Abstract
Background and Aims:
The supraclavicular and infraclavicular brachial plexus blocks have a similar distribution of anaesthesia, and both can be used effectively for surgeries of the upper limb. This study aimed to compare the supraclavicular and infraclavicular approaches of brachial plexus blocks, guided by ultrasound and neurostimulation.
Methods:
Sixty adult patients scheduled for elective upper limb surgery of the elbow and/or below were randomly divided into two groups: infraclavicular Group (I) and supraclavicular Group (S). All the blocks were performed with the aid of ultrasound-guided nerve stimulator confirmation. The two groups were compared with respect to block performance time, onset of sensory and motor blockade, readiness for surgery, success rate and complications. The statistical analysis was performed with Student t-test and Chi-square test.
Results:
The block performance time for the infraclavicular group was 9.57 ± 3.19 min, whereas for supraclavicular group, it was 11.53 ± 2.90 min with similar success rates (93.3%). Onset of sensory blockade was achieved earlier (6.43 ± 2.61 min) in Group I than Group S (8.45 ± 2.87 min, P = 0.006). The onset of motor blockade was similar in Group I (7.32 ± 2.90 min) and Group S (8.68 ± 3.50 min, P = 0.121). The patient satisfaction was similar in both the groups. One patient had a pneumothorax, three patients developed Horner syndrome and another had clinically symptomatic diaphragmatic paresis in Group S.
Conclusion:
The infraclavicular block is more rapidly executed compared to supraclavicular block with similar success rates and fewer complications in the presence of ultrasound and nerve stimulator and hence should be preferred.
Key words: Brachial plexus block, infraclavicular block, nerve stimulator, supraclavicular block, ultrasound
INTRODUCTION
A well-conducted regional anaesthetic technique has very much to offer to anaesthesiologist, surgeon, as well as patients owing to its advantages over general anaesthesia such as remaining conscious, avoiding polypharmacy, better haemodynamic stability and excellent post-operative analgesia.[1,2] The supraclavicular brachial plexus block is a popular technique for surgeries below the shoulder because of its quick onset and high success rate.[3] However, the major disadvantages are higher incidence of complications such as inadvertent vascular injections, pneumothorax, phrenic nerve palsy and Horner's syndrome. The introduction of ultrasonography has rekindled the interest in infraclavicular block. The main advantage of infraclavicular block is the fewer incidences of complications with ultrasound, and it is ideally suited for catheter techniques. The disadvantage is that plexus is situated deeper at this level and the angle of approach is more acute making synchronised visualisation of the relevant anatomy and needle challenging in inexperienced hands and in obese patients.[4]
Although both supraclavicular and infraclavicular blocks can be utilised for upper limb surgeries, anaesthesiologists often have an inclination for supraclavicular over infraclavicular block because of the technical difficulty and increased complications with the blind approach in the latter. The advent of ultrasonography in anaesthesia practice has made it a valuable adjunct in peripheral nerve blocks.[5] The inherent benefits of direct visualisation of nerves and surrounding anatomy, continual observation of the needle tip and spread of local anaesthetic make ultrasound-guided regional anaesthesia highly appealing. The utilisation of nerve stimulator alongside ultrasound increases the success rate and gives an added point of interest when educating residents. Hence, we hypothesised that infraclavicular block will be faster to perform and as safe as supraclavicular block with fewer complications while using both ultrasound and nerve stimulator.
There are fewer studies in the literature comparing supraclavicular and infraclavicular blocks using either ultrasonography or neurostimulation. However, there are no studies comparing the two routes of brachial plexus block using both ultrasound guidance and neurostimulation, to the best of our knowledge. The aim of this study is to compare infraclavicular and supraclavicular approaches to to brachial plexus block using ultrasound guided neurostimulation.
METHODS
After approval by the Institutional Ethical Committee, this prospective, randomised and observer-blinded study was done on 60 patients undergoing elective upper limb surgeries of the elbow, forearm and hand in a tertiary medical college hospital. Patients of the American Society of Anesthesiologists' (ASA) Physical status I or II, weighing between 50 and 100 kg and in the age group of 18–60 years, were included in the study. Unco-operative patients, patients with significant pulmonary pathology and those who were allergic to the amide local anaesthetics were excluded from the study. Patients with chest deformity, clavicle fracture and pregnancy were not included in the study. The written informed consent for the study was obtained from each patient. The patients were randomised to receive either infraclavicular (Group I) or supraclavicular (Group S) blocks by computer-generated random numbers and closed-envelope method. All the patients were premedicated with alprazolam 0.5 mg orally before shifting to the operation theatre. All the blocks were performed by the anaesthesiologist with experience of performing 10-30 blocks using both ultrasound and nerve stimulator under the supervision of an experienced anaesthesiologist. All the blocks were performed with 30 mL 0.5% ropivacaine. A randomisation envelope was opened at this stage and the patient was allocated to either Group I or S. After opening the envelope, all the blocks were performed by first anaesthesiologist who takes no further part in that case management.
A GE Vivid Ultrasonogram Machine, with 12 MHz linear probe with colour Doppler, was utilised for the study. A peripheral nerve stimulator (Innervator 272, Fisher and Paykel Healthcare international, NewZealand, model no: NS272AUU) and 5 cm short beveled, hypodermic, insulated needle were used for the blocks. The patient was in supine position with the head turned away from the side to be blocked for the infraclavicular block. The skin was disinfected and draped. The transducer was placed in the parasagittal plane just medial to the coracoid process and inferior to the clavicle, and the axillary artery was visualised. The needle was then inserted in-plane from the cephalic aspect, with the insertion point just inferior to the clavicle. The needle was aimed towards the posterior part of the axillary artery as it passes through the pectoralis muscles. The goal was to inject the local anaesthetic until it spread around the artery and not to target individual cords. Neurostimulation was used concurrently at 1 mA intensity, and posterior cord motor response of the finger and hand extensions was elicited as the needle was advanced. About 30 mL of 0.5% ropivacaine was administered under ultrasound visualisation to achieve a U-shaped spread around the artery.
The supraclavicular block was performed with the patient in supine position and the head tilted to the opposite side, and the skin was disinfected and draped. The transducer was positioned in the transverse plane immediately superior to the clavicle at approximately its midpoint. The subclavian artery, pleura and first rib were visualised along with brachial plexus. The objective was to place the needle in the brachial plexus sheath and inject ropivacaine to visualise the spread within the brachial plexus and the centrifugal displacement of the trunks and divisions. As the needle entered the brachial plexus sheath, a current intensity of 1 mA was given using the peripheral nerve stimulator. Motor response of the hand was elicited to confirm proper needle placement. The current intensity was then lowered to 0.5 mA at which lowest twitch response was elicited. After confirmation of needle placement, 30 ml of 0.5% ropivacaine was injected in two places.
The second anaesthesiologist who was blinded to the type of block given monitored all the study parameters and decided on further management of the patient. The onset and degree of sensory and motor block were observed every 5 min for 30 min till complete blockade was achieved. If after 30 min complete sensory blockade was not achieved and patient perceived pain, then it was a taken as a failed block. If the single nerve was spared, then a rescue block of the concerned nerve at appropriate level was given. If more than one nerve was spared, then general anaesthesia was administered. The sensory score was assessed using needle-prick method by testing the five individual nerves median nerve, radial nerve, ulnar nerve, musculocutaneous nerve and medial cutaneous nerve of the forearm. The scoring system adapted from Koscielniak-Nielsen et al.[6] was followed for checking sensory block (0 – sharp pain, 1 – touch sensation only and 2 – no sensation). The quality of motor block was observed on a four-point scale and was adapted from Lavoie et al. and Lahori et al.[7,8]: 0-Flexion and extension in both the hand and arm against resistance, 1-Flexion and extension in both the hand and arm against gravity but not against resistance, 2-Flexion and extension movements in the hand but not in the arm and 3-No movement in the entire upper limb.
The onset of sensory block was defined as the time elapsed between injection of drug and complete loss of pinprick sensation, whereas onset of motor blockade was outlined as the time elapsed from injection of drug to complete motor block. The patients were asked for their satisfaction level during the performance of block and surgery by the two point assessment scale 0-unsatisfied and 1-satisfied.[2] They were asked to mark it as satisfied only if they will be happy to accept the same block in future. The block performance time was defined as the time interval from placement of ultrasound probe to the removal of needle after injection of local anaesthetic. The time patient was ready for surgery was taken as the time after completing the block to the achievement of complete sensory and motor blockade. The following adverse effects were observed: accidental vascular puncture, pneumothorax, diaphragmatic paresis and Horner's syndrome.
The primary objectives of this prospective, randomised and observer-blinded study were to compare the block performance time and success rate of supraclavicular and infraclavicular approaches to brachial plexus block using ultrasound-guided neurostimulation. The secondary aims were to compare the onset of sensory and motor blockade, readiness for surgery, patient satisfaction and complications associated with each approach.
We hypothesised that infraclavicular block would have faster block performance time compared to supraclavicular block. The block performance time for infraclavicular block was assumed to be 5 min based on performance time in Koscielniak-Nielsen et al.[6] For the study to have 80% power and alpha error at 0.05, a minimum of 28 patients would be required in each group to detect a 20% difference in block times (with an effect size of 1 min), assuming a standard deviation of 1.5. Hence, we enrolled 30 patients in each group to compensate for possible dropouts. Data were entered in MS-Excel spreadsheet (2007) and were analysed using the statistical package for social sciences version 20 (trial version). Descriptive statistics including proportions, measures of central tendency and measures of dispersion were used to describe the data. Further, Student's t-test was used to compare means between the groups and Chi-square test was used to compare proportions. A P < 0.05 was considered to be statistically significant.
RESULTS
Sixty-eight patients were recruited into the study and a CONsolidated Standards of Reporting Trials flow diagram depicting the passage of participants through the study has been provided in Figure 1.
Figure 1.
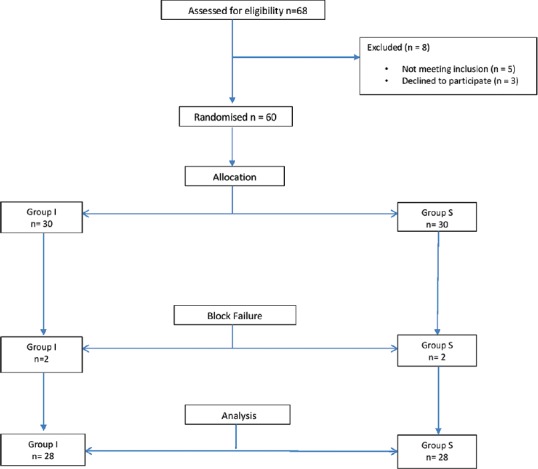
CONsolidated Standards of Reporting Trials flow chart
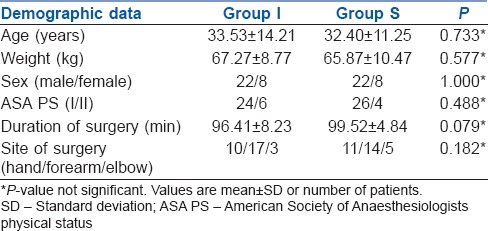
The patients who underwent elective surgeries of the upper limb were included in the study. Both the groups were comparable in terms of demographic profile [Table 1]. The duration of surgery and site of surgeries [Table 1] were also found to be similar, and no statistical significance was present. All the data obtained showed a normal distribution, and no skewed distribution was reported.
Table 1.
Demographic profile
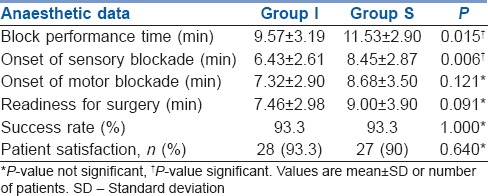
The block performance time was relatively quicker in Group I (9.57 ± 3.19 min) than Group S (11.53 ± 2.90 min) (P = 0.015) [Table 2]. The success rate of 93.3% was similar in both the groups (P = 1.000). There were four cases of block failure with two in each group. The ulnar nerve was spared in three patients (two in Group I and one in Group S), and it was supplemented. More than two nerves were spared in one patient in Group S, and general anaesthesia was administered. The data from these four patients were not taken for further analysis of sensory and motor blockade. The satisfaction score was better in Group I with 93.3% in comparison to Group S with a satisfaction score of 90%. However, there was no statistical significance in patient satisfaction (P = 0.640). The sensory blockade was achieved earlier (6.43 ± 2.61 min) in I Group than S Group (8.45 ± 2.87 min) and was found to be statistically significant (P = 0.006). The onset of motor blockade was faster in Group I (7.32 ± 2.90 min) than Group S (8.68 ± 3.50 min) but with a P = 0.121 which was not significant statistically. There was no statistically significant difference in the time taken for patients being ready for surgery, Group I patients were ready at 7.46 ± 2.98 min and Group S patients were ready at 9.00 ± 3.90 min for surgery (P = 0.091).
Table 2.
Anaesthetic data
The vital parameters heart rate, blood pressure and oxygen saturation were comparable between the two groups during the surgery, and there was no statistically significant difference between them [Figures 2 and 3]. One patient in Group S developed pneumothorax which needed intercostal drain insertion, and the patient recovered well. Three patients in Group S developed Horner's syndrome against none in Group I. All the three cases were managed conservatively with reassurance, and they recovered well within 24 h. One of these patients also developed clinically significant diaphragmatic paralysis which was confirmed with chest X-ray. The patient was having breathing difficulty and room air saturation of 92%. The patient was managed conservatively with oxygen by the face mask and continuous observation. The patient recovered well in 24 h. There were three cases of vascular puncture in Group S compared to one case in Group I. Although more complications were reported in Group S, they were not statistically significant (P = 0.704).
Figure 2.
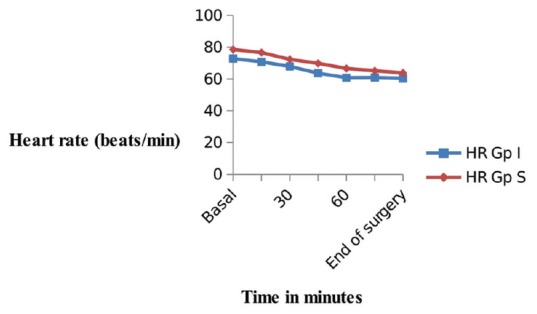
Changes in heart rate during surgery
Figure 3.
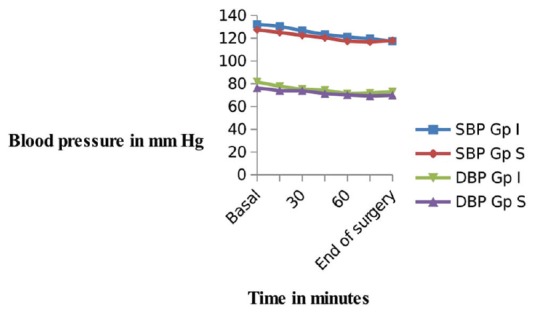
Changes in blood pressure during surgery
DISCUSSION
In this prospective, randomised, observer-blinded study, supraclavicular and infraclavicular blocks performed with the aid of ultrasound-guided neurostimulation were compared. The New York School of Regional Anaesthesia recommendations for performing both the blocks were followed. The supraclavicular block was performed by administering two aliquots of ropivacaine at two separate locations within the brachial plexus sheath.[3] We did the infraclavicular block by injecting the local anaesthetic until the U-shaped spread around the artery was documented.[4] The individual cords were not targeted, and the needle was aimed towards the posterior cords. However, some studies have suggested a single injection technique for the supraclavicular block as well.[9,10,11]
The block performance time for infraclavicular block was less compared to supraclavicular block. The additional minutes captivated for the supraclavicular block may be because the needle was targeted at two points in supraclavicular block, whereas the local anaesthetic was deposited at only one point in infraclavicular block. The mean block performance time of 5.7 min in the supraclavicular group and 5.0 min in the infraclavicular group was reported in one study.[6] The success rate of the brachial plexus block among the two groups in our study showed that 28 (93.3%) cases had a successful blockade while two (6.7%) cases in each group had block failure. The success rate of 93% in infraclavicular group compared with only 78% in supraclavicular block with ultrasound guidance was reported in one study.[6] However, three other studies[9,12,13,14] quoted a success rate of around 95% for ultrasound-guided supraclavicular blocks. A success rate of 90%–95% for ultrasound-guided infraclavicular block was quoted in few studies.[15,16] All these findings are similar to the success rate of our study.
In our study, we found that the onset of sensory blockade, as well as motor blockade, was slightly earlier in the infraclavicular group. In a study, where the sensory block to all seven terminal nerves following brachial plexus block was studied, they concluded that supraclavicular block had a significantly poorer block of the median and ulnar nerves but a better block of the axillary nerve.[6]
In our study, pneumothorax and ipsilateral diaphragmatic paresis occurred in one patient each in supraclavicular group but none in infraclavicular group. Horner's syndrome developed in three patients in supraclavicular group and all the patients were managed conservatively. Three patients had vascular puncture in supraclavicular group compared to one patient in infraclavicular group. This high incidence of vascular puncture may be attributed to relative inexperience of anaesthesiologist performing the block which was a drawback of our study. Horner's syndrome and diaphragmatic paresis were reported in 20% of patients with supraclavicular block in one study.[6] A 50% incidence of diaphragmatic paresis have been reported in supraclavicular block when using more sensitive methods of assessment such as ultrasound, plethysmography and pulmonary function tests.[17] Since we used only clinical assessment and chest X-ray for diagnosis, the incidence was only 3% in our study. A 3% incidence of diaphragmatic paresis in supraclavicular block on the basis of clinical diagnosis with breathing difficulties and chest X-ray was reported in one study,[13] and this correlates with our study. Pneumothorax was reported in two patients (4%) in supraclavicular block performed blindly.[2] One incidence of pneumothorax in our study shows that we need to be more careful even with the use of ultrasound for supraclavicular block and needle should not be advanced without observing the tip. The incidence of vascular puncture was three times more in supraclavicular block in our study. The vascular puncture incidence was reported from 2%[6] to 2.5%[9] in other studies
The infraclavicular block was performed faster and had similar success rate to supraclavicular block. The onset of sensory blockade was faster in infraclavicular group and had fewer complications. These findings support our hypothesis that infraclavicular block is safe can be performed faster than supraclavicular block in the presence of ultrasound and nerve stimulator.
There are three limitations in our study. First, although all the results were in favour of infraclavicular block, we could not establish a statistically significant difference in complication rate and readiness for surgery, and the post hoc power analysis showed that much larger sample size may be needed to achieve a statistical difference. Second, we did not use catheters for blocks. It was claimed that with infraclavicular block, the catheter can be maintained more easily than supraclavicular block. The future research can also involve the utilisation of catheters. Third, the incidence of vascular puncture and pneumothorax in the presence of ultrasound is controversial. Being a medical college hospital, all the blocks were performed by residents with minimum experience of 10 blocks in each group. If all the blocks were to be performed by an experienced anaesthesiologist, complications such as vascular puncture and pneumothorax may have been reduced. However, experience is not going to alter the other findings of Horner syndrome and diaphragmatic paresis. The existing evidence suggests that both infraclavicular and supraclavicular block are comparable when either ultrasound or nerve stimulator was used alone. This study adds to the evidence that when both ultrasound and nerve stimulator are used, infraclavicular block is safer, faster and as effective as supraclavicular block.
CONCLUSION
Ultrasound-guided neurostimulation technique resulted in faster performance of infraclavicular block compared to supraclavicular block.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Shah S, Mehta K, Patel K, Patel K. Comparison of infraclavicular brachial plexus block with supraclavicular brachial plexus block in upper limb surgeries. NHL J Med Sci. 2013;2:43–5. [Google Scholar]
- 2.Yang CW, Kwon HU, Cho CK, Jung SM, Kang PS, Park ES, et al. A comparison of infraclavicular and supraclavicular approaches to the brachial plexus using neurostimulation. Korean J Anesthesiol. 2010;58:260–6. doi: 10.4097/kjae.2010.58.3.260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Website – Nysora.com. The New York School of Regional Anesthesia. Ultrasound-Guided Supraclavicular Brachial Plexus Block. 2013. Sep 19, [Last accessed on 2017 Jun 15]. Available from: http://www.nysora.com/techniques/3015-ultrasound-guidedsupraclavicular-brachial-plexus-block.html .
- 4.Website – Nysora. The New York School of Regional Anesthesia. Ultrasound-Guided Infraclavicular Brachial Plexus Block. 2013. Jun 08, [Last accessed on 2017 Jun 18]. Available from: http://www.nysora.com/techniques/ultrasound-guided-techniques/upperxtremity/3016-ultrasound-guided-infraclavicular-brachialplexus-block.html .
- 5.Gray AT. Ultrasound-guided regional anesthesia: Current state of the art. Anesthesiology. 2006;104:368–73. doi: 10.1097/00000542-200602000-00024. [DOI] [PubMed] [Google Scholar]
- 6.Koscielniak-Nielsen ZJ, Frederiksen BS, Rasmussen H, Hesselbjerg L. A comparison of ultrasound-guided supraclavicular and infraclavicular blocks for upper extremity surgery. Acta Anaesthesiol Scand. 2009;53:620–6. doi: 10.1111/j.1399-6576.2009.01909.x. [DOI] [PubMed] [Google Scholar]
- 7.Lavoie J, Martin R, Tétrault JP, Côté DJ, Colas MJ. Axillary plexus block using a peripheral nerve stimulator: Single or multiple injections. Can J Anaesth. 1992;39:583–6. doi: 10.1007/BF03008322. [DOI] [PubMed] [Google Scholar]
- 8.Lahori VU, Raina A, Gulati S, Kumar D, Gupta SD. A randomized comparative study of efficacy of axillary and infraclavicular approaches for brachial plexus block for upper limb surgery using peripheral nerve stimulator. Indian J Anaesth. 2011;55:253–9. doi: 10.4103/0019-5049.82670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tran DQ, Russo G, Muñoz L, Zaouter C, Finlayson RJ. A prospective, randomized comparison between ultrasound-guided supraclavicular, infraclavicular, and axillary brachial plexus blocks. Reg Anesth Pain Med. 2009;34:366–71. doi: 10.1097/AAP.0b013e3181ac7d18. [DOI] [PubMed] [Google Scholar]
- 10.Soares LG, Brull R, Lai J, Chan VW. Eight ball, corner pocket: The optimal needle position for ultrasound-guided supraclavicular block. Reg Anesth Pain Med. 2007;32:94–5. doi: 10.1016/j.rapm.2006.10.007. [DOI] [PubMed] [Google Scholar]
- 11.Tran DQ, Munoz L, Russo G, Finlayson RJ. A trick shot to the corner pocket. Reg Anesth Pain Med. 2008;33:503–4. doi: 10.1016/j.rapm.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 12.Kapral S, Krafft P, Eibenberger K, Fitzgerald R, Gosch M, Weinstabl C. Ultrasound-guided supraclavicular approach for regional anesthesia of the brachial plexus. Anesth Analg. 1994;78:507–13. doi: 10.1213/00000539-199403000-00016. [DOI] [PubMed] [Google Scholar]
- 13.Williams SR, Chouinard P, Arcand G, Harris P, Ruel M, Boudreault D, et al. Ultrasound guidance speeds execution and improves the quality of supraclavicular block. Anesth Analg. 2003;97:1518–23. doi: 10.1213/01.ANE.0000086730.09173.CA. [DOI] [PubMed] [Google Scholar]
- 14.Arcand G, Williams SR, Chouinard P, Boudreault D, Harris P, Ruel M, et al. Ultrasound-guided infraclavicular versus supraclavicular block. Anesth Analg. 2005;101:886–90. doi: 10.1213/01.ANE.0000159168.69934.CC. [DOI] [PubMed] [Google Scholar]
- 15.Ootaki C, Hayashi H, Amano M. Ultrasound-guided infraclavicular brachial plexus block: An alternative technique to anatomical landmark-guided approaches. Reg Anesth Pain Med. 2000;25:600–4. doi: 10.1053/rapm.2000.18184. [DOI] [PubMed] [Google Scholar]
- 16.Sandhu NS, Capan LM. Ultrasound-guided infraclavicular brachial plexus block. Br J Anaesth. 2002;89:254–9. doi: 10.1093/bja/aef186. [DOI] [PubMed] [Google Scholar]
- 17.Neal JM, Moore JM, Kopacz DJ, Liu SS, Kramer DJ, Plorde JJ. Quantitative analysis of respiratory, motor, and sensory function after supraclavicular block. Anesth Analg. 1998;86:1239–44. doi: 10.1097/00000539-199806000-00020. [DOI] [PubMed] [Google Scholar]


