The history of HIV/AIDS is quite remarkable. AIDS was first recognized in mid-1981, when unusual clusters of Pneumocystis jirovecii pneumonia and Kaposi's sarcoma were reported in young, previously healthy homosexual men in New York City, Los Angeles, and San Francisco (1,2). In 1983, a retrovirus was isolated from persons with AIDS and associated conditions such as chronic lymphadenopathy (3,4) and by early 1985, serologic tests to detect evidence of infection with HIV had been developed and licensed. However, the first human infections with HIV likely occurred around 1933 in Africa as a result of cross-species transmission (5,6) and the introduction of HIV subtype into the Americas first occurred from Africa into Haiti around 1969 and from there to New York City around 1972 (7). In other words, by 1981 when the first case of AIDS were identified in 1981, HIV had been circulating in the US for a decade. Since then, more than 70 million people have been infected with HIV and about 35 million have died as a result. The World Health Organization (WHO) estimates that at the end of 2015, 36.7 million [34.0–39.8 million] people were living with HIV and an estimated 0.8% of adults aged 15 – 49 years are infected with HIV (8). Women represent a little over half of all adults living with HIV worldwide. The burden of the epidemic varies considerably between regions of the world and within countries. Sub-Saharan Africa accounts for approximately 70% of people living with HIV globally and remains the most severely affected region with an adult HIV prevalence of 4.4% (See Figure 1). In the rest of the world, the HIV prevalence is under 1% except for a few countries in the Caribbean like Haiti and the Bahamas. Even in Sub-Saharan Africa, the burden or the epidemic varies significantly. For example, the adult HIV prevalence in Swaziland, Botswana and Lesotho exceeds 20% while in Somalia and Senegal is around 0.5%. South Africa, with an estimated HIV prevalence of 19.2% is the country with the largest population of people living with HIV with an estimated 7 million persons living with HIV in 2015. However, even in South Africa, the HIV prevalence varies significantly between regions with Kwazulu Natal having an HIV prevalence of close to 40% while the Northern and Eastern Cape have an HIV prevalence of 18% (9).
Figure 1.
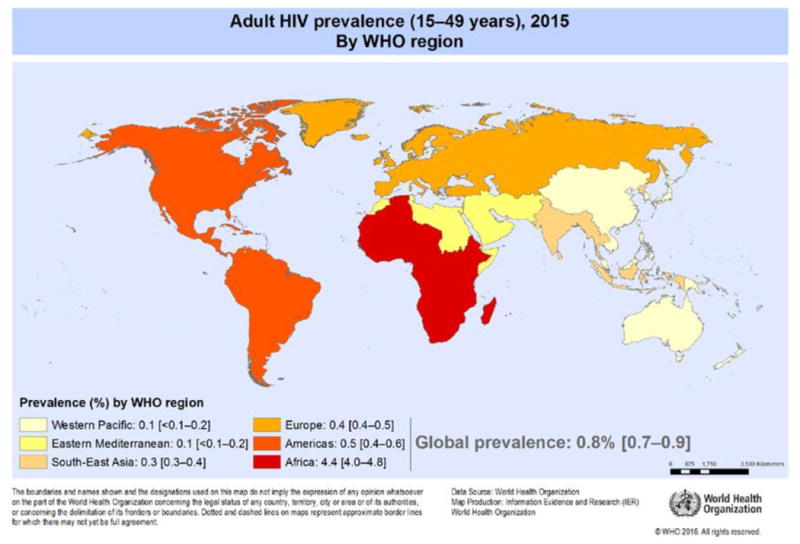
Source: http://www.who.int/gho/hiv/hiv_013.jpg?ua=1. (Accessed on May 7, 2017)
Trends in new infections and mortality over time reflect the impact of prevention and care services. Primarily because of scale up in antiretroviral treatment, mortality from HIV/AIDS has decreased by 45% since its peak in 2005 but still, with 1.1 million people dying of AIDS in 2015 (see Figure 2). However, HIV/AIDS remains the leading cause of death worldwide and the number one cause of death in Sub-Saharan Africa. The reduction in deaths since 2010 has been greater among women than men (33% vs. 15% decrease), reflecting higher treatment coverage for women. There were approximately 2.1 million new infections in 2015, which is a 35% decline in the number of new infections over the past decade however, the number of new infections is now rising in some regions. Because of a steeper decline in mortality than in new infections, the number of people living with HIV continues to raise globally. Besides HIV prevalence, what determines the burden of HIV in a country is the size of its population. India, with an HIV prevalence of only 0.3% but a population of 1.31 billion, has 2.1 million people living with HIV, which is the third largest number of any country behind South Africa and Nigeria.
Figure 2.
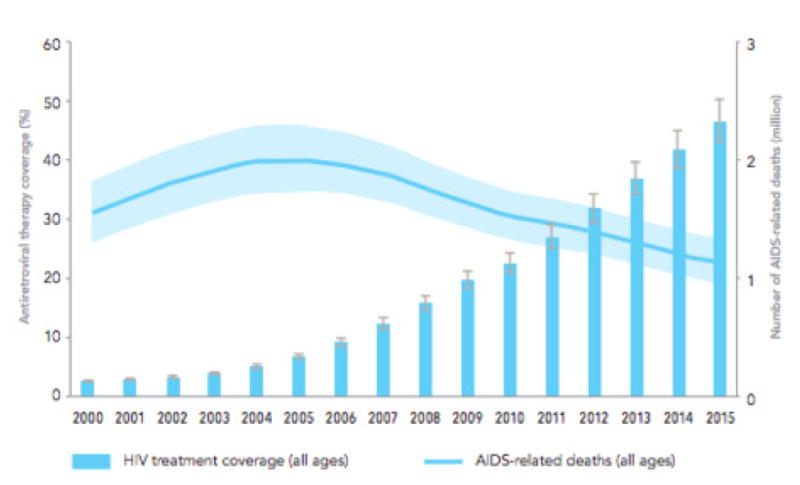
Antiretroviral treatment coverage and AIDS-related deaths, 200 – 2015 (11)
There are 1.8 million children living with HIV globally with the number of new infections among children declining significantly since 2001 largely due to prevention of mother to child transmission. However, new HIV infections are increasing among youth with young people ages 15 – 24 accounting for approximately one third of new infections and, in Sub-Saharan Africa, young women in that same age group account for 25% of new infections.
The unprecedented funding for antiretroviral therapy possible through a variety of initiatives including the Global Fund to Fight AIDS, Tuberculosis and Malaria, the U.S. President's Emergency Program for AIDS Relief (PEPFAR), the William J .Clinton Presidential Foundation and the World Bank's Multi- County HIV/AIDS Program has resulted in rapid scale –up of antiretroviral therapy. As a result the number of people on antiretroviral therapy globally increased from fewer than 400,000 at the end of 2003 (10) to 7.5 million by the end of 2010 and 17 million by the end of 2015 when global coverage of antiretroviral therapy reached 46% of those in need (11). In South Africa, alone 3.4 million people are on antiretroviral therapy, more than any country in the world. In fact, in Durban alone there are more people on antiretroviral therapy than in the entire United States. The antiretroviral treatment scale up has resulted in incidence and mortality declining but the gender gap in treatment coverage continues with 52% of women with HIV on antiretroviral therapy vs. 41% of men and results in men accounting for 58% of adult AIDS deaths globally (11).
The major mode of HIV transmission globally is heterosexual contact. Transmission through injection drug use is now a major driver of new infections in Russia and countries of the former Soviet Union. Transmission through transfusion of blood and blood products has been virtually eliminated in countries that have systematically instituted HIV antibody screening of donated blood and plasma and heat treatment of clotting factors.
Sub-Saharan Africa, home to 12% of the global population, accounts for 71% of the global burden of HIV infections (12). In fact, nine countries in Sub-Saharan Africa (Botswana, Lesotho, Malawi, Mozambique, Namibia, South Africa, Swaziland, Zambia and Zimbabwe) account for 1.6% of all adults but 36% of adults living with HIV in the world (13). Of the estimated 6,000 new infections that occur globally each day, two out of three occur in Sub-Saharan Africa and 74% of global AIDS deaths occur there (12). The major mode of HIV transmission in Sub-Saharan Africa is heterosexual sex and, as a result, women account for 58% of the total number of persons living with HIV there. Despite significant gains in HIV made in Sub-Saharan Africa, adolescent girls account for 80% of new infections among adolescents with 7,000 girls and young women aged 15 – 24 infected each week and having up to eight-fold higher rates of HIV infection compared to their male peers (13). Because of decreases in mother-to-child transmission and improved childhood survival there is a “youth bulge” about to occur in Sub-Saharan Africa. In 2010, 70% of the region was under the age of 30 and, by 2020, it is expected that the youth population will have doubled since the start of the HIV epidemic. At the current infection rate for young women the gains made in incidence and mortality will be rapidly reversed (14). For this reason, PEPFAR launched in 2014 a new initiative called DREAMS (Determined, Resilient, Empowered, AIDS-Free, Mentored, and Safe) to significantly reduce new infections in adolescent girls and young women. Besides treatment, prevention interventions also need to be scaled up. Of these, voluntary medical male circumcision (VMMC) and Pre-Exposure Prophylaxis (PrEP) are some of the most promising as they both have shown to significantly reduce heterosexually acquired HIV (15, 16).
Easter Europe and central Asia are the only regions of the world where HIV infections have continued to rise rapidly with a 57% increase in new infections between 2010 and 2015 (17). The epidemic here is primarily concentrated among persons who inject drugs and poor access to harm reduction combined with low access to antiretroviral therapy have resulted in an increase rather than a decrease in AIDS-related deaths from 38,000 in 2010 to 47,000 in 2015 (11, 18). In the United States the number of new infections decreased by 19% between 2005 and 2014 (19) yet, close to 40,000 new infections occurred in 2015 and, as people with HIV live longer, and new infections continue, the number of people living with HIV in the US now stands at nearly 1.2 million and continues to rise. While new infections have decreased nationally in most groups, rates have increased among men-who-have-sex with men (MSM) and in particular black young MSM. CDC reports a 35% increase in new infections among gay and bisexual men ages 25-34 and a 20% increase among Hispanic/Latino gay and bisexual men. In the United States, the HIV epidemic increasingly affects women, minorities, persons living in the Southeast and the poor. In fact, ten states accounted for two-thirds of HIV diagnoses in 2015 and half of those with HIV now live in the South (20).
HIV infection rates among the general population in Lain America have remained stable at less than 1% but the Caribbean remains an area with some of the highest HIV prevalence rates in the world (21). Increases in antiretroviral treatment coverage have resulted in a decline in mortality and a stable number of new infections between 2010 and 2015 in that region (11). In most countries in Lain America the epidemic is concentrated among key populations with MSM and transgender women having the highest prevalence rates (10.6% and 17.7% respectively) and most new infections occur among MSM (22).
It is impossible to talk about the epidemiology of HIV without talking about the epidemiology of tuberculosis (TB) as these two epidemics are inseparably linked. In Sub-Saharan Africa TB is the most common opportunistic infection and the leading cause of death in HIV-infected adults (23).
In recent years, the result of pivotal studies demonstrating that HIV-infected persons who are on antiretroviral therapy and suppressed do not transmit HIV and thus that “treatment is prevention” (24) have resulted in the United Nations AIDS Program (UNAIDS) “90-90-90” initiative (25). This initiative set ambitious targets to be reached by 2020: 90% of all persons living with HIV will know their status, of these 90% will receive antiretroviral therapy (ART), and 90% of those on therapy will have HIV viral suppression. If these goals are achieved, 73% of all people living with HIV will be virally surpassed and new HIV infections will further decrease and nearly stop. By the end of 2015, UNAIDS estimated that while 17 million people were receiving ART globally, only 57% of people living with HIV knew their HIV status, 46% were receiving ART, and 38% had achieved HIV viral suppression (26). Currently only Sweden has achieved the 90-90-90 goals and Botswana is the only African country close to achieving these goals (27, 28). Clearly much remains to be done to achieve the 90-90-90 goals.
From the perspective of the clinical pathologist a major challenge remains scaling up HIV testing necessary to achieve the “first 90”. It will be necessary to increase HIV testing significantly in order to diagnose the additional 12 million people with HIV infection needed to reach that goal. For that HIV testing will need to move out of healthcare facilities but must be conducted in non-clinical settings in the community as well as in the home. For the “third 90” to be met, viral load testing will need to be implemented in order to make viral load monitoring routine part of care globally. This will not be easy and will require laboratory system strengthening as well as tackling multiple programmatic and funding challenges (29).
Figure 3.
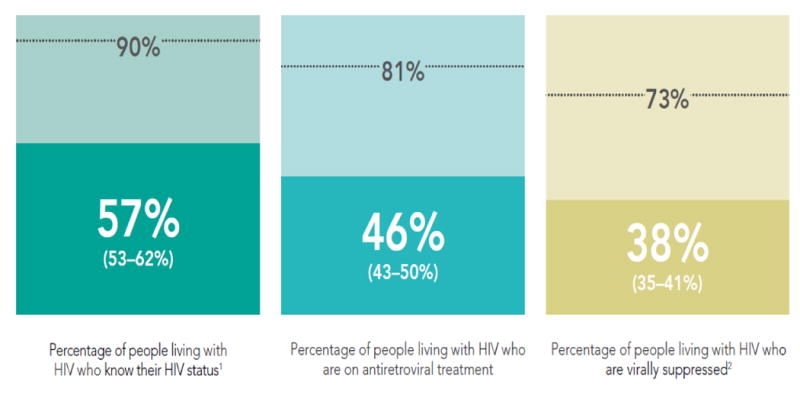
Global HIV treatment cascade, 2015. Adapted from: UNAIDS: 90-90-90 On the right track towards the global target (26)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Centers for Disease Control and Prevention. Pneumocystis pneumonia—Los Angeles. MMWR Morb Mortal Wkly Rep. 1981;30:250–252. [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Kaposi's sarcoma and Pneumocystis pneumonia among homosexual men—New York City and California. MMWR Morb Mortal Wkly Rep. 1981;30:305–308. [PubMed] [Google Scholar]
- 3.Barre-Sinoussi F, Chermann JC, Rey F, et al. Isolation of a T-lymphotropic retrovirus from a patient at risk for acquired immune deficiency syndrome (AIDS) Science. 1983;220:868–871. doi: 10.1126/science.6189183. [DOI] [PubMed] [Google Scholar]
- 4.Gallo RC, Sarin PS, Gelmann EP, et al. Isolation of human T-cell leukemia virus in acquired immune deficiency syndrome (AIDS) Science. 1983;220:865–867. doi: 10.1126/science.6601823. [DOI] [PubMed] [Google Scholar]
- 5.Zhu T, Korber BT, Nahmias AJ, et al. An African HIV-1 sequence from 1959 and implications for the origin of the epidemic. Nature. 1998;391:594–597. doi: 10.1038/35400. [DOI] [PubMed] [Google Scholar]
- 6.Worobey M, Gemmel M, Teuwen DE, et al. Direct evidence of extensive diversity in Kinshasa by 1960. Nature. 2008;455:661–664. doi: 10.1038/nature07390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Worobey M, Watts TD, McKay RA, et al. 1970s and “Patient 0” HIV-1 genomes illuminate early HIV/AIDS history in North America. Nature. 2016 Nov 3;539(7627):98–101. doi: 10.1038/nature19827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.WHO, Global Health Observatory (GHO) Data. [Accessed May 7, 2017]; Available at: http://www.who.int/gho/hiv/en/
- 9.UNAIDS. [Accessed: May 7, 2017];Prevention Gap Report 2016. Available at: http://www.unaids.org/sites/default/files/media_asset/2016-prevention-gap-report_en.pdf.
- 10.UNAIDS. 2004 Report on the Global AIDS epidemic: 4th Global Report. Geneva, Switzerland: [Google Scholar]
- 11.UNAIDS. Global AIDS Update 2016. Geneva, Switzerland: [Google Scholar]
- 12.Kharsany ABM, Karim QA. HIV Infection and AIDS in Sub-Saharan Africa: Current Status, Challenges and Opportunities. The Open AIDS Journal. 2016;10:34–48. doi: 10.2174/1874613601610010034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Williams BG, Gouws E, Somse P, et al. Epidemiological Trends for HIV in Southern Africa: Implications for Reaching the Elimination Targets. Curr HIV/AIDS Rep. 2015;12(2):196–206. doi: 10.1007/s11904-015-0264-x. [DOI] [PubMed] [Google Scholar]
- 14.Fleischman J, Peck K. Addressing HIV Risk in Adolescent Girls and Young Women. [Accessed May 7, 2017];Center for Strategic and International Studies 2015. Available at: https://csis-prod.s3.amazonaws.com/s3fs-public/legacy_files/files/publication/150410_Fleischman_HIVAdolescentGirls_Web.pdf.
- 15.Williams BG, Lloyd-Smith JO, Gouws E, et al. The potential impact of male circumcision on HIV in Sub-Saharan Africa. PLoS Med. 2006;3(7):e262. doi: 10.1371/journal.pmed.0030262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Beaten JM, Donnell D, Ndase P, et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N Engl J Med. 2012;367(5):399–410. doi: 10.1056/NEJMoa1108524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.AVERT, HIV and AIDS in Eastern Europe & Central Asia. [Accessed on May 7, 2017]; Available at: https://www.avert.org/professionals/hiv-around-world/eastern-europe-central-asia.
- 18.DeHovitz J, Uuskala A, El-Bassel N. The HIV epidemic in Eastern Europe and Central Asia. Curr HIV/AIDS Rep. 2014;11(2):168–76. doi: 10.1007/s11904-014-0202-3. [DOI] [PubMed] [Google Scholar]
- 19.CDC. [Accessed May 7, 2017];HIV in the United States: At a Glance. 2016 Dec; Available at: https://www.cdc.gov/hiv/statistics/overview/ataglance.html.
- 20.The Henry J. Kaiser Family Foundation. [Accessed May 7, 2017];The HIV/AIDS Epidemic in the United States: The Basics. Available at: http://kff.org/hivaids/fact-sheet/the-hivaids-epidemic-in-the-united-states-the-basics/
- 21.De Boni R, Veloso VG, Grinsztejn B. Epidemiology of HIV in Latin America and the Caribbean. Curr Opin HIV/AIDS. 2014;9(2):192–8. doi: 10.1097/COH.0000000000000031. [DOI] [PubMed] [Google Scholar]
- 22.Garcia PJ, Bayer A, Carcamo CP. The Changing Face of HIV in Latin America and the Caribbean. Curr HIV/AIDS Rep. 2014;11(2):146–157. doi: 10.1007/s11904-014-0204-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Martinson NA, Hoffmann CJ, Chaisson RE. Epidemiology of Tuberculosis and HIV. Proc Am Thorac Soc. 2011;8(3):288–293. doi: 10.1513/pats.201010-064WR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cohen MS, Chen YQ, McCauley M, Gamble T, et al. Antiretroviral Therapy for the Prevention of HIV-1 Transmission. New Engl J Med. 2016;375:830–839. doi: 10.1056/NEJMoa1600693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.UNAIDS. 90-90-90: An ambitious treatment target to help end the AIDS epidemic. Geneva, Switzerland: 2014. [Accessed May 7, 2017]. Available at: http://www.unaids.org/sites/default/files/media_asset/90-90-90_en.pdf. [Google Scholar]
- 26.UNAIDS. [Accessed on May 7, 2017];90-90-90 On the right track towards the global target. Available at: http://www.unaids.org/en/resources/documents/2017/90-90-90.
- 27.Gisslen M, Svedhem V, Lindborg L, et al. Sweden, the first country to achieve the Joint United Nations Programme on HIV/AIDS (UNAIDS)/World Health Organization (WHO) 90-90-90 continuum of HIV care targets. HIV Med. 2017;18(4):305–307. doi: 10.1111/hiv.12431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Goalathe T, Wirth KE, Holme MP, et al. Botswana's progress towards achieving the 2020 UNAIDS 90-90-90 antiretroviral therapy and virological suppression goals: a population-based survey. Lancet HIV. 2016;3(5):e221–230. doi: 10.1016/S2352-3018(16)00037-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Roberts T, Cohn J, Bonner K, Hargraves S. Scale-up of Routine Viral Load Testing in Resource-Poor Settings: Current and Future Implementation Challenges. Clin Infect Dis. 2016;62(8):1043–48. doi: 10.1093/cid/ciw001. [DOI] [PMC free article] [PubMed] [Google Scholar]


