Abstract
The mediational role of negative reinforcement smoking outcome expectancies in the relation between perceived stress and (1) perceived barriers to cessation, (2) severity of problematic symptoms during past quit attempts, and (3) smoking-specific experiential avoidance (AIS) was examined. Data were drawn from a baseline assessment of a larger clinical trial. Participants included 332 adult treatment-seeking smokers (47.3% female; Mage = 38.45; SD = .50; age range: 18–65 years). Results indicated that perceived stress was indirectly related to perceived barriers to smoking cessation, severity of problematic symptoms during past quit attempts, and AIS through negative reinforcement outcome expectancies. These results were evident after accounting for the variance explained by gender, negative affectivity, and alternative outcome expectancies for smoking. The present findings suggest that smokers with greater perceived stress experience greater negative reinforcement smoking expectancies, which in turn, may be related to numerous processes involved in the maintenance of smoking.
Keywords: Perceived Stress, Smoking, Negative Affect, Expectancies, Treatment
Extant work posits an interconnection between stress and substance use behavior (Sinha, 2001). Clinical reports, epidemiologic sources, and laboratory investigations converge on a consistent and robust association between elevated objective and subjective indices of stress and substance use and relapse (e.g. Brewer et al., 1998; Sinha, 2001). Indeed, objective and subjective stress indices reliably predict drug use behaviors, including craving/urge, withdrawal, and relapse (al’Absi et al., 2005; Sinha et al., 2006). Perceived stress, defined as the degree to which individuals experience life events as unpredictable, uncontrollable, or generally overloading (Cohen et al., 1983), is one stress construct of potential relevance to smoking. For example, current smokers report higher perceived stress than nonsmokers and ex-smokers (Carey et al., 1993; Cohen and Lichtenstein, 1990; Ng and Jeffery, 2003). Perceived stress also has been found to relate to odds of quit success and time to relapse (al’Absi et al., 2005), and lower confidence to refrain from smoking (Ng and Jeffery, 2003). Moreover, while smokers who are able to quit successfully report decreased perceived stress (Cohen and Lichtenstein, 1990), those who relapse report greater perceived stress (Carey et al., 1993). Although these data suggest perceived stress may be related to certain aspects of smoking behavior, the mechanisms underlying these and other smoking-related effects are unclear.
One possible mechanism that may help elucidate the perceived stress-smoking relation is smoking expectancies (Brandon and Baker, 1991; Brandon et al., 1999; Cohen et al., 2002; Downey and Kilbey, 1995; Kelemen and Kaighobadi, 2007; Niaura et al., 1991). Smoking outcome expectancies reflect anticipated consequences of smoking (Brandon et al., 1999; Cohen et al., 2002; Niaura et al., 1991). Specifically, smoking outcome expectancies include beliefs about positive reinforcement (“I enjoy the taste sensations while smoking”), negative reinforcement (“Smoking helps me calm down when I feel nervous”), negative consequences (“The more I smoke, the more I risk my health”), and appetite control (“Smoking helps me control my weight” (Brandon and Baker, 1991). Whereas positive reinforcement expectancies denote expectancies of receiving sensory gratification from smoking, negative reinforcement expectancies represents expectancies concerning negative emotion regulation and coping. Negative consequence expectancies embodies expectancies related to the long-term negative health smoking consequences. Lastly, appetite and weight control expectancies represent the expectancy that smoking will help control appetite and weight (Urbán, 2010). These expectancies are clinically relevant in terms of explaining various aspects of smoking behavior (Kelemen and Kaighobadi, 2007). For example, positive reinforcement smoking expectancies are related to greater smoking behavior (Copeland et al., 1995; Downey and Kilbey, 1995) and expectancies for negative reinforcement and negative consequences predict poor cessation success (Urbán, 2010). However, research has not yet examined smoking outcome expectancies in the context of perceived stress and numerous processes involved in the maintenance of smoking.
Building from self-regulation and coping theories for tobacco use (Abrams and Niaura, 1987; Shiffman and Wills, 1985), smokers with higher levels of perceived stress may come to learn to expect that smoking can lessen experiential discomfort. Specifically, smokers with higher relative to lower perceived stress may experience a greater degree of negative affect reduction from smoking (e.g., via attention reallocation, the pharmacological effects of nicotine, or both). Thus, even in the absence of any objective stress-reducing properties of nicotine, perceived stress may be related to negative reinforcement expectancies for smoking, which in turn, may be related to more problematic smoking behavior (e.g., perceived obstacles to quitting, more problems during quit attempts, and smoking to avoid or escape distress). Indeed, negative reinforcement smoking outcome expectancies may be a cognitive mechanism that helps to explain the relation between perceived stress and smoking.
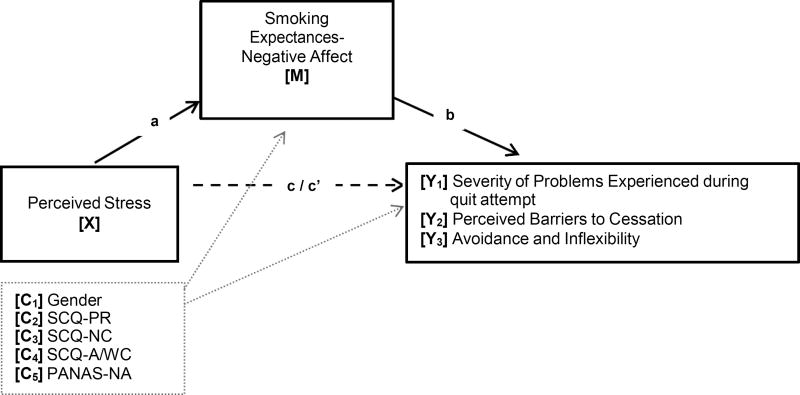
Together, the current study tested the hypothesis that, among treatment-seeking smokers, negative reinforcement expectancies for smoking would predict a wide array of smoking processes related to quit history and maintenance of cigarette use, which consistently are related to poorer treatment outcome (Cosci et al., 2009; Ockene et al., 2000; Schnoll et al., 2011). Specifically, negative reinforcement expectancies would explain the relation between perceived stress and severity of problematic symptoms during past quit attempts among treatment-seeking smokers, perceived barriers to cessation, and smoking-specific avoidance and inflexibility (AIS) (see Figure 1).
Figure 1.
Proposed model: Negative reinforcement smoking outcome expectancies as a potential mediation variable of the association between perceived stress and smoking cessation-related outcomes.
Note: a = Effect of X on M; b = Effect of M on Yi; c’i = Direct effect of X on Yi controlling for M; a*b = Indirect effect of X on Yi through M; three separate models were conducted for each criterion variable (Y1–3). PSS (Perceived Stress Scale) is the predictor, SCQ-NA (Smoking Expectancy for Negative Reinforcement/Negative Affect Reduction) is the mediation variable, and Quit Prob (Severity of Problems Experienced During a Past Quit Attempt; Y1), BCS (Perceived Barriers to Smoking Cessation; Y2), and AIS (Avoidance and Inflexibility Scale; Y3) are the outcome variables. Covariates included: Gender (C1), SCQ-PR (Smoking Consequences Questionnaire-Positive Reinforcement Subscale; C2), SCQ-AWC (Smoking Consequences- Appetite and Weight Control Subscale; C3), SCQ-NC (Smoking Consequences Questionnaire-Negative Consequences Subscale; C4), and PANAS-NA (Positive and Negative Affect Scale-Negative Affect Subscale; C5).
Method
Participants
Adult daily smokers were recruited from the community to participate in a randomized controlled dual-site clinical trial examining the efficacy of two smoking cessation interventions. The sample consisted of 332 treatment-seeking adult daily smokers (47.3% female; Mage = 38.45; SD = .500; age range: 18–65 years) who had an exhaled carbon monoxide level at baseline of at least 10 parts per million (ppm; Jarvis et al., 1987) and at least one serious lifetime quit attempt. Of the potential participants screened for eligibility (n=725), 393 were excluded because of a history of psychosis, current suicidality, expired carbon monoxide less than 10 ppm, zero serious previous quit attempts, or missing or incomplete data on study measures or covariates. See Table 1 for sample characteristics.
Table 1.
Participant characteristics
| M(SD)/N[%] | |
|---|---|
| Age | 38.45 (12.95) |
| Gender | |
| Male | 175 [52.7] |
| Female | 157 [47.3] |
| Race/ethnicity | |
| White | 290 [87.3] |
| Black Non-Hispanic | 23 [6.9] |
| Black Hispanic | 2 [0.6] |
| Hispanic | 7 [2.1] |
| Asian | 3 [0.9] |
| Other | 7 [2.1] |
| Education Completed | |
| Less than high school | 15 [4.5] |
| High school graduate or equivalent | 79 [23.8] |
| Some college | 97 [29.2] |
| Associates degree | 32 [9.6] |
| Bachelor degree | 56 [16.9] |
| Some graduate or professional school | 21 [6.3] |
| Graduate or professional school | 32 [9.6] |
| Marital Status | |
| Married or living with someone | 127 [38.3] |
| Widowed | 8 [2.4] |
| Separated | 18 [5.4] |
| Divorced or annulled | 62 [18.7] |
| Never married | 117 [35.2] |
| Baseline CO (ppm) | 22.6 (10.73) |
| Smoking Rate | 18.06 (9.28) |
| Nicotine Dependence | 5.08 (2.2) |
| Years a Daily Smoker | 20.02 (12.87) |
| Number of Past Serious Quit Attempts | 3.58 (2.29) |
| PANAS-NA | 18.81 (6.98) |
| SCQ-PR | 5.58 (1.51) |
| SCQ-AWC | 4.19 (2.33) |
| SCQ-NC | 6.62 (1.25) |
| PSS | 24.10 (7.56) |
| SCQ-NA | 5.68 (1.72) |
| AIS Total | 45.22 (10.62) |
| Barrier to Smoking Cessation | 25.32 (11.33) |
| Severity of Problems During Quit Attempt | 2.08 (0.65) |
Note. N = 332; M(SD) = Mean (Standard Deviation). CO (ppm) = Carbon Monoxide (parts per million); PANAS-NA = Positive and Negative Affect Scale-Negative Affect subscale (Watson et al., 1988); PSS = Perceived Stress Scale (Cohen et al., 1983); AIS = Avoidance and Inflexibility Scale (Gifford et al., 2004); SCQ-PR = Smoking Consequences Questionnaire-Positive Reinforcement Subscale, SCQ-AWC = Smoking Consequences- Appetite and Weight Control Subscale, SCQ-NC = Smoking Consequences Questionnaire-Negative Consequences Subscale SCQ-NA = Smoking Consequences- Negative Affect Subscale (Brandon and Baker, 1991).
Measures
Primary Predictor Variable
Perceived Stress Scale (PSS)
PSS (Cohen et al., 1983) assessed the individual’s perceived stress. PSS is a 14-item scale which measures the degree to which situations in one's life is appraised stressful during the past month. Participants respond to feeling stressed on a 0 (never) to 4 (very often) scale. Item content reflects the degree to which respondents report experiencing life events as unpredictable, uncontrollable, and generally overloading (e.g., “How often have you felt that you were able to control the important things in your life?”). The PSS score is derived by summing all items; total scores range from 0 to 56.The PSS has good internal consistency (r = .84 – .86) and test-retest reliability (r = .85; Cohen et al., 1983). In the present study, the PSS demonstrated acceptable internal consistency (Cronbach’s α = 0.86).
Smoking Consequences Questionnaire (SCQ)
The SCQ (Brandon and Baker, 1991) is a 50-item self-report measure that assesses tobacco use outcome expectancies believed to underlie smoking motivation on a Likert-type scale, ranging from 0 (completely unlikely) to 9 (completely likely). The measure consists of four key subscales: Positive Reinforcement/Sensory Satisfaction (SCQ-PR; 15 items), Negative Reinforcement/Negative Affect Reduction (SCQ-NA; 12 items), Negative Consequences (SCQ-NC; 18 items), and Appetite-Weight Control (SCQ-A/WC; 5 items). The entire measure and its factors exhibit good psychometric properties (Brandon and Baker, 1991; Downey and Kilbey, 1995; coefficient alpha’s for the subscales range from 0.88 to 1.93 in the current sample, indicating excellent internal consistency. SCQ-NA was entered as the mediation variable and all other subscales were covariates of the models.
Dependent Measures
Smoking History Questionnaire (SHQ)
The SHQ (Brown et al., 2002) is a self-report questionnaire used to assess smoking history (e.g., onset of regular daily smoking), pattern (e.g., number of cigarettes consumed per day), and problematic symptoms experienced during past quit attempts (e.g., weight gain, nausea, irritability, and anxiety (Brown et al., 2002). As is in past work (Zvolensky et al., 2004), a mean composite score of severity of problem symptoms experienced during past quit attempts was derived from this measure. Specifically, this measure includes 17 items such as “while trying to quit, how serious have each of the following problems been for you?” Items were rated on a 1 (not at all) to 5 (extremely) Likert scale. The severity of these items were summed and divided by 17 to compute the mean composite score. The SHQ was also employed to describe the sample smoking history.
Barriers to Cessation Scale (BCS)
The BCS assesses perceived barriers, or specific stressors, associated with smoking cessation (Macnee and Talsma, 1995). The BCS is a 19-item measure on which respondents indicate, according to a 4-point Likert-style scale 0 (not a barrier) to 3 (large barrier), the extent to which they identify with each specified barrier to cessation. Researchers report good internal consistency regarding the total score, and good content and predictive validity of the measure (Macnee and Talsma, 1995). The total score was utilized (Cronbach’s α = 0.90).
Avoidance and Inflexibility Scale (AIS)
The AIS is a 13-item self-reported measure of smoking-specific experiential avoidance (Gifford et al., 2004). Experiential avoidance is the unwillingness to experience aversive internal experiences (i.e. thoughts, feelings, bodily sensations) (Hayes, 2006). Respondents rate how they respond to difficult thoughts that encourage smoking (e.g., “I need a cigarette”), difficult feelings that encourage smoking (e.g., stress, fatigue, boredom), and bodily sensations that encourages smoking (e.g., “physical cravings or withdrawal symptoms”). Example items include “How likely is it you will smoke in response to [thoughts/feelings/sensations]?” and “How important is getting rid of [thoughts/feelings/sensations]?” Items are rated on a 5-point Likert scale from 1 (Not at all) to (5 Very much), with higher scores reflecting greater levels of smoking-specific experiential avoidance (possible range 13–65). The AIS has documented psychometric properties, including internal consistency (Gifford et al., 2004). In the current sample, the internal consistency was very good (Cronbach α = 0.92).
Additional Measures used as Covariates or Sample Descriptors
Demographics Questionnaire
Demographic information collected included gender, age, race, education, and marital status. Gender was entered as a covariate in all analyses.
Carbon Monoxide
Biochemical verification of smoking status was assessed by exhaled carbon monoxide (CO) analysis of breath samples collected using a CMD/CO Carbon Monoxide Monitor (Model 3110; Spirometrics, Inc.). A cut-off of 8 ppm has demonstrated excellent properties that distinguishing smokers from nonsmokers (Jarvis et al., 1987).
Positive and Negative Affect Scale (PANAS)
The PANAS (Watson et al., 1988) is a self-report trait-measure that requires participants to rate the extent to which they experience 20 different feelings and emotions during the past year (e.g., nervous, interested) based on a Likert-scale that ranges from 1 (Very slightly or not at all) to 5 (Extremely). The measure yields two factors, negative and positive affect, and has strong documented psychometric properties (Watson et al., 1988). The PANAS negative affectivity subscale (PANAS-NA; 10 items) is characterized as the propensity to experience negative affect. This subscale was utilized in the present study (Cronbach’s α = 0.91).
Fagerström Test for Nicotine Dependence (FTND)
The FTND (Heatherton et. al., 1991) is a 6-item self-report scale that was used to assess gradations in tobacco dependence. Scores range from 0–10, with higher scores reflecting high levels of physiological dependence on nicotine. The internal consistency in this sample was acceptable (Cronbach’s α = .59).
Procedure
After providing written informed consent, participants completed an interview and a computerized battery of self-report questionnaires. The Institutional Review Board at each study site approved the study protocol; all study procedures and treatment of human subjects were conducted in compliance with ethical standards of the American Psychological Association. The current study is based on secondary analyses of baseline (pre-treatment) data for a sub-set of the sample that met inclusion criteria for the current study and provided complete data for all studied variables.
Analytic Strategy
Descriptive data and zero-order correlations among all study variables were examined. Analyses were conducted using bootstrapping techniques through PROCESS, a conditional modeling program that utilizes an ordinary least squares-based path analytical framework to test for both direct and indirect effects (Hayes, 2013). Bootstrapping is the recommended approach when data distribution is nonnormal or unknown (Kelley, 2005; Kirby and Gerlanc, 2013); thus, nonnormality was not a principal concern due to the employed bootstrapping techniques. An indirect effect is presumed to be significant if the product of path a and path b is significant, i.e., confidence intervals (CIs) do not include zero (Preacher and Hayes, 2008; Zhao et al., 2010). Path a is the effect of the predictor on the mediation variable; and path b is the effect of the mediation variable on the entered outcome. Models included PSS as the predictor and SCQ-NA as the mediation variable. Covariates included gender, PANAS-NA, and SCQ subscales except SCQ-NA. See Figure 1. Three independent models were examined with severity of problems experienced during quit attempt (Model 1), perceived barriers to cessation (Model 2), and AIS (Model 3) as criterion variables. In all models, 10,000 bootstrap samples were performed and a 95-percentile confidence interval (CI) was estimated (as recommended by Hayes, 2009; Preacher and Hayes, 2004; Preacher and Hayes, 2008).
Results
Zero-order correlations are presented in Table 2. PSS was significantly correlated with severity of problem symptoms experienced during past quit attempts, perceived barriers to cessation, and AIS. SCQ-NA was significantly correlated with severity of problem symptoms experienced during past quit attempts, perceived barriers to cessation, and AIS. PSS and SCQ-NA were significantly correlated.
Table 2.
Descriptive statistics and correlations for study variables (n=332)
| Variable | 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Gendera | 1 | |||||||||
| 2. PANAS-NAa | .12* | 1 | ||||||||
| 3. SCQ-PRa | .02 | .20** | 1 | |||||||
| 4. SCQ-AWCa | .27** | .12* | .33** | 1 | ||||||
| 5. SCQ-NCa | .16** | .20** | .24** | .23** | 1 | |||||
| 6. PSSb | .16** | .62** | .16** | .23** | .14** | 1 | ||||
| 7. SCQ-NAc | .16** | .41** | .58** | .44** | .32** | .48** | 1 | |||
| 8. Quit Problemsd | .29** | .39** | .39** | .39** | .42** | .34** | .49** | 1 | ||
| 9. BCS Totald | .22** | .40** | .47** | .31** | .39** | .36** | .52** | .58** | 1 | |
| 10. AIS Totald | .19** | .25** | .34** | .24** | .49** | .27** | .44** | .48** | .58** | 1 |
Note.
p < .01,
p < .05;
Covariates;
Predictor;
Mediation Variable;
Criterion Variables
Gender: (coded 1 = male; 2 = female); PANAS-NA = Positive and Negative Affect Scale-Negative Affect Subscale (Watson et al., 1988); SCQ-PR = Smoking Consequences Questionnaire-Positive Reinforcement Subscale (Brandon and Baker, 1991); SCQ-AWC = Smoking Consequences- Appetite and Weight Control Subscale (Brandon and Baker, 1991); SCQ-NC = Smoking Consequences Questionnaire-Negative Consequences Subscale (Brandon and Baker, 1991); PSS = Perceived Stress Scale (Cohen et al., 1983); SCQ-NA = Smoking Consequences- Negative Affect Subscale (Brandon and Baker, 1991); Quit Problems = Mean severity rating of problems experienced while quitting per the Smoking History Questionnaire (Brown et al., 2002); BCS= Perceived Barriers, or Specific Stressors, Associated with Smoking (Macnee and Talsma, 1995); AIS = Avoidance and Inflexibility Scale (Gifford et al., 2004).
Regression Analyses
Regression results for paths a, b, c, and c’ are presented in Table 2. Model 1 for severity of problem symptoms experienced during past quit attempts revealed a significant total effect (R2 = .41, F[6, 325] = 37.88, p < .001), with gender, SCQ-PR, SCQ-NC, SCQ-A/WC, and PANAS-NA as significant predictors. The direct effect model was significant (R2 = .42, F[7, 324] = 33.58, p < .001), with SCQ-NA, gender, SCQ-PR, SCQ-NC, SCQ-A/WC, and PANAS-NA as significant predictors.
Model 2 for perceived barriers to cessation revealed a significant total effect (R2 = .41, F[6, 325] = 37.68, p < .001), with PSS, gender, SCQ-PR, SCQ-NC, and PANAS-NA as significant predictors. The direct effect model was significant (R2 = .42, F[7, 324] = 33.52, p < .001), with SCQ-NA, gender, SCQ-PR, SCQ-NC, and PANAS-NA as significant predictors.
Model 3 for AIS revealed a significant total effect (R2 = .34, F[6, 325] = 27.28, p < .001), with PSS, SCQ-PR, and SCQ-NC as significant predictors. The direct effect model was significant (R2 = .35, F[7, 324] = 25.13, p < .001), with SCQ-NA, SCQ-PR, and SCQ-NC as significant predictors.
Specificity Analyses
To further strengthen interpretation of results, PSS and SCQ-NA variables were reversed for each of the three models tested previously (Preacher and Hayes, 2004). Tests of the indirect effects in these models were estimated based on 10,000 bootstrap re-samples. All results of the reversed models were non-significant (all CIs for a*b indirect effects contained zero).
Discussion
Consistent with expectation, negative reinforcement smoking outcome expectancies played a mediational role in the relation between perceived stress and perceived barriers to smoking cessation, severity of problems experienced during quit attempt and AIS. These results suggest that perceived stress may contribute to negative reinforcement expectancies that, in turn, increase several aspects of smoking-related cognitions and behaviors. These results are broadly in line with past research that has indicated perceived stress is related to difficulties with quitting smoking (al’Absi et al., 2005; Carey et al., 1993; Cohen and Lichtenstein, 1990) and uniquely extend it to numerous indicators of smoking severity. Specifically, the effect of perceived stress on smoking was indirect and dependent upon the degree to which a person expected smoking to alleviate internal distress. Moreover, the present findings explain, in part, unique variance in the dependent variables that is distinguishable from variance accounted for by negative affectivity.
Notably, the observed indirect effects were evident after adjusting for additional factors that may influence smoking cessation-related outcomes, including gender, negative affect, and alternative smoking outcome expectancies other than negative reinforcement expectancy. Therefore, the observed effects were over and above that of other theoretically-relevant factors. Moreover, the alternative models tested, with the predictor and mediator reversed, showed no significant indirect effects, suggesting that the statistical mediation effect was specific to negative reinforcement expectancies. To more fully explore nature of the relation among these variables over time, future prospective modeling of the temporal ordering of perceived stress and negative reinforcement smoking outcome expectancies is warranted.
Clinically, the present findings suggest that it may be advisable to address negative reinforcement smoking outcome expectancies among smokers with elevated perceived stress to facilitate changes in smoking behavior. Indeed, the findings from the investigation may serve to conceptually inform the development of specialized intervention strategies for smokers with elevated perceived stress (Zvolensky et al., 2013). The current data suggest that it may be advisable to understand and clinically address negative reinforcement smoking expectancies to enhance psychological flexibility related to smoking, perceived barriers for quitting, and problematic symptoms during quit attempt in order to address maladaptive smoking cognitions and facilitate change in smoking behavior.
There are a number of interpretive caveats to the present study that may warrant further consideration. First, given the cross-sectional nature of these data, it is unknown whether perceived stress is causally related to greater negative reinforcement smoking expectancies or to the smoking cessation-related outcomes. The present tests were based on a theoretical framework (Brown et al., 2001) and did not allow for testing of temporal sequencing. Future prospective studies are necessary to determine the directional effects of these relations. Second, our sample consisted of community-recruited, treatment-seeking daily cigarette smokers with moderate levels of nicotine dependence. Studies may benefit by sampling from lighter and heavier smoking populations to ensure the generalizability of the results to the general smoking population. Third, the sample was largely comprised of a relatively homogenous group of treatment-seeking smokers. To rule out a selection bias and increase the generalizability of these findings, it will be important for future studies to recruit a more ethnically/racially diverse sample of smokers.
Overall, the present study serves as an initial investigation into the nature of the association between perceived stress, negative reinforcement smoking outcome expectancies, and smoking behavior. Future work is needed to explore the extent to which negative reinforcement smoking outcome expectancies accounts for relations between perceived stress and other smoking variables (e.g., withdrawal, cessation outcome) to further clarify theoretical models of emotional vulnerability and processes involved in the maintenance of smoking.
Table 3.
Regression models.
| Y | Model | b | SE | t | p | CI (lower) | CI (upper) |
|---|---|---|---|---|---|---|---|
| Quit Prob | PSS →SCQ-NA (a) | .066 | .011 | 5.977 | .000 | .045 | .088 |
| SCQ→Quit Prob (b) | .053 | .024 | 2.233 | .026 | .006 | .100 | |
| PSS→Quit Prob (c’) | .003 | .005 | .573 | .567 | −.007 | .013 | |
| PSS→Quit Prob (c) | .006 | .005 | 1.336 | .183 | −.003 | .016 | |
| PSS→SCQ-NA→Quit Prob (a*b) | .004 | .002 | .001 | .008 | |||
|
| |||||||
| BCS | SCQ→BCS (b) | .969 | .415 | 2.336 | .020 | .153 | 1.786 |
| PSS→BCS (c’) | .114 | .088 | 1.305 | .193 | −.058 | .286 | |
| PSS→BCS (c) | .178 | .084 | 2.135 | .034 | .014 | .343 | |
| PSS→SCQ→BCS (a*b) | .064 | .028 | .015 | .127 | |||
|
| |||||||
| AIS | SCQ→AIS (b) | 1.199 | .411 | 2.915 | .004 | .390 | 2.008 |
| PSS→AIS (c’) | .141 | .087 | 1.629 | .104 | −.029 | .312 | |
| PSS→AIS (c) | .221 | .083 | 2.653 | .008 | .057 | .385 | |
| PSS→SCQ→AIS (a*b) | .008 | .031 | .028 | .151 | |||
Note. Significant indirect effects are bolded. Path a is equal across all models; therefore, it presented only in the model with Y1 to avoid redundancies. N for analyses of models Y1–Y3 included 332 cases. The standard error and 95% CI for a*b are obtained by bootstrap with 10,000 re-samples. PSS (Perceived Stress Scale) is the predictor, SCQ (Smoking Expectancy for Negative Reinforcement/Negative Affect Reduction) is the mediation variable, and Quit Prob (Severity of Problems Experienced During a Past Quit Attempt; Y1), BCS (Perceived Barriers to Smoking Cessation; Y2), and AIS (Avoidance and Inflexibility; Y3) are the outcome variables. CI (lower) = lower bound of a 95% confidence interval; CI (upper) = upper bound; → = affects.
References
- Abrams DB, Niaura RS. Social learning theory. In: Blane HT, Leonard KE, editors. Psychological Theories of Drinking and Alcoholism. New York: The Guilford Press; 1987. pp. 131–178. [Google Scholar]
- al’Absi M, Hatsukami D, Davis GL. Attenuated adrenocorticotropic responses to psychological stress are associated with early smoking relapse. Psychopharmacology. 2005;181(1):107–117. doi: 10.1007/s00213-005-2225-3. [DOI] [PubMed] [Google Scholar]
- Brandon TH, Baker TB. The Smoking Consequences Questionnaire: The subjective expected utility of smoking in college students. Psychological Assessment: A Journal of Consulting and Clinical Psychology. 1991;3(3):484. [Google Scholar]
- Brandon TH, Juliano LM, Copeland AL. Expectancies for tobacco smoking. In: Kirsch I, editor. How expectancies shape experience. Washington, D.C: American Psychological Assosication; 1999. pp. 263–299. [Google Scholar]
- Brewer DD, Catalano RF, Haggerty K, Gainey RR, Fleming CB. A meta-analysis of predictors of continued drug use during and after treatment for opiate addiction. Addiction. 1998;93(1):73–92. [PubMed] [Google Scholar]
- Brown RA, Kahler CW, Zvolensky MJ, Lejuez C, Ramsey SE. Anxiety sensitivity: Relationship to negative affect smoking and smoking cessation in smokers with past major depressive disorder. Addictive Behaviors. 2001;26(6):887–899. doi: 10.1016/s0306-4603(01)00241-6. [DOI] [PubMed] [Google Scholar]
- Brown RA, Lejuez CW, Kahler CW, Strong DR. Distress tolerance and duration of past smoking cessation attempts. Journal of Abnormal Psychology. 2002;111(1):180–185. doi: 10.1037/0021-843X.111.1.180. [DOI] [PubMed] [Google Scholar]
- Carey MP, Kalra DL, Carey KB, Halperin S, Richards CS. Stress and unaided smoking cessation: a prospective investigation. Journal of Consulting and Clinical Psychology. 1993;61(5):831. doi: 10.1037//0022-006x.61.5.831. [DOI] [PubMed] [Google Scholar]
- Cohen LM, McCarthy DM, Brown SA, Myers MG. Negative affect combines with smoking outcome expectancies to predict smoking behavior over time. Psychology of Addictive Behaviors. 2002;16(2):91. doi: 10.1037//0893-164x.16.2.91. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24(4):385–396. [PubMed] [Google Scholar]
- Cohen S, Lichtenstein E. Perceived stress, quitting smoking, and smoking relapse. Health Psychology. 1990;9(4):466–478. doi: 10.1037/0278-6133.9.4.466. [DOI] [PubMed] [Google Scholar]
- Copeland AL, Brandon TH, Quinn EP. The Smoking Consequences Questionnaire-Adult: Measurement of smoking outcome expectancies of experienced smokers. Psychological Assessment. 1995;7(4):484. [Google Scholar]
- Cosci F, Corlando A, Fornai E, Pistelli F, Paoletti P, Carrozzi L. Nicotine dependence, psychological distress and personality traits as possible predictors of smoking cessation. Results of a double-blind study with nicotine patch. Addictive Behaviors. 2009;34(1):28–35. doi: 10.1016/j.addbeh.2008.08.003. [DOI] [PubMed] [Google Scholar]
- Downey KK, Kilbey MM. Relationship between nicotine and alcohol expectancies and substance dependence. Experimental and Clinical Psychopharmacology. 1995;3(2):174. [Google Scholar]
- Gifford EV, Kohlenberg BS, Hayes SC, Antonuccio DO, Piasecki MM, Rasmussen-Hall ML, Palm KM. Acceptance-Based Treatment for Smoking Cessation. Behavior Therapy. 2004;35(4):689–705. doi: 10.1016/j.beth.2011.03.002. [DOI] [PubMed] [Google Scholar]
- Hayes AF. Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Communication Monographs. 2009;76(4):408–420. [Google Scholar]
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. Methodology in the social sciences. New York, NY: The Guilford Press; 2013. [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerstorm KO. The Fagerström test for nicotine dependence: a revision of the Fagerstrom Tolerance Questionnaire. British journal of addiction. 1991;86(9):1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Jarvis MJ, Tunstall-Pedoe H, Feyerabend C, Vesey C, Saloojee Y. Comparison of Tests Used to Distinguish Smokers from Nonsmokers. American Journal of Public Health. 1987;77(11):1435–1438. doi: 10.2105/ajph.77.11.1435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelemen WL, Kaighobadi F. Expectancy and pharmacology influence the subjective effects of nicotine in a balanced-placebo design. Experimental and clinical psychopharmacology. 2007;15(1):93. doi: 10.1037/1064-1297.15.1.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelley K. The effects of nonnormal distributions on confidence intervals around the standardized mean difference: Bootstrap and parametric confidence intervals. Educational and Psychological Measurement. 2005;65(1):51–69. [Google Scholar]
- Kirby KN, Gerlanc D. BootES: An R package for bootstrap confidence intervals on effect sizes. Behavior Research Methods. 2013;45(4):905–927. doi: 10.3758/s13428-013-0330-5. [DOI] [PubMed] [Google Scholar]
- Macnee CL, Talsma A. Development and testing of the barriers to cessation scale. Nursing Research. 1995;44(4):214–219. [PubMed] [Google Scholar]
- Ng DM, Jeffery RW. Relationships between perceived stress and health behaviors in a sample of working adults. Health Psychology. 2003;22(6):638. doi: 10.1037/0278-6133.22.6.638. [DOI] [PubMed] [Google Scholar]
- Niaura R, Goldstein M, Abrams D. A bioinformational systems perspective on tobacco dependence. British Journal of Addiction. 1991;86(5):593–597. doi: 10.1111/j.1360-0443.1991.tb01814.x. [DOI] [PubMed] [Google Scholar]
- Ockene JK, Mermelstein RJ, Bonollo DS, Emmons KM, Perkins KA, Voorhees CC, Hollis JF. Relapse and maintenance issues for smoking cessation. Health Psychology. 2000;19(1S):17. doi: 10.1037/0278-6133.19.suppl1.17. [DOI] [PubMed] [Google Scholar]
- Preacher K, Hayes A. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, & Computers. 2004;36(4):717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Schnoll RA, Martinez E, Tatum KL, Glass M, Bernath A, Ferris D, Reynolds P. Increased self-efficacy to quit and perceived control over withdrawal symptoms predict smoking cessation following nicotine dependence treatment. Addictive behaviors. 2011;36(1):144–147. doi: 10.1016/j.addbeh.2010.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S, Wills TA. Coping and substance abuse. Academic Press; 1985. [Google Scholar]
- Sinha R. How does stress increase risk of drug abuse and relapse? Psychopharmacology. 2001;158(4):343–359. doi: 10.1007/s002130100917. [DOI] [PubMed] [Google Scholar]
- Sinha R, Garcia M, Paliwal P, Kreek MJ, Rounsaville BJ. Stress-induced cocaine craving and hypothalamic-pituitary-adrenal responses are predictive of cocaine relapse outcomes. Archives of General Psychiatry. 2006;63(3):324–331. doi: 10.1001/archpsyc.63.3.324. [DOI] [PubMed] [Google Scholar]
- Urbán R. Smoking outcome expectancies mediate the association between sensation seeking, peer smoking, and smoking among young adolescents. Nicotine & Tobacco Research. 2010;12(1):59–68. doi: 10.1093/ntr/ntp174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. Journal of Personality and Social Psychology. 1988;54(6):1063. doi: 10.1637/10T0-3590.19.3.253. [DOI] [PubMed] [Google Scholar]
- Zhao X, Lynch JG, Chen Q. Reconsidering Baron and Kenny: Myths and truths about mediation analysis. Journal of Consumer Research. 2010;37(2):197–206. [Google Scholar]
- Zvolensky MJ, Bogiaizian D, Salazar PL, Farris SG, Bakhshaie J. An anxiety sensitivity reduction smoking-cessation program for spanish-speaking smokers (argentina) Cognitive and Behavioral Practice. 2013;21(3):350–363. [Google Scholar]
- Zvolensky MJ, Lejuez CW, Kahler CW, Brown RA. Nonclinical panic attack history and smoking cessation: An initial examination. Addictive Behaviors. 2004;29(4):825–830. doi: 10.1016/j.addbeh.2004.02.017. [DOI] [PubMed] [Google Scholar]