INTRODUCTION
Otitic hydrocephalus is the rarest complication of middle ear infection. First described by Symonds [1] it is a syndrome of raised intracranial pressure associated with middle ear infection with normal CSF. The most frequent victims are children and adolescents. Here we present and discuss one such rare, unfortunate case of Otitic hydrocephalus.
Case Report
A-14 year- old male patient presented to the ENT OPD with history of foul smelling, scanty, blood stained discharge from (R) ear, off and on since childhood. He had been taking treatment for the same without relief. He also complained of diminished hearing in the (R) ear. There were no complaints of tinnitus or vertigo. He also complained of diminishing vision in both eyes for 06 months. This was initially accompanied by occasional headache, nausea and vomiting which subsided after a few months. There was no history of fever, alteration in sensorium, convulsions, change in speech or symptoms suggestive of focal cerebral or cerebellar involvement. He had undergone some ear surgery in the past in civil hospital details of which were not known. Clinical examination showed a well healed (R) postaural incision with the pinna displaced anteriorly. The external auditory meatus showed a fleshy polyp which did not bleed to touch and did not shrink with vasoconstrictors. The tympanic membrane could not be seen. Neurotological examination revealed (L) VI cranial nerve palsy. There was no nystagmus, facial palsy or cerebellar signs. Higher mental functions were normal. There was no other cranial nerve palsy nor any sensory or motor deficit. Ocular examination showed visual acuity of finger counting at 6” and fundus examination revealed post papilloedema optic atrophy. Examination of the neck was normal with no rigidity or phlebitis migrans. Tuning fork tests showed conductive deafness in Rt ear which was confirmed on audiometry with 40-50 db AB gap. There was absence of visual evoked potential in both eyes and reduced field of vision on perimetry. Xray mastoid showed sclerosis of Rt mastoid. CT Scan (Figs 1 & 2) showed bony defect in posterolateral part of Rt mastoid along with focal thrombosis of superior sagittal sinus and also thromosis of sigmoid sinus (RT). CSF examination did not show any pathogens and pressure was not raised. Patient was taken up for surgery. The mastoid was explored postaurally, there was complete dehiscence of tegmen antri and tegmen tympani with herniation of temporal lobe of brain into the antrum and prolapse of dura which was projecting as aural polyp. The polyp along with pultaceous debris was removed, disease cleared from the mastoid and tegmen defect reconstructed by anteriorly based temporalis muscle flap which was used to obliterate the mastoid cavity. Postoperative recovery was uneventful. However since the ocular condition was evidence of end stage otitic hydrocephalus without raised intracranial tension no further treatment could be offered to the patient.
Figs 1 & 2.

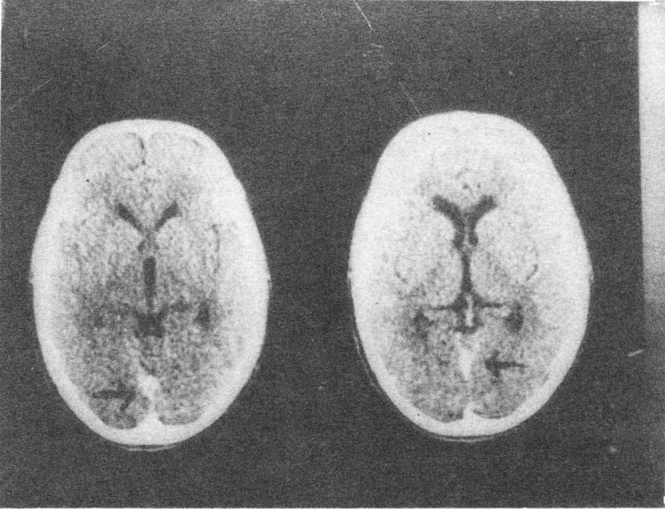
CT scan showing bony defect in posterolateral part of rt mastoid along with thrombosis of sigmoid sinus
The patient has been followed up for a period of six months postoperatively. There has been no deterioration of the ocular status, the middle ear cavity is well healed and dry and there is no recurrence of brain herniation.
Discussion
Otitic Hydrocephalus or Pseudotumour cerebri is a rare complication of the middle ear infection, of unknown mechanism. The condition may arise due to increased production or reduced absorption of CSF following obstruction of lateral sinus which affects cerebral venous outflow or extension of thrombus to superior sagittal sinus impeding CSF resorption [2] Gowers and Macguirt [3] however considered this entity as idiopathic benign intra cranial hypertension associated with ear disease and raised intra cranial pressure following lateral sinus thrombosis as different entity. The leading symptoms are headache, drowsiness, blurred vision, nausea and vomiting and sometimes diplopia. The onset may be many years after chronic middle ear disease. Clinical examination reveals papilloedema, lateral rectus palsy due to VIth cranial nerve stretching on one or both sides may be found and there is associated evidence of middle ear infection. The differential diagnosis includes other causes of raised intracranial pressure and CT Scan is essential to rule out brain abscess. Treatment consists of managing the ear infection and preventing visual impairment by reducing intra cranial pressure by use of steroid, diuretic and dehydrating agents. Repeated lumbar puncture or long term thecoperitoneal shunting may occasionally be needed. Treatment is to be continued over many weeks. Permanent deficits such as visual impairment are uncommon [4] and once they occur nothing can be done for these unfortunate patients.
REFERENCES
- 1.Symonds CD. Otitic Hydrocephalus. Brain. 1931;54:55–57. [Google Scholar]
- 2.Pfaltz CR, Griesemer C. Complications of Acute Suppurative Otitis Media. Annals Otol Rhinol Larygol. 1984;93:133–137. doi: 10.1177/00034894840930s423. [DOI] [PubMed] [Google Scholar]
- 3.Gower D, Mc Guirt WF. Intracranial complications of acute and chronic ear disease. Laryngoscope. 1983;93:1028–1033. doi: 10.1288/00005537-198308000-00010. [DOI] [PubMed] [Google Scholar]
- 4.Pennybacker J. Origin Discussion on intracranial complications of pyogenic. Proceedings of Royal society of Medicine. 1961;64:309–320. [PMC free article] [PubMed] [Google Scholar]


