Abstract
Objective
We compared an infrared temporal artery thermometer with our clinical standard axillary thermometer for temperature measurements in neonatal patients.
Study Design
We measured temporal artery (Tta), axillary (Tax, clinical standard), and rectal (Tr, gold standard) temperatures of 49 infants. The difference between Tr and Tta was compared with that between Tr and Tax, and the data were analyzed based on bed type and postmenstrual age.
Results
The mean Tta, Tax, and Tr were 37.16 (SD 0.36) °C, 36.61 (SD 0.30) °C, and 36.82 (SD 0.30) °C, respectively. The measurements by these methods were all significantly different. The mean Tr-Tax was 0.21 (SD 0.26) °C, and the mean Tr-Tta was −0.34 (SD 0.37) °C, indicating that Tax was closer to Tr than was Tta (p < 0.0001). Tta agreed more closely with Tr for infants in cribs than for those in incubators. Adjusting for bed type and body weight, with each week of postmenstrual age, the discrepancy between Tr-Tta and Tr-Tax decreased by 0.005°C (p = 0.034).
Conclusion
Compared with the gold standard, Tr, Tta is not more accurate than Tax. The temporal artery thermometer was less accurate for infants in incubators than for infants in cribs. The accuracy of temporal artery temperature increased with postmenstrual age.
Keywords: temporal artery temperature, axillary temperature, rectal temperature, neonate, infant
Accurate monitoring of body temperature is important in caring for preterm and critically ill newborn infants. These infants generally have reduced thermoregulatory capacity, and their caregivers have little margin for error in providing a protective thermal environment. Rectal thermometers are quite accurate as a reflection of core temperature but have been largely abandoned in most hospitals because of safety concerns.1–4 Axillary thermometers are thought to be sufficiently accurate and safer than rectal thermometers for small infants.5 The electronic axillary thermometer is the current clinical standard for monitoring temperature in most neonatal intensive care units and newborn nurseries. However, axillary thermometry also has its drawbacks. As with rectal temperature measurement, axillary temperature measurement requires repositioning and partial disrobing of the infant. This maneuver may alter vital signs and impair gastric emptying but, most important, it triggers a drop in body temperature. The temporal artery thermometer, a new device, allows estimation of core temperature in a few seconds by directing the probe in a sweep from the center of the forehead to the hairline.6 The thermometer detects thermal radiation emitted from the skin and displays the highest temperature found. If shown to be accurate, the infrared temporal artery thermometer offers an appealing alternative to axillary and rectal thermometers in infants, as it is less disturbing for the patient and more efficient for the health care provider.
Both the accuracy and reliability of a thermometer are crucial in a vulnerable population, for whom temperature management can affect outcome. With the goal of identifying the best thermometry method for clinical use in preterm and critically ill neonates, we set out to investigate the accuracy of the infrared temporal artery thermometer.
Methods
Measurements were taken from patients in the neonatal intensive care unit and newborn nursery at the University of Iowa Children's Hospital from May through August 2014. All infants with birth weight greater than 500 g cared for in incubators or in open, unheated cribs (or bassinets) were eligible except those with anal atresia, central nervous system malformation, hypoxic-ischemic encephalopathy, or clinical concerns for necrotizing enterocolitis or other bowel injury or discontinuity. The infant's sex, gestational age, and the postnatal age, body weight, and bed type on the day of study were recorded from the patient's medical record.
Temperature measurements were performed simultaneously (within 2 minutes) for each infant using three methods: (1) temporal artery temperature (Tta) using an infrared temporal artery thermometer (Model TAT-5000, Exergen Corporation, Watertown, MA); (2) axillary temperature (Tax) using a digital electronic thermometer (Model MDS9656, Medline Industries, Mundelein, IL); and (3) rectal temperature (Tr) using a soft, flexible, vinyl-covered thermistor probe (Model EW-08432-00, Cole-Parmer, Vernon Hills, IL, equivalent to YSI model 402). Room air temperature (Tair) was measured with an air temperature thermistor probe (Model EW-08438–00, Cole-Parmer, Vernon Hills, IL, equivalent to YSI model 405). The rectal and air thermistor probes were attached to a two-channel electronic thermometer (Model 4000A, YSI Inc., Yellow Springs, OH). The rectal probe was calibrated by InnoCal (Vernon Hills, IL, a division of Thermo Fisher Scientific), which issued a calibration report traceable to the National Institute of Standards and Technology. In addition, the probe was calibrated between 30° and 40°C in a water bath against a long-stem mercury-in-glass thermometer traceable to the National Institute of Standards and Technology.
The infant was placed in a supine position and unclothed before temperatures were measured. Methods for obtaining the temporal artery temperature (Tta) were based on the Exergen Model TAT-5000 reference manual's instructions for infants.6 The TAT-5000 probe was covered with a probe cap and placed on the center of the infant's forehead, midway between the eyebrow and hairline. Holding the scan button, the thermometer was moved toward the left hairline. The thermometer was removed at the infant's ear. Two Tta measurements were taken and averaged. Immediately following the Tta measurements, temperature was measured in the left axilla (Tax) using the clinical standard electronic thermometer, and rectal temperature (Tr) was recorded using the thermistor probe.5 Axillary temperature was measured at the warmest point in the axilla, by placing the thermometer tip in the apex halfway between the anterior and posterior margins of the axilla.7 The infant's arm was held against its body until the thermometer beep indicated the measurement was complete, and the thermometer was then removed. The rectal probe was coated with petroleum jelly, inserted to a depth of 5 cm (5 cm × body weight in kg for infants < 1 kg) into the rectum,8 and held in place until the temperature reading was stable. The rectal temperature was considered the most accurate approximation of core body temperature, the “gold standard.” The same investigator measured the temporal artery temperature and axillary temperature of every infant. A trained research nurse or neonatologist performed the rectal temperature measurements. Room air temperature was recorded during the measurements of body temperature for each patient.
After each measurement, the temporal artery thermometer probe cap and rectal thermistor probe were cleaned with a hospital-approved bleach solution followed by an alcohol solution. The probe cap and rectal thermistor probe were wiped down with alcohol and air-dried before each measurement. Infants in incubators had their temperature measured through the portholes to minimize heat loss.
Bland-Altman analysis was used to assess agreement of temporal artery and axillary temperature measurements with rectal temperature measurement.9,10 The differences between rectal and axillary and rectal and temporal artery temperatures were first tested for normal distribution. The difference between rectal and temporal artery temperatures was compared with that between rectal and axillary temperatures also using two-tailed t tests for paired observations. These temperature differences were compared for all patients together. In addition, the analyses were performed separately for each type of thermal environment: incubator and open crib. Multivariable linear regression analysis was performed to examine the impact of postmenstrual age and weight of the infant at time of measurement on the relative accuracy of temporal artery and axillary temperatures. The target sample size of 44 infants was chosen to allow detection of a mean difference between the rectal-axillary temperature gradient (Tr-Tax) and the rectal-temporal artery gradient (Tr-Tta) of 0.5 standard deviation at a significance level (α) of 0.05 and a power (1-β) of 0.90. We intended to enroll at least 12 infants in each of the four gestational age groups: extremely preterm (< 28 weeks), moderately preterm (28–32 weeks), late preterm (33–36 weeks), and full-term (≥ 37 weeks)—to allow detection of a mean difference between Tr-Tax and Tr-Tta of 1 standard deviation at a significance level (α) of 0.05 and a power (1-β) of 0.80. A sample of at least 12 infants in a given type of thermal environment, open crib or incubator, also provides 80% power to detect a mean difference between Tr-Tax and Tr-Tta of 1 standard deviation or greater. The study was approved by the institutional review board of the University of Iowa, and written informed consent was obtained from a parent of each participating infant. The study was in full compliance with the World Medical Association Declaration of Helsinki regarding the ethical conduct of research involving human subjects.
Results
Forty-nine infants were studied (Table 1). Their median gestational age was 34 weeks. At the time of study, their median age was 11 days, and their median weight was 2,235 g. Twenty-two infants were studied in incubators, and 27 were studied in open cribs.
Table 1. Patient characteristics.
| No. of patients | 49 |
| Sex, male, number (%) | 26 (53.1%) |
| Gestational age (wk), median (range) | 34 (25–40) |
| Study age (d), median (range) | 11 (1–78) |
| Study weight (g), median (range) | 2,235 (1,160–4,205) |
| Bed type | |
| Incubator, air temperature control | 15/49 |
| Incubator, skin temperature control | 7/49 |
| Crib | 27/49 |
The mean temporal artery, axillary, and rectal temperatures for all 49 infants were 37.16 (SD 0.36) °C, 36.61 (SD 0.30) °C, and 36.82 (SD 0.30) °C, respectively (Table 2). The mean Tr-Tax was 0.21 (SD 0.26) °C, and the mean Tr-Tta was −0.34 (SD 0.37) °C, indicating that Tax was closer statistically to Tr than was Tta(p < 0.0001). These relationships were also examined separately for infants in incubators and those in open cribs.
Table 2. Temperature measurements (°C).
| Tta | Tax | Tr | Tair | Tr–Tta | Tr–Tax | |
|---|---|---|---|---|---|---|
| Mean | 37.16 | 36.61 | 36.82 | 23.80 | −0.34 | 0.21 |
| SD | 0.36 | 0.30 | 0.30 | 0.95 | 0.37 | 0.26 |
| Median | 37.20 | 36.60 | 36.85 | 23.70 | −0.30 | 0.20 |
| IQR | 36.90–37.45 | 36.40–36.80 | 36.60–37.00 | 23.05–24.35 | −0.60–0.10 | 0.00–0.40 |
Abbreviations: IQR, interquartile range; SD, standard deviation; Tr, rectal temperature; Tta, temporal artery temperature; Tax, axillary temperature; Tair, room air temperature.
The mean temporal artery, axillary, and rectal temperatures for infants in incubators (n = 22) were 37.29 (SD 0.36) °C, 36.68 (SD 0.29) °C, and 36.88 (SD 0.32) °C, respectively (Table 3). The mean Tr-Tta was −0.40 (SD 0.34) °C, and the mean Tr-Tax was 0.20 (SD 0.20) °C, indicating that Tax was closer to Tr than was Tta (p < 0.0001), and the bias was in opposite directions (Figs. 1, 2). The 95% prediction limits for rectal and temporal artery temperatures (Tr-T ta) were −1.28°C and +0.55°C, and the difference and limits decreased with increasing body temperature, although this decrease in slope was not significant (p = 0.173 by simple linear regression F test) (Fig. 1). The 95% prediction limits for rectal and axillary temperatures (Tr-Tax) were −0.30°C and +0.75°C (Fig. 2); these values did not change with body temperature. The mean temporal artery, axillary, and rectal temperatures for infants in cribs (n = 27) were 37.03 (SD 0.30) °C, 36.55 (SD 0.31) °C, and 36.78 (SD 0.30) °C, respectively. The mean Tr-Tta was −0.24 (SD 0.37) °C, and the mean Tr-Tax was +0.23 (SD 0.31) °C, again indicating that Tax was closer statistically to Tr than was Tta (p < 0.0001). Tr-Tta was significantly larger for the infants in incubators than for those in open cribs (−0.40°C vs. −0.24°C, p = 0.027), indicating that the temporal artery temperature was farther from the gold standard rectal temperature for infants in incubators. We interpret this to mean that the temporal artery thermometer was less accurate when used within an incubator compared with an open crib. Adjusting for bed type and weight, with each increasing week of postmenstrual age, the discrepancy between Tr-Tta and Tr-Tax decreased by 0.005°C (p = 0.034). The mean Tair was 23.80°C (SD 0.95).
Table 3. Impact of bed type on temperature measurements (°C).
| Tta | Tax | Tr | Tr–Tta | Tr–Tax | |
|---|---|---|---|---|---|
| Incubator (n = 22), mean (SD) | 37.29 (0.36) | 36.68 (0.29) | 36.88 (0.32) | −0.40 (0.34) | 0.20 (0.20)a |
| Open crib (n = 27), mean (SD) | 37.03 (0.30) | 36.55 (0.31) | 36.78 (0.30) | −0.24 (0.37) | 0.23 (0.30)a |
Abbreviations: SD, standard deviation; SEM, standard error of the mean; Tr, rectal temperature; Tta, temporal artery temperature; Tax, axillary temperature.
Significantly different from Tr–Tta (p < 0.0001).
Fig. 1.
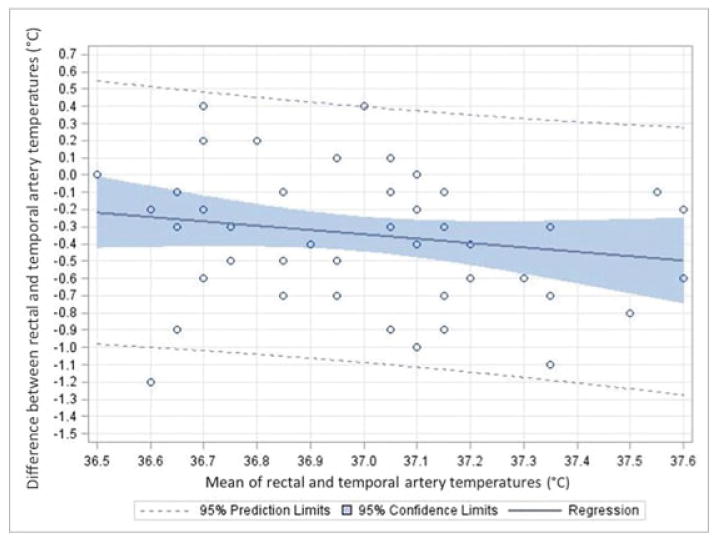
Bland-Altman plot of rectal and temporal artery temperatures (°C) recorded in 49 hospitalized newborn infants. On the y-axis is the difference between the temperatures and on the x-axis is the mean value of the temperatures. The solid line indicates the regression line and the shaded area the 95% confidence limit. The dotted line indicates the upper 95% prediction limit.
Fig. 2.
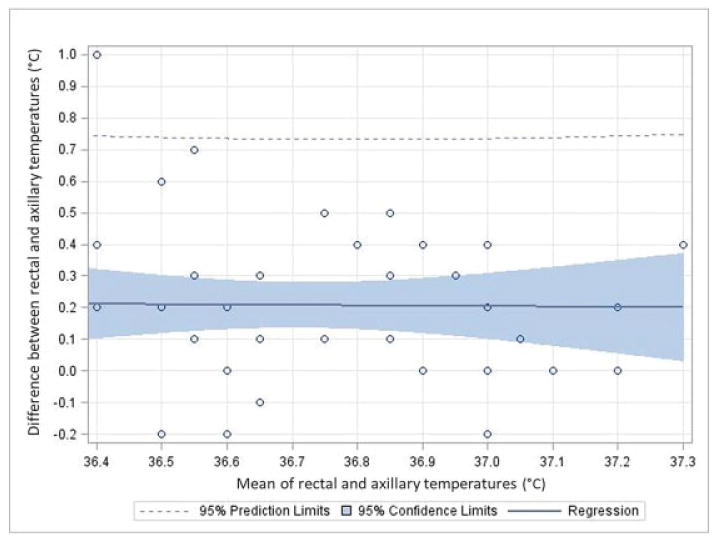
Bland-Altman plot of rectal and axillary temperatures (°C) recorded in 49 hospitalized newborn infants. On the y-axis is the difference between the temperatures and on the x-axis is the mean value of the temperatures. The solid line indicates the regression line and the shaded area the 95% confidence limit. The dotted line indicates the upper 95% prediction limit.
Discussion
Various methods of estimating core temperature in neonates have been investigated as alternatives to rectal thermometry because of concerns for the risk of rectal perforation.1–4 Previous studies have found that axillary temperature is an acceptable alternative,5 and this method is widely used in practice. Yet the axillary thermometer requires undressing the infant, and having the thermometer held in the axilla presumably causes some degree of discomfort.
Measurement of tympanic membrane temperature with a soft thermistor probe provides a good estimation of core temperature,11 but the procedure is difficult and possibly uncomfortable. Infrared tympanic thermometry has been evaluated in neonates but with conflicting results concerning accuracy.12–14 A systematic review comparing the accuracy of infrared ear thermometry to rectal thermometry in children did not find good agreement between the two methods.15
The temporal artery thermometer offers advantages that neither the rectal nor axillary thermometer provides. A health care provider can access the forehead without undressing the infant. Temporal artery temperature measurement is quick and prevents added heat loss and sleep disruption.
While the accuracy of temporal artery thermometers has been examined in adults and older children, few studies have investigated the accuracy and reliability of this method in neonates.16–20 Duran and coworkers16 compared temporal artery with axillary temperature measurements in 34 very-low-birth-weight infants; they found that the mean temperature was higher by 0.1°C and pain scores were lower with temporal artery measurement. Lee and collaborators17 studied 34 moderate and late preterm or term infants, recording simultaneously measured temporal artery and axillary temperatures and infant discomfort scores. They found similar temperatures with the two methods but lower discomfort scores with temporal artery temperature measurement. Haddad et al18 recorded temporal artery and axillary temperatures in 125 healthy term or near-term newborns and found temporal artery temperature to be, on average, 0.2°C higher than axillary temperature; although this difference was statistically significant, it was not considered to be clinically significant. Jarvis et al19 compared two temporal artery thermometers with measurements from an axillary thermometer. One of the temporal artery thermometers gave readings that were acceptably close to axillary temperature; the other (an Exergen temporal artery thermometer) did not.19 Sim et al20 compared 661 paired clinical measurements of temporal artery and axillary temperatures in 169 hospitalized term and preterm infants (mean gestational age 36 weeks) in different nursing environments. The mean temporal artery temperature (measured with the Thermo-flash LX-26 Evolution thermometer) was higher in all environments but was closest to axillary temperature in infants nursed in open cribs and farthest above axillary temperature in infants housed in incubators.20 The impact of maturity, that is, postmenstrual age on the accuracy of the temporal artery thermometer, has not been previously explored. It is important to understand the effects of these variables, as they may alter the reliability of measurements performed with the temporal artery thermometer.
We found that the temporal artery thermometer reads on average 0.3°C higher than the rectal thermometer, whereas the axillary thermometer reads on average 0.2°C lower than the rectal thermometer. This difference in accuracy of 0.1°C is not clinically significant, but it is important to understand that the difference from Tr is in opposite directions with Tta and Tax. The standard deviation for Tr-Tta was 0.37°C whereas the standard deviation for Tr-Tax was 0.26°C. This difference suggests that the gradient between rectal and temporal artery temperatures is less consistent from patient to patient than the gradient between rectal and axillary temperatures. To determine whether the temporal artery thermometer might be adopted for standard clinical use in neonatal units, the next step would be to further investigate the reproducibility of measurements with this device within and between health care providers.
Temporal artery measurements were closer to rectal measurements for infants in open, unheated cribs as compared with infants in incubators, suggesting that the temporal artery thermometer functions more accurately in ambient air than in the heated, enclosed environment of the incubator. This finding is in agreement with the study by Jarvis et al.19 Limitations of our study included the failure to allow thermal equilibration of the temporal artery thermometer when used to measure the temperature of infants in incubators. The manufacturer recommends allowing equilibration of the device to the measuring environment for at least 20 minutes.6 For the sake of expediency and representation of how the device would likely be used in practice, this recommendation was not followed; as a result, the temporal artery temperature measurements performed in incubators may have been less accurate than they would have been given sufficient time for thermal equilibration. Future studies should investigate the accuracy of the temporal artery thermometer in incubators after the 20-minute period recommended by the manufacturer. Another limitation was our failure to vary the order of measurements; however, all measurements were completed for a given infant within a 2-minute window, and the temporal artery temperature was measured first because it did not require exposing additional skin.
The accuracy of the temporal artery temperature measurements increased significantly with increasing postmenstrual age. Based on these results, neonates in noncritical care units seem to be more appropriate candidates for the use of the temporal artery thermometer, as they are usually in open cribs or bassinets and generally have more advanced postmenstrual age. The consistency of the temporal artery temperature measurements within and between users should be investigated further as well as its accuracy when used in incubators.
Acknowledgments
The authors thank the patients who participated and their parents, who granted consent for their participation. The authors thank Frank H. Morriss, Jr., MD, for advice about the Bland-Altman analysis. Ms. Syrkin-Nikolau was supported by a summer research fellowship from the University of Iowa Carver College of Medicine, which was funded by NIH grant T35 HL007485. This work was also supported by grant UL1 RR024979, awarded from the NIH to support the University of Iowa Institute for Clinical and Translational Science. The temporal artery thermometer was purchased by the investigators and not provided by the manufacturer, who had no knowledge of the study or its results.
Footnotes
Conflict of Interest: None.
References
- 1.Segnitz RH. Accidental transanal perforation of the rectum: an obscure cause of peritonitis in infancy and childhood. AMA J Dis Child. 1957;93(3):255–258. doi: 10.1001/archpedi.1957.02060040257010. [DOI] [PubMed] [Google Scholar]
- 2.Fonkalsrud EW, Clatworthy HW., Jr Accidental perforation of the colon and rectum in newborn infants. N Engl J Med. 1965;272:1097–1100. doi: 10.1056/NEJM196505272722104. [DOI] [PubMed] [Google Scholar]
- 3.Frank JD, Brown S. Thermometers and rectal perforations in the neonate. Arch Dis Child. 1978;53(10):824–825. doi: 10.1136/adc.53.10.824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lau JT, Ong GB. Broken and retained rectal thermometers in infants and young children. Aust Paediatr J. 1981;17(2):93–94. doi: 10.1111/j.1440-1754.1981.tb01912.x. [DOI] [PubMed] [Google Scholar]
- 5.Mayfield SR, Bhatia J, Nakamura KT, Rios GR, Bell EF. Temperature measurement in term and preterm neonates. J Pediatr. 1984;104(2):271–275. doi: 10.1016/s0022-3476(84)81011-2. [DOI] [PubMed] [Google Scholar]
- 6.Exergen Corporation. Watertown, MA: Exergen Corporation; [Accessed March 21, 2017]. Model TAT-5000 Reference Manual. p/n 818528 r5. undated. http://www.exergen.com/medical/PDFs/TAT5000Manualr5-5rev-ecl.pdf. [Google Scholar]
- 7.Abrams RM, Royston JP, Humphrey SJ, Wolff HS. Thermal features of the female axilla. J Appl Physiol. 1980;49(6):1042–1046. doi: 10.1152/jappl.1980.49.6.1042. [DOI] [PubMed] [Google Scholar]
- 8.Karlberg P. The significance of depth of insertion of the thermometer for recording rectal temperatures. Acta Paediatr. 1949;38:359–366. [Google Scholar]
- 9.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1(8476):307–310. [PubMed] [Google Scholar]
- 10.Giavarina D. Understanding Bland Altman analysis. Biochem Med (Zagreb) 2015;25(2):141–151. doi: 10.11613/BM.2015.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mayfield SR, Nakamura KT, Bhatia J, Rios GR, Bell EF. Tympanic membrane temperature of term and preterm neonates. Early Hum Dev. 1984;9(3):241–247. doi: 10.1016/0378-3782(84)90034-3. [DOI] [PubMed] [Google Scholar]
- 12.Johnson KJ, Bhatia P, Bell EF. Infrared thermometry of newborn infants. Pediatrics. 1991;87(1):34–38. [PubMed] [Google Scholar]
- 13.Weiss ME. Tympanic infrared thermometry for fullterm and preterm neonates. Clin Pediatr (Phila) 1991;30(4, Suppl):42–45. doi: 10.1177/0009922891030004S12. discussion 49. [DOI] [PubMed] [Google Scholar]
- 14.Weiss ME, Poeltler D, Gocka I. Infrared tympanic thermometry for neonatal temperature assessment. J Obstet Gynecol Neonatal Nurs. 1994;23(9):798–804. doi: 10.1111/j.1552-6909.1994.tb01955.x. [DOI] [PubMed] [Google Scholar]
- 15.Craig JV, Lancaster GA, Taylor S, Williamson PR, Smyth RL. Infrared ear thermometry compared with rectal thermometry in children: a systematic review. Lancet. 2002;360(9333):603–609. doi: 10.1016/S0140-6736(02)09783-0. [DOI] [PubMed] [Google Scholar]
- 16.Duran R, Vatansever Ü, Acunaş B, Süt N. Comparison of temporal artery, mid-forehead skin and axillary temperature recordings in preterm infants <1500 g of birthweight. J Paediatr Child Health. 2009;45(7-8):444–447. doi: 10.1111/j.1440-1754.2009.01526.x. [DOI] [PubMed] [Google Scholar]
- 17.Lee G, Flannery-Bergey D, Randall-Rollins K, et al. Accuracy of temporal artery thermometry in neonatal intensive care infants. Adv Neonatal Care. 2011;11(1):62–70. doi: 10.1097/ANC.0b013e3182087d2b. [DOI] [PubMed] [Google Scholar]
- 18.Haddad L, Smith S, Phillips KD, Heidel RE. Comparison of temporal artery and axillary temperatures in healthy newborns. J Obstet Gynecol Neonatal Nurs. 2012;41(3):383–388. doi: 10.1111/j.1552-6909.2012.01367.x. [DOI] [PubMed] [Google Scholar]
- 19.Jarvis M, Guy KJ, König K. Accuracy of infrared thermometers in very low birth weight infants and impact on newborn behavioural states. J Paediatr Child Health. 2013;49(6):471–474. doi: 10.1111/jpc.12207. [DOI] [PubMed] [Google Scholar]
- 20.Sim MA, Leow SY, Hao Y, Yeo CL. A practical comparison of temporal artery thermometry and axillary thermometry in neonates under different environments. J Paediatr Child Health. 2016;52(4):391–396. doi: 10.1111/jpc.13107. [DOI] [PubMed] [Google Scholar]


