Abstract
No-scalpel vasectomy employs a refined method of dissection and delivery of the vas deferens. We compared no-scalpel vasectomy with standard incisional vasectomy in 176 patients over a 33 month period. The haemorrhage rate was 1.08 per cent for no-scalpel vasectomy compared with 11.9 per cent for standard vasectomy (p < 0.005). The infection rate was 3.26 per cent for no-scalpel vasectomy as against 14.28 per cent for standard vasectomy (p < 0.01). There was a 37.5 per cent reduction in operating time and a substantial reduction in pain during and after the procedure when no-scalpel vasectomy was performed and also there was no failure of vasectomy. No-scalpel vasectomy is a satisfactory alternative to standard vasectomy with fewer complications and increased patient acceptability.
KEYWORDS: Male sterilization, Vasectomy
Introduction
No-scalpel vasectomy (NSV) is a new and innovative technique developed in China in 1974 for delivery and dissection of the vas deferens [1]. It has increased the acceptability of vasectomy by eliminating the fear of incision and reduced the morbidity by limiting the extent of dissection.
We made a comparative evaluation of no-scalpel vasectomy and standard incisional vasectomy (SIV) in 176 procedures done between December 1993 and August 1996. A study of the complication rate, time taken and effectiveness was made. We also studied the applicability of NSV for practice in the Armed Forces.
Material and Methods
One hundred and seventy six serving personnel between 30-39 years of age were included in this study. After informed consent the men underwent NSV or SIV at random. After the procedure each man was instructed to use a contraceptive for next 3 months and to have a semen analysis before resumption of unprotected intercourse. Tablet co-trimoxazole 160-800 mg bd for 5 days and tablet soluble aspirin 600 mg tds for 3 days was prescribed. Patients were told to return for review after one week, or earlier if required. All patients were questioned about the pain they felt during and after the procedure.
NSV was performed according to the technique of Li and associates [1] with minor modifications. The scrotal skin was shaved and prepared with warm savlon solution (chlorhexidine gluconate and cetrimide).
Local Anaesthesia : The vas deferens was manipulated under the median raphe of the scrotum. The right vas was firmly trapped over the middle of the left hand and under the index finger and the thumb. A superficial wheal was raised using a 23 gauge needle and 2 per cent plain lignocaine. The needle is then advanced in the perivasal sheath toward the external inguinal ring and 2-5 mL of lignocaine injected. This effects a vasal nerve block away from the actual vasectomy site. The left vas was then fixed under the previous skin puncture site and anaesthetized using the same 3-finger technique.
Fixation and delivery of the vas : After both vas had been anaesthetized, the right vas was again fixed under the site of the skin wheal with the left hand. The vas and overlying skin was grasped with an Allis forceps (Fig 1). We found the Allis forceps a satisfactory substitute for the special extracutaneous vas deferens fixation clamp designed by Li [1]. A curved mosquito artery forceps with the point sharpened was used as a dissecting clamp. The point of the clamp was used to puncture the scrotal skin, vas sheath and vas wall where the vas was most superficial and prominent. The blades were gently opened spreading all layers down to the bare vas wall (Fig 2). The vas was delivered through the puncture hole using the dissecting clamp while simultaneously releasing the Allis forceps (Fig 3). The Allis forceps was used to grasp the delivered vas. The sheath and vasal vessels were stripped gently away from the vas using the dissecting clamp.
Fig. 1.
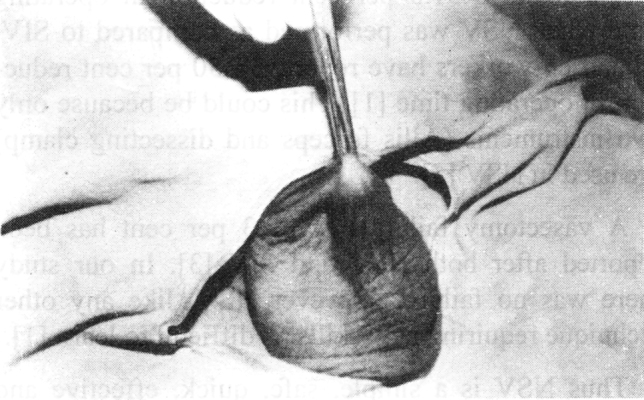
Vas grasped with Allis forceps
Fig. 2.
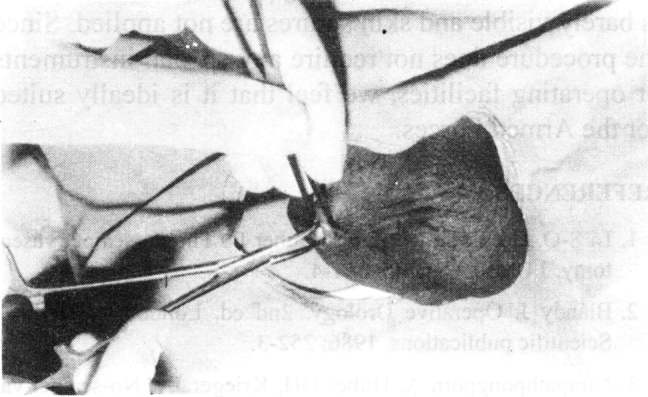
Dissection of vas with mosquito artery forceps
Fig. 3.
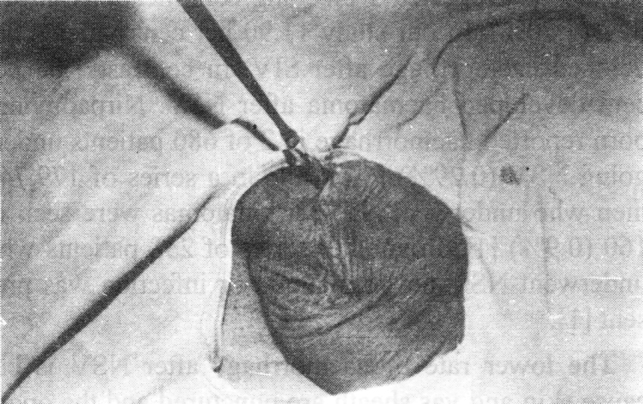
Vas delivered through puncture hole
One cm segment of the vas was resected and the two cut ends occluded with 2/0 silk sutures. The abdominal end of the vas was buried by closing its sheath with a silk suture. After occlusion the ends of the right vas were returned to the scrotum and the left vas fixed directly under the same puncture hole using the 3-finger technique. The remainder of the procedure was identical to that of the right side.
After both vas had been occluded and returned to the scrotum the puncture wound was pinched tightly for a minute and inspected for bleeding. The puncture hole would contracted and remain invisible to the patient (Fig 4). No suture was required for the closure. Povidone iodine 5 per cent ointment was applied and a sterile dressing held in place with a suspensory bandage.
Fig. 4.
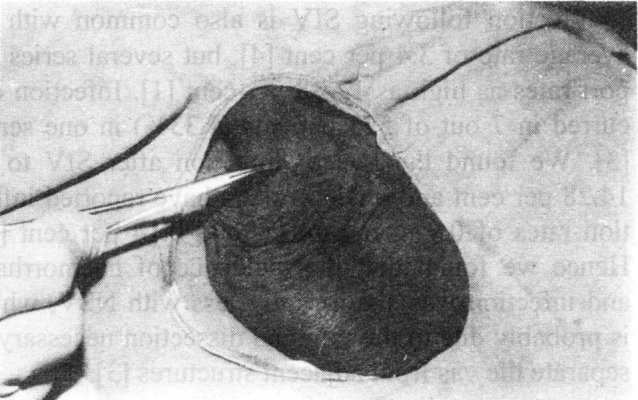
Puncture hole invisible after procedure
The SIV technique was essentially similar to that described by Blandy [2] and Nirapathpongporn and co-workers [3]. After administration of local anaesthesia a 0.5-1.0 cm incision was made with a scalpel in the median raphe of the scrotum. The vas was grasped with an Allis forceps, its sheath incised longitudinally and the vas lifted out of its sheath. The vas was ligated and divided in a manner similar to NSV. The procedure was repeated on the other side. Haemostasis was ensured and the skin and dartos closed with one or two 2/0 silk sutures. Wound was dressed like in NSV.
Statistical analysis of results was done using the chi-square test.
Results
One hundred and seventy six vasectomies were done in a 33 month period in our hospital. Ninety two (52.27%) underwent NSV while 84 (47.72%) underwent SIV. Common complications were haemorrhage and wound infection (Table). Haemorrhage was seen in 10 who underwent SIV (11.90%). Two required drainage of large scrotal haematomas. One haemorrhagic complication was observed after NSV (1.08%) (chi-square 8.76, df=1, p<0.005). Infection was seen in 12 men who underwent SIV (14.28%). Three patients after NSV had wound infection (3.26%) (chi-square 6.86, df=1, p<0.01). No damage to scrotal skin was noted with use of Allis forceps in NSV.
Nineteen patients (22.61%) who underwent SIV complained of moderate to severe pain, while 7 patients (7.60%) of the NSV group had such complaints.
The average time taken for SIV was 14 min with a range of 10-19.5 min, whereas the average operating time for NSV was 8.75 min with a range of 5-13 min. This represented a 37.5 per cent reduction in average operating time.
TABLE.
Complications after SIV and NSV
| SIV (n=84) | NSV (n=92) | ||
|---|---|---|---|
| Haemorrhage | 10 (11.90%) | 1 (1.08%) | p < 0.005 |
| Infection | 12 (14.28%) | 3 (3.26%) | P < 0.01 |
SIV – Standard incisional vasectomy, NSV – No-scalpel vasectomy
Both procedures were 100 per cent effective as shown by the absence of live sperms in the ejaculates of all 176 men at the end of 3 months.
Discussion
NSV is a novel technique for delivery and dissection of the vas deferens. It has been successfully used in over 80 lakh men in China, Thailand and other developing countries [3]. Our study indicates that NSV has advantages over the conventional incisional technique. NSV has a significantly lower complication rate than SIV. Haematoma is a common complication of SIV with an average incidence of 2 per cent and a range of 1-29 per cent [4]. Nirapathpongporn and associates [3] reported 9 bleeding complications in 523 SIV (1.70%). In our study 11.90 per cent patients developed haemorrhage after SIV. In contrast 1.08 per cent developed haematoma after NSV. Nirpathpongporn reported haemorrhage in 2 of 680 patients undergoing NSV (0.29%) [3], while in a series of 179,741 men who underwent NSV, haematomas were seen in 160 (0.9%) [1]. In another series of 238 patients who underwent NSV no haematoma or infection was present [1].
The lower rate of haemorrhage after NSV is because skin and vas sheath are punctured and the opening is then dilated, pushing aside blood vessels rather then cutting them [1].
Infection following SIV is also common with an average rate of 3.4 per cent [4], but several series report rates as high as 12-38 per cent [1]. Infection occurred in 7 out of 523 patients (1.33%) in one series [3]. We found the rate of infection after SIV to be 14.28 per cent and other workers have reported infection rates of 0.91 per cent [1] and 0.14 per cent [3]. Hence we found that the incidence of haemorrhage and infection was significantly less with NSV, which is probably due to the minimal dissection necessary to separate the vas from adjacent structures [3].
In our study 22.61 per cent of men who underwent SIV complained of moderate to severe pain as against 7.60 per cent who underwent NSV. Liu and Li have reported that 70 per cent of patients who underwent NSV experienced less pain during and after surgery than those who underwent conventional vasectomy [5].
We found a 37.5 per cent reduction in operating time when NSV was performed as compared to SIV. Li and co-workers have reported a 50 per cent reduction in operating time [1]. This could be because only two instruments (Allis forceps and dissecting clamp) are used in NSV [5].
A vasectomy failure rate of 3 per cent has been reported after both NSV and SIV [3]. In our study there was no failure. However NSV, like any other technique requiring new skills, is difficult to learn [1].
Thus NSV is a simple, safe, quick, effective and less painful method of male sterilisation. We have found it to be more acceptable to our patients since there is no incision with a scalpel, the puncture wound is barely visible and skin sutures are not applied. Since the procedure does not require any special instruments or operating facilities, we feel that it is ideally suited for the Armed Forces.
REFERENCES
- 1.Li S-Q, Goldstein M, Zhu J, Huber D. The no-scalpel vasectomy. J Urol 1991; 145: 341-4 [DOI] [PubMed]
- 2.Blandy J. Operative Urology. 2nd ed. London : Blackwell Scientific publications. 1986:252–253. [Google Scholar]
- 3.Nirapathpongporn A, Huber DH, Krieger JN. No-scalpel vasectomy at the Kings birthday vasectomy festival. Lancet. 1990;335:894–895. doi: 10.1016/0140-6736(90)90487-p. [DOI] [PubMed] [Google Scholar]
- 4.Kendrick JS, Gonzales B, Huber DH, Grubb GS, Rubin GL. Complications of vasectomies in the United States. J Fam Pract 1987; 25: 245 [PubMed]
- 5.Liu X, Li S. Vasal sterilization in China. Contraception. 1993;48:255–265. doi: 10.1016/0010-7824(93)90144-v. [DOI] [PubMed] [Google Scholar]


