Abstract
Objective
We discuss the strengths of the medical response to the Boston Marathon bombings that led to the excellent outcomes. Potential shortcomings were recognized, and lessons learned will provide a foundation for further improvements applicable to all institutions.
Background
Multiple casualty incidents from natural or man-made incidents remain a constant global threat. Adequate preparation and the appropriate alignment of resources with immediate needs remain the key to optimal outcomes.
Methods
A collaborative effort among Boston’s trauma centers (2 level I adult, 3 combined level I adult/pediatric, 1 freestanding level I pediatric) examined the details and outcomes of the initial response. Each center entered its respective data into a central database (REDCap), and the data were analyzed to determine various prehospital and early in-hospital clinical and logistical parameters that collectively define the citywide medical response to the terrorist attack.
Results
A total of 281 people were injured, and 127 patients received care at the participating trauma centers on that day. There were 3 (1%) immediate fatalities at the scene and no in-hospital mortality. A majority of the patients admitted (66.6%) suffered lower extremity soft tissue and bony injuries, and 31 had evidence for exsanguinating hemorrhage, with field tourniquets in place in 26 patients. Of the 75 patients admitted, 54 underwent urgent surgical intervention and 12 (22%) underwent amputation of a lower extremity.
Conclusions
Adequate preparation, rapid logistical response, short transport times, immediate access to operating rooms, methodical multidisciplinary care delivery, and good fortune contributed to excellent outcomes.
On April 15, 2013, 4 hours into the 117th running of the Boston Marathon, 2 improvised explosive devices (IEDs) were detonated among the spectators approximately 100 to 200 yards from the finish line. The first detonation occurred at 2:50 pm and the second followed 10 seconds later. There were 26,893 official entrants, and more than 500,000 people gathered along the marathon route to cheer on those runners and celebrate Patriot’s Day, the Massachusetts state holiday marking the “shot heard, round the world” and nationally recognized as the start of the American Revolution in 1775. Now some 238 years later, Massachusetts was again under siege.
With the exception of the Alfred P. Murrah building bombing in Oklahoma City in 1995, the United States had been mostly spared the volume and shock of terrorist attacks seen in other countries until the incendiary events of September 11, 2001.1–3 Over the past decade, most Americans have become all too familiar with the impact of IEDs in East Africa, Spain, London, Israel, Iraq, and Afghanistan.3
The Boston Athletic Association, Boston Emergency Medical Services (EMS), and the Boston health care community have planned and drilled for mass casualty incidents (MCIs) for many years (personal communication, Chris Troyanos). In preparation for the race, a temporary medical tent had been erected at the finish line to provide care for up to 2500 runners. The tent is staffed with paramedics, physicians, nurses, physical therapists, and others to provide for general heat- and overuse-related injuries. Boston EMS crews are stationed at the tent to transport those approximately 200 to 250 runners in need of further medical attention to the Boston area hospitals. The City of Boston, with its immediate population of approximately 636,479,4 is unique in that it is supported by 5 adult level I trauma centers and 4 pediatric trauma centers. The finish line for the race and the 2 blasts occurred in the geographic center of the surrounding trauma centers.
This report may serve as a template for other population centers to learn from what we have experienced and perhaps mitigate future morbidity and mortality as a result of multiple or MCIs through discussion, forethought, preparation, and above all training.
METHODS
Analysis
Each of the American College of Surgeons verified level I trauma centers abstracted the data on the victims from the medical records and trauma registries: Beth Israel Deaconess Medical Center, Boston Children’s Hospital, Boston Medical Center, Brigham and Women’s Hospital, Massachusetts General Hospital, and Tufts Medical Center. Study data were collected and managed using Research Electronic Data Capture (REDCap) (Vanderbilt University, Nashville, TN) hosted at Brigham and Women’s Hospital. The data were reviewed, cleaned, and prepared for analysis. Using Microsoft Excel, analyses were performed to aggregate the data, identify trends, and describe the medical care. The study protocols were approved by the individual institutional review board processes.
RESULTS
Patient Flow
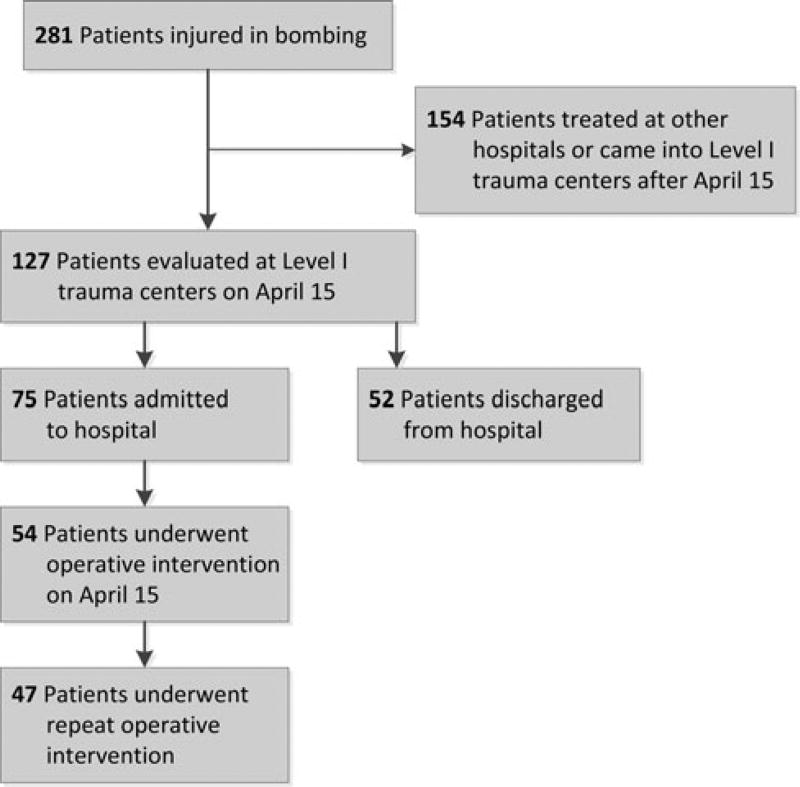
In all, 281 people were injured in the bomb blast (data from the One Fund Boston) and cared for at 26 hospitals (Fig. 1). The 127 patients evaluated at the Boston area’s level I trauma/pediatric centers on April 15, 2013, are reviewed in this report. The many other patients who received exemplary care in the outlying community hospitals were not included in this initial review.
FIGURE 1.
Patient flow into medical centers.
Demographics and Prehospital Care
A majority of the patients were adult spectators initially treated by bystanders, police, and fire personnel or prehospital medical providers prepositioned at the medical tent (Table 1). The medical tent served as a flow-through area for upward of 96 to 100 patients on their way to the hospitals with no specific medical evaluation (personal communication, Sophia Dyer, MD). A total of 118 patients were directly evacuated from the scene to the hospitals via ambulance because of the concern for additional explosions, scene safety, and the severity of injury. Eight-three percent of those patients presenting with exsanguinating extremity wounds received tourniquets in the field. The median time from the explosion to the hospital for the injured patient was 11 minutes.
TABLE 1.
Patient Demographics and Pre-Hospital Care
| No. (%) Patients | |
|---|---|
| Age group, yr | |
| ≥15 | 117 (92.1) |
| <15 | 10 (7.9) |
| Country of origin | |
| United States | 96 (75.6) |
| Outside the United States | 4 (3.2) |
| Unknown | 27 (21.2) |
| Role in the event | |
| Spectator | 95 (74.8) |
| Runner | 3 (2.4) |
| Police | 6 (4.7) |
| EMS | 1 (0.8) |
| Other | 4 (3.1) |
| Unknown | 18 (14.2) |
| Location at time of event | |
| Road/Sidewalk | 101 (79.5) |
| Public building | 4 (3.2) |
| Unspecified place | 21 (16.5) |
| Other | 1 (0.8) |
| Signs of exsanguinating extremity wounds | |
| Yes | 31 (24.4) |
| No | 96 (75.6) |
| Touniquet(s) applied if exsanguinating wounds | |
| Yes | 26 (83.9) |
| No | 5 (16.1) |
| Was a disaster tag applied? | |
| Yes | 1 (0.8) |
| No | 23 (18.1) |
| Unknown | 103 (81.1) |
| Mode of transport to hospital | |
| Ambulance | 81 (63.8) |
| Walk-in | 27 (21.3) |
| Police | 2 (1.6) |
| Other vehicle | 3 (2.4) |
| Unknown | 14 (11.0) |
| Time from scene departure to ED arrival, median | 11 min |
| Time from scene departure to ED arrival, range | 5–53 min |
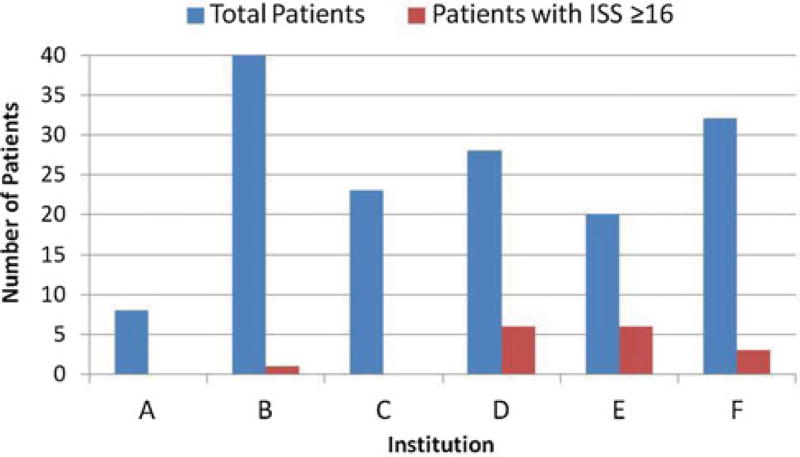
Distribution of Patients to Level I Trauma Centers
The severely injured patients, as determined by the Injury Severity Score (ISS) of 16 or higher on discharge, were relatively evenly distributed among the adult trauma centers (Fig. 2). This was dictated by the central command structure (CMED) of Boston EMS and is an established facility that keeps a daily census of the emergency department (ED) patient numbers within the city of Boston. The number of available operating rooms and intensive care unit (ICU) beds is not monitored by this organization.
FIGURE 2.
Patient surge into Boston trauma centers by injury severity score: April 15, 2013.
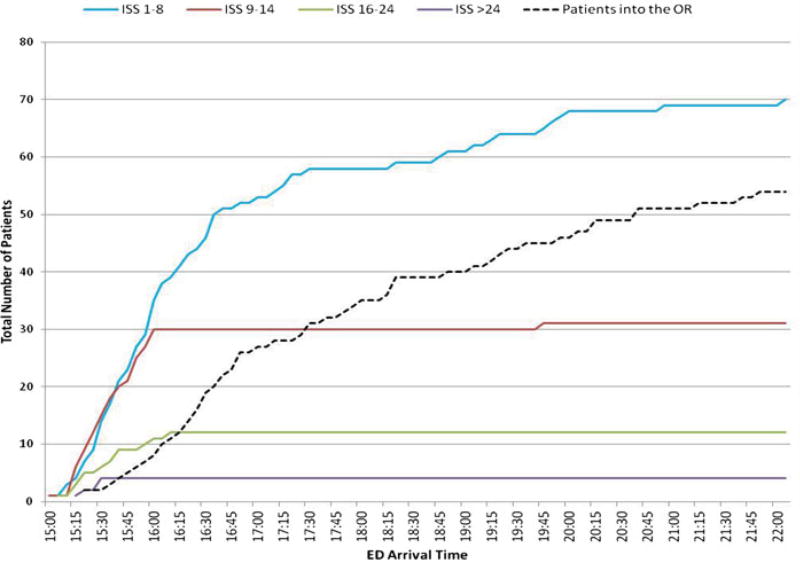
Surge Into Level I Trauma Centers
Within the first 30 minutes of the blast, those patients with ISS scores greater than 25 were all admitted (Fig. 3). Consolidation of the ISS curves indicates that 78% of the patients treated at the trauma centers arrived within 1½ hour of the initial event. The remainder presented over the next 5½ hours. The number of patients utilizing the operating room (black) presented a smoother more linear curve beginning shortly after the bombing and continuing at roughly the same rate into the evening hours.
FIGURE 3.
Patients by treating trauma center.
ED Phase of Care
Fifty-two (41%) of the patients evaluated at the trauma centers were discharged to home after initial evaluation in the ED. The remaining 75 patients (59.1%) were admitted for further evaluation and treatment (Table 2). As a surrogate for severity of injury and perhaps respiratory tract injury, fewer than 10% required emergent airway control in the form of endotracheal intubation and approximately 10% required immediate transfusion of packed red blood cells in the ED. Chest x-rays were performed on 50% with pelvic x-rays on 23% of the patients. The Focused Abdominal Ultrasound in Trauma (FAST) was performed on 18% of the patients. Various computerized tomographic (CT) scans were performed on 25% of these patients.
TABLE 2.
ED Status, Procedures, and Disposition
| Patient stats upon arrival in ED | |
| Blood pressure, range | 50/30 to 210/100 |
| Heart rate, median | 90 |
| Heart rate, range | 52 to 137 |
| No. (%) Patients | |
| Glasgow Coma Scale (GCS) | |
| ≤8 | 0(0) |
| 9–14 | 3 (2.4) |
| 15 | 92 (72.4) |
| Undocumented | 32 (25.2) |
| Interventions | |
| Emergency airway | 12 (9.5) |
| Central access | 1 (0.8) |
| PIV access | 39 (30.7) |
| IO access | 1 (0.8) |
| Crystalloids | 39 (30.7) |
| Colloids | 2 (1.6) |
| C-collar | 5 (3.9) |
| Analgesia | 43 (33.9) |
| Splint | 5 (3.9) |
| Other | 26 (20.5) |
| Radiologic studies | |
| CXR | 67 (52.8) |
| FAST | 23 (18.1) |
| Pelvis | 29 (22.8) |
| CT scan | 32 (25.2) |
| Transfusion administered? | |
| Yes | 15 (11.8) |
| No | 112 (88.2) |
| Type of transfusion | |
| Packed cells | 15 (11.8) |
| Plasma | 4 (3.2) |
| Platelets | 2 (1.6) |
| Patients admitted to hospital | 75 (59.1) |
| Patients discharged from hospital | 52 (40.9) |
| Location of admission from ED | |
| OR | 45 (60.0) |
| ICU | 11 (14.7) |
| Ward | 19 (25.3) |
| ED LOS, median | 106 min |
| ED LOS, range | 10 min to 481 min |
| ED LOS for patients admitted to OR, median | 45 min |
| ED LOS for patients admitted to ICU, median | 87 min |
| ED LOS for patients admitted to Ward, median | 129 min |
Disposition of Admitted Patients
The ED median length of stay was 106 minutes (range: 10–481 minutes). Seventy-five patients were admitted to the combined hospitals on the day of the bombing. Forty-five (60%) of those patients were admitted directly to the operating room with smaller numbers initially directed to the ICUs and the wards (Table 2).
Initial Operative Interventions and Inpatient Phase
A majority of the lead operative teams consisted of orthopedic and trauma surgeons with a much smaller initial requirement on behalf of the burn, neurosurgical, plastic, or vascular surgeons. Twenty-four (44%) required foreign body removal consisting of pieces of the pressure cookers used to create the IEDs and the ball bearings and nails that were packaged inside the devices. The plastic surgical services assumed a much more prominent and invaluable role in the reconstructive phase of the patient care in the days after the initial bombing (Table 3).5
TABLE 3.
OR Interventions, Inpatient Phase, and Discharge Disposition
| No. (%) Patients | |
|---|---|
| Patients who went directly to OR, April 15 | 45 |
| Patients who went to ICU, then OR, April 15 | 6 |
| Patients who went to ward, then OR, April 15 | 3 |
| No. procedures per patient, April 15 | |
| 1–2 | 15 |
| 3–5 | 29 |
| 6–10 | 9 |
| >10 | 1 |
| Patients who underwent operative procedures, April 15 | |
| Craniotomy | 0 |
| Thoracotomy | 0 |
| Laparotomy | 4 |
| Foreign body removal | 24 |
| External fixator | 7 |
| Soft tissue debridement | 54 |
| Vascular procedure | 14 |
| Lower extremity amputation | 12 |
| Fracture repair | 15 |
| Patients who underwent repeat operative procedures | 47 |
| Patients who underwent amputation after April 15 | 3 |
| ICU LOS, median | 4 d |
| ICU LOS, range | 1 to 22 d |
| Patients who experienced complications | 7 (5.5) |
| Hospital LOS, median | 8.5 d |
| Hospital LOS, range | 1 to 49 d |
| Discharge location | |
| Rehabilitation | 33 (44.0) |
| Home | 30 (40.0) |
| Home with services | 11 (14.7) |
| Skilled nursing facility | 1 (1.3) |
Of the 75 patients admitted to the hospitals, 49 (65%) underwent operative intervention for lower extremity injuries on the first day and 12 (25.5%) of those with lower extremity injuries required lower extremity amputations.
Forty-seven (87%) of the patients who were operated upon on the first day required at least a second operative procedure. The median length of stay in the ICU was 4 days (range: 1–22 days) with a median hospital length of stay of 8.5 days (range: 1–49 days).
DISCUSSION
The percentage of severely injured patients (ISS of ≥ 16) represented 12.5% of the total seen in the Boston attack was far less than that in other terrorist bombings, reported to be as high as 28.7%.6,7 Similar open-air bombing in the Israeli experience has been described to carry a lower overall mortality (7.5%) than that in closed spaces (49%).6,7 Burns, amputations, and open fractures have been far more commonly reported in the fatally injured people than in survivors.6,7 The overall mortality rate of 3/281 (1.0%) in this event was low, and all deaths occurred at the scene, none of whom suffered any form of amputation.
The lower mortality in the Boston bombing may be explained by the ground level location of the open-air bomb and lower grade explosive materials resulting in a fewer number of patients with high ISS scores. There was an absence of the extreme pressure changes and blast wave seen in the military-grade IEDs of Iraq and Afghanistan that tear apart armored vehicles and dismounted personnel with devastating consequences.8–12
The primary blast injury results from the pressure changes induced from the explosion and present as injury to organs with contained air or air-fluid interfaces.8,13 The tympanic membrane is particularly prone to rupture at pressures of 2 to 5 psi.14 Our data demonstrate a total of 15 patients treated at our hospitals on the day of the bombing with recognized unilateral or bilateral tympanic membrane ruptures. We believe that this number is an underestimate of the total number given that close follow-up over time is critical to identify all that suffer this injury. Estimates of upward of more than 100 patients out of the 281 have been reported to have sustained tympanic membrane or inner ear damage (personal communication, Daniel Lee, MD).
The lung is the second most susceptible organ to primary blast injury. The pressure differentials generated across the fluid filled capillary network of the lung and the air-filled alveoli leads to direct injury with hemorrhage, edema, laceration, cavity formation, and a prominent bilateral infiltrate. There appear to be 2 individuals, 1 adult and 1 child, who suffered a pulmonary blast injury. There were no hollow viscus injuries in the survivors as a result of blast injury. The overpressurization most likely was very limited in scope as it approached the 50 to 80 psi required to produce extensive direct pulmonary injury in only 2 patients from the blast wave.15
The majority of injuries seen in the Boston bombing resulted from secondary blast injuries as projectiles formed from the disintegrating pressure-cookers with metallic ball bearings and nails packed into the device. The projectiles resulting from this explosive device, although not completely accurate in a semantic sense, are often referred to as shrapnel in common parlance and served as the wounding agent in the overwhelming majority of cases. The fact that the majority of our patients had evidence for external injuries is a testament to the damage wrought by the secondary blast injury.16,17
Some terrorist bombings, termed suicide bomb attacks, involve the explosive charge strapped to the bombers themselves.18 In that event, disintegrated parts of the bomber become airborne projectiles and may result in secondary injury to personnel. This introduces the prospect of infectious complications resulting from airborne viral particles.18 All of our patients seen with evidence for external injury were screened for evidence of preexisting hepatitis B antibodies and treated accordingly.
Given that this was an outdoor bombing, we did not see any injuries from structural collapse or human projectiles as reported in tertiary blast effects.1,3
Prehospital Response
The minimal number of patients who had disaster tags applied (0.8%) and the short duration of scene departure after the blast to arrival in the ED (median 11 minutes) support an overall scoop and run policy and are consistent with the practice in other parts of the world after blast events.19–21 Airway control, needle decompression of the tension pneumothorax, and placement of a tourniquet in the appropriate situation are all that are needed at the scene of a multiple casualty event to expedite safe evacuation of the casualties.22–24 The preponderance of wounds in the lower extremity resulted in 31 (24.4%) patients with evidence for exsanguinating hemorrhage from those wounds. Eight-three percent of those patients with exsanguinating lower extremity wounds had a tourniquet applied in the field. It was unclear from the data analysis whether the type of tourniquet employed was of the improvised variety or a commercially available type, who in the field might have placed the device, and whether or not it was properly applied. Historically, the tourniquet has enjoyed a mixed review over the millennia.25 It was not until Drs Frank Butler, John Kragh, and John Holcomb and a multitude of military medics and nurses addressed the issue of prehospital care of the military injuries based on data from Operation Iraqi Freedom that the tourniquet became accepted practice.22–28 It has been reported that up to 2000 US military lives have been saved through tourniquet use.25,28 Appropriate tourniquet use for the control of arterial hemorrhage in the urban environment where the transport times are short is a very acceptable practice and saves lives. In our study of the Boston bombing, the prehospital data are inadequate to draw any new conclusions about the role of the tourniquet from this event. We remain staunch advocates of prehospital tourniquet use based on the recent well-documented extensive military experience.
The distribution of patients to the trauma centers in terms of absolute numbers and high ISS (>16) for the most part was equitable. There was no statistical difference (data not shown) because the numbers were small. Closer inspection reveals that one center that received 6 severely injured patients was in close proximity to another that received no severely injured patients suggesting that the distribution could have been more equitable. It is well documented that a single level I institution overwhelmed with mass casualties transforms it from a functional level I trauma unit into a dysfunctional one with a higher mortality rate hence this practice must be avoided.29 Particular attention to the even distribution of multiple casualties in the prehospital setting is critical to maintain smooth functioning of the trauma centers
Hospital ED Response
The ability to care for the influx of multiple patients at one time is predicated upon the ability of hospital personnel to evacuate the ED of the existing patients. At 3 pm, all of the EDs were near or over capacity. Because of the marathon, all of the area hospitals had their Hospital Incident Command System centers up and running, which facilitated the mobilization of the emergency response and rapid decompression of the EDs in preparation for the anticipated patient surge. All inpatient services were notified of the need for rapid triage of those patients in the ED and sent those resources to the ED to facilitate with that process.
In all of the trauma centers, the most senior trauma surgeons collaborated with the emergency medicine leaders in the triage of the trauma patients. These surgeons took on the role of the triage team leader for the more severely injured and assembled care teams that took stock of the resources available and opened immediate communication with the surgical subspecialties, anesthesia, and the operating rooms. All elective operations underway were completed and no new cases started after 3 pm until more information became available as to the expected number of injured patients. Triage of the “walking wounded” through another access in the ED or care location in the ED was not practiced as has been suggested by others.30
In the ED, emergency airway control was obtained in 12 (9.5%), transfusion started in 15 (11.8%), and most interventions characteristic of the care of the multiply injured trauma patient were limited. No surgical airways were needed most likely because of the infrequent finding of massive head or facial trauma more characteristic of high-explosive injuries. No chest tubes were placed, consistent with the infrequency of chest injuries seen whether by projectiles or from blast effect. The lack of skeletal traction and fasciotomies is consistent with a brief length of stay in the ED (median 45 minutes) for those taken directly to the OR for the lower extremity wounds. The majority of these wounds were major soft tissue defects in which fasciotomies might not be necessary as the compartments were widely decompressed through major tissue defects and the time sequence from injury to operating room was truncated.
Routine use of plain radiographs in trauma care has been an essential component of teaching in Advanced Trauma Life Support; however, recently the role of cervical spine films has been called into question.31 Raja et al32 reported extensive use of radiographic studies in their experience in a level III military hospital after multiple casualty events including CT scans and plain films. In our experience, about 25% to 50% of the patients received chest films, pelvic films, and FAST examinations in the ED. A few specific head CTs were done for obvious mental status changes or evidence for penetrating cranial wounds. Only 25% of the patients in our cohort required CT scans in the ED, consistent with MCIs reported elsewhere.33,34 This was a reflection of the preponderance of lower extremity injuries and the absence of tertiary blast injury in an outdoor bombing event.
Seventy-five (59.1%) patients were admitted to the hospital on the day of the bombing. The other 52 patients were seen in the ED and discharged to home. Forty-five (60%) of the admitted patients were transferred directly from the ED to the operating room. This is standard practice at a number of the trauma centers for life-threatening exsanguinating injuries. The median length of stay for all patients in the ED was 106 minutes (range: 10–481 minutes), whereas those admitted to the operating room had a median length of stay in the ED of 45 minutes. The ability to predict the total volume of patients and possible additional bombs forced the teams to identify those patients in need of immediate operations and those who had an operative injury but could wait for more information to determine their position in the cue. This might explain the broad range of dwell times in the ED for those patients who required urgent operative intervention.
Only a small percentage (14.7%) of patients required transfer directly into the ICU from the ED (median time of 87 minutes). A majority of the operative cases were cared for in the ICUs postoperatively for respiratory support and wound care. Although ICU resources were needed for many patients, there was sufficient time to move existing patients out of those occupied beds turn over the rooms and increase the number of nursing staff to prepare for the victims.
Initial Operating Room Response
Damage control surgery involving arrest of bleeding, completion of amputations, placement of external fixators, soft tissue debridement, and removal of foreign bodies was the standard approach as reported after bombings across the world.35,36 Eighteen percent of the patient cohort had injuries to the face and neck, with only 2 patients requiring operative intervention with neurological surgery for removal of foreign bodies. This is in stark contrast to the reports from Israel and Madrid, where head injuries were the most frequent location of penetrating wounds and reported in up to 54.5% of patients.17,36,37 This difference lies in the location and power of the bombs. The chest location of the bomb in a lone suicide bomber tends to disperse the projectiles at a higher level than ground level, and the closed site bombing in a bus or train tends to involve victims who are seated leading to more direct brain injury as the head is closer to the location of the device that is hidden beneath a seat or again strapped to the bomber.
The majority of patients presented with external injury and the “peppering” of the skin from multiple secondary projectiles. The combination of subcutaneous hemorrhage, abrasions, and lacerations has been described before as a characteristic triad of cutaneous injury in explosion victims.38 The majority of our patients presented with a variety of extremity injuries. The mechanism of injury from an explosion may result from the blast wave but more commonly from penetrating fragments resulting in cutaneous wounds, soft tissue avulsions, and bony fractures.9,17,35,37,39 Removal of debris, debridement of devitalized tissue, and delayed closure of these traumatic wounds have been the mainstay of therapy for decades. Well-vascularized flaps for the closure of soft tissue defects have been established as an effective method for closure of large soft tissue defects.5
Vascular injuries comprise about 4.7% of injuries in the recent conflicts in Iraq and Afghanistan40 and have been reported in 4.0% of terrorist attacks in Israel.6 The most significant penetrating vascular injuries are often associated with large soft tissue defects and bony fractures.41–43 Although vascular consultation was required in many of our cases, the number of specialized vascular reconstructions was limited. Mandatory fasciotomies are essential to reduce the incidence of compartment syndrome in those patients with ischemia-reperfusion, crush injury, hypotension, and/or venous ligation.43
The traumatic amputation at the scene of a bombing has been associated with very poor survival. Almogy et al35 reported on 74 patients with traumatic amputation in Israel with 63 (85.1%) deaths. Likewise, there were no survivors among the victims who presented with traumatic amputations after the terrorist bombing of the USS Cole off the coast of Yemen in October 2000.44 None of the 3 fatalities at the scene of the Boston bombing had an amputation.
Major limb amputation is reserved for either a life-threatening limb injury or one in which there is no reasonable success for salvage despite the best surgical efforts. On the day of the bombing, 12 patients (14 limbs) underwent either above or below knee lower extremity amputations. These were staged procedures with the surgical wounds left widely open incorporating a strategy to return at a later date for definitive therapy.45 There were 10 patients with below knee amputations, 3 with above knee amputations, and 2 patients with bilateral amputations. Forty-seven (87%) of the patients who underwent operative procedures on the day of the bombings required secondary operative procedures for definitive orthopedic stabilization, soft tissue debridement, and coverage after the initial damage control surgery.
The final hospital disposition of the cohort of injured patients indicated that 44% were sent to rehabilitation consistent with the extent of complicated lower extremity fractures and soft tissue reconstruction. Many (54.7%) were discharged to home with and without services, and only a small percentage (1.3%) required long-term care. In general, this is a reflection of the relatively young age of the injured patients and the preponderance of lower extremity injuries.
Boston’s first responder community, prepositioned at the finish line, set in motion the infrastructure of personnel to initiate the scene management of the response to the multiple casualty incident. The formal security and recognition of the Boston Marathon as a global event made this a desirable target for the misdirected but at the same time set in place monitoring devices at the starting and finish line to search for biologic or radiation hazards. There was no evidence at the time of the bombing that we were faced with these hazards. The streets surrounding the marathon were normally cordoned off for the runners, spectators, and the medical tent. This allowed some semblance of traffic control and easier evacuations in contrast to the traffic during a normal workday.
The proximity of 5 level I adult and 4 pediatric trauma centers only minutes after the bombings and the dedication of the American College of Surgeons to endorse the programs for the care of trauma patients in each of these centers established a favorable medical environment in Boston to manage the influx of a large number of patients in short order.46,47 Had the event occurred in a city or town with fewer medical services available, the outcomes may have been very different.
The timing of the bombing could not have been more favorable with a relatively light operative day, at the time of nursing shift change, and with Hospital Incident Command System and surgical teams already in place. A plethora of head, chest, and abdominal injuries would require more operative demand of the general, trauma, and neurological surgeons as well as radiology and the blood bank and may not have resulted in as many favorable outcomes. There was a notable lack of penetrating neurological injuries with the attendant guarded outcomes.10
The trauma response at each hospital, coordinated with the prehospital providers, did not occur in a vacuum. The training and drills since the terrorist events of 9/11 have been outlined in detail in other reports.2,48–50 These advantages allowed the trauma teams to practice as they would every day with the same multidisciplinary communication and team-based approach for each patient. The communication between the trauma and orthopedic surgeons with the ED and anesthesiologists ensured smooth patient transitions between prehospital, ED, and the operating rooms.
Security at the event was high with members of the Boston Police, Massachusetts State Police, Federal Bureau of Investigation, and reservist troops in place. In many of the hospitals, that level of security continued throughout the day and night. The Indian experience of potential secondary attacks on hospitals was responsible for this heightened response. We would encourage health care facilities to incorporate their local security agencies to participate in drills and form close alliances with the military, Federal Bureau of Investigation, State Police, and SWAT teams to allow seamless understanding of the simultaneous needs of the caregivers and the security forces.1,26,35,45
The volume of patients presenting to any one ED could easily overwhelm the clinical services of that hospital and convert a multiple casualty event into a mass casualty event unless the distribution of patients from the field is monitored carefully. The volume of patients at one time easily overwhelmed the registration practice at the hospitals with the current computer entry systems. The tracking registration system in some facilities is done ahead of time with registration packets organized by the patient number above the term “unidentified male or female.” In some cases, the patients were members of the same family with shared last names. In the current system, patient identification differed by one medical record number introducing the risk of a clerical error when tracking laboratory values, radiographic studies, and coordinating operative care. A corrective action includes changing the unidentified name to that of a state, town, city, or color so as to create a more obvious difference between patients. Other solutions to this uniform problem have been outlined in prior publications.11,50
The residents and fellows from all specialties responded admirably yet this event has underscored the need to incorporate disaster management into their formal training in an effort to make clear as to the roles of the various level trainees and to create a baseline of ED/Medical/Surgical workforce with knowledge of disaster management into the future.
The Future
There were 281 patients injured in Boston by a terrorist strike using 2 homemade IEDs. The ease with which widespread injury occurred should serve as a reminder that this is now potentially a part of daily life in the United States and across the globe. It is virtually impossible to predict the nature and location of the next event(s); however, it is clear that we remain at risk across the world.
All health care facilities should perform a gap analysis on their current disaster plans to determine next steps in an effort to minimize morbidity and mortality in the next mass casualty event. The importance of reevaluation, training, and preparation cannot be emphasized enough. Continued collaboration to identify best practices across the globe and to improve the medical response will serve as the best method for successful outcomes until a time comes when terror is marginalized by the citizens of the world and these events are no longer a threat.
Acknowledgments
The authors thank the following persons for their support: Chris Troyanos, Medical Services Director, Boston Athletic Association; Lynn Simpson, REDCap Administrator, Brigham and Women’s Hospital; Kathleen Allen, Senior Data Coordinator, Brigham and Women’s Hospital, Trauma and Burn Program; Kerri B. Carlson, MBA, Administrative Director, Trauma and Burn Program, Brigham and Women’s Hospital; Prof. Kobi Peleg, PhD, MPH, Tel Aviv University, Head of the Department of Disaster Medicine, School of Public Health, The Gertner Institute; Sophia Dyer, MD, Medical Director of Boston EMS; The One Fund Boston; and Daniel Lee, MD, Director of the Pediatric Ear, Hearing and Balance Center, Massachusetts Eye and Ear Infirmary.
Footnotes
Disclosure: The authors declare that there are no conflicts of interest and that no funding was received in support of this manuscript.
References
- 1.Shariat S, Stennies G, Waxweiler R, et al. Physical injuries and fatalities resulting from the Oklahoma City bombing. JAMA. 1996;276:382–387. [PubMed] [Google Scholar]
- 2.Cushman JG, Pachter HL, Beaton HL, et al. Two New York City hospitals’ surgical response to the September 11, 2001, terrorist attack in New York City. J Trauma. 2003;54:147–154. doi: 10.1097/00005373-200301000-00018. discussion 154–155. [DOI] [PubMed] [Google Scholar]
- 3.Feliciano DV, Anderson GV, Jr, Rozycki GS, et al. Management of casualties from the bombing at the centennial Olympics. Am J Surg. 1998;6:538–543. doi: 10.1016/s0002-9610(98)00263-3. [DOI] [PubMed] [Google Scholar]
- 4.U.S. Department of Commerce. United States Census Bureau. [Accessed August 31, 2013]; Available at: http://quickfacts.census.gov/qfd/states/25/2507000.html.
- 5.Caterson EJ, Carty M, Weaver MJ, et al. Boston bombings: a surgical view of lessons learned from combat casualty care and the applicability to Boston’s terrorist attack. J Craniofacial Surg. 2013;24:1061–1067. doi: 10.1097/SCS.0b013e31829ff967. [DOI] [PubMed] [Google Scholar]
- 6.Kluger Y, Peleg K, Daniel-Aharonson L, et al. Israeli Trauma Group. The special injury pattern in terrorist bombings. J Am Coll Surg. 2004;199:875–879. doi: 10.1016/j.jamcollsurg.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 7.Leibovici D, Gofrit ON, Stein M, et al. Blast injuries: bus versus open-air bombings—a comparative study of injuries in survivors of open-air versus confined-space explosions. J Trauma. 1996;41:1030–1035. doi: 10.1097/00005373-199612000-00015. [DOI] [PubMed] [Google Scholar]
- 8.Philips YY. Primary blast injuries. Ann Emerg Med. 1986;15:1446–1450. doi: 10.1016/s0196-0644(86)80940-4. [DOI] [PubMed] [Google Scholar]
- 9.Nelson TJ, Clark T, Stedje-Larsen ET, et al. Close proximity blast injury patterns from improvised explosive devices in Iraq: a report of 18 cases. J Trauma. 2008;65:212–217. doi: 10.1097/01.ta.0000196010.50246.9a. [DOI] [PubMed] [Google Scholar]
- 10.Ramasamy A, Harrisson SE, Clasper JC, et al. Injuries from roadside improvised explosive devices. J Trauma. 2008;65:910–914. doi: 10.1097/TA.0b013e3181848cf6. [DOI] [PubMed] [Google Scholar]
- 11.Hoskins JD, Graham RF, Robinson DR, et al. Mass casualty tracking with air traffic control methodologies. J Am Coll Surg. 2009;208:1001–1008. doi: 10.1016/j.jamcollsurg.2009.02.044. [DOI] [PubMed] [Google Scholar]
- 12.Ficke JR, Eastridge BJ, Butler FK, et al. Dismounted complex blast injury report of the army dismounted complex blast injury task force. J Trauma Acute Care Surg. 2012;73:S520–S532. [Google Scholar]
- 13.DePalma RG, Burris DG, Champion HR, et al. Blast injuries. N Engl J Med. 2005;352:1335–1342. doi: 10.1056/NEJMra042083. [DOI] [PubMed] [Google Scholar]
- 14.Jensen JH, Bonding P. Experimental pressure induced rupture of the tympanic membrane in man. Acta Otolaryngol. 1993;113:62–67. doi: 10.3109/00016489309135768. [DOI] [PubMed] [Google Scholar]
- 15.Katz E, Ofek B, Adler J, et al. Primary blast injury after a bomb explosion in a civilian bus. Ann Surg. 1989;209:484–488. doi: 10.1097/00000658-198904000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hiss J, Kahana T. Modern war wounds. In: Mason JK, Purdue BN, editors. The Pathology of Trauma. 3. London, UK: Edward Arnold; 2000. pp. 89–102. [Google Scholar]
- 17.Peleg K, Aharson-Daniel L, Michael M, et al. The Israel Trauma Group. Patterns of injury in hospitalized terrorist victims. Am J Emerg Med. 2003;21:258–262. doi: 10.1016/s0735-6757(03)00043-3. [DOI] [PubMed] [Google Scholar]
- 18.Eshkol Z, Katz K. Injuries from biologic material of suicide bombers. Injury. 2005;36:271–274. doi: 10.1016/j.injury.2004.06.016. [DOI] [PubMed] [Google Scholar]
- 19.Frykberg ER, Tepas JJ, 3rd, Alexander RH. The 1983 Beirut airport terrorist bombing. Injury patterns and implications for disaster management. Ann Surg. 1989;55:134–141. [PubMed] [Google Scholar]
- 20.Border JR, Lewis FR, Aprahamian C, et al. Panel: pre-hospital trauma cares-stabilize or scoop and run. J Trauma. 1983;23:708–711. [PubMed] [Google Scholar]
- 21.Waisman Y, Aharonson-Daniel L, Mor M, et al. The impact of terrorism on children: a two-year experience. Prehosp Disaster Med. 2004;19:370–371. doi: 10.1017/s1049023x00001114. [DOI] [PubMed] [Google Scholar]
- 22.Butler FK, Jr, Holcomb JB, Giebner SD, et al. Tactical combat casualty care 2007: evolving concepts and battlefield experience. Mil Med. 2007;172:1–19. doi: 10.7205/milmed.172.supplement_1.1. [DOI] [PubMed] [Google Scholar]
- 23.Shapira SC, Adatto-Levi R, Avitzour M, et al. Mortality in terrorist attacks: a unique modal temporal distribution. World J Surg. 2006;30:2071–2077. doi: 10.1007/s00268-006-0048-y. [DOI] [PubMed] [Google Scholar]
- 24.Peleg K, Michaelson M, Shapira SC, et al. Principles of emergency management in disasters. Adv Ren Replace Ther. 2003;10:117–121. doi: 10.1053/jarr.2003.50019. [DOI] [PubMed] [Google Scholar]
- 25.Kragh JF, Jr, Swan KG, Smith DC, et al. Historical review of emergency tourniquet use to stop bleeding. Am J Surg. 2012;203:242–252. doi: 10.1016/j.amjsurg.2011.01.028. [DOI] [PubMed] [Google Scholar]
- 26.Jacobs L, Wade D, McSwain NE, et al. Hartford consensus: a call to action for THREAT, a medical disaster preparedness concept. J Am Coll Surg. 2014;218:467–475. doi: 10.1016/j.jamcollsurg.2013.12.009. [DOI] [PubMed] [Google Scholar]
- 27.Kragh JF, Walters TJ, Westmorland T, et al. Tragedy into drama: an American history of tourniquet use in the current war. J Spec Oper Med. 2013;13:5–25. doi: 10.55460/QN66-A9MG. [DOI] [PubMed] [Google Scholar]
- 28.Holcomb JB, McMullin NR, Pearse L, et al. Causes of death in U.S. Special Operations forces in the global war on terrorism: 2001–2004. Ann Surg. 2007;245:986–991. doi: 10.1097/01.sla.0000259433.03754.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rodoplu U, Arnold JL, Yucel T, et al. Impact of the terrorist bombing of Hong Kong Shanghai Bank Corporation headquarters and the British Consulate on two hospitals in Istanbul, Turkey in November 2003. J Trauma. 2005;59:195–201. doi: 10.1097/01.ta.0000171527.49354.8f. [DOI] [PubMed] [Google Scholar]
- 30.Staudenmayer K, Schecter WP. Civilian hospital response to mass casualty events: Basic principles. Bulletin J Am Coll Surg. 2007;92:16–20. [PubMed] [Google Scholar]
- 31.Khurana B, Stella M, Ledbetter MS, et al. Current role of lateral cervical spine radiograph: a case report. Emerg Radiol. 2011;18:161–163. doi: 10.1007/s10140-010-0912-9. [DOI] [PubMed] [Google Scholar]
- 32.Raja AS, Propper BW, Vandenberg SL, et al. Image utilization during explosive multiple casualty incidents. J Trauma. 2010;68:1421–1424. doi: 10.1097/TA.0b013e3181cf7d32. [DOI] [PubMed] [Google Scholar]
- 33.Frykberg ER. Medical management of disasters and mass casualties from terrorist bombings: how can we cope? J Trauma. 2002;53:201–212. doi: 10.1097/00005373-200208000-00001. [DOI] [PubMed] [Google Scholar]
- 34.Kluger Y, Mayo A, Soffer D, et al. Functions and principles in the management of bombing mass casualty incidents: lesson learned at the Tel-Aviv Souraski Medical Center. Eur J Emer Med. 2004;11:329–334. doi: 10.1097/00063110-200412000-00006. [DOI] [PubMed] [Google Scholar]
- 35.Almogy G, Luria T, Richter E, et al. Can external signs of trauma guide management? Lessons learned from suicide bombing attacks in Israel. Arch Surg. 2004;140:390–393. doi: 10.1001/archsurg.140.4.390. [DOI] [PubMed] [Google Scholar]
- 36.Einav S, Aharonson-Daniel L, Weissman C, et al. Israel Trauma Group. In-hospital resource utilization during mass casualty incidents. Ann Surg. 2006;243:533–540. doi: 10.1097/01.sla.0000206417.58432.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mellor SG, Cooper GJ. Analysis of 828 servicemen killed or injured by explosion in Northern Ireland 1970–84: the Hostile Action Casualty System. Br J Surg. 1989;76:1006–1010. doi: 10.1002/bjs.1800761006. [DOI] [PubMed] [Google Scholar]
- 38.Saukko P, Knight B. Knight’s Forensic Pathology. 3. London, UK: Arnold; 2004. Gunshot and explosion deaths; pp. 245–280. [Google Scholar]
- 39.Hull JB, Cooper GJ. Pattern and mechanism of traumatic amputation by explosive blast. J Trauma. 1996;40:S198–S205. doi: 10.1097/00005373-199603001-00044. [DOI] [PubMed] [Google Scholar]
- 40.Clouse WD, Rasmussen TE, Peck MA, et al. In-Theater management of vascular injury: 2 years of the Balad vascular registry. J Am Coll Surg. 2007;204:625–631. doi: 10.1016/j.jamcollsurg.2007.01.040. [DOI] [PubMed] [Google Scholar]
- 41.Wolf YG, Rivkind A. Vascular trauma in high-velocity gunshot wounds and shrapnel-blast injuries in Israel. Surg Clin North Am. 2002;82:237–244. doi: 10.1016/S0039-6109(03)00152-X. [DOI] [PubMed] [Google Scholar]
- 42.Gates JD. Penetrating wounds of the extremities: exploration, arteriography, duplex, or physical exam to rule out arterial injury? Orthopedic Review: Aspects of Trauma. 1994:10–12. [PubMed] [Google Scholar]
- 43.Taller J, Kamdar JP, Greene JA, et al. Temporary vascular shunts as initial treatment of proximal extremity vascular injuries during combat operations: the new standard of care at echelon II facilities? J Trauma. 2008;65:595–603. doi: 10.1097/TA.0b013e31818234aa. [DOI] [PubMed] [Google Scholar]
- 44.Langworthy MJ, Sabra J, Gould M. Terrorism and blast phenomena: lessons learned from the attack on the USS Cole (DDG67) Clin Orthop Relat Res. 2004;422:82–87. [PubMed] [Google Scholar]
- 45.Peranteau WH, Havens JH, Harrington S, et al. Re-establishing surgical care at Port-au-Prince General Hospital, Haiti. J Am Coll Surg. 2010;211:126–130. doi: 10.1016/j.jamcollsurg.2010.04.015. [DOI] [PubMed] [Google Scholar]
- 46.Mahoney EJ, Harrington DT, Biffl WL, et al. Lessons learned from a nightclub fire: institutional disaster preparedness. J Trauma. 2005;58:487–491. doi: 10.1097/01.ta.0000153939.17932.e7. [DOI] [PubMed] [Google Scholar]
- 47.Frykberg ER. Disaster and mass casualty management: a commentary on the American College of Surgeons position statement. J Am Coll Surg. 2003;19:857–859. doi: 10.1016/S1072-7515(03)00809-3. [DOI] [PubMed] [Google Scholar]
- 48.Walls RA, Zinner MJ. The Boston Marathon response: why did it work so well? Viewpoint. JAMA. 2013;309:2441–2442. doi: 10.1001/jama.2013.5965. [DOI] [PubMed] [Google Scholar]
- 49.Goralnick E, Gates JD. Perspective: we fight like we train. N Engl J Med. 2013;368:1960–1961. doi: 10.1056/NEJMp1305359. [DOI] [PubMed] [Google Scholar]
- 50.Kellerman AL, Peleg K. Perspective: lessons from Boston. N Engl J Med. 2013;38:1956–1957. doi: 10.1056/NEJMp1305304. [DOI] [PubMed] [Google Scholar]