Abstract
Background
This study aimed to explore the factors affecting the level of hope and psychological health status of patients with cervical cancer (CC) during radiotherapy.
Material/Methods
A total of 480 CC patients were recruited. Psychological distress scale, Herth hope index, functional assessment cancer therapy-cervix, and Jolowiec coping scale were used to conduct surveys on psychological distress, level of hope, quality of life (QOL), and coping style to analyze the factors affecting the level of hope and psychological health status of CC patients.
Results
The morbidity of significant psychological distress in 480 CC patients during radiotherapy was 68%, and the main factors causing psychological distress were emotional problems and physical problems. During radiotherapy, most patients had middle and high levels of hope, and the psychological distress index of patients was negatively correlated with the level of hope. The QOL of CC patients during radiotherapy were at middle and high levels, and the QOL was positively correlated with confrontment, optimism, appeasement, and self-reliance, but it was negatively correlated with predestination and emotional expression.
Conclusions
For CC patients during radiotherapy, the morbidity of psychological distress was high, but they were at middle and high levels of hope.
MeSH Keywords: Hope; Quality of Life; Radioimmunotherapy; Signal Detection, Psychological; Uterine Cervical Neoplasms
Background
Cervical cancer (CC), as one of the most common malignancy cancer in females, occurs at the junction of the columnar epithelial cells of the cervical canal and the squamous epithelial cells of the cervical vagina or the transitional zone [1]. Notably, with approximately 530,000 new cases and 275,000 deaths each year, CC is still one of the leading causes of cancer among women worldwide [2]. Principally, persistent infection with oncogenic human papillomavirus (HPV) is regarded as the main cause of CC, and early gene coding proteins of HPV can lead virus to tumorigenesis in host cells [3]. Furthermore, other risk factors such as precocious intercourse, multiple sexual partners, higher number of pregnancies, and smoking are involved in the incidence of CC [4]. With the deep understanding of the pathology of CC, the treatments of CC mainly include surgery, chemotherapy, radiotherapy, concurrent radiochemotherapy, and targeted therapy [5,6].
As a major treatment for CC, radiotherapy can be widely used in each stage due to its wide range and high cure rate [7]. However, radiotherapy for CC could result in negative effects including physical conditions, psychology, and social functions to different degrees [8]. Additionally, a study reported that one-third of patients had obvious menopause symptoms, 60% had a major decline in the quality of sex life, and more than 50% suffered from hematuria, frequent micturition, bloody stool, and pain [9]. All these adverse reactions bring much psychological pain and negative emotions, which affect the treatment progress and prognosis of patients [10]. Hope, an intrinsic mental power, not only gives patients confidence and courage, but also is a key factor of treatment process to affect patients’ behavior and coping style, which further helps patients adapt to the disease, overcome difficulties, and improve the quality of life (QOL) [11]. Previous studies indicated that the level of hope was significantly correlated with psychological development and physical condition [7,8]. Therefore, the aim of our study was to analyze the factors affecting the level of hope and psychological health status of patients with CC during radiotherapy.
Material and Methods
Ethics statement
This study has been approved by Ethics Committee of People’s Hospital of Guangxi Zhuang Autonomous Region, and all patients and their families provided signed consent. All procedures in this study strictly complied with the guidelines and principles of the Declaration of Helsinki.
Subjects
A total of 480 CC patients aged 30–60 years old (mean age of 47.5±7.9 years old) admitted in the Department of Radiotherapy of People’s Hospital of Guangxi Zhuang Autonomous Region from January 2012 to December 2016 were enrolled in this study. Inclusion criteria were: patients diagnosed with CC via cervical scraping smear and biopsy; patients with complete clinic data; patients with normal hearing and communication skills; patients with the ability to fill out the scale independently. Exclusion criteria were: patients with local recurrence or other malignant tumors; patients with mental disease or intellectual disability; patients who are unable to fill out the scale. All the basic information of 480 CC patients during radiotherapy is provided in Table 1.
Table 1.
The basic characteristic of 480 CC patients during radiotherapy.
| Characteristics | Patient (person) | Characteristics | Patient (person) |
|---|---|---|---|
| Age (year) | Household income (RMB/month) | ||
| <45 years | 144 | ≤1500 | 123 |
| ≥45 years | 336 | 1500~3000 | 122 |
| Educational level | ≥3000 | 235 | |
| ≤ High school | 304 | Physical exercise time (hour/week) | |
| ≥ University | 176 | ≤3 | 236 |
| Marital status | >3 | 244 | |
| Single | 49 | Medical cost source | |
| Married | 431 | Full medical insurance | 40 |
| Work condition | Partial medical insurance | 344 | |
| Employed | 224 | Self-funded | 96 |
| Unemployed | 256 | Clinical stage | |
| Religion | I | 128 | |
| Yes | 108 | II | 232 |
| No | 372 | III | 120 |
Psychological distress scale
The survey was performed based on the distress thermometer (DT) recommended by National Comprehensive Cancer Network (NCCN) [12]. This scale consists of DT and problem lists (PL). The score of DT ranged from 0 to 10 (a total of 11 standards) in which 0 was no pain, 1~3 was mild pain, 4~6 was moderate pain, 7~9 was severe pain, and 10 was extreme pain. In this study, DT ≥4 was considered as significant psychological distress. PL included 5 domains with a total of 40 items: practical problems (6 items), communication problems (4 items), emotional problems (9 items), physical problems (20 items), and spiritual/religious problems (1 item), and each item can be answered by “Yes” or “No”. Questionnaires were issued and retrieved by professionally trained nurses, and all the contents were completed by patients independently.
Herth hope index (HHI)
The survey was carried out according to HHI translated and introduced by Zhao Haiping [13]. This scale was divided into temporality and future (T), positive readiness and expectancy (P), and interconnectedness (I), and has a total of 12 items whose results were in the form of scores: 1~4 scores meant strongly disagree, disagree, agree, and strongly agree, respectively. Here, 12~23 was defined as low level; 24~35 was defined as middle level; and 36~48 was defined as high level. Questionnaires were issued and retrieved by professionally trained nurses, and all the contents were completed by patients independently.
Functional assessment cancer therapy-cervix (FACT-Cx)
The survey was conducted according to FACT-Cx, which was translated into Chinese and tested by Wan Chonghua [14]. FACT-Cx consisted of functional assessment cancer therapy-general (FACT-G) and cervix cancer scale (CxCS), which involved 5 fields (a total of 42 items), including physical status (7 items), society/family status (7 items), emotional status (6 items), functional status (7 items), and affixation attention (15 items). The score of each item ranged from 0 to 4 and a higher score showed more agreement. The reverse item was scored as 4 minus the actual score, and an unanswered item was scored as missing. The scoring method for each field was: (the sum of total scores in this field × the number of items)/the number of items actually answered. Here, a higher total score indicates better QOL. Questionnaires were issued and retrieved by professionally trained nurses, and all the contents were completed by patients independently.
Coping style scale (JCS)
The assessment was performed based on the JCS developed by Jalowiec [15]. This questionnaire included 8 parts with a total of 60 items: confrontment (10 items), evasion (13 items), optimism (9 items), predestination (4 items), emotional expression (5 items), appeasement (7 items), support (5 items), and self-reliance (7 items). Each item was scored as 0 to 3, and a higher score showed that more items were used. Questionnaires were issued and retrieved by professionally trained nurses, and all the contents were completed by patients independently.
Statistical analysis
The data collected in the questionnaires were analyzed using SPSS 20.0 (SPSS Inc., Chicago, IL, USA). Measurement data are expressed as mean±standard deviation (SD) (x±s). The comparison between 2 groups was analyzed by the independent-samples t test, and one-way analysis of variance (ANOVA) was used in comparison among groups. Correlation analysis was carried out using Pearson correlation analysis. P<0.05 was considered statistically significant.
Results
Psychological distress index of CC patients during radiotherapy and 5 related factors
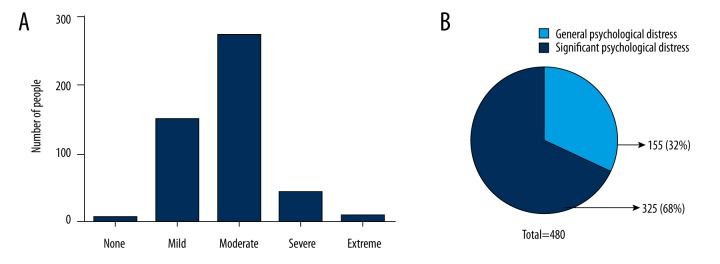
The average score of psychological distress index in 480 CC patients during radiotherapy was 4.33±1.95. As shown in Figure 1, 6 patients had no pain, 149 patients had mild pain, 273 paints had moderate pain, 43 patients had severe pain, and 9 patients had extreme pain. Therefore, the morbidity of significant psychological distress (DT ≥4) was 68%, and 356 patients needed to be further assessed and treated by professional psychologists. In addition, the survey results of related factors causing psychological distress in 480 patients (Table 2) revealed that practical problems accounted for 80%, emotional problems for 97%, physical problems for 96%, communication problems for 29%, and spiritual/religious problems for 8%.
Figure 1.
Distribution of psychological distress degree in CC patients during radiotherapy. CC – cervical cancer.
Table 2.
Five factors causing psychological distress in CC patients.
| Item | Patients (person) | Percentage (%) | |
|---|---|---|---|
| Practical problem | 1 Economic problem | 265 | 55 |
| 2 No time to take care of the children/the elder | 201 | 42 | |
| 3 No time and energy to do housework | 129 | 27 | |
| 4 Surroundings | 86 | 18 | |
| 5 Work/school | 80 | 17 | |
| 6 Transportation | 64 | 13 | |
| Emotional problem | 1 Worry | 331 | 69 |
| 2 Nervous | 173 | 36 | |
| 3 Depressed | 163 | 34 | |
| 4 Sad | 144 | 30 | |
| 5 Fear | 125 | 26 | |
| 6 Sleep | 120 | 25 | |
| 7 Loss of interest in normal activities | 110 | 23 | |
| 8 Lonely | 91 | 19 | |
| 9 Memory deterioration/inattention | 82 | 17 | |
| Communication problem | 1 Get along with the elder and children | 73 | 15 |
| 2 Get along with relatives and friends | 72 | 15 | |
| 3 Get along with companion | 71 | 15 | |
| 4 Get along with medical workers | 48 | 10 | |
| Physical problem | 1 Feed | 267 | 56 |
| 2 Fatigue | 263 | 55 | |
| 3 Dyspepsia | 203 | 42 | |
| 4 Pain | 153 | 32 | |
| 5 Astriction | 138 | 29 | |
| 6 Nausea | 132 | 28 | |
| 7 Bath/dress | 116 | 24 | |
| 8 Breath | 108 | 23 | |
| 9 Limited physical activity | 104 | 22 | |
| 10 Appearance/shape | 102 | 21 | |
| 11 Dry skin | 67 | 14 | |
| 12 Dizzy | 57 | 12 | |
| 13 Diarrhea | 38 | 8 | |
| 14 Numb hand/foot | 34 | 7 | |
| 15 Fever | 29 | 6 | |
| 16 Sex | 26 | 5 | |
| 17 Changed micturition | 28 | 6 | |
| 18 Edema | 20 | 4 | |
| 19 Dry nose/hyperemia | 18 | 4 | |
| 20 Oral pain | 5 | 1 | |
| Spiritual/religious problem | 37 | 8 |
Level of hope in CC patients during radiotherapy
As shown in Figure 2, the total HHI score of patients during radiotherapy was 31.78±4.60, in which T score was 10.05±2.70, P score was 8.21±2.88, and I score was 13.51±2.11. Among 480 patients, 124 patients (25.83%) had high level of hope, 341 patients (71.04%) had middle level of hope, and 15 patients (3.13%) had low level of hope. Therefore, the total was at middle and high levels of hope.
Figure 2.
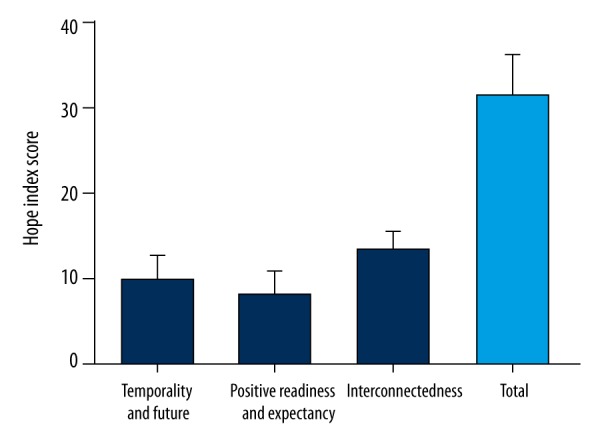
HHI score of CC patients during radiotherapy. HHI – herth hope index; CC – cervical cancer.
Correlation analysis between psychological distress index/related factors and level of hope
There were significant differences between the different psychological distress indexes and the level of hope in CC patients during radiotherapy (all P<0.05): patients with no pain and mild pain had high level of hope, patients with moderate and severe pain had middle level of hope, and patients with extreme pain had low level of hope. The overall level of hope of CC patients was decreased with the increase of psychological distress index, suggesting that the level of hope was negatively correlated with psychological distress index (r=−0.736, P<0.05). Table 3 shows that patients with different psychological distress factors had significantly different levels of hope (P<0.05). Patients with psychological distress caused by practical, emotional, and physical problems had middle level of hope, while patients with psychological distress caused by communication and spiritual/religious problem had high level of hope.
Table 3.
Level of hope score for patients with different psychological distress indexes and related factors.
| Total score of level of hope (x±s, score) | P | r | |
|---|---|---|---|
| Psychological distress index | <0.001 | −0.736 | |
| None pain | 42.17±2.32 | ||
| Mild pain | 35.30±3.89 | ||
| Moderate pain | 31.00±2.76 | ||
| Severe pain | 25.09±2.34 | ||
| Extreme pain | 21.78±3.23 | ||
| Related factors of psychological distress | <0.001 | ||
| Practical problem | 30.51±3.99 | ||
| Emotional problem | 31.75±6.13 | ||
| Communication problem | 36.31±4.20 | ||
| Physical problem | 31.55±2.67 | ||
| Spiritual/religious problem | 38.16±4.86 |
Level of hope of patients with different basic characteristics
There were significant differences in level of hope among CC patients with different age, marital status, household income, medical cost source, and clinical stage (all P<0.05), but the levels of hope were not significantly different among CC patients with different educational level, work condition, religion, and physical exercise time (all P>0.05). As shown in Table 4, patients had higher level of hope when they were older with higher household income and lower clinical stage. Moreover, patients with full medical insurance had better level of hope than those with partial medical insurance and self-funded, and the levels of hope of married patients were better than unmarried ones.
Table 4.
Comparison of level of hope for patients with different basic characteristics.
| Characteristics | Total score of level of hope (x±s, score) | P |
|---|---|---|
| Age | <0.001 | |
| <45 years | 30.18±5.73 | |
| ≥45years | 32.46±3.83 | |
| Educational level | 0.424 | |
| ≤ High school | 31.65±4.46 | |
| ≥ University | 31.99±4.53 | |
| Marital status | <0.001 | |
| Single | 25.39±2.68 | |
| Married | 32.50±4.19 | |
| Work condition | 0.924 | |
| Employed | 31.73±4.56 | |
| Unemployed | 31.69±4.64 | |
| Household income (RMB/month) | <0.001 | |
| ≤1500 | 27.30±2.63 | |
| 1500~3000 | 29.46±3.03 | |
| ≥3000 | 31.79±3.00 | |
| Medical cost source | 0.001 | |
| Full medical insurance | 36.63±4.38 | |
| Partial medical insurance | 32.07±4.04 | |
| Self-funded | 28.69±4.47 | |
| Religion | 0.648 | |
| Yes | 31.60±4.91 | |
| No | 31.83±4.51 | |
| Physical exercise time (hour/week) | 0.793 | |
| ≤3 | 31.72±4.61 | |
| >3 | 31.83±4.60 | |
| Clinical stage | 0.001 | |
| I | 35.34±3.65 | |
| II | 31.27±4.23 | |
| III | 28.95±3.74 |
QOL of CC patients during radiotherapy
The total FACT-Cx score of CC patients during radiotherapy was 119.39±9.37, in which physical status was 21.32±4.29, society/family was 20.92±3.89, emotional status was 17.81±4.46, functional status was 17.23±2.18, and affixation attention was 42.10±3.37 (Figure 3), indicating that the overall QOL was at middle and high levels.
Figure 3.
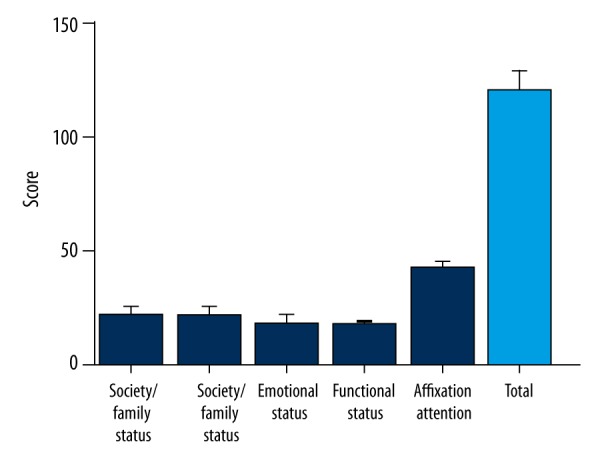
FACT-Cx score of CC patients during radiotherapy. FACT-Cx – functional assessment cancer therapy-cervix; CC – cervical cancer.
Correlation analysis between QOL and coping style for CC patients during radiotherapy
Figure 4 shows that the total coping style score of 480 CC patients during radiotherapy was 110.94±0.94. A total of 3 coping styles – optimism, predestination, and support – were associated with higher scores, and emotional expression score was the lowest. Furthermore, the total QOL of CC patients during radiotherapy was positively correlated with confrontment, optimism, appeasement, support, and self-reliance (all P<0.05), but was negatively correlated with predestination and evasion (both <0.05). In addition, physical status score had a significant positive correlation with confrontment, appeasement, support, and self-reliance, while physical status score was negatively correlated with evasion, predestination, and emotional expression. Similarly, functional status score and emotional status score were negatively correlated with emotional expression (all P<0.05) (Table 5).
Figure 4.
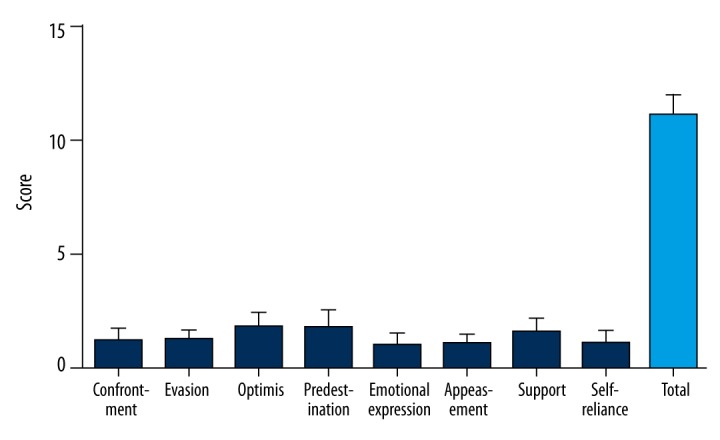
Coping style score of CC patients during radiotherapy. CC – cervical cancer.
Table 5.
Correlation between QOL and coping style for CC patients during radiotherapy.
| Coping style | Physical status | Society/family status | Emotional status | Functional status | Affixation attention | Overall situation |
|---|---|---|---|---|---|---|
| Confrontment | 0.092* | 0.003 | 0.035 | 0.051 | 0.060 | 0.094* |
| Evasion | −0.092* | −0.024 | −0.038 | −0.048 | −0.050 | −0.099* |
| Optimism | 0.097 | 0.035 | 0.033 | 0.051 | 0.050 | 0.104* |
| Predestination | −0.096* | −0.018 | −0.028 | −0.047 | −0.051 | −0.094* |
| Emotional expression | −0.094* | −0.009 | −0.026* | −0.043* | −0.045 | −0.086 |
| Appeasement | 0.099* | 0.017 | 0.031 | 0.051 | 0.055 | 0.099* |
| Support | 0.094* | 0.021 | 0.032 | 0.052 | 0.050 | 0.097* |
| Self-reliance | 0.101* | 0.014 | 0.025 | 0.052 | 0.041 | 0.090* |
Means P<0.05.
Discussion
Although radiotherapy is the major therapy for CC, it usually causes diarrhea, appetite loss, frequent micturition, painful urination, burning vagina, and fatigue constipation [16–18]. Other problems, such as the long duration of radiotherapy, interrupted sex life, and huge economic pressure, greatly troubled CC patients and often caused anxiety, fear, depression, and other psychological problems [7]. Therefore, this study aimed to explore the source of psychological distress, level of hope, and coping style to provide more positive guidance for CC patients during radiotherapy, which may improve their QOL and therapeutic effects.
In this study, the morbidity of significant psychological distress among 480 CC patients during radiotherapy was 68%, indicating that most CC patients suffered from psychological and spiritual pain during radiotherapy. Psychological distress is an unpleasant emotional expression involving h psychology and spirit, caused by a variety of reasons, which will further affect patient ability to cope with disease and the clinical manifestation and treatment of disease; all cancer patients will experience varying degrees of psychological distress [19,20]. In addition, we also found that emotional and physical problems were the main factors that cause psychological distress in CC patients. The main factor causing emotional problems may be uncertainty about disease; to some extent, patients do not understand the disease, lack related knowledge about diagnosis and treatment, and, especially, cannot predict therapeutic effects and prognosis, which all result in patient uncertainty [21]. In terms of physical problems, fatigue is the main factor, and previous studies reported that 90% of CC patients had cancer-related fatigue [22,23], which is a kind of extraordinary, lasting, subjective fatigue that disturbs normal functions and is related with cancer or cancer treatment; it disturbs self-care ability, functional status, QOL, and even aggravation [22].
Hope is a kind of multidimensional positive life power; in other words, it is an individual’s confident but uncertain expectation of a wonderful outcome [24]. This study demonstrated that CC patients during radiotherapy were at middle and high levels of hope, suggesting that although CC patients suffered from physical and psychological distress, most were still confident and hopeful about the future, which is consistent with the results of research by Gan Yanling et al. [25]. We also found that patients had higher levels of hope when they were older with higher household income and in lower clinical stage; patients with full medical insurance had better level of hope than those with partial medical insurance and self-funded, and the levels of hope of married patients were higher than unmarried ones. When compared with young CC patients, the older CC patients had less stress about the prognosis, such as changing femaleness, sex life disorder, relationship between wife and husband, and family harmony [26]. Patients with high household income had less psychological burden because of less economic pressure, while those at higher clinical stage were more difficult to cure, which may increase psychological pressures and reduce the level of hope via developing negative emotions like fear, despair, and tension [27]. Patients who do not have to pay all medical expenses themselves have less worry during treatment, which contributes to improved level of hope [28]. In addition, support may explain why married patients had better level of hope than unmarried ones, and Carpenter et al. reported that social support can benefit patients [29]. As the most important type of social support, marriage can make patients feel more support and care from family, which will improve their ability to cope with difficulties and increase their confidence in triumph over illness [24]. In this study, it was reported that patients’ psychological distress index was negatively correlated with level of hope, indicating that a higher level of hope could result in decreasing level of anxiety and depression for patients, thereby reducing the degree of psychological distress, which is beneficial to the treatment of disease [30].
As a subjective feeling, QOL is a multidimensional concept involving physical function, psychological function, and social function [31]. In this study, QOL of CC patients during radiotherapy were at middle and high levels. In addition, the correlation analysis of QOL and coping style found that QOL was positively correlated with confrontment, optimism, appeasement, and self-reliance, while QOL was negatively correlated with predestination and emotional expression. Coping style is the mental self-adaptation and psychological support mechanism that helps patients reduce mental stress, and it plays an important role in psychological health [32]. In terms of positive coping styles, confrontment, optimism, appeasement, and self-reliance are able to release psychological distress, thereby helping treatment and recovery [33], in which optimism helps patients to receive treatment positively and activate the immune system [34]. In addition, predestination and emotional expression were negative coping styles in which emotional expression manifests as losing temper, blaming others, and impulsiveness; however, these behaviors and emotions cannot change the status quo and reduce stress at all, but rather affect their relationship with others so as to result in psychological burden and damage to health [35].
Conclusions
To sum up, our study supports that for CC patients during radiotherapy, the morbidity of psychological distress was rather high, but they were at middle and high levels of hope. Moreover, a positive and healthy outlook is beneficial for patients to improve their QOL. Hope helps improve the QOL of CC patients during radiotherapy. Providing CC patients with good guidance about the level of hope and coping style can help patients understand the disease, reduce the psychological distress, and improve the level of hope so as to cope with disease positively.
Acknowledgments
The authors want to thank those who provided help in editing our paper.
Footnotes
Conflict of interests
The authors declare that there is no conflict of interests regarding the publication of this paper.
Source of support: This study was supported by a grant from the Health and Family Planning Commission Project of Guangxi Zhuang Autonomous Region (Z2014231)
References
- 1.Hang D, Yin Y, Han J, et al. Analysis of human papillomavirus 16 variants and risk for cervical cancer in Chinese population. Virology. 2016;488:156–61. doi: 10.1016/j.virol.2015.11.016. [DOI] [PubMed] [Google Scholar]
- 2.Sharma M, Bruni L, Diaz M, et al. Using HPV prevalence to predict cervical cancer incidence. Int J Cancer. 2013;132:1895–900. doi: 10.1002/ijc.27835. [DOI] [PubMed] [Google Scholar]
- 3.Lorin L, Bertaut A, Hudry D, et al. About invasive cervical cancer: A French population based study between 1998 and 2010. Eur J Obstet Gynecol Reprod Biol. 2015;191:1–6. doi: 10.1016/j.ejogrb.2015.04.007. [DOI] [PubMed] [Google Scholar]
- 4.Jiamset I, Hanprasertpong J. Risk factors for parametrial involvement in early-stage cervical cancer and identification of patients suitable for less radical surgery. Oncol Res Treat. 2016;39:432–38. doi: 10.1159/000447335. [DOI] [PubMed] [Google Scholar]
- 5.Rydzewska L, Tierney J, Vale CL, Symonds PR. Neoadjuvant chemotherapy plus surgery versus surgery for cervical cancer. Cochrane Database Syst Rev. 2012;12:CD007406. doi: 10.1002/14651858.CD007406.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kang YJ, O’Connell DL, Lotocki R, et al. Effect of changes in treatment practice on survival for cervical cancer: Results from a population-based study in Manitoba, Canada. BMC Cancer. 2015;15:642. doi: 10.1186/s12885-015-1624-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Serkies K, Jassem J. Concurrent weekly cisplatin and radiotherapy in routine management of cervical cancer: A report on patient compliance and acute toxicity. Int J Radiat Oncol Biol Phys. 2004;60:814–21. doi: 10.1016/j.ijrobp.2004.04.042. [DOI] [PubMed] [Google Scholar]
- 8.Wenzel L, DeAlba I, Habbal R, et al. Quality of life in long-term cervical cancer survivors. Gynecol Oncol. 2005;97:310–17. doi: 10.1016/j.ygyno.2005.01.010. [DOI] [PubMed] [Google Scholar]
- 9.Zi L, Juan W. [Investigation of the quality of life after radiotherapy of cervical cancer patient]. Modern Oncology. 2006;14:1180–81. [in Chinese] [Google Scholar]
- 10.Zhang J, Gao W, Wang P, Wu ZH. Relationships among hope, coping style and social support for breast cancer patients. Chin Med J (Engl) 2010;123:2331–35. [PubMed] [Google Scholar]
- 11.Western H. Altered living: Coping, hope and quality of life after stroke. Br J Nurs. 2007;16:1266–70. doi: 10.12968/bjon.2007.16.20.27573. [DOI] [PubMed] [Google Scholar]
- 12.Clover KA, Oldmeadow C, Nelson L, et al. Which items on the distress thermometer problem list are the most distressing? Support Care Cancer. 2016;24(11):4549–57. doi: 10.1007/s00520-016-3294-z. [DOI] [PubMed] [Google Scholar]
- 13.Chan KS, Li HC, Chan SW, Lopez V. Herth hope index: Psychometric testing of the Chinese version. J Adv Nurs. 2012;68:2079–85. doi: 10.1111/j.1365-2648.2011.05887.x. [DOI] [PubMed] [Google Scholar]
- 14.Salih SM, Albayrak S, Seo S, et al. Diminished utilization of in vitro fertilization following ovarian transposition in cervical cancer patients. J Reprod Med. 2015;60:345–53. [PMC free article] [PubMed] [Google Scholar]
- 15.Parvan K, Ahangar R, Hosseini FA, et al. Coping methods to stress among patients on hemodialysis and peritoneal dialysis. Saudi J Kidney Dis Transpl. 2015;26:255–62. doi: 10.4103/1319-2442.152409. [DOI] [PubMed] [Google Scholar]
- 16.du Toit GC, Kidd M. Prospective quality of life study of South African women undergoing treatment for advanced-stage cervical cancer. Clin Ther. 2015;37:2324–31. doi: 10.1016/j.clinthera.2015.08.018. [DOI] [PubMed] [Google Scholar]
- 17.Isik A, Deniz Firat Y, Peker K, et al. How could such a wide piece of tree root pass through the narrow pyloric orifice? An extremely rare case. Am J Case Rep. 2014;15:284–87. doi: 10.12659/AJCR.890713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Isik A, Peker K, Firat D, et al. Importance of metastatic lymph node ratio in non-metastatic, lymph node-invaded colon cancer: A clinical trial. Med Sci Monit. 2014;20:1369–75. doi: 10.12659/MSM.890804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hall AE, Sanson-Fisher RW, Carey ML, et al. Prevalence and associates of psychological distress in haematological cancer survivors. Support Care Cancer. 2016;24:4413–22. doi: 10.1007/s00520-016-3282-3. [DOI] [PubMed] [Google Scholar]
- 20.Hong J, Wei Z, Wang W. Preoperative psychological distress, coping and quality of life in Chinese patients with newly diagnosed gastric cancer. J Clin Nurs. 2015;24:2439–47. doi: 10.1111/jocn.12816. [DOI] [PubMed] [Google Scholar]
- 21.Lor M, Khang PY, Xiong P, et al. Understanding Hmong women’s beliefs, feelings, norms, and external conditions about breast and cervical cancer screening. Public Health Nurs. 2013;30:420–28. doi: 10.1111/phn.12043. [DOI] [PubMed] [Google Scholar]
- 22.Bower JE. Cancer-related fatigue – mechanisms, risk factors, and treatments. Nat Rev Clin Oncol. 2014;11:597–609. doi: 10.1038/nrclinonc.2014.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tomlinson D, Diorio C, Beyene J, Sung L. Effect of exercise on cancer-related fatigue: A meta-analysis. Am J Phys Med Rehabil. 2014;93:675–86. doi: 10.1097/PHM.0000000000000083. [DOI] [PubMed] [Google Scholar]
- 24.Yadav S. Perceived social support, hope, and quality of life of persons living with HIV/AIDS: A case study from Nepal. Qual Life Res. 2010;19:157–66. doi: 10.1007/s11136-009-9574-z. [DOI] [PubMed] [Google Scholar]
- 25.Yanling G, Huiling Z. [Correlations between expectations and anxiety and depression of cervical cancer patients]. Modern Clinical Training. 2014;13:29–32. [in Chinese] [Google Scholar]
- 26.Lammerink EA, de Bock GH, Pras E, et al. Sexual functioning of cervical cancer survivors: A review with a female perspective. Maturitas. 2012;72:296–304. doi: 10.1016/j.maturitas.2012.05.006. [DOI] [PubMed] [Google Scholar]
- 27.Li MY, Yang YL, Liu L, Wang L. Effects of social support, hope and resilience on quality of life among Chinese bladder cancer patients: A cross-sectional study. Health Qual Life Outcomes. 2016;14:73. doi: 10.1186/s12955-016-0481-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Koopman WJ, LeBlanc N, Fowler S, et al. Hope, coping, and quality of life in adults with myasthenia gravis. Can J Neurosci Nurs. 2016;38:56–64. [PubMed] [Google Scholar]
- 29.Carpenter KM, Fowler JM, Maxwell GL, Andersen BL. Direct and buffering effects of social support among gynecologic cancer survivors. Ann Behav Med. 2010;39:79–90. doi: 10.1007/s12160-010-9160-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vellone E, Rega ML, Galletti C, Cohen MZ. Hope and related variables in Italian cancer patients. Cancer Nurs. 2006;29:356–66. doi: 10.1097/00002820-200609000-00002. [DOI] [PubMed] [Google Scholar]
- 31.Domenici L, Palaia I, Giorgini M, et al. Sexual health and quality of life assessment among ovarian cancer patients during chemotherapy. Oncology. 2016;91:205–10. doi: 10.1159/000447403. [DOI] [PubMed] [Google Scholar]
- 32.Han Y, Hu D, Liu Y, et al. Coping styles and social support among depressed Chinese family caregivers of patients with esophageal cancer. Eur J Oncol Nurs. 2014;18:571–77. doi: 10.1016/j.ejon.2014.07.002. [DOI] [PubMed] [Google Scholar]
- 33.Leung J, Atherton I, Kyle RG, et al. Psychological distress, optimism and general health in breast cancer survivors: A data linkage study using the Scottish Health Survey. Support Care Cancer. 2016;24:1755–61. doi: 10.1007/s00520-015-2968-2. [DOI] [PubMed] [Google Scholar]
- 34.Iwanagaa M, Yokoyamab H, Seiwaa H. Coping availability and stress reduction for optimistic and pessimistic individuals. Personality & Individual Differences. 2004;36:11–22. [Google Scholar]
- 35.Sumei Z, Yongai Z, Li M, et al. Anxiety, depression and coping styles in cervical cancer patients undergoing radiotherapy. China Journal of Health Psychology. 2014;22:682–84. [Google Scholar]