bound plasmin: a novel role of plasminogen receptors of bacteria. FEBS letters. 1999;461:153–156. doi: 10.1016/S0014-5793(99)01440-4. [DOI] [PubMed] [Google Scholar]
- 84.Stojadinovic O, et al. Deregulation of keratinocyte differentiation and activation: a hallmark of venous ulcers. Journal of cellular and molecular medicine. 2008;12:2675–2690. doi: 10.1111/j.1582-4934.2008.00321.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Yang, R. H. et al. Epidermal stem cells (ESCs) accelerate diabetic wound healing via the Notch signalling pathway. Bioscience reports36, doi:10.1042/BSR20160034 (2016). [DOI] [PMC free article] [PubMed]
- 86.Mori R, Power KT, Wang CM, Martin P, Becker DL. Acute downregulation of connexin43 at wound sites leads to a reduced inflammatory response, enhanced keratinocyte proliferation and wound fibroblast migration. Journal of cell science. 2006;119:5193–5203. doi: 10.1242/jcs.03320. [DOI] [PubMed] [Google Scholar]
- 87.Nam Y, Sliz P, Pear WS, Aster JC, Blacklow SC. Cooperative assembly of higher-order Notch complexes functions as a switch to induce transcription. Proceedings of the National Academy of Sciences of the United States of America. 2007;104:2103–2108. doi: 10.1073/pnas.0611092104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Na J, et al. Role of type II protein arginine methyltransferase 5 in the regulation of Circadian Per1 gene. PloS one. 2012;7:e48152. doi: 10.1371/journal.pone.0048152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Lee K, et al. Molecular mechanism of Jmjd3‐mediated interleukin‐6 gene regulation in endothelial cells underlying spinal cord injury. Journal of neurochemistry. 2012;122:272–282. doi: 10.1111/j.1471-4159.2012.07786.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


