Abstract
In two meta-analyses on gender differences in depression in nationally representative samples we advance previous work by including studies of depression diagnoses and symptoms to 1) estimate the magnitude of the gender difference in depression across a wide array of nations and ages; 2) use a developmental perspective to elucidate patterns of gender differences across the lifespan; and 3) incorporate additional theory-driven moderators (e.g., gender equity). For major depression diagnoses and depression symptoms, respectively, we meta-analyzed data from 65 and 95 articles and their corresponding national datasets, representing data from 1,716,195 and 1,922,064 people in over 90 different nations. Overall, OR = 1.95, 95% CI [1.88, 2.03] and d = 0.27 [0.26, 0.29]. Age was the strongest predictor of effect size. The gender difference for diagnoses emerged earlier than previously thought, with OR = 2.37 at age 12. For both meta-analyses, the gender difference peaked in adolescence (OR = 3.02 for ages 13–15, and d = 0.47 for age 16) but then declined and remained stable in adulthood. Cross-national analyses indicated that larger gender differences were found in nations with greater gender equity, for major depression, but not depression symptoms. The gender difference in depression represents a health disparity, especially in adolescence, yet the magnitude of the difference indicates that depression in males should not be overlooked.
Keywords: depression, gender, meta-analysis, development, gender equity
Depression is a global health priority. According to the (World Health Organization 2016), depression accounts for fully 10 percent of the total non-fatal disease burden worldwide. Moreover, this burden falls disproportionately on girls and women. In one study, the global 12-month prevalence of major depressive disorder was 5.8% in females and 3.5% in males (Ferrari et al., 2013). The gender difference in depression – generally believed to be twice as many females experiencing major depression as males – represents a major health disparity. However, despite assertions that the gender difference in depression is among the most robust of findings in psychopathology research (e.g., Bebbington, 1996), and extensive empirical and theoretical work on gender differences in depression, this large body of sometimes inconsistent research has yet to be synthesized meta-analytically. The current set of meta-analyses advance previous work by including studies of depression diagnoses as well as symptoms to 1) estimate the magnitude of the gender difference in depression; 2) use a developmental lens to elucidate the patterns of gender differences across the lifespan; and 3) examine theory-driven, conceptually relevant moderators (e.g., nation-level gender equity).
Background
In the 1970s, Myrna Weissman first underscored the gender difference in depression, noting that approximately twice as many females experience depression as males among adults in clinical and community samples (Weissman & Klerman, 1977). Following this landmark article, there was a proliferation of research and theories on gender differences in depression (Bebbington, 1996; Kuehner, 2003; Nolen-Hoeksema, 1987; Piccinelli & Wilkinson, 2000; Weissman & Klerman, 1977; for an overview of explanatory models, see Hammerström, Lehti, Danielsson, Bengs, & Johansson, 2009). In the vast majority of epidemiological reports on adults, women have higher rates of major depression compared to men; on average, the ratio is 2:1 (Andrade et al., 2003; Bromet et al., 2011). However, findings also suggest that the 2:1 ratio is not universal and may vary substantially across nations. For example, in 18 countries from the WHO World Mental Health Surveys (Kessler & Usten, 2008), odds ratios (ORs, female/male) for 12-month major depressive episode (MDE1) ranged from 1.2 to 2.7 across 18 countries and 89,037 participants (Bromet et al., 2011). Given this variability, it is critical to use meta-analysis to estimate the overall magnitude and consistency of the gender difference in depression across different nations and with different assessments of major depression. Other widely held beliefs about gender differences, such as the gender difference in math performance, have sometimes been found to be inaccurate when the data are meta-analyzed (Hyde, Lindberg, Linn, Ellis, & Williams, 2008; Lindberg, Hyde, Petersen, & Linn, 2010). Moreover, given evidence of cross-national variations, it is important to understand nation-level variables (e.g., economic development, gender equity) that may account for variability in the magnitude of the gender difference.
In addition to examining variations in the gender difference in depression across nations, it is also critical to take a developmental perspective. Several studies indicate that, among the general population, there is no gender difference or even a somewhat higher prevalence of depression among boys than girls in childhood (Avenevoli, Knight, Kessler, & Merikangas, 2008; Twenge & Nolen-Hoeksema, 2002). The female preponderance in depression is thought to emerge by ages 13–15 (e.g., Hankin et al., 1998; Twenge & Nolen-Hoeksema, 2002; Wichstrøm, 1999; Wade, Cairney, & Pevalin, 2002). However, research on the time course of the emergence of the gender difference in adolescence has been accepted as a fundamental fact in the depression literature when it is actually based on only a few studies. For example, in a landmark article, Hankin and colleagues (1998) found that the gender difference in clinical depression emerged by ages 13–15 and then widened between ages 15 and 18. This conclusion has been widely accepted (the article had been cited 1693 times as of December 2016) based on findings from one sample from one region of New Zealand (see Kessler, McGonagle, Swartz, Blazer, & Nelson, 1993, for the other widely cited study on gender differences in adolescence, based on U. S. data). A meta-analysis on gender differences in depression with a developmental focus is the next major step in order to pinpoint the time course of the emerging gender difference in depression.
Additionally, developmental patterns of the gender difference beyond adolescence have been largely neglected empirically. The limited findings in adulthood are inconsistent with respect to both the magnitude and direction of the gender difference in depression (Angst et al., 2002; Mirowsky, 1996; Oksuzyan et al., 2010; Patten et al., 2016; Bebbington et al., 1998). Additionally, estimates of the gender difference in depression in older adults suggest marked variability. A meta-analysis of 24 studies among individuals ages 75 and older reported gender ratios between 1.4 and 2.2 (Luppa et al., 2012). It was one of the goals of the current meta-analyses to bring clarity to developmental patterns throughout the lifespan.
Lastly, despite much attention to the 2:1 ratio for the gender difference in major depression, the magnitude of the gender difference in levels of depression symptoms in the general population has received less attention. Psychiatric research in the past several decades has focused on the use of diagnostic categories as specified in the Diagnostic and Statistical Manual of Mental Disorders (DSM; American Psychiatric Association, 1980–2013) and International Classification of Disease (ICD; World Health Organization, 1992). However, there is increased recognition of the validity (e.g., Markon, Chmielewski, & Miller, 2011) and value (Cuthbert & Insel, 2013) of dimensional assessments, as well as the impairment associated with sub-threshold levels of symptoms that do not meet diagnostic criteria. Indeed, adolescents and adults with subthreshold depression symptoms and minor depression still experience significant impairment (e.g., Lewinsohn, Solomon, Seeley, & Zeiss, 2000) and are at elevated risk for later development of major depression and suicidal behaviors (Cuijpers, de Graaf, & van Dorsselaer, 2004; Fergusson, Horwood, Ridder, & Beautrais, 2005; Klein, Shankman, Lewinsohn, & Seeley, 2009). These important subthreshold levels are captured in symptom questionnaires; however, extant research on the magnitude of gender differences in depression symptoms is limited. One meta-analysis reported effect sizes ranging from d = −0.06 at age 12 to d = +0.22 at ages 14 and 15 (positive values indicate more depression symptoms among girls; Twenge & Nolen-Hoeksema, 2002). Although this study represented a step forward in the research literature, it was limited to the Children’s Depression Inventory (CDI; Kovacs, 1985) scale and samples of 8- to 16-year-old participants in the United States and Canada (n = 43,916). Given the impairment associated with high levels of depression symptoms in the absence of a diagnosis, it is critical to estimate the magnitude of the gender difference in depression symptoms more comprehensively: throughout the lifespan, across nations, and with multiple symptom measurements.
Thus, in the current set of meta-analyses using nationally representative samples, we estimated the magnitude of the gender difference in (1) major depression diagnoses and (2) levels of depression symptoms. Moreover, meta-analysis allowed us to chart the developmental course of the gender difference from childhood through late adulthood. Meta-analysis also enabled us to test whether the gender difference is universal across nations or whether there are cultural factors such as gender inequality that account for cross-national variations.
Gender Differences in Depression across the Lifespan
Based on both developmental psychopathology theory and past research (reviewed above), age was used as a moderator in the current set of meta-analyses to answer one of our fundamental questions: What is the pattern of gender differences in depression across the lifespan?
There now is consensus that the gender difference in depression has a multifactorial etiology (Cyranowski, Frank, Young, & Shear, 2000; Hyde, Mezulis, & Abramson, 2008). Theories of developmental psychopathology contend that there are multiple pathways to the gender difference in depression involving combinations and interactions of risk factors that span multiple levels of analysis (Cicchetti & Rogosch, 2002). Importantly, these pathways to the gender difference in depression occur in a developmental context. Theories highlight how specific vulnerability factors come on-line at critical developmental periods in adolescence and/or interact with stressors in adolescence to produce the gender difference in adolescence (reviewed by Hyde et al., 2008b). For example, there is a confluence of hormonal and neurodevelopmental changes that vary by sex during the pubertal transition and may influence the gender difference in depression. Thus, a developmental approach is key to understanding patterns in the gender difference across the adolescent transition and to understand if the gender difference persists across the lifespan.
In contrast to the focus on the emergence of the gender difference in adolescence, researchers have largely ignored development in adulthood when theorizing about and examining gender differences in depression. The field of developmental psychopathology encourages a lifespan perspective, as the process of adaptation continues from childhood through adulthood (Cicchetti & Rogosch, 2002). For example, with regard to depression, little is known about levels of stress for women compared with men across adulthood, nor about the importance of various life transitions in adulthood. Theorizing about gender differences in depression will be enriched by an understanding of developmental patterns across adulthood and it was one of the goals of these meta-analyses to elucidate those developmental patterns.
Gender Differences in Depression across Nations
Past research indicates variability in the magnitude of the gender difference in depression across nations. We used sociological theory and social-structural theory to guide our use of nation-level economic and gender equity indicators as moderators in the current set of meta-analyses.
Sociological theories
Sociological approaches to mental health emphasize the role of poverty, violence, and gender inequality as factors contributing to the gender difference in depression. Abundant evidence suggests a relationship between financial hardship and depression in both sexes (Reiss, 2013). Because of the feminization of poverty (Belle, 1990; Belle & Doucet, 2003), and the link between poverty and depression, gender differences might also be linked to income inequality and a national’s overall wealth. Similar to financial hardship, victimization is also related to depression in both males and females. To the extent that women report higher rates of violent victimization, this may contribute to the gender difference in depression (Koss et al., 1994). Lastly, gender inequality is linked to discrimination against women, which may contribute to the gender difference (Belle & Doucet, 2003). Thus, in the current meta-analyses we investigated nation-level economic factors and gender-equity indicators as moderators of the gender differences in depression.
Social-structural theory
Eagly and Wood’s social-structural theory (1999; Wood & Eagly, 2012) also provides a framework for understanding the relationship between gender inequality and the magnitude of psychological gender differences. According to the theory, a society’s division of labor by gender drives all other psychological gender differences. These gender differences result from individuals’ adaptations to the particular restrictions on or opportunities for their gender in their society. The theory predicts that larger gender differences should be observed in nations with more gender inequality. Evidence for this theory exists for several psychological gender differences, including mate preferences, mathematics performance, and some aspects of sexuality (Eagly & Wood, 1999; Else-Quest, Hyde, & Linn, 2010; Petersen & Hyde, 2010; Zentner & Mitura, 2012). However, other studies have found smaller gender differences in nations with more gender inequality. This pattern has been found for outcomes such as self-reports of personality traits and attitudes about mathematics (Else-Quest et al., 2010; Wood & Eagly, 2012). In the current meta-analyses, we sought to determine which of these patterns would occur (larger or smaller gender differences in nations with more gender inequality) when the outcome was gender differences in depression.
Cross-national variations: Research on economic and gender equity factors
Research on the relationship between nation-level economic factors and gender differences in depression is sparse. A study including 18 countries from the WHO World Mental Health Surveys (Kessler & Usten, 2008) reported that the relationship between gender and MDE did not differ significantly between high-income and low- to middle-income countries, suggesting that economic development does not explain the varying magnitudes of gender differences in different countries (Bromet et al., 2011). Alternatively, a different measure of nation-level economic development may be more sensitive in detecting a relationship to the gender difference in depression. In the current set of meta-analyses, we used two different measures of economic development (income category and income inequality; defined below) and included a more complete set of nations to examine the relationship between nation-level economic factors and gender differences in depression more comprehensively.
Nation-level gender equity indicators are increasingly being used in psychological research (Else-Quest & Grabe, 2012); however, few studies have investigated the relationship between nation-level gender equity and gender differences in depression. Two large multi-nation studies have reported conflicting results, finding that the gender gap in depression was smaller and larger, respectively, in low gender-equity countries compared to high gender-equity countries (Hopcroft & Bradley, 2007; Van de Velde, Huijts, Bracke, & Bambra, 2013). This relationship is especially complex given the multiple available measures of gender equity. We selected domain-specific indicators of gender equity (rather than composite indicators) that should, theoretically, be tied to gender differences in depression (e.g., contraceptive prevalence, representing a woman’s ability to control her own reproduction).
Additional Factors Influencing the Gender Difference in Depression
In addition to examining age and cross-national variations in national wealth and gender equity as moderators, we also explored whether the magnitude of the gender difference in depression varied according to ethnicity (in U.S. samples only) and over time, i.e., whether it is growing larger or smaller.
Ethnicity in the U.S. and Intersectionality
The extant literature indicates that the prevalence of major depression in the United States varies both by gender and by ethnicity (e.g., Breslau, Kendler, Su, Gaxiola-Aguilar, & Kessler, 2006). However, few studies have tested whether gender differences in depression vary by ethnicity. The importance of this question is highlighted in intersectionality theory, which emphasizes that all people belong to multiple social categories and that these categories are intertwined (Cole, 2009; Else-Quest & Hyde, 2016a). According to this approach, the category of gender should not be considered in isolation, but should be analyzed as it intersects with other categories such as ethnicity. Empirical evidence for these assertions is abundant; space does not permit a thorough review here (for reviews, see Else-Quest & Hyde, 2016a, b).
The limited research on ethnicity, gender, and depression in the United States does not indicate variation by ethnicity in the gender difference in depression (Barnes, Keyes, & Bates, 2013; Breslau et al., 2006; Oquendo et al., 2001; Siegel, Aneshensel, Taub, Cantwell, & Driscoll, 1998). Nonetheless, other meta-analyses on gender differences for related constructs have found notable variations across U.S. ethnic groups. For example, a meta-analysis of gender differences in self-esteem found a small difference favoring Caucasian males over Caucasian females, d = 0.20, but no gender difference for African American samples, d = −0.04 (Kling, Hyde, Showers, & Buswell, 1999). Therefore, it was important to test whether gender differences in depression vary across U.S. ethnic groups. We did not conduct analyses stratified by ethnicity in other nations because ethnic groups are distinct in each country and often are not reported.
Trends over time
One recent narrative review concluded that internalizing problems for girls increased from the late 20th century to the 21st century (Bor, Dean, Najman, & Hayatbakhsh, 2014). The findings for boys were mixed as to whether they experienced an increase. In contrast, Seedat and colleagues (2009) found a significant narrowing in the gender difference in depression in recent cohorts. We therefore tested meta-analytically whether gender differences in depression are widening or narrowing over time.
Sampling Issues
The current set of meta-analyses synthesized data from representative samples, based on an approach pioneered by Hedges and Nowell (1995). They argued that the strongest scientific evidence about gender differences does not come from small studies of convenience samples, but instead comes from larger studies based on representative samples of populations. The Hedges and Nowell strategy has since been used in other meta-analyses on gender differences in cognitive abilities (e.g., Else-Quest et al., 2010; Reilly et al., 2015). Beginning around 1990, with the formation of cross-national collaboration groups studying psychiatric epidemiology (e.g., Cross National Collaborative Group, 1992), data sets based on representative samples became available for gender differences in depression. We were therefore able to use this strong methodology for the current meta-analyses.
The Current Study
Given the abundance of available research on gender differences in major depression and in depression symptoms, a meta-analysis is possible and is needed to address the following key questions:
How large is the gender difference in major depression? How large is the gender difference in levels of depression symptoms?
Following from developmental psychopathology approaches, what is the pattern of gender differences in depression across the life span? How does the direction or magnitude of the gender difference change across development (i.e., at what ages do gender differences appear or disappear, widen or narrow)?
Guided by sociological and social-structural theory, does the magnitude of gender differences vary as a function of the nations’ gender equity or wealth?
Following from an intersectionality approach, are there variations across U.S. ethnic groups in the direction or magnitude of these gender differences?
Have gender differences in depression widened over time, i.e., across cohorts from the 1970s to 2013?
Methods
Identification of Studies and Data Sets
Database searches
Computerized database searches of PsycINFO and PubMed were used to generate an initial pool of potential articles. To identify all relevant articles and related datasets, the following search terms (selected in consultation with a university librarian) were used in PsycINFO and PubMed, respectively: (depression OR depressive OR depressed) AND (sex OR gender); depression AND (gender OR sex OR sex factors)2. The search terms were optimized for each database (e.g., using MESH terms in PubMed) and were conceptually similar in terms of article yield. Search limits restricted the results to articles that discussed research with human populations and that were published between 1970 and October 4, 2016 (including online first publications). 1970 was chosen as the earliest year in order to capture reasonably contemporary research with modern symptom measures and diagnoses from structured interviews based on the DSM and ICD. PsycINFO and PubMed identified 29,003 and 28,383 articles, respectively, which were considered for inclusion. In this section and throughout this paper, we follow MARS reporting standards (American Psychological Association Publications and Communications Board, 2008; see also Moher, Liberati, Tetzlaff, Altman, & the PRISMA Group, 2009).
Abstract processing
Abstracts and citations were imported into Endnote citation manager. Duplicates were deleted, resulting in 46,512 abstracts (see Figure 1). The abstracts were examined for relevant content. At this stage, we included any studies with potentially relevant depression data and, to ensure the quality of sampling, were based on a nationally representative dataset. We included abstracts that explicitly mentioned “nationally representative.” Abstracts were excluded for any of the following reasons: (a) the sample was not nationally representative (e.g., clearly a community study or a convenience sample); (b) the sample consisted of only one gender; (c) the study reported no empirical data (e.g., a review article); (d) the research was qualitative; (e) the research was conducted on nonhumans; (f) the participants in the study were younger than seven years old (this age cut-off was selected because, for the sake of uniformity, we included only self-report measures of depression symptoms and not, for example, parent or teacher report; we did not restrict the age range in the computerized database searches in order to avoid missing articles that were not tagged with an age); and (g) the abstract did not mention depression or a related construct (e.g., anxiety, stress, internalizing, emotion, psychological distress, psychiatric disorder, mental health). 44,431 abstracts were excluded due to the aforementioned reasons, resulting in 2081 remaining articles. See Figure 1 for additional information.
Figure 1.
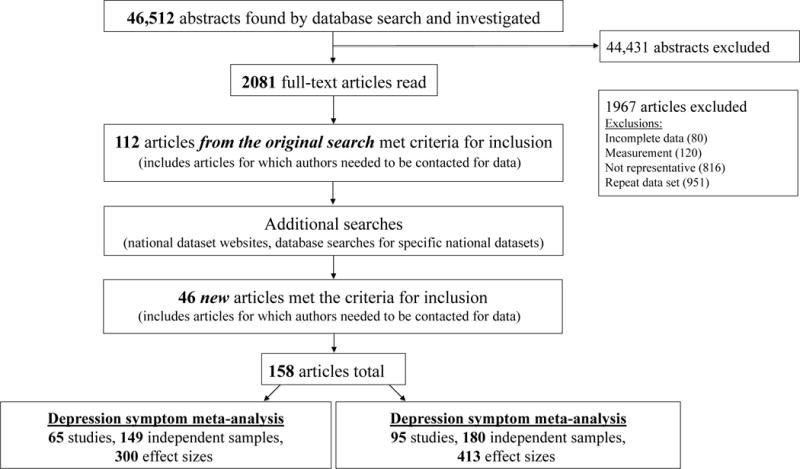
Flowchart of the search and selection procedure.
Article processing
The pdfs from these 2081 articles were retrieved and examined to determine whether the articles met the criteria for inclusion. At this stage, we excluded studies that were not based on national probability sampling. In other words, we included only population-based surveys representative of the country. We excluded national samples of college students, employees, veterans, twins, primary care patients, and married couples, as these samples do not represent the general population. We excluded representative samples that were limited to one large city or region or even several regions (if they were not randomly selected). We also excluded samples of inpatients or outpatients as this sampling strategy is vulnerable to the criticism that the study is detecting a gender difference in help seeking rather than an actual gender difference in depression (Nolen-Hoeksema, 1987; Pattyn, Verhaeghe, & Bracke, 2015). Nationally representative samples do include individuals currently receiving mental health treatment (unless they are institutionalized) or individuals with a history of receiving mental health treatment, so those individuals were not excluded.
Also, to ensure quality, studies that did not meet the measurement criteria were excluded at this stage. Studies were excluded if their measurement of depression symptoms did not meet the following criteria: 1) minimum of 3 items; 2) self-report; 3) Cronbach’s alpha ≥.70 (if provided); and 4) valid and reliable measure of depression based on previously published research3 (e.g., we excluded studies that used a general measure of psychological distress or negative affect). If a study used a measure that combined anxiety and depression subscales, we contacted the authors to obtain the data solely for the depression subscale.
Studies were excluded in the processing of articles if their measurement of depression diagnoses did not include a diagnostic interview with the participant. Thus, we excluded studies reporting depression diagnoses from the following sources: health insurance claims databases, participants’ self-report of physician-diagnosed depression, antidepressant use, and cut-off scores on depression symptom measures (e.g., a cut-off on the CES-D). We contacted authors who reported diagnoses based on symptom cut-off scores to obtain the continuous symptom data for the depression symptom meta-analysis.
If a particular sample of participants was used in more than one article, which was often the case with these national datasets, to maintain independence of samples, we selected the article that had the most complete data (including information on moderator variables such as age and ethnicity) and/or the largest sample size. For nationally representative longitudinal studies with multiple waves of data (e.g., Add Health), we included only one wave of data to maintain independence of samples. In these cases, we selected the article with baseline data (whenever possible) to obtain the largest sample size and avoid bias due to attrition.
Additional searches and author contact
If an article provided insufficient information for effect size calculations, we used three strategies to obtain relevant data for that particular national dataset: 1) we conducted computerized database searches using the dataset name and/or authors; 2) we searched the national data set websites for published tables with depression data; and 3) if the study assessed relevant information (e.g., reported on depression symptoms but did not provide the data separately for men and women), all authors of the study for whom we could find email addresses from the article, the Web directory of the authors’ academic institution, or a Google search, were contacted. Given our strong interest in age and ethnicity as moderator variables, we also contacted authors for data on gender differences in depression by age and, for U.S. samples, ethnicity if that information was not provided in the original article. We received relevant information for 103 out of the 186 articles for which we contacted authors.
Overall, 112 articles from the original search met criteria for inclusion, including articles for which authors needed to be contacted for data. We added 46 new articles that were not in the original search from additional searching for nationally representative datasets.
Final sample of studies
The final sample of studies (see Figure 1) for the meta-analyses included data from 65 (diagnosis meta-analysis) and 95 (symptom meta-analysis) articles and their corresponding data sets. Two articles were used in both meta-analyses (Graham et al., 2007; Maske et al., 2016); several samples were used in both meta-analyses, e.g., MIDUS. See Tables 1 and 2 for a list of all studies.
Table 1.
Studies of Gender Differences in Major Depression Diagnoses
| Study | OR | Country | NM | NF | Interview | Year | Age | Sample | E | F | M | T |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Alaimo et al. (2002) | 2.38 | US | 365 | 389 | DIS | 1991 | 15–16 | Third National Health and Nutrition Examination Survey (NHANES III) | 1 | 1 | 2 | 4 |
| Andrews et al. (2001)* | 2.40 | Australia | 461 | 608 | CIDI 2.1 | 1997 | 18–24 | Australian National Survey of Mental Health & Well-Being (NSMHWB) | 3 | 1 | 3 | |
| Andrews et al. (2001)* | 1.97 | Australia | 940 | 1249 | CIDI 2.1 | 1997 | 25–34 | NSMHWB | 3 | 1 | 3 | |
| Andrews et al. (2001)* | 1.97 | Australia | 1131 | 1349 | CIDI 2.1 | 1997 | 35–44 | NSMHWB | 3 | 1 | 3 | |
| Andrews et al. (2001)* | 1.69 | Australia | 815 | 1017 | CIDI 2.1 | 1997 | 45–54 | NSMHWB | 3 | 1 | 3 | |
| Andrews et al. (2001)* | 2.14 | Australia | 627 | 652 | CIDI 2.1 | 1997 | 55–64 | NSMHWB | 3 | 1 | 3 | |
| Andrews et al. (2001)* | 2.78 | Australia | 731 | 1061 | CIDI 2.1 | 1997 | 65+ | NSMHWB | 3 | 1 | 3 | |
| Arokiasamy et al. (2013) | 1.24 | India | 3302 | 3255 | CIDI | 2008 | 50+ | WHO Study on global Aging and adult health (SAGE) - India | 3 | 3^ | 3 | |
| Arokiasamy et al. (2013) | 1.41 | India | 1042 | 3620 | CIDI | 2008 | 18–49 | WHO SAGE- India | 3 | 3^ | 3 | |
| Avenevoli et al. (2015)* | 1.65 | US | 843 | 809 | WMH-CIDI | 2002 | 13 | National Comorbidity Survey- Adolescent Supplement (NCS- A) | 1 | 2 | 1 | 3 |
| Avenevoli et al. (2015)* | 5.50 | US | 1088 | 1130 | WMH-CIDI | 2002 | 14 | NCS- A | 1 | 2 | 1 | 3 |
| Avenevoli et al. (2015)* | 2.57 | US | 883 | 1004 | WMH-CIDI | 2002 | 15 | NCS- A | 1 | 2 | 1 | 3 |
| Avenevoli et al. (2015)* | 2.44 | US | 966 | 1044 | WMH-CIDI | 2002 | 16 | NCS- A | 1 | 2 | 1 | 3 |
| Avenevoli et al. (2015)* | 1.93 | US | 1173 | 1183 | WMH-CIDI | 2002 | 17–18 | NCS- A | 1 | 2 | 1 | 3 |
| Beals et al. (2005) | 1.79 | US | 606 | 817 | CIDI | 1998 | 15–54 | The American Indian Service Utilization, Psychiatric Epidemiology, Risk & Protective Factors Project (AI-SUPERPFP)- Southwest Tribe | 6 | 2 | 2 | 3 |
| Beals et al. (2005) | 1.94 | US | 778 | 840 | CIDI | 1998 | 15–54 | AI-SUPERPFP- Northern Plains Tribe | 6 | 2 | 2 | 3 |
| Bijl et al. (1998) | 1.90 | Netherlands | 3304 | 3772 | CIDI 1.1 | 1996 | 18–64 | Netherlands Mental Health Survey & Incidence Study (NEMESIS) | 2 | 2 | 3 | |
| Boyd et al. (2015) | 2.55 | Bulgaria | 2430 | 2888 | WMH-CIDI | 2005 | 18+ | Bulgaria National Survey of Health & StressW | 1 | 1 | 4 | |
| Boyd et al. (2015) | 1.67 | Romania | 1092 | 1265 | WMH-CIDI | 2006 | 18+ | Romania Mental Health SurveyW | 1 | 1 | 4 | |
| Boyd et al. (2015) | 2.44 | Portugal | 1632 | 2217 | WMH-CIDI | 2009 | 18+ | Portugal National Mental Health SurveyW | 1 | 1 | 4 | |
| Boyd et al. (2015) | 1.96 | France | 1329 | 1565 | WMH-CIDI | 2002 | 18+ | ESEMeDW | 1 | 1 | 4 | |
| Bromet et al. (2005)* | 3.58 | Ukraine | 462 | 608 | WMH-CIDI | 2002 | 18–32 | Comorbid Mental Disorders during Periods of Social Disruption (CMDPSD)W | 2 | 1 | 3 | |
| Bromet et al. (2005)* | 2.31 | Ukraine | 443 | 728 | WMH-CIDI | 2002 | 33–47 | CMDPSDW | 2 | 1 | 3 | |
| Bromet et al. (2005)* | 2.07 | Ukraine | 440 | 876 | WMH-CIDI | 2002 | 48–62 | CMDPSDW | 2 | 1 | 3 | |
| Bromet et al. (2005)* | 2.07 | Ukraine | 447 | 876 | WMH-CIDI | 2002 | 63+ | CMDPSDW | 2 | 1 | 3 | |
| Bromet et al. (2011) | 1.57 | Belgium | 1190 | 1229 | WMH-CIDI | 2002 | 18+ | The European Study of the Epidemiology of Mental Disorders (ESEMeD)W | 2 | 1 | 3 | |
| Bromet et al. (2011) | 1.71 | Germany | 1660 | 1895 | WMH-CIDI | 2003 | 18+ | ESEMeDW | 2 | 1 | 3 | |
| Bromet et al. (2011) | 1.60 | Israel | 2380 | 2479 | WMH-CIDI | 2003 | 21+ | Israel National Health SurveyW | 2 | 1 | 3 | |
| Bromet et al. (2011) | 2.54 | Italy | 2321 | 2391 | WMH-CIDI | 2002 | 18+ | ESEMeDW | 2 | 1 | 3 | |
| Bromet et al. (2011) | 2.32 | Netherlands | 1032 | 1340 | WMH-CIDI | 2003 | 18+ | ESEMeDW | 2 | 1 | 3 | |
| Bromet et al. (2011) | 1.96 | Colombia | 1700 | 2726 | WMH-CIDI | 2003 | 18–65 | Colombian National Study of Mental HealthW | 2 | 1 | 3 | |
| Bromet et al. (2011) | 2.11 | Lebanon | 1297 | 1560 | WMH-CIDI | 2003 | 18+ | Lebanese Evaluation of the Burden of Ailments and Needs of the NationW | 2 | 1 | 3 | |
| Bromet et al. (2011) | 2.17 | South Africa | 1718 | 2597 | WMH-CIDI | 2004 | 18+ | South Africa Stress and Health StudyW | 2 | 1 | 3 | |
| Center for Behavioral Health Statistics & Quality (CBHSQ) (2014) | 2.86 | US | 11363 | 10938 | WMH-CIDI | 2004 | 12–17 | National Survey on Drug Use & Health (NSDUH) | 1 | 1 | 3 | |
| CBHSQ (2014) | 3.26 | US | 11378 | 11156 | WMH-CIDI | 2005 | 12–17 | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 3.05 | US | 11718 | 11153 | WMH-CIDI | 2006 | 12–17 | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 2.80 | US | 11524 | 10909 | WMH-CIDI | 2007 | 12–17 | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 3.18 | US | 11517 | 11029 | WMH-CIDI | 2008 | 12–17 | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 2.69 | US | 11520 | 11106 | WMH-CIDI | 2009 | 12–17 | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 2.93 | US | 11140 | 10820 | WMH-CIDI | 2010 | 12–17 | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 2.92 | US | 12028 | 11482 | WMH-CIDI | 2011 | 12–17 | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 2.66 | US | 1918 | 1807 | WMH-CIDI | 2012 | 12 | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 5.22 | US | 1840 | 1838 | WMH-CIDI | 2012 | 13 | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 3.28 | US | 1883 | 1872 | WMH-CIDI | 2012 | 14 | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 2.98 | US | 1921 | 1817 | WMH-CIDI | 2012 | 15 | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 3.71 | US | 1937 | 1878 | WMH-CIDI | 2012 | 16 | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 2.66 | US | 1877 | 1885 | WMH-CIDI | 2012 | 17 | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 2.14 | US | 1824 | 1713 | WMH-CIDI | 2013 | 12 | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 3.76 | US | 1963 | 1849 | WMH-CIDI | 2013 | 13 | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 4.95 | US | 2026 | 1865 | WMH-CIDI | 2013 | 14 | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 3.98 | US | 1882 | 1868 | WMH-CIDI | 2013 | 15 | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 2.92 | US | 1940 | 1890 | WMH-CIDI | 2013 | 16 | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 3.12 | US | 1914 | 1760 | WMH-CIDI | 2013 | 17 | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 1.99 | US | 10774 | 11755 | WMH-CIDI | 2012 | 18–25 | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 1.89 | US | 1469 | 1593 | WMH-CIDI | 2012 | 26–29 | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 2.13 | US | 1559 | 1863 | WMH-CIDI | 2012 | 30–34 | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 1.39 | US | 1365 | 1537 | WMH-CIDI | 2012 | 35–39 | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 1.69 | US | 1394 | 1615 | WMH-CIDI | 2012 | 40–44 | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 1.73 | US | 1428 | 1737 | WMH-CIDI | 2012 | 45–49 | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 1.35 | US | 816 | 1013 | WMH-CIDI | 2012 | 50–54 | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 1.45 | US | 722 | 877 | WMH-CIDI | 2012 | 55–59 | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 1.76 | US | 598 | 736 | WMH-CIDI | 2012 | 60–65 | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 2.09 | US | 1360 | 1625 | WMH-CIDI | 2012 | 65+ | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 2.09 | US | 10671 | 11543 | WMH-CIDI | 2013 | 18–25 | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 1.80 | US | 1376 | 1603 | WMH-CIDI | 2013 | 26–29 | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 1.29 | US | 1529 | 1802 | WMH-CIDI | 2013 | 30–34 | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 1.67 | US | 1317 | 1562 | WMH-CIDI | 2013 | 35–39 | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 1.63 | US | 1437 | 1671 | WMH-CIDI | 2013 | 40–44 | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 1.34 | US | 1440 | 1631 | WMH-CIDI | 2013 | 45–49 | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 1.47 | US | 837 | 951 | WMH-CIDI | 2013 | 50–54 | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 1.61 | US | 711 | 909 | WMH-CIDI | 2013 | 55–59 | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 1.42 | US | 674 | 719 | WMH-CIDI | 2013 | 60–65 | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 3.55 | US | 1302 | 1659 | WMH-CIDI | 2013 | 65+ | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 1.90 | US | 21408 | 24366 | WMH-CIDI | 2005 | 18+ | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 1.75 | US | 20995 | 23936 | WMH-CIDI | 2006 | 18+ | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 1.91 | US | 21272 | 24165 | WMH-CIDI | 2007 | 18+ | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 1.88 | US | 21602 | 24588 | WMH-CIDI | 2008 | 18+ | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 1.77 | US | 21755 | 24319 | WMH-CIDI | 2009 | 18+ | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 1.73 | US | 21697 | 24147 | WMH-CIDI | 2010 | 18+ | NSDUH | 1 | 1 | 3 | |
| CBHSQ (2014) | 1.84 | US | 21750 | 24489 | WMH-CIDI | 2011 | 18+ | NSDUH | 1 | 1 | 3 | |
| Chan Chee et al. (2011) | 2.28 | France | 529 | 596 | CIDI-SF | 2005 | 15–19 | French Barometer Study | 2 | 1 | 3 | |
| Chan Chee et al. (2011) | 1.98 | France | 1813 | 2417 | CIDI-SF | 2005 | 20–34 | French Barometer Study | 2 | 1 | 3 | |
| Chan Chee et al. (2011) | 2.46 | France | 2655 | 3690 | CIDI-SF | 2005 | 35–54 | French Barometer Study | 2 | 1 | 3 | |
| Chan Chee et al. (2011) | 1.95 | France | 2081 | 3102 | CIDI-SF | 2005 | 55–75 | French Barometer Study | 2 | 1 | 3 | |
| Chan Chee et al. (2011) | 2.02 | France | 878 | 1060 | CIDI-SF | 2010 | 20–34 | French Barometer Study | 2 | 1 | 3 | |
| Chan Chee et al. (2011) | 1.52 | France | 1433 | 1725 | CIDI-SF | 2010 | 35–54 | French Barometer Study | 2 | 1 | 3 | |
| Chan Chee et al. (2011) | 2.65 | France | 1122 | 1527 | CIDI-SF | 2010 | 55–75 | French Barometer Study | 2 | 1 | 3 | |
| Cho et al. (2010)* | 2.40 | South Korea | 560 | 683 | K-CIDI 2.1 | 2007 | 18–29 | Korean National Epidemiologic Catchment Area Study- Replication (KECA-R) | 2 | 1 | 3 | |
| Cho et al. (2010)* | 2.55 | South Korea | 688 | 1136 | K-CIDI 2.1 | 2007 | 30–39 | KECA-R | 2 | 1 | 3 | |
| Cho et al. (2010)* | 1.26 | South Korea | 690 | 1065 | K-CIDI 2.1 | 2007 | 40–49 | KECA-R | 2 | 1 | 3 | |
| Cho et al. (2010)* | 1.85 | South Korea | 431 | 683 | K-CIDI 2.1 | 2007 | 50–59 | KECA-R | 2 | 1 | 3 | |
| Cho et al. (2007) | 3.18 | South Korea | 3524 | 2751 | K-CIDI 2.1 | 2001 | 18–64 | KECA | 2 | 1 | 3 | |
| Coyne & Marcus (2006) | 2.15 | US | 11612 | 14903 | CIDI-SF | 1999 | 18+ | National Health Interview Survey | 2 | 2 | 1 | 3 |
| Coyne & Marcus (2006) | 2.29 | US | 1590 | 2696 | CIDI-SF | 1999 | 18+ | National Health Interview Survey | 3 | 2 | 1 | 3 |
| Danielson et al. (2005). | 1.98 | US | 2020 | 2003 | NSA interview | 1995 | 12–17 | National Survey of Adolescents (NSA) | 1 | 2 | 1 | 3 |
| de Graaf et al. (2012) | 1.57 | Netherlands | 2977 | 3669 | WMH-CIDI | 2008 | 18–64 | NEMESIS II | 2 | 1 | 3 | |
| Farbstein et al. (2010) | 2.55 | Israel | 497 | 460 | DAWBA | 2005 | 14–17 | Israel Survey of Mental Health among Adolescents (ISMEHA) | 3 | 1 | 2 | |
| Ford et al. (2003)* | 1.51 | Great Britain | 1284 | 1340 | DAWBA | 1999 | 13–15 | British Child & Adolescent Mental Health Survey | 2 | 1 | 0 | |
| Gabilondo et al. (2010). | 2.83 | Spain | 733 | 834 | WMH-CIDI | 2002 | 18–34 | ESEMeDW | 2 | 1 | 3 | |
| Gabilondo et al. (2010). | 1.82 | Spain | 622 | 809 | WMH-CIDI | 2002 | 35–49 | ESEMeDW | 2 | 1 | 3 | |
| Gabilondo et al. (2010). | 2.83 | Spain | 437 | 587 | WMH-CIDI | 2002 | 50–64 | ESEMeDW | 2 | 1 | 3 | |
| Gabilondo et al. (2010). | 6.29 | Spain | 629 | 822 | WMH-CIDI | 2002 | 65+ | ESEMeDW | 2 | 1 | 3 | |
| Gavin et al. (2009) | 1.92 | US | 1217 | 2217 | WMH-CIDI | 2002 | 18+ | National Survey of American Life | 3 | 2 | 1 | 4 |
| Goodwin & Gotlib (2004) | 1.75 | US | 1492 | 1540 | CIDI-SF | 1996 | 25–74 | MIDUS (Midlife in the US) | 1 | 1 | 2 | 3 |
| Graham et al. (2007) | 2.06 | Canada | 6214 | 7878 | CIDI | 2005 | 18–76 | Gender Alcohol and Culture: An International Study (GENACIS) | 2 | 1 | 3 | |
| Grant (1995) | 1.31 | US | 21431 | 21431 | AUDADIS | 1992 | 18+ | National Longitudinal Alcohol Epidemiologic Survey (NLAES) | 1 | 2 | 1 | 4 |
| Gureje et al. (2006)* | 0.83 | Nigeria | 1595 | 1580 | WMH-CIDI | 2003 | 18–34 | Nigerian Survey of Mental Health & Wellbeing (NSMHW)W | 2 | 1 | 3 | |
| Gureje et al. (2006)* | 1.84 | Nigeria | 809 | 822 | WMH-CIDI | 2003 | 35–49 | NSMHWW | 2 | 1 | 3 | |
| Gureje et al. (2006)* | 1.28 | Nigeria | 503 | 601 | WMH-CIDI | 2003 | 50–64 | NSMHWW | 2 | 1 | 3 | |
| Haarasilta et al. (2001) | 1.36 | Finland | 437 | 505 | CIDI-SF | 1996 | 15–24 | Finnish Health Care Survey (FINHCS) | 2 | 2 | 3 | |
| Hasin et al. (2005)* | 1.93 | US | 2410 | 2789 | AUDADIS | 2002 | 18–24 | National Epidemiologic Survey on Alcohol & Related Conditions (NESARC) | 1 | 2 | 1 | 3 |
| Hasin et al. (2005)* | 2.08 | US | 1407 | 2060 | AUDADIS | 2002 | 25–29 | NESARC | 1 | 2 | 1 | 3 |
| Hasin et al. (2005)* | 3.28 | US | 1834 | 2458 | AUDADIS | 2002 | 30–34 | NESARC | 1 | 2 | 1 | 3 |
| Hasin et al. (2005)* | 1.65 | US | 1989 | 2661 | AUDADIS | 2002 | 35–39 | NESARC | 1 | 2 | 1 | 3 |
| Hasin et al. (2005)* | 2.36 | US | 2034 | 2406 | AUDADIS | 2002 | 40–44 | NESARC | 1 | 2 | 1 | 3 |
| Hasin et al. (2005)* | 1.84 | US | 1876 | 2142 | AUDADIS | 2002 | 45–49 | NESARC | 1 | 2 | 1 | 3 |
| Hasin et al. (2005)* | 2.53 | US | 1603 | 2004 | AUDADIS | 2002 | 50–54 | NESARC | 1 | 2 | 1 | 3 |
| Hasin et al. (2005)* | 1.76 | US | 1236 | 1611 | AUDADIS | 2002 | 55–59 | NESARC | 1 | 2 | 1 | 3 |
| Hasin et al. (2005)* | 1.41 | US | 1025 | 1343 | AUDADIS | 2002 | 60–64 | NESARC | 1 | 2 | 1 | 3 |
| Hasin et al. (2005)* | 2.38 | US | 927 | 1255 | AUDADIS | 2002 | 65–69 | NESARC | 1 | 2 | 1 | 3 |
| Hasin et al. (2005)* | 1.74 | US | 2177 | 3846 | AUDADIS | 2002 | 70 + | NESARC | 1 | 2 | 1 | 3 |
| Instituto Nacional de Salud Publica (2014) | 6.02 | Mexico | 1028 | 1176 | CIDI | 2010 | 50+ | WHO SAGE- Mexico | 3 | 3^ | 3 | |
| Joe et al. (2009)* | 0.98 | US | 563 | 607 | WMH-CIDI | 2002 | 13–17 | National Survey of American Life | 3 | 3 | 1 | 3 |
| Kessler et al. (2010) | 2.03 | US | 1375 | 1658 | WMH- CIDI | 2002 | 18–34 | National Comorbidity Survey- Replication (NCS- R)W | 1 | 2 | 1 | 3 |
| Kessler et al. (2010) | 1.59 | US | 1343 | 1522 | WMH- CIDI | 2002 | 35–49 | NCS-RW | 1 | 2 | 1 | 3 |
| Kessler et al. (2010) | 1.54 | US | 854 | 1068 | WMH- CIDI | 2002 | 50–64 | NCS-RW | 1 | 2 | 1 | 3 |
| Kessler et al. (2010) | 3.16 | US | 567 | 894 | WMH- CIDI | 2002 | 65+ | NCS-RW | 1 | 2 | 1 | 3 |
| Kessler et al. (1993) | 1.86 | US | 838 | 927 | CIDI | 1991 | 15–24 | National Comorbidity Survey (NCS) | 1 | 1 | 2 | 3 |
| Kessler et al. (1993) | 1.53 | US | 1246 | 1378 | CIDI | 1991 | 25–34 | NCS | 1 | 1 | 2 | 3 |
| Kessler et al. (1993) | 1.65 | US | 1065 | 1178 | CIDI | 1991 | 35–44 | NCS | 1 | 1 | 2 | 3 |
| Kessler et al. (1993) | 2.97 | US | 696 | 770 | CIDI | 1991 | 45–54 | NCS | 1 | 1 | 2 | 3 |
| Kiejna et al. (2015) | 1.82 | Poland | 1465 | 1430 | WMH-CIDI | 2011 | 18–29 | Epidemiology of Mental Health and Access to Care Survey (EZOP)W | 1 | 1 | 4 | |
| Kiejna et al. (2015) | 1.76 | Poland | 1069 | 1050 | WMH-CIDI | 2011 | 30–39 | EZOPW | 1 | 1 | 4 | |
| Kiejna et al. (2015) | 2.51 | Poland | 938 | 936 | WMH-CIDI | 2011 | 40–49 | EZOPW | 1 | 1 | 4 | |
| Kiejna et al. (2015) | 2.37 | Poland | 1411 | 1782 | WMH-CIDI | 2011 | 50–64 | EZOPW | 1 | 1 | 4 | |
| Kim et al. (2015)* | 2.36 | South Korea | 691 | 636 | K-CIDI | 2011 | 18–29 | KECA-2011 | 1 | 1 | 3 | |
| Kim et al. (2015)* | 2.02 | South Korea | 655 | 645 | K-CIDI | 2011 | 30–39 | KECA-2011 | 1 | 1 | 3 | |
| Kim et al. (2015)* | 2.50 | South Korea | 687 | 682 | K-CIDI | 2011 | 40–49 | KECA-2011 | 1 | 1 | 3 | |
| Kim et al. (2015)* | 2.01 | South Korea | 542 | 553 | K-CIDI | 2011 | 50–59 | KECA-2011 | 1 | 1 | 3 | |
| Kim et al. (2015)* | 3.40 | South Korea | 315 | 351 | K-CIDI | 2011 | 60–69 | KECA-2011 | 1 | 1 | 3 | |
| Kim et al. (2015)* | 3.65 | South Korea | 112 | 149 | K-CIDI | 2011 | 70+ | KECA-2011 | 1 | 1 | 3 | |
| Lara et al. (2015) | 1.80 | Spain | 435 | 523 | CIDI | 2012 | 18–49 | Collaborative Research on Aging in Europe (COURAGE)- Spain | 2 | 1 | 3 | |
| Lara et al. (2015) | 1.95 | Spain | 829 | 931 | CIDI | 2012 | 50–64 | COURAGE- Spain | 2 | 1 | 3 | |
| Lara et al. (2015) | 4.17 | Spain | 814 | 1051 | CIDI | 2012 | 65+ | COURAGE- Spain | 2 | 1 | 3 | |
| Lepine et al. (1997) | 1.75 | Belgium | 4032 | 4044 | MINI | 1995 | 18+ | DEPRES (Depression Research in European Society) | 2 | 1 | 2 | |
| Lepine et al. (1997) | 2.22 | France | 7162 | 7355 | MINI | 1995 | 15+ | DEPRES | 2 | 1 | 2 | |
| Lepine et al. (1997) | 1.58 | Germany | 7798 | 8386 | MINI | 1995 | 14+ | DEPRES | 2 | 1 | 2 | |
| Lepine et al. (1997) | 1.97 | Netherlands | 4224 | 3587 | MINI | 1995 | 16+ | DEPRES | 2 | 1 | 2 | |
| Lepine et al. (1997) | 2.12 | Spain | 8063 | 8069 | MINI | 1995 | 15+ | DEPRES | 2 | 1 | 2 | |
| Lepine et al. (1997) | 1.41 | UK | 7155 | 8588 | MINI | 1995 | 16+ | DEPRES | 2 | 1 | 2 | |
| Lorenzo-Blanco et al. (2013) | 1.77 | US | 1127 | 1427 | WMH-CIDI | 2003 | 18+ | National Latino & Asian American Study (NLAAS) | 5 | 1 | 1 | 3 |
| Maske et al. (2016)* | 3.69 | Germany | 371 | 413 | M-CIDI | 2011 | 18–34 | Germany Health Interview and Examination Survey for Adults- mental health module (DEGS1-MH) | 2 | 1 | 3 | |
| Maske et al. (2016)* | 4.33 | Germany | 291 | 332 | M-CIDI | 2011 | 35–44 | DEGS1-MH | 2 | 1 | 3 | |
| Maske et al. (2016)* | 1.41 | Germany | 414 | 524 | M-CIDI | 2011 | 45–54 | DEGS1-MH | 2 | 1 | 3 | |
| Maske et al. (2016)* | 1.21 | Germany | 399 | 444 | M-CIDI | 2011 | 55–64 | DEGS1-MH | 2 | 1 | 3 | |
| Maske et al. (2016)* | 3.10 | Germany | 628 | 592 | M-CIDI | 2011 | 65–79 | DEGS1-MH | 2 | 1 | 3 | |
| McMartin et al. (2013)* | 2.82 | Canada | 3228 | 3078 | CIDI-SF | 2001 | 12–14 | Canadian Community Health Survey (CCHS) | 2 | 1 | 3 | |
| McMartin et al. (2013)* | 3.22 | Canada | 5425 | 5380 | CIDI-SF | 2001 | 15–19 | CCHS 1.1 | 2 | 1 | 3 | |
| McMartin et al. (2013)* | 1.76 | Canada | 3350 | 3997 | CIDI-SF | 2001 | 20–24 | CCHS 1.1 | 2 | 1 | 3 | |
| McMartin et al. (2013)* | 1.88 | Canada | 3914 | 4586 | CIDI-SF | 2001 | 25–29 | CCHS 1.1 | 2 | 1 | 3 | |
| McMartin et al. (2013)* | 1.87 | Canada | 4644 | 5306 | CIDI-SF | 2001 | 30–34 | CCHS 1.1 | 2 | 1 | 3 | |
| McMartin et al. (2013)* | 1.85 | Canada | 5687 | 6429 | CIDI-SF | 2001 | 35–39 | CCHS 1.1 | 2 | 1 | 3 | |
| McMartin et al. (2013)* | 2.17 | Canada | 6073 | 6458 | CIDI-SF | 2001 | 40–44 | CCHS 1.1 | 2 | 1 | 3 | |
| McMartin et al. (2013)* | 2.06 | Canada | 5368 | 5647 | CIDI-SF | 2001 | 45–49 | CCHS 1.1 | 2 | 1 | 3 | |
| McMartin et al. (2013)* | 1.45 | Canada | 4759 | 5184 | CIDI-SF | 2001 | 50–54 | CCHS 1.1 | 2 | 1 | 3 | |
| McMartin et al. (2013)* | 2.23 | Canada | 3867 | 4226 | CIDI-SF | 2001 | 55–59 | CCHS 1.1 | 2 | 1 | 3 | |
| McMartin et al. (2013)* | 1.62 | Canada | 3136 | 3782 | CIDI-SF | 2001 | 60–64 | CCHS 1.1 | 2 | 1 | 3 | |
| McMartin et al. (2013)* | 1.72 | Canada | 2988 | 3625 | CIDI-SF | 2001 | 65–69 | CCHS 1.1 | 2 | 1 | 3 | |
| McMartin et al. (2013)* | 1.91 | Canada | 2607 | 3572 | CIDI-SF | 2001 | 70–74 | CCHS 1.1 | 2 | 1 | 3 | |
| McMartin et al. (2013)* | 2.27 | Canada | 1914 | 3140 | CIDI-SF | 2001 | 75–79 | CCHS 1.1 | 2 | 1 | 3 | |
| McMartin et al. (2013)* | 1.54 | Canada | 1783 | 3746 | CIDI-SF | 2001 | 80+ | CCHS 1.1 | 2 | 1 | 3 | |
| Merikangas et al. (2012) | 2.98 | US | 2147 | 2003 | NIMH DISC-IV | 2003 | 12–19 | National Health & Nutrition Examination Survey (NHANES), 2001–2004 | 1 | 2 | 1 | 3 |
| Mohammadi et al. (2005) | 2.84 | Iran | 12660 | 12530 | SADS | 2001 | 18+ | The national plan for epidemiologic study of psychiatric disorders in Iran | 2 | 1 | 4 | |
| Mommersteeg et al. (2013)* | 1.24 | Burkina Faso | 2272 | 2551 | WHO WHS | 2002 | 18+ | World Health Organization (WHO) World Health Survey (WHS) | 2 | 1 | 3 | |
| Mommersteeg et al.* | 1.42 | Chad | 2196 | 2447 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 1.70 | Comoros | 787 | 972 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 1.64 | Congo | 1167 | 1326 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 1.11 | Ethiopia | 2391 | 2544 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 1.67 | Ghana | 1773 | 2153 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 1.66 | Ivory Coast | 1818 | 1361 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 2.03 | Kenya | 1868 | 2541 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 2.17 | Malawi | 2197 | 3033 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 2.00 | Mali | 2354 | 1711 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 1.13 | Mauritania | 1465 | 2308 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 2.41 | Mauritius | 1872 | 2016 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 1.25 | Namibia | 1721 | 2524 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 2.01 | Senegal | 1641 | 1515 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 0.93 | Swaziland | 1417 | 1667 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 1.29 | Tunisia | 2344 | 2725 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 1.77 | Zimbabwe | 1489 | 2600 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 1.57 | Brazil | 2188 | 2812 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 1.94 | Dominican Republic | 2104 | 2430 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 1.85 | Ecuador | 2051 | 2602 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 2.48 | Mexico | 16377 | 22368 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 3.39 | Paraguay | 2353 | 2789 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 3.25 | Uruguay | 1449 | 1530 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 1.82 | Bangladesh | 2584 | 2966 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 2.01 | China | 1954 | 2039 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 2.21 | Georgia | 1165 | 1590 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 1.30 | India | 4849 | 5144 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 1.65 | Kazakhstan | 1544 | 2951 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 1.63 | Lao PDR | 2295 | 2594 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 1.37 | Malaysia | 2673 | 3366 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 2.01 | Myanmar | 2551 | 3335 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 1.52 | Nepal | 3698 | 4990 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 2.34 | Pakistan | 3565 | 2810 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 1.49 | Philippines | 4659 | 5416 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 0.83 | Sri Lanka | 3136 | 3596 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 0.84 | UAE | 617 | 563 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 7.04 | Vietnam | 1572 | 1919 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 3.82 | Bosnia & Herzegovina | 434 | 594 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 1.42 | Croatia | 401 | 589 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 1.46 | Czech Republic | 419 | 516 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 1.75 | Estonia | 366 | 645 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 2.57 | Hungary | 591 | 828 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 1.92 | Russia | 1592 | 2828 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 3.08 | Slovakia | 952 | 1530 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 1.70 | Spain | 2623 | 3740 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| Mommersteeg et al.* | 2.03 | Ukraine | 1001 | 1844 | WHO WHS | 2002 | 18+ | WHO World Health Survey | 2 | 1 | 3 | |
| National Research Institute of Public Health, Russian Academy of Medical Science (2013) | 3.02 | Russia | 1520 | 2376 | CIDI | 2009 | 50+ | WHO SAGE- Russia | 3 | 3^ | 3 | |
| Patten (2005)* | 2.74 | Canada | 1432 | 1434 | WMH-CIDI | 2002 | 15–19 | Canadian Community Health Survey (CCHS) 1.2 | 2 | 1 | 3 | |
| Patten (2005)* | 1.48 | Canada | 1305 | 1502 | WMH-CIDI | 2002 | 20–24 | CCHS 1.2 | 2 | 1 | 3 | |
| Patten (2005)* | 2.20 | Canada | 1074 | 1468 | WMH-CIDI | 2002 | 25–29 | CCHS 1.2 | 2 | 1 | 3 | |
| Patten (2005)* | 1.64 | Canada | 1498 | 1731 | WMH-CIDI | 2002 | 30–34 | CCHS 1.2 | 2 | 1 | 3 | |
| Patten (2005)* | 1.51 | Canada | 1669 | 1860 | WMH-CIDI | 2002 | 35–39 | CCHS 1.2 | 2 | 1 | 3 | |
| Patten (2005)* | 1.80 | Canada | 1775 | 1738 | WMH-CIDI | 2002 | 40–44 | CCHS 1.2 | 2 | 1 | 3 | |
| Patten (2005)* | 1.67 | Canada | 1443 | 1464 | WMH-CIDI | 2002 | 45–49 | CCHS 1.2 | 2 | 1 | 3 | |
| Patten (2005)* | 2.69 | Canada | 1282 | 1517 | WMH-CIDI | 2002 | 50–54 | CCHS 1.2 | 2 | 1 | 3 | |
| Patten (2005)* | 1.34 | Canada | 1264 | 1465 | WMH-CIDI | 2002 | 55–59 | CCHS 1.2 | 2 | 1 | 3 | |
| Patten (2005)* | 0.89 | Canada | 1092 | 1235 | WMH-CIDI | 2002 | 60–64 | CCHS 1.2 | 2 | 1 | 3 | |
| Patten (2005)* | 1.37 | Canada | 889 | 1184 | WMH-CIDI | 2002 | 65–69 | CCHS 1.2 | 2 | 1 | 3 | |
| Patten (2005)* | 1.13 | Canada | 834 | 1206 | WMH-CIDI | 2002 | 70–74 | CCHS 1.2 | 2 | 1 | 3 | |
| Patten (2005)* | 0.97 | Canada | 599 | 1042 | WMH-CIDI | 2002 | 75–79 | CCHS 1.2 | 2 | 1 | 3 | |
| Patten (2005)* | 0.22 | Canada | 617 | 1365 | WMH-CIDI | 2002 | 80+ | CCHS 1.2 | 2 | 1 | 3 | |
| Patten (2005)* | 3.03 | Canada | 967 | 1057 | WMH-CIDI | 2012 | 15–19 | CCHS- MH (Mental Health) | 2 | 1 | 3 | |
| Patten (2005)* | 1.17 | Canada | 923 | 1066 | WMH-CIDI | 2012 | 20–24 | CCHS- MH | 2 | 1 | 3 | |
| Patten (2005)* | 2.09 | Canada | 737 | 880 | WMH-CIDI | 2012 | 25–29 | CCHS- MH | 2 | 1 | 3 | |
| Patten (2005)* | 2.00 | Canada | 808 | 1061 | WMH-CIDI | 2012 | 30–34 | CCHS- MH | 2 | 1 | 3 | |
| Patten (2005)* | 1.52 | Canada | 827 | 902 | WMH-CIDI | 2012 | 35–39 | CCHS- MH | 2 | 1 | 3 | |
| Patten (2005)* | 1.41 | Canada | 877 | 814 | WMH-CIDI | 2012 | 40–44 | CCHS- MH | 2 | 1 | 3 | |
| Patten (2005)* | 1.37 | Canada | 795 | 875 | WMH-CIDI | 2012 | 45–49 | CCHS- MH | 2 | 1 | 3 | |
| Patten (2005)* | 2.04 | Canada | 904 | 1052 | WMH-CIDI | 2012 | 50–54 | CCHS- MH | 2 | 1 | 3 | |
| Patten (2005)* | 1.86 | Canada | 1016 | 1229 | WMH-CIDI | 2012 | 55–59 | CCHS- MH | 2 | 1 | 3 | |
| Patten (2005)* | 1.57 | Canada | 975 | 1231 | WMH-CIDI | 2012 | 60–64 | CCHS- MH | 2 | 1 | 3 | |
| Patten (2005)* | 2.31 | Canada | 847 | 1071 | WMH-CIDI | 2012 | 65–69 | CCHS- MH | 2 | 1 | 3 | |
| Patten (2005)* | 0.39 | Canada | 639 | 793 | WMH-CIDI | 2012 | 70–74 | CCHS- MH | 2 | 1 | 3 | |
| Patten (2005)* | 1.13 | Canada | 466 | 718 | WMH-CIDI | 2012 | 75–79 | CCHS- MH | 2 | 1 | 3 | |
| Patten (2005)* | 5.07 | Canada | 559 | 1024 | WMH-CIDI | 2012 | 80+ | CCHS- MH | 2 | 1 | 3 | |
| Peltzer & Phaswana-Mafuya (2013) | 1.08 | South Africa | 1638 | 2202 | WMH-CIDI | 2008 | 50+ | WHO SAGE- South Africa | 2 | 3^ | 3 | |
| Pirkola et al. (2005)* | 2.26 | Finland | 983 | 1094 | CIDI | 2001 | 30–44 | Health 2000 | 2 | 1 | 3 | |
| Pirkola et al. (2005) | 1.62 | Finland | 768 | 812 | CIDI | 2001 | 45–54 | Health 2000 | 2 | 1 | 3 | |
| Pirkola et al. (2005) | 2.10 | Finland | 486 | 563 | CIDI | 2001 | 55–64 | Health 2000 | 2 | 1 | 3 | |
| Pirkola et al. (2005) | 2.49 | Finland | 511 | 788 | CIDI | 2001 | 65+ | Health 2000 | 2 | 1 | 3 | |
| Rafful et al. (2012) | 1.65 | Mexico | 842 | 1218 | WMH- CIDI | 2002 | 18–29 | Mexico National Comorbidity Survey (M-NCS)W | 1 | 1 | 4 | |
| Rafful et al. (2012) | 2.40 | Mexico | 852 | 1384 | WMH- CIDI | 2002 | 30–44 | (M-NCS)W | 1 | 1 | 4 | |
| Rafful et al. (2012) | 2.20 | Mexico | 591 | 895 | WMH- CIDI | 2002 | 45–65 | (M-NCS)W | 1 | 1 | 4 | |
| Rapsey et al. (2015)* | 1.91 | Iraq | 2091 | 2241 | WMH- CIDI | 2007 | 18–96 | Iraq Mental Health Survey W | 3 | 1 | 4 | |
| Sandanger et al. (2007) | 1.55 | Norway | 803 | 888 | CIDI 1.2 | 2001 | 18+ | – | 1 | 1 | 3 | |
| Scott et al. (2010)* | 1.61 | New Zealand | 713 | 822 | WMH-CIDI | 2004 | 16–24 | New Zealand Mental Health Survey (NZMHS)W | 2 | 1 | 3 | |
| Scott et al. (2010)* | 2.10 | New Zealand | 1000 | 1414 | WMH-CIDI | 2004 | 25–34 | NZMHSW | 2 | 1 | 3 | |
| Scott et al. (2010)* | 1.23 | New Zealand | 1231 | 1659 | WMH-CIDI | 2004 | 35–44 | NZMHSW | 2 | 1 | 3 | |
| Scott et al. (2010)* | 1.70 | New Zealand | 1023 | 1222 | WMH-CIDI | 2004 | 45–54 | NZMHSW | 2 | 1 | 3 | |
| Scott et al. (2010)* | 3.28 | New Zealand | 730 | 934 | WMH-CIDI | 2004 | 55–64 | NZMHSW | 2 | 1 | 3 | |
| Scott et al. (2010)* | 3.31 | New Zealand | 937 | 1307 | WMH-CIDI | 2004 | 65+ | NZMHSW | 2 | 1 | 3 | |
| Shah et al. (2011) | 1.84 | US | 838 | 927 | DIS | 1991 | 17–39 | NHANES- III | 3 | 2 | 2 | 4 |
| Shah et al. (2011) | 2.34 | US | 1246 | 1378 | DIS | 1991 | 17–39 | NHANES- III | 2 | 2 | 2 | 4 |
| Shah et al. (2011) | 2.16 | US | 1065 | 1178 | DIS | 1991 | 17–39 | NHANES- III | 5 | 2 | 2 | 4 |
| Shanghai Municipal Center for Disease Control and Prevention (2012) | 1.58 | China | 6409 | 6466 | CIDI | 2009 | 50+ | WHO SAGE- China | 3 | 3^ | 3 | |
| Skapinakis et al. (2013) | 1.78 | Greece | 2427 | 2467 | CIS-R | 2010 | 18–70 | Psychiatric Morbidity Survey | 2 | 3^ | 1 | |
| Slade et al. (2009)* | 2.92 | Australia | 681 | 790 | WMH-CIDI | 2007 | 16–24 | National Survey of Mental Health and Well-Being (NSMHWB)W | 2 | 3^ | 3 | |
| Slade et al. (2009)* | 1.57 | Australia | 516 | 774 | WMH-CIDI | 2007 | 25–34 | NSMHWBW | 2 | 3^ | 3 | |
| Slade et al. (2009)* | 1.17 | Australia | 756 | 882 | WMH-CIDI | 2007 | 35–44 | NSMHWBW | 2 | 3^ | 3 | |
| Slade et al. (2009)* | 1.34 | Australia | 566 | 698 | WMH-CIDI | 2007 | 45–54 | NSMHWBW | 2 | 3^ | 3 | |
| Slade et al. (2009)* | 2.80 | Australia | 604 | 669 | WMH-CIDI | 2007 | 55–64 | NSMHWBW | 2 | 3^ | 3 | |
| Slade et al. (2009)* | 1.75 | Australia | 904 | 1001 | WMH-CIDI | 2007 | 65–85 | NSMHWBW | 2 | 3^ | 3 | |
| Spiers et al. (2012) | 1.60 | England | 4300 | 4318 | CIS-R | 1993 | 16–64 | National Psychiatric Morbidity Surveys (NPMS) | 2 | 3^ | 1 | |
| Spiers et al. (2012) | 1.17 | England | 3606 | 3622 | CIS-R | 2000 | 16–71 | NPMS | 2 | 3^ | 1 | |
| Spiers et al. (2012) | 1.50 | England | 3454 | 3553 | CIS-R | 2007 | 16–78 | NPMS | 2 | 3^ | 1 | |
| Subramaniam et al. (2013)* | 1.43 | Singapore | 1149 | 1144 | WMH-CIDI | 2010 | 18–34 | Singapore Mental Health Study | 2 | 1 | 3 | |
| Subramaniam et al. (2013)* | 1.00 | Singapore | 1162 | 1197 | WMH-CIDI | 2010 | 35–49 | Singapore Mental Health Study | 2 | 1 | 3 | |
| Subramaniam et al. (2013)* | 3.02 | Singapore | 978 | 976 | WMH-CIDI | 2010 | 50–89 | Singapore Mental Health Study | 2 | 1 | 3 | |
| Suttajit et al. (2012)* | 2.26 | Thailand | 1886 | 1786 | MINI | 2008 | 15–24 | Thai National Mental Health survey | 2 | 1 | 4 | |
| Suttajit et al. (2012)* | 1.52 | Thailand | 1831 | 1908 | MINI | 2008 | 25–34 | Thai National Mental Health survey | 2 | 1 | 4 | |
| Suttajit et al. (2012)* | 1.25 | Thailand | 1904 | 1982 | MINI | 2008 | 35–44 | Thai National Mental Health survey | 2 | 1 | 4 | |
| Suttajit et al. (2012)* | 1.57 | Thailand | 2875 | 2968 | MINI | 2008 | 45–59 | Thai National Mental Health survey | 2 | 1 | 4 | |
| Takeuchi et al. (2007)* | 0.81 | US | 998 | 1097 | WMH-CIDI | 2003 | 18+ | National Latino & Asian American Study (NLAAS) | 4 | 2 | 1 | 3 |
| Toussaint et al. (2008)* | 2.57 | US | 563 | 709 | CIDI-SF | 1998 | 18+ | - | 1 | 1 | 2 | 3 |
| University of Ghana Medical School (2013) | 1.72 | Ghana | 2241 | 2041 | CIDI | 2008 | 50+ | WHO SAGE- Ghana | 3 | 3^ | 3 | |
| Vicente et al. (2006) | 2.11 | Chile | 1281 | 1697 | CIDI | 1996 | 15+ | Chilean Psychiatric Prevalence Study | 2 | 2 | 3 | |
| Volken (2013)* | 1.25 | Switzerland | 7919 | 9936 | CIDI- SF | 2007 | 15+ | Swiss Health Survey | 2 | 1 | 3 | |
| Wade et al. (2002) | 1.93 | Canada | 643 | 677 | CIDI-SF | 1995 | 12–19 | National Population Health Survey (NPHS) | 1 | 2 | 3 | |
| Wittchen et al. (2000) | 2.17 | Germany | 1913 | 2268 | CIDI | 1998 | 18–65 | German National Health Interview and Examination Survey | 2 | 1 | 3 | |
| Zhao et al. (2006) | 2.21 | Canada | 12991 | 14399 | CIDI-SF | 1997 | 20–39 | NPHS | 1 | 2 | 3 | |
| Zhao et al. (2006) | 1.91 | Canada | 12386 | 13296 | CIDI-SF | 1997 | 40–64 | NPHS | 1 | 2 | 3 | |
| Zinzow et al. (2009)* | 3.24 | US | 923 | 885 | NSA interview | 2005 | 12–14 | National Survey of Adolescents-Replication (NSA-R) | 1 | 2 | 1 | 2 |
| Zinzow et al. (2009)* | 2.79 | US | 928 | 868 | NSA interview | 2005 | 15–17 | NSA-R | 1 | 2 | 1 | 2 |
| Zubrick et al. (2016)* | 4.96 | Australia | 183 | 160 | DISC-IV | 2014 | 14 | Second Australian Child and Adolescent Survey of Health and Well-being | 2 | 1 | 3 | |
| Zubrick et al. (2016)* | 3.16 | Australia | 168 | 141 | DISC-IV | 2014 | 15 | Second Australian Child and Adolescent Survey of Health and Well-being | 2 | 1 | 3 | |
| Zubrick et al. (2016)* | 3.55 | Australia | 353 | 365 | DISC-IV | 2014 | 16 | Second Australian Child and Adolescent Survey of Health and Well-being | 2 | 1 | 3 | |
| Zubrick et al. (2016)* | 2.08 | Australia | 325 | 309 | DISC-IV | 2014 | 17 | Second Australian Child and Adolescent Survey of Health and Well-being | 2 | 1 | 3 |
Note. Sample = sample name (not all samples had a name); Interview = diagnostic interview used; OR = untransformed Odds Ratio; NM = n males; NF = n females; Year = year of data collection; Age = age or age range (in years); E = ethnicity (only applies to U.S. samples): 1 = mixed, 2 = > 85% Caucasian, 3 = > 85% African American, 4 = > 85% Asian American, 5 = > 85% Hispanic, 6 = > 85% Native American; F = focus of article: 1 = gender, 2 = depression, 3 = other, no value = no title; M = diagnostic manual or classification system: 1 = DSM-IV or DSM-IV-TR; 2 = DSM-III or DSM-III-R; 3 = ICD-10; T = time span during which depression was diagnosed: 0 = current; 1 = 1 month, 2 = 6 months, 3 = 12 months, 4 = lifetime;
= received additional data from author;
= World Mental Health Survey Sample;
= ICD-10 depressive episode (all other diagnoses were major depressive episodes or major depressive disorders);
DIS = Diagnostic Interview Schedule (Robins et al., 1981); CIDI = Composite International Diagnostic Interview (World Health Organization, 1990, 1997; Smeets & Dingemans, 1993); WMH- CIDI = World Mental Health CIDI or CIDI 3.0 (Kessler & Ustun, 2004); CIDI-SF = CIDI- Short Form (Kessler et al., 1998); K-CIDI = Korean version of the CIDI (Cho et al., 2002); M-CIDI = German version of the CIDI (Wittchen & Pfister, 1997); DAWBA = Development and Well-Being Assessment (Goodman et al., 2000); AUDADIS = Alcohol Use Disorder and Associated Disabilities Interview Schedule (Grant et al., 2001); MINI = Mini-International Neuropsychiatric Interview (Sheehan et al., 1998); NIMH DISC-IV = National Institute of Mental Health Diagnostic Interview Schedule for Children Version IV (Shaffer et al., 2000); SADS = Schedule of Affective Disorders and Schizophrenia (Endicott & Spitzer, 1978); WHO WHS = World Health Organization World Health Survey- 2002 (World Health Organization, 2002); SCID = Structured Clinical Interview for Diagnostic and Statistical Manual (DSM)-IV Axis I Disorders (First et al., 2002); CIS-R = Clinical Interview Schedule- Revised (Lewis et al., 1992); CIS = Clinical Interview Schedule (Lewis et al., 1992).
Table 2.
Studies of Gender Differences in Depression Symptoms
| Study | d | Country | NM | NF | Measure | Year | Age | Sample | E | F |
|---|---|---|---|---|---|---|---|---|---|---|
| Aalto et al. (2012)* | 0.27 | Finland | 326 | 371 | BDI | 2001 | 30–34 | Health 2000 | 2 | |
| Aalto et al. (2012)* | 0.29 | Finland | 353 | 388 | BDI | 2001 | 35–39 | Health 2000 | 2 | |
| Aalto et al. (2012)* | 0.14 | Finland | 341 | 381 | BDI | 2001 | 40–44 | Health 2000 | 2 | |
| Aalto et al. (2012)* | 0.10 | Finland | 379 | 435 | BDI | 2001 | 45–49 | Health 2000 | 2 | |
| Aalto et al. (2012)* | 0.16 | Finland | 412 | 412 | BDI | 2001 | 50–54 | Health 2000 | 2 | |
| Aalto et al. (2012)* | 0.37 | Finland | 263 | 304 | BDI | 2001 | 55–59 | Health 2000 | 2 | |
| Aalto et al. (2012)* | 0.19 | Finland | 244 | 289 | BDI | 2001 | 60–64 | Health 2000 | 2 | |
| Aalto et al. (2012)* | 0.31 | Finland | 178 | 231 | BDI | 2001 | 65–69 | Health 2000 | 2 | |
| Aalto et al. (2012)* | 0.22 | Finland | 348 | 656 | BDI | 2001 | 70+ | Health 2000 | 2 | |
| Abebe et al. (2016)* | 0.47 | Norway | 12867 | 13146 | DMI | 2012 | 13 | Ungdata | 2 | |
| Abebe et al. (2016)* | 0.64 | Norway | 11018 | 11184 | DMI | 2012 | 14 | Ungdata | 2 | |
| Abebe et al. (2016)* | 0.70 | Norway | 12624 | 12369 | DMI | 2012 | 15 | Ungdata | 2 | |
| Abebe et al. (2016)* | 0.69 | Norway | 8266 | 7811 | DMI | 2012 | 16 | Ungdata | 2 | |
| Almqvist et al. (1999) | −0.11 | Finland | 2880 | 2805 | CDI | 1990 | 8–9 | Finnish Nationwide 1981 Birth Cohort Study | 2 | |
| Andersen et al. (2009)* | 0.14 | Denmark | 1701 | 2066 | MDI | 2000 | 40–49 | Danish Longitudinal Study on Work, Unemployment & Health | 2 | |
| Andersen et al. (2009)* | 0.14 | Denmark | 1695 | 1699 | MDI | 2000 | 50–56 | Danish Longitudinal Study on Work, Unemployment & Health | 2 | |
| Belanger et al (2011)* | 0.37 | Switzerland | 481 | 355 | DTS | 2002 | 16 | Swiss Multicenter Adolescent Survey on Health (SMASH) | 2 | |
| Belanger et al (2011)* | 0.50 | Switzerland | 996 | 976 | DTS | 2002 | 17 | SMASH | 2 | |
| Belanger et al (2011)* | 0.31 | Switzerland | 1135 | 1072 | DTS | 2002 | 18 | SMASH | 2 | |
| Belanger et al (2011)* | 0.41 | Switzerland | 782 | 592 | DTS | 2002 | 19 | SMASH | 2 | |
| Belanger et al (2011)* | 0.08 | Switzerland | 503 | 304 | DTS | 2002 | 20 | SMASH | 2 | |
| Bracke (1998) | 0.32 | Belgium | 2907 | 3204 | HDL-D | 1992 | 16+ | Panel Study of Belgian Households | 1 | |
| Bushman et al. (2012)* | 0.08 | US | 251 | 549 | CES-D | 2011 | 18–90 | – | 1 | 2 |
| Cardozo et al. (2005)* | 0.23 | Afghanistan | 240 | 357 | SCL-D | 2002 | 15+ | Mental Health in Afghanistan Survey | 1 | |
| Cater et al. (2015)* | 0.36 | Sweden | 203 | 200 | HADS-D | 2011 | 20 | Resume Project | 1 | |
| Cater et al. (2015)* | 0.32 | Sweden | 215 | 265 | HADS-D | 2011 | 21 | Resume Project | 1 | |
| Cater et al. (2015)* | 0.31 | Sweden | 253 | 252 | HADS-D | 2011 | 22 | Resume Project | 1 | |
| Cater et al. (2015)* | 0.32 | Sweden | 265 | 300 | HADS-D | 2011 | 23 | Resume Project | 1 | |
| Cater et al. (2015)* | 0.44 | Sweden | 250 | 297 | HADS-D | 2011 | 24 | Resume Project | 1 | |
| Chan et al. (2011) | 0.16 | Singapore | 759 | 786 | CES-D | 2009 | 60–64 | Panel on Health and Aging of Singaporean Elderly (PHASE), Wave 2, 2011 | 1 | |
| Chan et al. (2011) | 0.22 | Singapore | 908 | 1039 | CES-D | 2009 | 65–74 | PHASE, Wave 2, 2011 | 1 | |
| Chan et al. (2011) | 0.28 | Singapore | 411 | 586 | CES-D | 2009 | 75+ | PHASE, Wave 2, 2011 | 1 | |
| Clark et al. (2013)* | 0.17 | New Zealand | 762 | 914 | RADS-SF | 2013 | 13 | Youth’12 | 3 | |
| Clark et al. (2013)* | 0.33 | New Zealand | 868 | 965 | RADS-SF | 2013 | 14 | Youth’12 | 3 | |
| Clark et al. (2013)* | 0.33 | New Zealand | 742 | 941 | RADS-SF | 2013 | 15 | Youth’12 | 3 | |
| Clark et al. (2013)* | 0.29 | New Zealand | 686 | 831 | RADS-SF | 2013 | 16 | Youth’12 | 3 | |
| Clark et al. (2013)* | 0.32 | New Zealand | 467 | 652 | RADS-SF | 2013 | 17 | Youth’12 | 3 | |
| Collins et al. (2009)* | 0.30 | Taiwan | 2534 | 2176 | CES-D | 1996 | 50+ | Survey of Health & Living Status of the Near Elderly & Elderly | 2 | |
| Crimmins et al. (2011)* | 0.73 | Austria | 777 | 1072 | EURO-D | 2005 | 50+ | Survey of Health, Aging, & Retirement (SHARE) | 1 | |
| Crimmins et al. (2011)* | 1.04 | Belgium | 1715 | 1934 | EURO-D | 2005 | 50+ | SHARE | 1 | |
| Crimmins et al. (2011)* | 0.54 | Denmark | 757 | 858 | EURO-D | 2005 | 50+ | SHARE | 1 | |
| Crimmins et al. (2011)* | 0.36 | France | 1367 | 1671 | EURO-D | 2005 | 50+ | SHARE | 1 | |
| Crimmins et al. (2011)* | 0.30 | Germany | 1370 | 1571 | EURO-D | 2005 | 50+ | SHARE | 1 | |
| Crimmins et al. (2011)* | 1.04 | Greece | 1241 | 1428 | EURO-D | 2005 | 50+ | SHARE | 1 | |
| Crimmins et al. (2011)* | 0.36 | Italy | 1126 | 1382 | EURO-D | 2005 | 50+ | SHARE | 1 | |
| Crimmins et al. (2011)* | 0.56 | Netherlands | 1348 | 1517 | EURO-D | 2005 | 50+ | SHARE | 1 | |
| Crimmins et al. (2011)* | 0.57 | Spain | 989 | 1364 | EURO-D | 2005 | 50+ | SHARE | 1 | |
| Crimmins et al. (2011)* | 0.96 | Sweden | 1407 | 1590 | EURO-D | 2005 | 50+ | SHARE | 1 | |
| Crimmins et al. (2011)* | 0.66 | Switzerland | 455 | 505 | EURO-D | 2005 | 50+ | SHARE | 1 | |
| de Wit et al. (2009)* | 0.24 | Netherlands | 2632 | 2970 | MHI-D | 2004 | 18–29 | Continuous Survey of Living Conditions (CCSLC) | 2 | |
| de Wit et al. (2009)* | 0.22 | Netherlands | 3206 | 3780 | MHI-D | 2004 | 30–39 | CCSLC | 2 | |
| de Wit et al. (2009)* | 0.17 | Netherlands | 3437 | 3727 | MHI-D | 2004 | 40–49 | CCSLC | 2 | |
| de Wit et al. (2009)* | 0.17 | Netherlands | 3297 | 3331 | MHI-D | 2004 | 50–59 | CCSLC | 2 | |
| de Wit et al. (2009)* | 0.29 | Netherlands | 2404 | 2166 | MHI-D | 2004 | 60–69 | CCSLC | 2 | |
| de Wit et al. (2009)* | 0.31 | Netherlands | 1813 | 2020 | MHI-D | 2004 | 70–90 | CCSLC | 2 | |
| Dooley et al. (2015)* | −0.15 | Ireland | 84 | 90 | DASS-D | 2011 | 12 | My World Survey | 2 | |
| Dooley et al. (2015)* | 0.11 | Ireland | 462 | 515 | DASS-D | 2011 | 13 | My World Survey | 2 | |
| Dooley et al. (2015)* | 0.22 | Ireland | 588 | 609 | DASS-D | 2011 | 14 | My World Survey | 2 | |
| Dooley et al. (2015)* | 0.33 | Ireland | 508 | 488 | DASS-D | 2011 | 15 | My World Survey | 2 | |
| Dooley et al. (2015)* | 0.34 | Ireland | 451 | 564 | DASS-D | 2011 | 16 | My World Survey | 2 | |
| Dooley et al. (2015)* | 0.43 | Ireland | 371 | 368 | DASS-D | 2011 | 17 | My World Survey | 2 | |
| Dooley et al. (2015)* | 0.27 | Ireland | 142 | 215 | DASS-D | 2011 | 18 | My World Survey | 2 | |
| Everson-Rose et al. (2004)* | 0.31 | US | 333 | 407 | CES-D | 1986 | 24–34 | American Changing Lives Survey | 1 | 2 |
| Everson-Rose et al. (2004)* | 0.23 | US | 228 | 363 | CES-D | 1986 | 35–44 | American Changing Lives Survey | 1 | 2 |
| Everson-Rose et al. (2004)* | −0.01 | US | 168 | 222 | CES-D | 1986 | 45–54 | American Changing Lives Survey | 1 | 2 |
| Everson-Rose et al. (2004)* | 0.14 | US | 251 | 434 | CES-D | 1986 | 55–65 | American Changing Lives Survey | 1 | 2 |
| Everson-Rose et al. (2004)* | 0.26 | US | 239 | 526 | CES-D | 1986 | 65–74 | American Changing Lives Survey | 1 | 2 |
| Everson-Rose et al. (2004)* | 0.23 | US | 139 | 307 | CES-D | 1986 | 75+ | American Changing Lives Survey | 1 | 2 |
| Ferketich et al. (2000) | 0.25 | US | 2888 | 5006 | CES-D | 1983 | 30+ | National Health & Nutrition Examination Follow-up Study (NHEFS) | 1 | 1 |
| Fleiz Bautista et al. (2012)* | 0.31 | Mexico | 4613 | 4707 | CES-D | 2008 | 12–17 | National Survey on Addictions | 2 | |
| Fleiz Bautista et al. (2012)* | 0.24 | Mexico | 7343 | 7962 | CES-D | 2008 | 18–29 | National Survey on Addictions | 2 | |
| Fleiz Bautista et al. (2012)* | 0.29 | Mexico | 5199 | 5784 | CES-D | 2008 | 30–39 | National Survey on Addictions | 2 | |
| Fleiz Bautista et al. (2012)* | 0.34 | Mexico | 3833 | 4204 | CES-D | 2008 | 40–49 | National Survey on Addictions | 2 | |
| Fleiz Bautista et al. (2012)* | 0.29 | Mexico | 3623 | 3959 | CES-D | 2008 | 50–65 | National Survey on Addictions | 2 | |
| Fleming et al. (2014)* | 0.42 | New Zealand | 3074 | 2585 | RADS | 2007 | 12–15 | Youth 2000 | 2 | |
| Fleming et al. (2014)* | 0.32 | New Zealand | 1580 | 1453 | RADS | 2007 | 16–19 | Youth 2000 | 2 | |
| Gault-Sherman et al. (2009)* | 0.42 | Iceland | 1610 | 1596 | SCL- D | 2004 | 16 | Junior College Questionnaire | 1 | |
| Gault-Sherman et al. (2009)* | 0.36 | Iceland | 1138 | 1156 | SCL-D | 2004 | 17 | Junior College Questionnaire | 1 | |
| Gault-Sherman et al. (2009)* | 0.38 | Iceland | 835 | 927 | SCL-D | 2004 | 18 | Junior College Questionnaire | 1 | |
| Gault-Sherman et al. (2009)* | 0.33 | Iceland | 705 | 859 | SCL-D | 2004 | 19 | Junior College Questionnaire | 1 | |
| Gault-Sherman et al. (2009)* | 0.39 | Iceland | 314 | 284 | SCL-D | 2004 | 20 | Junior College Questionnaire | 1 | |
| Gettler & Oka (2016) | 0.14 | US | 1505 | 933 | PHQ-9 | 2012 | 20–60 | NHANES 2011–2012 | 1 | 1 |
| Graham et al. (2007) | 0.15 | Canada | 2781 | 3675 | CES-D | 2005 | 18–76 | Gender Alcohol & Culture: An International Study | 2 | |
| Guarnaccia et al. (1991) | 0.33 | US | 1369 | 1583 | CES-D | 1983 | 20–45 | HHANES | 5 | 2 |
| Guarnaccia et al. (1991) | 0.31 | US | 416 | 659 | CES-D | 1983 | 20–45 | HHANES | 5 | 2 |
| Guarnaccia et al. (1991) | 0.42 | US | 247 | 312 | CES-D | 1983 | 20–45 | HHANES | 5 | 2 |
| Gudmundsdottir et al. (2010) | 0.23 | Iceland | 967 | 955 | SCL-D | 1998 | 18–75 | - | 2 | |
| Hardie (2014) | 0.13 | US | 1116 | 1046 | CES-D | 1992 | 27–35 | National Longitudinal Survey of Youth (NLSY) ’79 | 3 | 2 |
| Hardie (2014) | 0.23 | US | 725 | 689 | CES-D | 1992 | 27–35 | NLSY ’79 | 5 | 2 |
| Hardie (2014) | 0.22 | US | 1841 | 1703 | CES-D | 1992 | 27–35 | NLSY ’79 | 2 | 2 |
| Haroz et al. (2014) | 0.45 | US | 585 | 785 | CES-D | 2014 | 13–14 | Teen Health and Technology | 1 | 2 |
| Haroz et al. (2014) | 0.27 | US | 856 | 1096 | CES-D | 2014 | 15–17 | Teen Health and Technology | 1 | 2 |
| Haroz et al. (2014) | 0.22 | US | 954 | 1404 | CES-D | 2014 | 18 | Teen Health and Technology | 1 | 2 |
| Haroz et al. (2014) | 0.16 | US | 95 | 99 | CES-D | 2008 | 11–12 | Growing up with Media | 1 | 2 |
| Haroz et al. (2014) | 0.47 | US | 201 | 191 | CES-D | 2008 | 13–14 | Growing up with Media | 1 | 2 |
| Haroz et al. (2014) | 0.11 | US | 192 | 172 | CES-D | 2008 | 15–17 | Growing up with Media | 1 | 2 |
| Haroz et al. (2014) | 0.25 | US | 94 | 106 | CES-D | 2012 | 18 | Growing up with Media | 1 | 2 |
| Haukkala et al. (2009)* | 0.19 | Finland | 622 | 833 | BDI | 1995 | 24–34 | Finrisk- 1995 | 1 | |
| Haukkala et al. (2009)* | 0.15 | Finland | 783 | 970 | BDI | 1995 | 35–44 | Finrisk- 1995 | 1 | |
| Haukkala et al. (2009)* | 0.07 | Finland | 885 | 991 | BDI | 1995 | 45–54 | Finrisk- 1995 | 1 | |
| Haukkala et al. (2009)* | 0.07 | Finland | 925 | 983 | BDI | 1995 | 55–64 | Finrisk- 1995 | 1 | |
| Haukkala et al. (2009)* | 0.22 | Finland | 493 | 189 | BDI | 1995 | 65–74 | Finrisk- 1995 | 1 | |
| Hauser et al. (2014)* | −0.07 | Germany | 128 | 144 | BDI | 2012 | 14–24 | Survey zu psychischen Befindlichkeiten Uni Leipzig | 2 | |
| Hauser et al. (2014)* | 0.08 | Germany | 166 | 181 | BDI | 2012 | 25–34 | Survey zu psychischen Befindlichkeiten Uni Leipzig | 2 | |
| Hauser et al. (2014)* | 0.15 | Germany | 165 | 195 | BDI | 2012 | 35–44 | Survey zu psychischen Befindlichkeiten Uni Leipzig | 2 | |
| Hauser et al. (2014)* | −0.09 | Germany | 208 | 252 | BDI | 2012 | 45–54 | Survey zu psychischen Befindlichkeiten Uni Leipzig | 2 | |
| Hauser et al. (2014)* | 0.07 | Germany | 212 | 250 | BDI | 2012 | 55–64 | Survey zu psychischen Befindlichkeiten Uni Leipzig | 2 | |
| Hauser et al. (2014)* | −0.07 | Germany | 209 | 195 | BDI | 2012 | 65–74 | Survey zu psychischen Befindlichkeiten Uni Leipzig | 2 | |
| Hauser et al. (2014)* | 0.18 | Germany | 76 | 113 | BDI | 2012 | 85+ | Survey zu psychischen Befindlichkeiten Uni Leipzig | 2 | |
| Huang & Chen (2015)* | 0.45 | Taiwan | 52 | 64 | CES-D | 2010 | 15 | – | 2 | |
| Huang & Chen (2015)* | −0.01 | Taiwan | 253 | 283 | CES-D | 2010 | 16 | – | 2 | |
| Huang & Chen (2015)* | 0.10 | Taiwan | 205 | 206 | CES-D | 2010 | 17 | – | 2 | |
| Huang & Chen (2015)* | 0.32 | Taiwan | 43 | 90 | CES-D | 2010 | 18 | – | 2 | |
| Hwang et al. (2009)* | 0.17 | Taiwan | 2904 | 2966 | - | 2004 | 12–17 | Adolescent Internet Use, Daily Life, & Depressive Mood Survey | 2 | |
| Inaba et al. (2005)* | 0.09 | Japan | 740 | 834 | CES-D | 1999 | 28–39 | National Family Research of Japan ’98 Survey (NFRJ98) | 1 | |
| Inaba et al. (2005)* | 0.15 | Japan | 675 | 732 | CES-D | 1999 | 40–49 | NFRJ98 | 1 | |
| Inaba et al. (2005)* | 0.18 | Japan | 670 | 794 | CES-D | 1999 | 50–59 | NFRJ98 | 1 | |
| Inaba et al. (2005)* | 0.17 | Japan | 906 | 977 | CES-D | 1999 | 60–78 | NFRJ98 | 1 | |
| Inaba et al. (2005)* | 0.27 | US | 1372 | 1413 | CES-D | 1994 | 28–39 | National Survey of Families & Households (NSFH) in the US | 1 | 1 |
| Inaba et al. (2005)* | 0.22 | US | 1013 | 987 | CES-D | 1994 | 40–49 | NSFH | 1 | 1 |
| Inaba et al. (2005)* | 0.38 | US | 594 | 716 | CES-D | 1994 | 50–59 | NSFH | 1 | 1 |
| Inaba et al. (2005)* | 0.29 | US | 856 | 1220 | CES-D | 1994 | 60–78 | NSFH | 1 | 1 |
| Ismayilova et al. (2013)* | 0.32 | Jordan | 3513 | 3252 | - | 2009 | 14–18 | – | 2 | |
| Jaddou et al. (2012)* | 0.36 | Jordan | 1008 | 2994 | DASS-D | 2009 | 25+ | – | 2 | |
| Jang et al. (2009) | 0.14 | South Korea | 1320 | 1648 | CES-D | 2006 | 45–54 | Korean Longitudinal Study of Aging | 1 | |
| Jang et al. (2009) | 0.19 | South Korea | 1163 | 1341 | CES-D | 2006 | 55–64 | Korean Longitudinal Study of Aging | 1 | |
| Jang et al. (2009) | 0.32 | South Korea | 1095 | 1306 | CES-D | 2006 | 65–74 | Korean Longitudinal Study of Aging | 1 | |
| Jang et al. (2009) | 0.26 | South Korea | 483 | 708 | CES-D | 2006 | 75–85 | Korean Longitudinal Study of Aging | 1 | |
| Kaji et al. (2010)* | 0.10 | Japan | 2543 | 2583 | CES-D | 2000 | 50–59 | Active Survey of Health & Welfare in Japan | 2 | |
| Kaji et al. (2010)* | 0.04 | Japan | 1691 | 1745 | CES-D | 2000 | 60–69 | Active Survey of Health & Welfare in Japan | 2 | |
| Kaji et al. (2010)* | 0.13 | Japan | 799 | 1003 | CES-D | 2000 | 70–79 | Active Survey of Health & Welfare in Japan | 2 | |
| Kaji et al. (2010)* | 0.10 | Japan | 200 | 495 | CES-D | 2000 | 80+ | Active Survey of Health & Welfare in Japan | 2 | |
| Karadog et al. (2014)* | 0.34 | Turkey | 400 | 342 | BDI | 2012 | 18–24 | Prevalence of Sleep Disorders in the Turkish Adult Population Epidemiology of Sleep (TAPES) Study | 1 | |
| Karadog et al. (2014)* | 0.34 | Turkey | 538 | 742 | BDI | 2012 | 25–34 | TAPES Study | 1 | |
| Karadog et al. (2014)* | 0.26 | Turkey | 448 | 661 | BDI | 2012 | 35–44 | TAPES Study | 1 | |
| Karadog et al. (2014)* | 0.20 | Turkey | 451 | 429 | BDI | 2012 | 45–54 | TAPES Study | 1 | |
| Karadog et al. (2014)* | 0.29 | Turkey | 319 | 270 | BDI | 2012 | 55–64 | TAPES Study | 1 | |
| Karadog et al. (2014)* | 0.44 | Turkey | 266 | 152 | BDI | 2012 | 65+ | TAPES Study | 1 | |
| Kim (2016) | 0.30 | South Korea | 1137 | 1256 | - | 2003 | 13–14 | Korea Youth Panel Survey | 3 | |
| Kliem et al. (2014)* | 0.03 | Germany | 2106 | 2374 | BDI | 2012 | 14–91 | – | 2 | |
| Klomek et al. (2009)* | −0.16 | Finland | 2651 | 2583 | CDI | 1989 | 8 | – | 2 | |
| Kocalevent et al. (2013) | 0.12 | Germany | 292 | 272 | PHQ-9 | 2006 | 14–24 | – | 2 | |
| Kocalevent et al. (2013) | 0.16 | Germany | 279 | 351 | PHQ-9 | 2006 | 25–34 | – | 2 | |
| Kocalevent et al. (2013) | 0.16 | Germany | 396 | 542 | PHQ-9 | 2006 | 35–44 | – | 2 | |
| Kocalevent et al. (2013) | −0.05 | Germany | 414 | 457 | PHQ-9 | 2006 | 45–54 | – | 2 | |
| Kocalevent et al. (2013) | 0.04 | Germany | 398 | 446 | PHQ-9 | 2006 | 55–64 | – | 2 | |
| Kocalevent et al. (2013) | 0.18 | Germany | 397 | 395 | PHQ-9 | 2006 | 65–74 | – | 2 | |
| Kocalevent et al. (2013) | 0.11 | Germany | 156 | 236 | PHQ-9 | 2006 | 75+ | – | 2 | |
| Kokkevi et al. (2009)* | 0.43 | Armenia | 1569 | 2231 | CES-D | 2007 | 16 | European School Survey Project on Alcohol & Other Drugs (ESPAD) | 3 | |
| Kokkevi et al. (2009)* | 0.59 | Bulgaria | 1098 | 1056 | CES-D | 2007 | 16 | ESPAD | 3 | |
| Kokkevi et al. (2009)* | 0.66 | Croatia | 1497 | 1438 | CES-D | 2007 | 16 | ESPAD | 3 | |
| Kokkevi et al. (2009)* | 0.53 | Cyprus | 2936 | 3182 | CES-D | 2007 | 16 | ESPAD | 3 | |
| Kokkevi et al. (2009)* | 0.42 | Faroe Islands | 247 | 281 | CESD | 2007 | 16 | ESPAD | 3 | |
| Kokkevi et al. (2009)* | 0.69 | Finland | 2242 | 2641 | CES-D | 2007 | 16 | ESPAD | 3 | |
| Kokkevi et al. (2009)* | 0.54 | Hungary | 1277 | 1386 | CES-D | 2007 | 16 | ESPAD | 3 | |
| Kokkevi et al. (2009)* | 0.48 | Iceland | 1634 | 1629 | CES-D | 2007 | 16 | ESPAD | 3 | |
| Kokkevi et al. (2009)* | 0.59 | Ireland | 932 | 1136 | CES-D | 2007 | 16 | ESPAD | 3 | |
| Kokkevi et al. (2009)* | 0.50 | Isle of Man | 356 | 362 | CES-D | 2007 | 16 | ESPAD | 3 | |
| Kokkevi et al. (2009)* | 0.57 | Latvia | 1059 | 1135 | CES-D | 2007 | 16 | ESPAD | 3 | |
| Kokkevi et al. (2009)* | 0.70 | Romania | 943 | 1231 | CES-D | 2007 | 16 | ESPAD | 3 | |
| Kokkevi et al. (2009)* | 0.60 | Slovak Rep. | 1166 | 1211 | CES-D | 2007 | 16 | ESPAD | 3 | |
| Kokkevi et al. (2009)* | 0.70 | Slovenia | 1525 | 1466 | CES-D | 2007 | 16 | ESPAD | 3 | |
| Kokkevi et al. (2009)* | 0.56 | UK | 909 | 1120 | CES-D | 2007 | 16 | ESPAD | 3 | |
| Kokkevi et al. (2009)* | 0.52 | Greece | 4631 | 5242 | CES-D | 2007 | 14–18 | ESPAD | 2 | |
| Kokkevi et al. (2011)* | 0.61 | Greece | 5169 | 5336 | CES-D | 1984 | 14–18 | Greek National School Population Survey | 2 | |
| Kopp et al. (1995) | 0.07 | Hungary | 7767 | 7979 | BDI | 1988 | 16–65 | – | 2 | |
| Lee (2015)* | 0.16 | South Korea | 617 | 779 | PHQ-9 | 2012 | 50.6 | Korean General Social Survey | 2 | |
| Lei et al. (2014) | 0.20 | China | 1285 | 1740 | CES-D | 2012 | 45–49 | China Health & Retirement Longitudinal Study (CHARLS) | 2 | |
| Lei et al. (2014) | 0.24 | China | 1050 | 1182 | CES-D | 2012 | 50–54 | CHARLS | 2 | |
| Lei et al. (2014) | 0.26 | China | 1484 | 1591 | CES-D | 2012 | 55–59 | CHARLS | 2 | |
| Lei et al. (2014) | 0.31 | China | 1294 | 1270 | CES-D | 2012 | 60–64 | CHARLS | 2 | |
| Lei et al. (2014) | 0.30 | China | 839 | 801 | CES-D | 2012 | 65–59 | CHARLS | 2 | |
| Lei et al. (2014) | 0.22 | China | 639 | 569 | CES-D | 2012 | 70–74 | CHARLS | 2 | |
| Lei et al. (2014) | 0.37 | China | 585 | 596 | CES-D | 2012 | 75+ | CHARLS | 2 | |
| Madianos et al. (1992) | 0.45 | Greece | 1820 | 2263 | CES-D | 1978 | 19–64 | – | 2 | |
| Madianos et al. (1992) | 0.33 | Greece | 1660 | 2046 | CES-D | 1984 | 19–64 | – | 2 | |
| Mäntyselkä et al. (2003)* | 0.35 | Finland | 258 | 389 | DEPS | 2002 | 15–24 | Finnish Pain Study | 3 | |
| Mäntyselkä et al. (2003)* | 0.17 | Finland | 278 | 378 | DEPS | 2002 | 25–34 | Finnish Pain Study | 3 | |
| Mäntyselkä et al. (2003)* | 0.12 | Finland | 309 | 399 | DEPS | 2002 | 35–44 | Finnish Pain Study | 3 | |
| Mäntyselkä et al. (2003)* | −0.08 | Finland | 336 | 432 | DEPS | 2002 | 45–54 | Finnish Pain Study | 3 | |
| Mäntyselkä et al. (2003)* | 0.16 | Finland | 381 | 441 | DEPS | 2002 | 55–64 | Finnish Pain Study | 3 | |
| Mäntyselkä et al. (2003)* | 0.14 | Finland | 417 | 437 | DEPS | 2002 | 65–74 | Finnish Pain Study | 3 | |
| Margraf et al. (2016)* | −0.12 | US | 1252 | 1786 | DASS-D | 2013 | 18+ | Bochum Optimism and Mental Health (BOOM)- US | 1 | 3 |
| Margraf et al. (2016)* | 0.08 | Germany | 826 | 1181 | DASS-D | 2013 | 18+ | BOOM- Germany | 3 | |
| Margraf et al. (2016)* | 0.13 | Russia | 1413 | 1607 | DASS-D | 2013 | 18+ | Boom- Russia | 3 | |
| Marmorstein (2009)* | 0.12 | US | 262 | 329 | CES-D | 1995 | 12 | National Longitudinal Student of Adolescent Health (Add Health) | 1 | 2 |
| Marmorstein (2009)* | 0.22 | US | 1039 | 1218 | CES-D | 1995 | 13 | Add Health | 1 | 2 |
| Marmorstein (2009)* | 0.30 | US | 1319 | 1472 | CES-D | 1995 | 14 | Add Health | 1 | 2 |
| Marmorstein (2009)* | 0.34 | US | 1778 | 1883 | CES-D | 1995 | 15 | Add Health | 1 | 2 |
| Marmorstein (2009)* | 0.31 | US | 2061 | 1991 | CES-D | 1995 | 16 | Add Health | 1 | 2 |
| Marmorstein (2009)* | 0.19 | US | 1981 | 1940 | CES-D | 1995 | 17 | Add Health | 1 | 2 |
| Marmorstein (2009)* | 0.21 | US | 1512 | 1427 | CES-D | 1995 | 18 | Add Health | 1 | 2 |
| Marmorstein (2009)* | 0.34 | US | 237 | 159 | CES-D | 1995 | 19 | Add Health | 1 | 2 |
| Maske et al. (2016)* | 0.27 | Germany | 722 | 781 | PHQ-9 | 2010 | 18–34 | Germany Health Interview and Examination Survey for Adults (DEGS1) | 2 | |
| Maske et al. (2016)* | 0.28 | Germany | 553 | 646 | PHQ-9 | 2010 | 35–44 | DEGS1 | 2 | |
| Maske et al. (2016)* | 0.28 | Germany | 741 | 858 | PHQ-9 | 2010 | 45–54 | DEGS1 | 2 | |
| Maske et al. (2016)* | 0.25 | Germany | 652 | 718 | PHQ-9 | 2010 | 55–64 | DEGS1 | 2 | |
| Maske et al. (2016)* | 0.30 | Germany | 915 | 937 | PHQ-9 | 2010 | 65–79 | DEGS1 | 2 | |
| Michal et al. (2011)* | −0.07 | Germany | 1090 | 1385 | HADS- D | 2009 | 14–94 | – | 2 | |
| Momtaz et al. (2016)* | 0.15 | Malaysia | 564 | 696 | GDS-15 | 2014 | 60–69 | Identifying Psychosocial and Identifying Economic Risk Factor of Cognitive Impairment among Elderly | 3 | |
| Momtaz et al. (2016)* | 0.14 | Malaysia | 423 | 387 | GDS-15 | 2014 | 70–79 | Identifying Psychosocial and Identifying Economic Risk Factor of Cognitive Impairment among Elderly | 3 | |
| Momtaz et al. (2016)* | 0.15 | Malaysia | 67 | 65 | GDS-15 | 2014 | 80+ | Identifying Psychosocial and Identifying Economic Risk Factor of Cognitive Impairment among Elderly | 3 | |
| Morozink et al. (2010)* | 0.10 | US | 541 | 705 | CES-D | 2004 | 35–86 | Midlife in the United States (MIDUS) | 1 | 2 |
| Mumford et al. (2013)* | 0.48 | US | 815 | 765 | MHI-D | 2000 | 15 | National Longitudinal Survey of Youth (NLSY) ’97 | 1 | 2 |
| Mumford et al. (2013)* | 0.33 | US | 819 | 774 | MHI-D | 2000 | 16 | NLSY ’97 | 1 | 2 |
| Mumford et al. (2013)* | 0.29 | US | 811 | 773 | MHI-D | 2000 | 17 | NLSY ’97 | 1 | 2 |
| Mumford et al. (2013)* | 0.22 | US | 766 | 767 | MHI-D | 2000 | 18 | NLSY ’97 | 1 | 2 |
| Mumford et al. (2013)* | 0.23 | US | 657 | 681 | MHI-D | 2000 | 19 | NLSY ’97 | 1 | 2 |
| Munhoz et al. (2016)* | 0.32 | Brazil | 6246 | 8075 | PHQ-9 | 2013 | 18–29 | Brazilian National Healthy Survey | 2 | |
| Munhoz et al. (2016)* | 0.34 | Brazil | 6049 | 8220 | PHQ-9 | 2013 | 30–39 | Brazilian National Healthy Survey | 2 | |
| Munhoz et al. (2016)* | 0.37 | Brazil | 5079 | 6326 | PHQ-9 | 2013 | 40–49 | Brazilian National Healthy Survey | 2 | |
| Munhoz et al. (2016)* | 0.37 | Brazil | 3991 | 5039 | PHQ-9 | 2013 | 50–59 | Brazilian National Healthy Survey | 2 | |
| Munhoz et al. (2016)* | 0.26 | Brazil | 2595 | 3643 | PHQ-9 | 2013 | 60–69 | Brazilian National Healthy Survey | 2 | |
| Munhoz et al. (2016)* | 0.27 | Brazil | 1428 | 2013 | PHQ-9 | 2013 | 70–79 | Brazilian National Healthy Survey | 2 | |
| Munhoz et al. (2016)* | 0.14 | Brazil | 532 | 966 | PHQ-9 | 2013 | 80+ | Brazilian National Healthy Survey | 2 | |
| Neumark-Sztainer et al. (2000)* | 0.12 | US | 239 | 267 | CDI | 1997 | 10 | Commonwealth Fund Survey (of the Health of Adolescent Girls & Boys) | 1 | 1 |
| Neumark-Sztainer et al. (2000)* | 0.02 | US | 254 | 305 | CDI | 1997 | 11 | Commonwealth Fund Survey | 1 | 1 |
| Neumark-Sztainer et al. (2000)* | 0.04 | US | 386 | 461 | CDI | 1997 | 12 | Commonwealth Fund Survey | 1 | 1 |
| Neumark-Sztainer et al. (2000)* | 0.29 | US | 420 | 484 | CDI | 1997 | 13 | Commonwealth Fund Survey | 1 | 1 |
| Neumark-Sztainer et al. (2000)* | 0.22 | US | 370 | 462 | CDI | 1997 | 14 | Commonwealth Fund Survey | 1 | 1 |
| Neumark-Sztainer et al. (2000)* | 0.31 | US | 361 | 503 | CDI | 1997 | 15 | Commonwealth Fund Survey | 1 | 1 |
| Neumark-Sztainer et al. (2000)* | 0.32 | US | 399 | 497 | CDI | 1997 | 16 | Commonwealth Fund Survey | 1 | 1 |
| Neumark-Sztainer et al. (2000)* | 0.25 | US | 314 | 372 | CDI | 1997 | 17 | Commonwealth Fund Survey | 1 | 1 |
| O’Halloran et al. (2014)* | 0.21 | Ireland | 603 | 727 | CES-D | 2010 | 50–54 | The Irish Longitudinal Study on Ageing (TILDA) | 2 | |
| O’Halloran et al. (2014)* | 0.18 | Ireland | 591 | 754 | CES-D | 2010 | 55–59 | TILDA | 2 | |
| O’Halloran et al. (2014)* | 0.20 | Ireland | 502 | 647 | CES-D | 2010 | 60–64 | TILDA | 2 | |
| O’Halloran et al. (2014)* | 0.19 | Ireland | 487 | 502 | CES-D | 2010 | 65–69 | TILDA | 2 | |
| O’Halloran et al. (2014)* | 0.35 | Ireland | 383 | 376 | CES-D | 2010 | 70–74 | TILDA | 2 | |
| O’Halloran et al. (2014)* | 0.27 | Ireland | 449 | 521 | CES-D | 2010 | 75+ | TILDA | 2 | |
| Oh et al. (2013)* | 0.30 | South Korea | 14452 | 16146 | CES-D | 2009 | 19–29 | Korean Community Health Survey | 2 | |
| Oh et al. (2013)* | 0.19 | South Korea | 20031 | 21340 | CES-D | 2009 | 30–39 | Korean Community Health Survey | 2 | |
| Oh et al. (2013)* | 0.17 | South Korea | 23381 | 24288 | CES-D | 2009 | 40–49 | Korean Community Health Survey | 2 | |
| Oh et al. (2013)* | 0.22 | South Korea | 19781 | 21722 | CES-D | 2009 | 50–59 | Korean Community Health Survey | 2 | |
| Oh et al. (2013)* | 0.39 | South Korea | 15986 | 19191 | CES-D | 2009 | 60–69 | Korean Community Health Survey | 2 | |
| Oh et al. (2013)* | 0.35 | South Korea | 12912 | 20365 | CES-D | 2009 | 70+ | Korean Community Health Survey | 2 | |
| Ojard et al. (2015)* | 0.29 | US | 8751 | 8802 | CES-D | 2005 | 45+ | Reasons for Geographic & Racial Differences in Stroke (REGARDS) | 2 | 2 |
| Ojard et al. (2015)* | 0.19 | US | 4705 | 7710 | CES-D | 2005 | 45+ | REGARDS | 3 | 2 |
| Okabayashi et al. (2004)* | 0.21 | Japan | 995 | 1205 | CES-D | 1987 | 60+ | – | 3 | |
| Oksuzyan et al. (2010)* | 0.13 | US | 640 | 1013 | CES-D | 2006 | 50–54 | US Health & Retirement Survey | 1 | 1 |
| Oksuzyan et al. (2010)* | 0.05 | US | 1051 | 1472 | CES-D | 2006 | 55–59 | US Health & Retirement Survey | 1 | 1 |
| Oksuzyan et al. (2010)* | 0.10 | US | 936 | 1463 | CES-D | 2006 | 60–64 | US Health & Retirement Survey | 1 | 1 |
| Oksuzyan et al. (2010)* | 0.11 | US | 1537 | 1879 | CES-D | 2006 | 65–69 | US Health & Retirement Survey | 1 | 1 |
| Oksuzyan et al. (2010)* | 0.12 | US | 1267 | 1560 | CES-D | 2006 | 70–74 | US Health & Retirement Survey | 1 | 1 |
| Oksuzyan et al. (2010)* | 0.16 | US | 906 | 1128 | CES-D | 2006 | 75–79 | US Health & Retirement Survey | 1 | 1 |
| Oksuzyan et al. (2010)* | 0.11 | US | 647 | 917 | CES-D | 2006 | 80–84 | US Health & Retirement Survey | 1 | 1 |
| Oksuzyan et al. (2010)* | 0.04 | US | 344 | 649 | CES-D | 2006 | 85–89 | US Health & Retirement Survey | 1 | 1 |
| Oksuzyan et al. (2010)* | 0.04 | US | 142 | 379 | CES-D | 2006 | 90+ | US Health & Retirement Survey | 1 | 1 |
| Oksuzyan et al. (2010)* | 0.01 | Japan | 181 | 213 | CES-D | 2006 | 67–69 | Nihon University Japanese Longitudinal Study of Aging (NUJLSOA) | 1 | |
| Oksuzyan et al. (2010)* | 0.00 | Japan | 435 | 469 | CES-D | 2006 | 70–74 | NUJLSOA | 1 | |
| Oksuzyan et al. (2010)* | −0.03 | Japan | 302 | 329 | CES-D | 2006 | 75–79 | NUJLSOA | 1 | |
| Oksuzyan et al. (2010)* | −0.03 | Japan | 263 | 373 | CES-D | 2006 | 80–84 | NUJLSOA | 1 | |
| Oksuzyan et al. (2010)* | 0.04 | Japan | 133 | 217 | CES-D | 2006 | 85–89 | NUJLSOA | 1 | |
| Olsen et al. (2006) | 0.31 | Denmark | 121 | 165 | SCL-D | 2000 | 19–34 | – | 2 | |
| Olsen et al. (2006) | 0.29 | Denmark | 133 | 184 | SCL-D | 2000 | 35–49 | – | 2 | |
| Olsen et al. (2006) | 0.28 | Denmark | 135 | 150 | SCL-D | 2000 | 50–64 | – | 2 | |
| Olsen et al. (2006) | 0.09 | Denmark | 143 | 121 | SCL-D | 2000 | 65–80 | – | 2 | |
| Ostbye et al. (2009)* | 0.20 | Sri Lanka | 463 | 623 | GDS | 2006 | 60+ | National Sri Lanka Aging Survey | 2 | |
| Park et al. (2012)* | −0.04 | South Korea | 98 | 309 | GDS | 2008 | 85+ | Nationwide Survey on Dementia in Korea | 2 | |
| Park et al. (2012)* | 0.13 | South Korea | 180 | 447 | GDS | 2008 | 80–84 | Nationwide Survey on Dementia in Korea | 2 | |
| Park et al. (2012)* | 0.17 | South Korea | 455 | 740 | GDS | 2008 | 75–79 | Nationwide Survey on Dementia in Korea | 2 | |
| Park et al. (2012)* | 0.36 | South Korea | 790 | 1037 | GDS | 2008 | 70–74 | Nationwide Survey on Dementia in Korea | 2 | |
| Park et al. (2012)* | 0.33 | South Korea | 885 | 1077 | GDS | 2008 | 64–69 | Nationwide Survey on Dementia in Korea | 2 | |
| Revah-Levy et al. (2011) | 0.43 | France | 19884 | 19658 | ADRS | 2008 | 17 | ESCAPAD 2008 (Enqueˆte sur lar Santé et les Consommations lors de l’Appel de Préparation à la Défense) | 1 | |
| Rey et al. (2001)* | 0.30 | Australia | 594 | 654 | CES-D | 1998 | 13–17 | National Survey of Mental Health & Well-being | 2 | |
| Rief et al. (2012)* | 0.06 | Germany | 1202 | 1316 | PHQ-9 | 2008 | 14+ | – | 2 | |
| Risal et al. (2016)* | 0.02 | Nepal | 189 | 300 | HADS-D | 2013 | 18–25 | – | 2 | |
| Risal et al. (2016)* | 0.32 | Nepal | 217 | 440 | HADS-D | 2013 | 26–35 | – | 2 | |
| Risal et al. (2016)* | 0.20 | Nepal | 196 | 242 | HADS-D | 2013 | 36–45 | – | 2 | |
| Risal et al. (2016)* | 0.37 | Nepal | 138 | 160 | HADS-D | 2013 | 46–55 | – | 2 | |
| Risal et al. (2016)* | 0.09 | Nepal | 121 | 97 | HADS-D | 2013 | 56–65 | – | 2 | |
| Sandman et al. (2015)* | 0.25 | Finland | 263 | 361 | BDI | 2007 | 25–34 | Finrisk- 2007 | 3 | |
| Sandman et al. (2015)* | 0.26 | Finland | 318 | 392 | BDI | 2007 | 35–44 | Finrisk- 2007 | 3 | |
| Sandman et al. (2015)* | 0.14 | Finland | 371 | 442 | BDI | 2007 | 45–54 | Finrisk- 2007 | 3 | |
| Sandman et al. (2015)* | 0.07 | Finland | 412 | 452 | BDI | 2007 | 55–64 | Finrisk- 2007 | 3 | |
| Sandman et al. (2015)* | 0.16 | Finland | 407 | 420 | BDI | 2007 | 65–74 | Finrisk- 2007 | 3 | |
| Sandman et al. (2015)* | 0.29 | Finland | 260 | 410 | BDI | 2012 | 25–34 | Finrisk- 2012 | 3 | |
| Sandman et al. (2015)* | 0.30 | Finland | 338 | 469 | BDI | 2012 | 35–44 | Finrisk- 2012 | 3 | |
| Sandman et al. (2015)* | 0.11 | Finland | 430 | 534 | BDI | 2012 | 45–54 | Finrisk- 2012 | 3 | |
| Sandman et al. (2015)* | 0.20 | Finland | 503 | 580 | BDI | 2012 | 55–64 | Finrisk- 2012 | 3 | |
| Sandman et al. (2015)* | 0.16 | Finland | 613 | 592 | BDI | 2012 | 65–74 | Finrisk- 2012 | 3 | |
| Scafato et al. (2012)* | 0.56 | Italy | 1713 | 1501 | GDS | 1993 | 65–84 | Italian Longitudinal Study on Aging | 2 | |
| Seaton et al. (2008) | 0.02 | US | 563 | 605 | CES-D | 2002 | 13–17 | National Survey of African Life | 3 | 2 |
| Seppälä et al. (2012)* | 0.19 | Finland | 391 | 483 | BDI | 2007 | 45–54 | FIN-D2D | 2 | |
| Seppälä et al. (2012)* | 0.21 | Finland | 450 | 511 | BDI | 2007 | 55–64 | FIN-D2D | 2 | |
| Seppälä et al. (2012)* | 0.23 | Finland | 487 | 484 | BDI | 2007 | 65–74 | FIN-D2D | 2 | |
| Shiovitz-Ezra et al. (2009)* | 0.23 | US | 521 | 484 | CES-D | 2006 | 57–64 | National Social Life, Health, & Aging Project (NSHAP) | 1 | 2 |
| Shiovitz-Ezra et al. (2009)* | 0.16 | US | 543 | 537 | CES-D | 2006 | 65–74 | NSHAP | 1 | 2 |
| Shiovitz-Ezra et al. (2009)* | 0.09 | US | 373 | 499 | CES-D | 2006 | 75–85 | NSHAP | 1 | 2 |
| Sigfusdottir et al. (2008) | 0.49 | Iceland | 1927 | 1802 | SCL-D | 1997 | 14–15 | Youth in Iceland- 1997 | 2 | |
| Sigfusdottir et al. (2008) | 0.39 | Iceland | 2908 | 3132 | SCL-D | 2000 | 14–15 | Youth in Iceland- 2000 | 2 | |
| Sigfusdottir et al. (2008) | 0.45 | Iceland | 1709 | 1662 | SCL-D | 2003 | 14–15 | Youth in Iceland- 2003 | 2 | |
| Sigfusdottir et al. (2008) | 0.55 | Iceland | 3437 | 3503 | SCL-D | 2006 | 14–15 | Youth in Iceland- 2006 | 2 | |
| Song (2011)* | 0.11 | US | 939 | 1124 | CES-D | 2005 | 21–64 | – | 2 | 3 |
| Song (2011)* | 0.30 | US | 167 | 188 | CES-D | 2005 | 21–64 | – | 3 | 3 |
| Song (2011)* | 0.21 | US | 187 | 225 | CES-D | 2005 | 21–64 | – | 5 | 3 |
| Sonnenberg et al. (2013)* | 0.26 | Netherlands | 449 | 483 | CES-D | 1993 | 55–64 | Longitudinal Aging Study Amsterdam | 1 | |
| Sonnenberg et al. (2013)* | 0.44 | Netherlands | 423 | 476 | CES-D | 1993 | 65–74 | Longitudinal Aging Study Amsterdam | 1 | |
| Sonnenberg et al. (2013)* | 0.31 | Netherlands | 497 | 495 | CES-D | 1993 | 75–85 | Longitudinal Aging Study Amsterdam | 1 | |
| Steptoe et al. (2012) | 0.28 | England | 3540 | 4255 | CES-D | 2009 | 50–90 | English Longitudinal Study of Ageing | 1 | |
| Strong et al. (2016)* | 0.22 | Taiwan | 2113 | 2148 | - | 2001 | 13 | Taiwan Education Panel Survey | 2 | |
| Sugihara et al. (2008) | 0.12 | Japan | 2533 | 1440 | CES-D | 1999 | 55–64 | Japanese Health & Retirement Study | 1 | |
| Symonds et al. (2016)* | 0.42 | England | 6549 | 6422 | GHQ-D | 2005 | 15 | Longitudinal Study of Young People in England | 3 | |
| Thege et al. (2009)* | 0.14 | Hungary | 5416 | 6709 | BDI | 2002 | 18–98 | Hungaro Study | 3 | |
| Thibodeau et al. (2014)* | 0.29 | US | 550 | 500 | PHQ-9 | 2008 | 18–29 | National Health & Nutrition Examination Survey (NHANES)- 2008 | 1 | 1 |
| Thibodeau et al. (2014)* | 0.34 | US | 431 | 447 | PHQ-9 | 2008 | 30–39 | NHANES- 2008 | 1 | 1 |
| Thibodeau et al. (2014)* | 0.30 | US | 391 | 452 | PHQ-9 | 2008 | 40–49 | NHANES- 2008 | 1 | 1 |
| Thibodeau et al. (2014)* | 0.23 | US | 418 | 400 | PHQ-9 | 2008 | 50–59 | NHANES- 2008 | 1 | 1 |
| Thibodeau et al. (2014)* | 0.29 | US | 434 | 459 | PHQ-9 | 2008 | 60–69 | NHANES- 2008 | 1 | 1 |
| Thibodeau et al. (2014)* | 0.25 | US | 483 | 482 | PHQ-9 | 2008 | 70+ | NHANES- 2008 | 1 | 1 |
| Torikka et al. (2014)* | 0.35 | Finland | 47586 | 47049 | BDI | 2001 | 14–16 | School Health Promotion Study, 2000–2001 | 2 | |
| Torikka et al. (2014)* | 0.34 | Finland | 50744 | 49236 | BDI | 2003 | 14–16 | School Health Promotion Study (SHPS), 2002–2003 | 2 | |
| Torikka et al. (2014)* | 0.35 | Finland | 53057 | 51713 | BDI | 2005 | 14–16 | SHPS 2004–2005 | 2 | |
| Torikka et al. (2014)* | 0.33 | Finland | 54315 | 54005 | BDI | 2007 | 14–16 | SHPS, 2006–2007 | 2 | |
| Torikka et al. (2014)* | 0.33 | Finland | 54132 | 54035 | BDI | 2009 | 14–16 | SHPS, 2008–2009 | 2 | |
| Torikka et al. (2014)* | 0.37 | Finland | 51116 | 51066 | BDI | 2011 | 14–16 | SHPS, 2010–2011 | 2 | |
| Torres & Wong (2013)* | 0.38 | Mexico | 1094 | 1523 | CES-D | 2001 | 60–69 | Mexican Health & Aging Study | 2 | |
| Torres & Wong (2013)* | 0.38 | Mexico | 672 | 843 | CES-D | 2001 | 70–79 | Mexican Health & Aging Study | 2 | |
| Torres & Wong (2013)* | 0.27 | Mexico | 208 | 330 | CES-D | 2001 | 80+ | Mexican Health & Aging Study | 2 | |
| Torres & Wong (2013)* | 0.49 | Mexico | 2027 | 2166 | CES-D | 2001 | 50–59 | Mexican Health & Aging Study | 2 | |
| Van de Velde et al. (2010)* | 0.14 | Austria | 1099 | 1285 | CES-D | 2007 | 15–99 | European Social Survey (ESS)- 3 | 1 | |
| Van de Velde et al. (2010)* | 0.33 | Belgium | 839 | 958 | CES-D | 2007 | 15–99 | ESS-3 | 1 | |
| Van de Velde et al. (2010)* | 0.21 | Bulgaria | 544 | 828 | CES-D | 2007 | 15–99 | ESS-3 | 1 | |
| Van de Velde et al. (2010)* | 0.17 | Switzerland | 840 | 963 | CES-D | 2007 | 15–99 | ESS-3 | 1 | |
| Van de Velde et al. (2010)* | 0.42 | Cyprus | 471 | 523 | CES-D | 2007 | 15–99 | ESS-3 | 1 | |
| Van de Velde et al. (2010)* | 0.21 | Germany | 1437 | 1473 | CES-D | 2007 | 15–99 | ESS-3 | 1 | |
| Van de Velde et al. (2010)* | 0.16 | Denmark | 729 | 756 | CES-D | 2007 | 15–99 | ESS-3 | 1 | |
| Van de Velde et al. (2010)* | 0.21 | Estonia | 658 | 855 | CES-D | 2007 | 15–99 | ESS-3 | 1 | |
| Van de Velde et al. (2010)* | 0.35 | Spain | 905 | 969 | CES-D | 2007 | 15–99 | ESS-3 | 1 | |
| Van de Velde et al. (2010)* | 0.09 | Finland | 915 | 976 | CES-D | 2007 | 15–99 | ESS-3 | 1 | |
| Van de Velde et al. (2010)* | 0.29 | France | 968 | 1018 | CES-D | 2007 | 15–99 | ESS-3 | 1 | |
| Van de Velde et al. (2010)* | 0.17 | UK | 1137 | 1257 | CES-D | 2007 | 15–99 | ESS-3 | 1 | |
| Van de Velde et al. (2010)* | 0.18 | Hungary | 640 | 874 | CES-D | 2007 | 15–99 | ESS-3 | 1 | |
| Van de Velde et al. (2010)* | 0.03 | Ireland | 812 | 928 | CES-D | 2007 | 15–99 | ESS-3 | 1 | |
| Van de Velde et al. (2010)* | 0.31 | Netherlands | 897 | 991 | CES-D | 2007 | 15–99 | ESS-3 | 1 | |
| Van de Velde et al. (2010)* | 0.15 | Norway | 889 | 859 | CES-D | 2007 | 15–99 | ESS-3 | 1 | |
| Van de Velde et al. (2010)* | 0.29 | Poland | 815 | 896 | CES-D | 2007 | 15–99 | ESS-3 | 1 | |
| Van de Velde et al. (2010)* | 0.37 | Portugal | 911 | 1309 | CES-D | 2007 | 15–99 | ESS-3 | 1 | |
| Van de Velde et al. (2010)* | 0.35 | Russian Fed | 994 | 1395 | CES-D | 2007 | 15–99 | ESS-3 | 1 | |
| Van de Velde et al. (2010)* | 0.28 | Sweden | 948 | 973 | CES-D | 2007 | 15–99 | ESS-3 | 1 | |
| Van de Velde et al. (2010)* | 0.23 | Slovenia | 665 | 807 | CES-D | 2007 | 15–99 | ESS-3 | 1 | |
| Van de Velde et al. (2010)* | 0.13 | Slovakia | 839 | 895 | CES-D | 2007 | 15–99 | ESS-3 | 1 | |
| Van de Velde et al. (2010)* | 0.21 | Ukraine | 849 | 1136 | CES-D | 2007 | 15–99 | ESS-3 | 1 | |
| Van de Velde (personal communication, April 2, 2015)* | 0.27 | Belgium | 910 | 958 | CES-D | 2013 | 15–99 | ESS-6 | 2 | |
| Van de Velde (2015)* | 0.24 | Bulgaria | 971 | 1282 | CES-D | 2013 | 15–99 | ESS-6 | 2 | |
| Van de Velde (2015)* | 0.41 | Cyprus | 485 | 631 | CES-D | 2013 | 15–99 | ESS-6 | 2 | |
| Van de Velde (2015)* | 0.23 | Czech Republic | 1012 | 977 | CES-D | 2013 | 15–99 | ESS-6 | 2 | |
| Van de Velde (2015)* | 0.20 | Denmark | 832 | 814 | CES-D | 2013 | 15–99 | ESS-6 | 2 | |
| Van de Velde (2015)* | 0.13 | Estonia | 999 | 1379 | CES-D | 2013 | 15–99 | ESS-6 | 2 | |
| Van de Velde (2015)* | 0.09 | Finland | 1074 | 1121 | CES-D | 2013 | 15–99 | ESS-6 | 2 | |
| Van de Velde (2015)* | 0.24 | Germany | 1487 | 1469 | CES-D | 2013 | 15–99 | ESS-6 | 2 | |
| Van de Velde (2015)* | 0.06 | Ireland | 1266 | 1357 | CES-D | 2013 | 15–99 | ESS-6 | 2 | |
| Van de Velde (2015)* | 0.09 | Israel | 1142 | 1354 | CES-D | 2013 | 15–99 | ESS-6 | 2 | |
| Van de Velde (2015)* | 0.25 | Kosovo | 619 | 676 | CES-D | 2013 | 15–99 | ESS-6 | 2 | |
| Van de Velde (2015)* | 0.24 | Netherlands | 866 | 979 | CES-D | 2013 | 15–99 | ESS-6 | 2 | |
| Van de Velde (2015)* | 0.14 | Norway | 855 | 763 | CES-D | 2013 | 15–99 | ESS-6 | 2 | |
| Van de Velde (2015)* | 0.31 | Poland | 908 | 985 | CES-D | 2013 | 15–99 | ESS-6 | 2 | |
| Van de Velde (2015)* | 0.28 | Portugal | 867 | 1284 | CES-D | 2013 | 15–99 | ESS-6 | 2 | |
| Van de Velde (2015)* | 0.27 | Russian Fed. | 978 | 1484 | CES-D | 2013 | 15–99 | ESS-6 | 2 | |
| Van de Velde (2015)* | 0.08 | Slovakia | 795 | 1046 | CES-D | 2013 | 15–99 | ESS-6 | 2 | |
| Van de Velde (2015)* | 0.22 | Slovenia | 572 | 684 | CES-D | 2013 | 15–99 | ESS-6 | 2 | |
| Van de Velde (2015)* | 0.35 | Spain | 912 | 975 | CES-D | 2013 | 15–99 | ESS-6 | 2 | |
| Van de Velde (2015)* | 0.20 | Sweden | 947 | 900 | CES-D | 2013 | 15–99 | ESS-6 | 2 | |
| Van de Velde (2015)* | 0.28 | Switzerland | 746 | 747 | CES-D | 2013 | 15–99 | ESS-6 | 2 | |
| Van de Velde (2015)* | 0.15 | UK | 990 | 1293 | CES-D | 2013 | 15–99 | ESS-6 | 2 | |
| van Praag et al. (2009) | 0.29 | Belgium | 9378 | 10085 | SCL-D | 2003 | 15+ | Belgian Health Interview Survey | 1 | |
| Villatoro et al. (1998)* | 0.08 | Mexico | 5319 | 5511 | CES-D | 1991 | 12 | 1991 National School Survey | 2 | |
| Villatoro et al. (1998)* | 0.24 | Mexico | 7002 | 6819 | CES-D | 1991 | 13 | 1991 National School Survey | 2 | |
| Villatoro et al. (1998)* | 0.29 | Mexico | 6305 | 5768 | CES-D | 1991 | 14 | 1991 National School Survey | 2 | |
| Villatoro et al. (1998)* | 0.35 | Mexico | 4848 | 4000 | CES-D | 1991 | 15 | 1991 National School Survey | 2 | |
| Villatoro et al. (1998)* | 0.36 | Mexico | 3349 | 2971 | CES-D | 1991 | 16 | 1991 National School Survey | 2 | |
| Villatoro et al. (1998)* | 0.42 | Mexico | 2197 | 1725 | CES-D | 1991 | 17 | 1991 National School Survey | 2 | |
| Villatoro et al. (1998)* | 0.39 | Mexico | 991 | 635 | CES-D | 1991 | 18 | 1991 National School Survey | 2 | |
| Villatoro et al. (1998)* | 0.28 | Mexico | 431 | 297 | CES-D | 1991 | 19 | 1991 National School Survey | 2 | |
| von Soest & Wichstrom (2014)* | 0.21 | Norway | 724 | 802 | SCL-D | 2002 | 13 | Young in Norway | 2 | |
| von Soest et al. (2014)* | 0.32 | Norway | 899 | 950 | SCL-D | 2002 | 14 | Young in Norway | 2 | |
| von Soest et al. (2014)* | 0.38 | Norway | 932 | 959 | SCL-D | 2002 | 15 | Young in Norway | 2 | |
| von Soest et al. (2014)* | 0.41 | Norway | 704 | 698 | SCL-D | 2002 | 16 | Young in Norway | 2 | |
| von Soest et al. (2014)* | 0.42 | Norway | 1004 | 992 | SCL-D | 2002 | 17 | Young in Norway | 2 | |
| von Soest et al. (2014)* | 0.42 | Norway | 714 | 906 | SCL-D | 2002 | 18 | Young in Norway | 2 | |
| von Soest et al. (2014)* | 0.21 | Norway | 418 | 416 | SCL-D | 2010 | 12 | Young in Norway | 2 | |
| von Soest et al. (2014)* | 0.21 | Norway | 694 | 761 | SCL-D | 2010 | 13 | Young in Norway | 2 | |
| von Soest et al. (2014)* | 0.38 | Norway | 610 | 653 | SCL-D | 2010 | 14 | Young in Norway | 2 | |
| von Soest et al. (2014)* | 0.52 | Norway | 573 | 695 | SCL-D | 2010 | 15 | Young in Norway | 2 | |
| von Soest et al. (2014)* | 0.45 | Norway | 621 | 612 | SCL-D | 2010 | 16 | Young in Norway | 2 | |
| von Soest et al. (2014)* | 0.41 | Norway | 76 | 714 | SCL-D | 2010 | 17 | Young in Norway | 2 | |
| Walker et al. (2005) | 0.13 | New Zealand | 4266 | 5049 | RADS | 2001 | 12–18 | Youth 2000 | 2 | |
| Wang et al. (2010)* | 0.29 | US | 1164 | 1186 | - | 2006 | 11 | Health Behavior in School-Aged Children (HBSC) | 1 | 2 |
| Wang et al. (2010)* | 0.44 | US | 892 | 951 | - | 2006 | 12 | HBSC | 1 | 2 |
| Wang et al. (2010)* | 0.49 | US | 789 | 997 | - | 2006 | 13 | HBSC | 1 | 2 |
| Wang et al. (2010)* | 0.51 | US | 721 | 742 | - | 2006 | 14 | HBSC | 1 | 2 |
| Wang et al. (2010)* | 0.59 | US | 793 | 804 | - | 2006 | 15 | HBSC | 1 | 2 |
| Wichstrom (1999)* | -0.88 | Norway | 628 | 689 | SCL-D | 1992 | 12 | Young in Norway | 1 | |
| Wichstrom (1999)* | 0.18 | Norway | 628 | 689 | SCL-D | 1992 | 13 | Young in Norway | 1 | |
| Wichstrom (1999)* | 0.44 | Norway | 827 | 802 | SCL-D | 1992 | 14 | Young in Norway | 1 | |
| Wichstrom (1999)* | 0.50 | Norway | 870 | 869 | SCL-D | 1992 | 15 | Young in Norway | 1 | |
| Wichstrom (1999)* | 0.58 | Norway | 919 | 898 | SCL-D | 1992 | 16 | Young in Norway | 1 | |
| Wichstrom (1999)* | 0.54 | Norway | 754 | 725 | SCL-D | 1992 | 17 | Young in Norway | 1 | |
| Wichstrom (1999)* | 0.58 | Norway | 665 | 710 | SCL-D | 1992 | 18 | Young in Norway | 1 | |
| Wichstrom (1999)* | 0.45 | Norway | 271 | 300 | SCL-D | 1992 | 19 | Young in Norway | 1 | |
| Wichstrom (1999)* | 0.59 | Norway | 96 | 161 | SCL-D | 1992 | 20 | Young in Norway | 1 | |
| Yamada & Teerawichitchainan (2015)* | 0.37 | Vietnam | 458 | 598 | CES-D | 2011 | 60–69 | Vietnam Aging Survey- 2011 | 3 | |
| Yamada et al. (2015)* | 0.53 | Vietnam | 280 | 395 | CES-D | 2011 | 70–79 | Vietnam Aging Survey- 2011 | 3 | |
| Yamada et al. (2015)* | 0.39 | Vietnam | 194 | 300 | CES-D | 2011 | 80+ | Vietnam Aging Survey- 2011 | 3 | |
| Zemore et al. (2013)* | 0.13 | US | 2306 | 2599 | CES-D | 2000 | 18+ | National Alcohol Surveys (NAS) | 2 | 3 |
| Zemore et al. (2013)* | 0.13 | US | 514 | 847 | CES-D | 2000 | 18+ | NAS | 3 | 3 |
| Zemore et al. (2013)* | 0.11 | US | 464 | 530 | CES-D | 2000 | 18+ | NAS | 5 | 3 |
| Zemore et al. (2013)* | 0.16 | US | 1903 | 2064 | CES-D | 2005 | 18+ | NAS | 2 | 3 |
| Zemore et al. (2013)* | 0.09 | US | 383 | 671 | CES-D | 2005 | 18+ | NAS | 3 | 3 |
| Zemore et al. (2013)* | 0.09 | US | 784 | 826 | CES-D | 2005 | 18+ | NAS | 5 | 3 |
| Zemore et al. (2013)* | 0.15 | US | 1904 | 2695 | CES-D | 2010 | 18+ | NAS | 2 | 3 |
| Zemore et al. (2013)* | 0.10 | US | 517 | 1078 | CES-D | 2010 | 18+ | NAS | 3 | 3 |
| Zemore et al. (2013)* | 0.09 | US | 517 | 936 | CES-D | 2010 | 18+ | NAS | 5 | 3 |
| Zunzunegui et al. (2007) | 0.52 | Israel | 523 | 550 | CES-D | 1989 | 75–84 | Cross Sectional & Longitudinal Aging Study | 1 |
Note. Sample = sample name (not all samples had a name); Measure = depression symptom measure (the version of each measure- including number of items, language, and response scale- varied for each sample); d = uncorrected effect size; NM = n males; NF = n females; Year = year of data collection; Age = age or age range (in years); E = ethnicity (only applies to U.S. samples): 1 = mixed, 2 = > 85% Caucasian, 3 = > 85% African American, 4 = > 85% Asian American, 5 = >85% Hispanic; F = focus of article: 1 = gender, 2 = depression, 3 = other;
= received additional data from author; BDI = Beck Depression Inventory (Beck et al., 1961, 1996); CDI = Children’s Depression Inventory (Kovacs, 1985); MDI = Major Depression Inventory (Bech et al., 2001); DTS = Depressive Tendencies Scale (Alsaker et al., 1991); HDL-D = Health and Daily Living Form- Depression Scale (Moos et al., 1985); CES-D = Center for Epidemiological Depression Scale (Radloff, 1977); EURO-D (Prince et al., 1999); MHI-D = Mental Health Inventory- Depression Items (Ware & Sherbourne, 1992); RADS = Reynolds Adolescent Depression Scale (Reynolds, 1986); SCL-D = Symptom Checklist-90- Depression items (Derogatis et al., 1973); SMFQ = Short Mood and Feelings Questionnaire (Angold et al., 1995); DASS-D = Depression Anxiety Stress Scales- Depression Subscale (Lovibond & Lovibond, 1995); PHQ-9 = Patient Health Questionnaire- 9 (Kroenke et al., 2001); DEPS = Depression Scale (Salokangas et al., 1995); HADS-D = Hospital Anxiety and Depression Scale- Depression subscale (Zigmond & Snaith, 1983); GDS = Geriatric Depression Scale (Yesavage et al., 1982); ADRS = Adolescent Depression Rating Scale (Revah-Levy et al., 2007); GHQ-D = General Health Questionnaire-Depression items (Symonds et al., 2016).
The 65 articles (59 in peer-reviewed journals, 6 online publications from national database websites) and their corresponding data sets for the meta-analysis on depression diagnoses provided data comprising 149 samples (this number includes different countries from the same international dataset as well as different years of data collection for cross-sectional national datasets), 300 effect sizes (this number includes separate effect sizes for different age groups and ethnicities), and 1,716,195 people (53% female). These studies were published from 1993 to 2016 with data from 1991–2014 collected in 75 different countries.
The 95 articles (92 in peer-reviewed journals, 2 government publications, 1 personal communication) and their corresponding data sets for the meta-analysis on depression symptoms utilized data comprising 180 samples, 413 effect sizes, and 1,922,064 people (52% female). These studies were published from 1991 to 2016 and yielded data from 1978–2014 collected from 53 different countries.
Coding of Studies
Studies were coded for information to compute effect sizes and for moderator variables4. We double coded 30 studies to compute interrater agreement. The following variables were coded: (a) age of the participants (measured on a continuous scale, using the reported mean or the midpoint of the age range), r = .99; (b) country, κ (kappa) = 1.00, was used to identify national economic indicators and national gender equity indicators; (c) for U.S. samples, predominant (≥ 85%) ethnic group of participants (Caucasian, African American, Asian American, Hispanic, Native American, other, mixed, or unreported), κ = 1.00; and (d) year of data collection, r = 1.00.
In any meta-analysis, there is a potential concern that the identified studies have a publication bias, i.e., a bias toward publishing studies that found significant and larger gender differences. If present, this bias could mean that the magnitude of the gender difference is overestimated because studies finding no difference are missing from the sample of studies. As one of several ways to address this potential concern, we coded the focus of the article (gender, depression, other), κ = .84. If the majority of the articles were not focused on gender, we would not be concerned about publication bias in regard to gender. We further tested whether the magnitude of the gender difference in depression varied as a function of the article focus to determine if articles that focused on gender reported larger gender differences than articles focused on depression. Gender was identified as the focus of the article if “gender” or a related term was included in the title. If gender was not identified as the focus, depression was identified as the focus of the article if “depress*” or a related term was included in the title, abstract, or keywords. If neither gender nor depression were the focus, “other” was coded.
The following measurement characteristics were also coded: (1) the type of measure used to assess depression diagnoses (diagnostic interview; e.g., CIDI, DIS) or depression symptoms (self-report measure; e.g., CES-D, BDI), κ = 1.0; (2) the manual used to diagnose depression (DSM-IV or DSM-IV-TR5; DSM-III or DSM-III-R; or ICD-10), κ = 1.0; (3) type of depression diagnosis (depressive episode versus depressive disorder), κ = .87; and (4) the time span for the depression diagnosis (current, 1 month, 6 months, 12 months, lifetime), κ = 1.00. If multiple time spans for the depression diagnosis were reported (e.g., 12-month and lifetime), 12-month was the preferred time span given our interest in developmental trends in gender differences in depression. For the major depression meta-analysis, all articles reported DSM major depression diagnoses or episodes (96%) or the roughly equivalent ICD-10 depressive episode (4%). Diagnoses of dysthymia were not included in this meta-analysis.
Nation-level Economic Indicators
To test the contribution of national wealth and development to gender differences in depression, we used two indicators: a categorical measure of national wealth (low-, middle-, and high-income), and income inequality. The World Bank classification of income categories was based on gross national income (GNI) per capita from 2003: high income ($9,386 or more), middle income ($766–9,385), and low income ($765 or less). Income categories were obtained from the Human Development Report 2005 (United Nations Development Programme, 2005). The GINI index was used as a measure of income inequality in a nation. It indicates the extent to which the income distribution deviates from a perfectly equal distribution across income categories, with gender not taken into account (World Bank, 2004). High scores indicate greater inequality. See Supplemental Table 1 for a list of each country and its associated indicators. For each of the economic and gender equity indicators, data are not available for all nations. Therefore, sample sizes vary in regression analyses, depending on the indicator.
Nation-level Gender Equity Indicators
We selected the following five domain-specific nation-level gender equity indicators as hypothesized moderators: contraceptive prevalence (percentage of women in a nation aged 15–49 using some form of contraception, an indicator of women’s ability to control their reproduction), executive positions (percentage of executive positions held by women, a measure of women’s equality in the workplace), literacy ratio (female: male ratio in percentage of the adult population that is literate, a measure of women’s equality in education), intimate-partner violence against women (lifetime prevalence of physical violence against women by intimate partners) and sexism ideals (higher scores indicate attitudes favoring gender equity in response to the item “When jobs are scarce, men should have more right to a job than women”).
Contraceptive prevalence, executive positions, and literacy indicators for each country were obtained from the Human Development Report 2005 (United Nations Development Programme, 2005). The intimate-partner violence measure came from the United Nations’ 2010 report, The World’s Women, for the years 2000–2006. The sexism ideals measure was obtained from the World Values Survey, Wave 4, 1999–2004 (World Values Survey, 2014). Although they were theoretically interesting, the intimate-partner violence and sexism ideals measures proved unsatisfactory because they were available for only a minority of the effect sizes in analyses. Those two measures are therefore not considered further. See Supplemental Table 1 for a list of each country and its associated indicators.
Effect Size Computation
The odds ratio (Lipsey & Wilson, 2001) was the effect size used for the meta-analysis on major depression diagnoses; Cohen’s d (Cohen, 1988) was the effect size used for the meta-analysis on depression symptoms. All effect sizes were computed using the Campbell Collaboration effect size calculator (Wilson). Data were entered in the calculator by two individuals to ensure accuracy.
Odds ratio
The odds ratio (OR) is an effect size that evaluates whether the odds of a certain outcome (e.g., depression) is the same for two groups (e.g., males and females). For the meta-analysis on gender differences in major depression, the OR measures the ratio of the odds of major depression among females (number of depressed females divided by number of non-depressed females) to the odds of major depression among males (number of depressed males divided by number of non-depressed males). Thus, values greater than 1 indicate that females have greater odds of depression compared to males. The OR is different from a simple ratio of depressed females to depressed males.6 Most studies in psychiatric epidemiology report ORs.
The OR for each independent sample was computed using either a 2 by 2 frequency table or the proportion depressed and total sample size for each gender. Separate effect sizes were computed for separate groups within each study (e.g., different age groups, different U.S. ethnic groups).
In synthesizing OR’s meta-analytically, raw OR effect sizes were transformed using a natural log transformation. The logged ORs for individual samples were weighted by the inverse of the variance, and averaged across all studies (Lipsey & Wilson, 2001). See Table 1 for a list of all raw effect sizes (not log transformed) along with corresponding study information.
Cohen’s d
Cohen’s d (Cohen, 1988) is the effect size for the standardized mean difference between two groups on a continuous variable (e.g., the mean difference between females and males on a continuous measure of levels of depression symptoms). The d for each sample in the depression symptom meta-analysis was computed such that positive values indicated that females reported more symptoms than males (the mean score for females minus the mean score for males, divided by the within-groups standard deviation). Effect sizes of d = 0.20, d = .50, and d = .80 are considered to be small, medium, and large, respectively (Cohen, 1988). Separate effect sizes were computed for separate groups within each sample (e.g., different age groups, different ethnic groups). Raw effect sizes were corrected for bias (i.e., the upward-bias of effect sizes among small samples; Hedges, 1981); however, most correction factors were close to 1.0 given the large sample sizes. Although we corrected from Cohen’s d to Hedges’ g, we continue to refer to the results as d values. Effect size variances were calculated using these unbiased effect sizes. Then unbiased effect sizes for individual samples were weighted by the inverse of the variance and averaged across all studies (Lipsey & Wilson, 2001). See Table 2 for a list of all raw effect sizes (not corrected for bias) along with corresponding study information.
Data-Analytic Plan
Results were analyzed using SPSS/PASW Version 21 with macros provided by Wilson (2006). First, mean weighted effect sizes were computed for OR and d. For ease of interpretation, anti-log values are reported for mean OR. We evaluated the homogeneity statistic (Q) to determine whether the distribution of effect sizes was heterogeneous, and thus required further analysis. If the Q statistics associated with OR and d were significant, results were further analyzed using a mixed-effects model to account for variability between studies (Lipsey & Wilson, 2001). The mixed-effects model assumes that variability among effects sizes beyond subject-level sampling error has both systematic components (accounted for by moderator variables) and random components (i.e., error variance). When the Q statistic is significant, this mixed-effects approach is preferable to random-effects and fixed-effects models, each of which involve untenable assumptions; the random-effects model assumes that all variability among effect sizes (beyond subject-level sampling error) is due to error and therefore not systematic, and the fixed-effects model assumes that all variability in effects sizes is accounted for by moderators. Random-effects analyses also have lower statistical power than mixed-effects models. In mixed-effects models, a random-effects variance component is estimated after accounting for moderator variables. Then the inverse variance weights are recalculated with the random variance component, and the model is refit.
Moderator variables were tested in separate analyses (one moderator as the independent variable) using an analog to analysis of variance for categorical moderator variables and an analog to regression for continuous moderator variables (i.e., weighted ordinary least squares). We used mixed-effects models with estimation via full information maximum likelihood for all moderator analyses (Wilson, 2006). Anti-log values are reported for moderator analyses using OR.
To test developmental effects sensitively, lifetime depression diagnoses and samples with large age ranges (e.g., 18–64) were excluded for analyses with age as a moderator. Furthermore, given the focus on developmental trends, we analyzed age as both a categorical and a continuous variable. The age categories were determined based on theory, existing research, and available data. We created the categories of 13–15 and 16–19 to correspond to findings in the much-cited Hankin et al. paper (1998), so that our results could be compared directly to those findings. After that, we used decades (e.g., 20–29). Below that, we formed a childhood age category that corresponded to the available data, i.e., the ages at which we had data. For age as a continuous variable, we included both linear (mean-centered) and quadratic variables for age in a multiple regression, given the potential for non-linear findings.
All analyses were run with the full data set and then re-run excluding outliers. Following procedures recommended by Tabachnick and Fidell (1996), we identified outliers as effect sizes more than 3.29 standard deviations from the mean logged OR and mean d. The value of 3.29 SD corresponds to p < .001. We report the results using the full data set, and note when results differed if outliers were excluded. Comprehensive Meta-Analysis software, Version 3 (Borenstein, Hedges, Higgins, & Rothstein, 2014) and an online program (https://vevealab.shinyapps.io/WeightFunctionModel/) were used for bias and sensitivity analyses.
Results
Analysis for Possible Bias and File Drawer Effects
We guarded against sample bias, publication bias, and file drawer effects (Rosenthal, 1979) in several ways. First, all datasets were nationally representative, indicating that any bias in sampling is minimized.
Focus of article
Second, we coded the focus of the article to determine if the identified studies were predominantly focused on gender given the computerized database search for depression and gender. Importantly, the majority of effect sizes were from articles that focused on depression (70% for major depression; 56% for depression symptoms), not gender (see Table 3). This indicates that most studies were published on the basis of the work on depression and not on the basis of a gender difference, so publication bias in the direction of gender differences should not be a problem.
Table 3.
Descriptive Statistics for Moderator Variables Included in Major Depression Meta-analysis and Depression Symptom Meta-analysis
| Major Depression | Depression Symptoms | ||
|---|---|---|---|
| Moderators | Frequency (%) or M(SD) | Frequency (%) or M(SD) | |
| Age+ | 44.81 (18.40) Range: 12–85 |
42.69 (22.97) Range: 8–92 |
|
| Nationality | |||
| US/ Canadian | 137 (46%) | 88 (21%) | |
| European | 58 (19%) | 219 (53%) | |
| Asian | 28 (12%) | 61 (15%) | |
| African | 35 (8%) | 0 (0%) | |
| Australian/ New Zealander | 18 (7%) | 9 (2%) | |
| Central/ South American | 12 (4%) | 24 (6%) | |
| Russian | 8 (3%) | 8 (2%) | |
| Middle Eastern | 5 (2%) | 4 (1%) | |
| GDP | |||
| High-income | 223 (74%) | 330 (80%) | |
| Low- to middle- income | 77 (26%) | 83 (20%) | |
| Ethnicity (U.S.) | |||
| Mixed | 79 (89%) | 66 (76%) | |
| African Americans | 4 (4%) | 7 (8%) | |
| European Americans | 2 (2%) | 6 (7%) | |
| Hispanic Americans | 2 (2%) | 8 (9%) | |
| Native Americans | 2 (2%) | 0 (0%) | |
| Asian Americans | 1 (1%) | 0 (0%) | |
| Year of data collection | 2004.53 (5.52) Range: 1991–2014 |
2004.70 (7.25) Range: 1978–2014 |
|
| Data source | |||
| Unpublished data | 167 (56%) | 337 (86%) | |
| Published data | 133 (44%) | 56 (14%) | |
| Focus of article | |||
| Depression | 210 (70%) | 233 (56%) | |
| Other | 62 (21%) | 61 (15%) | |
| Gender | 28 (9%) | 119 (29%) | |
| Type of Assessment | |||
| Diagnostic Interview | Symptom Measure | ||
| WMH-CIDI | 135 (45%) | CES-D | 198 (48%) |
| CIDI (not WMH- or -SF) | 47 (16%) | BDI | 49 (12%) |
| 2002 World Health Survey | 46 (15%) | SCL-D | 36 (9%) |
| CIDI-SF | 31 (10%) | PHQ-9 | 28 (7%) |
| AUDADIS | 12 (4%) | DASS-D | 11 (3%) |
| MINI | 10 (4%) | EURO-D | 11 (3%) |
| DISC-IV | 5 (3%) | HADS-D  | 11 (3%) |
| CIS-R | 4 (1%) | MHI-D | 11 (3%) |
| DIS | 4 (1%) | CDI | 10 (2%) |
| NSA interview | 3 (1%) | GDS | 10 (2%) |
| DAWBA | 2 (1%) | Other | 8 (2%) |
| SADS | 1 (<1%) | RADS | 8 (2%) |
| DEPS | 6 (2%) | ||
| DTS | 5 (1%) | ||
| DMI | 4(1%) | ||
| MDI | 2(1%) | ||
| ADMSS | 1 (<1%) | ||
| ADRS | 1 (<1%) | ||
| GHQ-D | 1 (<1%) | ||
| HDL-D | 1 (<1%) | ||
| HSCL-D | 1 (<1%) | ||
| Manual | |||
| DSM-IV/ DSM- IV-TR | 265 (88%) | ||
| DSM-III/ DSM- III-R | 18 (6%) | ||
| ICD-10 | 17 (6%) | ||
| Type | |||
| Depressive Episode | 215 (72%) | ||
| Major Depressive Disorder | 85 (28%) | ||
| Time span | |||
| 12 months | 263 (88%) | ||
| Lifetime | 23 (8%) | ||
| 6 months | 9 (3%) | ||
| 1 month | 4 (1%) | ||
| Current | 1 (<1%) | ||
Note. MDE = major depressive episode (also includes ICD-10 depressive episode). MDD = major depressive disorder. Descriptive statistics for major depression meta-analysis reflect all 300 effect sizes, except for U.S. ethnicity (90 effect sizes). Descriptive statistics for depression symptom meta-analysis reflect all 413 effect sizes, except for U.S. ethnicity (87 effect sizes).
We further tested whether effect sizes differed between articles that focused on depression rather than on gender. For the major depression meta-analysis, article focus accounted for significant variation in effect sizes (see Table 4). However, in follow-up analyses, effect sizes from articles that focused on gender were not significantly different than effect sizes from articles that focused on depression (QB = 2.22, p = 0.14) or something other than gender or depression (QB = 0.91, p =0.34). For the depression symptom meta-analysis, article focus did not account for effect size variability. Moreover, when excluding outliers, effect sizes for articles that focused on depression and articles that focused on gender were both d = 0.26.
Table 4.
Weighted ANOVAs with each Moderator Predicting Gender Differences in Major Depression (unshaded) and Gender Differences in Depression Symptoms (shaded)
| Categorical Moderators | OR | d | 95% CI | k | Qbetween | Qwithin |
|---|---|---|---|---|---|---|
| Age Group (in years) | 184@ | 122.54** | 231.75* | |||
| 12 | 2.37 | 0.48 | [1.68, 3.37] | 2 | 0.38 | |
| 13–15 | 3.02 | 0.61 | [2.76, 3.30] | 24 | 43.13* | |
| 16–19 | 2.69 | 0.55 | [2.39, 3.03] | 17 | 14.54 | |
| 20–29 | 1.93 | 0.36 | [1.76, 2.12] | 26 | 23.43 | |
| 30–39 | 1.83 | 0.33 | [1.65, 2.03] | 20 | 15.89 | |
| 40–49 | 1.71 | 0.30 | [1.56, 1.87] | 29 | 28.04 | |
| 50–59 | 1.80 | 0.32 | [1.63, 2.00] | 25 | 17.85 | |
| 60–69 | 1.79 | 0.32 | [1.56, 2.06] | 18 | 18.21 | |
| 70+ | 2.02 | 0.39 | [1.75, 2.33] | 23 | 70.28* | |
| Age group (in years) | 324@ | 117.90** | 319.00 | |||
| 8–12 | 1.18 | 0.09 | [0.00, 0.17] | 13 | 17.52 | |
| 13–15 | 1.89 | 0.35 | [0.32, 0.39] | 53 | 51.19 | |
| 16–19 | 2.10 | 0.41 | [0.37, 0.44] | 66 | 84.60* | |
| 20–29 | 1.72 | 0.30 | [0.23, 0.37] | 19 | 9.44 | |
| 30–39 | 1.52 | 0.23 | [0.17, 0.29] | 21 | 6.16 | |
| 40–49 | 1.46 | 0.21 | [0.15, 0.26] | 24 | 8.27 | |
| 50–59 | 1.41 | 0.19 | [0.14, 0.25] | 29 | 24.59 | |
| 60–69 | 1.57 | 0.25 | [0.21, 0.29] | 44 | 66.89* | |
| 70–79 | 1.52 | 0.23 | [0.18, 0.28] | 29 | 29.55 | |
| 80+ | 1.46 | 0.21 | [0.15, 0.26] | 26 | 20.80 | |
| GDP | 300 | 4.13* | 316.25 | |||
| High-income | 2.00 | 0.38 | [1.91, 2.09] | 223 | 238.33 | |
| Low- to middle- income | 1.82 | 0.33 | [1.69, 1.97] | 77 | 77.92 | |
| GDP | 413 | 1.66 | 405.53 | |||
| High-income | 1.60 | 0.26 | [0.25, 0.28] | 330 | 351.71 | |
| Low- to middle- income | 1.69 | 0.29 | [0.26, 0.33] | 83 | 53.82 | |
| Ethnicity (U.S.) | 89 | 2.24 | 88.34 | |||
| Mixed | 2.20 | 0.43 | [2.05, 2.36] | 81 | 85.40 | |
| African Americans | 1.74 | 0.31 | [1.23, 2.46] | 4 | 2.71 | |
| European Americans | 2.23 | 0.44 | [1.45, 3.43] | 2 | 0.04 | |
| Hispanic Americans | 1.95 | 0.37 | [1.24, 3.07] | 2 | 0.18 | |
| Native Americans | 1.86 | 0.34 | [1.05, 3.30] | 2 | 0.02 | |
| Ethnicity (U.S.) | 87 | 5.24 | 85.92 | |||
| Mixed | 1.52 | 0.23 | [0.21, 0.26] | 66 | 75.20 | |
| African Americans | 1.57 | 0.13 | [0.04, 0.22] | 7 | 2.59 | |
| European Americans | 1.39 | 0.18 | [0.09, 0.27] | 6 | 1.69 | |
| Hispanic Americans | 1.49 | 0.22 | [0.13, 0.31] | 8 | 6.44 | |
| Data Source | 300 | 111.54** | 316.34 | |||
| Unpublished data | 1.83 | 0.33 | [1.74, 1.93] | 167 | ||
| Published data | 2.09 | 0.41 | [1.98, 2.20] | 133 | ||
| Data Source | 413 | 1.21 | 405.99 | |||
| Unpublished data | 1.63 | 0.27 | [0.26, 0.29] | 357 | 367.42 | |
| Published data | 1.57 | 0.25 | [0.20, 0.29] | 56 | 38.56 | |
| Focus of article | 300 | 15.31** | 319.19 | |||
| Depression | 1.86 | 0.34 | [1.77, 1.94] | 210 | 219.21 | |
| Other | 2.21 | 0.44 | [2.05, 2.38] | 62 | 91.28* | |
| Gender | 2.04 | 0.39 | [1.80, 2.32] | 28 | 8.69 | |
| Focus of article | 413 | 2.37 | 405.52 | |||
| Depression | 1.60 | 0.26 | [0.24, 0.28] | 233 | 167.47 | |
| Other | 1.69 | 0.29 | [0.24, 0.33] | 61 | 685.28* | |
| Gender | 1.66 | 0.28 | [0.25, 0.31] | 119 | 152.77* | |
| Diagnostic Interview | 300 | 0.85 | 316.59 | |||
| WMH-CIDI | 1.99 | 0.38 | [1.88, 2.11] | 135 | 181.95* | |
| Other | 1.92 | 0.36 | [1.82, 2.02] | 165 | 134.65 | |
| Symptom Measure | 413 | 18.26** | 406.14 | |||
| CES-D | 2.48 | 0.25 | [0.23, 0.28] | 198 | 158.23 | |
| BDI | 1.44 | 0.20 | [0.15, 0.25] | 49 | 23.28 | |
| Other | 1.75 | 0.31 | [0.28, 0.33] | 166 | 224.63 | |
| Manual for Major Depression | 300 | 2.42 | 315.51 | |||
| DSM-IV/ DSM-IV-TR | 1.97 | 0.37 | [1.89, 2.05] | 265 | 282.46 | |
| DSM-III/ DSM- III-R | 1.97 | 0.37 | [1.69, 2.30] | 18 | 4.89 | |
| ICD-10 | 1.73 | 0.30 | [1.47, 2.03] | 17 | 28.16* | |
| Type for Major Depression | 300 | 0.82 | 313.80 | |||
| Depressive Episode | 1.93 | 0.36 | [1.85, 2.02] | 215 | 251.50* | |
| Major Depressive Disorder | 2.01 | 0.38 | [1.87, 2.17] | 85 | 62.30 | |
| Time span for Major Depression | 299 | 2.96 | 313.99 | |||
| 12 months | 1.96 | 0.37 | [1.88, 2.04] | 263 | 298.14+ | |
| Lifetime | 1.98 | 0.38 | [1.72, 2.28] | 23 | 9.78 | |
| 6 months | 2.01 | 0.38 | [1.63, 2.47] | 9 | 5.16 | |
| 1 month | 1.49 | 0.22 | [1.09, 2.04] | 4 | 0.91 |
Note. OR = weighted mean effect size. d = weighted mean effect size. 95% CI = 95% confidence interval for d. k = number of effect sizes for moderator or category in each moderator. Qbetween = Significant values indicate that there is significant variability accounted for by the moderator. Qwithin = Significant values indicate that studies are still heterogeneous after accounting for the moderator variable. MDE = major depressive episode (also includes ICD-10 depressive episode).
p <.10.
p <.05.
p <.001.
= To more sensitively test developmental effects, lifetime depression was excluded for major depression diagnoses and samples with large age ranges (e.g., 18–64) were excluded for both meta-analyses.
Thus, the similarity of the effect sizes for articles focused on depression and gender, combined with the small proportion of gender-focused studies, suggests that publication bias for articles finding gender differences is not a serious concern in these meta-analyses.
Unpublished data
Third, we followed up with authors to retrieve data on gender differences in depression and moderating variables (e.g., age and U.S. ethnicity) when these were not reported sufficiently in the article. For many of the studies, the gender analyses were not reported in the article or were reported in little detail. For the meta-analysis on depression diagnoses, we received data from authors for 24 (37%) of the 65 articles, such that 167 (56%) of the 300 effect sizes were based on obtained rather than published data. For the meta-analysis on depression symptoms, we received data from authors for 71 (75%) of the 95 articles, such that 357 (86%) of the 413 effect sizes were based on obtained data. This protects the data from file drawer effects.
For the major depression meta-analysis, effect sizes from unpublished data (OR = 1.83) were significantly smaller than effect sizes from published data (OR = 2.09). However, the majority of effect sizes included in this meta-analysis were from unpublished data, making potential publication bias less of a concern. For the depression symptom meta-analysis, effect sizes did not differ as a function of publication status.
Funnel plot and test for asymmetry
Fourth, we used funnel plots as a visual tool to detect small-study effects. See Supplemental Tables 2 and 3 for a plot of effect size against precision (the inverse of standard error) for both meta-analyses. It is important to note that the notion of “small-study effects” is in the context of relatively large nationally representative samples. The average sample size was 5720 (minimum = 261) for the major depression meta-analysis and 4654 (minimum = 101) for the symptom meta-analysis. Nonetheless, we used the Begg and Mazumdar (1994) rank correlation test to evaluate asymmetry in the funnel plots. We selected this test given the skewness of the sample size variable and adequate power with the large number of effect sizes in each meta-analysis. For the major depression meta-analysis, Tau = 0.07, p = 0.07. For the depression symptom meta-analysis, Tau = −0.03, p = 0.49. Thus, neither of the tests for skewness was statistically significant, indicating no evidence of bias in the set of effect sizes, for both meta-analyses.
Sensitivity analysis
Finally, we used the Vevea and Hedges Weight-Function Model for Publication Bias (Vevea & Woods, 2005). A recent review on adjusting for publication bias in meta-analysis encouraged the use of sensitivity measures (McShane, Böckenholt, & Hansen, 2016). The likelihood ratio tests (LRT) comparing the unadjusted to adjusted models (using p-value cut points of 0.05, 0.01, and 0.001) for the major depression and depression symptom meta-analyses, respectively, were not statistically significant, p = 0.073 and p = 0.3226. Although the LRT showed a marginal effect for the major depression meta-analysis, the weighted average from the unadjusted model (logged OR = 0.67) and the adjusted model (logged OR = 0.62) were quite similar. The goal of sensitivity analyses is to determine whether the results are robust to various methodological choices that were made in the process of conducting the meta-analysis. The Vevea and Woods test assesses for evidence of publication bias and provides no evidence for it in the sets of effects sizes in these two meta-analyses.
Description of the Samples for each Meta-analysis
See Table 3 for a list of descriptive information about moderator variables and other variables that describe the sample of studies for both meta-analyses. The samples of studies have similarities across the two meta-analyses. They both include mostly high-income countries and cover the lifespan. However, they differ in terms of the distribution of nations and year of data collection. The major depression analysis includes the most effect sizes from the US/Canada (46%), and the depression symptom meta-analysis includes the most effect sizes from Europe (53%). The depression symptom meta-analysis covers data collected from 1978–2014 whereas the major depression meta-analysis only includes data collected from 1991–2014.
The vast majority of effect sizes for the major depression meta-analysis were 12-month major depressive episodes based on the DSM-IV or DSM-IV-TR using a version of the CIDI. For the symptom meta-analysis, most effect sizes were based on the C ES-D measure.
Magnitude of the Gender Difference in Depression
Major depression
The random-effects estimate of the weighted mean effect size for the gender difference in major depression was OR = 1.95, 95% CI [1.88, 2.03]. The diagnosis effect size of OR = 1.95 is equivalent to d = 0.37. The random effects variance component was 0.07. The set of effect sizes using the fixed effects model was significantly heterogeneous, Qt(299) = 1961.63, p <.001. Thus, moderator analyses were appropriate. We identified 7 outlier effect sizes (2% of all effect sizes) that were more than 3.29 standard deviations from the mean logged odds ratio (0.67 ± 0.96). After excluding these outliers, the random-effects estimate of the overall weighted mean effect size changed only slightly, OR = 1.94, 95% CI [1.87, 2.01].
For the benefit of U.S. policy makers, we repeated all analyses using just U.S. samples. These analyses can be found in the supplemental tables.
Depression symptoms
The random-effects estimate of the weighted mean effect size for the gender difference in depression symptoms was d = 0.27, 95% CI [0.26, 0.29]. The symptom effect size of d = 0.27 is equivalent to logged OR = 0.49 and OR = 1.64. The random effects variance component was 0.02. The set of effect sizes using the fixed effects model was significantly heterogeneous, Qt(412) = 9542.50, p <.001. Thus, moderator analyses were appropriate. We identified 3 outlier effect sizes (1% of all effect sizes) that were more than 3.29 standard deviations from the mean (0.27 ± 0.47). After excluding these outliers, the random-effects estimate of the overall weighted mean effect size did not change, d = 0.27, 95% CI [0.25, 0.28].
Developmental Trends
As both a categorical variable and continuous variable, age predicted variability in effect size for diagnoses and symptoms. The patterns were highly similar in both meta-analyses. See Figure 2 (for diagnoses) and Figure 3 (for symptoms) for a graphical representation of age trends.
Figure 2. Effect Size for Gender Difference in Major Depression Across Age.
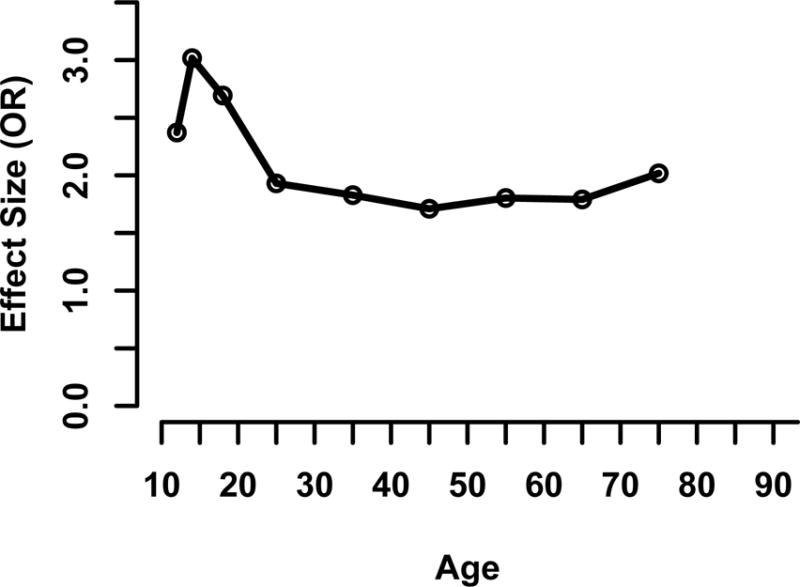
Note. Data points represent effect sizes reported in Table 4 for the following ages: 12, 13–15, 16–19, 20–29, 30–39, 40–49, 50–59, 60–69, and 70+.
Figure 3. Effect Size for Gender Difference in Depression Symptoms Across Age.
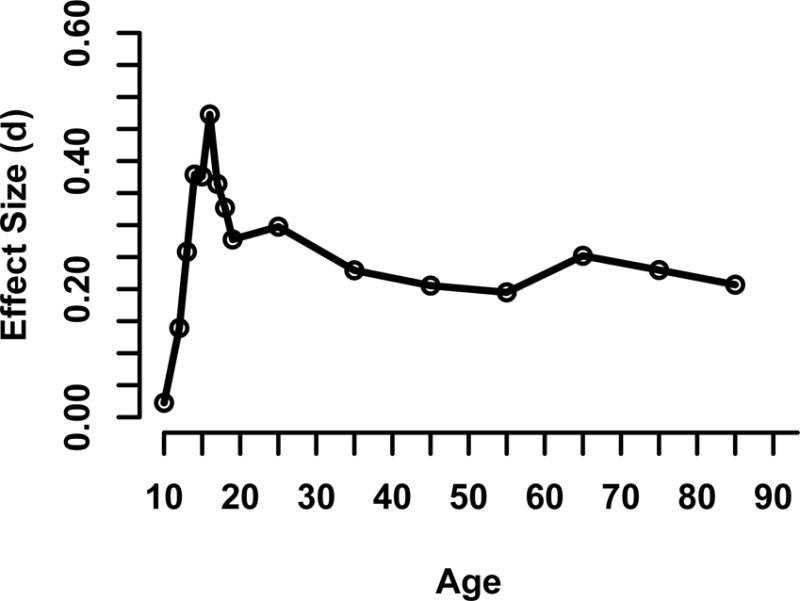
Note. Data points represent effect sizes for the following ages: 8–11 (d = 0.02), 12 (d = 0.14), 13 (d = 0.26), 14 (d = 0.38), 15 (d = 0.38), 16 (d = 0.47), 17 (d = 0.36), 18 (d = 0.33), 19 (d = 0.28), 20–29 (d = 0.30), 30–39 (d = 0.23), 40–49 (d = 0.21), 50–59 (d = 0.19), 60–69 (d = 0.25), 70–79 (d = 0.23), and 80+ (d = 0.21).
Major depression
Effect sizes ranged from OR = 1.71 to OR = 3.02, with ORs >2.0 during adolescence and ORs between 1.71 and 2.02 in adulthood. Note that the youngest age group available for these analyses was 12 years old, making it impossible to observe the emergence of the gender difference from childhood to adolescence. When outliers were excluded, the age 13–15 OR decreased from 3.02 to 2.92 and the age 70+ OR increased from 2.02 to 2.20.
Follow-up testing with pairs of consecutive age groups indicated that the ORs for ages 12 (2.37), 13–15 (3.02), and 16–19 (2.69) were not statistically different (QB= 1.19, QB= 1.98, ps > 0.15, respectively). However, significance tests for moderators in meta-analysis tend to have low statistical power (Hedges & Pigott, 2004), which would especially be the case for age 12 when only 2 effect sizes were available. The OR at ages 16–19 (2.69) was significantly larger than the OR for ages 20–29 (1.93), QB = 43.19, p < .001, indicating a significant decrease in the gender difference from adolescence to the 20s. Differences between 20–29 and later ages were not significant.
Depression symptoms
Effect sizes ranged from d = 0.09 to d = 0.41, peaking at ages 16–19, declining in the 20s, and staying relatively stable at roughly d = 0.20 after that. Removal of outliers did not change the estimates of effect sizes. In Figure 3 we present weighted effect sizes for each year in adolescence to describe in more detail the development of the gender difference in depression in adolescence (with each age having at least 5 effect sizes).
Follow-up testing with pairs of consecutive age groups indicated that the effect sizes for ages 8–12 (0.09), 13–15 (0.35), and 16–19 (0.41) were statistically different (QB = 23.01 and QB = 8.06, ps< .01, respectively), such that the effect size for each consecutively age group was significantly larger than the previous age group. The effect size for ages 20–29 (0.30) was significantly smaller than the effect size for ages 16–19, QB = 7.26, p < .01. Differences between 20–29 and later ages were not significant.
Nation-level economic indicators
See Table 4 for income category results. See Table 5 for income inequality results.
Table 5.
Separate Weighted OLS Regressions with each Moderator predicting Gender Differences in Major Depression (unshaded) and Gender Differences in Depression Symptoms (shaded)
| Continuous Moderators | β | Exp(β) | k | Qmodel | Qresidual | R2 |
|---|---|---|---|---|---|---|
| Year of data collection | 0.14* | 1.01 | 300 | 6.25* | 316.48 | 0.02 |
| Year of data collection | 0.00 | 413 | 0.66 | 405.64 | 0.00 | |
| Age@ | 184 | 82.47** | 221.35* | 0.27 | ||
| Linear | −0.45** | 0.99 | ||||
| Quadratic | 0.35** | 1.00 | ||||
| Age@ | 324 | 40.06** | 319.83 | 0.11 | ||
| Linear | −0.37** | |||||
| Quadratic | 0.12* | |||||
| Nation-level economic indicators | ||||||
| Income inequality | 0.09 | 1.01 | 234 | 2.19 | 252.70 | 0.01 |
| Nation-level economic indicators | ||||||
| Income inequality | −0.11* | 316 | 3.73* | 308.77 | 0.01 | |
| Nation-level gender equity indicators | ||||||
| Contraceptive prevalence | 0.22** | 1.01 | 294 | 16.14** | 308.79 | 0.05 |
| Executive positions | 0.10 | 1.00 | 256 | 2.65 | 271.35 | 0.01 |
| Literacy ratio | 0.18** | 1.84 | 297 | 11.08** | 313.62 | 0.03 |
| Nation-level gender equity indicators | ||||||
| Contraceptive prevalence | 0.03 | 369 | 0.36 | 362.30 | 0.00 | |
| Executive positions | −0.06 | 376 | 1.24 | 369.63 | 0.00 | |
| Literacy ratio | −0.03 | 404 | 0.28 | 397.68 | 0.00 |
Note. Each moderator was run in a separate regression, except for the age variables which were run in a multiple regression. β = Beta. Negative values indicate that there are larger reported gender differences at lower levels of the moderator and smaller reported gender differences at higher levels of the moderator. k = number of effect sizes for each age. 95% CI = 95% confidence interval for β. Exp(β) = Exponent of Beta. Significance for Exp(β) is not indicated because it is the same as β. Qmodel = Significant values indicate that there is significant variability accounted for by the moderator. Qresidual = Significant values indicate that studies are still heterogeneous after accounting for the moderator variable. R2 = Amount of variance accounted for by the moderator(s).
p <.10.
p <.05.
p <.001.
= For age as a moderator, lifetime depression was excluded and samples with large age ranges (e.g., 18–64) were excluded to more sensitively test developmental effects.
Major depression
Income category (high versus low to middle) was a significant predictor of effect size. Larger gender differences in depression were found in wealthier countries (OR = 2.00) compared to low- to middle- income countries (OR = 1.82). Income inequality was not a significant predictor.
Depression symptoms
Income category (high versus low to middle) was not a significant predictor of effect size. However, when outliers were removed, the effect became marginally significant (QB = 3.09, p = 0.08) with smaller gender differences in high-income nations (d = 0.26) compared to low- to middle- income nations (d = 0.29). Income inequality was a significant predictor of effect size, such that larger gender differences were reported in nations with low levels of income inequality. Yet, when outliers were removed, this effect become non-significant (p = 0.13). Neither of these results are reliable given the sensitivity when outliers were excluded.
Nation-level gender equity indicators
See Table 5 for nation-level gender equity results.
Major depression
Contraceptive prevalence and literacy ratio both predicted variability in effect size. As the percentage of women using some form of contraception increased (range = 8 – 84%), the effect size also increased. For literacy, the effect size increased as the ratio of the female: male adult literate population increased. Importantly, there was not a range restriction for the literacy variable (ratios ranged from .31 to 1.07), which can have substantial negative skew (Else-Quest & Grabe, 2012). When outliers were excluded, executive positions had a marginal effect on effect size, such that as the percentage of executive positions held by women increased (range = 2 – 58%), the effect size increased. Thus, for all three indicators, greater gender equity was associated with a larger gender difference in major depression.
Depression symptoms
Contraceptive prevalence, executive positions, and the literacy ratio did not predict variation in effect size. These conclusions, however, should be qualified because the variability for all three indicators was limited.
Additional Moderators
U.S. ethnicity
In both meta-analyses, U.S. ethnicity did not account for significant variation in effect size (see Table 4).
Trends over time
As shown in Table 5, for the major depression meta-analysis, year of data collection was a significant predictor of effect size, such that gender differences were larger more recently. To better understand this pattern, we created a categorical variable for year of data collection and obtained the following effect size estimates: 1991–1996= 1.84, k = 22; 1997–2002= 1.88, k = 134; 2003–2008= 1.91, k = 59; 2009–2014 = 2.17, k = 85. Thus, although the range of OR = 1.84 to 2.17 is not great, the positive relationship is clear. For the depression symptom meta-analysis, year of data collection did not predict variation in effect size.
Type of assessment
As shown in Table 4, diagnostic interview (WMH-CIDI v. Other) did not account for significant variation in effect sizes in the major depression meta-analysis. Symptom measure significantly predicted variation in effect size. In follow-up tests, all pair-wise comparisons were significantly different from each other, such that the smallest effect size was for the BDI (d = 0.20) and the largest effect size was for scales other than the BDI and CES-D (d = 0.31).
Other major depression moderators
As shown in Table 4, manual for major depression (e.g., DSM-IV, ICD-10), type of depression (episode versus disorder) and depression time span (1 month, 6 months, 12 months, and lifetime) did not predict effect size variation. However, when outliers were excluded, manual for major depression predicted significant variation in effect size, QB = 7.26, p = .013. Follow up analyses, excluding outliers, indicated that diagnoses using the ICD were significantly smaller than both diagnoses using DSM-IV/DSM-IV-TR (QB = 6.86, p < .01) and DSM-III/ DSM- III-R TR (QB = 9.60, p < .01). However, the difference between OR = 1.73 for ICD and OR = 1.97 for both DSMs is not a large difference.
Discussion
The current meta-analyses advance research by synthesizing data from representative samples of more than 1.7 million women and men each, with three main goals: (1) to determine the magnitude of gender differences in diagnoses of major depression and in levels of depression symptoms; (2) to elucidate developmental trends in the magnitude of the gender difference, with the goal of identifying the age at which the gender difference in depression emerges in adolescence and whether the gender difference remains the same across adulthood; and (3) to identify other moderators of these gender differences, focusing especially on nation-level indicators of gender equity and national wealth. In the sections that follow, we highlight and discuss the findings related to each goal.
Magnitude of the Gender Difference in Depression
Overall, the odds ratio was 1.95 for gender differences in diagnoses of major depression; this is the first time that this odds ratio has been estimated meta-analytically and across such a large sample. For gender differences in depression symptoms, we found d = 0.27; this is the first meta-analytic estimate of gender differences in symptoms based on samples across the lifespan.
Analyses of moderating variables revealed variations in the magnitude of gender differences in depression, not the direction of the gender difference. That is, among different subgroups, all odds ratios for diagnoses were > 1.0, and all effect sizes for symptoms were positive. This emphasizes the consistency with which females have higher levels major depression and depression symptoms than males.
How do we interpret the magnitude of the gender difference? An OR of 1.95 is a medium, not a large, effect size, yet it is still a health disparity. Oversimplified thinking about the odds ratio for gender differences in major depression diagnoses can lead to beliefs that many women are depressed and few men are. This is simply not an accurate inference with an OR of 1.95. For example, in a nation where 10% of females have major depression, this means that, 5.4% of males also have major depression.
One possible negative consequence of emphasizing the preponderance of women with depression is that depression becomes a female-stereotyped disorder. Such a stereotype can be harmful to both women and men. The stereotype might lead to over-diagnosis of depression in women, and, potentially, overmedication. For men, the stereotype may mean that their depression is overlooked. It is important that clinicians do not overlook depression among men, particularly because gender biases in diagnosis have been documented (Hartung & Widiger, 1998). Men may be less likely to develop depression than women; however, this does not mean that depressed men are not distressed and impaired.
Comparison of the Diagnosis and Symptom Findings
Expressed in the Cohen’s d metric, the two effect sizes are similar: d = 0.37 for major depression and d = 0.27 for depression symptoms. Ideally, the same samples would be included in both meta-analyses in order to perfectly compare these effect sizes; however, across a wide variety of nations, measures, and ages, the magnitude of the gender difference for depression symptoms and diagnoses was very comparable.
We would not expect findings across the two meta-analyses to be identical given key differences between measures of depression symptoms and diagnoses of major depression. For example, the typical assessment of symptoms often represents a short period of time, such as a week, whereas diagnoses involve aggregation over longer periods, often a year (Haeffel et al., 2003). Thus, most individuals who are currently experiencing a major depressive episode will, indeed, score high on a measure of depression symptoms. However, an individual who scores in the moderate-to-low range on a measure of current depression symptoms may have experienced a major depressive episode earlier that year. Despite this difference in amount of time captured by each assessment, the magnitude of the effect for both diagnoses and symptoms was similar.
In the moderator analyses, developmental trends were also highly consistent across both meta-analyses (see Table 6 for a summary of comparisons between the symptom and diagnostic findings). However, some findings did not replicate across meta-analyses (e.g., nation-level indicators, trends over time), which may be influenced by the different set of nations and studies included in the two meta-analyses. Each of these moderator findings is discussed in the sections that follow.
Table 6.
Comparison of Key Findings of Diagnosis Meta-analysis and Symptom Meta-analysis
| Major Depression | Depression Symptoms | |
|---|---|---|
| Overall effect size for gender differences | OR = 1.95 | d = 0.27 |
| Age trends | Significant quadratic trend. OR peaked at ages 13–15, declined into the 20s, and stayed stable after that. |
Significant quadratic trend. No gender difference at ages 8–11. d peaked at age 16, declined into the 30s, and stayed stable after that. |
| Nation-level economic indicators | ||
| High-income v. low- to middle-income |
Larger OR in wealthier nations | n.s. (significant with outliers excluded, smaller OR in wealthier nations) |
| Income inequality | n.s. | Smaller d in nations with greater income inequality (n.s. with outliers excluded) |
| Nation-level gender-equity indicators | ||
| Contraceptive prevalence | Larger OR with greater contraception | n.s. |
| Executive positions | n.s. (significant with outliers excluded, larger OR with more executive positions) | n.s. |
| Literacy ratio | Larger OR with greater female: male literacy |
n.s. |
| Ethnicity, U.S. | n.s. | n.s. |
Note. n.s. = not significant.
The Developmental Pattern of Gender Differences in Depression
Age was the strongest predictor of effect size, compared with all other moderator variables. For both meta-analyses, the effect size peaked in adolescence but then declined and remained stable in adulthood, a finding that has not been identified previously. The consistency of the findings across the two meta-analyses indicates that the findings are robust.
Adolescence
One of the goals of these meta-analyses was to ascertain the time course of the emerging gender difference in depression. In the major depression meta-analysis, we could not examine the emergence of the gender difference given that the youngest age in the studies was 12, when the OR was already 2.37. These results differ from those of Hankin and colleagues (1998), who found that that the gender gap in major depression emerged between ages 13 and 15 and then widened between ages 15 and 18. The odds ratio for the 13–15 age group in our meta-analysis was already 3.02 and declined, not widened, to OR = 2.69 for ages 16–19.
In the symptom meta-analysis, the gender difference emerged in adolescence with a trivial gender difference for ages 8–11 (see Figure 3) and then a steep increase, reaching a peak in the gender difference at age 16. The gender difference in depression symptoms emerged somewhat earlier in adolescence in our meta-analysis (d = .02 for ages 8–11, d = .14 for age 12, d = .26 for age 13, d = .38 for age 14) compared to the Twenge and Nolen-Hoeksema (2002) meta-analysis of CDI data (d = −.06 for age 12, d = .08 for age 13, d = .22 for age 14). The gender difference in adolescence in our meta-analysis was also larger (largest adolescent d = .47 for age 16) compared to the Twenge and Nolen-Hoeksema meta-analysis (largest adolescent d = .22 for ages 14 and 15). The difference in findings may be due to the greater recency of many of our studies, the greater number of nations, or the inclusion of multiple measures of depression symptoms.
Taken together, our results provide powerful evidence that the gender difference in depression emerges earlier than previously thought (by at least age 12 for diagnoses, at age 12 for symptoms), which has important implications for the timing of preventive interventions.
Adulthood
In addition to clarifying the time course of the emerging gender difference in depression in adolescence, these meta-analyses also shed light on patterns of gender differences in adulthood, an area that has been largely neglected. In both meta-analyses, the gender difference declined in early adulthood and then remained relatively stable, hovering between OR = 1.71 – 2.02 and d = 0.19 – 0.30. This pattern is a new finding and should be robust because it is based on large-scale meta-analyses and was consistent across both diagnosis and symptom measures. This finding has major implications for theories of gender differences in depression, as discussed in Theoretical Implications below.
Future empirical directions
Future research should explore how absolute levels of depression diagnoses and symptoms among males and females contribute to this pattern of a peak gender difference in adolescence, followed by a subsequent decrease and leveling off. Do males have lower depression symptoms and diagnoses in adolescence that then increase in their 20s, contributing to the observed decrease in the gender difference from adolescence to adulthood? Or do females’ depression symptoms and diagnoses decrease in their 20s? Alternatively, it may be that a combination of both patterns occurs. Understanding these patterns will be important for theories of the etiology of depression and for informing prevention work. One latent growth curve analysis indicated that girls’ depression symptoms accelerated early in adolescence and then leveled off, whereas boys’ symptom levels accelerated in late adolescence (Salk, Petersen, Abramson, & Hyde, 2016), consistent with the first possibility above.
Theoretical implications
As noted earlier, theories guided by developmental psychopathology have focused on explaining the emergence of the gender difference in adolescence (summarized by Hyde et al., 2008b), but did not attend to development across adulthood. The strongest theory will take development into account, not only adolescent development, but also adult development. Future theoretical work will need to account not only for the peak in the magnitude of the gender difference in adolescence, but also for (a) the decline into early adulthood and (b) stability across adulthood. Here we provide examples of exciting directions in which such theorizing might go, for three factors hypothesized to be important in the development of depression: temperament, cognitive vulnerability-stress interactions, and puberty.
According to one theoretical account, temperament, present from infancy and early childhood, predicts later depression (summarized by Hyde et al., 2008b). In particular, individuals who are high in negative affectivity and low on positive affectivity are vulnerable to later depression. Given no gender difference in negative affectivity in infancy and childhood (Else-Quest et al., 2006), for temperament to account for the emergence of the gender difference in depression in adolescence requires an interaction between vulnerable temperament and some other factor, such as stress, with stress increasing dramatically in adolescence and increasing more for females than males. How, then, would such a theory account for the decline in the gender difference in the 20s and beyond? It might posit a narrowing of the gender gap in stress beginning in early adulthood. Empirical studies of developmental trends in gender differences in stress in adulthood are lacking and would be a fruitful avenue for future research.
Another theoretical account rests on cognitive vulnerability-stress models of depression, which have been well supported in samples of college students and adults (summarized by Hyde et al., 2008b). Research suggests that negative cognitive style may not emerge as a stable trait until ages 9.5 to 12.5, and the cognitive vulnerability-stress interaction does not become a reliable predictor of depression until ages 13.5 to 14.5, i.e., in early adolescence (Cole et al., 2008). According to this model, the gender difference in depression in adolescence may be accounted for by (a) higher levels of negative cognitive style in girls than boys beginning in early adolescence; (b) higher levels of stress for girls than boys beginning in early adolescence; or (c) both. How would this theoretical framework account for the narrowing of the gender gap in depression in adulthood? One possibility is that the gender gap in negative cognitive style narrows in the 20s. The other is that the gender gap in stress narrows in early adulthood. Again, strong empirical studies of these possibilities are lacking.
Another set of theories emphasizes biological factors in explaining the gender difference in depression (summarized by Hyde et al., 2008b). Here we focus on puberty and the role of pubertal timing, which have been invoked especially to explain why the gender difference in depression appears in early adolescence. Importantly, our meta-analytic findings confirm that the gender difference in depression symptoms emerges around puberty, supporting continued theorizing about the role of puberty. According to one theoretical account, early puberty is disadvantageous for girls but not boys, for outcomes such as depression (Ge, Conger, & Elder, 2001). Thus the gender difference in depression is created at least in part by girls who go through puberty early, because of any of several processes, such as early-puberty girls encountering more peer sexual harassment than boys and on-time girls (Lindberg, Grabe, & Hyde, 2007). The narrowing of the gender gap in depression in adulthood, in the early puberty account, might result from a diminution of the effects of early puberty over time (Copeland et al., 2010), especially 10 or more years later. Again, empirical data on this point are lacking, but the developmental patterns identified by our meta-analysis suggest new directions for both theory and research.
Theories in developmental psychopathology as well as sociology will also be advanced by considering why the gender difference remains relatively stable in adulthood. The following are some possible directions. First, today, at least in the U.S. and many other Western nations, adult women’s and men’s work and family roles are much more equalized than before. For example, in the 21st century women constitute 47% of the U.S. labor force, compared to 30% in 1950 (Costello et al., 2003). Thus, employment is much more of a constant factor in most adult women’s lives, just as it has been in men’s. This may serve to level out stressors and buffers to stress across adulthood. Second, major life transitions that formerly occurred at standard ages and could be major sources of stress, no longer occur at such regular ages. Life course sociologists have called this a “de-standardization of the life course” (Bruckner & Mayer, 2005) or “disorder in the life course” (Rindfuss, Swicegood, & Rosenfeld, 1987). Today, the ages of major events such as marriage, childbirth, and divorce do not occur at the same time for all or most individuals. The result is that stressors attached to these transitions are spread out more evenly across adulthood, leading to more even rates of depression across age for both women and men, and a stable gender gap. A third possibility results from the observation that depression is a recurrent disorder (e.g., Lewinsohn, Rohde, Seeley, Klein, & Gotlib, 2000). As such, it may be that most first cases of depression occur in adolescence, and then recur at variable times in adulthood, as a result of the uneven timing of major stressors. Again, prevalence would remain stable across adulthood for both women and men, leading to a stable gender gap, created by the original gender gap in adolescence.
Cross-national Variations
For major depression diagnoses, variability in the gender difference in depression was linked to measures of national wealth and gender equity.
Several caveats are in order before interpreting the cross-national findings. First, a different set of nations was represented in the symptom meta-analysis compared with the diagnosis meta-analysis. Second, gender equity measures were missing for some nations; thus, the analyses did not capture patterns among all nations included. Third, depression may manifest differently in different cultures (Tsai & Chentsova-Dutton, 2002). The depression measures used in the current meta-analyses used standard diagnostic interviews and symptom questionnaires that are based on Western conceptualizations of depression, as codified in the DSM and the ICD. In some cases, phrases were changed, such that the terms used to describe specific symptoms were customized to the local settings (Harkness et al., 2008). However, cultural adaptations that changed diagnostic criteria were not made and, thus, measures may fail to capture some aspects of depression that appear in other cultures (e.g., Beals et al., 2005).
Economic indicators
Following from sociological theories, we examined the relationship between gender differences in depression and a nation’s wealth and income inequality. There was a marginal difference between high-income nations (d = 0.26) and other nations (low- to middle-income; d = 0.29) in the magnitude of the gender difference for symptom measures. For diagnoses, the OR was significantly higher in high-income nations (2.00) than in other nations (1.82). However, the difference between these odds ratios is small, and the 95% confidence intervals overlap, suggesting that this difference is not a major effect. This absence of any substantial effect for nation-level wealth is consistent with other research (Bromet et al., 2011) indicating that economic development is not a major factor in cross-national variations in the magnitude of gender differences in depression.
Because of the feminization of poverty, we expected to observe large gender differences in depression in nations with more income inequality. However, there was no relation to the gender effect size for diagnoses; it was negatively related for symptom measures but lost significance when outliers were excluded. Therefore, we cannot reach confident conclusions about the relationship between income inequality and the magnitude of the gender difference in depression. The findings reported here indicate that there is probably little or no relationship.
Cross-national variations: Gender equity
Guided by sociological and social-structural theory, we examined the relationship between gender equity and the gender difference in depression. In the major depression meta-analysis, gender differences in depression diagnoses were larger in nations where women had more control over their reproduction, held more executive positions, and were more similar to men in literacy rates. That is, perhaps counterintuitively, gender differences were larger in nations with more gender equity, a finding that was consistent across three indicators. On the face of it, greater contraceptive prevalence should indicate women’s greater control over reproduction and a lower rate of unwanted pregnancies, which are a risk factor for depression (e.g., Mercier, Garrett, Thorp, & Siega-Riz, 2013). Yet, as noted in the introduction, some primary studies have found similar patterns to ours regarding gender differences and gender equity, for outcomes such as self-construals (Guimond et al., 2007) and emotion (Fischer, Rodriguez Mosquera, van Vianen, & Manstead, 2004).
To explain why larger psychological gender differences are sometimes found in nations with greater gender equity, we must look at the pattern according to the type of outcome measure. For objective measures such as mathematics performance, or for ratings of others such as mate preferences, the gender gap is smaller in more equitable nations (e.g., Else-Quest et al., 2010; Zentner & Mitura, 2012). It is in the domain of subjective self-ratings that gender differences are larger in more equitable nations (Wood & Eagly, 2012). Such judgments about the self require participants to construct estimates about the self. Guimond and colleagues (2007) proposed that gender differences in self-construals are larger in contexts in which individuals make intergroup social comparisons, e.g., when they compare themselves to an out-group such as the other gender. Gender differences are smaller when individuals’ social comparisons are made intragroup, e.g., comparing themselves to other members of their own gender. For example, girls may come to see themselves as high in depression if they compare themselves to boys instead of girls. It is precisely in higher gender-equity nations, where males and females interact more (e.g., girls are more literate because they have more equal access to schooling with boys), that intergroup comparisons are likelier, leading to larger gender differences. In low-gender-equity nations, intergroup interactions are often greatly restricted, and gender differences on a variable such as depression are smaller due to mostly intragroup comparisons.
These findings of larger gender differences in nations with greater gender equity did not replicate with the meta-analysis of depression symptoms, suggesting that caution is needed in interpreting the findings for diagnoses. It will be important for future research to examine the relationship between gender equity and the gender difference in depression symptoms among a set of nations that has greater variability in gender equity.
We set out to test two other gender equity indicators – interpersonal violence against women and sexism beliefs – for their relationship to gender differences in depression across nations. We had to abandon these analyses, though, because values were available for only a minority of nations. Both variables are theoretically important, and future research is needed to improve them and make them useful in analyses such as the ones reported here.
Additional Factors Influencing the Gender Difference in Depression
Ethnicity in the U.S
Guided by intersectionality theory, we examined whether effect sizes for gender differences in depression varied across U.S. ethnic groups. In both the diagnosis and symptom meta-analyses, differences among ethnic groups were not significant. Notably, gender differences were smallest for African Americans in both meta-analyses. These analyses, however, were based on small numbers of studies. Therefore, power to detect ethnic-group differences was limited. Much more work is needed on the intersection of gender and ethnicity for depression in the U.S. as well as in other nations.
Trends over time
We sought to determine whether the gender difference in depression has been widening or narrowing over time. The symptom meta-analysis found no significant trend over time and the diagnosis meta-analysis found a positive trend, meaning that gender differences are growing larger. However, this effect was small, accounting for only 2% of the variance. Specifically, the OR increased from 1.84 in 1991–1996 to 2.17 in 2009–2014. It should be noted that the diagnosis meta-analysis did not cover the 1970s and 1980s or earlier decades, because researchers were not yet conducting studies based on nationally representative samples. The gender difference in depression should be monitored for possible changes going forward.
Implications for Policy
These meta-analytic findings can inform global health policy. Given that depression is a global health priority (World Health Organization, 2016), it is imperative to understand disparities in depression and which subgroups are most in need of services. These results suggest that women are at significantly greater risk of depression diagnoses and symptoms compared to men worldwide, and that adolescent girls are at the greatest risk. Universal screening in primary care settings is imperative (O’Connor, Whitlock, Beil, & Gaynes, 2009), with a strong emphasis on screening adolescents. The emphasis on adolescents is particularly important because depression is a recurring disorder, so an episode in adolescence can predispose the individual to later episodes (e.g., Lewinsohn, Rohde, Seeley, Klein, & Gotlib, 2000). Research to identify preventive interventions is even more important (Muñoz et al., 2010). What the current meta-analyses cannot tell us is whether these interventions need to be tailored by gender. However, the magnitude of these gender findings is critically important. If global health efforts only targeted women, they would be missing a substantial proportion of depressed individuals, men.
An important clarification in regard to policy implications is that the findings of the current studies yield information only on the gender gap in depression, not on prevalence levels for either gender. For example, assuming equal numbers of males and females, an OR = 2.0 can result from a 9.05% prevalence in females and a 4.85% prevalence in males, or from an 18% prevalence in females and a 10.1% prevalence in males. Policy makers should monitor not only gender disparities, but also prevalence rates.
Strengths and Limitations
By synthesizing nationally representative studies with data from over 1.7 million participants spanning the globe in each of the two meta-analyses, we have provided a comprehensive quantitative review of data on gender differences in major depression diagnoses and depression symptoms across the lifespan. The findings represent especially strong scientific evidence because they are not based on small community or convenience samples and are instead based on representative samples with strong measurement. We also made extensive efforts to obtain data for as many national data sets as possible by conducting additional computerized searches and contacting authors. Overall, 76% of the effect sizes for the symptom meta-analysis and 56% of the effect sizes for the diagnosis meta-analysis were based on data supplied by researchers, and not published in articles, reducing concerns about publication bias.
Despite these strengths, several limitations should be acknowledged. First, we did not have sufficient data to examine gender differences in major depression for children younger than age 12 (and we had only 2 samples for age 12), even though the minimum age criterion was 7. Research is needed on gender differences in major depression for children ages 7 through 12, based on nationally representative samples. The current study also highlights the need for more nationally representative data on gender differences in major depression in developing countries. The results reported here are weighted toward European and North American samples because so much more research has been conducted in those regions.
Second, focusing on large, nationally representative datasets meant that the diagnostic interviews for major depression were conducted not by skilled clinicians, but instead by trained lay interviewers, as is standard practice in these large-scale, epidemiological studies. However, evidence indicates high reliability between clinicians and lay interviewers. For example, in one methodological study, participants were given diagnostic interviews separately by a clinician and a highly trained non-clinician (Wittchen, Robins, Cottler, Sartorius, Burke, & Regier, 1991). Results indicated high agreement between the two; for major depressive disorder, kappa = 0.97, with 99.7% agreement between the two sources (see also Brugha, Nienhuis, Bagchi, Smith, & Meltzer, 1999).
Third, both diagnostic measures and symptom questionnaire measures rely on self-reports from participants. If there are gender differences in willingness to disclose symptoms, then the resulting data may be biased. One early review concluded that the gender difference in depression is a real difference and not a measurement artifact (Weissman & Klerman, 1977). However, this issue deserves continued attention.
Fourth, our database search included only articles in English. We believe that this did not lead to the omission of nations in which English is not the predominant language for two reasons. The two meta-analyses included data from more than 90 nations. Thus, we achieved the goal of including data from a wide array of nations from all regions of the world. Moreover, mounting a study based on a nationally representative sample is a major, costly undertaking that should almost certainly result in multiple publications, at least one of them in English, so we should have detected such studies.
Conclusions
In two separate meta-analyses including nationally representative samples with over 1.7 million people each, we found evidence for a 1.95 odds ratio for gender differences in major depression and a Cohen’s d of 0.27 for gender differences in depression symptoms. Our results provide powerful evidence that the gender difference in major depression diagnoses and depression symptoms peaks in adolescence, with the gender gap in diagnoses emerging earlier than previously thought (OR = 2.37 at age 12). The gender gap then narrows and remains stable in adulthood, a finding that has not been identified previously and has important implications for both theory and preventive interventions. Larger gender differences in major depression were found in nations with greater gender equity and in more recent studies. The gender difference in depression represents a major health disparity, especially in adolescence, yet the magnitude of the difference indicates that depression in males should not be overlooked.
Supplementary Material
Acknowledgments
This material is based upon work supported by the following: National Science Foundation Graduate (DGE- 071823; DRL 1138114); National Institute of Mental Health (T32 MH018269-30); the Graduate School and the Office of the Vice Chancellor for Research and Graduate Education at the University of Wisconsin-Madison with funding from the Wisconsin Alumni Research Foundation. The content is solely the responsibility of the authors, and any opinions, findings, and conclusions or recommendations expressed in this material are those of the authors and do not necessarily reflect the views of the NSF or NIMH. We thank the following: Rebecca Emery, Larry Hedges, Marsha Marcus, and Nicole Else-Quest for their ongoing and invaluable advice; Emily Clarke, Diane Hsieh, Cecelia Olin, and Caitlin Ziegler for help with various aspects of the meta-analyses. We also thank all of the authors who provided us with data to be included in these meta-analyses.
Footnotes
Major depressive episode (MDE) and major depressive disorder (MDD) are distinct. MDD requires the presence of a major depressive episode (MDE) and the absence of a manic, mixed, or hypomanic episode. Thus, MDE includes depressive episodes that occur in both unipolar depression and bipolar disorder, whereas MDD includes only unipolar depression. However, the vast majority of lifetime and twelve-month MDE is MDD.
The broadest search term would only have included search terms related to depression. This would ensure that the identified articles included studies that were not focused on gender differences but still reported the relevant statistics. However, PsycINFO and PubMed each identified over 100,000 articles when the search term was soltely “depression,” leading us to narrow the search to both depression and (gender or sex) in the search terms.
Some researchers have questioned the construct validity of self-report depression symptom questionnaires, suggesting that these measures may assess general distress and not specifically depression in the general population (e.g., Kendall, Hollon, Beck, Hammen, & Ingram, 1987). The CES-D, which was the most frequently used symptom questionnaire in the depression symptom meta-analysis, was not designed for clinical diagnoses; however, the items are based on symptoms of major depression. Numerous validation studies are available; in one, the CES-D had a sensitivity of 100% and a specificity of 88% for 1-month major depression diagnoses (Beekman et al., 1997). The CES-D had a weighted sensitivity of 40% for all anxiety disorders in the past year, suggesting specificity for depression versus anxiety.
The majority of studies provided sample sizes for each gender and for each gender stratified by moderating variables; however, for several studies in which this information was not available, we estimated sub-group sample sizes from the total sample size.
All studies in the meta-analysis were conducted with DSM-IV-TR or earlier so we rely on it as the source. In DSM-IV-TR and DSM-5 (American Psychiatric Association, 2013), the criteria for a major depressive episode are nearly identical. The one exception is that the bereavement exclusion criterion was removed in DSM-5. In the DSM-IV-TR, criterion E for a major depressive episode specified “the symptoms are not better accounted for by Bereavement, i.e., after the loss of a loved one, the symptoms persist for longer than 2 months or are characterized by marked functional impairment, morbid preoccupation with worthlessness, suicidal ideation, psychotic symptoms, or psychomotor retardation” (American Psychiatric Association, 2000, p. 356).
For example, consider a sample with 1000 females and 1000 males, where 100 females and 50 males are depressed. The ratio of depressed females to males is 2:1 (100/50). The OR is 2.11 ((100/900)/ (50/950)). If we maintain the 2:1 ratio but increase the prevalence of depression (200 depressed females, 100 depressed males), then the OR increases to 2.25.
References
References marked with one asterisk (*) indicate studies included in the depression symptom meta-analysis. References marked with two asterisks (**) indicate studies included in the depression diagnosis meta-analysis.
- *.Aalto AM, Elovainio M, Kivimaki M, Uutela A, Pirkola S. The Beck Depression Inventory and General Health Questionnaire as measures of depression in the general population: a validation study using the Composite International Diagnostic Interview as the gold standard. Psychiatry Research. 2012;197(1–2):163–171. doi: 10.1016/j.psychres.2011.09.008. [DOI] [PubMed] [Google Scholar]
- *.Abebe DS, Froyland LR, Bakken A, von Soest T. Municipal-level differences in depressive symptoms among adolescents in Norway: Results from the cross-national Ungdata study. Scandinavian Journal of Public Health. 2016;44(1):47–54. doi: 10.1177/1403494815604764. [DOI] [PubMed] [Google Scholar]
- **.Alaimo K, Olson CM, Frongillo EA. Family food insufficiency, but not low family income, is positively associated with dysthymia and suicide symptoms in adolescents. Journal of Nutrition. 2002;132(4):719–725. doi: 10.1093/jn/132.4.719. [DOI] [PubMed] [Google Scholar]
- *.Almqvist F, Kumpulainen K, Ikaheimo K, Linna SL, Henttonen I, Huikko E, Moilanen I. Behavioural and emotional symptoms in 8–9-year-old children. European Child Adolescent Psychiatry. 1999;8:7–16. doi: 10.1007/pl00010698. [DOI] [PubMed] [Google Scholar]
- Alsaker FD, Dundas I, Olweus D. A growth curve approach to the study of parental relations and depression in adolescence. Paper presented in Seattle; April.1991. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 3rd. Washington, DC: American Psychiatric Association; 1980. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 3rd. Washington, DC: American Psychiatric Association; 1987. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th. Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- American Psychological Association. Publication manual. Washington, DC: APA; 2010. [Google Scholar]
- APA Publications and Communications Board Working Group on Journal Article Reporting Standards. Reporting standards for research in psychology. American Psychologist. 2008;63:839–851. doi: 10.1037/amp0000191. [DOI] [PubMed] [Google Scholar]
- *.Andersen I, Thielen K, Nygaard E, Diderichsen F. Social inequality in the prevalence of depressive disorders. Journal of Epidemiology and Community Health. 2009;63(7):575–581. doi: 10.1136/jech.2008.082719. [DOI] [PubMed] [Google Scholar]
- Andrade, et al. The epidemiology of major depressive episodes: results from the International Consortium of Psychiatric Epidemiology (ICPE) Surveys. International Journal of Methods in Psychiatric Research. 2003;12:3–21. doi: 10.1002/mpr.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **.Andrews G, Henderson S, Hall W. Prevalence, comorbidity, disability and service utilization: Overview of the Australian National Mental Health Survey. The British Journal of Psychiatry. 2001;178:145–153. doi: 10.1192/bjp.178.2.145. [DOI] [PubMed] [Google Scholar]
- Angold A, Costello EJ, Messer SC, Pickles A, Winder F, Silver D. Development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. International Journal of Methods in Psychiatric Research. 1995;5(4):237–250. [Google Scholar]
- Angst J, Gamma A, Gastpar M, Lépine JP, Mendlewicz J, Tylee A. Gender differences in depression. Epidemiological findings from the European DEPRES I and II studies. European Archives of Psychiatry and Clinical Neuroscience. 2002;252:201–209. doi: 10.1007/s00406-002-0381-6. [DOI] [PubMed] [Google Scholar]
- **.Arokiasamy P, Parasuraman S, Sekher TV, Lhungdim H. India: Study on global AGEing and adult health (SAGE), Wave 1 International Institute for Population Sciences. Geneva: World Health Organization; 2013. [Google Scholar]
- Avenevoli S, Knight E, Kessler RC, Merikangas KR. Epidemiology of depression in children and adolescents. In: Abela JRZ, Hankin BL, editors. Handbook of depression in children and adolescents. New York: Guilford; 2008. pp. 6–32. [Google Scholar]
- **.Avenevoli S, Swendsen J, He JP, Burnstein M, Merikangas KR. Major depression in the national comorbidity survey-adolescent supplement: prevalence, correlates, and treatment. Journal of the American Academy of Child and Adolescent Psychiatry. 2015;54:37–44. doi: 10.1016/j.jaac.2014.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes DM, Keyes KM, Bates LM. Racial differences in depression in the United States: how do subgroup analyses inform a paradox? Social Psychiatry and Psychiatric Epidemiology. 2013;48(12):1941–1949. doi: 10.1007/s00127-013-0718-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **.Beals J, Manson SM, Whitesell NR, Mitchell CM, Novins DK, Simpson S, Spicer P. Prevalence of major depressive episode in two American Indian reservation populations: unexpected findings with a structured interview. American Journal of Psychiatry. 2005;162(9):1713–1722. doi: 10.1176/appi.ajp.162.9.1713. [DOI] [PubMed] [Google Scholar]
- Bebbington PE. The origins of sex differences in depressive disorder: Bridging the gap. International Review of Psychiatry. 1996;8:295–332. [Google Scholar]
- Bebbington PE, Dunn G, Jenkins R, Lewis G, Brugha T, Farrell M, Meltzer H. The influence of age and sex on the prevalence of depressive conditions: Report from the National Survey of Psychiatric Morbidity. Psychological Medicine. 1998;28(1):9–19. doi: 10.1017/s0033291797006077. [DOI] [PubMed] [Google Scholar]
- Bech P, Rasmussen N, Olsen LR, Noerholm V, Abildgaard W. The sensitivity and specificity of the Major Depression Inventory, using the Present State Examination as the index of diagnostic validity. Journal of Affective Disorders. 2001;66(2–3):159–64. doi: 10.1016/s0165-0327(00)00309-8. [DOI] [PubMed] [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Beekman AT, Deeg DJ, Van Limbeek J, Braam AW, De Vries MZ, Van Tilburg W. Criterion validity of the Center for Epidemiologic Studies Depression scale (CES-D): results from a community-based sample of older subjects in The Netherlands. Psychological Medicine. 1997;27:231–235. doi: 10.1017/s0033291796003510. [DOI] [PubMed] [Google Scholar]
- Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–1101. [PubMed] [Google Scholar]
- *.Belanger RE, Akre C, Berchtold A, Michaud PA. A U-shaped association between intensity of internet use and adolescent health. Pediatrics. 2011;127:e330–335. doi: 10.1542/peds.2010-1235. [DOI] [PubMed] [Google Scholar]
- Belle D. Poverty and women’s mental health. American Psychologist. 1990;45:385–389. [Google Scholar]
- Belle D, Doucet J. Poverty, inequality, and discrimination as sources of depression among U. S. women. Psychology of Women Quarterly. 2003;27:1–12. [Google Scholar]
- **.Bijl RV, Ravelli A, Van Zessen G. Prevalence of psychiatric disorder in the general population: results of The Netherlands Mental Health Survey and Incidence Study (NEMESIS) Social Psychiatry Psychiatric Epidemiology. 1998;33:587–595. doi: 10.1007/s001270050098. [DOI] [PubMed] [Google Scholar]
- Bor W, Dean AJ, Najman J, Hayatbakhsh R. Are child and adolescent mental health problems increasing in the 21st century? A systematic review. Australian and New Zealand Journal of Psychiatry. 2014;48:606–616. doi: 10.1177/0004867414533834. [DOI] [PubMed] [Google Scholar]
- Borenstein M, Hedges LV, Higgins J, Rothstein H. Comprehensive Meta-Analysis. Biostat Inc.; Englewood: 2014. 3.3.070 edn. [Google Scholar]
- **.Boyd A, Van de Velde S, Vilagut G, de Graaf R, O’Neill S, Florescu S, EU-WMH Investigators Gender differences in mental disorders and suicidality in Europe: Results from a large cross-sectional population-based study. Journal of Affective Disorders. 2015;173:245–254. doi: 10.1016/j.jad.2014.11.002. [DOI] [PubMed] [Google Scholar]
- *.Bracke P. Sex differences in the course of depression: evidence from a longitudinal study of a representative sample of the Belgian population. Social Psychiatry Psychiatric Epidemiology. 1998;33:420–429. doi: 10.1007/s001270050075. [DOI] [PubMed] [Google Scholar]
- Breslau J, Kendler KS, Su M, Gaxiola-Aguilar S, Kessler RC. Lifetime risk and persistence of psychiatric disorders across ethnic groups in the United States. Psychological Medicine. 2005;35:317–327. doi: 10.1017/s0033291704003514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **.Bromet E, Andrade LH, Hwang I, Sampson NA, Alonso J, de Girolamo G, Kessler RC. Cross-national epidemiology of DSM-IV major depressive episode. BMC Medicine. 2011;9:90. doi: 10.1186/1741-7015-9-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **.Bromet EJ, Gluzman SF, Paniotto VI, Webb CP, Tintle NL, Zakhozha V, Schwartz JE. Epidemiology of psychiatric and alcohol disorders in Ukraine: Findings from the Ukraine World Mental Health Survey. Social Psychiatry Psychiatric Epidemiology. 2005;40:681–690. doi: 10.1007/s00127-005-0927-9. [DOI] [PubMed] [Google Scholar]
- Brückner H, Mayer KU. De-standardization of the life course: What it might mean? And if it means anything, whether it actually took place? Advances in Life Course Research. 2005;9:27–53. [Google Scholar]
- Brugha TS, Nienhuis F, Bagchi D, Smith J, Meltzer H. The survey form of SCAN: The feasibility of using experienced lay survey interviewers to administer a semi-structured systematic clinical assessment of psychotic and non-psychotic disorders. Psychological Medicine. 1999;29:703–711. doi: 10.1017/s003329179900834x. [DOI] [PubMed] [Google Scholar]
- *.Bushman BJ, Moeller SJ, Konrath S, Crocker J. Investigating the link between liking versus wanting self?esteem and depression in a nationally representative sample of American adults. Journal of Personality. 2012;80(5):1453–1469. doi: 10.1111/j.1467-6494.2012.00781.x. [DOI] [PubMed] [Google Scholar]
- *.Cardozo BL, Bilukha OO, Gotway CA, Wolfe MI, Gerber ML, Anderson M. Mental Health of Women in Postwar Afghanistan. Journal of Women’s Health. 2005;14(4):285–293. doi: 10.1089/jwh.2005.14.285. [DOI] [PubMed] [Google Scholar]
- *.Cater ÅK, Miller LE, Howell KH, Graham-Bermann SA. Childhood exposure to intimate partner violence and adult mental health problems: Relationships with gender and age of exposure. Journal of Family Violence. 2015;30(7):875–886. doi: http://dx.doi.org/10.1007/s10896-015-9703-0. [Google Scholar]
- **.Center for Behavioral Health Statistics and Quality. 2013 National Survey on Drug Use and Health: Mental Health Detailed Tables. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2014. [Google Scholar]
- **.Chan Chee C, Gourier-Fréry C, Guignard R, Beck F. The current state of mental health surveillance in France. Santé Publique. 2011;23:11–29. [PubMed] [Google Scholar]
- *.Chan A, Malhotra C, Malhotra R, Ostbye T. Living arrangements, social networks and depressive symptoms among older men and women in Singapore. International Journal of Geriatric Psychiatry. 2011;26(6):630–639. doi: 10.1002/gps.2574. [DOI] [PubMed] [Google Scholar]
- **.Cho MJ, Chang SM, Lee YM, Bae A, Ahn JH, Son J, Kim BS. Prevalence of DSM-IV major mental disorders among Korean adults: A 2006 national epidemiological survey (KECA-R) Asian Journal of Psychiatry. 2010;3:26–30. doi: 10.1016/j.ajp.2010.01.009. [DOI] [PubMed] [Google Scholar]
- Cho MJ, Hahm BJ, Suh DW, Hong JP, Bae JN, Kim JK, Cho SJ. Development of a Korean version of the composite international diagnostic interview (K-CIDI) Journal of Korean Neuropsychiatric Association. 2002;41:123–137. [Google Scholar]
- **.Cho MJ, Kim JK, Jeon HJ, Suh T, Chung IW, Hong JP, Hahm BJ. Lifetime and 12-month prevalence of DSM-IV psychiatric disorders among Korean adults. Journal of Nervous and Mental Disease. 2007;195:203–210. doi: 10.1097/01.nmd.0000243826.40732.45. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA. A developmental psychopathology perspective on adolescence. Journal of Consulting and Clinical Psychology. 2002;70:6–20. doi: 10.1037//0022-006x.70.1.6. [DOI] [PubMed] [Google Scholar]
- *.Clark T, Fleming T, Bullen P, Crengle S, Denny S, Dyson B, Fortune S, Peiris-John R, Robinson E, Rossen F. Youth’12 Prevalence Tables: The health and wellbeing of New Zealand secondary school students in 2012. Auckland, New Zealand: University of Auckland; 2013. [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- Cole DA, Ciesla J, Dallaire DH, Jacquez FM, Pineda A, LaGrange B, Truss AE, Folmer A, Osborne-Tilghman C, Felton J. Emergence of attributional style and its relation to depressive symptoms. Journal of Abnormal Psychology. 2008;117:16–31. doi: 10.1037/0021-843X.117.1.16. [DOI] [PubMed] [Google Scholar]
- Cole ER. Intersectionality and research in psychology. American Psychologist. 2009;64:170–180. doi: 10.1037/a0014564. [DOI] [PubMed] [Google Scholar]
- *.Collins AL, Glei DA, Goldman N. The role of life satisfaction and depressive symptoms in all-cause mortality. Psychology and Aging. 2009;24:696–702. doi: 10.1037/a0016777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copeland, et al. Do the negative effects of early pubertal timing on adolescent girls continue into young adulthood? American Journal of Psychiatry. 2010;167:1218–1225. doi: 10.1176/appi.ajp.2010.09081190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello CB, Wight VR, Stone AJ. The American woman 2003–2004. New York: Palgrave/Macmillan; 2003. [Google Scholar]
- **.Coyne JC, Marcus SC. Health disparities in care for depression possibly obscured by the clinical significance criterion. American Journal of Psychiatry. 2006;163:1577–1579. doi: 10.1176/appi.ajp.163.9.1577. [DOI] [PubMed] [Google Scholar]
- Cross National Collaborative Group. The changing rate of major depression. Cross-national comparisons. Journal of the American Medical Association. 1992;268:3098–3105. doi: 10.1001/jama.1992.03490210080039. [DOI] [PubMed] [Google Scholar]
- *.Crimmins EM, Kim JK, Solé-Auró A. Gender differences in health: Results from SHARE, ELSA and HRS. European Journal of Public Health. 2011;21(1):81–91. doi: 10.1093/eurpub/ckq022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuijpers P, de Graaf R, van Dorsselaer S. Minor depression: risk profiles, functional disability, health care use and risk of developing major depression. Journal of Affective Disorders. 2004;79:71–79. doi: 10.1016/S0165-0327(02)00348-8. [DOI] [PubMed] [Google Scholar]
- Cuthbert BN, Insel TR. Toward the future of psychiatric diagnosis: The seven pillars of RDoC. BMC Medicine. 2013;11:126. doi: 10.1186/1741-7015-11-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cyranowski JM, Frank E, Young E, Shear MK. Adolescent onset of the gender difference in lifetime rates: A theoretical model. Archives of General Psychiatry. 2000;57:21–27. doi: 10.1001/archpsyc.57.1.21. [DOI] [PubMed] [Google Scholar]
- **.Danielson CK, de Arellano MA, Kilpatrick DG, Saunders BE, Resnick HS. Child maltreatment in depressed adolescents: differences in symptomatology based on history of abuse. Child Maltreatment. 2005;10(1):37–48. doi: 10.1177/1077559504271630. [DOI] [PubMed] [Google Scholar]
- **.De Graaf R, ten Have M, van Gool C, van Dorsselaer S. Prevalence of mental disorders and trends from 1996 to 2009. Results from the Netherlands Mental Health Survey and Incidence Study-2. Social Psychiatry and Psychiatric Epidemiology. 2012;47(2):203–213. doi: 10.1007/s00127-010-0334-8. [DOI] [PubMed] [Google Scholar]
- *.de Wit LM, van Straten A, van Herten M, Penninx BW, Cuijpers P. Depression and body mass index, a u-shaped association. BMC Public Health. 2009;9:14. doi: 10.1186/1471-2458-9-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis LR, Lipman RS, Covi L. SCL-90: An outpatient psychiatric rating scale- Preliminary report. Psychopharmacology Bulletin. 1973;9(1):13–28. [PubMed] [Google Scholar]
- *.Dooley B, Fitzgerald A, Giollabhui NM. The risk and protective factors associated with depression and anxiety in a national sample of Irish adolescents. Irish Journal of Psychological Medicine. 2015;32(Spec Iss1):93–105. doi: 10.1017/ipm.2014.83. doi: http://dx.doi.org/10.1017/ipm.2014.83. [DOI] [PubMed] [Google Scholar]
- Eagly AH, Wood W. The origins of sex differences in human behavior: Evolved dispositions versus social roles. American Psychologist. 1999;54:408–423. [Google Scholar]
- Else-Quest NM, Grabe S. The political is personal: Measurement and application of nation-level indicators of gender equity in psychological research. Psychology of Women Quarterly. 2012;36:131–144. [Google Scholar]
- Else-Quest NM, Hyde JS. Intersectionality in quantitative psychological research: I. Theoretical and epistemological issues. Psychology of Women Quarterly. 2016a;40:155–170. [Google Scholar]
- Else-Quest NM, Hyde JS. Intersectionality in quantitative psychological research: II. Methods and techniques. Psychology of Women Quarterly 2016b [Google Scholar]
- Else-Quest NM, Hyde JS, Goldsmith HH, Van Hulle CA. Gender differences in temperament: A meta-analysis. Psychological Bulletin. 2006;132:33–72. doi: 10.1037/0033-2909.132.1.33. [DOI] [PubMed] [Google Scholar]
- Else-Quest NM, Hyde JS, Linn MC. Cross-national patterns of gender differences in mathematics: A meta-analysis. Psychological Bulletin. 2010;136:103–127. doi: 10.1037/a0018053. [DOI] [PubMed] [Google Scholar]
- Endicott J, Spitzer RL. A diagnostic interview: The schedule for affective disorders and schizophrenia. Archive of General Psychiatry. 1978;35(7):837–44. doi: 10.1001/archpsyc.1978.01770310043002. [DOI] [PubMed] [Google Scholar]
- *.European Social Survey. Measuring and Reporting on Europeans’ Wellbeing: Findings from the European Social Survey. 2015 Retrieved from: www.esswellbeingmatters.org.
- *.Everson-Rose SA, House JS, Mero RP. Depressive symptoms and mortality risk in a national sample: Confounding effects of health status. Psychosomatic Medicine. 2004;66(6):823–830. doi: 10.1097/01.psy.0000145903.75432.1f. [DOI] [PubMed] [Google Scholar]
- **.Farbstein I, Mansbach-Kleinfeld I, Levinson D, Goodman R, Levav I, Vograft I, Apter A. Prevalence and correlates of mental disorders in Israeli adolescents: Results from a national mental health survey. Journal of Child Psychology and Psychiatry. 2010;51(5):630–639. doi: 10.1111/j.1469-7610.2009.02188.x. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, Ridder EM, Beautrais AL. Subthreshold depression in adolescence and mental health outcomes in adulthood. Archives of General Psychiatry. 2005;62:66–72. doi: 10.1001/archpsyc.62.1.66. [DOI] [PubMed] [Google Scholar]
- *.Ferketich AK, Schwartzbaum JA, Frid DJ, Moeschberger ML. Depression as an antecedent to heart disease among women and men in the NHANES I study. National Health and Nutrition Examination Survey. Archives of Internal Medicine. 2000;160(9):1261–1268. doi: 10.1001/archinte.160.9.1261. [DOI] [PubMed] [Google Scholar]
- Ferrari AJ, Somerville AJ, Baxter AJ, Norman R, Patten SB, Vos R, Whiteford HA. Global variation in the prevalence and incidence of major depressive disorder: a systematic review of the epidemiological literature. Psychological Medicine. 2013;43(3):471–481. doi: 10.1017/S0033291712001511. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for DSM-IV-TR Axis I Disorders. New York: Biometrics Research Department, New York State Psychiatric Institute; 2002. [Google Scholar]
- Fischer AH, Rodriguez Mosquera PM, van Vianen AEM, Manstead ASR. Gender and culture differences in emotion. Emotion. 2004;4:87–94. doi: 10.1037/1528-3542.4.1.87. [DOI] [PubMed] [Google Scholar]
- *.Fleiz Bautista C, Villatoro Velazquez J, Mora Icaza ME, Moreno Lopez M, Gutierrez Lopez Mde L, Oliva Robles N. Sociodemographic and personal factors related to depressive symptomatology in the Mexican population aged 12 to 65. Revista Brasileira de Psiquiatria. 2012;34(4):395–404. doi: 10.1016/j.rbp.2012.03.004. [DOI] [PubMed] [Google Scholar]
- *.Fleming TM, Clark T, Denny S, Bullen P, Crengle S, Peiris-John R, Lucassen M. Stability and change in the mental health of New Zealand secondary school students 2007–2012: Results from the national adolescent health surveys. Australian & New Zealand Journal of Psychiatry. 2014;48(5):472–480. doi: 10.1177/00048674135144489. [DOI] [PubMed] [Google Scholar]
- **.Ford T Goodman R, Meltzer H. The British Child and Adolescent Mental Health Survey 1999: the prevalence of DSM-IV disorders. Journal of the Academy of Child and Adolescent Psychiatry. 2003;42:1203–1211. doi: 10.1097/00004583-200310000-00011. [DOI] [PubMed] [Google Scholar]
- **.Gabilondo A, Rojas-Farreras S, Vilagut G, Haro JM, Fernandez A, Pinto-Meza A, Alonso J. Epidemiology of major depressive episode in a southern European country: Results from the ESEMeD-Spain project. Journal of Affective Disorders. 2010;120(1–3):76–85. doi: 10.1016/j.jad.2009.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Gault-Sherman M, Silver E, Sigfúsdóttir ID. Gender and the associated impairments of childhood sexual abuse: A national study of Icelandic youth. Social Science & Medicine. 2009;69(10):1515–1522. doi: 10.1016/j.socscimed.2009.08.037. [DOI] [PubMed] [Google Scholar]
- **.Gavin AR, Chae DH, Takeuchi D. Association between family structure in childhood and lifetime depressive disorder in adulthood among a nationally representative sample of Blacks. General Hospital Psychiatry. 2009;31(5):484–493. doi: 10.1016/j.genhosppsych.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ge X, Conger RD, Elder GH. Pubertal transition, stressful life events, and the emergence of gender differences in adolescent depressive symptoms. Developmental Psychology. 2001;37:404–417. doi: 10.1037//0012-1649.37.3.404. [DOI] [PubMed] [Google Scholar]
- *.Gettler LT, Oka RC. Are testosterone levels and depression risk linked based on partnering and parenting? Evidence from a large population-representative study of U.S. men and women. Social Science & Medicine. 2016;163:157–167. doi: 10.1016/j.socscimed.2016.06.044. doi: http://dx.doi.org/10.1016. [DOI] [PubMed] [Google Scholar]
- Goodman R, Ford T, Richards H, Gatward R, Meltzer H. The Development and Well-Being Assessment: Description and initial validation of an integrated assessment of child and adolescent psychopathology. Journal of Child Psychology and Psychiatry. 2000;41(5):645–655. doi: 10.1111/j.1469-7610.2000.tb02345.x. [DOI] [PubMed] [Google Scholar]
- **.Goodwin RD, Gotlib IH. Gender differences in depression: The role of personality factors. Psychiatry Research. 2004;126(2):135–142. doi: 10.1016/j.psychres.2003.12.024. [DOI] [PubMed] [Google Scholar]
- *,**.Graham K, Massak A, Demers A, Rehm J. Does the association between alcohol consumption and depression depend on how they are measured? Alcoholism: Clinical and Experimental Research. 2007;31(1):78–88. doi: 10.1111/j.1530-0277.2006.00274.x. [DOI] [PubMed] [Google Scholar]
- **.Grant BF. Comorbidity between DSM-IV drug use disorders and major depression: Results of a national survey of adults. Journal of Substance Abuse. 1995;7(4):481–497. doi: 10.1016/0899-3289(95)90017-9. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Hasin DS. The Alcohol Use Disorder and Associated Disabilities Interview Schedule–DSM–IV Version. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2001. [Google Scholar]
- *.Guarnaccia PJ, Angel R, Worobey JL. The impact of marital status and employment status on depressive affect for Hispanic Americans. Journal of Community Psychology. 1991;19(2):136–149. doi: 10.1002/1520-6629(199104)19:2<136::AID-JCOP2290190205>3.0.CO;2-6. [DOI] [Google Scholar]
- *.Gudmundsdottir G, Vilhjalmsson R. Group differences in outpatient help-seeking for psychological distress: Results from a national prospective study of Icelanders. Scandinavian Journal of Public Health. 2010;38(2):160–167. doi: 10.1177/1403494809357357. [DOI] [PubMed] [Google Scholar]
- Guimond S, Branscbome NR, Brunot S, Buunk AP, Chatard A, Désert M, Yzerbyt V. Culture, gender, and the self: Variations and impact of social comparison processes. Journal of Personality and Social Psychology. 2007;92:1118–1134. doi: 10.1037/0022-3514.92.6.1118. [DOI] [PubMed] [Google Scholar]
- **.Gureje O, Uwakwe R, Oladeji B, Makanjuola VO, Esan O. Depression in adult Nigerians: Results from the Nigerian Survey of Mental Health and Well-being. Journal of Affective Disorders. 2010;120(1–3):158–164. doi: 10.1016/j.jad.2009.04.030. [DOI] [PubMed] [Google Scholar]
- **.Haarasilta L, Marttunen M, Kaprio J, Aro H. The 12-month prevalence and characteristics of major depressive episode in a representative nationwide sample of adolescents and young adults. Psychological Medicine. 2001;31(7):1169–1179. doi: 10.1017/s0033291701004573. [DOI] [PubMed] [Google Scholar]
- Haeffel GJ, Abramson LY, Voelz ZR, Metalsky GI, Halberstadt L, Dykman BM, Donovan P, Hogan ME, Hankin BL, Alloy LB. Cognitive vulnerability to depression and lifetime history of Axis I psychopathology: A comparison of negative cognitive styles (CSQ) and dysfunctional attitudes (DAS) Journal of Cognitive Psychotherapy: An International Quarterly. 2003;17:3–22. [Google Scholar]
- Hammerström A, Lehti A, Danielsson U, Bengs C, Johansson EE. Gender-related explanatory models of depression: A critical evaluation of medical articles. Public Health. 2009;123:689–693. doi: 10.1016/j.puhe.2009.09.010. [DOI] [PubMed] [Google Scholar]
- Hankin BL, Abramson L, Moffitt T, Silva P, McGee R, Angell KE. Development of depression from preadolescence to young adulthood: Emerging gender differences in a 10-year longitudinal study. Journal of Abnormal Psychology. 1998;107:128–140. doi: 10.1037//0021-843x.107.1.128. [DOI] [PubMed] [Google Scholar]
- *.Hardie JH. The consequences of unrealized occupational goals in the transition to adulthood. Social Science Research. 2014;48:196–211. doi: 10.1016/j.ssresearch.2014.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harkness J, Pennell BE, Villar A, Gebler N, Aguilar-Gaxiola S, Bilgen I. In: Translation procedures and translation assessment in the World Mental Health Survey Initiative In The WHO World Mental Health Surveys: Global Perspectives on the Epidemiology of Mental Disorders. Kessler RC, Ustün TB, editors. New York, NY: Cambridge University Press; 2008. pp. 91–113. [Google Scholar]
- *.Haroz EE, Ybarra ML, Eaton WW. Psychometric evaluation of a self-report scale to measure adolescent depression: the CESDR-10 in two national adolescent samples in the United States. Journal of Affective Disorders. 2014;158:154–160. doi: 10.1016/j.jad.2014.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartung CM, Widiger TA. Gender differences in the diagnosis of mental disorders: Conclusions and controversies of the DSM-IV. Psychological Bulletin. 1998;123:260–278. doi: 10.1037/0033-2909.123.3.260. [DOI] [PubMed] [Google Scholar]
- **.Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of major depressive disorder: results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Archives of General Psychiatry. 2005;62(10):1097–1106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- *.Haukkala A, Konttinen H, Uutela A, Kawachi I, Laatikainen T. Gender differences in the associations between depressive symptoms, cardiovascular diseases, and all-cause mortality. Annuals of Epidemiology. 2009;19(9):623–629. doi: 10.1016/j.annepidem.2009.01.010. [DOI] [PubMed] [Google Scholar]
- *.Hauser W, Schmutzer G, Brahler E, Schiltenwolf M, Hilbert A. The impact of body weight and depression on low back pain in a representative population sample. Pain Medicine. 2014;15(8):1316–1327. doi: 10.1111/pme.12458. [DOI] [PubMed] [Google Scholar]
- Hedges LV. Distribution theory for Glass’s estimator of effect size and related estimators. Journal of Educational Statistics. 1981;6:107–128. [Google Scholar]
- Hedges LV, Nowell A. Sex differences in mental test scores, variability, and numbers of high-scoring individuals. Science. 1995;269(5220):41–45. doi: 10.1126/science.7604277. [DOI] [PubMed] [Google Scholar]
- Hedges LV, Pigott TD. The power of statistical tests for moderators in meta-analysis. Psychological Methods. 2004;9:426–445. doi: 10.1037/1082-989X.9.4.426. [DOI] [PubMed] [Google Scholar]
- Hopcroft RL, Bradley DB. The sex difference in depression across 29 countries. Social Forces. 2007;85:1483–1507. [Google Scholar]
- *.Huang YT, Chen YW. Risk factors for depressed mood in a Taiwanese school-based sample of adolescents: Does spirituality have protective effects? British Journal of Social Work. 2015;45(7):2020–2037. [Google Scholar]
- *.Hwang JM, Cheong PH, Feeley TH. Being young and feeling blue in Taiwan: Examining adolescent depressive mood and online and offline activities. New Media and Society. 2009;11(7):1101–1121. doi: 10.1177/1461444809341699. [DOI] [Google Scholar]
- Hyde JS, *Lindberg SM, Linn MC, Ellis A, *Williams C. Gender similarities characterize math performance. Science. 2008a;321:494–495. doi: 10.1126/science.1160364. [DOI] [PubMed] [Google Scholar]
- Hyde JS, Mezulis AH, Abramson LY. The ABCs of depression: Integrating affective, biological, and cognitive models to explain the emergence of the gender difference in depression. Psychological Review. 2008b;115:291–313. doi: 10.1037/0033-295X.115.2.291. [DOI] [PubMed] [Google Scholar]
- *.Inaba A, Thoits PA, Ueno K, Gove WR, Evenson RJ, Sloan M. Depression in the United States and Japan: Gender, marital status, and SES patterns. Social Science & Medicine. 2005;61(11):2280–2292. doi: 10.1016/j.socscimed.2005.07.014. [DOI] [PubMed] [Google Scholar]
- **.Instituto Nacional de Salud Publica (INSP) Mexico: Study on global AGEing and adult health (SAGE), Wave 1. Geneva: World Health Organization; 2014. [Google Scholar]
- *.Ismayilova L, Hmoud O, Alkhasawneh E, Shaw S, El-Bassel N. Depressive symptoms among Jordanian youth: Results of a national survey. Community Mental Health Journal. 2013;49(1):133–140. doi: 10.1007/s10597-012-9529-7. [DOI] [PubMed] [Google Scholar]
- *.Jaddou HY, Batieha AM, Khader YS, Kanaan SH, El-Khateeb MS, Ajlouni KM. Depression is associated with low levels of 25-hydroxyvitamin D among Jordanian adults: Results from a national population survey. Europeans Archives Psychiatry Clinical Neuroscience. 2012;262(4):321–327. doi: 10.1007/s00406-011-0265-8. [DOI] [PubMed] [Google Scholar]
- *.Jang SN, Kawachi I, Chang J, Boo K, Shin HG, Lee H, Cho SI. Marital status, gender, and depression: Analysis of the baseline survey of the Korean Longitudinal Study of Ageing (KLoSA) Social Science & Medicine. 2009;69(11):1608–1615. doi: 10.1016/j.socscimed.2009.09.007. [DOI] [PubMed] [Google Scholar]
- **.Joe S, Baser RS, Neighbors HW, Caldwell CH, Jackson JS. 12-month and lifetime prevalence of suicide attempts among Black adolescents in the National Survey of American Life. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48(3):271–282. doi: 10.1097/CHI.0b013e318195bccf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Kaji T, Mishima K, Kitamura S, Enomoto M, Nagase Y, Li L, Kaneita Y, Ohida T, Uchiyama M. Relationship between late-life depression and life stressors: Large-scale cross-sectional study of a representative sample of the Japanese general population. Psychiatry and Clinical Neurosciences. 2010;64(4):426–434. doi: 10.1111/j.1440-1819.2010.02097.x. [DOI] [PubMed] [Google Scholar]
- *.Karadag H, Oner O, Karaoglan A, Orsel S, Demir AU, Firat H, Itil O. Body mass index and sexual dysfunction in males and females in a population study. Klinik Psikofarmakoloji Bülteni / Bulletin of Clinical Psychopharmacology. 2014;24(1):76–83. [Google Scholar]
- Kendall PC, Hollon SD, Beck AT, Hammen CL, Ingram RE. Issues and recommendations regarding use of the Beck Depression Inventory. Cognitive Therapy and Research. 1987;1:289–299. [Google Scholar]
- Kendler KS, Gardner CO. Sex differences in the pathways to major depression: A study of opposite-sex twin pairs. American Journal of Psychiatry. 2014;171(4):426–435. doi: 10.1176/appi.ajp.2013.13101375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Andrews G, Mroczek D, Ustun B, Wittchen HU. The World Health Organization Composite International Diagnostic Interview Short Form (CIDI-SF) International Journal of Methods in Psychiatric Research. 1998;7(4):171–185. doi: 10.1002/mpr.47. [DOI] [Google Scholar]
- **.Kessler RC, Birnbaum H, Bromet E, Hwang I, Sampson N, Shahly V. Age differences in major depression: Results from the National Comorbidity Surveys Replication (NCS-R) Psychological Medicine. 2010;40(2):225–237. doi: 10.1017/S0033291709990213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Bromet E. The epidemiology of depression across cultures. Annual Review of Public Health. 2013;34:119–138. doi: 10.1146/annurev-publhealth-031912-114409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **.Kessler RC, McGonagle KA, Swartz M, Blazer DG, Nelson CB. Sex and depression in the National Comorbidity Survey. I: Lifetime prevalence, chronicity and recurrence. Journal of Affective Disorders. 1993;29(2–3):85–96. doi: 10.1016/0165-0327(93)90026-g. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Ustun TB. The World Mental Health (WMH) survey initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) International Journal of Methods Psychiatric Research. 2004;13(2):93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Ustün TB. The WHO World Mental Health Surveys: Global Perspectives on the Epidemiology of Mental Disorders. New York, NY: Cambridge University Press; 2008. [Google Scholar]
- **.Kienja A, Piotrowski P, Adamowski T, Moskalewicz J, Wciorka J, Stokwiszewski J, Kessler R. The prevalence of common mental disorders in the population of adult Poles by sex and age structure- an EZOP Poland study. Psychiatry Poland. 2015;49:15–27. doi: 10.12740/PP/30811. [DOI] [PubMed] [Google Scholar]
- *.Kim HS. Sexual debut and mental health among South Korean adolescents. Journal of Sex Research. 2016;53(3):313–320. doi: 10.1080/00224499.2015.1055855. doi: http://dx.doi.org/10.1080/00224499.2015.1055855. [DOI] [PubMed] [Google Scholar]
- **.Kim JH, Cho MJ, Hong JP, Bae JN, Cho SJ, Hahm BJ, Chang SM. Gender Differences in Depressive Symptom Profile: Results from Nationwide General Population Surveys in Korea. Journal of Korean Medical Science. 2015;30(11):1659–1666. doi: 10.3346/jkms.2015.30.11.1659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein DN, Shankman SA, Lewinsohn PM, Seeley JR. Subthreshold depression in adolescents: Predictors of escalation to full syndrome depressive disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48:703–710. doi: 10.1097/CHI.0b013e3181a56606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Kliem S, Mossle T, Zenger M, Brahler E. Reliability and validity of the Beck Depression Inventory-Fast Screen for medical patients in the general German population. Journal of Affective Disorders. 2014;156:236–239. doi: 10.1016/j.jad.2013.11.024. [DOI] [PubMed] [Google Scholar]
- Kling KC, Hyde JS, Showers C, Buswell B. Gender differences in self-esteem: A meta-analysis. Psychological Bulletin. 1999;125:470–500. doi: 10.1037/0033-2909.125.4.470. [DOI] [PubMed] [Google Scholar]
- *.Klomek AB, Sourander A, Niemela S, Kumpulainen K, Piha J, Tamminen T, Gould MS. Childhood bullying behaviors as a risk for suicide attempts and completed suicides: A population-based birth cohort study. Journal of the American Academy of Child Adolescent Psychiatry. 2009;48(3):254–261. doi: 10.1097/CHI.0b013e318196b91f. [DOI] [PubMed] [Google Scholar]
- *.Kocalevent RD, Hinz A, Brahler E. Standardization of the depression screener patient health questionnaire (PHQ-9) in the general population. General Hospital Psychiatry. 2013;5:551–555. doi: 10.1016/j.genhosppsych.2013.04.006. [DOI] [PubMed] [Google Scholar]
- *.Kokkevi A, Fotiou A. The Psychosocial Module. In: Hibell B, Guttormsson U, Ahlstrom S, Balakireva O, Bjarnason T, Kokkevi A, Kraus L, editors. The 2007 ESPAD Report: Substance Use Among Students in 35 European Countries. The Swedish Council for Information on Alcohol and other Drugs (CAN); Stockholm, Sweden: 2009. [Google Scholar]
- *.Kokkevi A, Rotsika V, Arapaki A, Richardson C. Changes in associations between psychosocial factors and suicide attempts by adolescents in Greece from 1984 to 2007. European Journal of Public Health. 2011;21(6):694–698. doi: 10.1093/eurpub/ckq160. [DOI] [PubMed] [Google Scholar]
- *.Kopp MS, Skrabski A, Szedmak S. Socioeconomic factors, severity of depressive symptomatology, and sickness absence rate in the Hungarian population. Journal of Psychosomatic Research. 1995;39(8):1019–1029. doi: 10.1016/0022-3999(95)00513-7. [DOI] [PubMed] [Google Scholar]
- Koss MP, Goodman LA, Browne A, Fitzgerald LF, Russo NF, Keita GP. No safe haven: Male violence against women at home, at work, and in the community. Washingt, DC: American Psychological Association; 1994. [Google Scholar]
- Kovacs M. The Children’s Depression Inventory (CDI) Psychopharmacology Bulletin. 1985;21:995–998. [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuehner C. Gender differences in unipolar depression: An update of epidemiological findings and possible explanations. Acta Psychiatrica Scandinavica. 2003;108(3):163–74. doi: 10.1034/j.1600-0447.2003.00204.x. [DOI] [PubMed] [Google Scholar]
- **.Lara E, Olaya B, Garin N, Ayuso-Mateos JL, Miret M, Moneta V, Haro JM. Is cognitive impairment associated with suicidality? A population-based study. European Neuropsychopharmacology. 2015;25(2):203–213. doi: 10.1016/j.euroneuro.2014.08.010. [DOI] [PubMed] [Google Scholar]
- *.Lee MA. Emotional abuse in childhood and suicidality: The mediating roles of re-victimization and depressive symptoms in adulthood. Child Abuse and Neglect. 2015;44:130–139. doi: 10.1016/j.chiabu.2015.03.016. [DOI] [PubMed] [Google Scholar]
- *.Lei X, Sun X, Strauss J, Zhang P, Zhao Y. Depressive symptoms and SES among the mid-aged and elderly in China: Evidence from the China Health and Retirement Longitudinal Study national baseline. Social Science and Medicine. 2014;120:224–232. doi: 10.1016/j.socscimed.2014.09.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **.Lepine JP, Gastpar M, Mendlewicz J, Tylee A. Depression in the community: the first Pan-European study DEPRES (Depression Research in European Society) International Clinical Psychopharmacology. 1997;12:19–29. [PubMed] [Google Scholar]
- Lewis G, Pelosi AJ, Araya A, Dunn G. Measuring psychiatric disorder in the community: A standard assessment for use by lay interviewers. Psychological Medicine. 1992;22:465–486. doi: 10.1017/s0033291700030415. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Seeley JR, Klein DN, Gotlib IH. Natural course of adolescent major depressive disorder in a community sample: Predictors of recurrence in young adults. American Journal of Psychiatry. 2000;157:584–1591. doi: 10.1176/appi.ajp.157.10.1584. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Solomon A, Seeley JR, Zeiss A. Clinical implications of “subthreshold” depressive symptoms. Journal of Abnormal Psychology. 2000;109(2):345–351. [PubMed] [Google Scholar]
- Lindberg SM, Grabe S, Hyde JS. Gender, pubertal development, and peer sexual harassment predict objectified body consciousness in early adolescence. Journal of Research on Adolescence. 2007;17:723–742. [Google Scholar]
- Lindberg SM, Hyde JS, Petersen J, Linn MC. New trends in gender and mathematics performance: A meta-analysis. Psychological Bulletin. 2010;136:1123–1135. doi: 10.1037/a0021276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipsey MW, Wilson DB. Practical meta-analysis. Thousand Oaks, CA: Sage; 2001. [Google Scholar]
- **.Lorenzo-Blanco EI, Cortina LM. Latino/a depression and smoking: An analysis through the lenses of culture, gender, and ethnicity. American Journal of Community Psychology. 2013;51:332–346. doi: 10.1007/s10464-012-9553-3. [DOI] [PubMed] [Google Scholar]
- Lovibond SH, Lovibond PF. Manual for the Depression Anxiety Stress Scales. Sydney: Psychology Foundation; 1995. [Google Scholar]
- Luppa M1, Sikorski C, Luck T, Ehreke L, Konnopka A, Wiese B, Weyerer S, König HH, Riedel-Heller SG. Age- and gender-specific prevalence of depression in latest-life–systematic review and meta-analysis. Journal of Affective Disorders. 2012;136(3):212–21. doi: 10.1016/j.jad.2010.11.033.. [DOI] [PubMed] [Google Scholar]
- *.Madianos MG, Stefanis CN. Changes in the prevalence of symptoms of depression and depression across Greece. Social Psychiatry Psychiatric Epidemiology. 1992;27:211–219. doi: 10.1007/BF00788931. [DOI] [PubMed] [Google Scholar]
- *.Mäntyselkä PT, Turunen JH, Ahonen RS, Kumpusalo EA. Chronic pain and poor self-rated health. JAMA. 2003;290(18):2435–2442. doi: 10.1001/jama.290.18.2435. [DOI] [PubMed] [Google Scholar]
- *.Margraf J, Lavallee K, Zhang X, Schneider S. Social Rhythm and Mental Health: A Cross-Cultural Comparison. PLoS One. 2016;11(3):e0150312. doi: 10.1371/journal.pone.0150312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markon KE, Chmielewski &, Miller CJ. The reliability and validity of discrete and continuous measures of psychopathology: A quantitative review. Psychological Bulletin. 2011;137:856–879. doi: 10.1037/a0023678. [DOI] [PubMed] [Google Scholar]
- *.Marmorstein NR. Longitudinal associations between alcohol problems and depressive symptoms: Early adolescence through early adulthood. Alcoholism: Clinical and Experimental Research. 2009;33(1):49–59. doi: 10.1111/j.1530-0277.2008.00810.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *,**.Maske UE, Buttery AK, Beesdo-Baum K, Riedel-Heller S, Hapke U, Busch MA. Prevalence and correlates of DSM-IV-TR major depressive disorder, self-reported diagnosed depression and current depressive symptoms among adults in Germany. Journal of Affect Disorders. 2016;190:167–177. doi: 10.1016/j.jad.2015.10.006. [DOI] [PubMed] [Google Scholar]
- **.McMartin SE, Jacka FN, Colman I. The association between fruit and vegetable consumption and mental health disorders: Evidence from five waves of a national survey of Canadians. Preventive Medicine. 2013;56(3–4):225–230. doi: 10.1016/j.ypmed.2012.12.016. [DOI] [PubMed] [Google Scholar]
- McShane BB, Böckenholt U, Hansen KT. Adjusting for Publication Bias in Meta-analysis: An Evaluation of Selection Methods and Some Cautionary Notes. Perspectives on Psychological Science. 2016;11(5):730–749. doi: 10.1177/1745691616662243. [DOI] [PubMed] [Google Scholar]
- Mercier RJ, Garrett J, Thorp J, Siega-Riz AM. Pregnancy intention and postpartum depression: secondary data analysis from a prospective cohort. BJOG: An International Journal of Obstetrics and Gynaecology. 2013;120:1116–1122. doi: 10.1111/1471-0528.12255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **.Merikangas AK, Mendola P, Pastor PN, Reuben CA, Cleary SD. The association between major depressive disorder and obesity in US adolescents: Results from the 2001–2004 National Health and Nutrition Examination Survey. Journal of Behavioral Medicine. 2012;35(2):149–154. doi: 10.1007/s10865-011-9340-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Michal M, Glaesmer H, Zwerenz R, Knebel A, Wiltink J, Brahler E, Beutel ME. Base rates for depersonalization according to the 2-item version of the Cambridge Depersonalization Scale (CDS-2) and its associations with depression/anxiety in the general population. Journal of Affective Disorders. 2011;128(1–2):106–111. doi: 10.1016/j.jad.2010.06.033. [DOI] [PubMed] [Google Scholar]
- Mirowsky J. Age and the gender gap in depression. Journal of Health and Social Behavior. 1996;37(4):362–380. [PubMed] [Google Scholar]
- **.Mohammadi R, Davidian H, Noorbala AA, Malekafzali H, Naghavi HR, Pouretemad HR, Ghanizadeh A. An epidemiological survey of psychiatric disorders in Iran. Clinical Practice and Epidemiology in Mental Health. 2005;1:16. doi: 10.1186/1745-0179-1-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **.Mommersteeg PM, Herr R, Pouwer F, Holt RI, Loerbroks A. The association between diabetes and an episode of depressive symptoms in the 2002 World Health Survey: An analysis of 231,797 individuals from 47 countries. Diabetic Medicine. 2013;30(6):e208–214. doi: 10.1111/dme.12193. [DOI] [PubMed] [Google Scholar]
- *.Momtaz YA, Hamid TA, Haron SA, Bagat MF. Flourishing in later life. Archives of Gerontology and Geriatrics. 2016;63:85–91. doi: 10.1016/j.archger.2015.11.001. doi: http://dx.doi.org/10.1016/j.archger.2015.11.001. [DOI] [PubMed] [Google Scholar]
- Moos RH, Cronkite RC, Billings AG, Finney JW. Health and Daily Living Form manual, revised version Social Ecological Laboratory. Veterans Administration; and Stanford University Medical Centers, Stanford: 1985. [Google Scholar]
- *.Morozink JA, Friedman EM, Coe CL, Ryff CD. Socioeconomic and psychosocial predictors of Interleukin-6 in the MIDUS national sample. Health Psychology. 2010;29(6):626–635. doi: 10.1037/a0021360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Mumford EA, Liu W, Hair EC, Yu TC. Concurrent trajectories of BMI and mental health patterns in emerging adulthood. Social Science & Medicine. 2013;98:1–7. doi: 10.1016/j.socscimed.2013.08036. [DOI] [PubMed] [Google Scholar]
- *.Munhoz TN, Nunes BP, Wehrmeister FC, Santos IS, Matijasevich A. A nationwide population-based study of depression in Brazil. Journal of Affective Disorders. 2016;192:226–233. doi: 10.1016/j.jad.2015.12.038. [DOI] [PubMed] [Google Scholar]
- Munoz RF, Cuijpers P, Smit F, Barrera AZ, Leykin Y. Prevention of major depression. Annual Review of Clinical Psychology. 2010;6:181–212. doi: 10.1146/annurev-clinpsy-033109-132040. [DOI] [PubMed] [Google Scholar]
- **.National Research Institute of Public Health, Russian Academy of Medical Sciences (RAMS) The Russian Federation: Study on global AGEing and adult health (SAGE), Wave 1. Geneva: World Health Organization; 2013. [Google Scholar]
- *.Neumark-Sztainer D, Hannan PJ. Weight-related behaviors among adolescent girls and boys: Results from a national survey. Archives of Pediatrics & Adolescent Medicine. 2000;154(6):569–577. doi: 10.1001/archpedi.154.6.569. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S. Sex differences in unipolar depression: Evidence and theory. Psychological Bulletin. 1987;101(2):259–282. [PubMed] [Google Scholar]
- O’Connor EA, Whitlock EP, Beil TL, Gaynes BN. Screening for depression in adult patients in primary care settings: A systematic evidence review. Annals of Internal Medicine. 2009;151:793–803. doi: 10.7326/0003-4819-151-11-200912010-00007. [DOI] [PubMed] [Google Scholar]
- *.O’Halloran AM, Kenny RA, King-Kallimanis BL. The latent factors of depression from the short forms of the CES-D are consistent, reliable and valid in community-living older adults. European Geriatric Medicine. 2014;5(2):97–102. doi: 10.1016/j.eurger.2013.12.004. [DOI] [Google Scholar]
- *.Oh DH, Kim SA, Lee HY, Seo JY, Choi BY, Nam JH. Prevalence and correlates of depressive symptoms in Korean adults: Results of a 2009 Korean community health survey. Journal of Korean Medical Science. 2013;28(1):128–135. doi: 10.3346/jkms.2013.28.1.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Ojard C, Donnelly JP, Safford MM, Griffin R, Wang HE. Psychosocial stress as a risk factor for sepsis: A population-based cohort study. Psychosomatic Medicine. 2015;77:93–100. doi: 10.1097/PSY.0000000000000120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Okabayashi H, Liang J, Krause N, Akiyama H, Sugisawa H. Mental health among older adults in Japan: Do sources of social support and negative interaction make a difference? Social Science & Medicine. 2004;59:2259–2270. doi: 10.1016/j.socscimed.2004.02.024. [DOI] [PubMed] [Google Scholar]
- *.Oksuzyan A, Crimmins E, Saito Y, O’Rand A, Vaupel JW, Christensen K. Cross-national comparison of sex differences in health and mortality in Denmark, Japan and the US. European Journal of Epidemiology. 2010;25(7):471–480. doi: 10.1007/s10654-010-9460-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Olsen LR, Mortensen EL, Bech P. Mental distress in the Danish general population. Acta Psychiatrica Scandinavica. 2006;113(6):477–484. doi: 10.1111/j.1600-0447.2005.00743.x. [DOI] [PubMed] [Google Scholar]
- Oquendo MA, Ellis SP, Greenwald S, Malone KM, Weissman MM, Mann JJ. Ethnic and sex differences in suicide rates relative to major depression in the United States. American Journal of Psychiatry. 2001;158(10):1652–1658. doi: 10.1176/appi.ajp.158.10.1652. [DOI] [PubMed] [Google Scholar]
- *.Ostbye T, Malhotra R, Chan A. Thirteen dimensions of health in elderly Sri Lankans: results from a National Sri Lanka Aging Survey. Journal of the American Geriatrics Society. 2009;57(8):1376–1387. doi: 10.1111/j.1532-5415.2009.02350.x. [DOI] [PubMed] [Google Scholar]
- *.Park JH, Kim KW, Kim MH, Kim MD, Kim BJ, Kim SK, Cho MJ. A nationwide survey on the prevalence and risk factors of late life depression in South Korea. Journal of Affective Disorders. 2012;138(1–2):34–40. doi: 10.1016/j.jad.2011.12.038. [DOI] [PubMed] [Google Scholar]
- **.Patten SB. Markov models of major depression for linking psychiatric epidemiology to clinical practice. Clinical Practice and Epidemiology in Mental Health. 2005;1:2. doi: 10.1186/1745-0179-1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patten SB, Williams JV, Lavorato DH, Wang JL, Bulloch AG, Sajobi T. The association between major depression prevalence and sex becomes weaker with age. Soc Psychiatry Psychiatr Epidemiol. 2016;51(2):203–10. doi: 10.1007/s00127-015-1166-3.. [DOI] [PubMed] [Google Scholar]
- Pattyn E, Verhaeghe M, Bracke P. The gender gap in mental health service use. Social Psychiatry and Psychiatric Epidemiology. 2015;50(7):1089–1095. doi: 10.1007/s00127-015-1038-x. doi: http://dx.doi.org/10.1007/s00127-015-1038-x. [DOI] [PubMed] [Google Scholar]
- **.Peltzer K, Phaswana-Mafuya N. Depression and associated factors in older adults in South Africa. Global Health Action. 2013;6:1–9. doi: 10.3402/gha.v6i0.18871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen JL, Hyde JS. A meta-analytic review of research on gender differences in sexuality: 1993 to 2007. Psychological Bulletin. 2010;136:21–38. doi: 10.1037/a0017504. [DOI] [PubMed] [Google Scholar]
- Piccinelli M, Wilkinson G. Gender differences in depression: Critical review. British Journal of Psychiatry. 2000;177:486–492. doi: 10.1192/bjp.177.6.486. [DOI] [PubMed] [Google Scholar]
- **.Pirkola SP, Isometsa E, Suvisaari J, Aro H, Joukamaa M, Poikolainen K, Lonnqvist JK. DSM-IV mood-, anxiety- and alcohol use disorders and their comorbidity in the Finnish general population: Results from the Health 2000 Study. Social Psychiatry and Psychiatric Epidemiology. 2005;40:1–10. doi: 10.1007/s00127-005-0848-7. [DOI] [PubMed] [Google Scholar]
- Prince MJ, Reischies F, Beekman ATF, Fuhrer C, Jonker SL, Kivela BA, Copeland JR. Development of the EURO-D scale–a European: Union initiative to compare symptoms of depression in 14 European centres. British Journal of Psychiatry. 1999;174(4):330–338. doi: 10.1192/bjp.174.4.330.. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- **.Rafful C, Medina-Mora ME, Borges G, Benjet C, Orozco R. Depression, gender, and the treatment gap in Mexico. Journal of Affective Disorders. 2012;138(1–2):165–169. doi: 10.1016/j.jad.2011.12.040. [DOI] [PubMed] [Google Scholar]
- **.Rapsey CM, Lim CC, Al-Hamzawi A, Alonso J, Bruffaerts R, Caldas-de-Almeida JM, Scott KM. Associations between DSM-IV mental disorders and subsequent COPD diagnosis. Journal of Psychosomatic Research. 2015;79(5):333–339. doi: 10.1016/j.jpsychores.2015.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reilly D, Neumann DL, Andrews G. Sex differences in mathematics and science achievement: A meta-analysis of National Assessment of Educational Progress Assessments. Journal of Educational Psychology. 2015;107:645–662. [Google Scholar]
- Reiss F. Socioeconomic inequalities and mental health problems in children and adolescents: A systematic review. Social Science & Medicine. 2013;90:24–31. doi: 10.1016/j.socscimed.2013.04.026. [DOI] [PubMed] [Google Scholar]
- Revah-Levy A, Birmaher B, Gasquet I, Falissard B. The Adolescent Depression Rating Scale (ADRS): A validation study. BMC Psychiatry. 2007;7:2. doi: 10.1186/1471-244X-7-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Revah-Levy A, Speranza M, Barry C, Hassler C, Gasquet I, Moro MR, Falissard B. Association between Body Mass Index and depression: The “fat and jolly” hypothesis for adolescents girls. BMC Public Health. 2011;11:649. doi: 10.1186/1471-2458-11-649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Rey JM, Sawyer MG, Clark JJ, Baghurst PA. Depression among Australian adolescents. Medical Journal of Australia. 2001;175(1):19–23. doi: 10.5694/j.1326-5377.2001.tb143505.x. [DOI] [PubMed] [Google Scholar]
- Reynolds WM. RADS Professional Manual. Odessa, FL: Psychological Assessment Resources; 1986. [Google Scholar]
- *.Rief W, Glaesmer H, Baehr V, Broadbent E, Brahler E, Petrie KJ. The relationship of modern health worries to depression, symptom reporting and quality of life in a general population survey. Journal of Psychosomatic Research. 2012;72(4):318–320. doi: 10.1016/j.jpsychores.2011.11.017. [DOI] [PubMed] [Google Scholar]
- Rindfuss RR, Swicegood CG, Rosenfeld RA. Disorder in the life course: How common and does it matter? American Sociological Review. 1987;52:785–801. [Google Scholar]
- *.Risal A, Manandhar K, Linde M, Steiner TJ, Holen A. Anxiety and depression in Nepal: Prevalence, comorbidity and associations. BMC Psychiatry. 2016;16 doi: 10.1186/s12888-016-0810-0. doi: http://dx.doi.org/10.1186/s12888-016-0810-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robins LN, Helzer JE, Croughan J, Ratcliff KS. National Institute of Mental Health Diagnostic Interview Schedule: Its history, characteristics, and validity. Archives of General Psychiatry. 1981;38(4):381–389. doi: 10.1001/archpsyc.1981.01780290015001. [DOI] [PubMed] [Google Scholar]
- Rosenthal R. The “file drawer problem” and tolerance for null results. Psychological Bulletin. 1979;86:638–661. [Google Scholar]
- Salk RH, Petersen JL, Abramson LY, Hyde JS. The contemporary face of gender differences and similarities in depression throughout adolescence: Development and chronicity. Under review. 2016 doi: 10.1016/j.jad.2016.03.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salokangas RK, Poutanen O, Stengard E. Screening for depression in primary care. Development and validation of the Depression Scale, a screening instrument for depression. Acta Psychiatrica Scandinavica. 1995;92:10–16. doi: 10.1111/j.1600-0447.1995.tb09536.x. [DOI] [PubMed] [Google Scholar]
- **.Sandanger I, Nygard JF, Sorensen T, Dalgard OS. Return of depressed men: Changes in distribution of depression and symptom cases in Norway between 1990 and 2001. Journal of Affective Disorders. 2007;100(1–3):153–162. doi: 10.1016/j.jad.2006.10.006. [DOI] [PubMed] [Google Scholar]
- *.Sandman N, Valli K, Kronholm E, Revonsuo A, Laatikainen T, Paunio T. Nightmares: risk factors among the Finnish general adult population. Sleep. 2015;38(4):507–514. doi: 10.5665/sleep.4560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Scafato E, Galluzzo L, Ghirini S, Gandin C, Rossi A, Solfrizzi V, Farchi G. Changes in severity of depressive symptoms and mortality: The Italian Longitudinal Study on Aging. Psychological Medicine. 2012;42(12):2619–2629. doi: 10.1017/s0033291712000645. [DOI] [PubMed] [Google Scholar]
- **.Scott KM, Oakley Browne MA, Elisabeth Wells J. Prevalence, impairment and severity of 12-month DSM-IV major depressive episodes in Te Rau Hinengaro: New Zealand Mental Health Survey 2003/4. Australian & New Zealand Journal of Psychiatry. 2010;44(8):750–758. doi: 10.3109/00048671003781780. [DOI] [PubMed] [Google Scholar]
- *.Seaton EK, Caldwell CH, Sellers RM, Jackson JS. The prevalence of perceived discrimination among African American and Caribbean Black youth. Developmental Psychology. 2008;44(5):1288–1297. doi: 10.1037/a0012747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seedat S, Scott KM, Angermeyer MC, Berglund P, Bromet EJ, Brugha TS, Kessler RC. Cross-national associations between gender and mental disorders in the World Health Organization World Mental Health Surveys. Archives of General Psychiatry. 2009;66(7):785–795. doi: 10.1001/archgenpsychiatry.2009.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Seppala J, Koponen H, Kautiainen H, Eriksson JG, Kampman O, Mannisto S, Vanhala M. Association between folate intake and melancholic depressive symptoms. A Finnish population-based study. Journal of Affective Disorders. 2012;138(3):473–478. doi: 10.1016/j.jad.2012.01.007. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- **.Shah AJ, Veledar E, Hong Y, Bremner JD, Vaccarino V. Depression and history of attempted suicide as risk factors for heart disease mortality in young individuals. Archives of General Psychiatry. 2011;68(11):1135–1142. doi: 10.1001/archgenpsychiatry.2011.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **.Shanghai Municipal Center for Disease Control and Prevention (SCDC) China: Study on global AGEing and adult health (SAGE), Wave 1. Geneva: World Health Organization; 2012. [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Dunbar GC. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry. 1998;59(20):22–33. [PubMed] [Google Scholar]
- Siegel JM, Aneshensel CA, Taube B, Cantwell DP, Driscoll AK. Adolescent depression in a multi-ethnic sample. Journal of Youth and Adolescence. 1998;27:413–427. [Google Scholar]
- *.Shiovitz-Ezra S, Leitsch S, Graber J, Karraker A. Quality of life and psychological health indicators in the national social life, health, and aging project. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2009;64:i30–37. doi: 10.1093/geronb/gbn020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Sigfusdottir ID, Asgeirsdottir BB, Sigurdsson JF, Gudjonsson GH. Trends in depressive symptoms, anxiety symptoms and visits to healthcare specialists: A national study among Icelandic adolescents. Scandinavian Journal Public Health. 2008;36(4):361–368. doi: 10.1177/1403494807088457. [DOI] [PubMed] [Google Scholar]
- **.Skapinakis P, Bellos S, Koupidis S, Grammatikopoulos I, Theodorakis PN, Mavreas V. Prevalence and sociodemographic associations of common mental disorders in a nationally representative sample of the general population of Greece. BMC Psychiatry. 2013;13:163. doi: 10.1186/1471-244x-13-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **.Slade T, Johnston A, Browne MAO, Andrews G, Whiteford H. 2007 National Survey of Mental Health and Wellbeing: Methods and key findings. Australian and New Zealand Journal of Psychiatry. 2009;43(7):594–605. doi: 10.1080/00048670902970882. [DOI] [PubMed] [Google Scholar]
- Smeets RMW, Dingemans PMAJ. Composite International Diagnostic Interview (CIDI), version 1.1. Amsterdam/Geneva: World Health Organization; 1993. [Google Scholar]
- *.Song L. Social capital and psychological distress. Journal of Health and Social Behavior. 2011;52(4):478–492. doi: 10.1177/0022146511411921. [DOI] [PubMed] [Google Scholar]
- *.Sonnenberg CM, Deeg DJ, van Tilburg TG, Vink D, Stek ML, Beekman AT. Gender differences in the relation between depression and social support in later life. International Psychogeriatrics. 2013;25(1):61–70. doi: 10.1017/s1041610212001202. [DOI] [PubMed] [Google Scholar]
- **.Spiers N, Brugha TS, Bebbington P, McManus S, Jenkins R, Meltzer H. Age and birth cohort differences in depression in repeated cross-sectional surveys in England: The National Psychiatric Morbidity Surveys, 1993 to 2007. Psychological Medicine. 2012;42(10):2047–2055. doi: 10.1017/s003329171200013x. [DOI] [PubMed] [Google Scholar]
- *.Steptoe A, Demakakos P, de Oliveira C, Wardle J. Distinctive biological correlates of positive psychological well-being in older men and women. Psychosomatic Medicine. 2012;74(5):501–508. doi: 10.1097/PSY.0b013e31824f82c8. [DOI] [PubMed] [Google Scholar]
- *.Strong C, Tsai MC, Lin CY, Cheng CP. Childhood adversity, timing of puberty and adolescent depressive symptoms: A longitudinal study in Taiwan. Child Psychiatry and Human Development. 2016;47(3):347–357. doi: 10.1007/s10578-015-0570-y. http://dx.doi.org/10.1007/s10578-015-0570-y. [DOI] [PubMed] [Google Scholar]
- **.Subramaniam M, Abdin E, Vainganker JA, Nan L, Heng D, McCrone P, Chong SA. Impact of psychiatric disorders and chronic physical conditions on health-related quality of life: Singapore Mental Health Study. Journal of Affective Disorders. 2013;147(1–3):325–330. doi: 10.1016/j.jad.2012.11.033. [DOI] [PubMed] [Google Scholar]
- *.Sugihara Y, Sugisawa H, Shibata H, Harada K. Productive roles, gender, and depressive symptoms: evidence from a national longitudinal study of late-middle-aged Japanese. Journals of Gerontology Series B: Psychological Sciences & Social Sciences. 2008;63(4):227–234. doi: 10.1093/geronb/63.4.P227. [DOI] [PubMed] [Google Scholar]
- **.Suttajit S, Kittirattanapaiboon P, Junsirimongkol B, Likhitsathian S, Srisurapanont M. Risks of major depressive disorder and anxiety disorders among Thais with alcohol use disorders and illicit drug use: Findings from the 2008 Thai National Mental Health survey. Addictive Behaviors. 2012;37(12):1395–1399. doi: 10.1016/j.addbeh.2012.06.014. [DOI] [PubMed] [Google Scholar]
- *.Symonds J, Dietrich J, Chow A, Salmela-Aro K. Mental health improves after transition from comprehensive school to vocational education or employment in England: A national cohort study. Developmental Psychology. 2016;52(4):652–665. doi: 10.1037/a0040118. http://dx.doi.org/10.1037/a0040118. [DOI] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. Using multivariate statistics. 3rd. New York: HarperCollins; 1996. [Google Scholar]
- **.Takeuchi DT, Zane N, Hong S, Chae DH, Gong F, Gee GC, Alegria M. Immigration-related factors and mental disorders among Asian Americans. American Journal of Public Health. 2007;97(1):84–90. doi: 10.2105/ajph.2006.088401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Thege BK, Bachner YG, Kushnir T, Kopp MS. Relationship between meaning in life and smoking status: Results of a national representative survey. Addictive Behaviors. 2009;34(1):117–120. doi: 10.1016/j.addbeh.2008.09.001. [DOI] [PubMed] [Google Scholar]
- *.Thibodeau MA, Asmundson GJG. The PHQ-9 assesses depression similarly in men and women from the general population. Personality and Individual Differences. 2014;56:149–153. doi: 10.1016/j.paid.2013.08.039. [DOI] [Google Scholar]
- *.Torikka A, Kaltiala-Heino R, Rimpelä A, Marttunen M, Luukkaala T, Rimpelä M. Self-reported depression is increasing among socio-economically disadvantaged adolescents - repeated cross-sectional surveys from Finland from 2000 to 2011. BMC Public Health. 2014;14:408. doi: 10.1186/1471-2458-14-408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Torres JM, Wong R. Childhood poverty and depressive symptoms for older adults in Mexico: A life-course analysis. Journal of Cross-Cultural Gerontology. 2013;28(3):317–337. doi: 10.1007/s10823-013-9198-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **.Toussaint LL, Williams DR, Musick MA, Everson-Rose SA. The association of forgiveness and 12-month prevalence of major depressive episode: Gender differences in a probability sample of U.S. adults. Mental Health, Religion & Culture. 2008;11(5):485–500. doi: 10.1080/13674670701564989. [DOI] [Google Scholar]
- Tsai JL, Chentsova-Dutton Y. Understanding depression across cultures. In: Gotlib IH, Hammen CL, editors. Handbook of depression. New York: Guilford; 2002. pp. 467–491. [Google Scholar]
- Twenge J, Nolen-Hoeksema S. Age, gender, race, socioeconomic status, and birth cohort differences in the Children’s Depression Inventory: A meta-analysis. Journal of Abnormal Psychology. 2002;111:578–588. doi: 10.1037//0021-843x.111.4.578. [DOI] [PubMed] [Google Scholar]
- United Nations. The world’s women. 2010 http://unstats.un.org/unsd/demographic/products/Worldswomen/WW_full%20report_color.pdf Retrieved December 30, 2015.
- United Nations Development Programme. Human Development Report 2005. 2005 Retrieved from http://hdr.undp.org/en/content/human-development-report-2005.
- **.University of Ghana Medical School, Department of Community Health. Ghana: Study on global AGEing and adult health (SAGE), Wave 1. Geneva: World Health Organization; 2013. [Google Scholar]
- *.Van de Velde S, Bracke P, Levecque K. Gender differences in depression in 23 European countries: Cross-national variation in the gender gap in depression. Social Science & Medicine. 2010;71(2):305–313. doi: 10.1016/j.socscimed.2010.03.035. [DOI] [PubMed] [Google Scholar]
- Van de Velde S, Huijts T, Bracke P, Bambra C. Macro-level gender equality and depression in men and women in Europe. Sociology of Health and Illness. 2013;35(5):682–698. doi: 10.1111/j.1467-9566.2012.01521.x. [DOI] [PubMed] [Google Scholar]
- *.van Praag L, Bracke P, Christiaens W, Levecque K, Pattyn E. Mental health in a gendered context: Gendered community effect on depression and problem drinking. Health Place. 2009;15(4):990–998. doi: 10.1016/j.healthplace.2009.04.003. [DOI] [PubMed] [Google Scholar]
- Vevea JL, Woods CM. Publication bias in research synthesis: Sensitivity analysis using a priori weight functions. Psychological Methods. 2005;10:428–443. doi: 10.1037/1082-989X.10.4.428. [DOI] [PubMed] [Google Scholar]
- **.Vicente B, Kohn R, Rioseco P, Saldivia S, Levav I, Torres S. Lifetime and 12-month prevalence of DSM-III-R disorders in the Chile psychiatric prevalence study. American Journal of Psychiatry. 2006;163(8):1362–1370. doi: 10.1176/appi.ajp.163.8.1362. [DOI] [PubMed] [Google Scholar]
- *.Villatoro JA, Medina-Mora ME, Juarez F, Rojas E, Carreno S, Berenzon S. Drug use pathways among high school students of Mexico. Addiction. 1998;93(10):1577–1588. doi: 10.1046/j.1360-0443.1998.9310157715.x. [DOI] [PubMed] [Google Scholar]
- **.Volken T. Second-stage non-response in the Swiss health survey: determinants and bias in outcomes. BMC Public Health. 2013;13:167. doi: 10.1186/1471-2458-13-167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.von Soest T, Wichstrom L. Secular trends in depressive symptoms among Norwegian adolescents from 1992 to 2010. J Abnorm Child Psychol. 2014;42(3):403–415. doi: 10.1007/s10802-013-9785-1. [DOI] [PubMed] [Google Scholar]
- **.Wade TJ, Cairney J, Pevalin DJ. Emergence of gender differences in depression during adolescence: National panel results from three countries. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41(2):190–198. doi: 10.1097/00004583-200202000-00013. [DOI] [PubMed] [Google Scholar]
- *.Walker L, Merry S, Watson PD, Robinson E, Crengle S, Schaaf D. The Reynolds Adolescent Depression Scale in New Zealand adolescents. Australian and New Zealand Journal of Psychiatry. 2005;39:136–140. doi: 10.1080/j.1440-1614.2005.01534.x. [DOI] [PubMed] [Google Scholar]
- *.Wang J, Iannotti RJ, Luk JW, Nansel TR. Co-occurrence of victimization from five subtypes of bullying: Physical, verbal, social exclusion, spreading rumors, and cyber. Journal of Pediatric Psychology. 2010;35(10):1103–1112. doi: 10.1093/jpepsy/jsq048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ware JE, Sherbourne CD. The MOS Short-Form Health Survey (SF-36): I. Conceptual framework and item selection. Medical Care. 1992;30(6):473–483. [PubMed] [Google Scholar]
- Weissman MM, Klerman GL. Sex differences and the epidemiology of depression. Archives of General Psychiatry. 1977;34:98–111. doi: 10.1001/archpsyc.1977.01770130100011. [DOI] [PubMed] [Google Scholar]
- *.Wichstrom L. The emergence of gender difference in depressed mood during adolescence: the role of intensified gender socialization. Developmental Psychology. 1999;35(1):232–245. [PubMed] [Google Scholar]
- Wilson DB. Practical Meta-Analysis Effect Size Calculator [Online calculator] Retrieved May 1, 2014 from https://www.campbellcollaboration.org/this-is-a-web-based-effect-size-calculator/explore/this-is-a-web-based-effect-size-calculator.
- Wilson DB. Meta-analysis macros for SAS, SPSS, and Stata. 2006 Retrieved May 1, 2015 from http://mason.gmu.edu/~dwilsonb/ma.html.
- **.Wittchen HU, Carter RM, Pfister H, Montgomery SA, Kessler RC. Disabilities and quality of life in pure and comorbid generalized anxiety disorder and major depression in a national survey. International Clinical Psychopharmacology. 2000;15(6):319–328. doi: 10.1097/00004850-200015060-00002. [DOI] [PubMed] [Google Scholar]
- Wittchen HU, Pfister H. DIA-X-Interviews:ManualfürScreening-Verfahren und Interview;InterviewheftLängsschnittuntersuchung(DIA-X-Lifetime);Er- gänzungsheft (DIA-X-Lifetime);InterviewheftQuerschnittuntersuchung(DIA- X-12Monate);Ergänzungsheft(DIA-X-12Monate);PC-ProgrammzurDurch- führung desInterviews(Längs-undQuerschnittuntersuchung) Auswertung- sprogrammSwetsundZeitlinger; Frankf: 1997. [Google Scholar]
- Wittchen HU, Robins LN, Cottler LB, Sartorius N, Burke JD, Regier D. Cross-cultural feasibility, reliability and sources of variance of the Composite International Diagnostic Interview. British Journal of Psychiatry. 1991;159:645–653. doi: 10.1192/bjp.159.5.645. [DOI] [PubMed] [Google Scholar]
- Wood W, Eagly AH. Biosocial construction of sex differences and similarities in behavior. Advances in Experimental Social Psychology. 2012;46:55–123. [Google Scholar]
- World Bank. GINI index. 2004 http://data.worldbank.org/indicator/SI.POV.GINI?page=2&order=wbapi_data_value_2011%20wbapi_data_value%20wbapi_data_value-first&sort=asc Retrieved December 30, 2015.
- World Health Organization. Composite International Diagnostic Interview (CIDI), version 1.0. Geneva: World Health Organization; 1990. [Google Scholar]
- World Health Organization. The ICD-10 classification of mental and behavioural disorders: Clinical descriptions and diagnostic guidelines. Geneva: World Health Organization; 1992. [Google Scholar]
- World Health Organization. Composite International Diagnostic Interview, Version 2.1. Geneva: World Health Organization; 1997. [Google Scholar]
- World Health Organization. World Health Survey. 2002 < http://www.who.int/healthinfo/survey/en/index.html>.
- World Health Organization. Out of the shadows: Making mental health a global development priority. 2016 http://www.who.int/mental_health/advocacy/wb_background_paper.pdf?ua=1 Retrieved November 26, 2016.
- World Values Survey. Wave 4, 1999–2004. 2014 Retrieved from http://www.worldvaluessurvey.org/WVSDocumentationWV4.jsp, December 30, 2015.
- *.Yamada K, Teerawichitchainan B. Living Arrangements and Psychological Well-Being of the Older Adults After the Economic Transition in Vietnam. J Gerontol B Psychol Sci Soc Sci. 2015;70(6):957–968. doi: 10.1093/geronb/gbv059. [DOI] [PubMed] [Google Scholar]
- Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, Leirer VO. Development and validation of a geriatric depression screening scale: A preliminary report. Journal of Psychiatric Research. 1982;17(1):37–49. doi: 10.1016/0022-3956(82)90033-4. [DOI] [PubMed] [Google Scholar]
- *.Zemore SE, Karriker-Jaffe KJ, Mulia N. Temporal trends and changing racial/ethnic disparities in alcohol problems: Results from the 2000 to 2010 National Alcohol Surveys. Journal of Addiction Research and Therapy. 2013;4 doi: 10.4172/2155-6105.1000160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zentner M, Mitura K. Stepping out of the caveman’s shadow: Nations’ gender gap predicts degree of sex differentiation in mate preferences. Psychological Science. 2012;23:1176–1185. doi: 10.1177/0956797612441004. [DOI] [PubMed] [Google Scholar]
- **.Zhao W, Chen Y, Lin M, Sigal RJ. Association between diabetes and depression: Sex and age differences. Public Health. 2006;120(8):696–704. doi: 10.1016/j.puhe.2006.04.012. [DOI] [PubMed] [Google Scholar]
- Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatrica Scandinavica. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- **.Zinzow HM, Ruggiero KJ, Resnick H, Hanson R, Smith D, Saunders B, Kilpatrick D. Prevalence and mental health correlates of witnessed parental and community violence in a national sample of adolescents. Journal Child Psychology & Psychiatry. 2009;50(4):441–450. doi: 10.1111/j.1469-7610.2008.02004.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **.Zubrick SR, Hafekost J, Johnson SE, Lawrence D, Saw S, Sawyer M, Buckingham WJ. Suicidal behaviours: Prevalence estimates from the second Australian Child and Adolescent Survey of Mental Health and Wellbeing. Australian and New Zealand Journal of Psychiatry. 2016;50(9):899–910. doi: 10.1177/0004867415622563. doi: http://dx.doi.org/10.1177/00048674156. [DOI] [PubMed] [Google Scholar]
- *.Zunzunegui MV, Minicuci N, Blumstein T, Noale M, Deeg D, Jylha M, Pedersen NL. Gender differences in depressive symptoms among older adults: a cross-national comparison: the CLESA project. Social Psychiatry and Psychiatric Epidemiology. 2007;42(3):198–207. doi: 10.1007/s00127-007-0158-3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


