Abstract
Elevated blood pressure is common in the emergency department, but the relationship between antihypertensive medication adherence and blood pressure in the emergency department is unclear. This cross sectional study tested the hypothesis that higher antihypertensive adherence is associated with lower systolic blood pressure in the emergency department among adults with hypertension who sought emergency department care at an academic hospital from July 2012-April 2013. Biochemical assessment of antihypertensive adherence was performed using a mass spectrometry blood assay, and the primary outcome was average emergency department systolic blood pressure. Analyses were stratified by number of prescribed antihypertensives (<3, ≥3) and adjusted for age, sex, race, insurance, literacy, numeracy, education, body mass index, and co-morbidities. Among 85 patients prescribed ≥3 antihypertensives, mean systolic blood pressure for adherent patients was 134.4 mm Hg (+/− 26.1 mm Hg), and in adjusted analysis was −20.8 mmHg (95% CI −34.2 to −7.4 mm Hg, p=0.003) different from non-adherent patients. Among 176 patients prescribed <3 antihypertensives, mean SBP was 135.5 mm Hg (+/− 20.6 mm Hg) for adherent patients, with no difference by adherence in adjusted analysis (+2.9 mm Hg, 95% CI −4.7 to 10.5 mm Hg, p=0.45). Antihypertensive non-adherence identified by biochemical assessment was common and associated with higher systolic blood pressure in the emergency department among patients who had a primary care provider and health insurance and who were prescribed ≥3 antihypertensives. Biochemical assessment of antihypertensives could help distinguish medication non-adherence from other contributors to elevated blood pressure and identify target populations for intervention.
Keywords: hypertension, medication adherence, blood pressure, emergency service, blood pressure
INTRODUCTION
Hypertension is the most common modifiable risk factor for cardiovascular disease, and treatment lowers the risk of stroke, renal disease, heart failure, cardiac disease, and death.1, 2 Despite the impact that lowering blood pressure (BP) has on clinical outcomes, less than 50% of patients achieve BP <140/90 mm Hg because of complex patient and system factors.3 While a small proportion of patients have resistant hypertension due to secondary causes, medication non-adherence plays a critical role in elevated BP for many patients.4 Medication adherence, or the degree to which patients take medications as prescribed, is influenced by multiple factors. These factors include: number of prescribed medications, dosing frequency, medication side effects, co-morbid medical conditions, and socio-economic conditions, including the ability to pay for medications.5–7 Distinguishing patients with uncontrolled hypertension due to secondary causes from those with medication non-adherence is critical in order to best tailor treatment and interventions for improving health outcomes.
Annually, there are approximately 27 million emergency department (ED) visits related to hypertension.8 In nearly half of all ED visits, the first BP is ≥140/90 mm Hg, regardless of the reason for seeking emergency care.9 Despite the burden of elevated BP and hypertension among ED patients,10, 11 the relationship between antihypertensive medication adherence and BP measured in the ED is unclear. Evaluation of antihypertensive adherence in the ED has previously been limited to patient-report, and other adherence measures such as prescriptions refills, pill counts, and surveys have not been validated in the ED setting.12–14 Accurately identifying antihypertensive adherence and identifying a relationship between elevated BP among patients who seek ED care may provide valuable clinical insight into antihypertensive therapy and identify patients and populations likely to benefit from additional intervention. Therefore the primary objective of this study was to test the hypothesis that higher antihypertensive medication adherence, biochemically assessed by a liquid chromatography mass spectrometry (LC-MS) blood assay, would be associated with lower BP in the ED setting after adjusting for multiple patient demographic and clinical factors.
METHODS
We conducted a prospective, cross-sectional evaluation of a convenience sample of patients with treated hypertension who sought care at the Vanderbilt University Medical Center (VUMC) Adult ED. The Institutional Review Board reviewed and approved the study, and all patients provided written informed consent and were offered $5 for participating.
Study Population and Procedures
Adult patients (≥ 18 years old) who were seen in the VUMC Adult ED from July 1, 2012 to April 25, 2013, were eligible if they had a diagnosis of hypertension recorded in their electronic medical record, were prescribed at least one of 14 common antihypertensive medications detected by the mass spectrometry assay (Table S1, please see http://hyper.ahajournals.org.proxy.library.vanderbilt), and had a VUMC primary care provider. The study enrolled patients with a VUMC primary care provider in order to allow review of medication, clinical, and demographic information from clinic visits, pharmacy notes, and patient summaries in the electronic health record; it also allowed confirmation of the most recent primary care clinic date, and it reduced the risk of potential unmeasured confounders that might have led patients to seek a primary care provider at a tertiary care center.
Patients were excluded if they did not have a peripheral IV or declined a blood draw, were pregnant, were unable to provide consent, had previously been enrolled in this study, sought care in the ED for acute stroke or alcohol withdrawal, or had been in the ED for more than 36 hours. Trained research assistants screened patients who presented to the ED with the above inclusion criteria via the electronic medical record during working hours (20 hours/day during weekdays and 10 hours/day on weekends).
Research assistants enrolled participants, obtained written informed consent, and collected demographic data, clinical information, and medication lists. The number and type of prescribed antihypertensive medications were obtained through a combination of standardized interview questions and review of the electronic medical record. Where there was apparent discrepancy between patient-reported medications and medications listed in the electronic health record, consensus was achieved through additional review of clinic notes, discharge summaries, electronic prescriptions, and clinical communications in the electronic health record, discussion with the patient, and calling outpatient pharmacies. There was no case in which consensus of the medication list among these sources was not achieved. Research assistants obtained blood for the mass spectrometry assay from either an existing peripheral IV, venipuncture, or blood sample (serum) remaining from the clinical encounter. Participants completed the Adherence to Refills and Medications Scale (ARMS) scale (Table S2, please see http://hyper.ahajournals.org.proxy.library.vanderbilt),12 measures of numeracy15 and health literacy.16
Antihypertensive Adherence by Assay
The LC-MS assay is a sensitive and specific biochemical assessment of adherence to multiple cardiovascular medications. Details of the assay’s analytic and clinical validation among patients who received cardiovascular medication under medical supervision has been described previously.17 For the purposes of this study, we considered 14 commonly prescribed medications that are included on the assay when defining antihypertensive adherence: amlodipine, atenolol, carvedilol, clonidine, diltiazem, hydrochlorothiazide, hydralazine, lisinopril, losartan, metoprolol, nifedipine, ramipril, valsartan, and verapamil. For each of these antihypertensives, previously published detection thresholds were used to determine drug presence or absence.17
The ratio of the number of antihypertensives detected in blood to the number of antihypertensives that had been prescribed (of the 14 assay antihypertensives) was used to categorize patients as adherent (ratio = 1.0) or non-adherent (ratio < 1.0). For example, a patient prescribed lisinopril, hydrochlorothiazide, and amlodipine who had all three of these medications detected by the assay was given a ratio of 1 and was classified as adherent. There were no cases in which patients were falsely classified as adherent due to a discrepancy between the prescribed and detected antihypertensive medications (e.g., amlodipine was prescribed but lisinopril was detected).
Blood Pressure in the Emergency Department
In the ED, BP was measured approximately every two hours as part of clinical care using the oscillometric method by clinical care technicians, who recorded the information in the electronic medical record. Clinical care technicians are trained to obtain BP using an appropriately sized BP cuff at the level of the patient’s heart and with the patient seated on a gurney. Up to 10 measures of BP obtained during the course of clinical care were recorded. Each patient also had a single measure of BP using the oscillometric method performed by trained research staff. The research BP measurement was obtained in a standard fashion using the appropriately sized BP cuff at heart height with patients in either seated or semi recumbent position (sitting up on a gurney). The primary outcome was the average ED systolic blood pressure (SBP), which was computed using all clinical BP measures, but excluded the first BP measure (triage BP) and any measures obtained after administration of antihypertensive medications, furosemide, or nitroglycerin via any route.
Covariates
The following covariates were included in multivariable models as potential confounders based on prior causal evidence18–20: age, sex, race (white, non-white), health insurance (commercial; Medicare, Medicaid, or federal; self-pay or unknown), co-morbid conditions measured by the Elixhauser index,21 diagnosis of chronic renal insufficiency listed in the electronic medical record, body mass index (BMI in kg/m2), health literacy (continuous, measured using the Brief Health Literacy Screen22), numeracy (continuous, measured by the Subjective Numeracy Scale15), and years of education (continuous).
Statistical Analyses
Patient demographics and clinical characteristics are reported using means and standard deviation or medians and interquartile ranges for continuous variables and frequencies and proportions for categorical variables. Medication adherence decreases with increasing number of prescribed antihypertensives,7 and three antihypertensives including a thiazide diuretic or equivalent may identify patients with resistant hypertension23; therefore, we evaluated for evidence of interaction between adherence and the number of prescribed medications (<3, ≥3 antihypertensives). Because we found strong evidence for an interaction (interaction P-value <0.001), all analyses were stratified by <3, or 3 or more antihypertensives.
The unadjusted relationship between medication adherence and mean SBP was examined using box plots; Wilcoxon rank-sum tests were performed to examine whether differences were statistically significant. We performed multiple linear regression models to compare mean SBP for patients classified as adherent versus non-adherent, after adjusting for the above covariates. For 18 subjects with missing numeracy, we performed multiple imputations.24 A two sided alpha of 0.05 was used for all analyses.25 By post-hoc calculations, 260 subjects provided 80% power with an alpha of 0.05 to detect a difference in blood pressure by adherence of 14 mm Hg.
Sensitivity Analyses
We examined the sensitivity of these results to the definitions of the outcome and exposure. First, we varied the outcome definition to determine the association of antihypertensive adherence measured by the blood assay with the single SBP obtained by a research assistant. Then, we examined two alternative definitions of medication adherence. The first alternative definition was patient-report of medication adherence via the ARMS, which is 12-item patient-reported measure of global adherence that assesses medication taking and refilling behaviors on a 4-point Likert like scale (Table S2, please see http://hyper.ahajournals.org.proxy.library.vanderbilt).12 The ARMS does not specify a time frame over which the participant is to base his/her responses, nor does it specify type of medications. Consistent with prior work, the minimum ARMS summary score of 12 was used to classify patients as adherent, and >12 was used to define non-adherence.26 To examine which measure of adherence explained a statistically significantly larger proportion of variance in mean SBP, the likelihood ratio was computed comparing a model with both the assay and ARMS to a model with only the ARMS.
The second definition of medication adherence combined both objective and subjective adherence measures, the assay and ARMS, respectively. Each subject was categorized as one of four mutually exclusive levels: (1) adherent by both the assay and ARMS; (2) adherent by the assay only; (3) adherent by the ARMS only; and (4) non-adherent by both. Multiple linear regression was performed using the 4-level adherence variable as the exposure, stratified by the number of prescribed antihypertensives and covariates as described above.
RESULTS
A total of 2,011 patients were screened, and of these 1,538 were excluded for ineligibility and 172 declined to participate (Figure S1, please see http://hyper.ahajournals.org.proxy.library.vanderbilt). Of the 301 subjects enrolled, two were subsequently excluded, one because propranolol was prescribed for headaches and the other because the patient did not have a VUMC primary care provider. Thirty-eight patients were given medication that lowers BP as part of their clinical care immediately following the triage SBP measurement, leaving 261 patients in the primary analyses. There were 176 (67.4%) patients prescribed <3 antihypertensives, and 85 (32.6%) patients prescribed ≥3 antihypertensives (Figure S1, please see http://hyper.ahajournals.org.proxy.library.vanderbilt), of which 78 (91.7%) were prescribed hydrochlorothiazide, amlodipine, or nifedipine.
Population Characteristics
Demographics and clinical characteristics of patients included in the primary analyses are reported in Table 1, stratified by the number of antihypertensive medications that were prescribed, based on medication reconciliation. Overall, mean age was 59.2 years (standard deviation, SD, 11.4 years), 53.3% were female, 63.2% were white, and 19.5% had not completed high school. Thirty-four patients (13.0%) had low health literacy defined as a Brief Health Literacy score ≤ 9, and 127 (52.3%) had low numeracy, defined as a Subjective Numeracy Scale score ≤35. Most patients, 161 (62.7%), reported they had been diagnosed with hypertension for more than 10 years. Comorbidities were common: 37.9% had diabetes, and 24.9% had chronic renal insufficiency. Patients sought ED care for a wide range of symptoms, including 85 (32.6%) with cardiovascular chief complaints of chest pain, shortness of breath, arrhythmia, or palpitations, and nine specifically for hypertension. The most common chief complaints were chest pain, dyspnea, abdominal pain, and generalized weakness; there was no difference in the frequency of these complaints between the two groups (P>0.05 for each chief complaint). No patients sought care for refill of medication.
Table 1.
Demographics and clinical characteristics stratified by number of medications and adherence by assay (N = 261)*
| Prescribed <3 BP Medications | Prescribed ≥3 BP Medications | |||||
|---|---|---|---|---|---|---|
| Patient Characteristics | Adherent (N = 139) | Non-adherent (N = 37) | P-value | Adherent (N = 50) | Non-adherent (N = 35) | P-value |
| Age, mean (sd) years | 58.9 (11.4) | 54.5 (13.1) | 0.05 | 62.5 (9.4) | 61.0 (10.4) | 0.44 |
| median (IQR) | 58 (52, 67) | 54 (47, 64) | 63 (57, 68) | 61 (53, 67) | ||
| Female, no. (%) | 70 (50.4) | 19 (51.4) | 0.92 | 27 (54.0) | 23 (65.7) | 0.28 |
| White, no. (%) | 92 (66.2) | 21 (56.8) | 0.29 | 33 (66.0) | 19 (54.3) | 0.28 |
| Non-Hispanic, no. (%) | 136 (98.6) | 35 (94.6) | 0.61 | 50 (100.0) | 35 (100.0) | – |
| Insurance, no. (%) | 0.64 | 0.28 | ||||
| Private | 59 (42.5) | 14 (37.8) | 17 (34.0) | 16 (45.7) | ||
| Medicare/Medicaid/Federal | 76 (54.7) | 22 (59.5) | 33 (66.0) | 19 (54.3) | ||
| Self-pay, unknown | 4 (2.9) | 1 (2.7) | 0 (0.0) | 0 (0.0) | ||
| Atrial Fibrillation, no. (%) | 16 (11.5) | 2 (5.4) | 0.94 | 5 (10.0) | 6 (17.1) | 0.90 |
| Diabetes, no. (%) | 45 (32.4) | 14 (37.8) | 0.53 | 22 (44.0) | 18 (51.4) | 0.50 |
| Chronic Renal | 33 (23.7) | 10 (27.0) | 0.68 | 15 (30.0) | 7 (20.0) | 0.30 |
| Insufficiency, no. (%) | ||||||
| Elixhauser, mean (sd) | 13.0 (10.6) | 16.2 (13.5) | 0.25 | 15.1 (11.3) | 10.4 (11.4) | 0.05 |
| median (Q1, Q3) | 11 (4, 21) | 15 (5, 22) | 14.5 (5, 22) | 9 (2, 17) | ||
| BMI (kg/meter2), | 0.23 | 0.01 | ||||
| mean (sd) | 31.4 (9.3) | 33.1 (9.6) | 32.6 (9.4) | 36.8 (9.5) | ||
| median (IQR) | 29.5(24.8,35.3) | 31.5(27.3,36.8) | 30.7(25.8,36.8) | 36.7(31.0,41.3) | ||
| Number of medications by patient report, | 0.03 | 0.06 | ||||
| 7.7 (4.9) | 9.7 (5.2) | 10.2 (5.0) | 8.7 (5.5) | |||
| mean (sd) | 7 (4, 10) | 8 (6, 13) | 9.5 (6, 12) | 7 (6, 10) | ||
| median (IQR) | ||||||
| Number of antihypertensives by patient report, | 0.73 | 0.92 | ||||
| 1.6 (1.0) | 1.4 (0.7) | 2.6 (1.1) | 2.6 (1.0) | |||
| 1 (1, 2) | 1 (1, 2) | 3 (2, 3) | 3 (2, 3) | |||
| mean (sd) | ||||||
| median (IQR) | ||||||
| Highest Level of Education | 0.62 | 0.85 | ||||
| mean (sd) years | 12.3 (1.8) | 12.2 (1.7) | 12.4 (1.9) | 12.5 (1.9) | ||
| median (IQR) | 13 (12, 13) | 12 (12, 13) | 13 (12, 14) | 13 (12, 14) | ||
| Health Literacy Level | 0.67 | 0.31 | ||||
| mean (sd) | 13.2 (3.0) | 13.1 (3.0) | 13.2 (2.8) | 13.7 (2.2) | ||
| median (IQR) | 15 (12, 15) | 15 (12, 15) | 15 (13, 15) | 15 (13, 15) | ||
| Numeracy | 0.06 | 0.05 | ||||
| mean (sd) | 32.6 (8.0) | 30.0 (7.4) | 32.2 (8.3) | 29.0 (8.3) | ||
| median (IQR) | 33 (27, 39) | 31.5 (24, 36) | 35 (28, 38) | 31 (22, 34) | ||
| Hypertension >10 years | 77 (55.8) | 19 (51.43) | 0.99 | 42 (84.0) | 25 (71.4) | 0.14 |
| no. (%) | ||||||
P-values by Kruskall-Wallis for continuous variables, by the nonparametric test for trends across groups for categorical variables
Abbreviations: BP, blood pressure; sd, standard deviation; no., number; BMI, body mass index; IQR, interquartile range
Among patients who were confirmed to have been prescribed ≥3 antihypertensive medications, patients commonly underestimated the number of their prescribed antihypertensive medications; the mean patient-reported number of antihypertensive medications was 2.6 (sd 1.0), and of the 85 patients confirmed to be prescribed ≥3 antihypertensive medications, 38 (44.7%) reported they were prescribed fewer than three.
Prescribed Antihypertensives and Assay-Based Medication Adherence
The number of prescribed antihypertensives and number of antihypertensives detected by the blood assay are displayed in Table 2. The mean number of prescribed antihypertensives was 2.1 (SD 1.1 median 2.0, interquartile range, IQR, 1.0, 3.0), and the mean number of antihypertensives detected by the blood assay was 1.8 (SD 1.0; median 2.0, IQR 1.0 to 2.0). There were clinically important differences in adherence among the antihypertensives, with fewer than 80% of patients having detectible medication levels for clonidine, hydrochlorothiazide, nifedipine, and ramipril. Based on blood assay results, 79.0% of patients prescribed <3 antihypertensives were adherent, and 58.8% of patients prescribed ≥3 antihypertensives were adherent as defined by an adherence ratio of 1.0.
Table 2.
Antihypertensive medications, prescribed and detected by mass spectrometry blood assay* (N = 261)
| Medication | Prescribed | Detected | Adherent (95% CI)† |
|---|---|---|---|
| Amlodipine | 71 | 64 | 90.1 (81.0, 95.1) |
| Atenolol | 19 | 17 | 89.5 (68.6, 97.1) |
| Carvedilol | 41 | 40 | 97.6 (87.4, 99.6) |
| Clonidine | 25 | 13 | 52.0 (33.5, 70.0) |
| Diltiazem | 21 | 21 | 100.0 (84.5, 100.0) |
| Hydrochlorothiazide | 74 | 51 | 68.9 (57.7, 78.3) |
| Hydralazine | 18 | 16 | 88.9 (67.2, 96.8) |
| Lisinopril | 115 | 97 | 84.4 (76.6, 89.9) |
| Losartan | 29 | 24 | 82.8 (65.5, 92.4) |
| Metoprolol | 88 | 74 | 84.1 (75.0, 90.3) |
| Nifedipine | 34 | 26 | 76.5 (60.0, 87.6) |
| Ramipril | 6 | 3 | 50.0 (18.8, 81.2) |
| Valsartan | 11 | 9 | 81.8 (52.3, 94.9) |
| Verapamil | 8 | 7 | 87.5 (52.9, 97.8) |
Bold indicates fewer than 80% of patients prescribe the antihypertensive had detectible blood levels
Wilson 95% confidence intervals computed for the proportion of adherence subjects for each antihypertensive
Abbreviation: CI, confidence interval
There were 85 patients who did not report when they last took their blood pressure medications, and five patients reported they had stopped taking their medication more than four days prior because of cost or side effects. Of the remaining 171 patients who reported taking their blood pressure medication within the 96 hours prior to the ED visit, the mean time between ingestion and blood draw was 15.8 (sd 11.4) hours and median time was 12.3 (IQR 7.25, 21.2) hours.
Relationship Between Assay Adherence and Blood Pressure
Mean SBP in the ED was 137.4 mm Hg (SD 23.4 mmHg), and patients had on average 3.2 BPs measured (SD 1.8) over a mean duration of 270 minutes in the ED (SD 120 minutes). Among the 176 patients prescribed <3 antihypertensives, there was no significant difference in mean SBP between adherent and non-adherent patients (135.5 mm Hg versus 132.7 mm Hg, p=0.64; Figure 2). Among the 85 patients prescribed ≥3 antihypertensives, mean SBP was significantly lower for patients classified as adherent compared to non-adherent (134.4 mm Hg vs. 154.2 mm Hg, p=0.0007). Independent associations between covariates and mean ED SBP are reported in Table S3 (please see http://hyper.ahajournals.org.proxy.library.vanderbilt).
Figure 2.
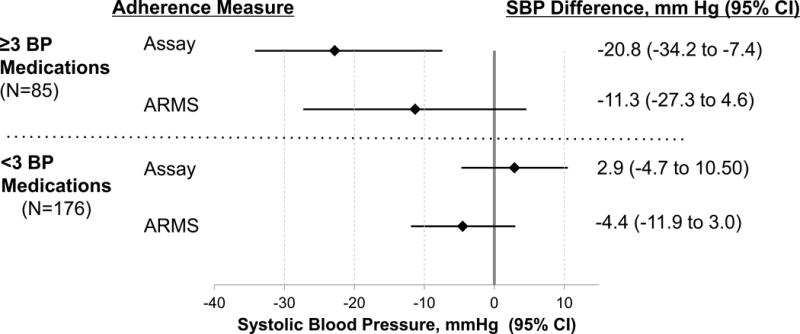
Difference in mean ED SBP for patients classified as adherent vs. non-adherent and stratified by number of prescribed BP medications.* Adherence is shown by both the blood assay and Adherence to Refills and Medications Scale (ARMS).
* The analysis demonstrates results of multivariable linear regression models of the difference in systolic blood pressure between patients who were adherent and non-adherent. All analyses were adjusted for age, pain, sex, race, health insurance, health literacy, numeracy, BMI, chronic renal insufficiency, comorbid conditions, and duration of hypertension diagnosis
Abbreviations: ED, emergency department; BP, blood pressure; BMI, body mass index
Figure 2 illustrates results of the multiple linear regression models between medication adherence measured by the blood assay and SBP, stratified by number of prescribed antihypertensives and adjusted for covariates. Results of analyses using the ARMS as the measure of antihypertensive adherence are included for comparison. Among 176 patients prescribed <3 antihypertensives, mean SBP was no different from patients classified as being non-adherent (+2.9 mm Hg, 95% CI −4.7 to 10.5 mm Hg, p=0.45). Among 85 patients prescribed ≥3 antihypertensives, mean SBP for adherent patients was −20.8 mmHg (95% CI −34.2 to −7.4 mm Hg, p=0.003) different (lower) compared to non-adherent patients.
Sensitivity Analyses
To test the sensitivity of these findings to the outcome definition, we conducted the same analyses using the research SBP measure (N = 297), and found essentially the same results (Table S4 and Figure S2, please see http://hyper.ahajournals.org.proxy.library.vanderbilt). Mean research SBP was 136.7 mm Hg (SD 24.4 mm Hg), or <1 mm Hg lower than mean ED SBP. For patients prescribed <3 antihypertensives, research SBP was −4.3 mm Hg (95% CI −12.6 to 3.9 mm Hg, p=0.30) for adherent vs. non-adherent by the assay. For patients prescribed ≥3 antihypertensives, research SBP was −20.8 mm Hg (95% CI −31.6 to −10.0 mm Hg, p<0.001) for adherent vs. non-adherent by the assay.
When adherence was measured by the ARMS, there was not a detectible relationship between medication adherence and SBP (Table 3, Table S3, Figure S3). By the ARMS, 59 (22.6%) patients reported complete adherence to refilling and medication-taking behaviors. The assay explained more variance in mean SBP than the ARMS (p=0.003), although the 4-level measure of adherence derived from combining the assay and ARMS was also strongly associated with mean SBP in a step-wise fashion among those prescribed more than 3 antihypertensives (Figure 3, Table S5).
Table 3.
Differences in average ED SBP for patients classified as adherent vs. non-adherent by blood assay, ARMS, and 4-level adherence variable, stratified by number of prescribed BP medications*
| Mean ED SBP | Adherent by Assay, mm Hg (95% CI) | Adherent by ARMS, mm Hg (95% CI) | Adherent by Assay and ARMS, mm Hg (95% CI) |
|---|---|---|---|
| Mean ED | 2.9 | −4.4 | −1.3 |
| SBP: <3 BP medications (N = 176) | (−4.7 to 10.5) | (−11.9 to 3.0) | (−11.2 to 8.6) |
| Mean ED | −20.8 | −11.3 | −24.1 |
| SBP: ≥3 BP medications (N = 85) | (−34.2 to −7.4) | (−27.3 to 4.6) | (−54.8 to 8.1) |
Adjusted for: age, sex, race, insurance status, health literacy, numeracy, BMI, chronic renal insufficiency, comorbidity index; multiple imputation performed for missing numeracy
Bold indicates P<0.05
Abbreviations: ED SBP, emergency department systolic blood pressure; ARMS, adherent to refills and medications scale; CI, confidence interval
Figure 3.
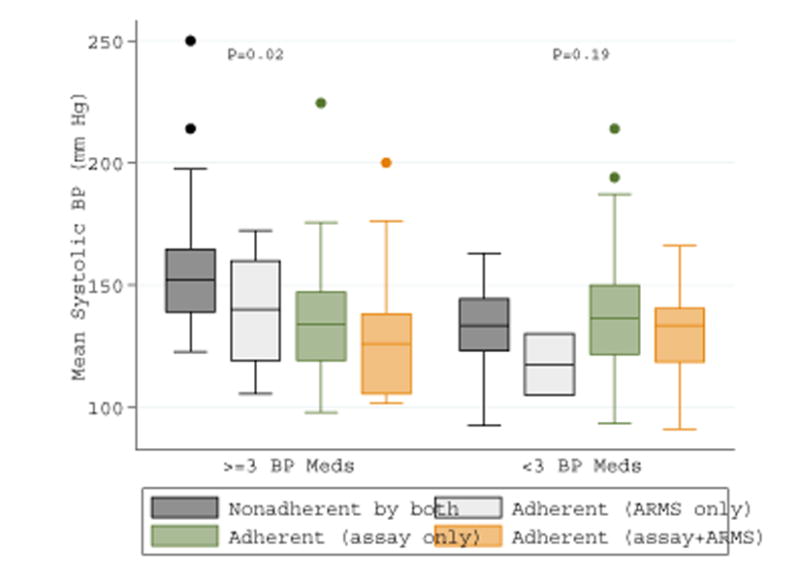
Mean systolic blood pressure by 4-level measure of adherence, stratified by number of prescribed antihypertensive medications
Abbreviations: BP, blood pressure; meds, medications; Adherence to Refills and Medications Scale, ARMS
DISCUSSION
In this cross-sectional study of adults with treated hypertension in the ED, among patients prescribed ≥3 antihypertensives, mean SBP was approximately 20 mm Hg lower for patients found to be adherent by a blood assay than for those determined to be non-adherent. There was, however, no detectible difference in blood pressure by adherence among patients prescribed fewer than three antihypertensive medications. While this is the first study to use a blood assay to measure antihypertensive adherence in an ED setting, patterns of adherence by number and class of prescribed antihypertensive medications and the relationship between adherence and SBP were similar to previous studies conducted in outpatient specialty clinics and among patients with resistant hypertension,27–38 supporting the validity of our findings.
By the LC-MS assay, nearly 28% of patients were non-adherent to prescribed antihypertensive medications despite having a primary care physician and health insurance. Adherence was generally highest for angiotensin II receptor blockers (ARB) and angiotensin-converting enzyme (ACE) inhibitors, followed by calcium channel blockers, diuretics, and beta-blockers, similar to patterns of adherence by antihypertensive classes found in previous work.37–43 In this study, fewer than 80% of patients who were prescribed hydrochlorothiazide, clonidine, ramipril, or nifedipine had detectible blood levels at the time of study enrollment. In post-hoc analyses, patients prescribed HCTZ had 2.7 (95% CI 1.5 to 4.9) greater odds of non-adherence compared to patients who were not prescribed HCTZ after adjusting for age, sex, race, insurance, health literacy, numeracy, and education, which is similar to recent work conducted in hypertension clinics.38 Urinary frequency, orthostatic hypotension, and sexual dysfunction may contribute to the estimated 44.2% non-adherence to hydrochlorothiazide37,38 and oral clonidine’s dosing frequency is an independent risk factor for non-adherence.42 Though adherence to ACE inhibitors is generally better than other antihypertensive classes, 50% adherence to ramipril is similar to adherence measured by a urine assay among patients with resistant hypertension in a clinical trial.44 Though suboptimal, adherence to nifedipine in this study was higher than the 14%–68% range of adherence to calcium channel blockers found in previous studies.39
Therapeutic drug monitoring of medication concentrations in urine and blood as a measure of adherence is becoming more widely available,27–38 and understanding and using results therapeutic drug monitoring is relevant to a wide range of clinicians. Complete non-adherence defined by lack of detection of any prescribed antihypertensive medications ranged from 10% to 54% in studies conducted in specialty clinics or clinical trials.31–38 Among patients who described themselves as adherent, ~33% were completely non-adherent according to therapeutic drug monitoring,32, 35 which is similar to our findings of 32% complete non-adherence among the 202 patients who reported being adherent by the ARMS in the current study. The difference of ~20 mm Hg between adherent and non-adherent patients prescribed ≥3 antihypertensives in the current study is also similar to the 18 mm Hg difference between adherent and non-adherent patients referred to a hypertension specialty clinic.33
The assay provides the most clinical value for patients with elevated BP who report being adherent; in these patients, the assay distinguishes medication non-adherence from medication ineffectiveness (Figure 2). The assay is more closely associated with SBP than the ARMS, possibly because these two measures address different aspects of medication adherence. In preliminary work comparing adherence measured by a urine assay and the 4-item Morisky survey, which is closely related to the ARMS, there was little to no correlation between the two measures of adherence.36 In this study, 27.6% of patients were non-adherent according to the assay, compared to 77.4% of patients who were non-adherent according to the ARMS. This apparent discrepancy reflects differences in the aspects of adherence addressed by an assay versus patient report. The assay is a sensitive measure of adherence over the prior 24–36 hours and is closely tied to SBP, while the ARMS relies on patient report of medication-taking and medication-refilling behaviors of medication in general without a timeframe. Despite their weak relationships to each other, we found that combining information from both the assay and ARMS provided additional information beyond that available only from the assay.
Antihypertensive non-adherence should be explored as a potential cause of consistently or markedly elevated SBP among patients with hypertension in the ED. Hypertension-related ED visits are common and becoming more frequent, with a more than 20% increase between 2006 and 2012.8 Of the more than 136 million ED visits annually in the United States, 27.2% of patients had blood pressure (BP) ≥140/90 mmHg and 16.3% had BP ≥160/100 mm Hg.45 General medication non-adherence is itself associated with ED visits,46, 47 and high BP in the ED often persists after discharge home.48–50 Because uncontrolled blood pressure is rarely symptomatic, and elevated BP is highly prevalent across ED chief complaints,51 we did not restrict enrollment to patients with hypertension-related concerns; overall, 33% of patients reported a chief complaint of chest pain, dyspnea, or hypertension. Patients seeking emergency care for conditions unrelated to hypertension who are found to have markedly elevated blood pressure may gain the most from its identification because they are the least likely to be aware of it. This study was conducted at an academic referral center, but patient characteristics were similar to those found in U.S. academic emergency departments.9 We found patterns and prevalence of non-adherence similar to those of specialty and other outpatient settings, and the relationship with SBP was similar to previous work, suggesting that patterns of non-adherence among patients with hypertension who seek ED care have some characteristics in common with patients in outpatient and specialty clinic settings.
At a minimum, consistently elevated BP during an ED visit should be discussed with patients and integrated into their follow-up plan. Medication non-adherence should routinely be explored with neutral, non-judgmental language that acknowledges the difficulties patients face in managing medications for chronic illness, and post-ED follow up should be emphasized. Brinker et al. noted that among 16 patients from a hypertension who initially reported being adherent and were later provided results of serum tests confirming non-adherence, issues such as difficulty remembering to take medications, debilitating fatigue attributed to medication, and inability to pay for medications were subsequently reported. After non-adherence was identified and addressed, SBP in these patients improved by an average of 46 mm Hg without a change in the number of prescribed antihypertensives.32
Our study has limitations that should be noted. Interpretation of assay results should take into consideration factors that can affect blood concentration, including medication absorption, metabolism, and elimination, time since last dose, concurrent drug ingestion, diet, exercise, infection, and genetics. For example, patients prescribed an antihypertensive with a relatively short half-life but long duration of effect, such as losartan, could miss multiple doses and be classified as non-adherent while still experiencing blood pressure-lowering effect from the medication. Validations studies of the assay did not reveal evidence that processing or storage conditions impact drug detection,17 but these factors may influence assay results for medications such as nifedipine, which decomposes in ultraviolet light. Thresholds for assay detection were set according to published ranges in healthy subjects, and the assay was validated among hospitalized patients who were administered these medications17; despite this, the difference between when patients stop taking medication as prescribed and when they no long experience BP reduction from the medication may in part explain the apparent lack of relationship between adherence and SBP among patients prescribed <3 antihypertensive medications. We did not exclude patients who reported taking non-steroidal anti-inflammatory medications or decongestants prior to arrival; post-hoc analysis excluding these patients did not change point estimates, although with reduced sample size the confidence intervals were wide. Our findings should also be considered in light of use of a convenience sample of patients enrolled at an academic medical center, since these patients may not be reflective of patients with hypertension who seek care in other emergency department settings. Finally, “white coat adherence,” or patients taking medication before going to the emergency department, may have occurred.
PERSPECTIVES
Biochemical assessment of antihypertensive adherence is closely tied to SBP in the ED among patients with hypertension prescribed ≥3 BP medications. Antihypertensive non-adherence should be explored as a potential cause of consistently or markedly elevated SBP in the ED among patients with hypertension.
Supplementary Material
Figure 1.
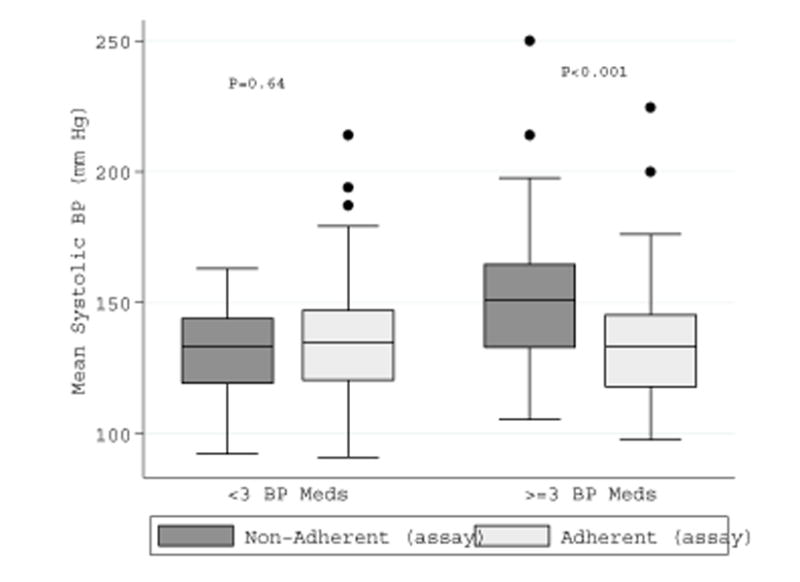
Mean systolic blood pressure by adherence, stratified by number of prescribed antihypertensive medications
Novelty and Significance.
What is new?
Non-adherence to antihypertensive medication measured by a mass spectrometry blood assay was common among emergency department patients, despite having a primary care provider and either health insurance or Medicaid.
Among patients who were prescribed 3 or more antihypertensives, non-adherence was closely tied to mean emergency department SBP.
What is relevant?
Biochemical assessment of medication adherence could help distinguish non-adherence from other causes of elevated blood pressure, particularly among patients who report being adherent to medication.
Summary
Among patients with hypertension who were prescribed ≥3 antihypertensive medications, non-adherence was associated with elevated blood pressure during emergency department visits, after adjusting for multiple demographic and clinical factors.
Acknowledgments
We would like to thank Mr. Lee Smalling, Dr. Carlos M. Ferrario, and the Vanderbilt Center for Effective Health Communication for their important contributions to this study.
SOURCES OF FUNDING
The project was partially supported by CTSA award No. UL1TR000445 and VR3269 as well as K12HL109019 and K23HL125670. Its contents are solely the responsibility of the authors and do not necessarily represent official views of the National Center for Advancing Translational Sciences or the National Institutes of Health.
Footnotes
DISCLOSURES
The authors have no relevant competing interests. A portion of the results were presented the American Heart Association’s High Blood Pressure Research Council meeting on September 14–17, 2015 in Washington D.C.
References
- 1.Writing Group M. Mozaffarian D, Benjamin EJ, Go AS, et al. American Heart Association Statistics C and Stroke Statistics S Executive Summary: Heart Disease and Stroke Statistics-2016 Update: A Report From the American Heart Association. Circulation. 2016;133:447–454. doi: 10.1161/CIR.0000000000000366. [DOI] [PubMed] [Google Scholar]
- 2.Wright JT, Jr, Williamson JD, Whelton PK, et al. A Randomized Trial of Intensive versus Standard Blood-Pressure Control. N Engl J Med. 2015;373:2103–2116. doi: 10.1056/NEJMoa1511939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Peterson AM, Takiya L, Finley R. Meta-analysis of trials of interventions to improve medication adherence. Am J Health Syst Pharm. 2003;60:657–665. doi: 10.1093/ajhp/60.7.657. [DOI] [PubMed] [Google Scholar]
- 4.Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487–497. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- 5.Irvin MR, Shimbo D, Mann DM, Reynolds K, Krousel-Wood M, Limdi NA, Lackland DT, Calhoun DA, Oparil S, Muntner P. Prevalence and correlates of low medication adherence in apparent treatment-resistant hypertension. J Clin Hypertens (Greenwich) 2012;14:694–700. doi: 10.1111/j.1751-7176.2012.00690.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vrijens B, Vincze G, Kristanto P, Urquhart J, Burnier M. Adherence to prescribed antihypertensive drug treatments: longitudinal study of electronically compiled dosing histories. BMJ. 2008;336:1114–1117. doi: 10.1136/bmj.39553.670231.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sutherland JJ, Daly TM, Liu X, Goldstein K, Johnston JA, Ryan TP. Co-prescription trends in a large cohort of subjects predict substantial drug-drug interactions. PLoS One. 2015;10:e0118991. doi: 10.1371/journal.pone.0118991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McNaughton CD, Self WH, Zhu Y, Janke AT, Storrow AB, Levy P. Incidence of Hypertension-Related Emergency Department Visits in the United States, 2006 to 2012. Am J Cardiol. 2015;116:1717–1723. doi: 10.1016/j.amjcard.2015.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Niska R, Bhuiya F, Xu J. National health statistics reports; no 26. Hyattsville, MD: National Center for Health Statistics; 2010. National Hospital Ambulatory Medical Care Survey: 2007 Emergency Department Summary. [PubMed] [Google Scholar]
- 10.Joyner-Grantham J, Mount DL, McCorkle OD, Simmons DR, Ferrario CM, Cline DM. Self-reported influences of hopelessness, health literacy, lifestyle action, and patient inertia on blood pressure control in a hypertensive emergency department population. Am J Med Sci. 2009;338:368–372. doi: 10.1097/MAJ.0b013e3181b473dc. [DOI] [PubMed] [Google Scholar]
- 11.Joyner J, Moore AR, Mount DL, Simmons DR, Ferrario CM, Cline DM. Emergency department patients self-report higher patient inertia, hopelessness, and harmful lifestyle choices than community counterparts. J Clin Hypertens (Greenwich) 2012;14:828–835. doi: 10.1111/jch.12001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kripalani S, Risser J, Gatti ME, Jacobson TA. Development and evaluation of the Adherence to Refills and Medications Scale (ARMS) among low-literacy patients with chronic disease. Value Health. 2009;12:118–123. doi: 10.1111/j.1524-4733.2008.00400.x. [DOI] [PubMed] [Google Scholar]
- 13.Choo PW, Rand CS, Inui TS, Lee ML, Cain E, Cordeiro-Breault M, Canning C, Platt R. Validation of patient reports, automated pharmacy records, and pill counts with electronic monitoring of adherence to antihypertensive therapy. Med Care. 1999;37:846–857. doi: 10.1097/00005650-199909000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Cook CL, Wade WE, Martin BC, Perri M. Concordance among three self-reported measures of medication adherence and pharmacy refill records. J Am Pharm Assoc (2003) 2005;45:151–159. doi: 10.1331/1544345053623573. [DOI] [PubMed] [Google Scholar]
- 15.Fagerlin A, Zikmund-Fisher BJ, Ubel PA, Jankovic A, Derry HA, Smith DM. Measuring numeracy without a math test: development of the Subjective Numeracy Scale. Med Decis Making. 2007;27:672–680. doi: 10.1177/0272989X07304449. [DOI] [PubMed] [Google Scholar]
- 16.Chew LD, Griffin JM, Partin MR, Noorbaloochi S, Grill JP, Snyder A, Bradley KA, Nugent SM, Baines AD, Vanryn M. Validation of screening questions for limited health literacy in a large VA outpatient population. J Gen Intern Med. 2008;23:561–566. doi: 10.1007/s11606-008-0520-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dias E, Hachey B, McNaughton C, Nian H, Yu C, Straka B, Brown NJ, Caprioli RM. An LC-MS assay for the screening of cardiovascular medications in human samples. J Chromatogr B Analyt Technol Biomed Life Sci. 2013;937:44–53. doi: 10.1016/j.jchromb.2013.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gazmararian JA, Kripalani S, Miller MJ, Echt KV, Ren J, Rask K. Factors associated with medication refill adherence in cardiovascular-related diseases: a focus on health literacy. J Gen Intern Med. 2006;21:1215–1221. doi: 10.1111/j.1525-1497.2006.00591.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.George J, Shalansky SJ. Predictors of refill non-adherence in patients with heart failure. Br J Clin Pharmacol. 2007;63:488–493. doi: 10.1111/j.1365-2125.2006.02800.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ho PM, Lambert-Kerzner A, Carey EP, Fahdi IE, Bryson CL, Melnyk SD, Bosworth HB, Radcliff T, Davis R, Mun H, Weaver J, Barnett C, Baron A, Del Giacco EJ. Multifaceted intervention to improve medication adherence and secondary prevention measures after acute coronary syndrome hospital discharge: a randomized clinical trial. JAMA Intern Med. 2014;174:186–193. doi: 10.1001/jamainternmed.2013.12944. [DOI] [PubMed] [Google Scholar]
- 21.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med. 2004;36:588–594. [PubMed] [Google Scholar]
- 23.Calhoun DA, Jones D, Textor S, Goff DC, Murphy TP, Toto RD, White A, Cushman WC, White W, Sica D, Ferdinand K, Giles TD, Falkner B, Carey RM. Resistant hypertension: diagnosis, evaluation, and treatment. A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Hypertension. 2008;51:1403–1419. doi: 10.1161/HYPERTENSIONAHA.108.189141. [DOI] [PubMed] [Google Scholar]
- 24.Azur MJ, Stuart EA, Frangakis C, Leaf PJ. Multiple imputation by chained equations: what is it and how does it work? Int J Methods Psychiatr Res. 2011;20:40–49. doi: 10.1002/mpr.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Savitz DA, Olshan AF. Describing data requires no adjustment for multiple comparisons: a reply from Savitz and Olshan. Am J Epidemiol. 1998;147:813–814. doi: 10.1093/oxfordjournals.aje.a009532. [DOI] [PubMed] [Google Scholar]
- 26.Kripalani S, Goggins K, Nwosu S, Schildcrout J, Mixon AS, McNaughton C, McDougald Scott AM, Wallston KA, Vanderbilt Inpatient Cohort S Medication Nonadherence Before Hospitalization for Acute Cardiac Events. J Health Commun. 2015;20(Suppl 2):34–42. doi: 10.1080/10810730.2015.1080331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Azizi M, Pereira H, Hamdidouche I, et al. Adherence to Antihypertensive Treatment and the Blood Pressure-Lowering Effects of Renal Denervation in the Renal Denervation for Hypertension (DENERHTN) Trial. Circulation. 2016;134:847–857. doi: 10.1161/CIRCULATIONAHA.116.022922. [DOI] [PubMed] [Google Scholar]
- 28.Berra E, Azizi M, Capron A, Hoieggen A, Rabbia F, Kjeldsen SE, Staessen JA, Wallemacq P, Persu A. Evaluation of Adherence Should Become an Integral Part of Assessment of Patients With Apparently Treatment-Resistant Hypertension. Hypertension. 2016;68:297–306. doi: 10.1161/HYPERTENSIONAHA.116.07464. [DOI] [PubMed] [Google Scholar]
- 29.Gupta P, Patel P, Horne R, Buchanan H, Williams B, Tomaszewski M. How to Screen for Non-Adherence to Antihypertensive Therapy. Curr Hypertens Rep. 2016;18:89. doi: 10.1007/s11906-016-0697-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lawson AJ, Shipman KE, George S, Dasgupta I. A Novel ‘Dilute-and-Shoot’ Liquid Chromatography-Tandem Mass Spectrometry Method for the Screening of Antihypertensive Drugs in Urine. J Anal Toxicol. 2016;40:17–27. doi: 10.1093/jat/bkv102. [DOI] [PubMed] [Google Scholar]
- 31.Ewen S, Meyer MR, Cremers B, Laufs U, Helfer AG, Linz D, Kindermann I, Ukena C, Burnier M, Wagenpfeil S, Maurer HH, Bohm M, Mahfoud F. Blood pressure reductions following catheter-based renal denervation are not related to improvements in adherence to antihypertensive drugs measured by urine/plasma toxicological analysis. Clin Res Cardiol. 2015;104:1097–1105. doi: 10.1007/s00392-015-0905-5. [DOI] [PubMed] [Google Scholar]
- 32.Brinker S, Pandey A, Ayers C, Price A, Raheja P, Arbique D, Das SR, Halm EA, Kaplan NM, Vongpatanasin W. Therapeutic drug monitoring facilitates blood pressure control in resistant hypertension. J Am Coll Cardiol. 2014;63:834–835. doi: 10.1016/j.jacc.2013.10.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tomaszewski M, White C, Patel P, Masca N, Damani R, Hepworth J, Samani NJ, Gupta P, Madira W, Stanley A, Williams B. High rates of non-adherence to antihypertensive treatment revealed by high-performance liquid chromatography-tandem mass spectrometry (HP LC-MS/MS) urine analysis. Heart. 2014;100:855–856. doi: 10.1136/heartjnl-2013-305063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jung O, Gechter JL, Wunder C, Paulke A, Bartel C, Geiger H, Toennes SW. Resistant hypertension? Assessment of adherence by toxicological urine analysis. J Hypertens. 2013;31:766–774. doi: 10.1097/HJH.0b013e32835e2286. [DOI] [PubMed] [Google Scholar]
- 35.Ceral J, Habrdova V, Vorisek V, Bima M, Pelouch R, Solar M. Difficult-to-control arterial hypertension or uncooperative patients? The assessment of serum antihypertensive drug levels to differentiate non-responsiveness from non-adherence to recommended therapy. Hypertens Res. 2011;34:87–90. doi: 10.1038/hr.2010.183. [DOI] [PubMed] [Google Scholar]
- 36.Hamdidouche I, Jullien V, Billaud EM, Boutouyrie P, Azizi M, Laurent S. 7b.06: Routine Urinary Detection of Antihypertensive Drugs for Estimation of Adherence to Treatment: A Cross Sectional Study. J Hypertens. 2015;33(Suppl 1):e93. doi: 10.1097/HJH.0000000000001402. [DOI] [PubMed] [Google Scholar]
- 37.Kronish IM, Woodward M, Sergie Z, Ogedegbe G, Falzon L, Mann DM. Meta-analysis: impact of drug class on adherence to antihypertensives. Circulation. 2011;123:1611–1621. doi: 10.1161/CIRCULATIONAHA.110.983874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gupta P, Prashanth P, Branislav S, et al. Risk factors for nonadherence to antihypertensive treatment. Hypertension. 2017;69:1113–1120. doi: 10.1161/HYPERTENSIONAHA.116.08729. [DOI] [PubMed] [Google Scholar]
- 39.Elliott WJ. Improving outcomes in hypertensive patients: focus on adherence and persistence with antihypertensive therapy. J Clin Hypertens (Greenwich) 2009;11:376–382. doi: 10.1111/j.1751-7176.2009.00138.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Elliott WJ, Plauschinat CA, Skrepnek GH, Gause D. Persistence, adherence, and risk of discontinuation associated with commonly prescribed antihypertensive drug monotherapies. J Am Board Fam Med. 2007;20:72–80. doi: 10.3122/jabfm.2007.01.060094. [DOI] [PubMed] [Google Scholar]
- 41.Schroeder K, Fahey T, Ebrahim S. How can we improve adherence to blood pressure-lowering medication in ambulatory care? Systematic review of randomized controlled trials. Arch Intern Med. 2004;164:722–732. doi: 10.1001/archinte.164.7.722. [DOI] [PubMed] [Google Scholar]
- 42.Rizzo JA, Simons WR. Variations in compliance among hypertensive patients by drug class: implications for health care costs. Clin Ther. 1997;19:1446–1457. doi: 10.1016/s0149-2918(97)80018-5. discussion 1424–5. [DOI] [PubMed] [Google Scholar]
- 43.Saini SD, Schoenfeld P, Kaulback K, Dubinsky MC. Effect of medication dosing frequency on adherence in chronic diseases. Am J Manag Care. 2009;15:e22–33. [PubMed] [Google Scholar]
- 44.Azizi M, Menard J, Peyrard S, Lievre M, Marre M, Chatellier G. Assessment of patients’ and physicians’ compliance to an ACE inhibitor treatment based on urinary N-acetyl Ser-Asp-Lys-Pro determination in the Noninsulin-Dependent Diabetes, Hypertension, Microalbuminuria, Proteinuria, Cardiovascular Events, and Ramipril (DIABHYCAR) study. Diabetes Care. 2006;29:1331–1336. doi: 10.2337/dc06-0255. [DOI] [PubMed] [Google Scholar]
- 45.Niska RW. NCHS data brief, no 72. Hyattsville, MD: National Center for Health Statistics; 2011. Blood pressure measurements at emergency department visits by adults: United States, 2007–2008. [PubMed] [Google Scholar]
- 46.Olshaker JS, Barish RA, Naradzay JF, Jerrard DA, Safir E, Campbell L. Prescription noncompliance: contribution to emergency department visits and cost. J Emerg Med. 1999;17:909–912. doi: 10.1016/s0736-4679(99)00109-2. [DOI] [PubMed] [Google Scholar]
- 47.Sokol MC, McGuigan KA, Verbrugge RR, Epstein RS. Impact of medication adherence on hospitalization risk and healthcare cost. Med Care. 2005;43:521–530. doi: 10.1097/01.mlr.0000163641.86870.af. [DOI] [PubMed] [Google Scholar]
- 48.Backer HD, Decker L, Ackerson L. Reproducibility of increased blood pressure during an emergency department or urgent care visit. Ann Emerg Med. 2003;41:507–512. doi: 10.1067/mem.2003.151. [DOI] [PubMed] [Google Scholar]
- 49.Chernow SM, Iserson KV, Criss E. Use of the emergency department for hypertension screening: a prospective study. Ann Emerg Med. 1987;16:180–182. doi: 10.1016/s0196-0644(87)80012-4. [DOI] [PubMed] [Google Scholar]
- 50.Shiber-Ofer S, Shohat Z, Grossman A. Elevated Diastolic, But Not Systolic, Blood Pressure Measured in the Emergency Department Predicts Future Development of Hypertension in Normotensive Individuals. J Clin Hypertens (Greenwich) 2015;17:359–363. doi: 10.1111/jch.12513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Karras DJ, Ufberg JW, Heilpern KL, Cienki JJ, Chiang WK, Wald MM, Harrigan RA, Wald DA, Shayne P, Gaughan J, Kruus LK. Elevated blood pressure in urban emergency department patients. Acad Emerg Med. 2005;12:835–843. doi: 10.1197/j.aem.2005.04.015. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


