Abstract
Background
The prognostic significance of adenosine-mediated dormant pulmonary vein conduction, and whether such dormant conduction should be eliminated, remains controversial. We sought to perform a meta-analysis of data from eligible studies to delineate the prognostic impact of adenosine-guided radiofrequency catheter ablation of atrial fibrillation.
Methods
A systematic literature search was performed using online databases in order to identify relevant studies from January 2004 to September 2016. Ten studies [six observational and four randomized control trials (RCTs)] were included in the analysis.
Results
Five studies (two observational and three RCTs) compared the efficacy of adenosine-mediated elimination of dormant conduction versus no adenosine test. Overall, the adenosine-guided ablation strategy displayed better long-term outcomes as compared with no adenosine testing (RR 1.08, 95% CI 1.01–1.14, p=0.02; Heterogeneity: I2=42%, p: 0.14). The meta-analysis of only RCTs failed to show any differences between the two strategies (RR 1.03, 95% CI 0.96–1.11, p=0.37; Heterogeneity: I2 0%, p: 0.41). Eight studies (five observational and three RCTs) addressed the efficacy of adenosine-induced dormant conduction and additional ablation versus no dormant conduction during adenosine challenge. Overall, a trend towards a better outcome in those without dormant conduction during drug challenge was noted (RR 0.89, 95% CI 0.77–1.03, p=0.11; Heterogeneity: I2 65% p: 0.006). The pooled analysis of RCTs failed to show any differences between the two arms (RR 0.90, 95% CI 0.62–1.30, p= 0.57; Heterogeneity: I2 88%, p: 0.0002).
Conclusions
Adenosine-guided radiofrequency catheter ablation of atrial fibrillation does not provide additional benefit in terms of freedom of arrhythmia recurrence.
Keywords: Ablation, Atrial fibrillation, Pulmonary veins, Adenosine, Dormant conduction
1. Introduction
Pulmonary vein isolation (PVI) has become the procedural end-point in patients undergoing left atrial ablation for symptomatic drug-refractory atrial fibrillation (AF) [1]. The aim of PVI is abolishment of all conducted electrical activity beyond the isolating lesions. Pulmonary vein recovery of conduction in at least one vein has been verified in up to 80% of patients undergoing a second ablation procedure, and seems to be the dominant mechanism of AF recurrence [2]. Acute pulmonary vein reconnection within 30 min after ablation is also commonly seen and has been associated with late AF recurrence [3]. Furthermore, pulmonary vein reconnection has been associated with histopathological evidences of non-transmural lesions along the ablation line. Non-transmural ablation may create a dynamic cellular substrate with features of reversible injury; interestingly, the reversibility of the thermal injury appears to be an important determinant of recovery of conduction and recovery from injury that may explain recurrences of AF following PVI [4]. Adenosine administration following acute PVI may unmask residual—so-called “dormant”—- conduction between the pulmonary veins and the left atrium [5]. Observational studies have offered conflicting results about the prognostic significance of dormant pulmonary vein conduction revealed by adenosine, and whether such dormant conduction should be eliminated [5], [7], [8], [9], [10], [11], [12]. Four recent randomized control trials (RCTs) have also given opposing results [13], [14], [15], [16]. In the light of such conflicting information, a systematic review of published data, including the recent randomized trials, appears to be timely and may provide the best way to determine the prognostic impact of adenosine-guided ablation of AF.
2. Methods
2.1. Search strategy
A systematic literature search was performed by two investigators (K.P.L. and S.G.) using the online databases of PubMed, Embase and the Web of Science in order to identify relevant studies from January 2004 to September 2016. We used the following keywords: “atrial fibrillation,” “ablation,” “adenosine,” “ATP,” “pulmonary vein isolation,” “pulmonary vein reconnection” and “dormant conduction.” Study titles and abstracts as well as reference lists were manually checked independently by two investigators. All potentially relevant reports were retrieved as complete manuscripts, and then their eligibility assessed according to the inclusion criteria. Any disagreements or uncertainties between the two investigators were resolved through consensus after rechecking the source data and consultation with a third investigator (T. L.).
2.2. Inclusion/exclusion criteria
This meta-analysis included observational and RCTs studies on human subjects published in the English language with the following primary objectives: (1) freedom from arrhythmia recurrence in patients who undergo additional radiofrequency ablation to eliminate adenosine-mediated dormant conduction compared to those who did not receive adenosine; and (2) freedom from arrhythmia recurrence in patients with adenosine-mediated dormant conduction and additional radiofrequency ablation as compared with those without pulmonary vein reconnection during adenosine testing. Patient characteristics (age, gender); AF status (paroxysmal AF, persistent AF, duration of AF); echocardiographic markers (left atrial size, left ventricular ejection fraction); details of the ablation procedure (PVI strategy, prior ablation, outcomes, duration of follow-up); and the adenosine protocol used were carefully assessed. For the purpose of this article, we used the term “adenosine” for all chemical preparations of adenosine that were clinically applied [e.g. adenosine triphosphate (ATP)]. Studies using single-shot ablation devices for AF ablation (cryoballoon and/or multielectrode phased-radiofrequency catheters) were excluded from the analysis.
2.3. Data extraction
The following information was extracted from the selected studies: (1) study characteristics (name of the first author, year of publication, journal, PMID, study design, mean follow-up duration); (2) baseline characteristics of study subjects (number of patients, age, sex, type of cardiomyopathy, type of AF, echocardiographic markers, other comorbidities, medication); (3) the incidence of dormant conduction provoked during adenosine testing; and, finally, (4) the main outcomes of each study (incidence of recurrent atrial tachyarrhythmias during the follow-up in each group).
2.4. Statistical analysis
Data analysis was performed using the Review Manager (RevMan) software, version 5.3. The risk ratio (RR) and corresponding 95% confidence interval (CI) were separately calculated by using the provided crude data to account for the arrhythmia-free survival of adenosine-guided PVI with or without dormant conduction, as well as conventional PVI. The statistical heterogeneity of the study was assessed by using the I2 index. We considered values around 25% (I2=25), 50% (I2=50) and 75% (I2=75) to be low, medium and high heterogeneity, respectively [17]. A random effect model was used in cases in which we had I2>50%. Funnel plots were constructed by using RevMan software to assess publication bias. P-values <0.05 were considered to be statistically significant.
2.5. Quality assessment
We assessed the methodological quality of the included RCTs by using elements included in the Cochrane collaboration tool for assessing risk of bias [18]. The domains used in the present systematic review pertained to randomization and allocation concealment (selection bias), blinding (performance and detection bias), and lost to follow-up and adherence to the intention-to-treat principle (attrition bias). The quality assessment of the observational studies was performed according to the Newcastle-Ottawa scale for assessing the quality of nonrandomized studies [19].
3. Results
3.1. Characteristics of the studies
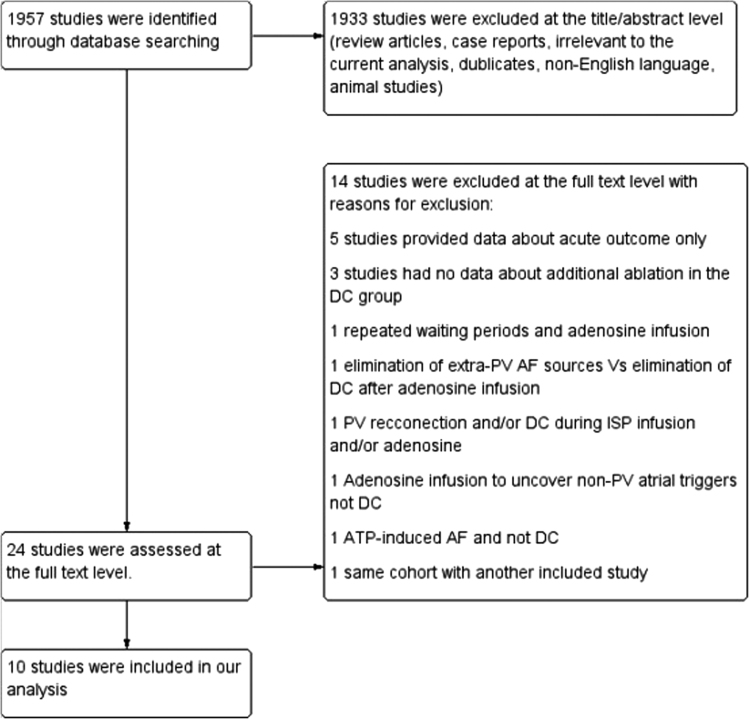
A flow diagram of the data search and study selection is presented in Fig. 1. After screening the titles and abstracts, 1957 records initially identified by the primary literature search, with 1933 studies excluded because they were either review articles, case reports, irrelevant to the current analysis, duplicates, not in the English language and/or not involving human subjects. A second review was performed in 24 studies and 14 of them were excluded. Ten studies (six observational and four RCTs) comprising 3785 patients (2876 males) were finally included in this meta-analysis [7], [8], [9], [10], [11], [12], [13], [14], [15], [16]. The baseline characteristics of the patients, the adenosine protocol used and the outcomes data of each study are summarized in Table 1. Paroxysmal AF was the predominant type of arrhythmia (75.5%), and the mean duration of AF was provided in six studies and ranged from three to five years. ATP was administered in five studies, in a dose ranging from 10 mg to 40 mg in four of them, while the dose was based on the body weight (0.4 mg/kg) in one study [8], [9], [10], [11], [14]. In the other five studies, adenosine was administered in dose that ranged from 6 mg to 24 mg [7], [12], [13], [15], [16]. The time of the drug challenge in relation to PVI varied significantly among the studies. As shown in Table 1, the test was performed either directly after PVI or after a waiting period of 10–57 min [7], [8], [9], [10], [11], [12], [13], [14], [15], [16]. The mean duration of follow-up ranged from 189 to 903 days. The primary endpoint was the recurrence of AF in five studies and the recurrence of AF or atrial tachyarrhythmias in the other five studies [7], [8], [9], [10], [11], [12], [13], [14], [15], [16]. There was a blanking period of three months postablation in four studies and one month in two studies [9], [11], [12], [13], [14], [15], [16]. Clinical visits were performed periodically in all patients, Holter monitoring was used in eight studies, event recorders in two studies and continuous mobile telemetry monitors in one study [7], [8], [9], [10], [11], [12], [13], [14], [15], [16].
Fig. 1.
Flow diagram of the trial selection process.
Table 1.
Clinical, procedural and outcome data of the studies included in the meta-analysis.
| Ref. | Study design | No of pts | Study groups | No of pts in each group | PAF | Age (years) | Males [%] | FU (days) | Duration of AF (years) | LA size (mm) | LVEF (%) | Prior ablation | Adenosine protocol | Primary end point | Freedom of primary endpoint | Repeat ablation |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Randomized control trials | ||||||||||||||||
| Efremidis et al.[16] | Prosp | 161 | Adenosine guided PVI | 80 | 80 | 54.17±10.71 | 58 (72.5) | 342±157.5 | 4.4±3.65 | 39.75±5.25 | 61.17±4.77 | 0 | 12–24 mg of adenosine after 30 min waiting period | Documented symptomatic or asymptomatic AF episodes lasting >30 sec or documented AT after a 3-month blanking period | 50 (62.5%) | 8 (10%) |
| Subgroup with DC and additional ablation | 26 | 12 (46.2%) | 4 (15.3%) | |||||||||||||
| Subgroup without DC | 54 | 38 (70.4%) | 4 (7.4%) | |||||||||||||
| No adenosine | 81 | 81 | 56.65±11.50 | 52 (64.2) | 341.7±149.4 | 4.59±4.26 | 38.70±4.61 | 61.67±4.95 | 0 | N/A | 54 (66.7%) | |||||
| Ghanbari et al.[15] | Prosp | 129 | Adenosine guided PVI | 61 | 61 | 59.7±8.7 | 37 (61) | 278.6±211.9 | NA | 41±5.3 | 59.7±5.4 | 20 (33) | 6–24 mg of adenosine for each PV and ISP at rates of 5,10,15 and 20 μg/min for 2 min at each infusion rate | Recurrence of AF | 37 (61%) | 12 (20%) |
| Subgroup with DC and additional ablation | 23 | |||||||||||||||
| Subgroup without DC | 38 | |||||||||||||||
| No adenosine | 68 | 68 | 58.9±10.7 | 53 (78) | 278.6±211.9 | N/A | 41.2±6.4 | 59.3±5.6 | 20 (29) | ISP infusion at same rates as above | 45 (66%) | 9 (43%) | ||||
| Kobori et al.[14] | Prosp | 2113 | Adenosine guided PVI | 1112 | 737 | 58.6±8.6 | 856 (77) | 365 | N/A | 38.9±6.3 | 64.2±7.9 | 0 | ATP 0.4 mg/kg body weight after a median waiting period of 57 [33–87] min | Recurrent AT lasting for 30 sec or those requiring repeat ablation, hospital admission, or usage of Vaughan Williams class I or III anti-arrhythmic drugs at 1 year with the blanking period of 90 days post-ablation | 625 (69%) | N/A |
| Subgroup with DC and additional ablation | 307 | 163 (64%) | N/A | |||||||||||||
| Subgroup without DC | 805 | 462 (71%) | N/A | |||||||||||||
| No adenosine | 1001 | 683 | 68.5±8.8 | 723 (73) | 365 | N/A | 39.2±6.2 | 64.6±7.3 | 0 | ISP infusion was not mandatory in the adenosine test | 533 (67%) | N/A | ||||
| Macle et al.[13] | Prosp | 401 | DC and additional ablation | 147 | 147 | 60.2±9.9 | 108 (74) | 368±43 | 4 (1.5–7) | 40.1±4.5 | 59.9±5.8 | 0 | 12 mg of adenosine after 20 min waiting period | Freedom from symptomatic AF, Af, AT after a single ablation procedure between 91–365 days after the procedure | 102 (69%) | 30 (20%) |
| DC, no further ablation | 137 | 137 | 58.4±9.7 | 97 (71) | 368±43 | 3.4 (1.7–8) | 39.6±5.9 | 60.1±7.1 | 0 | As above | 58 (42%) | 48 (35%) | ||||
| No DC | 117 | 117 | 58.9±10.9 | 87 (74) | 368±43 | 3 (1.3–8) | 40.1±4.9 | 59.1±6.6 | 0 | As above | 64 (56%) | N/A | ||||
| Observational studies | ||||||||||||||||
| Cheung et al.[12] | Prosp | 152 | DC and additional ablation | 44 | 29 | 62±9 | 34 | 374 | NA | 40±0.6 | 60±11 | 0 | 12 mg of adenosine without waiting period | Recurrence of AF was defined as any AT or AF recorded lasting ≥30 sec after a 3 month blanking period | 28 (64%) | 5 (11%) |
| (77) | (323–418) | |||||||||||||||
| No DC | 108 | 67 | 60±11 | 86 | 374 | NA | 43±0.7 | 59±11 | 0 | As above | 82 (76%) | 13 (12%) | ||||
| (80) | (323–418) | |||||||||||||||
| Miyazaki et al.[11] | Retrosp | 109 | DC and additional ablation | 39 | 39 | 59.4±10.3 | 33 (85) | 365 | 4.7±3.6 | 39.4±5.5 | 66.4±9 | N/A | 40 mg ATP without waiting period | Recurrence of AF after a 1 month blanking period after ablation | 20 (51%) | 10 (26%) |
| No DC | 70 | 70 | 61.4±11.2 | 58 (83) | 365 | 5.05±4.9 | 38.1±5.4 | 65.8±8.3 | N/A | 51 (73%) | 22 (31%) | |||||
| Matsuo et al.[9] | Retrosp | 233 | DC and additional ablation | 139 | 89 | 54.±9.6 | 122 (88) | 903±394 | 4.5±4 | 38.5±5.5 | 65.9±6.6 | N/A | 20 mg ATP after 20 min waiting period under ISP infusions at a rate of 5 up to 20 μg/min | Maintenance of SR (no sustained AT >30 sec) without AAD during the entire follow-up period (minimum 12 months) after a 1 month blanking period after ablation | 87 (63%) | 43 (31%) |
| No DC | 94 | 55 | 54.2±10.9 | 84 (89) | 903±394 | 4.3±3.7 | 39.7±5.7 | 65.8±7.4 | N/A | 62 (66%) | 28 (30%) | |||||
| Kumagai et al.[10] | Retrosp | 206 | Adenosine guided PVI | 106 | 94 | 58±11 | 74 (70) | 480±156 | 4.5±3.9 | 39.4±5.4 | 65.1±8.9 | N/A | 10 mg ATP during ISP infusion (5 μg/min) without waiting period | Recurrence of AF (sustained AF lasting more than 1 min) | 81 (76%) | 11 (10%) |
| Subgroup with DC and additional ablation | 54 | |||||||||||||||
| Subgroup without DC | 52 | |||||||||||||||
| No adenosine | 106 | 86 | 59±10 | 83 (78) | 480±207 | 5.0±5.5 | 39.7±5.7 | 63.8±9.6 | N/A | ISP infusion as above | 66 (62%) | 10 (9%) | ||||
| Hachiya et al.[8] | Retrosp | 252 | Adenosine guided PVI | 82 | 62 | 56±9 | 67 (82) | 183±99 | N/A | 41.7±6 | N/A | N/A | 30 mg ATP during ISP infusion (1–3 μg/min) without waiting period | Recurrence of AF | 60 (73%) | N/A |
| Subgroup with DC and additional ablation | 34 | 23 (68%) | ||||||||||||||
| Subgroup without DC | 48 | 37 (77%) | ||||||||||||||
| No adenosine | 170 | 135 | 54±9 | 143 (84) | 183±99 | N/A | 41.3±6 | N/A | N/A | 102 (60%) | N/A | |||||
| Tritto et al.[7] | Prosp | 29 | Adenosine induced PV activity | 16 | N/A | N/A | 12 mg of adenosine after 10 min waiting period | Recurrence of AF | 11 (69%) | |||||||
| No PV activity | 13 | 21 | 55.3±7.6 | 21 (72) | 189±72 | 5 (3–8) | 43.3±4.2 | 9 (69%) | 6 (21%) | |||||||
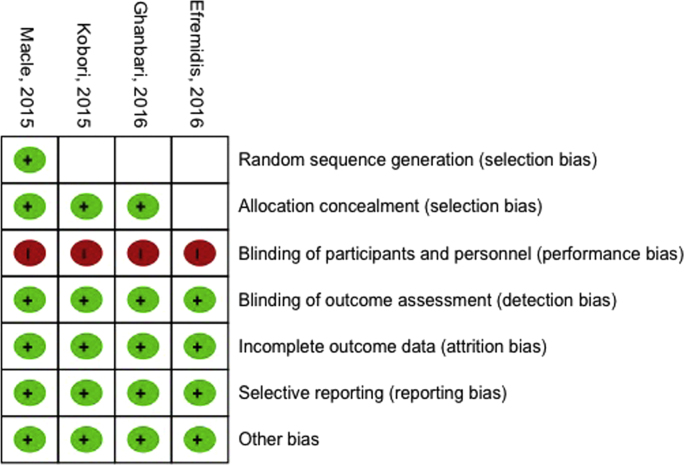
The assessment of the risk of bias in the RCTs is presented in Fig. 2. The random sequence generation was unclear for three of the included studies, while the allocation concealment was low risk in three studies and unclear in the last one. All studies demonstrated high risk for the blinding of participants and personnel, while were classified as low risk about the detection, attrition, reporting and other biases. When we assessed the six observational studies using the Newcastle-Ottawa scale for nonrandomized studies, all studies obtained a score of ≥5 stars.
Fig. 2.
Risk of bias assessment of each RCT.
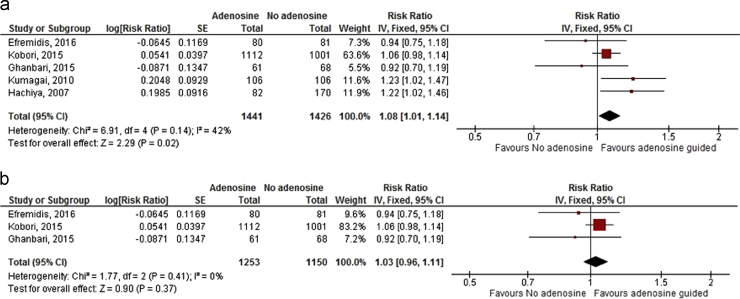
3.2. Elimination of adenosine-mediated dormant conduction versus no testing for dormant conduction
Five studies (two observational and three RCTs) encompassing 2867 patients (2146 males) compared the efficacy of the administration of adenosine and subsequent elimination of dormant conduction on top of the standard PVI versus no adenosine testing [8], [10], [14], [15], [16]. Paroxysmal AF was the predominant type of arrhythmia (72.8%). The mean left atrial diameter ranged between 38.7 mm and 41.7 mm, and the mean left ventricular ejection fraction was provided in four studies only and ranged between 59.3% and 65.1%. The mean follow-up period varied between 183 and 480 days with a blanking period of three months in two studies. The primary endpoint was the recurrence of AF in three studies and the recurrence of AF or atrial tachyarrhythmias in two studies [8], [10], [14], [15], [16]. The meta-analysis of all of the studies (including observational data) showed that adenosine-guided PVI is superior to no adenosine test strategy (RR 1.08, 95% CI 1.01–1.14, p=0.02; Heterogeneity: I2=42%, p: 0.14) (Fig. 3a). However, the pooled analysis of only the RCTs failed to show any differences between the two strategies (RR 1.03, 95% CI 0.96 1.11, p=0.37; Heterogeneity: I2 0%, p: 0.41) (Fig. 3b).
Fig. 3.
Forest plots of the meta-analysis. (a) Elimination of adenosine-mediated dormant conduction versus no adenosine testing (all studies). (b) Elimination of adenosine -mediated dormant conduction versus no adenosine test (only RCTs).
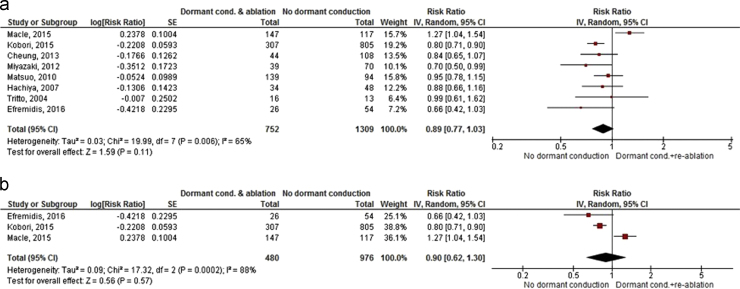
3.3. Adenosine-mediated dormant conduction and additional ablation versus no dormant conduction during the test
Eight studies (five observational and three RCTs) addressed the efficacy of elimination of adenosine-mediated dormant conduction versus no adenosine-mediated dormant conduction [7], [8], [9], [11], [12], [13], [14], [15], [16]. Τhe total number of patients was 2061 (1614 males), and 73.4% of them exhibited paroxysmal AF. The duration of AF was reported in five studies and ranged between three and five years. The mean left atrial diameter was provided in all studies and ranged between 38.1 mm and 43.3 mm and the mean left ventricular ejection fraction was provided in six studies and ranged between 59% and 66.4%. The mean follow-up was from 183 to 903 days with a blanking period of three months in four studies and one month in two studies. The primary endpoint was the recurrence of AF in three studies and the recurrence of AF or atrial tachyarrhythmias in five studies [7], [8], [9], [11], [12], [13], [14], [15], [16].
Overall, a trend towards a better outcome of patients without dormant conduction during adenosine challenge was seen as compared with those with adenosine-induced pulmonary vein reconnection and subsequent elimination of dormant conduction (RR 0.89, 95% CI 0.77–1.03, p=0.11). However, significant heterogeneity among these studies was noted (Heterogeneity: I2 65% p: 0.006) (Fig. 4a). The pooled analysis of only RCTs failed to show any significant differences between the two arms, with significant heterogeneity among studies (RR 0.90, 95% CI 0.62–1.30, p=0.57; Heterogeneity: I2 88%, p: 0.0002) (Fig. 4b).
Fig. 4.
Forest plots of the meta-analysis. (a) Adenosine-mediated dormant conduction and additional ablation versus no adenosine-mediated dormant conduction (all studies). (b) Adenosine-mediated dormant conduction and additional ablation versus no adenosine-mediated dormant conduction (only RCTs).
4. Discussion
The main findings of the present meta-analysis are the following: (1) that adenosine-guided elimination of dormant conduction as an adjunct to the standard PVI does not provide clinical benefits as compared with no adenosine testing in terms of arrhythmia recurrence. The pooled analysis of RCTs did not confirm the positive results of the initial analysis including all studies; and (2) that there is no difference in long-term outcomes in patients with adenosine-induced pulmonary vein reconnection and subsequent elimination of dormant conduction compared to those without dormant conduction during adenosine challenge.
4.1. Mechanistic concept underlying adenosine testing
Adenosine testing following successful PVI was first clinically applied in 2004 by Arentz and colleagues [5]. At the same time, a muscarinergic ionic current was identified in canine atria that hyperpolarize membrane potentials [20]. Radiofrequency ablation damages cardiac cells and leads to depolarization (i.e., less negative membrane potential) [6]. Adenosine selectively hyperpolarizes (i.e., pulls membrane potential to more negative values) canine pulmonary veins by increasing a muscarinergically activated repolarizing potassium (IKAdo) current [6]. Pulmonary veins with dormant conduction show less radiofrequency-induced depolarization than non-dormant veins do, allowing for adenosine-induced hyperpolarization to restore excitability by removing voltage-dependent sodium current (INa) inactivation at less negative membrane potentials. This reversal by hyperpolarization explains the restoration of conduction in dormant pulmonary veins [6]. Thus, in theory, adenosine testing could help to identify pulmonary veins with a high potential to reconnect.
4.2. Adenosine-guided AF ablation: results of observational studies
Adenosine testing reveals dormant conduction in 30% to 50% of patients with paroxysmal AF undergoing PVI [13], [15]. In the initial report, patients with acutely adenosine-“positive” pulmonary veins had a numerically higher rate of recovery of conduction at a second ablation procedure than adenosine-negative veins (71% vs.35%) [5]. Observational studies have given conflicting data regarding the prognostic significance of adenosine testing [5], [7], [8], [9], [10], [11], [12]. A previous meta-analysis of unadjusted retrospective observational studies showed that patients undergoing adenosine testing and ablation of dormant conduction displayed better long-term outcomes than those where adenosine testing was not used [21]. In addition, this analysis documented a tendency towards higher rates of AF recurrence despite additional ablation of dormant conduction, as compared with patients without adenosine-mediated pulmonary vein reconnection [21].
4.3. Adenosine-guided AF ablation: results of RCTs
Four recent randomized trials provided more reliable data, but have also given conflicting data on this topic [13], [14], [15], [16]. In the ADVICE multicentre randomized superiority trial, adenosine-guided ablation eliminated dormant conduction in 97% of patients, and led to an absolute risk reduction of 27.1% of arrhythmia recurrence as compared with patients with no further ablation. Patients without dormant pulmonary vein conduction displayed a better long-term outcome in relation to those with dormant conduction and no further ablation (55.7 vs. 42.3%, respectively) [13]. However, three recent RCTs have been published with the opposite findings. The UNDER-ATP trial randomly assigned 2113 patients with paroxysmal, persistent or long-lasting AF to either ATP-guided PVI or conventional PVI [14]. Additional radiofrequency energy applications successfully eliminated dormant conduction in 98.4% of these patients. However, at one year, 68.7% of patients in the ATP-guided PVI group and 67.1% of patients in the conventional PVI group were free from the primary endpoint, with no significant difference [14]. Similarly, Ghanbari et al. has shown that adenosine administration, and additional ablation of the gaps, does not improve the long-term outcomes of patients with paroxysmal AF undergoing PVI [15]. Efremidis et al. has demonstrated that adenosine-mediated pulmonary vein reconnection is predictive of future arrhythmic events [16]. However, elimination of dormant conduction with additional ablation lesions did not improve the long-term outcome of the procedure as compared with the standard PVI. A recent meta-analysis including both observational and RCTs concluded that adenosine-guided PVI is associated with lower rates of arrhythmia recurrence compared with conventional PVI [22]. However, there are significant differences from our meta-analysis. First, our meta-analysis included two additional RCTs [13], [16]. Second, we additionally addressed the clinical outcome of patients with adenosine-mediated dormant conduction and additional ablation versus no dormant conduction during adenosine challenge. Third, Chen et al. included four studies using single-shot ablation devices for AF ablation (three studies using cryoballoon and one study using PVAC), in contrast to our meta-analysis that encompasses only studies using point-by-point radiofrequency catheter ablation [22].
4.4. Adenosine testing at the index procedure and incidence of reconnected veins in repeated procedures
Adenosine may be effective in identifying acute pulmonary vein reconnections, but is not useful in identifying pulmonary veins that are likely to recover during follow-up. Matsuo et al. has demonstrated that there is no significant difference in the rate of reconnection in the repeated procedure between the pulmonary veins with or without dormant conduction in the initial procedure (53.8% vs. 58.9%) [9]. In particular, reconnection at the initial sites of conduction gaps was seen in only 26.7% of cases [9]. In a similar study, reconnection was observed in 70% of pulmonary veins without dormant conduction at the index procedure [11]. Another study by Lin et al. has shown that nearly half of pulmonary veins without dormant conduction at the index ablation will eventually develop chronic resumption of conduction [23]. Similarly, Ghanbari et al. have elegantly demonstrated that only 14% of the reconnected pulmonary veins identified during repeat procedures displayed dormant conduction with adenosine test at the initial procedure [15]. These results clearly underscore the inability of the adenosine test to predict the long-term reconnected veins at the second procedure. A high incidence of pulmonary vein reconnection is similarly observed in patients with and without recurrence of AF, suggesting that sustained PVI may not be required for freedom from clinical recurrence of AF [24]. Furthermore, the role of extra-pulmonary vein sources in AF becomes important in AF ablation procedures [25].
Adenosine-mediated dormant conduction is predictive of future arrhythmic events despite the elimination of dormant conduction [16]. Failure to achieve transmural lesions in patients with pulmonary vein reconnections after adenosine testing, despite re-ablation efforts, is the most plausible explanation. The thicker left atrial wall found at sites of adenosine-mediated dormant conduction is an explanation [26]. The use of contact force catheters that have been shown to reduce the prevalence of dormant conduction after PVI may overcome this limitation [27]. However, in a recent randomized trial, despite the reduction of adenosine-mediated acute pulmonary vein reconnection 60 min after PVI, the use of contact force catheters did not improve the long-term outcomes of the procedure [27]. This may possibly explain the low predictive value of adenosine testing.
4.5. When to perform the adenosine testing after pulmonary vein isolation?
Observation time following initial PVI plays a crucial role in the detection of pulmonary vein reconnection. Spontaneous recovery of the pulmonary veins is a time-dependent process and occurs approximately 30 min after the initial electrical PVI [3], [6]. Yamane et al. demonstrated that both spontaneous pulmonary vein and adenosine-induced reconnection were most frequently seen within 60 min after PVI [28]. In the ADVICE multicentre randomized superiority trial, the spontaneous pulmonary vein reconnection seen during a waiting period of 20 min after the PVI was successfully eliminated, and adenosine testing was subsequently performed [13]. On the contrary, in the UNDER-ATP trial, the drug challenge was performed after a median duration of 57 min following PVI [14]. It is therefore not surprising that spontaneous pulmonary vein reconnection was higher and that the adenosine-induced dormant conduction was lower in the UNDER-ATP trial as compared with the ADVICE trial. In the same line, Ganbari et al. have shown that the incidence of reconnection is significantly higher if adenosine is given <60 min after initial PVI than if it is given >60 min after isolation (75% vs. 9.4%) [15]. This may possibly explain the inconsistent findings among the studies included in the present meta-analysis, in which adenosine testing was performed either directly after PVI or after a waiting period ranging from 10 to 57 min. The implementation of a waiting period after PVI may improve the efficacy of adenosine-guided AF ablation. Immediately after PVI, adenosine testing may not be able to restore the hyperpolarization state required for excitability in ablated lesions. However, this may be possible after a waiting period of 30–60 min, which facilitates adenosine-induced hyperpolarization and restores conduction between pulmonary veins and left atrium.
5. Limitations
The present meta-analysis has limitations. First, there were only a small number of RCTs with different adenosine testing protocols available for inclusion. Accordingly, there was evidence of significant heterogeneity in the pooled analysis of RCTs (I2>50%) comparing the efficacy of adenosine-mediated dormant conduction and additional ablation versus no adenosine-mediated dormant conduction. Therefore, larger studies involving a homogenous population are needed. Second, a potential publication bias cannot be excluded. However, the asymmetrical funnel plot of the studies showed that there was not significant publication bias.
6. Conclusion
Adenosine-guided radiofrequency catheter ablation of atrial fibrillation does not provide additional benefit in terms of freedom of arrhythmia recurrence.
Conflict of Interest
All authors declare no conflict of interest related to this study.
References
- 1.Calkins H, Kuck KH, Cappato R, et al. h/EHRA/ECAS expert consensus statement on catheter and surgical ablation of atrial fibrillation: recommendations for patient selection, procedural techniques, patient management and follow-up, definitions, endpoints, and research trial design: a report of the Heart Rhythm Society (HRS) Task Force on Catheter and Surgical Ablation of Atrial Fibrillation. Developed in partnership with the European Heart Rhythm Association (EHRA), a registered branch of the European Society of Cardiology (ESC) and the European Cardiac Arrhythmia Society (ECAS); and in collaboration with the American College of Cardiology (ACC), American Heart Association (AHA), the Asia Pacific Heart Rhythm Society (APHRS), and the Society of Thoracic Surgeons (STS). Endorsed by the governing bodies of the American College of Cardiology Foundation, the American Heart Association, the European Cardiac Arrhythmia Society, the European Heart Rhythm Association, the Society of Thoracic Surgeons, the Asia Pacific Heart Rhythm Society, and the Heart Rhythm Society Heart Rhythm, 2012 (9). 2012. p. 632-696. [DOI] [PubMed]
- 2.Ouyang F., Bansch D., Ernst S. Complete isolation of left atrium surrounding the pulmonary veins: new insights from the double-Lasso technique in paroxysmal atrial fibrillation. Circulation. 2004;110:2090–2096. doi: 10.1161/01.CIR.0000144459.37455.EE. [DOI] [PubMed] [Google Scholar]
- 3.Efremidis M., Letsas K., Giannopoulos G. Early pulmonary vein reconnection as a predictor of left atrial ablation outcomes for paroxysmal atrial fibrillation. Europace. 2015;17:741–746. doi: 10.1093/europace/euu216. [DOI] [PubMed] [Google Scholar]
- 4.Kowalski M., Grimes M.M., Perez F.J. Histopathologic characterization of chronic radiofrequency ablation lesions for pulmonary vein isolation. J Am Coll Cardiol. 2012;59:930–938. doi: 10.1016/j.jacc.2011.09.076. [DOI] [PubMed] [Google Scholar]
- 5.Arentz T., Macle L., Kalusche D. "Dormant" pulmonary vein conduction revealed by adenosine after ostial radiofrequency catheter ablation. J Cardiovasc Electrophysiol. 2004;15:1041–1047. doi: 10.1046/j.1540-8167.2004.04031.x. [DOI] [PubMed] [Google Scholar]
- 6.Datino T., Macle L., Qi X.Y. Mechanisms by which adenosine restores conduction in dormant canine pulmonary veins. Circulation. 2010;121:963–972. doi: 10.1161/CIRCULATIONAHA.109.893107. [DOI] [PubMed] [Google Scholar]
- 7.Tritto M., De Ponti R., Salerno-Uriarte J.A. Adenosine restores atrio-venous conduction after apparently successful ostial isolation of the pulmonary veins. Eur Heart J. 2004;25:2155–2163. doi: 10.1016/j.ehj.2004.08.023. [DOI] [PubMed] [Google Scholar]
- 8.Hachiya H., Hirao K., Takahashi A. Clinical implications of reconnection between the left atrium and isolated pulmonary veins provoked by adenosine triphosphate after extensive encircling pulmonary vein isolation. J Cardiovasc Electrophysiol. 2007;18:392–398. doi: 10.1111/j.1540-8167.2006.00753.x. [DOI] [PubMed] [Google Scholar]
- 9.Matsuo S., Yamane T., Date T. Comparison of the clinical outcome after pulmonary vein isolation based on the appearance of adenosine-induced dormant pulmonary vein conduction. Am Heart J. 2010;160:337–345. doi: 10.1016/j.ahj.2010.05.025. [DOI] [PubMed] [Google Scholar]
- 10.Kumagai K., Naito S., Nakamura K. ATP-induced dormant pulmonary veins originating from the carina region after circumferential pulmonary vein isolation of atrial fibrillation. J Cardiovasc Electrophysiol. 2010;21:494–500. doi: 10.1111/j.1540-8167.2009.01667.x. [DOI] [PubMed] [Google Scholar]
- 11.Miyazaki S., Kuwahara T., Kobori A. Impact of adenosine-provoked acute dormant pulmonary vein conduction on recurrence of atrial fibrillation. J Cardiovasc Electrophysiol. 2012;23:256–260. doi: 10.1111/j.1540-8167.2011.02195.x. [DOI] [PubMed] [Google Scholar]
- 12.Cheung J.W., Lin F.S., Ip J.E. Adenosine-induced pulmonary vein ectopy as a predictor of recurrent atrial fibrillation after pulmonary vein isolation. Circ Arrhythm Electrophysiol. 2013;6:1066–1073. doi: 10.1161/CIRCEP.113.000796. [DOI] [PubMed] [Google Scholar]
- 13.Macle L., Khairy P., Weerasooriya R. ADVICE trial investigators. Adenosine-guided pulmonary vein isolation for the treatment of paroxysmal atrial fibrillation: an international, multicentre, randomised superiority trial. Lancet. 2015;386:672–679. doi: 10.1016/S0140-6736(15)60026-5. [DOI] [PubMed] [Google Scholar]
- 14.Kobori A., Shizuta S., Inoue K. Adenosine triphosphate-guided pulmonary vein isolation for atrial fibrillation: the UNmasking Dormant Electrical Reconduction by Adenosine TriPhosphate (UNDER-ATP) trial. Eur Heart J. 2015;36:3276–3287. doi: 10.1093/eurheartj/ehv457. [DOI] [PubMed] [Google Scholar]
- 15.Ghanbari H., Jani R., Hussain-Amin A. Role of adenosine after antral pulmonary vein isolation of paroxysmal atrial fibrillation: a randomized controlled trial. Heart Rhythm. 2016;13:407–415. doi: 10.1016/j.hrthm.2015.10.016. [DOI] [PubMed] [Google Scholar]
- 16.Efremidis M., Letsas K.P., Lioni L. Adenosine-guided pulmonary vein antral isolation for paroxysmal atrial fibrillation: a randomized study. J Cardiovasc Electrophysiol. 2016;27:1288–1292. doi: 10.1111/jce.13059. [DOI] [PubMed] [Google Scholar]
- 17.Huedo-Medina T.B., Sanchez-Meca J., Marin-Martinez F. Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychol Methods. 2006;11:193–206. doi: 10.1037/1082-989X.11.2.193. [DOI] [PubMed] [Google Scholar]
- 18.Higgins J.P., Altman D.G., Gotzsche P.C. The Cochrane Collaboration׳s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wells G, Shea B, O׳Connell D et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa: Ottawa Hospital Research Institute. 〈http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp〉.
- 20.Ehrlich J.R., Cha T.J., Zhang L. Characterization of a hyperpolarization-activated time-dependent potassium current in canine cardiomyocytes from pulmonary vein myocardial sleeves and left atrium. J Physiol. 2004;557:583–597. doi: 10.1113/jphysiol.2004.061119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McLellan A.J., Kumar S., Smith C. The role of adenosine following pulmonary vein isolation in patients undergoing catheter ablation for atrial fibrillation: a systematic review. J Cardiovasc Electrophysiol. 2013;24:742–751. doi: 10.1111/jce.12121. [DOI] [PubMed] [Google Scholar]
- 22.Chen Y.H., Lin H., Xie C.L. Role of adenosine-guided pulmonary vein isolation in patients undergoing catheter ablation for atrial fibrillation: a meta-analysis. Europace. 2016 doi: 10.1093/europace/euw201. [Oct 12] [DOI] [PubMed] [Google Scholar]
- 23.Lin F.S., Ip J.E., Markowitz S.M. Limitations of dormant conduction as a predictor of atrial fibrillation recurrence and pulmonary vein reconnection after catheter ablation. Pacing Clin Electrophysiol. 2015;38:598–607. doi: 10.1111/pace.12596. [DOI] [PubMed] [Google Scholar]
- 24.Jiang R.H., Po S.S., Tung R. Incidence of pulmonary vein conduction recovery in patients without clinical recurrence after ablation of paroxysmal atrial fibrillation: mechanistic implications. Heart Rhythm. 2014;11:969–976. doi: 10.1016/j.hrthm.2014.03.015. [DOI] [PubMed] [Google Scholar]
- 25.Chang H.Y., Lo L.W., Lin Y.J. Long-term outcome of catheter ablation in patients with atrial fibrillation originating from non-pulmonary vein ectopy. J Cardiovasc Electrophysiol. 2013;24:250–258. doi: 10.1111/jce.12036. [DOI] [PubMed] [Google Scholar]
- 26.Iso K., Okumura Y., Watanabe I. Wall thickness of the pulmonary vein-left atrial junction rather than electrical information as the major determinant of dormant conduction after contact force-guided pulmonary vein isolation. J Interv Card Electrophysiol. 2016;46:325–333. doi: 10.1007/s10840-016-0147-0. [DOI] [PubMed] [Google Scholar]
- 27.Ullah W., McLean A., Tayebjee M.H. Randomized trial comparing pulmonary vein isolation using the SmartTouch catheter with or without real-time contact force data. Heart Rhythm. 2016;13:1761–1767. doi: 10.1016/j.hrthm.2016.05.011. [DOI] [PubMed] [Google Scholar]
- 28.Yamane T., Matsuo S., Date T. Repeated provocation of time- and ATP-induced early pulmonary vein reconnections after pulmonary vein isolation: eliminating paroxysmal atrial fibrillation in a single procedure. Circ Arrhythm Electrophysiol. 2011;4:601–608. doi: 10.1161/CIRCEP.110.960138. [DOI] [PubMed] [Google Scholar]