Abstract
OBJECTIVE:
Healthcare-associated infections are one of the most important problems of all health institutions. This study was conducted to evaluate results of training about infection control measures provided to patients treated and hospitalized in clinics of obstetrics and gynecology, and to their relatives, as well as subsequent effect on infection rate.
METHODS:
The study was conducted in clinics of obstetrics and gynecology of a state hospital. Study group comprised midwives and nursing staff, and inpatients and their relatives. Survey made up of 16 questions was administered to patients and relatives before and after training provided by infection nurses. Survey with 18 questions was administered to midwives/nurses to evaluate compliance of patients and relatives with infection control measures. Study data were analyzed using statistical analysis software and findings were evaluated as numbers and percentages using Student’s t-test.
RESULTS:
According to survey of patients and relatives, mean knowledge level score before and after training was 20.07±46.76 and 96.36±11.85, respectively. Results indicated that training about infection control measures was effective at increasing knowledge level and compliance of patients and their relatives (p<0.05). Of the total, 87.5% of midwives/nurses stated that educating patients and relatives about infection control measures facilitated treatment and healthcare processes. In all, 95.9% of midwives/nurses thought that such education contributed to observance of infection control measures by patients and relatives.
CONCLUSION:
It is thought that regular education about infection control measures provided to patients and relatives would have positive effect and reduce incidence rate of healthcare-associated infection.
Keywords: Education, nosocomial infection, patients, relatives of patient
Healthcare-associated infection is among the most important indicators of the quality of healthcare delivered during hospitalization period. These infections have great impact on mortality and morbidity rates, threaten patient safety, prolong hospitalization, and increase healthcare expenses [1, 2]. Healthcare-associated infections are vital issue in monitoring and treatment processes of inpatients in both developed and developing countries [3]. In a report released by the Centers for Disease Control and Prevention (CDC) in 2016, nosocomial infections were considered to be most important preventable healthcare problem [4]. This report indicated that nearly 4% of patients in the USA had suffered from hospital-acquired infection, and in studies performed in other countries, incidence rate has ranged between 3.1% and 14.1% [4–6].
It is possible to prevent healthcare-associated infection with effective infection control programs [7]. In a CDC report published in 2009, it was reported that if minimal infection control measures were implemented in institutions where healthcare services and treatment are offered, 6% of all healthcare-associated infections could be prevented, and 32% could be avoided with thorough infection control program [8]. In 2007, the World Health Organization (WHO) established international standards for infection control programs. These standards involve monitoring outcomes of follow-up; training of healthcare professionals, patients, and patient relatives; compliance with hand hygiene; use of protective equipment; prevention of sharp injuries; clean environment; waste sorting; and cleaning and disinfection of equipment [6, 9]. In our country, scope of infection control measures became more comprehensive with “The Regulations for Infection Control Measures to be Implemented in Inpatient Treatment Institutes,” published in the Official Gazette on August 11, 2015 (Issue #25903). This regulation mandated establishment of infection control committees in every hospital. Infection control committees are held responsible for preparation of infection control program that is to encompass basic tasks, such as preparation of written infection control standards, training of healthcare personnel, follow-up, and determination of effectiveness of infection control programs based on data [10].
Training programs aimed at providing more qualified and cost-effective healthcare services and preventing accidents and errors by ensuring safety of the patients in hospitals are available [11]. Implementation of effective infection control measures can be achieved with compliance of not just healthcare professionals, but also participation of patients and their relatives. Educational courses for patients and their relatives provided within the context of the quality standards for healthcare mandated by the Ministry of Health are to include infection control measures related to hand hygiene [12]. In a study performed by McGuckin et al., hygiene program with infection control measures was prepared and training was provided for healthcare professionals and patients. As a result, frequency of handwashing increased by at least 50% [13]. Terzi et al. indicated that 82.9% of healthcare professionals had received training on infection control measures, and 63.2% of them expressed wishes to receive further training on preventive measures [14]. Training in infection control measures is inexpensive, and it is possible to increase awareness, knowledge level, and compliance of healthcare professionals, patients, and patients’ relatives. Luby et al. reported that training in use of soap and other methods of hand hygiene decreased incidence of impetigo by 34%, diarrheic diseases by 53%, and pneumonia by 50% [15, 16]. Since healthcare professionals have incomplete knowledge of the patient, and because family will likely have effect on health behaviors, sustained educational programs according to knowledge and skill level of healthcare professionals and patients should be implemented. Ineffective application of training programs for inpatients plays important role in development of hospital-acquired infection. Healthcare professionals receive in-service training, and patients and their relatives receive individualized and disease-specific training. In departments with heavy patient circulation, occasionally implementation of this program may prove difficult. Patient training programs to protect and maintain wellbeing of individuals and to develop behavioral changes should be instituted using systematic, programmed approach [17].
This study was performed to evaluate effect of training provided to inpatients and their relatives concerning infection control measures and to assess subsequent rate of infection.
MATERIALS AND METHODS
Study was quasi-experimental research performed at the clinics of obstetrics and gynecology of a special branch hospital between November 2015 and January 2016.
Using guidelines on infection control measures published by the WHO and the CDC, a guide with visual and written content was prepared by researchers, the “Information Guide for Patients and their Relatives on Infection Control Measures.” First page of the guide contained definition of hospital-acquired infection, general infection control measures, and illustrations on handwashing technique. In detailed table on second page, waste materials were classified and proper waste sorting was explained in detail. Third and fourth pages explained importance of handwashing, general hygiene practices, use of protective equipment, and rules that should be followed by companions attending to patient and visitors. Total of 197 patients and relatives were included in the study. Data collection form comprising 16 questions to determine knowledge level of the participants was created in line with information in the guide. Another data collection form was prepared by researchers to ask 24 participating midwives and nurses 18 questions designed to assess compliance of the patients and their relatives with infection control measures following training. In the first phase of the study, preliminary test consisting of 16 questions was administered to patients hospitalized in the clinics of obstetrics and gynecology in order to evaluate their baseline knowledge level of infection control measures. Following pretest, infection control nurses provided one-to-one training for the patients using the “Information Guide for Patients and their Relatives on Infection Control Measures.” Participants were retested on same day to evaluate knowledge. After completion of training and testing, guideline materials were given to the patients. Midwives and nurses working in the clinics of obstetrics and gynecology were requested to observe compliance during treatment and visiting hours and record findings in data collection survey form. They were asked to evaluate hand hygiene, change in use of hand antiseptic, proper waste sorting, and compliance with measures to be followed by those attending to or visiting patient. Data analysis was performed with SPSS Statistics for Windows, Version 22.0 (IBM Corp., Armonk, NY, USA) software using numbers and percentages, and analyzed using Student’s t-test. Approval of the Zeynep Kamil Maternity and Children’s Diseases Training and Research Hospital ethics committee, and institutional approval of the hospital were obtained before beginning the research. Objective of the survey was explained to employees of the unit and patients, and written, informed consent was obtained.
RESULTS
Sociodemographic characteristics of the patients and their relatives were examined. Mean age was 32.89±9.92 years. In study group, 60% were primary school graduates, and 82% were unemployed.
Fifty percent of participant nurses and midwives were in age group of 31-40 years. In all, 50% had bachelor’s degree, and 41.7% had work experience of ≥6 years.
Average knowledge level score of the patients and their relatives determined before and after training based on questionnaire form is displayed in Figure 1. Correlation between training provided on infection control measures and knowledge level of participants (p<0.05) was calculated, and increase in post-training knowledge level was determined. Mean score before and after training was 20.07±46.76 and 96.36±11.85, respectively.
FIGURE 1.
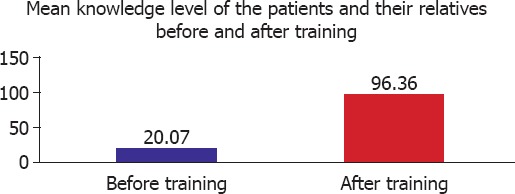
Mean knowledge level of the patients and their relatives before and after training.
Details of knowledge level of the patients and their relatives with respect to infection control measures before and after training are presented in Table 1. Increase in knowledge of infection control measures after training was demonstrated.
TABLE 1.
Participants ’ knowledge of infection control measures
| Before training | After training | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes | No | No opinion | Yes | No | No opinion | ||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | ||
| Do you know anything about hospital-acquired infection? | 88 | 44.7 | 84 | 42.6 | 25 | 12.7 | 188 | 95.4 | 4 | 2.0 | 4 | 2.5 | |
| Does hospital-acquired infection prolong hospital stay? | 147 | 74.6 | 39 | 19.8 | 11 | 5.6 | 193 | 98 | 2 | 1.0 | 2 | 1.0 | |
| Can hospital-acquired infection be prevented? | 144 | 73.46 | 40 | 20.3 | 12 | 6.1 | 197 | 100 | – | – | – | – | |
| During your hospital stay,should hands be washed with soap and water? | 192 | 97.5 | 3 | 1.5 | 2 | 1.0 | 197 | 100 | – | – | – | – | |
| During your hospital stay,should hand antiseptics be used? | 160 | 81.2 | 29 | 14.7 | 8 | 4.1 | 195 | 99 | 1 | 0.5 | 1 | 0.5 | |
| Do you know which waste material should be discarded in garbage bins containing red plastic bags? | 104 | 52.8 | 81 | 41.1 | 12 | 6.1 | 192 | 97.5 | 4 | 2.0 | 1 | 0.5 | |
| Do you know which waste materials should be discarded in garbage bins containing black plastic bags? | 112 | 56.9 | 74 | 37.6 | 11 | 5.6 | 193 | 98 | 2 | 1.0 | 2 | 1.0 | |
| Do you know which waste materials should be discarded in garbage bins containing blue plastic bags? | 75 | 38.1 | 108 | 54.8 | 14 | 7.1 | 189 | 95.9 | 4 | 2.0 | 4 | 2.0 | |
| Do you know which waste materials should be discarded in garbage bins containing yellow plastic bags? | 43 | 21.9 | 137 | 69.5 | 16 | 8.1 | 184 | 93.4 | 6 | 3.0 | 7 | 3.6 | |
| Do you know the precautions that should be taken by your hospital companion concerning infection control? | 76 | 38.6 | 106 | 53.8 | 15 | 7.6 | 190 | 96.4 | 6 | 3.0 | 1 | 0.5 | |
| Do you know the infection control measures that visitors should observe? | 80 | 40.6 | 100 | 50.8 | 17 | 8.6 | 190 | 96.4 | 6 | 3.0 | 1 | 0.5 | |
Most (95.8%) of the nurses and midwives working in obstetrics and gynecology clinics indicated that training was provided to patients, and 87.5% of the staff group stated that training on infection control measures facilitated treatment and healthcare procedures.
Nurses also evaluated behavioral changes in patients observed after training on infection control measures, and 95.9% of them thought that the training provided contributed favorably to compliance with infection control measures.
According to staff working in the clinics of obstetrics and gynecology, increase in compliance with infection control measures was seen after training (Figure 2).
FIGURE 2.
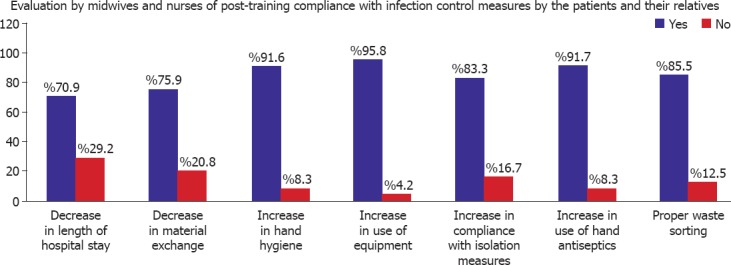
Compliance of the patients and their relatives with infection control measures.
Evaluation of postoperative healthcare-associated infection rate after training regarding infection control measures determined that there was decrease in infection rate. Incidence of surgical site infection when training was not uniformly provided was 1.05%, while rate between November 2015 and January 2016 when training using the “Information Guide for Patients and their Relatives on Infection Control Measures” was provided was 0.77% (Figure 3).
FIGURE 3.
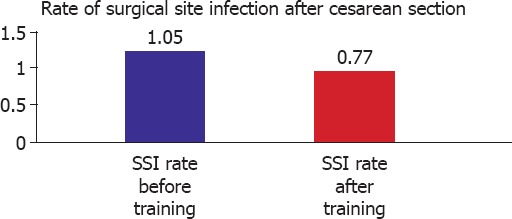
Incidence rate of surgical site infection (SSI) before and after training of patients and their relatives.
DISCUSSION
Training is one of the most important components of an infection control program [18]. Karakuş defined training as the process of acquiring knowledge, skills and attitudes required to develop behaviors that will make life easier [11]. According to this definition, informing patients and their relatives about healthcare-associated infection control measures will enable them to develop their knowledge and change their attitudes and behaviors to help prevent infection. Uyar indicated that encouraging and providing opportunities for training patients and their relatives increases rate of compliance with infection control measures [18]. Particularly effective in the prevention of infection are observance of guidelines related to hand hygiene and proper waste sorting, visitor recognition of hospital rules, and prevention of sharing personal items between patients and with visitors. Greater knowledge of these issues increases compliance of patients and relatives with infection control measures [11].
Ocran and Tagoe reported that training for healthcare professionals and patients concerning prevention of healthcare-associated infection to encourage behavioral changes and compliance with recommended measures was related to educational level, and that greater level of formal education led to more positive contributions to preventive practices [19]. Uner et al. indicated that mean score of patients’ knowledge level and favorable attitudes about handwashing increased with greater schooling level [20]. In our study, however, 60% of the patients and their relatives were primary school graduates and increase in knowledge level of the patients relative to baseline was not correlated with level of formal education.
Kurcer et al. demonstrated significant improvement in knowledge and attitudes of patients after training and counseling services were provided about how to live a healthy life [21]. Hanci et al. isolated various microorganisms that can cause hospital-acquired infection from the hands of visitors to patients. They stated that providing information to visitors about infection control measures was effective in prevention of nosocomial infections [16]. In the present study, mean knowledge level score of patients before and after training was 20.07±46.76 and 96.36±11.85 points, respectively (Figure 1).
Materials used to train the patients and their relatives included clear and easy to understand messages prepared to be suitable for individuals of every education level. It is thought that this aspect of the training was helpful to increase knowledge level of the participants. Avsar et al. indicated that training provided to patients should be easily comprehensible and age-appropriate [22]. Clear, simple language contributed favorably to the effectiveness of the training in the present study.
Healthcare professionals are to provide patients with training on various subjects from the time of admission to the hospital. Guidelines released by the Ministry of Health concerning quality standards in healthcare services include training for patients and relatives about drugs to be used, issues related to patient’s care, use of equipment and medical devices, hand hygiene, nutrition and healthy diet, exercise, and procedure for referral to appropriate specialist [12]. In 2002, Yetkin et al. reported that 33% of nurses provided training for patients, 52.3% of those surveyed trained their patients from time to time, and 14.7% of them indicated that they did not train their patients at all [17]. Present study results revealed that 95.8% of the nursing staff reported training patients about infection control measures. High rate of training currently provided in hospitals is considered to be result of implementation of ministry quality standards beginning in 2007.
Viewpoints of clinical nurses about development of behavioral changes in the patients concerning compliance with infection control measures and waste sorting after receiving training were evaluated, and it was determined that exchange of personal materials had decreased (75.9%), hand hygiene was more strictly observed (91.7%), use of hand antiseptic solutions increased (91.7%), and waste sorting also improved (85.5%) (Figure 2).
Though surgical site infections have many etiological factors, application of effective infection control training may increase awareness of the patients and healthcare professionals, and literature studies have indicated that these programs are effective at reducing infection rate. In our study, reduction in incidence of surgical site infection following training using the “Information Guide for Patients and their Relatives on Infection Control Measures” from 1.05% at baseline to 0.77% was found (Figure 3). An informative report published by The Joint Commission in 2010 indicated that patient training contributed to a decrease in postsurgical infection rate from 3.61% to 1.83% [23]. Outcome of present study is supported by this report.
Conclusion
Observations of nursing staff at conclusion of the study with respect to effectiveness of educational course on prevention of healthcare-associated infection and infection control measures provided to patients and their relatives in easily understandable language were as follows:
Hospitalization period of the patients decreased,
Compliance of the patients and their relatives to hand hygiene was strengthened,
Visitors and companions attending to patients observed infection control measures more frequently, and
The patients and their relatives sorted domestic, medical, hazardous, and recyclable/glass waste more accurately.
We conclude that providing regular training for inpatients and their relatives about infection control measures using written and visual educational material will decrease risk of hospital-acquired infection.
Footnotes
Conflict of Interest: None declared.
Financial Disclosure: The authors declared that this study has received no financial support.
Authorship contributions: Concept – F.O.E., Y.D.M.; Design – F.O.E., Y.D.M.; Data collection &/or processing – F.O.E., C.K.G.; Analysis and/or interpretation – F.O.E., Y.D.M., A.A.; Writing – F.O.E., A.A.; Critical review – Y.D.M.
REFERENCES
- 1.Orucu M, Geyik MF. Yoğun bakım ünitesinde sık görülen enfeksiyonlar. Düzce Tıp Fakültesi Dergisi. 2008;1:40–3. [Google Scholar]
- 2.Yüceer S, Demir SG. Yoğun bakım ünitesinde nozokomiyal enfeksiyonların önlenmesi ve hemşirelik uygulamaları. Dicle Tıp Dergisi. 2009;36:226–32. [Google Scholar]
- 3.Asl HM, Nateghian A. Epidemiology of Nosocomial Infections in a Pediatric Intensive Care Unit (PICU) Archives of Clinical Infectious Diseases. 2009;4:83–6. [Google Scholar]
- 4.National and state healthcare associated infections progress report, CDC. 2016. [access date:3 April 2017]. https://www.cdc.gov/hai/pdfs/progress-report/hai-progress-report.pdf .
- 5.Özçetin M, Saz EU, Karapınar B, Özen S, Aydemir Ş, Vardar F. Hastane enfeksiyonları;sıklığıve risk faktörleri. J Pediatr Inf. 2009;3:49–53. [Google Scholar]
- 6.Ağırbaş İ. Hastane enfeksiyonlari maliyet analizi, Ankara Üniversitesi Bilimsel Araştırma Projesi. 2013. [access date:11 April 2017]. http://acikarsiv.ankara.edu.tr/browse/24778/Enfeksiyon-maliyet-2013.pdf?show .
- 7.Karahocagil MK, Yaman G, Göktaş U, Sünnetçioğlu M, Çıkman A, Bilici A, et al. Van Tıp Dergisi. 2011;18:27–32. [Google Scholar]
- 8.Preventing Healthcare-Associated Infections. Council of State and Territorial Epidemiologists Sunday Workshop, June 7. 2009. [access date:11 April 2017]. https://www.cdc.gov/nhsn/ra/pdf/csteworkshopdhqp6709final.pdf .
- 9.Standard precautions in health care, WHO. 2007. [access date:3 April 2017]. http://www.who.int/csr/resources/publications/EPR_AM2_E7.pdf?ua=1 .
- 10.T.C. Sağlık BakanlığıYataklıTedavi KurumlarıEnfeksiyon Kontrol Yönetmeliği. [access date:3 April 2017];T.C. Resmi Gazete. 2005 25903 http://www.asm.gov.tr/UploadGenelDosyalar/Dosyalar/143/MEVZUAT/18_08_2010_12_59_33.pdf . [Google Scholar]
- 11.Karakuş Z. Enfeksiyon Kontrol Hemşirelerinin Çalışma Alanında YaşadığıGüçlükler ve Eğitimin Rolü. Marmara Üniversitesi Sağlık Bilimleri EnstitüsüHemşirelik Öğretimi Anabilim DalıYüksek Lisans Tezi. 2008 [Google Scholar]
- 12.T.C.Sağlık BakanlığıSağlık Hizmetleri Genel MüdürlüğüSağlıkta Kalite ve Akreditasyon Daire Başkanlığı. [access date:3 April 2017];Sağlıkta Kalite StandartlarıHastane. 2016 5 http://www.kalite.saglik.gov.tr/Eklenti/3460,skshastanesetiv5r1pdf.pdf?0 . [Google Scholar]
- 13.McGuckin M, Waterman R, Storr IJ, Bowler IC, Ashby M, Topley K, et al. Evaluation of a patient-empowering hand hygiene programme in the UK. J Hosp Infect. 2001;48:222–7. doi: 10.1053/jhin.2001.0983. [DOI] [PubMed] [Google Scholar]
- 14.Terzi Ö, Aker S, Sünter AT, Pekşen Y. Hastane temizlik elemanlarıve mesleki enfeksiyon riski:Bilgi ve davranışlar üzerine bir çalışma. İnönüÜniversitesi Tıp Fakültesi Dergisi. 2009;16:7–12. [Google Scholar]
- 15.Luby SP, Agboatwalla M, Feikin DR, Painter J, Billhimer W, Altaf A, et al. Effect of handwashing on child health:a randomised controlled trial. Lancet. 2005;366:225–33. doi: 10.1016/S0140-6736(05)66912-7. [DOI] [PubMed] [Google Scholar]
- 16.Hancı H, Ayyıldız A, Çelebi D. Hasta ziyaretleri için hastaneye gelen kişilerin ziyaret öncesi ve sonrasıel floralarının karşılaştırılması. Atatürk Üniversitesi Veteriner Bilimleri Dergisi. 2012;7:113–21. [Google Scholar]
- 17.Yetkin A. Hemşirelerin Hasta ve Ailesinin Eğitimi İle İlgili Görüşve Uygulamaları. Atatürk Üniversitesi Hemşirelik Yüksekokulu Dergisi. 2002;5:53–59. [Google Scholar]
- 18.Uyar Y. Hastane infeksiyonlarınıönlemede personel sağlık kontrol çalışmalarıve eğitim stratejileri. IV. Ulusal Sterilizasyon Dezenfeksiyon Kongresi (Kongre Kitabı) Ankara 20 - 24 Nisan. 2005:493–503. [Google Scholar]
- 19.Ocran I, Tagoe DNA. Knowledge and attitude of healthcare workers and patients on healthcare associated infections in a regional hospital in Ghana. Asian Pac J Trop Dis. 2014;4:135–39. doi: 10.1016/S2222-1808(14)60330-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Üner S, Sevencan F, Başaran E, Balcı C, Bilaloğlu B. Bir sağlık ocağına başvuran kişilerin sosyal el yıkama ile ilgili bazıbilgi ve tutumların saptanması. TAF Prev Med Bull. 2009;8:207–16. [Google Scholar]
- 21.Kurçer MA, Özbay A. Koroner arter hastalarında uygulanan yaşam tarzıeğitim ve danışmanlığının yaşam kalitesine etkisi. Anadolu Kardiyol Derg. 2011;11:107–13. doi: 10.5152/akd.2011.028. [DOI] [PubMed] [Google Scholar]
- 22.Avşar G, Kaşıkcı M. Ülkemizde Hasta Eğitiminin Durumu. Atatürk Üniversitesi Hemşirelik Yüksekokulu Dergisi. 2009;12:67–73. [Google Scholar]
- 23.Educating Patients About Surgical Site Infections:Complying with NPSG.07.05.01. The Joint Commission Perspectives on Patient Safety, December 2010. [acces date:3 April 2017]. http://www.jcrinc.com/educating-patients-about-surgical-site-infections-complying-with-npsg-07-05-01/


