Abstract
Acute Myocardial Infarction as a cause of death is diagnosed in many cases of sudden death based on the indirect evidence of critical narrrowing (75%) of one or more coronary arteries. Microscopic evidence of infarction is seen in H & E stained sections only if the person has survived for a minimum period of 6 hours after sustaining fatal ischaemic attack. In this study we have used two laboratory methods for visualisation of infarcts of lesser ‘age’, viz.-Triphenyl Tetrazolium Chloride (TTC) Macro Test and Acridine Orange Fluorescence Study. The former is a gross staining procedure which can reveal infarcts of 5-6 hours age, while the later is UV Fluorescent microscopic examination capable of detecting infarcts of 2 hours age. Although these procedures are well accepted ones, the aim of this article is to induce Forensic Pathologists to incorporate these tests in the study protocol of all sudden death cases with the aim of ‘visualising’ the infarct rather than basing the diagnosis on indirect evidence of critical narrowing of Coronaries.
KEY WORDS: Acridine Orange Fluorescence, Age of infarct, Chloride macro test, Myocardial infarct, Triphenyl Tetrazolium chloride macro test
Introduction
Myocardial infarction due to atherosclerotic ischaemic heart disease is probably the commonest diagnosis made in majority of sudden death cases subjected to clinical and medicolegal autopsies. This is so because “Heart Attack” as a cause of sudden death has ready acceptance not only amongst non-medical men like police officials, coroners and judges, but also amongst medical men. The scientific reason for frequent resortance to this diagnosis during autopsies is that, an indirect diagnosis of Myocardial Infarction (MI) is accepted in many such instances. That is, the diagnosis is not based on actual visualisation of the infarcted myocardial tissue by any means but the presence of significant narrowing of one or more major coronary vessels is considered as sufficient evidence for coming to a conclusion. This criterion is applied in cases where the patient did not survive for sufficient time for either gross or microscopic findings of infarct to appear after sustaining fatal ischaemic attack. It is known that microscopic and gross findings can be detected in the infarcted tissue only if the infarct is of six and twelve hours old respectively. If the patient dies within 6 hours after sustaining MI, the indirect evidence is relied upon. This criterion is not only unscientific but also will lead to over diagnosis of MI as cause of death, especially in cases with less than six-hour post-infarction survival.
This study is aimed at minimising such unscientific diagnosis by resorting to two methods for Postmortem Diagnosis of Early MI, viz. Triphenyl Tetrazolium Chloride (TTC) staining of slices of myocardium and Acridine Orange Fluorescent Staining of sections. The former method can detect MI of 4-5 hours age and latter of around 2 hours.
Material and Methods
PM study was carried out in 18 clinically suspected/confirmed cases of MI. In addition 10 cases of sudden death due to other causes were also included in the study as negative controls as well as for standardization of the TTC staining procedure. 10 Paraffin embedded tissue blocks of known, histologically proven, cases of MI were selected from the preserved blocks and used as positive controls and for standardization of acridine orange fluorescence study.
Hearts obtained from the test cases were subjected to meticulous gross examination of all three coronary vessels and their major branches by serial transverse sectioning of the vessel to note the degree of atherosclerotic narrowing. Hearts with significant (75% or more) narrowing of one or more coronaries only were included in the test group. Complete transverse slices of ventricular myocardium from sites suggested by ECG; containing evident or suspected fresh infarct by gross appearance; significant degree of narrowing of vessel supplying the area etc were subjected to TTC macro test. In the absence of any of these pointers, multiple slices were studied. Routine microscopic examination of the suspected infarct/peripheral areas of a visible fresh infarct by H & E staining was also undertaken. In cases where there were no pointers for selection of tissue blocks, spiral-step sampling of myocardium in successive slices was undertaken and a minimum of 10 blocks were studied. Sections from the same blocks were also subjected to acridine orange fluorescence microscopic study.
TTC Macro Test
Knife-cut 1 cm thick fresh slice from ventricular part of heart, selected from an area likely to contain the infarct as per guidelines mentioned above, is incubated in 1% solution of 2,3,5 Triphenyl Tetrazolium Chloride (TTC) for 20-30 mins. The slice is dipped in running water before incubating to remove excess of blood from the surface of the slice. The incubating fluid is prepared by dissolving 1 gm of TTC powder in 100 ml of phosphate buffer of pH 8.5. The staining can be carried out at room temperature, although some authors advocate incubation at 37–40°C.
Appropriate sized wide mouthed container with screw cap, which can hold a complete transverse slice, is to be used to carry out the staining. We used a transparent plastic cylindrical container of 7.5 cm diameter and 9.5 cm height. During the process of incubation the container is to be closed by its screw cap and kept in a dark place. As exposure to air and light will make the solution lose its potency. TTC solution is freshly prepared everytime and is used within half an hour. The slice is to be immersed completely in the solution during the process, the upper surface of it being at least 2 cm below the fluid level. We found that 100 ml of 1% of TTC solution poured into the above sized container fulfils this criteria, when one slice of heart is immersed into it. The most important precaution of all is to regulate the pH of the incubating fluid at 8.5 otherwise the formation of formazan pigments will be unsatisfactory. For better results the slice should be turned over once or twice during the process. At the end of the staining procedure the slice is transferred to a jar containing 10% formal saline. This will halt the reaction immediately in addition to fixing the tissue.
On completion of the staining the infarcted myocardium will show up as pale pink coloured area as against the bright red coloured normal myocardium. Even old infarcts and scars get delineated. In the absence of infarction, both the surfaces of the slice will show uniform bright red coloration.
The results can be photographed or the slices themselves can be preserved as museum specimen by Gough-Wentworth method of gelatin embedding and paper mounting. Photographic preservation of results was used in our study and some of the results are illustrated.
Another aspect studied was the duration of PM interval upto which the procedure can be used. It was found that if the body has been preserved in cold storage the reaction could be carried out even upto 68 hours after death. At 72 hours the colour developed was not only less intense but also was not uniform. This will give a false positive result.
The above staining procedure is the one recommended by Knight B [1] and Lie JT et al [2].
Acridine Orange Fluorescence Study
This study is carried out with the aim of detecting infarcts of 2 hours age. Thin sections of Paraffin embedded myocardial tissue from areas containing infarcts are stained with acridine orange and studied under UV fluorescent microscope. Infarcted tissue is detected by its bright grass green fluorescence as against the golden brown fluorescence of normal myocardium.
Staining procedure
-
1.
1% solution, of Acridine Orange was prepared by dissolving 1 gm of the powder in 100 ml of Phosphate buffer of pH 7.2
-
2.
Paraffin embedded sections were brought to water.
-
3.
Staining with acridine orange solution was effected for 3-5 secs, the slides being continuously adjusted during this time to avoid non specific deposition of acridine orange.
-
4.
The stained sections were repeatedly rinsed in phosphate buffer for 10–15 min using 2–3 changes of buffer solution. This resulted in washing away of non-specific deposits of the stain.
-
5.
The sections were then mounted in buffer solution and viewed under UV Fluorescent microscope immediately.
At the end of the staining the sections attained moderately dark brown colour to the naked eye, the correct intensity of which could be judged after gaining some experience.
Examination under fluorescent microscope using low power magnification revealed infracted tissue by its grass green colour. The intensity of the green colour was directly proportional to the severity of the damage-established scar tissue being brightest; early infarcts showing only light green fluorescence. Intermediate grades of infarcts showed different shades of green colour according to the severity of the process. Considerable difficulty was experienced in picking up the fine tinge of light green fluorescence of early infarcts till expertise was gained.
Acridine orange fluorescence study has been used by many workers for detection of early infarcts and its specificity and sensitivity has been established by workers like AL-Rufaie H.K. et al [3] and Knight B [1]. Other workers who have carried out similar studies are Sahai VB and Knight B [4]; Hecht A and Wehr M [5] and Yashoda Rani et al [6].
Results
Eighteen cases of death due to suspected MI were subjected to the study. Of these 13 were male and five were female. Eleven persons belonged to >60 years age group. Four persons were aged between 41 to 59 years. The remaining 3 persons were of less than 40 years. In four cases the survival time after onset of symptoms was between 2-4 hours. In one case it was 5½ hours. Of these five cases, two showed acute MI only, which was detected by acridine orange study alone. Two cases showed acute on chronic infarcts. In these cases too the acute infarcts were detected by acridine orange study while the old infarcts were visible even in H & E stained sections. In all these cases the survival time was around two hours after onset of symptoms. The fifth case, although the survival time was around 5½ half hours, showed early scarring in H & E sections. Thus acridine orange staining helped to detect infarcts of around two hours of age. Other cases with older infarcts too were subjected to acridine orange study. These pieces of infarcted myocardium showed varying degrees of green fluorescence, intensity of which was directly proportional to the extent of damage. Thus, while established scars showed bright green fluorescence, early infarcts were of light green colour. These and the known cases of MI (controls) helped in gaining experience in detecting finer change in the shades of green fluorescence.
Since the only case with post infarction survival time around 5½ hours showed much older infarct under H & E staining, TTC staining did not serve any diagnostic purpose in our study. However, it helped in the study of other cases with much older infarcts by way of causing better delineation of the infarct and the extent of such infarcts was revealed to be 1 mm more than as seen by naked eye before TTC staining. This helped in taking tissue sections for H & E study from areas sustaining sub lethal damageedge of the infarct.
Thus the results of our study establish the usefulness of TTC and acridine orange fluorescence, staining in detecting infarcts which are ‘invisible’ by H & E staining. In addition these procedures have a role to play in the study of older infarcts too. These results are consistent with the inferences drawn by Brody et al [7] and Yashoda Rani et al [6]. The results of the study, (TTC staining), are illustrated in Fig. 1, Fig. 2, Fig. 3.
Fig. 1.
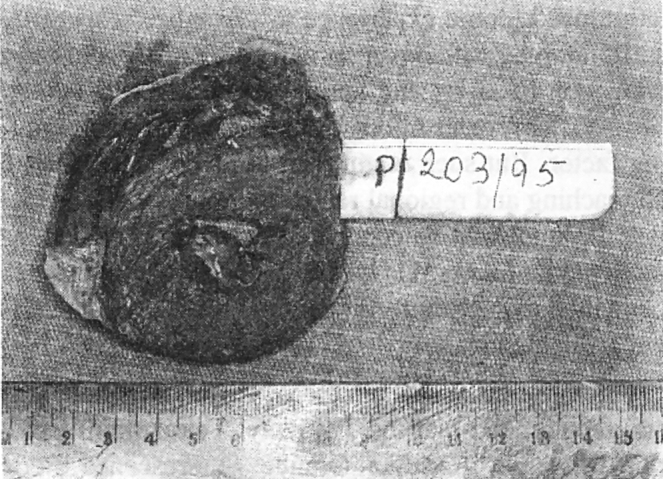
TTC stain – Normal myocardium uniformly stained.
Fig. 2.
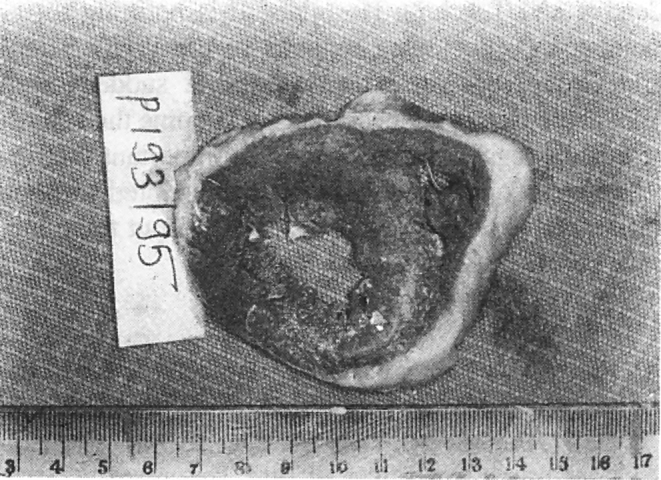
TTC stain – Old infarct seen as pale stained area.
Fig. 3.
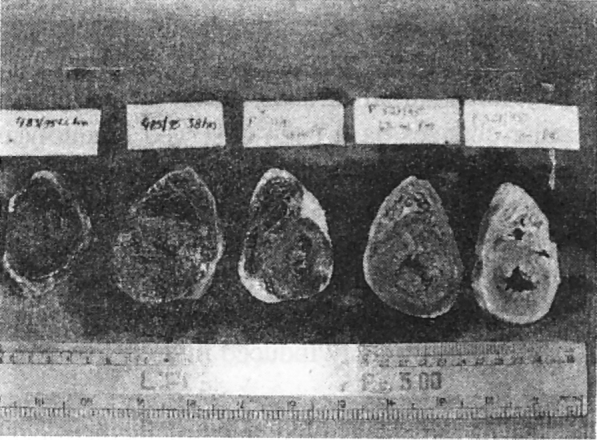
TTC stain – slices of normal myocardium stained after different PM intervals; pigment deposition (TTC stain) uniform upto 62 hours.
Discussion
The absence of gross as well as microscopic changes before the appearance of neutrophils at the scene of infarct, which is estimated to take minimum of 6-8 hours in terms of post-infarction survival time, has been a major hurdle in establishing the cause of death in cases of early death due to myocardial infarction.
Since biochemical alterations following injury to any tissue form the basis of pathological changes observed subsequently, different studies were conducted by workers to recognise the biochemical alterations. In the event of ischaemia persisting beyond 20 mins, the resultant injury leads to irreversible myocardial cell death-infarction. Obviously the changes include microscopic and metabolic changes occurring in the early part of the process. Following death of myocardial cells, electrolytes like K+, Mg++, phosphates etc which were kept inside the cell by active energy pumps, are lost to the interstitial space. Similarly, enzymes and low molecular weight co-factors diffuse out of the dead cell and enter the blood stream. The detection of enzymes specific to the myocardial cell, in increased quantities in the peripheral blood thus indicates irreversible myocardial cell death. In addition, other intracellular substances like the energy binding phosphates and glycogen are degraded inside the cell. Even at this stage the morphology of these dead cells remains normal to routine technique of light microscopy. However, the decreased activity of the enzyme systems and the altered biochemical structure of the cell interior can be demonstrated by histochemical techniques. The TTC reaction depends upon the activity of multiple dehydrogenase enzymes. Absence of the dehydrogenase enzyme activity either due to leakage of the enzyme or due to exhaustion of glycogen stores from within the dead cell, leads to non deposition of formazan pigments over the area of infarction. It can further be pointed out at this stage that dehydrogenases disappear from non-infarcted myocardium after about 60 hours if the heart is refrigerated and 36 hours if not [1]. This means that autolysis and infarction have different effects over the dehydrogenases as the enzymes disappear from the infarcted tissue after as early as 6 hours.
Apart from TTC reaction, many other histochemical methods based on changes in the activity of various enzyme systems have been recommended by the WHO Scientific Group [8] for early diagnosis of MI.
As regards changes in the Acridine Orange Fluorescence pattern of infarcted cells, there is much to be learnt about the intracellular changes causing it.
Mention must be made of Electron Microscopic (EM) studies carried out to diagnose early changes in infarcted tissue. Such studies have revealed depletion of peri-nuclear glycogen, increase in the sarcoplasmic space, peripheral aggregation of nuclear chromatin and mitochondrial structural changes. Unfortunately similar changes have been observed in autolysing tissues. The changes produced by autolysis are in fact artifacts. In future improved methods of fixation and embedding may be developed limiting such artifacts enabling better evaluation of early infarcts. Till then EM will remain only an experimental tool applicable to study of artificially induced infarcts in animal models.
One of the major objectives of medico-legal postmortem is to establish the cause of death. Exact diagnosis of the cause of death has wide-ranging implications. Apart from making the official recording of death more authentic, it helps to solve many civil and criminal problems especially when the death has occurred under suspicious or unattended circumstances. Needless to emphasize the amount of unnecessary wastage of effort and resources of investigative agencies that will be saved, apart from the agony to the bereaved family members, if such deaths can be conclusively proved to be due to a natural cause like myocardial infarction. Another field where the diagnosis of myocardial infarction as cause of death is of immense relevance is in cases of aviation accidents. Many times the cause of such accidents has been proved to be Acute Myocardial Infarction sustained by the pilot, while in flight. This helps not only in reconstruction of events but also in taking preventive measures like periodic thorough medical check-ups of pilots. Keeping all this in view as well as the limitations of current methods of diagnosis which depend mainly on the indirect evidence of critical atherosclerotic narrowing of coronaries, this study was conducted to establish the validity of the TTC macro staining method and acridine orange fluorescence staining method as means of demonstrating Early Myocardial Infarcts (of less than 6 hours age).
The study has been able to establish the usefulness of the two procedures in diagnosing the infarcts of around 2 hours of age. The techniques of both the procedures are quite simple and easy to perform. The reagents required are not out of reach (financially) of a moderate sized laboratory. As regards interpretation of results, the TTC macro-method did not pose any problems. The acridine orange fluorescence study interpretation needs some experience to ‘visualize’ especially early infarcts, which can be gained by any pathologist with a bit of effort and aptitude. The non-availability of U-V fluorescent microscope might become a limiting factor. But such equipment is readily available in all teaching and regional referral laboratories. The fact that the study can be conducted on paraffin embedded sections eliminates this hurdle as the tissue blocks can be mailed to such ‘referral centres’ if the equipment is not available locally.
Having considered all these aspects we conclude and recommend that the Triphenyl Tetrazolium Chloride Test and Acridine Orange Fluorescence study should be included in the study protocol of all sudden death cases, at least at the level of Regional Referral Centres and Teaching Hospitals. It is befitting to remember the concluding remarks of the WHO Scientific Group [8]-“Since many cases of sudden death from acute ischaemic heart disease become the subject of medico-legal autopsy, it is most important that forensic pathologists should be well acquainted with the most suitable techniques and be able to put them into practice”.
REFERENCES
- 1.B Knight, In: Camps FE, Editor, Myocardial Ischaemia-Recent advances in Forensic pathology. 1969 : 20-34
- 2.Lie JT, Pairolero PC, Keith HE, Titus JL. Microscopic enzyme mapping-verification of large, homogeneous, experimental myocardial infarcts of predictable size and location in dogs. J Thorac Cardiovasc Surg. 1975;69:599–605. [PubMed] [Google Scholar]
- 3.Al-Rufaie HK, Florio RA, Olsen EG. Comparison of HBFP method and fluorescence of H & E stained sections for identification of early myocardial infarction. J Clin Pathol. 1983;36(6):646–649. doi: 10.1136/jcp.36.6.646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sahai VB, Knight B. The postmortem detection of early myocardial infarction by fluorescent method. Med Sci and Law. 1976;16:1. doi: 10.1177/002580247601600106. [DOI] [PubMed] [Google Scholar]
- 5.Hecht A, Wehr M. The so-called Paling off the heart muscle and its value in expression of ischaemic myocardial damage. Zentralbl Allg Pathol (Germany-East) 1985;130(6):467–471. [PubMed] [Google Scholar]
- 6.Yashoda R, Dikshit PC, Kumar B. Journal of Forensic. Medicine and Toxicology. 1994;2:15–20. [Google Scholar]
- 7.Brody GL, Belding WH, Belding RM, Fieldman SA. The identification and delineation of myocardial infarcts. Arch Pathology. 1967;84:312. [PubMed] [Google Scholar]
- 8.WHO Scientific Group. The Pathological diagnosis of acute ischaemic heart disease. WHO Tech Rep Ser 1970; 441:5-27 [PubMed]


