INTRODUCTION
Advancements in various surgical techniques may be attributed to advances in the field of anaesthesia, and more so on account of better monitoring techniques.[1,2,3] In the last 50 years, there has been a significant reduction in anaesthesia-related morbidity and mortality. Patients undergoing surgery in low-income group countries still have 2- to 3-fold increased mortality risk in comparison with high-income group countries.[4]
The World Health Organization (WHO) brought global oximeter project according to which pulse oximeter use is mandatory in health-care areas.[5] The WHO introduced a new global standard for perioperative care in the year 2008 including the words ‘… pulse oximeter attached and working’.[6]
The Indian Society of Anaesthesiologists (ISA) recommends that it is mandatory for oxygenation to be monitored by pulse oximetry, which displays both saturation and heart rate.[7]
During the deliberations in the 58th Annual Conference of ISA in December 2010, it was brought to our notice that non-availability of pulse oximeters in remote areas was adversely affecting anaesthesia-related outcomes. Therefore, after successful completion of the conference, the organising committee decided to address this issue by providing pulse oximeters to members of the ISA, who were not using a pulse oximeter due to lack of its availability.
METHODS
In the period between January 2012 and December 2014, a pulse oximeter requisition form was mailed to all the members of the ISA via Indian Postal Services (n = 11,530). In response, we received a total of 1416 applications requesting delivery of a free pulse oximeter. All the requests were thoroughly reviewed by the organising committee based on the following criteria:
Anaesthesiologists were working in areas where a pulse oximeter was not available
Willingness of the anaesthesiologists to regularly use the pulse oximeter if made available and provide regular feedback.
The organising committee approved 1064 requests and thereafter a pulse oximeter was dispatched (free of cost) to all these members via registered post [Figure 1].
Figure 1.
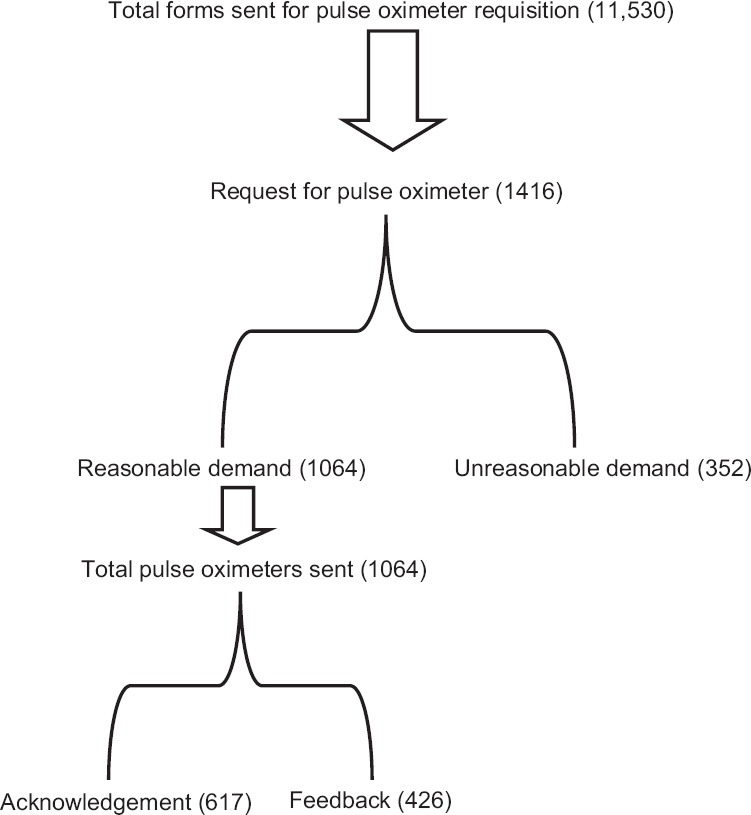
Flow diagram showing process of distribution of pulse oximeter its acknowledgment and feedback process
The pulse oximeter provided was portable fingertip probe type [Figure 2]. An undertaking was taken from the members that they would use the pulse oximeter to enhance patients' safety. All pulse oximeter receivers would maintain a logbook of pulse oximeter use, share the information and provide us with feedback at timely intervals.
Figure 2.

Picture of pulse oximeter which was distributed
RESULTS
Availability of pulse oximeter changed the anaesthesia practice of anaesthesiologists as they started using this pulse oximeter not only for intraoperative monitoring but also for post-operative monitoring of these patients [Table 1]. Further, they started using the pulse oximeter outside the confines of the operation theatres, e.g., for upper or lower gastrointestinal endoscopy, radiotherapy and biopsy procedures under sedation performed in the outpatient department (190 uses). They also started using the pulse oximeter during the pre-anaesthetic check-up to record baseline oxygen saturation, particularly in patients with compromised cardiopulmonary reserve (109 uses).
Table 1.
Critical events identified with the help of portable pulse oximeter
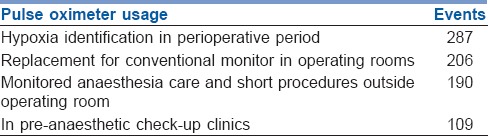
A total 287 incidents of hypoxia identification were reported with the use of pulse oximeter during anaesthesia administration.
DISCUSSION
Kotur[8] stated that in some parts of India, ‘the anaesthesiologist is expected to work with a bottle of ether and use the same two hands for monitoring pulse and blood pressure’.[2,8] In resource-limited countries, around 77,000 operating rooms are still in need of pulse oximeters. The numbers of pulse oximeters required may be as high as 100,000 if other clinical areas are also taken into consideration.[9]
Our pulse oximeter distribution programme among anaesthesiologists augmented the WHO surgical safety checklist launched in June 2008; this list is simple and can be completed in <2 min; one of the important parts of the checklist is to ensure that a proper functioning pulse oximeter is attached to the patient.[10] Our pulse oximeter distribution programme helped in identification of 287 events of hypoxia in perioperative period, which prompted prompt preventive and remedial actions and thus prevented further complications of hypoxia.
Our portable pulse oximeter was used as replacement for conventional monitor when either conventional monitor was malfunctioning or even absent. As many as 206 reported events were collected from feedback forms. Finch et al. evaluated effect of large-scale donation of pulse oximeters to non-physician anaesthesiologists in Uganda and found that oximetry and hypoxia management test scores improved after training and continued to improve at the follow-up visit.[11] Funk et al. estimated global operating theatre distribution and pulse oximetry supply from 54 countries and found that around 77,700 theatres worldwide were not equipped with pulse oximeters.[12] They also estimated that around 32 million operations are undertaken every year without a pulse oximeter and major chunk was from third world countries. Hence, there is a major disparity between the number of surgical procedures and essential monitoring equipment, and the pulse oximeter, which is a basic monitor in developed countries, is still a luxury in developing and third world countries. The pulse oximeter was also useful in monitored anaesthesia care and short procedures outside operating room (190 reported feedbacks till now).
The limitation of our work was lack of proper feedback by the users as many failed to respond. Second, only ISA members were enrolled for this study. Our work was more of a medical philanthropy and it can further be reinforced by a much greater and larger distribution of portable pulse oximeter to the nook and corners of India with a better long term follow-up. We have used “freebies concept” in distribution of pulse oximeters and after review of the feed back forms we felt the need of percolation of this data to other members of the society too.
CONCLUSION
We are of the opinion that there is a definite need for more medical philanthropy, especially in making pulse oximeter available in every nook and corner of India for saving precious human life during anaesthesia.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
We would like to acknowledge the ISA Branch, Lucknow, Uttar Pradesh, India.
REFERENCES
- 1.Moller JT, Jensen PF, Johannessen NW, Espersen K. Hypoxaemia is reduced by pulse oximetry monitoring in the operating theatre and in the recovery room. Br J Anaesth. 1992;68:146–50. doi: 10.1093/bja/68.2.146. [DOI] [PubMed] [Google Scholar]
- 2.Moller JT, Johannessen NW, Espersen K, Ravlo O, Pedersen BD, Jensen PF, et al. Randomized evaluation of pulse oximetry in 20,802 patients: II. Perioperative events and postoperative complications. Anesthesiology. 1993;78:445–53. doi: 10.1097/00000542-199303000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Pedersen T, Møller AM, Hovhannisyan K. Pulse oximetry for perioperative monitoring. Cochrane Database Syst Rev. 2014 Mar 17;3:CD002013. doi: 10.1002/14651858.CD002013.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bainbridge D, Martin J, Arango M, Cheng D. Evidence-based Peri-operative Clinical Outcomes Research (EPiCOR) Group. Perioperative and anaesthetic-related mortality in developed and developing countries: A systematic review and meta-analysis. Lancet. 2012;380:1075–81. doi: 10.1016/S0140-6736(12)60990-8. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organisation. WHO Surgical Safety Checklist and Implementation Manual. [Last accessed on 2016 Apr 10]. Available from: http://www.who.int/patientsafety/safesurgery/ss_checklist/en/index.html .
- 6.World Health Organisation. Safe Surgery Saves Lives: The Second Global Patient Safety Challenge. 2008. [Last accessed on 2016 Jan 15]. Available from: http://www.who.int/patientsafety/challenge/safe.surgery/en/
- 7.Indian Society of Anaesthesiologists. Monitoring Standards for Providing Anaesthesia. India. [Last accessed on 2016 Jan 15]. Available from: http://www.isaweb.in/Downloads/monitoring_standards.pdf .
- 8.Kotur PF. Monitoring and the anaesthesiologist. Editorial. Indian J Anaesth. 2002;46:244–5. [Google Scholar]
- 9.Howitt P, Darzi A, Yang GZ, Ashrafian H, Atun R, Barlow J, et al. Technologies for global health. Lancet. 2012;380:507–35. doi: 10.1016/S0140-6736(12)61127-1. [DOI] [PubMed] [Google Scholar]
- 10.World Health Organisation. WHO Surgical Safety Checklist and Implementation Manual. [Last accessed on 2016 Jan 15]. Available from: http://www.who.int/patientsafety/safesurgery/ss_checklist/en/index.html .
- 11.Finch LC, Kim RY, Ttendo S, Kiwanuka JK, Walker IA, Wilson IH, et al. Evaluation of a large-scale donation of Lifebox pulse oximeters to non-physician anaesthetists in Uganda. Anaesthesia. 2014;69:445–51. doi: 10.1111/anae.12632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Funk LM, Weiser TG, Berry WR, Lipsitz SR, Merry AF, Enright AC, et al. Global operating theatre distribution and pulse oximetry supply: An estimation from reported data. Lancet. 2010;376:1055–61. doi: 10.1016/S0140-6736(10)60392-3. [DOI] [PubMed] [Google Scholar]


