Surgery is performed to save lives and improve the quality of life of patients. However, unsafe surgical care can lead to significant harm. The crude mortality rate after major surgery varies from 0.5% to 5%.[1] In the European Surgical Outcomes Study, an international, 7-day cohort study, 1855 out of the 46,539 adult patients undergoing non-cardiac surgery died, giving a relatively high crude mortality rate of 4%.[2] A recent international survey of 44,814 patients from 474 hospitals in 27 countries found the crude perioperative mortality rate of 0.46%.[3] Complications after inpatient operations occur in up to 25% of patients; and at least, half of the cases in which surgery led to harm are considered preventable.[1]
Anaesthesia may be either solely responsible or may contribute to perioperative mortality. It is believed that anaesthesia today is extremely safe and that mortality due to anaesthesia has declined considerably over the last few decades. However, this may not hold true in many parts of the world. Deaths due either to anaesthesia alone, or where anaesthesia was a contributory factor have reduced in countries with a high developmental index (HDI), whereas in countries with a low developmental index, mortality has remained more or less static from the 1970s till after the twenty- first century, and is significantly higher than that in HDI countries [Figure 1].[4] Mortality from general anaesthesia alone is reported to be as high as one in 150 in some parts of sub-Saharan Africa.[1]
Figure 1.
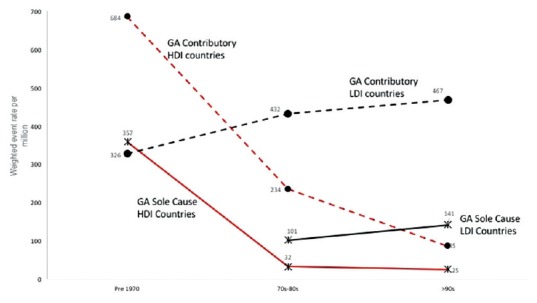
Weighted event rate (death rate) per million against period. Solid lines: Death rate where anaesthesia was the sole cause of mortality; Dashed lines: Death rate when general anaesthesia. Contributed to perioperative mortality; Black lines: Low development index countries; Red lines: High development index countries; GA: General anaesthesia; HDI: High development index; LDI: Low development index
The World Health organization (WHO) estimates that at least half of all surgical complications are avoidable and has made Safe Surgery Saves Lives the Second Global Patient Safety Challenge. The four areas in which dramatic improvements could be made in the safety of surgical care include surgical site infection prevention, safe anaesthesia, safe surgical teams and measurement of surgical services.[1] The surgical safety checklist (SSCL) is an integral part of the safe surgery campaign,[5] and has been shown to reduce perioperative complications and mortality by over 30%.[6] Pulse oximetry is an essential component of both safe anaesthesia and the SSCL. The only equipment in the SSCL is the pulse oximeter, and unfortunately, the only component that is not currently achievable in every operating room in the world is pulse oximetry.[7]
A large number of anaesthesia providers in low-resource settings lack sufficient training about monitoring oxygen levels in the blood. The WHO and the World Federation of Societies of Anaesthesiologists (WFSA) have undertaken several initiatives to rectify this problem. WHO Patient Safety, together with the WFSA, the Association of Anaesthetists of Great Britain and Ireland (AAGBI) and others, has developed a training toolkit to improve provider response to hypoxemia. WFSA and the AAGBI joined with the Harvard School of Public Health and Brigham and Women's Hospital, Boston, to form the Lifebox Foundation, registered as a charity in the UK 2011 and then in the United States in 2015.[7,8,9] The Lifebox Foundation is an independent charity focused on making surgery safer in low-resource countries. It is estimated that more than 70,000 operating rooms worldwide lack access to pulse oximetry, and the risk of anaesthesia mortality can be as high as 1 in 133.[8] With support from WFSA and its members worldwide, Lifebox has provided more than 15,000 pulse oximeters in 100 countries.[7] The Lifebox pulse oximeter is a robust, accurate device which is suitable for use in developing countries. Each oximeter is accompanied by an education programme consisting of a manual, a video and slide sets to improve provider response to hypoxemia. These include an algorithm for managing hypoxia and a set of clinical cases for practice, and presentations on the use and maintenance of the oximeter itself.[9]
The Indian Society of Anaesthesiologists (ISA) is an active member of the WFSA and participates in these WFSA initiatives. Recently, as part of the ‘Safe Anaesthesia, Safe Country’ project, the WFSA and the ISA launched a project on training anaesthesia providers in the detection and response to hypoxia, and distribution of pulse oximeters where necessary in the state of Telangana (Dr. Muralidhar Joshi, Governing Council Member, WFSA, personal communication). ISA Nanded conducted a needs assessment survey for the Lifebox Foundation covering public as well as private health care facilities in the Nanded district of Maharashtra. In some hospitals, especially in rural areas, pulse oximetry was not available at all; in others, pulse oximetry was available during surgery in the operating room, but not in the immediate recovery period. Based on this survey, Lifebox Foundation pulse oximeters and training material will be given to nearly 200 centres in Nanded district by the President-Elect of the WFSA during the Maharashtra State Conference of the ISA in October this year (Dr. Someshwar Patange, ISA Nanded, Personal Communication).
An article published in this journal in 2011 reported that from December 2007 to January 2008, it was not possible to monitor every patient undergoing a surgical procedure with a pulse oximeter in four hospitals in Haryana state (including a tertiary referral hospital). The deficit of 20 oximeters was reduced by the donation of 12 units through the Global Oximetry project.[10]
In a Brief Communication in this issue of the IJA, Rastogi et al. describe the results of an initiative taken by the Organizing Committee of the 50th Annual Conference of the ISA held in December 2010. In response to a questionnaire sent to over 11,000 members of the ISA, they received 1416 applications requesting delivery of a free pulse oximeter and distributed 1064 free pulse oximeters to anaesthesiologists working in areas where a pulse oximeter was not available. Needless to say, the availability of the pulse oximeters changed practice and improved patient care and safety.[11]
These reports clearly demonstrate that even in the year 2017, it is not possible to meet the minimum requirements laid down by the WHO and several professional associations, including the ISA,[12] to provide safe anaesthesia in India. The initiatives undertaken by Lifebox Foundation, the Global Oximetry project and those undertaken by the Organizing Committee of the 50th Annual Conference of the ISA are commendable and necessary. They help bridge the ‘oximetry gap’.
However, if India aspires to play a leading role in the world stage, the health of its citizens cannot be jeopardised by a lack of availability of simple, basic equipment. There may be several reasons why a pulse oximeter may not be used during each and every anaesthetic. These include non-availability of the oximeter, breakdown of the instrument, damaged probes and non-replacement of batteries. However, these should be considered as excuses, rather than valid reasons. Admittedly, there are several other issues that need to be addressed to provide safe anaesthesia for all. These include the shortage of qualified workforce and maldistribution of the trained workforce between the rural and urban areas.[13] Nevertheless, universal availability of working pulse oximeters is a simple, inexpensive and achievable target.
Medical philanthropy can be a short term solution that can reduce the magnitude of the problem. In the long run, it is the responsibility of the health care system in India, public and private, to make our operation theatres and surgical wards self-sufficient and capable of providing at least the bare basics of safe anaesthesia and safe surgery. It is the duty of all hospital administrators, whether in government or private hospitals, and rural or urban health centres as well as practitioners to ensure that working pulse oximeters are available for every surgery. Each institution should have mechanisms to ensure an uninterrupted availability of supplies and spares to ensure that all oximeters are in working condition. There must be accountability for failure to achieve this simple goal. Awareness of these simple facts must be created among government agencies, non-governmental organisations, professional associations, lay public and the media.
Every citizen must be able to access safe surgery and safe anaesthesia.
'But I have promises to keep
And miles to go before I sleep
And miles to go before I sleep'.
-Robert Frost
REFERENCES
- 1.World Health Organisation. Safe Surgery. [Last accessed on 2017 Jul 05]. Available from: http://www.who.int/patientsafety/topics/safe-surgery/en/
- 2.Pearse RM, Moreno RP, Bauer P, Pelosi P, Metnitz P, Spies C, et al. Mortality after surgery in Europe: A 7 day cohort study. Lancet. 2012;380:1059–65. doi: 10.1016/S0140-6736(12)61148-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kahan BC, Koulenti D, Arvaniti K, Beavis V, Campbell D, Chan M, et al. Critical care admission following elective surgery was not associated with survival benefit: Prospective analysis of data from 27 countries. Intensive Care Med. 2017;43:971–79. doi: 10.1007/s00134-016-4633-8. [DOI] [PubMed] [Google Scholar]
- 4.Bainbridge D, Martin J, Arango M, Cheng D. Evidence-based Peri-operative Clinical Outcomes Research (EPiCOR) Group. Perioperative and anaesthetic-related mortality in developed and developing countries: A systematic review and meta-analysis. Lancet. 2012;380:1075–81. doi: 10.1016/S0140-6736(12)60990-8. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organisation. Surgical Safety Checklist. [Last accessed on 2017 Jul 05]. Available from: http://www.whqlibdoc.who.int/publications/2009/9789241598590_eng_Checklist.pdf .
- 6.Haynes AB, Weiser TG, Berry WR, Lipsitz SR, Breizat AH, Dellinger EP, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med. 2009;360:491–9. doi: 10.1056/NEJMsa0810119. [DOI] [PubMed] [Google Scholar]
- 7.Pulse Oximetry. [Last accessed on 2017 Jul 05]. Available from: http://www.lifebox.org/what-we-do/pulse-oximetry/
- 8.World Federation of Societies of Anaesthesiologists, Lifebox. [Last accessed on 2017 Jul 05]. Available from: http://www.wfsahq.org/our-work/safety-quality .
- 9.Enright A, Merry A, Walker I, Wilson I. Lifebox: A global patient safety initiative. A A Case Rep. 2016;6:366–9. doi: 10.1213/XAA.0000000000000335. [DOI] [PubMed] [Google Scholar]
- 10.McHugh GA, Pollard BJ, Hooda S, Thoms GM. The impact of increasing oximetry usage in India: A pilot study. Indian J Anaesth. 2011;55:235–41. doi: 10.4103/0019-5049.82662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rastogi A, Agarwal A, Singh PK, Haldar R, Kannaujia A. Distributing pulse oximeter: An initiative for improving patient safety and care. Indian J Anaesth. 2017;61:594–6. doi: 10.4103/ija.IJA_89_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Indian Society of Anaesthesiologists: Monitoring Standards for Providing Anaesthesia. [Last accessed on 2017 Jul 05]. Available from: http://www.isaweb.in/Downloads/monitoring_standards.pdf .
- 13.World Federation of Societies of Anaesthesiologists. Safe Anaesthesia in the South Asian Region: Reflections on safety At the SAARC-AA Congress. [Last accessed on 2017 Jul 05]. Available from: http://www.wfsahq.org/latest-news/latestnews/692-safe-anaesthesia-inthe-south-asian-region-reflections-on-safety-at-the-saarc-aacongress .


