Introduction
Mediastinal fibrosis, also referred to as chronic or sclerosing mediastinitis, is a rare condition and constitutes a small fraction of all mediastinal diseases. It causes slow progressive and dense fibrosis of the mediastinum. Specific etiology of this condition is unknown. However most cases are thought to be associated with tuberculosis or histoplasmosis, but sarcoidosis, silicosis, and other fungal diseases are at times causative [1, 2]. It is hypothesized that fibrosing mediastinitis results from a delayed hypersensitivity reaction to fungal, mycobacterial or other antigens. Furthermore, irrespective of the underlying cause hilar nodes undergo a caseous, granulomatous reaction with perinodal fibrosis [3]. Riedel's thyroiditis and other autoimmune disorders are sometimes associated with mediastinal and retroperitoneal fibrosis [4]. Progressive entrapment of the pulmonary veins, superior vena cava, pulmonary arteries, aorta, portion of tracheobronchial tree, phrenic or recurrent laryngeal nerve and oesophagus either alone or in various combinations may take place over many years. Diagnosis is difficult and invariably needs biopsy of the tissue from mediastinum in addition to imaging procedures like Computerized Tomography (CT) and Magnetic Resonance Imaging (MRI). We present a case of mediastinal fibrosis who had left recurrent laryngeal and phrenic nerve palsy.
Case Report
A 40-year-old army officer was in good health till Jan 98 when he developed hoarseness of voice and dry cough. His symptoms progressed gradually over the period of next 8 months. He also developed low-grade fever 15 days prior to admission in August 98. There was no history of exposure to any dust or drugs like Methysergide.
On examination he was 180 cm in height and weighed 75 kg. There was no pallor, clubbing, icterus or lymphadenopathy. He was afebrile with pulse 78/min, BP 120/70 mm Hg and respiratory rate 18/min. Chest examination revealed vesicular breath sounds bilaterally with no adventitious sounds. There was no hepatosplenomegaly. Indirect laryngoscopy revealed left vocal cord palsy. Other systems were normal.
Investigations:-Hb 11.5 gm/dl, TLC 8300/cmm, DLC P67 L30 E2 M3, Blood Sugar Fasting 92 mg%, PP 116 mg%. Renal and Liver function tests were normal, Mantoux 15 mm, Electrocardiogram and Pulmonary Function Tests were normal. Sputum was negative for AFB and malignant cells. Chest radiograph (Fig-1) showed a raised dome of left diaphragm and opacity just above left hilum and merging with it. Fibreoptic bronchoscopy and ENT examination confirmed left vocal cord palsy. Tests for ANF, LE cells and dsDNA were negative.
Fig. 1.

Chest radiograph PA view showing raised dome of left diaphragm and an opacity just above left hilum and merging with it.
CT thorax showed ill-defined lesion of soft density, which could not be differentiated from aortic arch. MRI (Fig-2) showed a soft tissue mass lesion (isointense to muscle) in superior mediastinum surrounding the aortic arch and its branches. Aorta did not show any aneurysm or dilatation. An open biopsy with a midline sternotomy showed a hard mass (5×3×2 cm) overlying the aortic arch and its branches in anterior mediastinum, which was densely adherent to the vessels. Macroscopically it was yellowish greasy soft tissue, which on cut section showed foci of greyish black areas. Histopathology of mass showed thick fibrocollagenous bands with scattered mononuclear inflammatory cells (Fig-3). A diagnosis of chronic fibrosing mediastinitis was made and he was exhibited steroids for 3 months and ATT (2EHRZ/4HR).
Fig. 2.
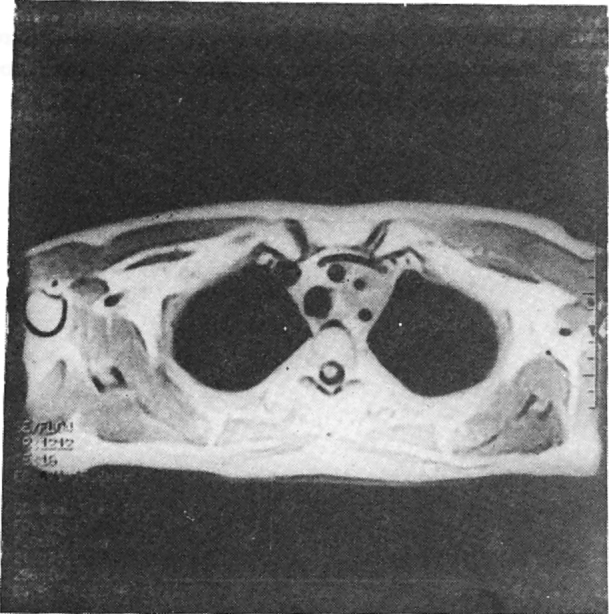
MRI of chest showing a soft tissue mass lesion in superior mediastinum surrounding the aortic arch and its branches.
Fig. 3.
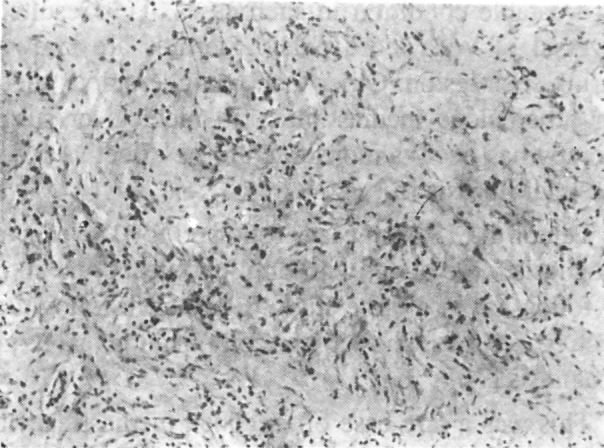
Microsection of the biopsy (low power) showing thick fibrocollagenous bands with scattered mononuclear inflammatory cells
A review after twelve months did not show any change in chest roentgenogram and Pulmonary Function Tests but indirect laryngoscopy showed normal movement of both vocal cords suggesting reversal of left recurrent laryngeal nerve palsy. The patient gained 15 kgs weight in one year post-treatment and was asymptomatic.
Discussion
The spectrum of chronic mediastinitis ranges from granulomatous inflammation of the lymph nodes in the mediastinum to fibrosing mediastinitis. Specific aetiology is unknown, however, most cases are thought to be due to tuberculosis or histoplasmosis, but sarcoidosis, silicosis, and other fungal diseases are at times causative. Patients with granulomatous mediastinitis are usually asymptomatic. Those with fibrosing mediastinitis usually have signs of compression of some mediastinal structure such as the superior vena cava or large airways, phrenic or recurrent laryngeal nerve paralysis, or obstruction of the pulmonary artery or proximal pulmonary veins [1].
The site of lesion can be localised in the mediastinum as in the present case it was localised in anterior mediastinum and involved left phrenic and recurrent laryngeal nerves. Lerner and Katz reported such localised left vocal cord palsy associated with oesophageal diverticulum due to mediastinal fibrosis [5]. Baslaim and deVarennes reported similar localised idiopathic fibrosing mediastinitis as a cause of SVC syndrome [6]. Sometimes it may progress to involve the retroperitoneum [4]. Depending on the site of lesion various structures became progressively encased by the fibrosis resulting in entrapment of arteries, veins, nerves or other hollow structures like trachea, bronchi and oesophagus [6, 7, 8]. Papandreou et al reported idiopathic mediastinal fibrosis in a 45-year-old army officer who presented with left pulmonary artery occlusion and left upper lobe stenosis [9].
Riedel's thyroiditis and other autoimmune disorders are sometimes associated with mediastinal and retroperitoneal fibrosis. Our patient did not show any-features of autoimmune disorder, also his blood was tested negative for ANF, LE cells and dsDNA.
CT and MRI are important diagnostic tools to demonstrate mediastinal opacity. MRI is definitely better than CT as proved in this case. The ability to perform T1-and T2-weighted images allows clear delineation of mediastinal masses from surrounding soft tissue.
Surgery is performed in most cases to exclude malignancy. Biopsy and histopathology diagnose most cases of mediastinal fibrosis. In the present case it is the mediastinal exploration and subsequent histopathology, which not only ruled out malignancy but also established benign fibrosis as the underlying cause. The mass was as hard and dense as in most malignant cases. Only rarely acid-fast bacilli can be found in caseous residua of lymph nodes of such lesions.
Since the patient had fever, positive Mantoux and history of weight loss, ATT along with corticosteroids were given, as tuberculosis is thought to be commonest treatable condition in such cases. This resulted in reversal of vocal cord palsy. Steroids are known to shrink such lesion. Other than antituberculous therapy for tuberculous mediastinitis, no medical or surgical therapy has been demonstrated to be effective for mediastinal fibrosis [5].
Ten of the 18 such cases followed for 15 years after diagnosis were alive, with only two death and six lost to follow up in a large study. Long-term follow up of such cases has shown no complications and good prognosis [7].
This was a rare case of localized mediastinal fibrosis, scant reported from our country, especially in Armed Forces. Reversal of left recurrent laryngeal nerve palsy with ATT and steroids is an uncommon event. To conclude sclerosing mediastinitis is a slowly progressive condition associated with tuberculosis and outlook is excellent.
REFERENCES
- 1.Light RW. Disorders of the pleura, mediastinum and diaphragm. In: Fauci AS E Braunwald Harrison's Principles of Internal Medicine. McGraw-Hill. 1998:1472–1476. [Google Scholar]
- 2.Schowengerdt CG, Suyemoto R, Main FB. Granulomatous and fibrous mediastinitis: A review and analysis of 180 cases. J Thorac Cardiovasc Surg. 1969;57:365–379. [PubMed] [Google Scholar]
- 3.Goodwin RA, Nickell JA, Des Prez RM. Mediastinal fibrosis complicating healed primary histoplasmosis and tuberculosis. Medicine. 1972;51:227–246. doi: 10.1097/00005792-197205000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Comings DE, Skubi KB, Eyer JV, Motulsky AG. Familial multifocal fibrosclerosis: Finding suggesting that retroperitoneal fibrosis, mediastinal fibrosis, sclerosing cholangitis, Riedel's thyroiditis and pseudotumor of the orbit may be different manifestations of a single disease. Ann Intern Med. 1967;66:884–892. doi: 10.7326/0003-4819-66-5-884. [DOI] [PubMed] [Google Scholar]
- 5.Lerner MA, Katz R. A new syndrome of left vocal cord paresis and esophageal diverticulum due to mediastinal fibrosis. Am J Roentgenol Radium Ther Nucl Med. 1975;125:193–197. doi: 10.2214/ajr.125.1.193. [DOI] [PubMed] [Google Scholar]
- 6.G Baslaim, deVarennes B. Localized idiopathic fibrosing mediastinitis as a cause of superior vena cava syndrome: a case report. Can J Surg 1998:41(1):68-71. [PMC free article] [PubMed]
- 7.Mole TM, Glover J, Shepard MN. Sclerosing mediastinitis. A report on 18 cases Thorax. 1995;50:280–283. doi: 10.1136/thx.50.3.280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kalweit G, Huwer H, Straub U, Gams E. Mediastinal compression syndromes due to idiopathic fibrosing mediastinitis-report of three cases and review of the literautre. Thorac Cardiovasc Surg. 1996;44(2):105–109. doi: 10.1055/s-2007-1011996. [DOI] [PubMed] [Google Scholar]
- 9.Papandreou L, Panagou P, Bouros D. Mediastinal fibrosis and radiofrequency radiation exposure: Is there any association? Respiration. 1992;59:181–184. doi: 10.1159/000196054. [DOI] [PubMed] [Google Scholar]


