Abstract
Background and Aims:
Minimum alveolar concentration (MAC) monitoring is an integral part of modern-day anaesthesia. Both MAC and MAC-awake are age dependant, and age of the patient needs to be entered in the monitor. This study was aimed to assess the practice of patient birth year entry in the anaesthesia monitor and its impact on MAC monitoring.
Methods:
Sixty volatile anaesthetic-based general anaesthetics (GAs) were observed silently in two tertiary care teaching hospitals with regard to ‘birth year’ entry in the patient monitor. The impact on MAC for non-entry of age was assessed. The observed MAC reading and the MAC corrected for age (MACage) of the patients were noted. Paired t-test was used to compare the differences in observed MAC and MACage values. P <0.05 was significant.
Results:
Sixty GAs of patients aged between 10 and 68 years were observed; 96.67% anaesthetics were conducted without entering ‘birth year’. Thirty-four patients (mean age 35.14 ± 15.38 years) were further assessed for impact of non-entry of age. The observed MAC was similar to MACage in patients aged 40 ± 5 years (36–45 years group). Nearly 79.41% of the observed MACs were incorrect; 55.88% patients were potentially underdosed whereas 23.53% were overdosed.
Conclusion:
Omitting patient age entry in the monitor results in erroneous MAC values, exposing patients <40 years to underdosing and older patients to overdose.
Key words: Anaesthetics, anaesthesia, drug, general, inhalation, intraoperative monitoring, monitoring, patient monitoring
INTRODUCTION
Minimum alveolar concentration (MAC) derived from the end-tidal anaesthetic concentration is commonly used for monitoring depth of anaesthesia during general anaesthesia using volatile anaesthetics.[1] Volatile anaesthetic agent monitoring facility is widely available in the present-day anaesthesia monitors. In human subjects, there is an age-dependent change in sensitivity to volatile agents, which is represented by a change in both MAC and MAC-awake with age. Each increasing decade of life is associated with a 6%–6.7% decrease in MAC.[2,3] Anaesthesiologists not only monitor MAC but also plan anaesthesia with target MAC. The age of the patient is, however, required to be entered manually in the patient monitor. If age is not entered, the monitor will display the MAC for a 40–year-old patient by default.[4] We aimed to assess the practice of patient admission (birth year entry) in the anaesthetic agent monitor. In the second part of the study, we assessed the impact of wrong age entry on the observed MAC monitored in relation to the age-specific MAC (MACage).
METHODS
After approvals from the authority, the study was conducted in two tertiary care teaching hospitals. Sixty volatile anaesthetic based-general anaesthetics (GAs) were observed silently (without the knowledge of the anaesthesiologist, surgeon and technician who were conducting the case) and patients' admission in the monitor in terms of ‘birth year’ entry were noted at the starting and till the induction phase was over for the case.
The assessment of impact for age non-entry on MAC was done by noting the observed reading on the anaesthetic agent monitor, and then by noting the MACage after entering the birth year in the patient monitor. No intervention to change the anaesthetic management of the ongoing GA was done. GAs where nitrous oxide was contraindicated and GAs which did not extend >20 min in the maintenance phase of anaesthesia were excluded from the second part of the study. The Mindray WATO EX 65 anaesthesia machine and Beneview T8 monitor (Mindray Medical International Limited, China) with anaesthetic agent monitoring facility were used. Isoflurane as well as sevoflurane (both from Abbott Laboratories, USA) were used for anaesthesia using the Mindray V60 and Drager Tec7 vaporiser, respectively. The age, sex, body weight, American Society of Anesthesiologists physical status and surgical category as per National Institute of Health and Clinical Excellence were noted.[5]
The observed MAC reading and MACage data were taken during maintenance phase of anaesthesia at least 20 min after induction. Fixed fresh gas flow (FGF) of both oxygen and nitrous oxide (N2O) and dial settings of agents for at least 5 min were ensured (if any changes were done towards the end of 20 min of maintenance phase) before taking data. Total FGF, fraction of inspired (Fi) and fraction of expired (Fe) N2O and other volatile agents were also noted at the time of recording MAC data. Quantitative data were expressed in absolute number and percentage scale. Data were further analysed for measuring central tendencies and dispersions. MACage and 0.7 MACage were compared with monitored MAC using paired t-test. INSTAT software (GraphPad Prism Software, La Jolla, CA, USA) was used for statistical measurements and P < 0.05 was considered statistically significant.
RESULTS
There were 34 anaesthesiologists and anaesthesia residents in the two institutes where the study was performed; 21 of them were involved in the cases. Sixty volatile anaesthetic-based GA cases (aged between 10 and 68 years with mean [95% confidence interval [CI] 36.73 (32.67–40.78) years; 38 [63.33%] females and 22 [36.67%] males) were observed. On twenty-two occasions, it was required to change the patient type (i.e., adult, paediatric and infant) in patient monitor; this was done in 19 (86.36%) occasions. In all the sixty cases, the birth year was required to be changed/entered. However, 58 (96.67%) of the observed anaesthetics were conducted without entering or changing the ‘birth year’ in the monitor.
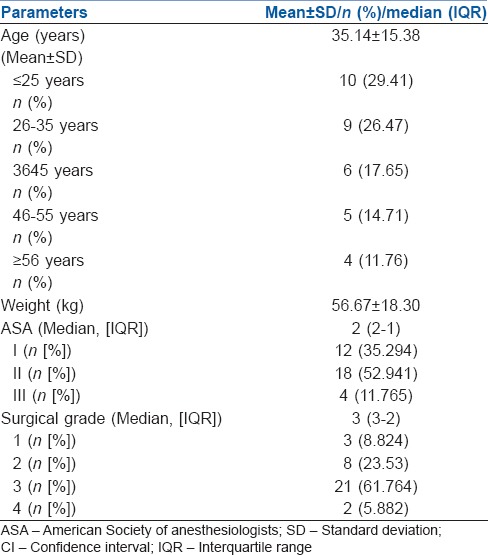
Twenty-six GAs were excluded as per exclusion criteria for comparison of MAC values. Data from 34 eligible GAs (22 [64.71%] female, 12 [35.29%] male) were collected for comparison of observed MAC and MACage. The age groups, surgical categories and physical status of the cohort for MAC comparison are presented in Table 1. Nine (26.47%) patients had comorbid medical conditions such as obesity, hypertension, hypothyroidism, diabetes mellitus and chronic obstructive pulmonary diseases either singly in different combinations.
Table 1.
Age, weight, physical class and surgical grade of the cohort analysed for age minimum alveolar concentration interaction
Twenty-four (70.59%) GAs were conducted using isoflurane. The mean ± standard deviation (SD) (95% CI) FGF of sevoflurane was significantly higher than isoflurane (1730 ± 565.78 [1325.3–2134.7] ml vs. 654.08 ± 123.78 [599.81–704.36] ml; P < 000.1). The mean ± SD of FiN2O, Fi isoflurane and Fi sevoflurane was 55.00 ± 4.69, 1.084 ± 0.16 and 1.546 ± 0.309, respectively, and FeN2O, Fe isoflurane and Fe sevoflurane 50.47 ± 4.91, 0.948 ± 0.14 and 1.23 ± 0.205, respectively, at the time of taking MAC readings.
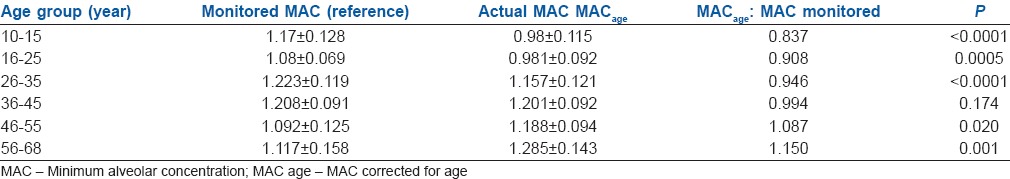
The observed MAC was comparable with the MACage in the age group of 36–45 years (P > 0.05). It was significantly higher in the patients aged <35 years and lower in patients aged >46 years. In 27 (79.41%) out of 34 patients, the observed MAC values were significantly erroneous; 19 (55.88%) of the observed MAC values were higher than age-corrected MAC (MACage), whereas 8 (23.53%) were lower than MACage. If the cases would have been conducted with target MAC (without entering birth year in patient monitor), 55.88% patients of the patients aged <35 years would have been potentially prone for underdosing whereas 23.53% patients aged >46 years would have been exposed to excess anaesthetic agent. However, in the current cohort, all patients (including patients up to 10 years of age) were found to have the observed MAC above the threshold of MAC awareness (0.7 MACage) [Table 2].
Table 2.
Comparison of mean±standard deviation of monitored minimum alveolar concentration, MACage and their ratio analysed using paired t-test
DISCUSSION
Volatile anaesthetics have been playing a central role in anaesthetic practice for nearly 170 years.[1] The concept of MAC was introduced in 1965 as a measure of anaesthetic potency and has remained a standard for the purpose.[6] Anaesthetic gas monitoring has evolved into a de facto standard of care in anaesthetic practice.[7] Respiratory gas analysis has become an integral part of the present-day anaesthesia workstations. With the increasing use of low flow anaesthesia, the need of gas analysers is even more essential.[8] The Associations of Anaesthetists of Great Britain and Ireland states that the use of a vapour analyser is essential during anaesthesia whenever a volatile anaesthetic agent or nitrous oxide is in use.[9] It also recommends that accurate records of the values determined by monitors must be kept and even included vapour concentration (end-tidal concentration) monitoring along with heart rate, blood pressure, etc., in the minimum data to be recorded.[9] As MAC is calculated from the end-tidal concentrations of anaesthetic agents, MAC monitoring can also be regarded as one of the minimum monitoring standards.
MAC was defined as alveolar concentration at which 50% of patients will not show a motor response to a standardised surgical incision at one atmosphere.[1] It is also a surrogate of depth of anaesthesia. Anaesthetic agent monitors derive the MAC from the end-tidal concentration (alveolar concentration) of the anaesthetic agent. The alveolar concentrations for different agents for deriving MAC values are published by the United States Food and Drug Administration for a healthy 40-year-old male patient.[4] For the patients of other ages, the monitor uses an algorithm to derive the MAC corrected for the age of the patient (MACage), which needs patients age[4] to be entered in the monitor
MACage = MAC40 × 10(−0.00269 × (age-40)), where MAC40-MAC standard or default for a healthy 40-year-old male patient.[4]
Therefore, to get accurate, reliable and appropriate MAC (MACage), entry of the patients' age in the monitor is must. Otherwise, the monitor by default displays the MAC value for a 40 year old patient. Changing the patient type from adult, paediatric or infant, changes the default settings of haemodynamics and ventilation but not the MAC default. Further, if previously a 65 year old patient was admitted and the next patient, a 15 year old, is taken without restarting or readmitting the patient in the monitor, the monitor will display the MAC value for a 65 year old patient, and not the default for a 40 year old patient. Recent evidence suggests that the protocol which alerts anaesthesiologists whenever end-tidal anaesthetic concentration falls to 0.7 MAC has the potential to decrease intra-operative awareness with explicit recall.[10] This indicates that a 30% variation (low record) of MAC may lead to awareness. If we take the previous example, the latter patient is potentially in the range of awareness (6.7%/decade × 5 decades = 33.5% variation). Although in the present cohort, the mean MACage and observed MAC ratio as well as values were not <0.7; from the above example, it is clear that age non-entry can leave a young patient potentially in awareness range.
Wrong age entry in the patient record at the time of hospital admission also does happen, especially in illiterate patients. The present study finding indicates that if the age entered in the monitor is within 5 years of the patient's correct age, the monitored MAC will be statistically indifferent from MACage95% of times.
There are few data on awareness during anesthesia from the Indian population. One study has concluded that the incidence is <1 in 300 (0.33%).[11] However, awareness under anaesthesia is distressing and has a potential for long-term consequences. It is also opined that every effort should be undertaken to prevent it.[11] Anaesthesia hazards can happen both due to the equipment failure and human error. Hardware failures in modern anaesthesia delivery equipment leading to hazards are uncommon.[12] It is rather more common due to the unintentional misuse of the equipment, human error or equipment failure without the user being aware that a failure had taken place.[12] The present study finding of 96% of ‘birth year’ non-entry in the monitor leading to incorrect readings can be regarded as a human error which can potentially culminate in hazards of overdose, underdosing and even awareness. This error can be avoided by making ‘birth year’ entry as a part of checklist before starting any case. The monitor software also probably can be configured in future to prompt ‘birth year’ entry in the monitor or machine before displaying agent monitoring values or starting the cases and even when monitor is activated to measure mode from standby mode.
Misinterpretation of MAC value in context to age has been reported before too.[13] However, the present study finding of patient age not being entered in 96% of all anaesthetics, leading to erronous MAC readings in 79% of these indicates that this issue needs to be publicised more. Avoiding this simple and common human error can have a major impact on MAC monitoring.
The present study is limited with regard to observations made in only two hospitals with small samples. Moreover, the case mixes, especially age group variation are also very much likely to be different in different hospitals. However, the very high percentage of wrong MAC recording indicates that the finding is likely to have a strong implication in clinical practice.
CONCLUSION
Patient's age entry in the monitor was rarely practiced. This human error, in turn, resulted in wrong MAC values being displayed and potentially exposed patients younger than 40 years to underdosing and older patients to drug overdose. We suggest that entry of patients' age in the anaesthetic agent monitor should be included as one of the items in the preoperative checklist before starting a case.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Eger EI, 2nd, Saidman LJ, Brandstater B. Minimum alveolar anesthetic concentration: A standard of anesthetic potency. Anesthesiology. 1965;26:756–63. doi: 10.1097/00000542-196511000-00010. [DOI] [PubMed] [Google Scholar]
- 2.Mapleson WW. Effect of age on MAC in humans: A meta-analysis. Br J Anaesth. 1996;76:179–85. doi: 10.1093/bja/76.2.179. [DOI] [PubMed] [Google Scholar]
- 3.Eger EI., 2nd Age, minimum alveolar anesthetic concentration, and minimum alveolar anesthetic concentration-awake. Anesth Analg. 2001;93:947–53. doi: 10.1097/00000539-200110000-00029. [DOI] [PubMed] [Google Scholar]
- 4.Beneview T8 Patient Monitor: Operator's Manual. Shenzhen: Shenzhen Mindray Bio-Medical Electronics Co. Ltd; 2016. Mindray MAC values; pp. 22–3. [Google Scholar]
- 5.National Guideline Centre (UK) NICE Guideline No. 45. London: National Institute for Health and Care Excellence (UK); 2016. [Last cited on 2016 Dec 24]. Preoperative Tests (Update): Routine Preoperative Tests for Elective Surgery. Available from: https://www.nice.org.uk/guidance/ng45/chapter/recommendations . [PubMed] [Google Scholar]
- 6.Bovill JG. Inhalation anaesthesia: From diethyl ether to xenon. Handb Exp Pharmacol. 2008;182:121–42. doi: 10.1007/978-3-540-74806-9_6. [DOI] [PubMed] [Google Scholar]
- 7.Langton JA, Hutton A. Respiratory gas analysis. Contin Educ Anaesth Crit Care Pain. 2009;9:19–23. [Google Scholar]
- 8.Garg R, Gupta RC. Analysis of oxygen, anaesthesia agent and flows in anaesthesia machine. Indian J Anaesth. 2013;57:481–8. doi: 10.4103/0019-5049.120144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Checketts MR, Alladi R, Ferguson K, Gemmell L, Handy JM, Klein AA, et al. Recommendations for standards of monitoring during anaesthesia and recovery 2015: Association of Anaesthetists of Great Britain and Ireland. Anaesthesia. 2016;71:85–93. doi: 10.1111/anae.13316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aranake A, Mashour GA, Avidan MS. Minimum alveolar concentration: Ongoing relevance and clinical utility. Anaesthesia. 2013;68:512–22. doi: 10.1111/anae.12168. [DOI] [PubMed] [Google Scholar]
- 11.Ambulkar RP, Agarwal V, Ranganathan P, Divatia JV. Awareness during general anesthesia: An Indian viewpoint. J Anaesthesiol Clin Pharmacol. 2016;32:453–7. doi: 10.4103/0970-9185.173363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eisenkraft JB. ASA Refresh Courses in Anesthesiology. Vol. 37. Philadelphia: Lippincot Williams & Wilkins; 2009. Hazards of the anesthesia workstation; pp. 37–55. [Google Scholar]
- 13.Byrappa V, Kamath S, Venkataramaiah S. Misinterpretation of minimum alveolar concentration: Importance of entering demographic variables. Indian J Anaesth. 2014;58:504–5. doi: 10.4103/0019-5049.139034. [DOI] [PMC free article] [PubMed] [Google Scholar]


