Abstract
To investigate patient outcomes following hospitalization for out-of-hospital cardiac arrest (OHCA) in the United States. We used the 2002 to 2013 Nationwide Inpatient Sample database to identify adults ≥ 18 years old with an ICD-9-CM principal diagnosis code of cardio-respiratory arrest (427.5) or ventricular fibrillation (VF) (427.41). In 4 pre-defined federal geographic regions: Northeast, Midwest, South and West, means and proportions of survival, survival stratified by initial rhythm, hospital charges and cost were estimated. Multiple linear and logistic regression models were conducted. Of 154,177 OHCA patients hospitalized in the U.S, 25,873 (16.8%) were in the Northeast, 38,296 (24.8%) in the Midwest, 57,305 (37.2%) in the South, and 32,703 (21.2%) in the West. Variability in survival was noted in VF arrests; compared to the Northeast, survival was higher in the Midwest and South [AOR 1.16, 95% CI (1.02–1.32) and AOR 1.24, 95% CI (1.09–1.40) respectively], with no difference detected in the West [AOR 0.93, 95% CI (0.82–1.06)]. No variability in survival was noted following non-VF arrests (p > 0.05). Hospital charges rose significantly across all regions of the United States (P-trend < 0.001), and were higher in the West as compared with the Northeast [(Hospital charges >$109,000/admission, AOR 1.76; 95% CI (1.50–2.06)]. In conclusion, Nationwide, we observed significant regional variability in survival of hospitalized patients following out of hospital VF cardiac arrest, no survival variability following non-VF arrests and a steady increase in hospital charges.
Keywords: Cardiopulmonary Resuscitation, Cardiac Arrest, Cost and Resource Utilization, Regional Variation
Investigators have reported regional variations in the incidence and survival following Out-of-Hospital Cardiac Arrest (OHCA) in 10 US and Canadian resuscitation centers.1,2 More recently, Girotra et al have examined variations in survival following OHCA across 31 US states.3 Data from these studies, resulted from cardiac arrest registries that focused primarily on centers of excellence that are highly resourced and motivated to specifically target improved outcomes. Outcomes from the broad national population remain unknown; therefore, in an effort to reflect real-life experience of the total United States population, we sought to study regional variation in survival, total hospital charges and total hospital cost following OHCA in the Nationwide Inpatient Sample.
Methods
Data were obtained from the 2002–2013 Healthcare Cost and Utilization Project Nationwide Inpatient Sample. Annually, the Nationwide Inpatient Sample collects data covering 7–8 million hospital stays, reflecting all discharges from ~1000 hospitals. The database contains patient-level hospital discharge data provided by States that participate in the Agency for Healthcare Research and Quality's Project (n=44 in 2013). Using a sampling probability of ~20%, the design of the Nationwide Inpatient Sample is stratified and includes U.S. non-rehabilitation, community hospitals, with the target universe being all acute care hospital discharges in the United States.4,5
We used the International Classification of Diseases, Ninth Edition Clinical Modification (ICD-9-CM) codes of cardio-respiratory arrest (427.5) or ventricular fibrillation (427.41) to identify adults ≥ 18 years of age with a principal diagnosis of OHCA. These codes have been used in prior studies to identify patients with out-of-hospital cardiac arrest.6, 7 Prior studies of state-wide databases as well as Medicare/Medicaid claims data have shown ICD-9-CM codes, using principal diagnosis, to be reliable in accurately identifying patients with OHCA.8–10 All patients with concomitant diagnosis of injury were excluded. This selection process yielded a final sample of 154,177 OHCA patients (Supplemental-eFigure1). The Johns Hopkins University School of Medicine’s Institutional Review Board granted a waiver for this study.
Four key outcomes of interest were examined: (A) Survival to hospital discharge, overall and by arrest rhythm, (B) Length of hospital stay (days), (C) Total hospital charges (US $) and (D) Total hospitalization cost (US $). Hospital charges and cost were adjusted for inflation using the 2015 consumer price index. Other secondary outcomes were: (E) Discharge disposition, and (F) use of Percutaneous Coronary Intervention (PCI). Patients’ characteristics studied across the 4 pre-defined federal geographic regions (Northeast, Midwest, South and West), included patient age, gender, race, primary payer, house hold income, co morbidities (hypertension, diabetes, coronary artery disease, congestive heart failure, peripheral vascular disease, chronic pulmonary disease, metastatic cancer, chronic anemia, liver disease, renal failure, drug abuse and alcohol use, smoking, dyslipidemia, previous myocardial infarction, previous percutaneous coronary intervention, previous coronary artery bypass grafting, depression, atrial fibrillation, family history of coronary artery disease, carotid artery disease, previous cardiac arrest, family history of sudden cardiac death), and the Charlson co-morbidity index. Hospital-level characteristics were similarly studied and included size and location/teaching status. Relevant co-morbidities that were not readily available in the Nationwide Inpatient Sample were obtained using the appropriate ICD-9-CM codes (Supplemental eTable 1).
Statistical analyses were performed using Stata 13.0, accounting for survey design complexity, sampling weights, primary sampling units and strata. Consequently, population estimates of proportions, means and regression coefficients were obtained. Standard errors were estimated using Taylor series linearization. First, patient demographics, co-morbidities and hospital characteristics were compared across the 4 geographic regions using Pearson χ2 test for categorical variables and linear regression (1-way ANOVA) for continuous variables. Second, means and proportions of outcomes of interest were similarly compared. Third, multiple logistic regression models were conducted to examine the association between geographic regions and outcomes of interest. These models were adjusted for age, sex, race, arrest rhythm, income, primary payer, Charlson co-morbidity index, hospital size and hospital location/teaching status. Adding calendar year to the model, adjusted trends in outcomes were estimated taking 2002 as the referent year. In a third multiple logistic regression model, those trends were compared across regions with continuous Year (centered at 2006=median year), categorical region and Year×Region interaction terms added along with potentially confounding covariates. Fourth, regional differences in survival were examined by rhythm type, adjusting for the same covariates in addition to PCI use. Other related secondary analyses were also conducted to examine linear trends in survival, hospital charges and cost using multiple linear and logistic regression models with continuous year as the main predictor and stratifying the models by geographic region. Additional details on statistical analyses can be found in the supplemental file. All P values were 2 sided and type I error was set at 0.05.
Results
Our study included 154,177 OHCA patients who survived to hospital admission, with mean age 66.2 ±0.1 years and 59 % males. Of those patients, 78,540 (51%) had ventricular fibrillation while 75,637 (49%) patients had non-VF as initial arrest rhythm, with no regional differences in type of initial rhythm (p > 0.05). Compared to the Northeast, the South had a higher proportion of African American, the Midwest had a higher proportion of Caucasian, and the West had a higher proportion of Hispanics and Asians.
Patients in the West were less likely to have Medicare as a primary payer and more likely to have Medicaid and private insurance. Patients in the South had the lowest proportion of patients with a household income in the highest quartile. The regional distribution of other co-morbidities and Charlson co-morbidity index are presented in (Table1 and Supplemental eTable 2).
Table 1.
Regional Baseline Characteristics of Patients with Out-of-hospital Cardiac Arrest.
| Characteristics | All Patients | Northeast | Midwest | South | West | P Value | |
|---|---|---|---|---|---|---|---|
| (n=154,177) | (n=25,873) | (n=38,296) | (n=57,305) | (n=32,703) | |||
| Initial arrest Rhythm | |||||||
| Non-Ventricular fibrillation | 75,637 (49%) | 12,478 (48%) | 18,882 (49%) | 29,244 (51%) | 15,033 (46%) | 0.34 | |
| Ventricular fibrillation | 78,540 (51%) | 13,395 (52%) | 19,414 (51%) | 28,061 (49%) | 17,670 (54%) | 0.34 | |
| Age, Mean ±SE | 66.2 ±0.1 | 67.4±0.3 | 66.4±0.2 | 65.8±0.2 | 65.8±0.2 | <0.001 | |
| Male | 91,215 (59%) | 15,202 (59%) | 22,960 (60%) | 32,854 (57%) | 20,199 (62%) | 0.10 | |
| White | 113,713 (74%) | 19,970 (77%) | 30,616 (80%) | 40,425 (70.5%) | 22,703 (69%) | <0.001 | |
| Black | 25,157 (16%) | 4,055 (16%) | 6,071 (16%) | 11,918 (21%) | 3,113 (9.5%) | ||
| Hispanic | 10,846 (7%) | 1,447 (6%) | 1,078 (3%) | 4,156 (7%) | 4,165 (13%) | ||
| Asian/Pacific Islander | 3,482 (2%) | 334 (1.3%) | 308 (0.8%) | 466 (0.8%) | 2,374 (7%) | ||
| Native American | 979 (0.6%) | 67 (0.3%) | 223 (0.6%) | 340 (0.6%) | 348 (1%) | ||
| Household income | 0.007 | ||||||
| 1st quartile for zip code | 41,276 (27%) | 4,931 (19%) | 9,188 (24%) | 21,386 (37%) | 5,770 (18%) | ||
| 2nd quartile for zip code | 39,456 (26%) | 5,382 (21%) | 11,072 (29%) | 15,492 (27%) | 7,510 (23%) | ||
| 3rd quartile for zip code | 37,892 (25%) | 6,342 (24.5%) | 10,480 (27%) | 12,108 (21%) | 8,962 (27%) | ||
| 4th quartile for zip code | 35,553 (23%) | 9,218 (36%) | 7,556 (20%) | 8,319 (14.5%) | 10,460 (32%) | ||
| Hospital size | 0.01 | ||||||
| Small | 17,670 (11.5%) | 3,716 (14%) | 4,754 (12%) | 5,778 (10%) | 3,423 (10.5%) | ||
| Medium | 38,700 (25%) | 7,267 (28%) | 8,751 (23%) | 14,342 (25%) | 8,339 (25.5%) | ||
| Large | 97,807 (63%) | 14,890 (57.5%) | 24,791 (65%) | 37,185 (65%) | 20,941 (64%) | ||
| Hospital location/teaching status | <0.001 | ||||||
| Rural | 18,097 (12%) | 1,813 (7%) | 5,089 (13%) | 8,644 (15%) | 2,551 (8%) | ||
| Urban, non-teaching | 68,253 (44%) | 8,443 (33%) | 13,224 (34.5%) | 27,080 (47%) | 19,506 (60%) | ||
| Urban, teaching | 67,117 (43.5%) | 15,617 (60%) | 19,602 (51%) | 21,349 (37%) | 10,549 (32%) | ||
| Missing | 710 (0.5%) | 0 (0%) | 380 (1%) | 233 (0.4%) | 97 (0.3%) | ||
| Comorbidities | |||||||
| Congestive heart failure | 2,092 (1.4%) | 334 (1.3%) | 491 (1.3%) | 817 (1.4%) | 450 (1.4%) | 0.68 | |
| Chronic pulmonary disease | 34,868 (23%) | 5,297 (20.5%) | 9,285 (24%) | 13,173 (23%) | 7,113 (22%) | 0.60 | |
| Diabetes, uncomplicated | 38,523 (25%) | 6,319 (24%) | 10,074 (26%) | 14,847 (26%) | 7,284 (22%) | <0.001 | |
| Drug abuse | 5,067 (3%) | 705 (2.7%) | 1,184 (3%) | 1,674 (3%) | 1,504 (5%) | <0.001 | |
| Hypertension | 76,588 (50%) | 12,578 (49%) | 19, 642 (51%) | 28,521 (50%) | 15,848 (48.5%) | 0.008 | |
| Coronary artery disease | 59,657 (39%) | 10,209 (39%) | 15,823 (41%) | 21,318 (37%) | 12,307 (38%) | 0.001 | |
| Dyslipidemia | 37,796 (24.5%) | 6,225 (24%) | 10,301 (27%) | 13,435 (23%) | 7,835 (24%) | 0.07 | |
| Smoking | 26,335 (17%) | 3,459 (13%) | 7,089 (18.5%) | 9,832 (17%) | 5,956 (18%) | <0.001 | |
| Acute myocardial infarction | 16,088 (10%) | 2,559 (10%) | 3,995 (10%) | 5,912 (10%) | 3,622 (11%) | 0.11 | |
| Charlson Comorbidity Index | 0.04 | ||||||
| 0 | 38,142 (25%) | 6,221 (24%) | 9,284 (24%) | 13,838 (24%) | 8,799 (27%) | ||
| 1 | 42,835 (28%) | 7,395 (29%) | 10,192 (27%) | 16,148 (28%) | 9,101 (28%) | ||
| 2 | 32,816 (21%) | 5,704 (22%) | 8,263 (22%) | 12,448 (22%) | 6,401 (20%) | ||
| 3 | 19,179 (12%) | 3,173 (12%) | 5,092 (13%) | 7,072 (12%) | 3,841 (12%) | ||
| ≥4 | 21,205 (14%) | 3,381 (13%) | 5,465 (14%) | 7,799 (14%) | 4,561 (14%) | ||
n: number, %: percentage, SE: standard Error.
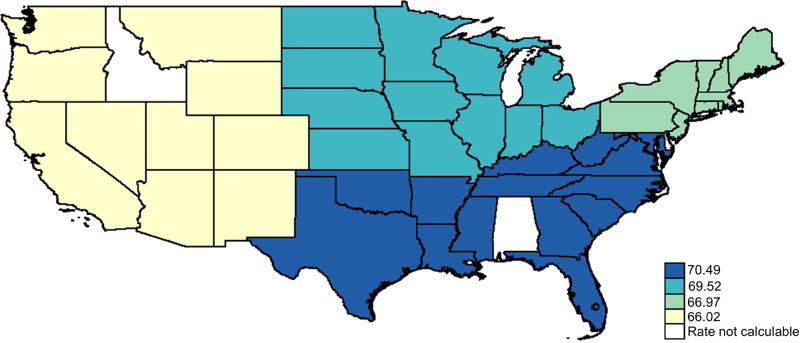
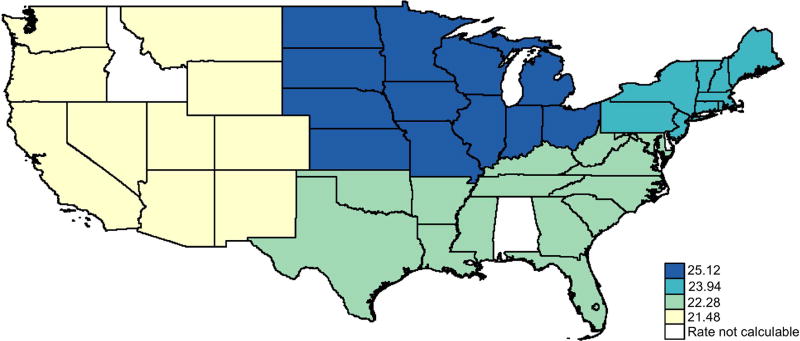
Overall, 45% were discharged alive and no significant regional difference in survival was detected (p = 0.64). Nevertheless, following adjustment, survival was significantly higher in the Midwest compared with the Northeast, marginally higher in the South and similar between the West and the Northeast (Supplemental eTable 3,4). After stratifying the total population by initial arrest rhythm, 70% of VF patients and only 15.5% of non-VF patients survived to hospital discharge. Survival in VF patients was higher in the Midwest and South compared to the Northeast, and not different in the West. There was no statistically significant regional variation in survival in the non-VF group (Figure 1A, B; Table 2).
Fig. 1.
Regional Risk-Adjusted (A)Ventricular Fibrillation, (B) Non-Ventricular Fibrillation Cardiac Arrest Survival in the United States: 2002–2013.
Table 2.
Regional Differences in Survival by Arrest Rhythm
| Northeast | Midwest | South | West | |
|---|---|---|---|---|
| Survival Outcome | (n=25,873) | (n=38,295) | (n=57,304) | (n=32,702) |
| Overall | ||||
| Survival to discharge | 11,317 (44%) | 17,655 (46%) | 25,417 (44%) | 14,408 (44%) |
| Unadjusted OR | reference | 1.10 (0.99–1.22) | 1.03 (0.93–1.13) | 1.01 (0.91–1.13) |
| Adjusted OR*† | reference | 1.12 (1.01–1.25) | 1.10 (0.99–1.21) | 0.90 (0.81–1.01) |
| Non-Ventricular Fibrillation | ||||
| Survival to discharge | 1,928/12,478 (15.5%) | 3,273/18,882 (17%) | 4,579/29,243 (16%) | 2,229/15,032 (15%) |
| Unadjusted OR | reference | 1.15 (0.98–1.35) | 1.02 (0.87–1.19) | 0.95 (0.80–1.14) |
| Adjusted OR* | reference | 1.04 (0.88–1.23) | 0.90 (0.77–1.06) | 0.86 (0.72–1.03) |
| Ventricular fibrillation | ||||
| Survival to discharge | 9,389/13,395 (70%) | 14,382/ 19,413 (74%) | 20,838/28,061 (74%) | 12,179/17,670 (69%) |
| Unadjusted OR | reference | 1.22 (1.07–1.38) | 1.23 (1.09–1.39) | 0.95 (0.83–1.07) |
| Adjusted OR* | reference | 1.16 (1.02–1.32) | 1.24 (1.09–1.40) | 0.93 (0.82–1.06) |
Adjusted for age, sex, race, income, primary payer, Charlson Comorbidity Index, hospital size and hospital location/teaching status, coronary artery disease, weekend admission, smoking, dyslipidemia, atrial fibrillation, dementia, carotid disease, previous percutaneous coronary intervention, previous coronary artery bypass grafting, previous cardiac arrest, family history of sudden arrest, family history of coronary artery disease, and percutaneous coronary intervention (on this admission).
Adjusted for initial rhythm
Overall survival to hospital discharge decreased over 12 years of study by an average of 2% annual decrement [AOR 0.98, 95% CI (0.97–0.99), P-trend < 0.001], while remaining stable in the Northeast and the West, slightly decreasing in the South and Midwest. When stratified by arrest rhythm, the decrease in survival trend was confined to the non-VF group for all regions combined as well as in each region separately. Additionally, no change was observed over the years in VF survival (Supplemental eTable5).
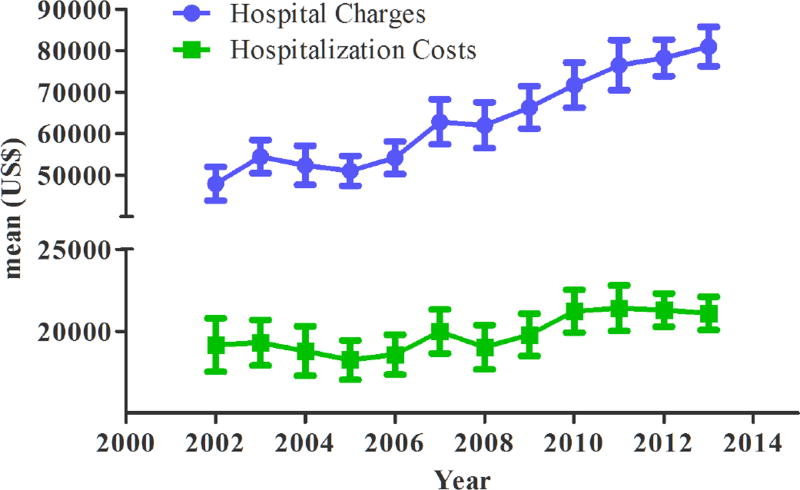
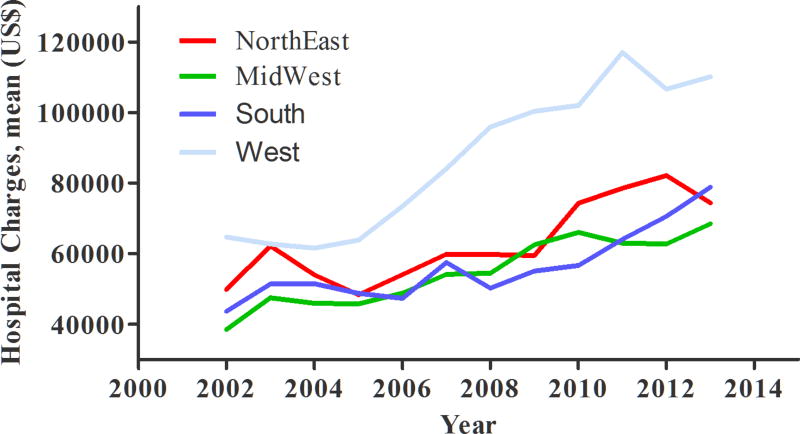
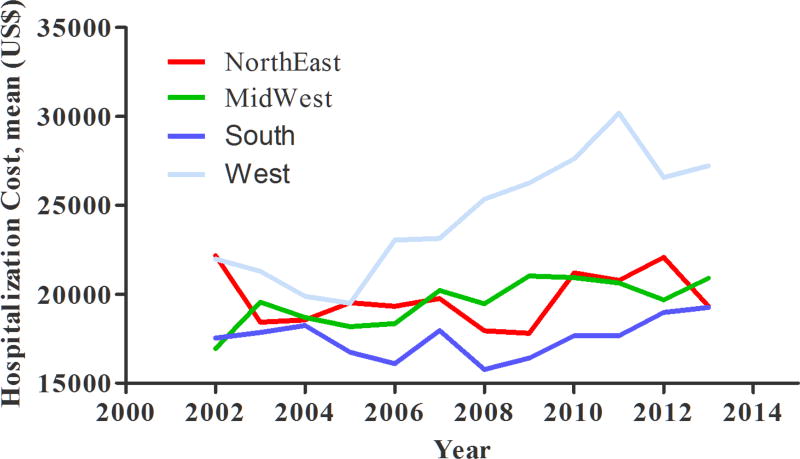
Mean total hospital charges per case was $63,826 while mean total hospitalization cost per case was $19,911. Both outcomes were highest in the West: $87,226 and $24,426, respectively (eTable 3). Similarly, following adjustment for key covariates including demographics, primary payer, co-morbidities and hospital characteristics, significantly higher cost and charges were observed in the West compared with the Northeast. Over the years, there was an increasing trend in both total hospital charges and total hospitalization cost (Figure 2A, B, C). This increase was confined to the Midwest and the West for hospitalization cost, with the West experiencing a significantly faster increase compared with the Northeast (interaction term Year×Hospital Region, p < 0.05) (Supplemental-eTable 4).
Fig. 2.
Trends in (A) Overall Hospital Charges and Hospitalization Costs, (B) Regional Hospital Charges, (C) Regional Hospital Costs in Out-of-hospital Cardiac Arrest patients in the United States: 2002–2013. Data is adjusted for inflation using the 2015 consumer price index.
Length of hospital stay was significantly lower in the West compared to the Northeast, and not different in other regions (eTable 4). Of all patients who survived to hospital discharge (68,798), 53.2% were discharged home, 17.4% discharged to short-term rehab, 20% discharged to skilled nursing facilities, 8.3% to home health care, and 1.1% to another facility. Discharge home was a more likely event in regions other than the Northeast (Supplemental eFigure2).
PCI following arrest was more likely to be used in the Midwest and the West compared to the Northeast, both overall and within the VF patient group (Supplemental eTable6).
Discussion
In this large nationally representative study of non-traumatic out-of-hospital cardiac arrest patients who survived to hospital admission, we observed regional variation in survival and expenditure. Survival rates following VF arrest were higher in the Midwest and the South compared with the Northeast, while hospital charges and costs were highest in the West and home discharge rates were higher in all regions compared with the Northeast. The use of PCI was more likely in the Midwest and the West compared with the Northeast. Regional variation in survival was evident following VF arrest. However, there were no regional differences in survival following non-VF arrest. The slight decreases in survival trends were confined to the non-VF group.
Regional variation in survival following OHCA arrest has been studied using quality improvement registries.1–3,11 Investigators reported regional variability in OHCA survival from 3% to 16.3%1, others reported survival variability at county level from 3.4% to 22%.3 The overall survival rate in our study of 45% (range from 44% in the Northeast to 46% in the Midwest) is derived from patients who survived to hospital admission after out-of-hospital cardiac arrest. The Nationwide Inpatient Sample database does not provide information about OHCA patients who died before hospital admission. Therefore, survival rates calculated in the Nationwide Inpatient Sample represent the proportion of hospitalized OHCA patients who were discharged alive (OHCA survival rate=Number of OHCA patients discharged alive/Total number of OHCA patients admitted to the hospital). Cardiac arrest registries estimate OHCA survival to hospital admission to be in the range of 14.3% to 20.8%.12 Therefore, the overall rate of survival to hospital discharge in our study would approximately range from 6.4% [14.3%×44.6%] to 9.3% [20.8%×44.6%] comparable to other rates reported in the literature.1–3 The higher survival rate noted in the Midwest was also evident in studies of in-hospital arrest using the same database 13 as well as other databases.14
This variation has been attributed to variability in patient demographics, cardiac arrest characteristics, bystander cardiopulmonary resuscitation, and the use of automated external defibrilator.1–3 Other important variables that would likely impact reported variability in survival include: Emergency Medical Services response time, quality of cardiopulmonary resuscitation, care withdrawal and the applications of life sustaining therapies post return of spontaneous circulation such as therapeutic hypothermia and early percutaneous coronary interventions. In our study, we were able to adjust for many variables including patient demographics, age, race, gender, social status, hospital characteristics, initial rhythm, acute myocardial infarction, co-morbidities and the use of percutaneous coronary interventions. The Nationwide Inpatient Sample does not provide pre-hospital information; therefore, the regional difference in survival of OHCA patients using this database would mainly reflect differences in post-arrest care following hospital admission.
The use of PCI following cardiac arrest of presumed cardiac etiology with or without ST elevation was recommended by the American Heart Association and the European Resuscitation Council 2015 guidelines.15,16 In our study, we accounted for the use of PCI and despite the increase in performing PCI following arrest, and its positive impact on survival,17,18 the low percentages of performed PCI following arrest might explain the small impact on survival noted in the adjusted models. Our data pre-dates the latest American Heart Association and the European Resuscitation Council guidelines recommending cardiac catheterization and PCI following cardiac arrest; therefore, a larger impact of PCI could be expected in the years following the 2015 guidelines.
The use of therapeutic hypothermia following out-of-hospital cardiac arrest has been shown to improve survival as well as neurologically intact survival.19 Therefore, the availability and variability in its use may impact reported outcomes.20 However, using ICD-9-CM codes for therapeutic hypothermia has not shown to be reliable,21 and thus we chose not to account for its use.
The poor survival rates noted following non-shockable rhythm, decrease trend of survival and the lack of regional variability is likely related to multiple factors namely increased co morbidity burden, treating sicker patients and limited therapeutic options following non-shockable rhythms. Reports of survival trends in the cardiac arrest registries indicated increase survival trends in both VF/VT and to a lesser degree in non-VF/VT rhythm.22 This improvement in centers of excellence might not be reflected in all hospitals nationally.
There was significant regional variation in total hospitalization cost and hospital charges with the highest cost and charges in the West. This increase in charges and cost is further perplexing to explain since the West had a lower length of hospital stay, and could be related to procedural costs, imaging, consultations, diagnostic and therapeutic procedures (PCI, therapeutic hypothermia and implantable cardioverter defibrillator). Identifying the specific driving factors for such increase is an important area for further research.
The significant regional variability in survival and expenditure noted in our study suggest that quality improvement efforts emphasizing post-arrest care may present an opportunity for improving overall survival and providing cost effective therapies. Indeed, the Institute of Medicine has put forth multiple strategies to improve quality of care and survival following cardiac arrest that can be accomplished by adopting models of excellence in high performing communities throughout the United States.23
There are limitations to our study; First, similar to other administrative databases, it is not possible to account for all treatment interventions and medications directly used in patient care. Therefore, the magnitude of such factors cannot be measured. The use of ICD-9-CM codes for therapeutic hypothermia is not reliable as previously mentioned, and the outpatient use of medications that decrease the incidence of cardiac arrest; such as Beta blockers 24 and statins,25 cannot be assessed. Second, there are no specific ICD-9-CM codes for Pulseless Electrical Activity and Asystole, therefore we considered those coded with ICD-9-CM code 427.5 as presenting with non-VF cardiac arrest. Third, the Nationwide Inpatient Sample database lacks pre-hospital variables (e.g. location of OHCA, time delay between the onset of OHCA and cardiopulmonary resuscitation, time to return of spontaneous circulation, bystander cardiopulmonary resuscitation, quality of cardiopulmonary resuscitation, time to defibrillation), which may vary among Emergency Medical Services systems and influence OHCA survival.26 Finally, the variability of care withdrawal following cardiac arrest would likely impact reported survival and was not captured by the database. That said it is still a valid, broad overview of national trends that can be used to better examine care and broadly identify areas of excellence, whose systems of care may warrant further detailed examination.
Supplementary Material
Acknowledgments
Funding Sources, and Acknowledgements:
This was work was supported in part by the Intramural Research Program of the National Institute on Aging, NIA/NIH/IRP.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Statement: Aiham Albaeni, May A. Beydoun, Hind A. Beydoun, Bolanle Akinyele, Lekshminarayan RaghavaKurup, Nisha Chandra-Strobos, and Shaker M. Eid declare no conflict of interest.
References
- 1.Nichol G, Thomas E, Callaway CW, Hedges J, Powell JL, Aufderheide TP, Rea T, Lowe R, Brown T, Dreyer J, Davis D, Idris A, Stiell I Resuscitation Outcomes Consortium Investigators. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300:1423–1431. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang HE, Devlin SM, Sears GK, Vaillancourt C, Morrison LJ, Weisfeldt M, Callaway CW ROC investigators. Regional variations in early and late survival after out-of-hospital cardiac arrest. Resuscitation. 2012;83:1343–1348. doi: 10.1016/j.resuscitation.2012.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Girotra S, Diepen SV, Nallamothu BK, Carrel M, Vellano K, Anderson ML, McNally B, Abella BS, Sasson C, Chan PS CARES Surveillance Group and the HeartRescue Project. Regional Variation in Out-of-Hospital Cardiac Arrest Survival in the United States. Circulation. 2016;133:2159–2168. doi: 10.1161/CIRCULATIONAHA.115.018175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.U.S. Agency for Healthcare Research and Quality. [Accessed June 18, 2016];Overview of the National (Nationwide) Inpatient Sample. Available at: https://www.hcup-us.ahrq.gov/nisoverview.jsp. Published February 2016.
- 5.U.S. Agency for Healthcare Research and Quality. HCUP Methods Series. [Accessed June 18, 2016];Nationwide Inpatient Sample Redesign Final Report. Available at : https://www.hcup-us.ahrq.gov/reports/methods/2014-04.pdf. Published April 4, 2014.
- 6.Jonhson NJ, Salhi RA, Abella BS, Neumar RW, Gaieski DF, Carr BG. Emergency department factors associated with survival after sudden cardiac arrest. Resuscitation. 2013;84:292–297. doi: 10.1016/j.resuscitation.2012.10.013. [DOI] [PubMed] [Google Scholar]
- 7.Mumma BE, Diercks DB, Danielsen B, Holmes JF. Probabilistic linkage of prehospital and outcomes data in out-of-hospital cardiac arrest. Prehosp Emerg Care. 2015;19:358–364. doi: 10.3109/10903127.2014.980474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hennessy S, Leonard CE, Freeman CP, Deo R, Newcomb C, Kimmel SE, Strom BL, Bilker WB. Validation of diagnostic codes for outpatient-originating sudden cardiac death and ventricular arrhythmia in Medicaid and Medicare claims data. Pharmacoepidemiol Drug Saf. 2010;19:555–562. doi: 10.1002/pds.1869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tamariz L, Harkins T, Nair V. A systematic review of validated methods for identifying ventricular arrhythmias using administrative and claims data. Pharmacoepidemiol Drug Saf. 2012;21(Suppl 1):148–153. doi: 10.1002/pds.2340. [DOI] [PubMed] [Google Scholar]
- 10.De Bruin ML, van Hemel NM, Leufkens HG, Hoes AW. Hospital discharge diagnoses of ventricular arrhythmias and cardiac arrest were useful for epidemiologic research. J Clin Epidemiol. 2005;58:1325–1329. doi: 10.1016/j.jclinepi.2005.04.009. [DOI] [PubMed] [Google Scholar]
- 11.Adabag S, Hodgson L, Garcia S, Anand V, Frascone R, Conterato M, Lick C, Wesley K, Mahoney B, Yannopoulos D. Outcomes of sudden cardiac arrest in a state-wide integrated resuscitation program: Results from the Minnesota Resuscitation Consortium. Resuscitation. 2017;110:95–100. doi: 10.1016/j.resuscitation.2016.10.029. [DOI] [PubMed] [Google Scholar]
- 12.Chan PS, McNally B, Tang F, Kellermann A CARES Surveillance Group. Recent trends in survival from out-of-hospital cardiac arrest in the United States. Circulation. 2014;18(130):1876–1882. doi: 10.1161/CIRCULATIONAHA.114.009711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kolte D, Khera S, Aronow WS, Palaniswamy C, Mujib M, Ahn C, Iwai S, Jain D, Sule S, Ahmed A, Cooper HA, Frishman WH, Bhatt DL, Panza JA, Fonarow GC. Regional variation in the incidence and outcomes of in-hospital cardiac arrest in the United States. Circulation. 2015;131:1415–1425. doi: 10.1161/CIRCULATIONAHA.114.014542. [DOI] [PubMed] [Google Scholar]
- 14.Girotra S, Nallamothu BK, Spertus JA, Li Y, Krumholz HM, Chan PS American Heart Association Get with the Guidelines-Resuscitation Investigators. Trend in survival after in-hospital cardiac arrest. NEngl J Med. 2012;367:1912–1920. doi: 10.1056/NEJMoa1109148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Neumar RW, Shuster M, Callaway CW, Gent LM, Atkins DL, Bhanji F, Brooks SC, de Caen AR, Donnino MW, Ferrer JM, Kleinman ME, Kronick SL, Lavonas EJ, Link MS, Mancini ME, Morrison LJ, O’Connor RE, Samson RA, Schexnayder SM, Singletary EM, Sinz EH, Travers AH, Wyckoff MH, Hazinski MF. Part 1: Executive Summary: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015;132:S315–S367. doi: 10.1161/CIR.0000000000000252. [DOI] [PubMed] [Google Scholar]
- 16.Nolan JP, Hazinski MF, Aickin R, Bhanji F, Billi JE, Callaway CW, Castren M, de Caen AR, Ferrer JM, Finn JC, Gent LM, Griffin RE, Iverson S, Lang E, Lim SH, Maconochie IK, Montgomery WH, Morley PT, Nadkarni VM, Neumar RW, Nikolaou NI, Perkins GD, Perlman JM, Singletary EM, Soar J, Travers AH, Welsford M, Wyllie J, Zideman DA. Part 1: Executive summary: 2015 international Consensus on cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Resuscitation. 2015;95:e1–31. doi: 10.1016/j.resuscitation.2015.07.039. [DOI] [PubMed] [Google Scholar]
- 17.Callaway CW, Schmicker RH, Brown SP, Albrich JM, Andrusiek DL, Aufderheide TP, Christenson J, Daya MR, Falconer D, Husa RD, Idris AH, Ornato JP, Rac VE, Rea TD, Rittenberger JC, Sears G, Stiell IG ROC Investigators. Early coronary angiography and induced hypothermia are associated with survival and functional recovery after out-of-hospital cardiac arrest. Resuscitation. 2014;85:657–663. doi: 10.1016/j.resuscitation.2013.12.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kern KB, Lotun K, Patel N, Mooney MR, Hollenbeck RD, McPherson JA, McMullan PW, Unger B, Hsu CH, Seder DB INTCAR-Cardiology Registry. Outcomes of comatose cardiac arrest survivors with and without ST-Segment elevation myocardial infarction: importance of coronary angiography. JACC Cardiovasc Interv. 2015;8:1031–1040. doi: 10.1016/j.jcin.2015.02.021. [DOI] [PubMed] [Google Scholar]
- 19.Nielsen N, Wetterslev J, Gronberg T, Erlinge D, Gasche Y, Hassager C, Horn J, Hovdenes J, Kjaergaard J, Kuiper M, Pellis T, Stammet P, Wanscher M, Wise MP, Aneman A, Al-Subaie N, Boesqaard S, Bro-Jeppesen J, Brunetti I, Bugge JF, Hingston CD, Juffermans NP, Koopmans M, Køber L, Langørgen J, Lija G, Møller JE, Rundgren M, Rylander C, Smid O, Werer C, Winkel P, Friberg H TTM Trial Investigators. Targeted temperature management at 33°C versus 36° C after cardiac arrest. N Engl J Med. 2013;369:2197–2206. doi: 10.1056/NEJMoa1310519. [DOI] [PubMed] [Google Scholar]
- 20.Merchant RM, Soar J, Skrifvars MB, Silfvast T, Edelson DP, Ahmad F, Huang KN, Khan M, Vanden Hoek TL, Becker LB, Abella BS. Theraputic hypothermia utilization among physicians after resuscitation from cardiac arrest. Crit Care Med. 2006;34:1935–1940. doi: 10.1097/01.CCM.0000220494.90290.92. [DOI] [PubMed] [Google Scholar]
- 21.Fugate JE, Brinjiki W, Manderkar JN, Cloft HJ, White RD, Wijdicks EF, Rabinstein AA. Post-cardiac arrest mortality is declining: a study of the US National Inpatient Sample 2001 to 2009. Circulation. 2012;126:546–550. doi: 10.1161/CIRCULATIONAHA.111.088807. [DOI] [PubMed] [Google Scholar]
- 22.Daya MR, Schmicker RH, Zive DM, Rea TD, Nichol G, Buick JE, Brooks S, Christenson J, MacPhee R, Craig A, Rittenberger JC, Davis DP, May S, Wigginton J, Wang H Resuscitation Outcomes Consortium Investigators. Out-of-hospital cardiac arrest survival improving over time: Results from the Resuscitation Outcomes Consortium (ROC) Resuscitation. 2015;91:108–115. doi: 10.1016/j.resuscitation.2015.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Institute of Medicine (IOM) [Accessed March ,2017];Report "Strategies to improve cardiac arrest survival: A time to act. 2015 Available at http://iom.nationalacademies.org/Reports/2015/Strategies-to-Improve-Cardiac-Arrest-Survival.aspx." Published June, 2015.
- 24.Domanski MJ, Krause-Steinrauf H, Massie BM, Deedwania P, Follmann D, Kovar D, Murray D, Oren R, Rosenberg Y, Young J, Zile M, Eichhorn E BEST Investigators. A comparative analysis of the results from 4 trials of beta-blocker therapy for heart failure: BEST, CIBIS-II, MERIT-HF, and COPERNICUS. J Card Fail. 2003;9:354–363. doi: 10.1054/s1071-9164(03)00133-7. [DOI] [PubMed] [Google Scholar]
- 25.Mitchell LB, Powell JL, Gillis AM, Kehl V, Hallstrom AP AVID Investigators. Are lipid-lowering drugs also antiarrhythmic drugs? An analysis of the Antiarrhythmics versus Implantable Defibrillators (AVID) trial. J Am Coll Cardiol. 2003;42:81–87. doi: 10.1016/s0735-1097(03)00498-4. [DOI] [PubMed] [Google Scholar]
- 26.Govindarajan P, Lin L, Landman A, McMullan JT, McNally BF, Crouch AJ, Sasson C. Practice variability among the EMS systems participating in cardiac arrest registry to enhance survival (CARES) Resuscitation. 2012;83:76–80. doi: 10.1016/j.resuscitation.2011.06.026. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.