Abstract
Recent increases in hurricanes led to a need to evaluate access to medical care, medical needs, and personal and community impact on vulnerable populations, particularly elderly, low income, and minority communities. This article examines access to care, interruptions in medical services, personal impact from Hurricane Sandy, and agreement with ecological statements related to storms, flooding and damages in Hispanic/Latino patients receiving health care at Federally Qualified Health Centers in New Jersey. Only 10 % of 335 Hispanic interviewees were U.S. born. Self-identified personal impact was a better indicator of effects from Sandy, health center use, and medical issues, than was a community impact rating. Respondents who gave a high personal impact rating were more likely to have evacuated, had longer power outage, were more likely to need medical care, had more trouble getting to centers, and had more medical interruptions during Sandy. A higher percentage of respondents who evacuated, needed the center, had trouble getting there, and had more “medical need” than those who did not evacuate. The greatest impacts were on respondents who were told to evacuate before the storm, but did not (46 % had “medical need”). The respondents had high agreement ratings for “storms are due to climate change”, followed by “frequent and stronger storms will come more often”, “flooding is due to sea level rise”, and “changing climate is due mainly to human activity and not natural causes”. These ratings will aid public policy makers and planners in developing resiliency strategies for vulnerable coastal communities.
Introduction
Public health and ecosystems management require planning, research, and public involvement in decision-making. Optimally, research should include science and social-science based studies, including the perceptions and concerns of people. While a great deal of attention has been devoted to examining health risks and risk perception of people living near “Superfund” sites (the National Priorities List established under the Comprehensive Environmental Responsibility, Compensation, and Liability Act, CERCLA), chemical plants, and nuclear facilities, only recently have studies examined health risks, perceptions and concerns during disaster events. Examining health risks, increasing incidences of diseases and accidents, access to medical services, and perceptions and concerns during and following a disaster came to the forefront during Hurricane Katrina (Trumbo et al., 2011; Sastry and Gregory, 2013), and several devastating storms thereafter (Bergan et al., 2015; O’Neill and van Abs, 2016).
In late October 2012, Hurricane Sandy hit the Northeastern United States, and stalled over the state of New York and New Jersey for several days. It produced record setting storm surges and flooding. Sandy was one of the largest storms on record, had a diameter twice the size of Hurricane Katrina (Abramson et al., 2015), and overall, affected 60 million people in 24 states (Neria and Shultz, 2012). In New Jersey, there were over 345,000 housing units destroyed, over $70 billion in damages, $3 billion in damages to NJ transit roads and bridges, and many people were displaced from homes due to storm surges, flooding, and loss of power (BBB, 2012; Freedman, 2013; Burger and Gochfeld, 2014a,b). Three years later, some people were still displaced, and others had abandoned their homes along the shore.
Damages and injuries following hurricanes often derive from flooding, loss of electricity, and loss or destruction of infrastructures and health care facilities. Similarly, severe storms and hurricanes can destroy coastal dunes and salt marsh ecosystems (Houser et al., 2008; USGS, 2010, 2013; Hsu, 2013). Serious health conditions, emotional distress, and grief follow such disasters and post-disaster needs assessments are critical for recovery and understanding post-disaster mental health (Kessler et al., 2008; North et al., 2012; Swerdel et al., 2016). Minority, low-income, and older people are more vulnerable to serious impacts than others (Elder et al., 2007; Behr and Diaz, 2013; Price et al., 2013).
In this paper access to medical care, medical need, medical interruptions, and experiences were examined in a Hispanic/Latino population in New Jersey with respect to demographics, personal impact rating (self-identified), and community impact rating (after Halpin, 2013). One objective was to determine if respondents’ self-rating of impact correlated with the adverse effects they suffered from Sandy, including access to care and medical services. In other words, can respondents accurately evaluate their adverse impacts from a disaster such as Sandy, or are community evaluations a better measure of individual effects. Additionally, respondents’ perceptions of the relationships between increasing storm frequency, climate change, sea level rise, shore damage, and loss of salt marshes and dunes were explored. The ecological statements were ones that most scientists accept as fact (e.g. global warming is occurring, and humans play a major contributory role in global warming [IPCC, 2007, 2014], and dunes and salt marshes protect coastal areas from flooding and damage [Psuty and O’Fiara, 2002, Pries et al., 2008; Plant et al., 2010]).
Patients using Federally Qualified Health Centers in New Jersey were interviewed because the centers generally serve the uninsured and underinsured, with low economic status, populations that are often invisible in such studies. Understanding health care risks during disasters is a first step toward improving health care for vulnerable populations, and understanding their perceptions of the relationship between ecological barriers to coastal storm damage is essential to gaining support for improving these soft infrastructures. The Hispanic/Latino population has experienced unprecedented growth in the past few decades in the U.S. (Pew Hispanic Center, 2006; Dawson, 2012), especially in New Jersey (Greenberg, 2005). In 2000, Hispanic/Latinos accounted for 13.3 % of New Jersey’s population, and in 2015, they accounted for 19.7 % (US. Census Bureau, 2002, 2017), and this proportion is expected to increase. Hispanic/Latinos made up 56 % of the patients interviewed at the seven participating Community Health Centers.
Methods
Patients were interviewed at 7 Federally Qualified Health Centers clinics, including some located along the Jersey shore that were greatly impacted by storm surge, flooding, evacuations and damage from Hurricane Sandy. The Centers chosen for interviews were: 1). Eric B. Chandler Health Center in New Brunswick, Middlesex County, 2). CHEMED in Lakewood, Ocean County, 3). Horizon Health Center in Jersey City, Hudson County, 4). Monmouth Family Health Center in Long Branch, Monmouth County, 5). Neighborhood Health Center in Plainfield, 6). Neighborhood Health Center in Elizabeth (5 and 6 in Union County), and 7). Ocean Health Initiatives in Toms River, Ocean County.
Interviews were conducted in 2014–2015 by the authors and well-trained interviewers with prior experience, half of whom had Spanish as a first language. The questionnaire used for interviews was partly based on previous questionnaires (Burger and Gochfeld, 2014a,b; Burger, 2015), but was modified for the health centers. Pilot interviews were conducted to test the format, the appropriateness of questions, and to increase reliability among interviewers, and some questions were modified as a result of the pilot study. The questionnaire contained several sections: demographics, concerns, evacuation, Sandy impacts, normal center use, transportation to the center, medical conditions, access to centers, interruption of care or medications, and agreement ratings for ecological questions. Respondents evaluated their personal impact on a scale of 0 (no effect) to 5 (large effects). Ecological statements were framed “Some experts say….” “stronger storms are due to climate change”, “storms will come more often”, “flooding is due to sea level rise”, “changing climate is due to human activity”, and “damage from Sandy was due to loss of dunes or salt marshes”. Respondents rated the ecological statements on a scale of 1 (strongly disagree) to 5 (strongly agree). Ethnic and racial status was by self-identification and this paper includes only those who identified as Hispanic or Latino.
When patients arrived at centers, they either went to a general waiting room or to a department-specific waiting room. Interviewers were present in both locations, approached respondents in the order they came into waiting rooms, identified themselves from Rutgers University, asked permission to interview them, and informed them that it was entirely voluntary, that no individual identifiers would be recorded, and that information would be available on a web site or they could contact the investigators or the Rutgers Institutional Review Board. Once they consented, interviews were conducted in a secluded place or alcove. The refusal rate was less than 15 %, and mostly reflected lack of time, presence of children or elderly charges, and about half of the interruptions were due to being called for their appointments. Incomplete interviews that progressed beyond demographics, were included in analysis, when the data were relevant. Although most interviews required only 15–20 minutes, many were longer when patients wanted to talk about their experiences or their frustration with lack of state or federal government response to their plight (lack of loans and grants for re-building).
Interviewees were asked about their need for medical services, and interruption of medical services and medications during and after Sandy. The investigators used these responses and answers to several of the open-ended questions to compute a “medical need” composite score based on whether a patient needed medicines, medical services, drug refills, or needed to get to a doctor, to the center, to an emergency room, or a pharmacy. Adverse health consequences with a high “medical need” score, included diabetes, kidney disease or dialysis, heart arrhythmia, asthma, blood clots, cancer, infections, and needing oxygen, among others.
After the study was initiated, Halpin (2013) reported on several measures of community impact of Hurricane Sandy on 553 of New Jersey’s 565 towns. This allowed placement of the study population within a state context. Six of the seven participating clinics were in the five worst hit counties (Halpin, 2013). Thus, for analysis, the 7 facilities were ranked based on Halpin’s (2013) community ratings: 1) hardest hit impact, 2) community hardship rank, and 3) household hardship rank. From this, the seven centers were divided into “very high impact”, “high impact”, or “medium impact”.
The data from the present study were thus examined as a function of two measures: self-assessment of personal impact, and Halpin’s community impact rating (Halpin, 2013). Analyses included calculating frequencies and percentages, means and standard deviations, Kruskal-Wallis One Way Analysis of Variance (ANOVA) analysis, and 95 % confidence intervals (SAS, 2005).
RESULTS
Demographics, General Effects and Health Care
The Hispanic/Latino population interviewed was 68 % female, with a mean (± standard error) age of 40 ± 0.7 years. Only 9.7 % were U.S born; 83 % listed Spanish as their primary language. The foreign-born respondents had been in the U.S. for an average of 15.6 ± 0.6 years. Most Hispanic/Latinos interviewed lived in apartments (60 %), compared to Blacks (48 %) and Whites (41 %; X2 = 14.8, P < 0.0006).
Only 17 % evacuated their homes before, during, or after Sandy (compared to 12 % of Blacks and 21 % of Whites, not significant). Of those Hispanic/Latinos who evacuated, they were evacuated for an average of 22 ± 6 days. Three years after Sandy, 10 % of those who evacuated were still not able to return to their Sandy-damaged homes. Their self-rating of personal impact averaged 3.4 ± 0.1 (out of 5). Respondents had previously used the centers an average of 7.3 ± 0.8 years (prior to the interview). About 12 % responded that they needed the center during Sandy or immediately after (compared to 14 % for Blacks and 4 % for Whites, X2 = 7.8, P < 0.02)). 9 % of Hispanic/Latinos had trouble getting to the center when they needed it. However, the investigators determined that 19.4 % actually needed medical services (= medical need) based on several different indicators of need (based on medical condition and interrupted access to doctors, clinics, emergency rooms, pharmacies or medications). “Medical need” was similar for Hispanic/Latinos and Blacks (both 19 %), but was higher than for Whites (14 %, although not significant).
Health Care as a Function of Impact
There were two measures of impact in this study: self-evaluation of personal impact, and a composite community impact (derived from Halpin, 2013). The self-rating of impact for Hispanic/Latinos was 3.4 ± 0.1, compared to 3.1 ± 0.1 for Blacks and 3.0 + 0.1 for Whites (X2 = 8.6, P < 0.01). There were few demographic differences in the Hispanic/Latinos responses as a function of personal impact rating (except for U.S born). However, there were significant differences in effects due to Sandy, transportation, and medical issues as a function of personal impact rating (Table 1). As personal impact rating increased, so did the percent that evacuated, the days evacuated, and the percent still not back in their houses, as well as the percent needing the centers during Sandy, the percent having trouble getting there, and all measures of medical need. Respondents who rated their personal impact low did not need the centers during Sandy, and did not feel they had interruption of any medical services or medicines. However, when the investigators examined a complex of indicators of “medical need”, 7 % of those with low personal impact did need the centers (compared to 27 % for the respondents who rated their personal impact ‘high’, Table 1).
Table 1.
Demographics and other characteristics for Hispanic/Latino population by Hurricane Sandy personal impact rating (0–1=Low, 2–3=Medium, 4–5=High).
| Characteristic | Low | Medium | High | X2 (p) |
|---|---|---|---|---|
|
| ||||
| Number interviewed | 28 | 142 | 153 | |
|
| ||||
| Demographics | ||||
|
| ||||
| % Female | 60.7% | 64.8% | 73.2% | NS |
|
| ||||
| Mean Age | 37.6 ± 1.8 | 39.8 ± 1.0 | 41.2 ± 1.0 | NS |
|
| ||||
| US born | 11.1% | 14.9% | 6.0% | 6.3 (0.04) |
|
| ||||
| Years in USa | 13.0 ± 1.7 | 16.1 ± 0.9 | 16.0 ± 0.9 | NS |
|
| ||||
| Sandy effects | ||||
|
| ||||
| % told to evacuate | 7.7% | 8.7% | 23.5% | 13.2 (0.001) |
|
| ||||
| % evacuated | 11.5% | 8.7% | 25.5% | 14.9 (0.0006) |
|
| ||||
| Days evacuatedb range | 2.3 ± 0.9 1–4 | 14 ± 4.8 1–60 | 26.9 ± 9.0 2–190 | 5.6 (0.06) |
|
| ||||
| % still out of housec | 0.0% | 0.0% | 15.2% | NS |
|
| ||||
| Days no power | 5.3 ± 1.0 | 8.4 ± 0.6 | 11.4 ± 1.5 | 15.7 (0.0004) |
|
| ||||
| Center Use | ||||
|
| ||||
| How long going to center? (years) | 5.5 ± 1.1 | 6.3 ± 0.6 | 7.3 ± 0.6 | NS |
|
| ||||
| % used this center before Sandy? | 44.4% | 62.0% | 60.5% | NS |
|
| ||||
| Center visits/yr (95th percentile) | 6.2 ± 1.3 (19) | 5.4 ± 0.4 (12) | 7.4 ± 0.8 (26) | NS |
|
| ||||
| How do you get to center? d | 14.9 (0.06) | |||
| Car | 50.0% | 46.5% | 38.5% | |
| Walk | 14.3% | 33.1% | 26.4% | |
| Taxi | 17.9% | 9.9% | 23.6% | |
| Bus | 17.9% | 11.3% | 15.5% | |
| Other | 0.0% | 1.4% | 0.7% | |
|
| ||||
| Medical issues | ||||
| % had trouble getting to Center | 3.6% | 5.9% | 13.2% | 5.6 (0.06) |
|
| ||||
| % needed Center during Sandy? | 0.0% | 7.9% | 17.0% | 9.5 (0.009) |
|
| ||||
| % with any medical interruption in medical services or medication due to Sandy | 0.0% | 5.0% | 14.1% | 10.5 (0.005) |
|
| ||||
| % with any "medical need" during or immediately after Sandy | 7.1% | 14.8% | 26.8% | 9.8 (0.008) |
. If not born in the United States.
. If the person had to evacuate and were able to return home.
. If the person had to evacuate and had not returned home at the time of the survey in 2015.
. People can take more than one method.
In contrast, there were differences in demographics as a function of the community impact ratings for Hispanic/Latinos (after Halpin, 2013). There were significantly more females in the very high community impact group than in the others, and a greater percentage of those were U.S. born, compared to the low community impact group (Table 2). Surprisingly, the personal impact rating varied significantly by community impact, but it was not linear (the lowest mean personal impact was given by respondents in the high community impact group, and not the medium or very high group). Other endpoints also showed significant differences that were not linear (e.g. percent evacuated, days without power), which reflects that community impact rating does not necessarily reflect self-identified personal impact for the vulnerable population within the county. There were no significant differences in the percent that needed the center, or had trouble getting to centers as a function of community impact, while interruption of medical services and “medical need” did differ (Table 2). Medical need was highest in the high, but not the very high, community impact group.
Table 2.
Demographics and other characteristics for Hispanic/Latino population for interviews at federally qualified health centers in New Jersey by home impact. The home impact ratings of medium, high, and very high are a composite we developed from impact ratings given by Halpin (2013).
| Characteristic | Medium | High | Very High | X2 (p) |
|---|---|---|---|---|
|
| ||||
| Number interviewed | 185 | 64 | 91 | |
|
| ||||
| Demographics | ||||
|
| ||||
| % Female | 65.4% | 60.9% | 78.0% | 6.2 (0.04) |
|
| ||||
| Mean Age | 41.4 ± 0.9 | 38.2 ± 1.4 | 39.5 ± 1.2 | NS |
|
| ||||
| US born | 4.9% | 11.7% | 18.7% | 13.3 (0.001) |
|
| ||||
| Years in USa | 15.4 ± 0.7 | 14.8 ± 1.3 | 16.7 ± 1.2 | NS |
|
| ||||
| Sandy effects | ||||
|
| ||||
| % told to evacuate | 11.1% | 26.8% | 16.9% | 8.2 (0.02) |
|
| ||||
| % evacuated | 12.2% | 32.1% | 15.7% | 12.1 (0.002) |
|
| ||||
| Days evacuatedb range | 16.0 ± 3.4 3–60 | 20.3 ± 13.5 1–180 | 29.2 ± 13.8 2–190 | 5.3 (0.07) |
|
| ||||
| % still out of housec | 15.8% | 7.1% | 6.7% | NS |
|
| ||||
| Days no power | 9.9 ± 0.6 | 13.9 ± 3.9 | 6.6 ± 0.6 | 24.0 (<0.0001) |
|
| ||||
| Rating of Sandy impact on patientd | 3.6 ± 0.1 | 3.0 ± 0.2 | 3.3 ± 0.1 | 7.0 (0.03) |
|
| ||||
| Center Use | ||||
|
| ||||
| How long going to center? | 7.1 ± 0.5 | 6.1 ± 0.8 | 6.1 ± 0.8 | 5.1 (0.08) |
|
| ||||
| % used this center before Sandy? | 67.4% | 45.0% | 54.7% | 5.0 (0.08) |
|
| ||||
| Center visits/yr (95th percentile) | 7.4 ± 0.7 (24) | 6.5 ± 0.8 (12) | 4.5 ± 0.5 (12) | 14.5 (0.0007) |
|
| ||||
| How do you get to center? e | 52.4 (<0.0001) | |||
| Car | 42.0% | 53.6% | 38.5% | |
| Walk | 27.3% | 28.6% | 29.7% | |
| Taxi | 27.3% | 8.9% | 2.2% | |
| Bus | 6.8% | 12.5% | 28.6% | |
| Other | 0.6% | 1.8% | 1.1% | |
|
| ||||
| Medical Issues | . | |||
|
| ||||
| % had trouble getting to Center | 11.5% | 3.6% | 7.8% | NS |
|
| ||||
| % needed Center during Sandy? | 13.1% | 12.1% | 9.9% | NS |
|
| ||||
| % with any medical interruption in medical services or medication due to Sandy | 11.8% | 10.5% | 3.3% | 4.9 (0.08) |
|
| ||||
| % with any "medical need" during or immediately after Sandy | 18.4% | 29.7% | 13.2% | 6.8 (0.03) |
. If not born in the United States.
. If the person had to evacuate and were able to return home.
. If the person had to evacuate and had not returned home at the time of the survey in 2015.
. On a scale of 0 (no impact) to 5 (severely).
. People can take more than one method.
For several days before the hurricane, there were directives from the Governor to evacuate coastal communities. Evacuation would remove people from injury and might allow better access to health care. However, many people who chose to shelter in place had to evacuate during or after the storm. While tables 1 and 2 provide the percent that were told to evacuate, as well as some key effects variables, they do not indicate the effects for those who evacuated or not. Those who evacuated suffered significantly more days without power, gave a higher personal effects rating, had more trouble getting to centers, needed the centers more, had more interruptions of medical services, and had more “medical need” than those who did not evacuate (Table 3). The group that was effected most strongly, however, was the group that was told to evacuate, and did not (Table 4). Fully 46 % of those who ignored the evacuation order, had “medical needs” during or immediately following Sandy. There were no gender differences in evacuation rates.
Table 3.
Ratings of Hispanic respondents as a function of evacuated verses non-evacuated. Personal impact rating on a scale of 0=No effect to 5=Very High. Sample sizes differ because only half the respondents were asked to rate the ecological statements.
| Evacuated | Non- evacuated |
χ2 (p) | |
|---|---|---|---|
|
| |||
| Sample Size | 53 | 260 | |
|
| |||
| Days no power | 16.6 ± 4.2 | 8.2 ± 0.3 | 6.1 (0.01) |
|
| |||
| Rating of Sandy impact on patient | 3.9 ± 0.2 | 3.3 ± 0.1 | 13.5 (0.0002) |
|
| |||
| % had trouble getting to Center | 14.3% | 8.0% | NS |
|
| |||
| % needed Center during Sandy? | 20.8% | 10.2% | 4.6 (0.03) |
|
| |||
| % with any medical interruption in medical services or medication due to Sandy | 11.8% | 8.4% | NS |
|
| |||
| % with any "medical need" during or immediately after Sandy | 32.1% | 18.2% | 5.2 (0.02) |
|
| |||
| Sample Size | 23 | 169 | |
|
| |||
| Storms due to climate change | 4.6 ± 0.1 | 4.4 ± 0.1 | NS |
| Storms will come more often | 4.4 ± 0.2 | 4.0 ± 0.1 | 3.5 (0.06) |
| Flooding due to sea level rise | 4.0 ± 0.2 | 4.0 ± 0.1 | NS |
| Changing climate due to human activity | 4.2 ± 0.3 | 3.9 ± 0.1 | NS |
| Sandy damage due to loss of sand dunes | 3.4 ± 0.2 | 3.2 ± 0.1 | NS |
| Sandy damage due to loss of salt marshes | 3.6 ± 0.2 | 3.2 ± 0.1 | 3.9 (0.05) |
Table 4.
Relationship between being advised (or not) to evacuate and the percent that did, their personal impact, and their percent medical need. Personal impact rating on a scale of 0=No effect to 5=Very High.
| Told to Evacuate |
Not Told | χ2 (p) | |
|---|---|---|---|
| Sample Size | 49 | 268 | |
| Percent Evacuated | 77.6% | 5.6% | |
| Rating of Sandy impact on patient | 4.0 ± 0.2 | 3.9 ± 0.3 | NS |
| % with any "medical need" during or immediately after Sandy | 36.8% | 20.0% | NS |
| Percent Not Evacuated | 22.4% | 94.4% | |
| Rating of Sandy impact on patient | 4.1 ± 0.3 | 3.3 ± 0.1 | 4.4 (0.04) |
| % with any "medical need" during or immediately after Sandya | 45.5% | 17.0% | 5.7 (0.02) |
. Composite need determined by investigators from five variables.
For the total population interviewed (Hispanics, Whites, Blacks), Hispanics were more likely to walk to the centers (28 %), than other ethnic groups (14 % for Blacks and 9 % for Whites; X2 = 23.7, P < 0.001). This suggests that more Hispanics had less access to a car than others, and they would have less opportunity to evacuate, putting them more at risk for health problems.
Rating of Environmental Issues: Climate Change, Sea Level Rise and Damages
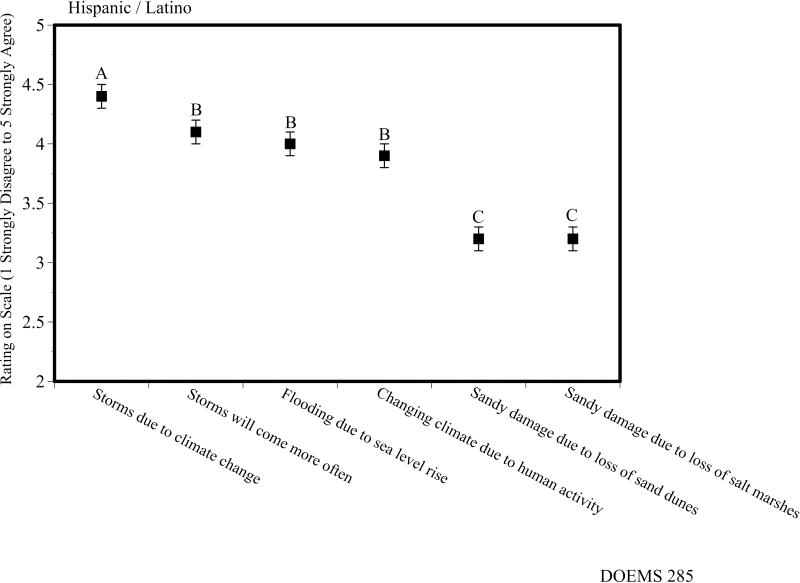
Of the ecological statements, respondents agreed most strongly with “more frequent and severe storms are due to climate change”, followed by “storms will occur more often”, “flooding is due to sea level rise”, and “changing climate is due mainly to human activity rather than natural causes” (Fig. 1). Their rating for the damages being due to loss of dunes or salt marshes were significantly lower. The perceptions about these ecological statements were rather tight, with little variation (Fig. 1), and there were no differences with respect to personal impact or community impact ratings. However respondents who did not evacuate rated 2 of the 6 environmental statements lower than did those who evacuated (Table 3).
Figure 1.
Agreement of Hispanics interviewed at Federally Qualified Health Centers in New Jersey with ecological statements accepted as true by experts. 1 = strongly disagree to 5 = strongly agree. Given are means ± standard errors. All statements started with “Experts agree that…”
DISCUSSION
Impact Measures, Impacts, and Evacuation
One of the objectives of this study was to examine whether personal-identification of impact, or a community impact measure best indicated the evacuation behavior, center use, and medical issues of Hispanic/Latinos affected by Hurricane Sandy. Personal impact rating was a better measure of effects from Sandy and medical issues than was the community impact rating. There are several possible explanations: 1) people who evacuated and never returned to the area were not surveyed, and they would have been the most impacted, 2) community rating includes the whole county and not smaller units, neighborhoods or individual blocks, which could have been very highly impacted, and 3) respondents who gave a personal rating were integrating a range of issues, including whether they had children or elders they were responsible for, whether anyone in their family needed medicines or doctors, whether they could walk to the centers, whether their first floor was flooded, whether they had mold or not, and whether they received government money to aid in their recovery, among other factors.
All the measures of medical need differed significantly as a function of self-rating of personal impact from Sandy, again indicating that individuals correctly evaluated their overall impact. In contrast, there were often significant differences among the medical need variables as a function of community rating, but they were not directional. That is, the group with a community rating of very high did not always have the highest percent with effects from Sandy or medical issues (refer to Table 2). This indicates that as well as considering community impact assessment for recovery planning, government funding, and resiliency planning, information from individuals within those communities may be needed to assess the effects and medical needs, particularly of Hispanic/Latinos living within those communities, and using health care facilities.
Respondents who evacuated (either before, during or immediately after Sandy) experienced greater adverse effects from Sandy and had a higher percentage with medical interruptions or “medical needs” than those who did not. People evacuated during the storm because of flooding and after the storm because of power and heat outages. This supports the State government’s mandatory evacuation orders in the days before Sandy. The severity and date of impact for Sandy were accurately projected 4–5 days before it made landfall in New Jersey. Further, the hardest hit respondents were those who were told to evacuate, but did not; 46 % of these had “medical need” during or immediately following Sandy. Again, this argues for stronger enforcement of evacuation orders, or provisions for those who choose not to evacuate, especially access to emergency care, doctors and medicines, and access to shelters.
Factors influencing personal evacuation decisions are very complex (Riad et al., 1999), and involve interplays of communication, past experience, and risk perceptions involving social and geographic vulnerability (Cutter and Emrich, 2006). Each community and each storm may have unique features determining responses to evacuation orders or threats. Minorities are more reluctant to evacuate than majority residents in the same communities (Elder et al., 2006). Evacuation requires transportation and shelter options, and entails additional costs and loss of wages (and perhaps jobs), to already economically challenged families. Security issues and fear of robbery enter evacuation decisions in some communities. In the present study, more Hispanics than others had to walk to the centers (as opposed to using cars), which would also have made it more difficult for evacuation. The social and economic inequities are particularly evident in coastal communities, since the wealthy live right along the coast, and much poorer people live only a block away. New Jersey is not unique in this coastal pattern with the very rich living just behind the beach or dunes (Cutter and Emrich, 2006).
Medical Issues
It is often difficult to determine effects from disasters such as Sandy from interviews because perceptions of the same events may differ. Thus, questions about the same issue were asked in different places on the survey (“did you have trouble getting your medicines before during or after” was asked early in the interview, and “did you have interruption of your medicines” was asked later in the interview). Further, the questionnaire was designed so that there was information on “medical need”, including questions on interruption of medical services and medicines, needing to get to the centers, having medical conditions requiring frequent visits (e.g. diabetes, asthma, heart rhythms, cancer, dialysis), did you have trouble getting there. These were used to assign a “medical need” score. The data from the interviews indicates that there was almost twice as much “medical need” as was affirmed by the respondents on direct questions (refer to Table 1). Whether this is unique to Hispanic/Latinos (as opposed to other ethnicities), low income, or vulnerable communities, or to other communities elsewhere, is unclear. However, it suggests that interviews with patients will be most useful when a range of questions are asked, and when investigators (and physicians) examine the answers from each respondent carefully to determine their professional evaluation of “medical need”.
Evaluation of ecological statements
Many studies have reported that minorities have less access to medical care (Abraido-Lanza, 1999; Fiscella et al., 2002; Norris et al., 2002; Jacquez et al., 2016) than the white population. Far fewer studies have examined ethnic differences in environmental concerns, and some of these have reported that minorities are less concerned (Arp and Kenny, 1996; Bronfrian and Cifuentes, 2003), although this is not always the case (Burger, 1998; Greenberg, 2005). However, ethnic differences in environmental concerns have generally been the subject of extensive study with respect to exposure to chemicals as an environmental justice issue (Bullard, 1994; Greenberg, 2005; Burger and Greenberg, 2006). Merely understanding the general evaluation of “environmental concern” is less useful than understanding perceptions of specific concerns that might aid in educational programs or public policy and management decisions (for example, the role of dunes and marshes in flood protection). It is in this context that understanding culturally-dependent concerns and knowledge is important for managing ecological and human communities along coasts (Huerta and Macario, 1999). Indeed, increasing resilience of coastal communities depends on understanding different perceptions and concerns that affect public policy or public support for policies (Freedman, 2013), and may require in-depth studies of specific ethnic groups faced with a specific risk, threat, or disaster. Only by understanding perceptions of specific ecological issues or concerns can managers and planners move forward. That is, ratings of general ecological concern may be high or low, while ratings of specific environmental issues (like the risk from a chemical plant, or the importance of dunes to coastal protection) may be different. For example, an assessment of environmental concerns rated specific ecological actions (e.g. enlarging parks, creating bird foraging habitats, preserving wild areas around water supplies) and found both differences among the issues, and ethnic differences within the rating of issues (Burger and Greenberg, 2006). For developing public policy and management actions, perceptions of relevant specific issues need to be examined as a function of demographics and other contributing factors.
In this paper, respondents agreed with the scientists about climate change, storms, sea level rise, flooding, coastal ecosystems and the role of humans (IPCC, 2007, 2014; Sallenger et al., 2012). Respondents recognized the connections between global warming, more frequent and severe storms, sea level rise and flooding, and that global warming is due to human activity. This is encouraging in that a recognition of the role of climate change and sea level rise to community well-being is necessary for development of a resiliency strategy. However, there was less agreement with the ecological statements that damages from flooding were due to loss of dunes or salt marshes (the ratings for these two averaged about 3 out of 5). This indicates a need for further education about the role of soft infrastructures (beaches, dunes, salt marshes) in protection of coastal communities. Enlisting the aid and support of the growing Hispanic/Latino populations in New Jersey, and elsewhere, in the public support for coastal zone management will be increasingly important in hardening the shoreline and increasing resiliency.
Implications for Public Policy and Actions
Disaster preparedness requires data to understand what people do in a disaster, how they are impacted, and the relationship between these. This study of vulnerable Hispanic/Latino respondents using Federally Qualified Health Centers in New Jersey indicates that they were heavily impacted, and that their personal rating of impacts was a better predictor of their effects from Sandy and of medical issues than was a composite community rating (after Halpin, 2013). This suggests, as expected, that there is variation within communities (and counties) in the effects that individuals face, that personal ratings need to be considered in disaster planning and recovery, that there may be pockets of high impact within those with generally lower impact, and that Hispanic/Latino communities within counties may be more vulnerable than others. Indeed Halpin (2013) reported that low income families were over-represented among the hardest hit households in New Jersey.
The respondents interviewed were by definition low income vulnerable communities that use the Federally Qualified Health Centers. There was a high rate of foreign-born among the respondents (90 %), as well as being without power, needing the centers, having trouble getting to the centers, and having interruption of medical services. Accordingly, a high percentage of the interviews were conducted in Spanish, which elicited many responses to the questions. Special attention needs to be directed to this vulnerable population in New Jersey, particularly with respect to following evacuation orders, planning for future disasters by obtaining sufficient medicines, and other preparedness actions. However, the results suggest that planners and managers need to attend to this population with education, more information about preparedness and evacuation, and directed programs to ensure transportation, open health centers, and available locations for access to doctors and medicines.
CONCLUSIONS
Hispanic/Latinos are the fastest growing population group in New Jersey, and many reside in low income, minority-dominated communities near the shore, and were vulnerable to the effects of flooding, downed trees, damaged transportation infrastructure, and prolonged loss of electricity from Hurricane Sandy. Some more inland Hispanic/Latino communities also suffered from flooding, downed trees and prolonged loss of electricity, but their plight was less recognized because the houses were not blown down or swept away by surge tides (as they were along the shore). Only 10 % of the Hispanic/Latino respondents interviewed at Federally-Qualified Health Centers were born in the U.S., even though those born elsewhere had been in the U.S. an average of 16 years. Evacuation rates, days evacuated, days without power, percent needing health centers, and the percent with medical needs varied significantly as a function of respondents’ self-evaluation of impact, rather than a measure of community impact. This suggests that evaluating damage, providing relief immediately after a severe hurricane, and providing federal funds for people in vulnerable communities should be on the basis of individual impacts, rather than on a wider geographical basis. Further, all groups, regardless of self-identification of needing the center and interruption of medical services, underestimated their “medical need” as determined by the investigators overall evaluation. People who evacuated, mainly from areas with substantial flooding and community devastation, had significantly greater medical need than those that did not evacuate. Respondents that reported the highest medical need were those that were told to evacuate, but did not. This suggests that first responders need to attend to those in evacuation areas that did not evacuate (and go into these communities to find them), followed by those attempting to evacuate during or immediately after a disaster.
Overall the Hispanic/Latinos interviewed agreed with statements that “increased frequency and severity of storms was due to climate change”, that “storms will come more often”, “flooding was due to sea level rise”, and “changing climate was due mainly to human activity”. Recognizing the importance of climate change and sea level rise is a first step to acknowledging the problem of living in low-lying coastal communities. Their perceptions are encouraging for public planners and managers who need to develop strategies to improve resiliency of coastal communities. However, the key role of dunes and salt marshes in protecting coastal communities from flooding was not as accepted, which is a serious deficit as future resiliency planning may rely on intact, ecological systems as one measure of coastal protection.
Acknowledgments
This study was supported by the Centers for Disease Control and Prevention Public Health Preparedness and Response Research to Aid Recovery from Hurricane Sandy (CDC-RFA-13-001) grant to New Jersey Department of Health, which included collaboration with the New Jersey Medical School, Rutgers University, New Jersey Department of Human Services, and the Division of Life Sciences, Rutgers University, as well as the NIEHS Center (P30ES005022). The project and protocol were approved by the New Jersey Primary Care Association (NJPCA), the Directors of the participating Federally Qualified Health Centers, the Rutgers Institutional Review Board (Protocol E14-319, Notice of Exemption), and the New Jersey Department of Health. Thanks are extended to K. Grant Davis (CEO of New Jersey Primary Care Association), her Executive Board, and the Center Directors of the Federally Qualified Health Centers for allowing the interviewing of their patients, their staff for being so accommodating, Clarimel Cepeda, Marta Hernandez, Ahmend Nezar, Alan Perez, and Ana Quintero for aid in interviewing, and all those who patients who consented to be interviewed. This paper represents the views of the authors, and not the funding agencies or the NJPCA.
References
- Abraido-Lanza AF, Dohrenwend BP, Ng-Mak DS, Turner JB. The Latino mortality paradox: a test of the “salmon bias” and healthy migrant hypotheses. Am. J. Publ. Health. 1999;89:1543–1548. doi: 10.2105/ajph.89.10.1543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abramson DM, Van Alst D, Merdjanoff A, Piltch-Loeb R, Beedasy J, Findley P, Tobin-Gurley J. The Hurricane Sandy Place Report: Evacuation Decisions, Housing Issues and Sense of Community. National Center for Disaster Preparedness, Columbia University; 2015. [Accessed Sept. 1, 2016]. http://academiccommons.columbia.edu/catalog/ac:187430. [Google Scholar]
- Arp W, III, Kenny C. Black environmentalism in the local community context. Environ. Behav. 1996;28:267–282. [Google Scholar]
- Barnegat Bay Beat (BBB) Special Report: Sandy-a record setting storm. Barnegat Bay Partnership Quarterly Publication; 2012. p. 20127. [Google Scholar]
- Behr JG, Diaz R. Disparate health implications stemming from the propensity of elderly and medically fragile populations to shelter in place during severe storms. J. Publ. Health Manag. Pract. Suppl. 2013;2:S55–S62. doi: 10.1097/PHH.0b013e318297226a. [DOI] [PubMed] [Google Scholar]
- Bergen T, Thomas D, Schwartz E, McKibben J, Rusiecki J. Sleep deprivation and adverse health effects in United States Coast Guard responders during Hurricanes Katrina and Rita. Sleep Health. 2015;1:208–274. doi: 10.1016/j.sleh.2015.09.010. [DOI] [PubMed] [Google Scholar]
- Bronfman N, Cifuentes L. Risk perception in a developing country: the case of Chile. Risk Anal. 2003;23:1271–1285. doi: 10.1111/j.0272-4332.2003.00400.x. [DOI] [PubMed] [Google Scholar]
- Bullard RD. Unequal protection: environmental justice and communities. Sierra Club Books; California: 1994. [Google Scholar]
- Burger J. Environmental studies and perceptions of future land use at the Savannah River Site: are there racial differences? J. Toxicol. Environ. Health. 1998;53:255–262. doi: 10.1080/009841098159268. [DOI] [PubMed] [Google Scholar]
- Burger J. Ecological concerns following Superstorm Sandy: stressor level and recreational activity levels affect perceptions of ecosystems. Urban Ecosys. 2015;18:553–575. doi: 10.1007/s11252-014-0412-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burger J, Gochfeld M. Health concerns and perceptions of central and coastal New Jersey residents in the 100 days following Superstorm Sandy. Sci. Total Environ. 2014a;481:611–618. doi: 10.1016/j.scitotenv.2014.02.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burger J, Gochfeld M. Perceptions of personal and governmental actions to improve responses to disasters such as Superstorm Sandy. Environ.l Hazards. 2014b;13:200–210. [Google Scholar]
- Burger J, Greenberg M. Ethnic differences in ecological concerns: Spanish-speaking Hispanics are more concerned than others. Environ. Res. 2006;102:36–45. doi: 10.1016/j.envres.2005.12.009. [DOI] [PubMed] [Google Scholar]
- Cutter SL, Emrich CT. Moral Hazard, Social Catastrophe: The Changing Face of Vulnerability along the Hurricane Coasts. Annals Amer Acad Political & Social Sci. 2006;604:102–112. [Google Scholar]
- Dawson P. Hispanics and health care in the United States: Access, information and knowledge. J. Youth Dev. 2012;7:1–2. [Google Scholar]
- Elder K, Xirasagar S, Miller N, Bowen SA, Glover S, Piper C. African Americans’ decisions not to evacuate New Orleans before Hurricane Katrina: a qualitative study. Am. J. Publ. Health. 2007;97:S124–129. doi: 10.2105/AJPH.2006.100867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiscella K, Franks P, Doescher MP, Saver BG. Disparities in health care by race, ethnicity, and language among the insured. Med. Care. 2002;40:52–29. doi: 10.1097/00005650-200201000-00007. [DOI] [PubMed] [Google Scholar]
- Freedman A. Heeding Sandy's lessons, before the next big storm. [Accessed June 5, 2015];Climate Central. 2013 2013. Available at: http://www.climatecentral.org/news/four-key-lessons-learned-from-hurricane-Sandy-15928.
- Greenberg M. Concern about the environment: how much difference do race and ethnicity make? Environ. Health Perspect. 2005;113:369–374. doi: 10.1289/ehp.7611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halpin SH. The impact of Superstorm Sandy on New Jersey towns and households. Report, Rutgers University School of Public Affairs and Administration; Newark, NJ: 2013. [Google Scholar]
- Houser C, Hapke C, Hamilton S. Controls on coastal dune morphology, shoreline erosion and barrier island response to extreme storms. Geomorphol. 2008;100:223–240. [Google Scholar]
- Hsu SA. Storm surges in New York during Hurricane Sandy in 2012: a verification of the wind-stress tide relation. Boundary-Layer Meteorol. 2013;148:593–598. [Google Scholar]
- Huerta EE, Macario E. Communicating health risk to ethnic groups: reaching Hispanics as a case study. J. Natl. Cancer Inst. Monogr. 1999;35:23–26. doi: 10.1093/oxfordjournals.jncimonographs.a024202. [DOI] [PubMed] [Google Scholar]
- Intergovernmental Panel on Climate Change (IPCC) Contribution of working groups I, II and III to the fourth assessment report of the intergovernmental panel on climate change. Geneva, Switzerland: IPPC; 2007. Climate change 2007: synthesis report. [Google Scholar]
- Intergovernmental Panel on Climate Change (IPCC) Intergovernmental panel on climate change. Geneva, Switzerland: PPCI; 2014. [Accessed August 2016]. Climate change 2014: impacts, adaptation and vulnerability. http://www.ipcc.ch/report/ar5/wg2. [Google Scholar]
- Jacquez F, Vaughn L, Zhen-Duan J, Graham C. Health care use and barriers to care among Latino immigrants in a new migration area. J. Health Care Poor Underserv. 2016;27:1759–1776. doi: 10.1353/hpu.2016.0161. [DOI] [PubMed] [Google Scholar]
- Kessler R, Keane T, Ursano R, Mokdad A, Zaslavsky A. Sample and design considerations in post-disaster mental health needs assessment tracking surveys. Int. J. Methods Psychiat.. Res. 2008;17:S6–S20. doi: 10.1002/mpr.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neria Y, Shultz JM. Mental health effects of hurricane Sandy: characteristics, potential aftermath, and responses. JAMA. 2012;308:2571–2572. doi: 10.1001/jama.2012.110700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norris FH, Friedman MM, Watson PJ, Byrne CM, Diaz E, Kaniasty K. 60,000 diaster victims speak: Part I. An empirical review of the empirical literature, 1981–2001. Psychiatr. 2002;65:207–239. doi: 10.1521/psyc.65.3.207.20173. [DOI] [PubMed] [Google Scholar]
- North C, Oliver J, Pandya A. Examining a comprehensive model of disaster-related posttraumatic stress disorder in systematically studied survivors of 10 disasters. Am. J. Publ. Health. 2012;102:e40–e48. doi: 10.2105/AJPH.2012.300689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Neill KM, Van Abs DJ. Taking chances: the coast after Hurricane Sandy. Rutgers Univ. Press; New Brunswick, NJ: 2016. [Google Scholar]
- Pew Hispanic Center. From 200 million to 300 million: The numbers behind population growth. Washing. D.C: 2006. [Google Scholar]
- Plant NG, Stockdon HF, Sallenger AH, Jr, Turco MJ, East JW, Taylor AA, Shaffer WA. Forecasting hurricane impact on coastal topography. Eos. 2010;91:65–72. [Google Scholar]
- Pries AJ, Miller DL, Branch LC. Identification of structural features that influence storm-related dune erosion along a barrier island ecosystem in the Gulf of Mexico. J. Coastal Res. 2008;24:168–176. [Google Scholar]
- Price M, Davidson TM, Andrews JO, Ruggiero KJ. Access, use, and competition of a brief disaster mental health intervention among Hispanics, African Americans and White affected by Hurricane Ike. J. Telemed. Telecare. 2013;19:70–74. doi: 10.1177/1357633X13476230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Psuty NP, O’Fiara DD. Coastal hazard management. Rutgers Press; New Brunswick, NJ: 2002. [Google Scholar]
- Riad JK, Norris FH, Riback RB. Predicting evacuation in two major disasters: risk perception, social influence, and access to resources. J. Appl. Social Psychol. 1999;29:918–934. [Google Scholar]
- SAS (Statistical Analysis System) Statistical Analysis. SAS; Cary, NC: 2005. [Google Scholar]
- Sallenger AK, Doran KS, Howd PA. Hotspot of accelerated sea-level rise on the Atlantic coast of North America. Nature. 2012;2:884–888. [Google Scholar]
- Sastry N, Gregory J. The effect of Hurricane Katrina on the prevalence of health impairments and disability among adults in New Orleans: differences by age, race, and sex. Soc. Sci. Med. 2013;80:121–129. doi: 10.1016/j.socscimed.2012.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swerdel JN, Rhoads GG, Cosgrove NM, Kostis JB. Rates of hospitalization for dehydration following Hurricane Sandy in New Jersey. Disaster Med. Publ. Health Prep. 2016;10:188–192. doi: 10.1017/dmp.2015.169. [DOI] [PubMed] [Google Scholar]
- Trumbo C, Lueck M, Marlatt H, Peek L. The effect of proximity to hurricanes Katrina and Rita on subsequent hurricane outlook and optimistic bias. Risk Anal. 2011;31:1907–1918. doi: 10.1111/j.1539-6924.2011.01633.x. [DOI] [PubMed] [Google Scholar]
- US Census Bureau. New Jersey: 2000. U.S. Department of Commerce; 2002. [Accessed Feb. 13, 2017]. Census 2000 Profile. https://www.census.gov/prod/2002pubs/c2kprof00-nj.pdf. [Google Scholar]
- US Census Bureau. New Jersey: U.S. Census Bureau. U.S. Department of Commerce; 2017. [Accessed Feb. 13, 2017]. Quick facts. http://www.census.gov/quickfacts/table/PST045216/34. [Google Scholar]
- US. Geological Survey (USGS) Fact Sheet 2010–3012. US Dept Interior; Washing. D. C: 2010. Impacts and predictions of coastal change during hurricanes. [Google Scholar]
- US. Geological Survey (USGS) Hurricane Sandy: updated assessment of potential coastal-change impacts. [Accessed December 15 2016];2013 http://coastal.er.usgs.gov/hurricanes/sandy/coastal-change/initialassessment.php.