Abstract
Importance
Healthcare professionals commonly recommend increased water consumption, typically to 8 cups/d, as part of a weight-reducing diet. However, this recommendation is based on limited evidence and virtually no experimental data in the pediatric age range.
Objective
The aim of this study was to compare two standard weight-loss diets, either with (Water) or without (Control) additional advice and behavioral support to increase habitual water intake to 8 cups/d.
Design
6-month randomized controlled parallel-group design.
Setting
The trial was conducted at Boston Children’s Hospital, Boston, Massachusetts, between February 2011 and June 2014.
Participants
38 overweight and obese adolescents who reported drinking ≤4 cups of water/d.
Intervention
Both groups received similar weight-reducing interventions, differentiated by water messages but controlled for other dietary recommendations and treatment intensity. The interventions included dietary counseling, daily text messages, and a cookbook with health guides. To support adherence to 8 cups water/d, the Water group received well-defined water messages through counseling and daily text messages, a water bottle, and a water pitcher with filters. The Control group received no specific advice on water consumption.
Main Outcome and Measures
Primary outcome was 6-month change in body mass index (BMI) z-score.
Results
All randomized participants completed the study. Both groups reported drinking ~2 cups/d water at baseline. Self-reported change in water intake was greater in the Water Group compared to the Control Group (difference between groups, 1.6; 95% CI, 0.2 to 3.0 cups/d; P=0.03). The 6-month change in BMI z-score did not differ between groups (−0.0; 95% CI, −0.1 to 0.1; P=0.88).
Conclusions and Relevance
Contrary to hypothesis, advice and behavioral supports to consume 8 cups water/d in the context of a weight-reducing diet did not affect body weight among overweight and obese adolescents. Despite intensive behavior supports, few achieved the 8 cups/d water target. Environmental interventions to reduce barriers to water consumption at school may be necessary in future research of feasibility and effectiveness to achieve the target of an 8-cup/d intake of water in adolescents.
Clinical Trial Registration
ClinicalTrials.gov, NCT01044134, https://clinicaltrials.gov/ct2/show/NCT01044134
Keywords: water, weight loss, obesity, adolescents, clinical trial
INTRODUCTION
Adequate water intake is essential for health, but any benefit for weight management remains unclear. Nevertheless, healthcare professionals commonly recommend increasing water intake, typically to 8 cups/d, as part of a weight-reducing diet. Despite its widespread adoption, the evidence base is limited, with virtually no experimental data in the pediatric population 1.
The origin of the 8 cups of water/d recommendation is unclear 2. Adequate intake of total water for adolescents is 2.4–3.3L for boys and 2.1–2.3L for girls 3. The adequate intake was set at the median total water intake based on national survey data. However, dehydration is estimated in more than half of US children and adolescents 4 and almost one quarter report no intake of any plain water 5. The practicality of increasing habitual water intake to 8 cups/d is unknown.
No trials to date have tested increasing water to 8 cups/d. Increased water intake was inversely associated with weight gain in a pooled analysis of prospective cohort studies 6 and associated with greater weight reduction in a post-hoc analysis of data from an interventional study 7. Cross-sectional studies show a positive association in children and adolescents 5, but not in adults 8. However, these studies are subject to residual confounding and reverse causation. In adults, trials of water preloads showed mixed results compared to no water preloads for weight loss 9,10. In children, trials that tested differences in advice to drink water 11 and a school-based intervention 12 did not result in significant weight loss compared to the control group.
Various mechanisms may plausibly relate increased water intake to weight loss. These include increased gastric distension 13,14, fullness 9,15,16, or energy expenditure via water-induced thermogenesis 17,18; decreased hunger 9,16, energy intake 15, or solid food consumption from decreased thirst cues mistaken for hunger cues 19; reduced activation of adipose tissue RAS components associated with dehydration 20; displacement of calorie-containing beverages 6,21,22; and improvements in diet quality 5,7,23.
The aim of this study was to compare the effects of recommending consumption of 8 cups water/d on weight loss in adolescents with overweight or obesity during a 6-month weight-reducing diet.
SUBJECTS AND METHODS
Design
We conducted a 6-month randomized, controlled parallel-group study comparing two weight loss interventions, comprising standard dietary recommendations either with (Water) or without (Control) additional advice and behavioral support to increase habitual water intake to 8 cups/d. We hypothesized that increasing water intake to 8 cups/d would decrease 6-month change in BMI z-score (primary outcome) and other anthropometric outcomes. Participants were recruited from newspaper advertisements, internet listings, and pediatric primary care practices, with the study presented as an opportunity for weight loss. A multi-step screening and enrollment process was used to confirm eligibility.
The institutional review board at Boston Children’s Hospital approved the protocol. Participants provided written informed assent and a parent provided written informed consent. Participants who completed the study received $120 as compensation for their time and effort. The study was conducted between February 2011 and June 2014.
Participants
Adolescents aged 12 to 17 years with a BMI ≥85th percentile 24 were eligible for the study. Other inclusion criteria included access to a working cell phone, at least one parent willing and able to participate in the intervention with the participant, and medical clearance from a treating physician. Exclusion criteria were water intake of >4 cups/d (i.e., individuals for whom the intervention would likely produce relatively little change in habitual intake), BMI ≥40 kg/m2, smokers, diagnosis of a major medical illness, and chronic use of medications that may affect study outcomes. To prevent contamination of random group assignments, members of the same family or household, or friends, classmates or co-workers who interacted with each other ≥1 time per week were not enrolled.
Master randomization assignments using a blocked randomization design stratified by sex and ethnicity/race (non-Hispanic white, other) with sequential randomization numbers, were prepared in advance by the study statistician. Individual group assignments were specified in a sequence of sealed envelopes, labeled with the same randomization numbers. The appropriate envelope was opened for each enrolled participant the day of the first in-person session with the dietitian.
Intervention
The two groups received similar weight-reducing interventions, comprising diets that were differentiated only with regard to specificity of recommendations for water consumption. The standardized weight-reducing intervention consisted of monthly individual nutrition education and behavioral counseling by a registered dietitian (alternating between in-person sessions and telephone counseling calls, 6 total contacts), and daily text messages. The standardized intervention was intentionally designed to be less intensive where any large reductions in body weight could potentially mask the effects of increasing water intake to 8 cups/d. Well-defined key messages consistent with national dietary guidelines (USDA MyPyramid 25 and MyPlate 26 food guidance systems) included recommendations to eat ample vegetables, fruits, and legumes; whole rather than refined grains; and high-quality proteins at most meals and snacks. Additional messages focused on limiting intake of added fats and sugars, juices, and sugar-sweetened beverages. Participants were provided a cookbook with health guides and recipes written specifically for adolescents and a Corelle® plate with appropriate divisions to convey reasonable portion sizes and facilitate meal assembly. Telephone calls were conducted using a patient-centered counseling model 27,28 to encourage adherence. Daily text messages were sent using client-based messaging software (HipLink™, Semotus Solutions, Inc.) to reinforce key messages, foster adherence, and provide ongoing support with motivating and encouraging phrases. Text messages were sent on the hour between 4–7pm on weekdays and 9am–7pm on weekends to avoid school and sleeping hours. Physical activity advice consistent with current guidelines was the same in both groups 29,30.
Participants were masked to the specific aims of the study in order to maximize adherence to their group assignment. The Water group was counseled to increase water intake to 8 cups/d, “8×8” (eight 8-oz glasses of water/d). Water was defined as tap and plain bottled water. To support adherence, the Water group received well-defined water messages through counseling and daily text messages, a stainless steel water bottle, and a water pitcher with replacement filters. The Control group received no specific advice on water intake or altering beverage intake other than those as part of the standard weight-reducing diet described above. When asked, the dietitian advised that drinking plain water was the best way to satisfy thirst and instructed them to drink when thirsty.
Treatment Fidelity
Several strategies were implemented to maximize treatment fidelity. Scripts and education materials for presenting topics during the in-person sessions included well-defined messages for each diet. Guides for telephone counseling calls were designed to foster dietitian adherence to a patient-centered counseling model, with adequate flexibility for responding to the unique needs of each participant. Telephone calls were digitally recorded and a random selection (33%) was reviewed for quality control.
Process Evaluation
Participant adherence was evaluated based on attendance at in-person sessions that included spot urines to measure hydration status, completion of telephone counseling calls, and self-reported dietary and water intake. We also evaluated participant satisfaction with the intervention.
Diet and physical activity were assessed by 3 unannounced 24-hour recall interviews (2 weekdays, 1 weekend day) at baseline and again at 6-months. The interviewer was masked to group assignment. Dietary data were collected using the Nutrition Data System for Research (NDSR) software versions 2010–2013, developed by the Nutrition Coordinating Center, University of Minnesota, Minneapolis. Final calculations were completed using NDSR version 2013. Physical activity data were collected using established methods 31,32 and are presented as metabolic equivalents (METs) 33. At each in-person session, participants provided a spot urine sample that was immediately analyzed for specific gravity (MultiStix 10 SG reagent strips; Siemens Healthcare Diagnostics Inc.). At the end of the study, participants responded to satisfaction questions related to the standard weight loss diet using 10-cm visual analog scales with appropriate verbal anchors. The Water group completed additional questions related to the “8×8” recommendation.
Outcomes
Outcomes were assessed after a 12-hour overnight fast at baseline and 6-months. Outcome assessors were masked to random group assignment. Data were managed using Research Electronic Data Capture 34.
BMI z-score and percentile were calculated using reference data for sex and age 24. Body weight and height were measured using a calibrated electronic scale and wall-mounted stadiometer, respectively. BMI was calculated as weight (kg) divided by height (m) squared. Waist and hip circumferences were measured according to established methods 35,36.
Statistical Analysis
In this study, the planned sample size of 30 per group, based on a previous trial 37, provided 80% power to detect a difference between arms for 6-month change in weight (3.7kg) and BMI z-score (0.122). We randomized 38 participants (=2/3 of target) and stopped enrollment after 2.8y due to slow recruitment.
Data are presented as mean (95% CI) unless otherwise noted. All analyses followed the intention-to-treat principle. Baseline characteristics were compared between groups using the Fisher exact test for categorical variables and t-test for continuous variables. The primary outcome was 6-month change in BMI z-score. To adjust for variations in BMI based on sex and age of adolescents, BMI was transformed to BMI z-score (i.e. adjusting for sex and age based on reference data). The 6-month changes from baseline in outcomes were compared between groups using a general linear model. The findings of the primary outcome did not materially change with the inclusion of baseline covariates (water intake, BMI z-score, sex, age, height, income, race, energy intake, % calories from fat). Secondary outcomes were also analyzed with the inclusion of variance reducing baseline covariates (BMI z-score, water intake) and the findings did not materially change with the inclusion. We further tested covariates for potential effect modification (interaction). The null hypothesis was that the 6-month change from baseline would not differ between diet groups. Relationships of BMI z-score with water intake and urine specific gravity for changes over 6 months were calculated using Pearson correlations. SAS software (SAS Institute Inc., Cary, NC) was used for all computations.
RESULTS
Recruitment and Retention
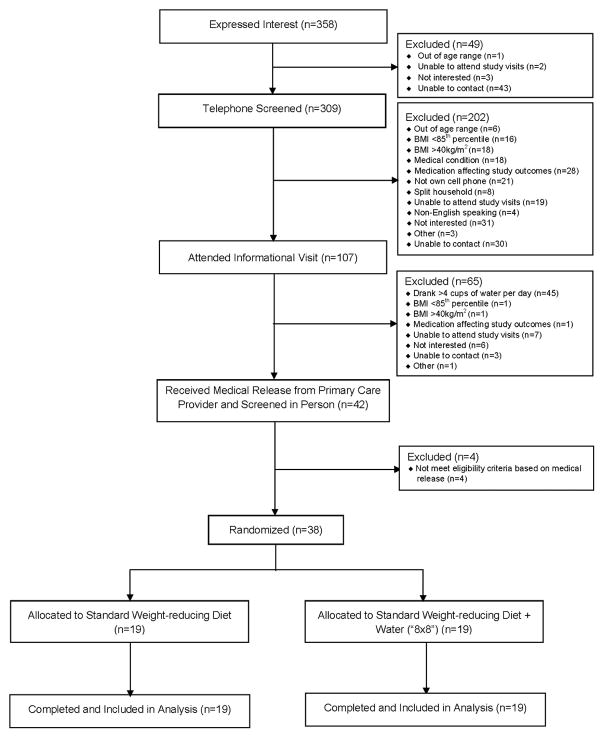
Over 100 adolescents attended an informational visit after initial telephone screening for eligibility. Of these, 42% reported drinking >4 cups of water/d and were excluded (Figure 1). A total of 38 participants were randomized to a diet group. Baseline characteristics are presented in Table 1. There were no differences at baseline between groups except for annual household income and age. Study completion rate was 100% and all randomized participants were included in the primary analysis.
Figure 1.
Flow of Participants Through the Trial
Table 1.
Baseline Characteristicsa
| Variable | Unadjusted Data
|
||
|---|---|---|---|
| Control (n=19) | Water (n=19) | P value | |
| Sex (Males/Females) | 6/13 | 5/14 | 1.00 |
|
| |||
| Race or Ethnic Group | |||
| Race | 1.00 | ||
| White | 9 | 8 | |
| Black | 5 | 6 | |
| Asian | 2 | 1 | |
| Native American/Alaskan Native | 0 | 1 | |
| Multiple or Other | 3 | 3 | |
| Ethnic Group | 1.00 | ||
| Hispanic | 1 | 2 | |
| Non Hispanic | 18 | 17 | |
|
| |||
| Annual Household Income | 0.04 | ||
| < $30,000 | 4 | 1 | |
| $30,000 – $59,999 | 2 | 6 | |
| $60,000 – $89,999 | 4 | 8 | |
| ≥ $90,000 | 7 | 4 | |
| Unknown or Refused | 2 | 0 | |
|
| |||
| Age(yr), Mean±SD | 15.7±1.4 | 14.1 ±1.7 | 0.004 |
Differences in baseline characteristics by diet group were assessed using the Fisher exact test for categorical variables and t-test for continuous variables. P-value tests the hypothesis of zero difference between diet groups.
Process Measures
Completion of in-person sessions and telephone calls and receipt of daily text messages did not differ between groups. Participants attended 95% of in-person visits and received 89% of telephone counseling calls and 95% of text messages.
Compared to baseline, urine specific gravity decreased significantly at 6-months in the Water group [−0.007 (−0.012 to −0.002); P=0.012], with no change in the Control group [−0.001 (−0.007 to 0.004); P=0.59] (Table 2). However, at 6-months, no significant difference was observed with changes in urine specific gravity between diet groups [−0.006 (−0.013 to 0.002); P=0.13].
Table 2.
Process Dataa
| Variable | Study Group | Unadjusted Data Mean (95% CI) | Change from Baseline Mean (95% CI) | ||
|---|---|---|---|---|---|
|
|
|
||||
| Baselineb | 6 months | 6 months | P value | ||
|
|
|
||||
| Energy (kcal) | Control | 1646 (1374 to 1918) | 1315 (1149 to 1482) | −330 (−555 to−106) | 0.005 |
|
| |||||
| Water | 1617 (1364 to 1871) | 1274 (1109 to 1439) | −344 (−568 to−119) | 0.004 | |
|
| |||||
| Water - Control | −13 (−331 to 305) | 0.93 | |||
|
|
|
||||
| Carbohydrate (% energy) | Control | 51.9(49.1 to 54.6) | 48.1 (44.7 to 51.4) | −3.8 (−7.5 to−0.1) | 0.044 |
|
| |||||
| Water | 51.7 (50.1 to 53.3) | 46.1 (43.5 to 48.7) | −5.6 (−9.3 to−1.9) | 0.004 | |
|
| |||||
| Water - Control | −1.8 (−7.0 to 3.4) | 0.49 | |||
|
|
|
||||
| Protein (% energy) | Control | 17.0 (15.3 to 18.7) | 21.7 (19.0 to 24.4) | 4.7 (1.9 to 7.5) | 0.002 |
|
| |||||
| Water | 16.8 (15.0 to 18.7) | 23.1 (20.9 to 25.4) | 6.3 (3.5 to 9.1) | <0.0001 | |
|
| |||||
| Water - Control | 1.6 (−2.4 to 5.6) | 0.42 | |||
|
|
|
||||
| Fat (% energy) | Control | 31.1 (28.8 to 33.4) | 30.2 (27.1 to 33.4) | −0.9 (−4.0 to 2.2) | 0.58 |
|
| |||||
| Water | 31.5 (29.3 to 33.6) | 30.7 (29.0 to 32.4) | −0.7 (−3.8 to 2.4) | 0.64 | |
|
| |||||
| Water - Control | 0.1 (−4.2 to 4.5) | 0.95 | |||
|
|
|
||||
| SFA (% energy) | Control | 11.5 (10.1 to 12.8) | 10.4 (9.1 to 11.6) | −1.1 (−2.7 to 0.5) | 0.17 |
|
| |||||
| Water | 11.3 (10.0 to 12.6) | 10.5 (9.2 to 11.8) | −0.8 (−2.4 to 0.8) | 0.30 | |
|
| |||||
| Water - Control | 0.3 (−2.0 to 2.5) | 0.81 | |||
|
|
|
||||
| MUFA (% energy) | Control | 10.1 (9.2 to 11.1) | 10.0 (8.7 to 11.2) | −0.2 (−1.4 to 1.1) | 0.78 |
|
| |||||
| Water | 10.5 (9.7 to 11.2) | 10.3 (9.7 to 10.9) | −0.1 (−1.4 to 1.1) | 0.81 | |
|
| |||||
| Water - Control | 0.0 (−1.8 to 1.8) | 0.98 | |||
|
|
|
||||
| PUFA (% energy) | Control | 6.7 (5.5 to 8.0) | 7.0 (5.6 to 8.4) | 0.3 (−1.3 to 1.8) | 0.74 |
|
| |||||
| Water | 6.9 (5.6 to 8.1) | 6.9 (5.8 to 8.0) | 0.1 (−1.5 to 1.7) | 0.94 | |
|
| |||||
| Water - Control | −0.2 (−2.4 to 2.1) | 0.86 | |||
|
|
|
||||
| Fiber (g/1000 kcal) | Control | 7.8 (6.4 to 9.2) | 9.5 (8.0 to 11.0) | 1.7 (0.2 to 3.3) | 0.030 |
|
| |||||
| Water | 7.9 (6.6 to 9.2) | 9.9 (8.7 to 11.1) | 1.9 (0.4 to 3.5) | 0.016 | |
|
| |||||
| Water - Control | 0.2 (−2.0 to 2.4) | 0.84 | |||
|
|
|
||||
| Dietary Cholesterol (mg/d) | Control | 245.9 (178.8 to 313.0) | 205.0 (129.6 to 280.5) | −40.9 (−95.1 to 13.3) | 0.13 |
|
| |||||
| Water | 218.2 (171.0 to 265.3) | 187.5 (152.6 to 222.4) | −30.7 (−84.8 to 23.5) | 0.26 | |
|
| |||||
| Water - Control | 10.2 (−66.4 to 86.8) | 0.79 | |||
|
|
|
||||
| Water Intake (8 Fluid ounce servings) | Control | 2.3 (1.5 to 3.1) | 3.5 (2.6 to 4.4) | 1.2 (0.2 to 2.2) | 0.02 |
|
| |||||
| Water | 2.0 (1.4 to 2.7) | 4.8 (3.8 to 5.9) | 2.8 (1.8 to 3.8) | <0.0001 | |
|
| |||||
| Water - Control | 1.6 (0.2 to 3.0) | 0.03 | |||
|
|
|
||||
| Urine Specific Gravityc | Control | 1.019 (1.015 to 1.023) | 1.018 (1.013 to 1.022) | −0.001 (−0.007 to 0.004) | 0.59 |
|
| |||||
| Water | 1.019 (1.015 to 1.023) | 1.012 (1.007 to 1.016) | −0.007 (−0.012 to−0.002) | 0.012 | |
|
| |||||
| Water - Control | −0.006 (−0.013 to 0.002) | 0.13 | |||
|
|
|
||||
| Physical Activity (METs) | Control | 1.5 (1.4 to 1.6) | 1.5 (1.4 to 1.5) | 0.0 (−0.1 to 0.1) | 0.86 |
|
| |||||
| Water | 1.5 (1.4 to 1.6) | 1.6 (1.5 to 1.7) | 0.0 (−0.1 to 0.2) | 0.49 | |
|
| |||||
| Water - Control | 0.0 (−0.2 to 0.2) | 0.72 | |||
N=38 (19 Water, 19 Control)
35 (17 Water, 18 Control)
Levels [mean (95% CI)] by study group at baseline and 6 months. Change [mean (95% CI)] from baseline assessed using the general linear model. P-value for each diet group tests the hypothesis of zero mean change from baseline within diet groups. P-value for “Water – Control” tests the hypothesis of zero difference between diet groups.
There were no differences between diet groups at baseline assessed using t-test (P≥0.05).
Baseline water intake was ~2 cups/d in both groups. Reported change in water intake was greater in the Water group compared to the Control group [1.6 (0.2 to 3.0) cups/d; P=0.03]. At 6-months, the Water group reported 4.8 (3.8 to 5.9) cups of water/d and the Control group 3.5 (2.6 to 4.4) cups/d. In the Water group, 1/19 subjects (~5%) reported drinking >8 cups water/d and 2/19 (~11%) ≥ 7.5 cups/d. One subject reported drinking ≥7.5cups/d in the Control group. No differences were reported between diet groups in energy and dietary intake whereas both groups reported similar changes while following the standard weight-reducing diet (Table 2). No difference between groups was reported in physical activity.
Both groups were equally satisfied with the intervention where overall satisfaction was ~8 on a 10-point scale (eTable 1). Specific to the Water group, participants reported a mean of ~7 for the ease of following the “8×8” recommendation and usefulness of the water bottle, water pitcher, and daily water-specific text messages.
Outcomes
Outcomes are presented in Table 3. Changes in BMI z-score did not differ significantly between diet groups [−0.0 (−0.1 to 0.1); P=0.88], although both groups decreased from baseline by 0.1. Changes in other anthropometric measures also did not differ between groups. There were no significant interactions detected.
Table 3.
Study Outcomesa
| Variable | Study Group | Unadjusted Data Mean (95% CI) | Change from Baseline Mean (95% CI) | ||
|---|---|---|---|---|---|
|
|
|
||||
| Baselineb | 6 months | 6 months | P value | ||
|
|
|
||||
| BMI z-score | Control | 2.0 (1.8 to 2.2) | 1.9 (1.7 to 2.1) | −0.1 (−0.2 to −0.0) | 0.008 |
|
| |||||
| Water | 2.1 (1.9 to 2.3) | 2.0 (1.8 to 2.2) | −0.1 (−0.2 to−0.0) | 0.005 | |
|
| |||||
| Water - Control | −0.0 (−0.1 to 0.1) | 0.88 | |||
|
|
|
||||
| BM (kg/m2) | Control | 31.9 (30.1 to 33.7) | 31.5 (29.5 to 33.5) | −0.4 (−1.1 to 0.3) | 0.24 |
|
| |||||
| Water | 32.0 (29.7 to 34.3) | 31.4 (29.2 to 33.5) | −0.6 (−1.3 to 0.1) | 0.091 | |
|
| |||||
| Water - Control | −0.2 (−1.2 to 0.8) | 0.71 | |||
|
|
|
||||
| Body Weight (kg) | Control | 88.3 (80.4 to 96.1) | 87.6 (79.3 to 96.0) | −0.6 (−2.7 to 1.5) | 0.56 |
|
| |||||
| Water | 85.4 (77.4 to 93.4) | 85.0 (77.7 to 92.2) | −0.4 (−2.6 to 1.7) | 0.68 | |
|
| |||||
| Water - Control | 0.2 (−2.8 to 3.2) | 0.90 | |||
|
|
|
||||
| Height (cm) | Control | 165.8 (161.8 to 169.8) | 166.2 (162.0 to 170.5) | 0.4 (−0.2 to 1.1) | 0.14 |
|
| |||||
| Water | 163.1 (159.1 to 167.1) | 164.4 (160.6 to 168.2) | 1.3 (0.7 to 1.9) | 0.0001 | |
|
| |||||
| Water - Control | 0.9 (−0.0 to 1.7) | 0.05 | |||
|
|
|
||||
| BM Percentile | Control | 96.8 (95.4 to 98.2) | 95.5 (93.1 to 98.0) | −1.3 (−2.2 to −0.3) | 0.01 |
|
| |||||
| Water | 97.5 (96.3 to 98.7) | 96.6 (94.9 to 98.4) | −0.8 (−1.8 to 0.2) | 0.10 | |
|
| |||||
| Water - Control | 0.4 (−0.9 to 1.8^ | 0.51 | |||
|
|
|
||||
| Waist Circumference (cm) | Control | 106.0 (100.3 to 111.7) | 104.4 (98.8 to 110.0) | −1.6 (−3.8 to 0.6) | 0.15 |
|
| |||||
| Water | 102.2 (96.8 to 107.5) | 101.6 (96.7 to 106.6) | −0.6 (−2.7 to 1.6) | 0.61 | |
|
| |||||
| Water - Control | 1.0 (−2.1 to 4.1) | 0.51 | |||
|
|
|
||||
| Hip Circumference (cm) | Control | 113.7 (109.5 to 117.8) | 114.0 (109.2 to 118.8) | 0.3 (−1.6 to 2.2) | 0.73 |
|
| |||||
| Water | 111.4 (107.4 to 115.5) | 111.4 (107.4 to 115.5) | −0.0 (−1.9 to 1.9) | 1.00 | |
|
| |||||
| Water - Control | −0.3 (−3.0 to 2.4) | 0.81 | |||
Abbreviation: BMI, body mass index N=38 (19 Control, 19 Water).
Levels [mean (95% CI)] by study group at baseline and 6 months. Change [mean (95% CI)] from baseline assessed using the general linear model. P-value for each diet group tests the hypothesis of zero mean change from baseline within diet groups. P-value for “Water - Control” tests the hypothesis of zero difference between diet groups.
There were no differences between diet groups at baseline assessed using t-test (P≥0.05).
No significant correlation existed between change in BMI z-score and changes in water intake or urine specific gravity.
Challenges and Barriers to “8×8” Recommendation
Subjects in the Water group reported being comfortable drinking water in front of their immediate family, relatives, and friends. At school, although water was accessible, water fountains were reported to be inconveniently located (26%) and to provide unsafe drinking water (21%). Furthermore, 16% reported not being allowed to bring water to school and 32% were not allowed to drink water in class. Outside of school or home, lack of convenient places to drink water from a fountain (47%) or refill a water bottle (37%) was also reported. Results are presented in eTable 2 and 3.
DISCUSSION
The present study evaluated two standardized 6-month interventions, comprising standard dietary recommendations for weight loss, either with or without additional advice and behavioral support to increase habitual water intake to 8 cups/d in adolescents with overweight or obesity. Contrary to the study hypothesis, advice and behavioral support to consume 8 cups water/d in the context of a weight-reducing diet did not affect BMI z-score among overweight and obese adolescents.
All randomized participants completed the study, although recruitment was less than expected. Based on the observed difference between groups and standard error, >6500 participants/group would be required to demonstrate a significant finding in BMI z-score with 80% power. Thus, had we achieved our recruitment goal, we likely would not have detected a significant group effect.
A novel aspect of the study was the “8×8” recommendation, which has not been tested in previous trials. On average, water intake increased by 3 cups/d to a mean of 5 cups/d in the Water group. Although less than 8 cups/d, water intake increased 2.5 times from baseline and the two groups appeared well-differentiated with regards to water intake. Reported changes in water intake were consistent with changes in urine specific gravity. However, lack of adherence, based on self-report, to advice to increase habitual water intake to 8 cups/d was the main study limitation. In addition to well-defined messages provided during the in-person sessions and telephone counseling calls, the study utilized several behavioral supports to foster adherence to advice to drink 8 cups water/d. Usefulness rating for the water bottle, water pitcher, and text messages were between 6 and 7 on a 10-point scale. Despite intensive efforts, the ease of the “8×8” recommendation was rated at 6.6 on a 10-point scale, suggesting that increasing habitual water intake to 8 cups/d may be simple in concept, but difficult or impractical in reality, raising the issue of feasibility. Environmental barriers and challenges outside the home may have been key factors compromising adherence. Given these barriers, the observed increase in water intake may be at best what can be expected among adolescents.
Almost one-third of the Water group reported not being able to drink water in class at school, presenting a significant barrier to adherence. Furthermore, ~40% reported lack of convenient places to drink water from a fountain or refill a water bottle outside of school or home. These barriers may have limited the ability of our participants to achieve the “8×8” recommendation. Access to drinking water often is compromised in schools due to older plumbing infrastructure and related cost implications and/or municipal water safety issues 38,39. These challenges may also be contributors to the high rate of dehydration among adolescents 4. Future studies testing advice to drink 8 cups/d water for weight loss will need to consider study designs that overcome the environmental barriers associated with the provision and/or accessibility of potable water, such as placement of ‘water jets’ in school cafeterias to increase access to drinking water 40.
Strengths of the present study include the randomized design, inclusion of a pediatric population, 100% completion rate, and masking of participants to the specific aims of the study. Additional strengths include the control for treatment intensity, a well differentiated water message with the same background standard weight-reducing intervention, and use of various behavioral supports to maximize differentiation and adherence. In addition to the suboptimal adherence to the “8×8” recommendation as discussed above, other study limitations include small sample size and reliance on self-report for dietary assessment, recognizing the well-documented potential for recall and social desirability biases.
In conclusion, the present study found that advice and behavioral supports to consume 8 cups water/d in the context of a weight-reducing diet had no added benefits on body weight reduction among adolescents with overweight or obesity. Despite intensive behavioral supports, few achieved the 8 cups/d water target, likely due to environmental barriers. Future research to test feasibility and effectiveness may need to focus on environmental interventions – such as water provision at school – to achieve the target of 8 cups/d.
Supplementary Material
KEY POINTS.
Question
Are there differences in weight loss between two standardized weight-loss diets, either with or without additional advice and behavioral support to increase habitual water intake to 8 cups/d?
Findings
In this randomized controlled trial of 38 adolescents with overweight or obesity, the 6-month change in BMI z-score did not differ significantly between groups. Increasing water intake to 8 cups/d may not be feasible without interventions focused on environmental barriers and challenges.
Meaning
Additional advice and behavioral supports to consume 8 cups water/d in the context of a weight-reducing diet did not affect body weight in adolescents.
Acknowledgments
We thank Jacqueline Ballou, MS, RD (Boston Children’s Hospital, Boston, Massachusetts) for assistance in delivering the dietary interventions; Jillian Aronovitz, BA and Meghan Leary, BA (Boston Children’s Hospital, Boston, Massachusetts) for clinic recruitment, organization of study visits, data collection, and data entry; Linda Seger-Shippee, DT (Boston Children’s Hospital, Boston, Massachusetts) for conducting the 24-hour dietary and physical activity recall interviews; Sarah Steltz, MPH (Boston Children’s Hospital, Boston, Massachusetts) for quality control protocols and development and maintenance of the REDCap database; Catherine Matero, BS, and Veronica Gragnano, MA (Boston Children’s Hospital, Boston, Massachusetts) for administrative support; and clinic providers at Boston Children’s Hospital, and The Pediatric Physicians’ Organization at Children’s (PPOC) for recruitment efforts. Mss. Ballou, Aronovitz, Leary, Seger-Shippee, Steltz, Matero, and Gragnano received compensation for their work in the form of salary support. The physicians from PPOC received compensation in the form of a nominal fee ($20) per valid HIPAA Authorization form returned to the study office, this was for the time involved in completing the necessary form. We also thank Bodimojo.com for providing us with the “teen-generated and approved” encouraging and supportive text messages. We would also like to express our sincere gratitude to the staff of the Center for Young Women’s Health and the Young Men’s Health Task Force at Boston Children’s Hospital for effort and support in developing and producing the Quick and Easy Recipes for Teens - A Cookbook and Guide to Healthy Eating. The Center for Young Women’s Health and the Young Men’s Health Task Force at Boston Children’s Hospital received compensation for developing and producing the Cookbook.
Sources of Support: This work was conducted with grants from the Airborne Cy Pres Fund and New Balance Foundation and with support from the Harvard Catalyst (Harvard Clinical and Translational Science Center, National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health Award UL1 TR001102).
Dr. Wong was a recipient of a Canadian Institutes of Health Research (CIHR) Fellowship Award in the area of Clinical Research and a CIHR Randomized Controlled Trials—Mentoring Program Training Grant. Dr. Ludwig was supported by a mid-career mentoring award from the National Institute of Diabetes and Digestive and Kidney Diseases (K24 DK082730).
Footnotes
The content is solely the responsibility of the authors and does not necessarily represent the official views of the funders.
Conflicts of Interest Disclosures
Dr. Ludwig received royalties for books on obesity and nutrition. Other authors declare no conflicts of interest relevant to this manuscript.
Authors’ Contributions
JMWW, CBE, HF, and DSL designed research; JMMW and LR conducted research; JMMW and HF analyzed data; JMMW, CBE, HF, and DSL wrote the paper; JMMW and DSL have primary responsibility for final content. All authors read and approved the final manuscript.
DSL and JMWW had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Role of Sponsor
The funding organizations played no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
References
- 1.Casazza K, Brown A, Astrup A, et al. Weighing the Evidence of Common Beliefs in Obesity Research. Crit Rev Food Sci Nutr. 2015;55(14):2014–2053. doi: 10.1080/10408398.2014.922044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Valtin H. “Drink at least eight glasses of water a day.” Really? Is there scientific evidence for “8 × 8”? Am J Physiol Regul Integr Comp Physiol. 2002 Nov;283(5):R993–1004. doi: 10.1152/ajpregu.00365.2002. [DOI] [PubMed] [Google Scholar]
- 3.Panel on Dietary Reference Intakes for Electrolytes and Water, Standing Committee on the Scientific Evaluation of Dietary Reference Intakes, Food and Nutrition Board, Institute of Medicine. Dietary Reference Intakes for Water, Potassium, Sodium, Chloride, and Sulfate. Washington, DC: National Academy Press; 2004. [Google Scholar]
- 4.Kenney EL, Long MW, Cradock AL, Gortmaker SL. Prevalence of Inadequate Hydration Among US Children and Disparities by Gender and Race/Ethnicity: National Health and Nutrition Examination Survey, 2009–2012. Am J Public Health. 2015 Aug;105(8):e113–118. doi: 10.2105/AJPH.2015.302572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kant AK, Graubard BI. Contributors of water intake in US children and adolescents: associations with dietary and meal characteristics--National Health and Nutrition Examination Survey 2005–2006. Am J Clin Nutr. 2010 Oct;92(4):887–896. doi: 10.3945/ajcn.2010.29708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pan A, Malik VS, Hao T, Willett WC, Mozaffarian D, Hu FB. Changes in water and beverage intake and long-term weight changes: results from three prospective cohort studies. Int J Obes (Lond) 2013 Oct;37(10):1378–1385. doi: 10.1038/ijo.2012.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stookey JD, Constant F, Popkin BM, Gardner CD. Drinking water is associated with weight loss in overweight dieting women independent of diet and activity. Obesity (Silver Spring) 2008 Nov;16(11):2481–2488. doi: 10.1038/oby.2008.409. [DOI] [PubMed] [Google Scholar]
- 8.Kant AK, Graubard BI, Atchison EA. Intakes of plain water, moisture in foods and beverages, and total water in the adult US population--nutritional, meal pattern, and body weight correlates: National Health and Nutrition Examination Surveys 1999–2006. Am J Clin Nutr. 2009 Sep;90(3):655–663. doi: 10.3945/ajcn.2009.27749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dennis EA, Dengo AL, Comber DL, et al. Water consumption increases weight loss during a hypocaloric diet intervention in middle-aged and older adults. Obesity (Silver Spring) 2010 Feb;18(2):300–307. doi: 10.1038/oby.2009.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Parretti HM, Aveyard P, Blannin A, et al. Efficacy of water preloading before main meals as a strategy for weight loss in primary care patients with obesity: RCT. Obesity (Silver Spring) 2015 Sep;23(9):1785–1791. doi: 10.1002/oby.21167. [DOI] [PubMed] [Google Scholar]
- 11.Stookey JD, Del Toro R, Hamer J, et al. Qualitative and/or quantitative drinking water recommendations for pediatric obesity treatment. J Obes Weight Loss Ther. 2014 Oct 11;4(4):232. doi: 10.4172/2165-7904.1000232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Muckelbauer R, Libuda L, Clausen K, Toschke AM, Reinehr T, Kersting M. Promotion and provision of drinking water in schools for overweight prevention: randomized, controlled cluster trial. Pediatrics. 2009 Apr;123(4):e661–667. doi: 10.1542/peds.2008-2186. [DOI] [PubMed] [Google Scholar]
- 13.Geliebter A. Gastric distension and gastric capacity in relation to food intake in humans. Physiol Behav. 1988;44(4–5):665–668. doi: 10.1016/0031-9384(88)90333-2. [DOI] [PubMed] [Google Scholar]
- 14.Geliebter A, Westreich S, Gage D. Gastric distention by balloon and test-meal intake in obese and lean subjects. Am J Clin Nutr. 1988 Sep;48(3):592–594. doi: 10.1093/ajcn/48.3.592. [DOI] [PubMed] [Google Scholar]
- 15.Van Walleghen EL, Orr JS, Gentile CL, Davy BM. Pre-meal water consumption reduces meal energy intake in older but not younger subjects. Obesity (Silver Spring) 2007 Jan;15(1):93–99. doi: 10.1038/oby.2007.506. [DOI] [PubMed] [Google Scholar]
- 16.Lappalainen R, Mennen L, van Weert L, Mykkanen H. Drinking water with a meal: a simple method of coping with feelings of hunger, satiety and desire to eat. Eur J Clin Nutr. 1993 Nov;47(11):815–819. [PubMed] [Google Scholar]
- 17.Dubnov-Raz G, Constantini NW, Yariv H, Nice S, Shapira N. Influence of water drinking on resting energy expenditure in overweight children. Int J Obes (Lond) 2011 Oct;35(10):1295–1300. doi: 10.1038/ijo.2011.130. [DOI] [PubMed] [Google Scholar]
- 18.Boschmann M, Steiniger J, Franke G, Birkenfeld AL, Luft FC, Jordan J. Water drinking induces thermogenesis through osmosensitive mechanisms. J Clin Endocrinol Metab. 2007 Aug;92(8):3334–3337. doi: 10.1210/jc.2006-1438. [DOI] [PubMed] [Google Scholar]
- 19.Atkins RC. Atkins for Life: The Complete Controlled Carb Program for Permanent Weight Loss and Good Health. St. Martin’s Griffin; 2004. [Google Scholar]
- 20.Kalupahana NS, Moustaid-Moussa N. The renin-angiotensin system: a link between obesity, inflammation and insulin resistance. Obes Rev. 2012 Feb;13(2):136–149. doi: 10.1111/j.1467-789X.2011.00942.x. [DOI] [PubMed] [Google Scholar]
- 21.Ludwig DS, Peterson KE, Gortmaker SL. Relation between consumption of sugar-sweetened drinks and childhood obesity: a prospective, observational analysis. Lancet. 2001 Feb 17;357(9255):505–508. doi: 10.1016/S0140-6736(00)04041-1. [DOI] [PubMed] [Google Scholar]
- 22.Ebbeling CB, Feldman HA, Chomitz VR, et al. A randomized trial of sugar-sweetened beverages and adolescent body weight. N Engl J Med. 2012 Oct 11;367(15):1407–1416. doi: 10.1056/NEJMoa1203388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Popkin BM, Barclay DV, Nielsen SJ. Water and food consumption patterns of U.S. adults from 1999 to 2001. Obes Res. 2005 Dec;13(12):2146–2152. doi: 10.1038/oby.2005.266. [DOI] [PubMed] [Google Scholar]
- 24.Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, et al. CDC growth charts: United States. Adv Data. 2000 Jun 8;(314):1–27. [PubMed] [Google Scholar]
- 25.Center for Nutrition Policy and Promotion U.S. Department of Agriculture. [Accessed August 19, 2009];MyPyramid Food Guidance System. http://www.cnpp.usda.gov/default.htm.
- 26.Center for Nutrition Policy and Promotion U.S. Department of Agriculture. MyPlate. [Accessed June 8, 2011]. [Google Scholar]
- 27.Rosal MC, Ebbeling CB, Lofgren I, Ockene JK, Ockene IS, Hebert JR. Facilitating dietary change: the patient-centered counseling model. J Am Diet Assoc. 2001 Mar;101(3):332–341. doi: 10.1016/S0002-8223(01)00086-4. [DOI] [PubMed] [Google Scholar]
- 28.Resnicow K, Davis R, Rollnick S. Motivational interviewing for pediatric obesity: Conceptual issues and evidence review. J Am Diet Assoc. 2006 Dec;106(12):2024–2033. doi: 10.1016/j.jada.2006.09.015. [DOI] [PubMed] [Google Scholar]
- 29.Daniels SR, Arnett DK, Eckel RH, et al. Overweight in children and adolescents: pathophysiology, consequences, prevention, and treatment. Circulation. 2005 Apr 19;111(15):1999–2012. doi: 10.1161/01.CIR.0000161369.71722.10. [DOI] [PubMed] [Google Scholar]
- 30.Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002 Feb 7;346(6):393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bouchard C, Tremblay A, Leblanc C, Lortie G, Savard R, Theriault G. A method to assess energy expenditure in children and adults. Am J Clin Nutr. 1983 Mar;37(3):461–467. doi: 10.1093/ajcn/37.3.461. [DOI] [PubMed] [Google Scholar]
- 32.Weston AT, Petosa R, Pate RR. Validation of an instrument for measurement of physical activity in youth. Med Sci Sports Exerc. 1997 Jan;29(1):138–143. doi: 10.1097/00005768-199701000-00020. [DOI] [PubMed] [Google Scholar]
- 33.Ainsworth BE, Haskell WL, Herrmann SD, et al. 2011 Compendium of Physical Activities: a second update of codes and MET values. Med Sci Sports Exerc. 2011 Aug;43(8):1575–1581. doi: 10.1249/MSS.0b013e31821ece12. [DOI] [PubMed] [Google Scholar]
- 34.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009 Apr;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lohman TG, Roche AF, Martorell R, editors. Anthropometric Standardization Reference Manual. Champaign, IL: Human Kinetics Books; 1988. [Google Scholar]
- 36.Centers for Disease Control and Prevention. NHANES Anthropometry Procedures Manual. 2009. [Google Scholar]
- 37.Ebbeling CB, Leidig MM, Feldman HA, Lovesky MM, Ludwig DS. Effects of a low-glycemic load vs low-fat diet in obese young adults: a randomized trial. JAMA. 2007 May 16;297(19):2092–2102. doi: 10.1001/jama.297.19.2092. [DOI] [PubMed] [Google Scholar]
- 38.Cradock AL, Wilking CL, Olliges SA, Gortmaker SL. Getting back on tap: the policy context and cost of ensuring access to low-cost drinking water in Massachusetts schools. Am J Prev Med. 2012 Sep;43(3 Suppl 2):S95–101. doi: 10.1016/j.amepre.2012.05.016. [DOI] [PubMed] [Google Scholar]
- 39.Ramirez SM, Stafford R. Equal and universal access?: water at mealtimes, inequalities, and the challenge for schools in poor and rural communities. J Health Care Poor Underserved. 2013 May;24(2):885–891. doi: 10.1353/hpu.2013.0078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schwartz AE, Leardo M, Aneja S, Elbel B. Effect of a School-Based Water Intervention on Child Body Mass Index and Obesity. JAMA Pediatr. 2016 Mar;170(3):220–226. doi: 10.1001/jamapediatrics.2015.3778. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.