Abstract
Interest in the knowledge of salivary gland tumours is highlighted. A sample of 315 cases, collected over a period of 25 years in a busy pathology centre, is analysed both on total and individual aspects of tumours. The findings are compared to earlier works on the subject and also with contemporary literature.
KEY WORDS: Pathological study, Salivary tumours
Introduction
Tumours of salivary glands have continually interested the medical profession, pathologists in particular because of a number of peculiarities of the subject. These peculiarities are: (i) their diverse histological forms (ii) unpredictable clinical behaviour (iii) and different opinions expressed by several workers of long experience on different aspects of these tumours. In developing countries like India, where malnutrition is still a reckonable ill of society, these tumours are said to be commoner, their locations are rather more unusual, and their vulnerability to malignancy is more than in developed countries [1, 2]. Incidence of salivary gland tumours has been reported differently by several workers in this field. It is estimated at 0.5 to 2 percent of all neoplasia [3, 4, 5]. Overall incidence of these tumours in different geographical locations is substantially the same except in Canada, where the condition is unusually prevalent in excess among Eskimos [6]. Location wise, Parotid gland is involved in about eighty percent (80%) of salivary tumours, however it is reported that the Chinese origin Malaysians show great preponderance for submandibular glands [1], Ugandans over palate [2] and people of West Indies over the sublingual and minor salivary glands [7]. However a number of Indian authors have recorded the incidence of parotid gland involvement at a lower level viz. fifty percent (50%) [8] and sixty four percent (64%) [10]. About twelve percent of all salivary gland tumours arise in the lachrymal gland and the mucous glands of the inner surface of the upper lip, palate, base and borders of tongue, nasopharynx, larynx and accessory nasal sinuses [11, 12].
Diversities of phenomenology of tumours of salivary glands are best illustrated by the fact that till date several classifications have been attempted. Starting from Ewing 1928 [13], there have been at least six such attempts to encompass the whole subject, till Thackray and Sobin [14] gave a histological typing on behalf of WHO (Geneva WHO 1972). Though this classification is currently being followed by majority of centres, this is not the end of it. Many queries are still to be cleared. As late as 1988 a fresh classification was brought out by Ellis and Gnepp, 1988 [15] and which is currently being followed by the Armed Forces Institute of Pathology (AFIP) [16]. This classification brings out 10 varieties of benign tumours and 18 types of malignant tumours. Such is the diversity of the subject.
Histogenesis of the salivary tumours still remains elusive. Several hypothesis have been postulated to cover the varied histological picture. At last Crumpler et al, 1976, [17] after a brilliant study with electron microscopy, tissue culture and histochemistry have shown that in the myxomatous and chondromatous areas of the mixed tumours are mostly myoepithelial cells. The matter is still open for further studies.
In view of the diversities of these tumours in different aspects, it was thought that a larger sample for study on the subject, with both retrospective as well as prospective analysis will be a useful addition to the current knowledge in this field.
Material and Methods
Sample of the study covered:
-
a)
all the cases worked on in the Department of Pathology, Medical College, Jabalpur (M.P), India, during 1967 to 1990, i.e. for a period of 23 years. Paraffin embedded tissue sections, kept in the Histology Section, along with records of these surgically resected tumours, was the material for retrospective analysis. Total number of such cases was 306.
-
b)
Six cases from the same department and three cases from Military Hospital, Jabalpur, obtained from surgical sections during one year period, 01 April 91 to 31 March 92, i.e. a total of 9 cases was the material for prospective analysis. Thus the total material for study was 315 cases. All these cases were studied in detail as regards their clinical, morphological and histological features.
-
i)Clinical study covered particulars of subjects, their age, sex, duration of growth and associated clinical features.
-
ii)Morphological characteristics of the tumour were recorded under the following headings: size, consistency, external appearance
-
iii)Histological studies were done by microscopic study of Haematoxylene and Eosin stained tissue sections as per standard procedure. Special stains were used as and when necessary. Histological classification of these tumours was done as per classification criteria of WHO (1972) [14].
-
i)
Observations
As mentioned earlier, this study covers a period of 23 years (1967–1990). During this period a total number of 33, 109 neoplastic specimens were received by the department. Salivary neoplasms numbered 315, constituting 0.95 percent of all neoplastic specimens. Of the total salivary tumours, 192 (61%) were benign tumours while 123 (39%) were malignant (Table-1 shows frequency of occurrence of different types of tumour).
TABLE 1.
Frequency of tumours (n=315)
| Type of tumour | Number | Percent |
|---|---|---|
| Pleomorphic adenoma | 150 | 47.60 |
| Monomorphic adenoma | 019 | 06.00 |
| Adenolymphoma | 014 | 04.50 |
| Oncocytoma | 001 | 00.31 |
| Haemangioma | 008 | 02.52 |
| Adenoid cystic carcinoma | 042 | 13.30 |
| Mucoepidermoid carcinoma | 026 | 08.26 |
| Carcinoma in Pleomorphic adenoma | 015 | 04.80 |
| Epidermoid carcinoma | 017 | 05.40 |
| Adenocarcinoma | 012 | 03.81 |
| Acinic cell carcinoma | 006 | 01.90 |
| Undifferentiated carcinoma | 005 | 01.60 |
| Total | 315 | 100.00 |
In the benign group the largest number was Pleomorphic adenoma (47.60%) and in the malignant, the Adenoid cystic carcinoma (13.30%) was the largest.
Location wise parotid tumours were 243 accounting for 77 percent of the total, submandibular 28 (9%) 2 cases in sublingual gland and 42 cases in minor salivary glands (14%). Preponderance of malignancy was more in minor salivary glands:24 out of 42, making 51% of the total. However, in parotid and submandibular the malignant tumours were 85 out of 243 (30%) and 9 out of 28 cases (32%) respectively. Right sided tumours were slightly more (54.6%) than left sided (45.4%).
A large number of cases (58) of benign tumours was found in the third decade followed by 54 cases in the fourth decade. Malignancy was maximum in the fifth decade. Average age for benign case was 35.5 years while for malignancy it was 47.5 years.
Females had slight preponderance of 54.3 percent in benign conditions while males were slightly more in malignant cases (52.8%). Haemangioma occurred in the smaller age group (average age 24 years). Mucoepidermoid carcinoma also occurred relatively in younger age groups (average age 28.5 years). For the rest of the tumours average age varied from 35.5 to 44 years.
Majority, 264 (84%) cases presented as swellings of common clinical type; 51 cases presented rather differently and the clinical presentation and diagnosis were varied, 28 cases were diagnosed clinically with lymph gland involvement, 21 cases were diagnosed as lymph adenitis and 2 cases as secondaries till histology confirmed the nature of the pathology, 4 cases presented as abscess, 2 fistula, 2 diagnosed as nasal polyp and 2 as ulcer tongue/palate. 8 patients were diagnosed as cysts-dermoid/sebaceous over different areas, 4 presented as carcinoma of maxillary antrum and 1 as carcinoma cheek.
Duration of the tumours varied for benign and malignant, minimum duration for benign tumours was 1½ years while for malignant cases duration was less (1 year). Maximum duration for benign was 8 years and for malignant 2½ years.
Clinico pathological details of different varieties of tumours are vast to incorporate in a short paper.
However a short picture of the common types will be quite appropriate. Of the benign growths, adenomas form a large majority. Pleomorphic adenomas were 150 and monomorphic adenomas were 19, together constituting 169 out of 315 making 54%. Histological features of mixed tumours exhibit extremely diverse structural pattern (Fig. 1). Table 2 shows various histological pattern.
Fig. 1.
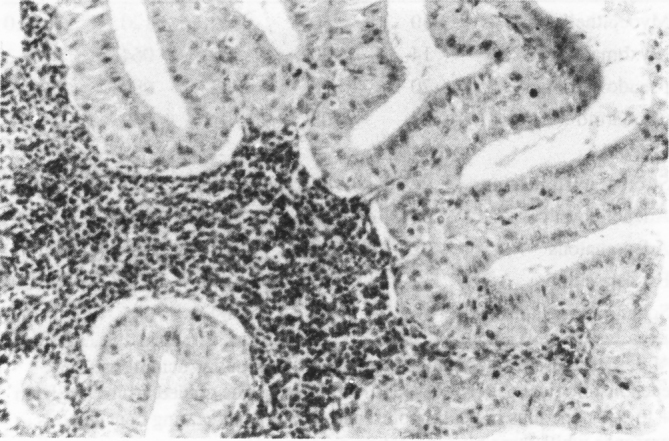
Warthins tumour showing classical lymphoid tissue surrounding which are epithelial and myoepithelial cells of salivary gland
TABLE 2.
Histological pattern of mixed tumours*
| Histological pattern |
Intensity of occurrence |
Total |
Percentage |
||
|---|---|---|---|---|---|
| + | ++ | +++ | |||
| Myoepithelial | 40 | 50 | 30 | 120 | 80.0 |
| Myxomatous | 14 | 20 | 30 | 064 | 42.3 |
| Pseudo cartilage | 20 | 48 | 22 | 090 | 60.0 |
| Chondroid | 03 | 05 | 01 | 009 | 06.0 |
| Osteoid | − | − | − | − | − |
| Stromal hyalinization | 06 | 07 | 02 | 015 | 10.0 |
| Adenoid cystic | 08 | 08 | 07 | 023 | 15.0 |
| Adenomatous | 02 | 04 | 02 | 008 | 05.0 |
| Fat deposition | 12 | 14 | 07 | 033 | 22.0 |
| Squamous metaplasia | 16 | 20 | 09 | 045 | 30.0 |
In order to assess the relative frequency of various structural patterns; each histological pattern present in the tumour was graded arbitrarily from + to +++, one plus indicating presence, two plus indicating conspicuous presence while three plus indicating prominence.
In the malignant group, common varieties were adenoid cystic carcinoma (42 cases; 13.30%), mucoepidermoid carcinoma (26 cases; 8.26%) (Fig. 2). Carcinoma in pleomorphic adenoma (15 cases; 4.80%) (Fig. 3) and epidermoid carcinoma (17 cases;5.40%). A few words about the tumours of minor salivary glands would be appropriate since in the present study there were 42 cases making 13.33 percent of the total sample. 24 of the cases (57.2%) turned out to be malignant. This was statistically significant. Commonest site of occurrence was cheek and commonest carcinoma was Adenoid Cystic variety. Details of site of occurrence are given in Table 3.
Fig. 2.
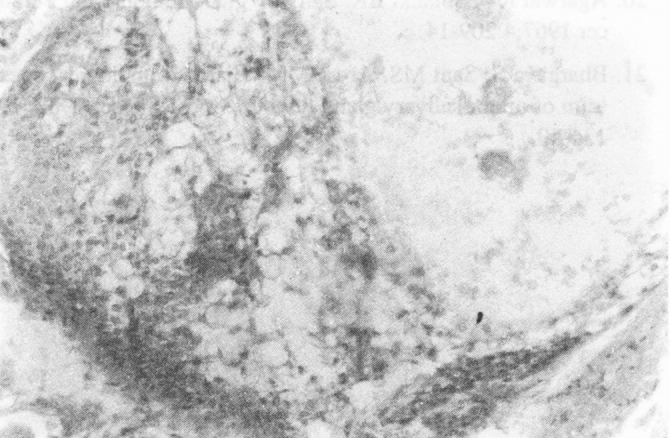
Mucoepidermoid carcinoma of parotid gland showing epidermoid and mucoid elements
Fig. 3.
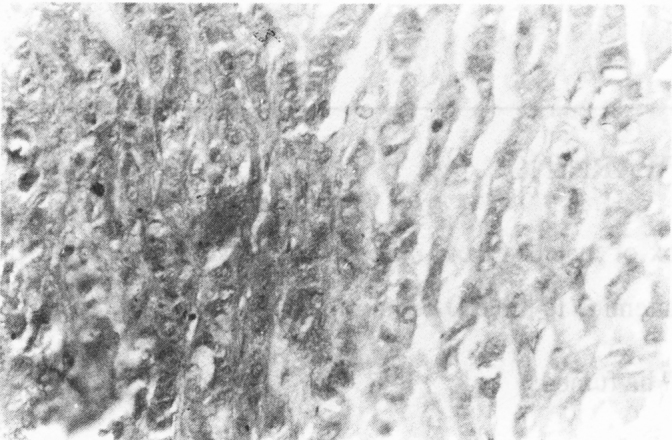
Carcinoma in pleomorphic adenoma. Note the abrupt change to hyperchromatic nuclei with mitotic figures
TABLE 3.
Site of occurrence – minor salivary gland tumours
| Type of tumour | Palate | Cheek | Tongue | Floor of Mouth | Lip | Nose | Max antrum | Tonsils | Larynx | Alveolar margin |
|---|---|---|---|---|---|---|---|---|---|---|
| Pleomorphic adenoma | 3 | 7 | 2 | − | 1 | − | − | 3 | 2 | − |
| Adenoid cystic carcinoma | 4 | 6 | 1 | − | − | 1 | 3 | − | − | 1 |
| Mucoepidermoid carcinoma | − | 1 | − | 1 | − | − | 1 | − | − | − |
| Acinic cell tumour | − | − | − | − | − | − | − | − | − | 1 |
| Adenocarcinoma | − | 1 | − | − | − | 1 | − | − | − | − |
| Epidermoid CA | − | 1 | − | − | − | − | − | − | − | − |
| CA in pleomorphic adenoma | − | − | − | − | − | − | − | 1 | − | − |
Discussion
Though salivary gland tumours have always interested pathologists, their overall incidence vis a vis total tumour occurrence is rather small. A survey of the incidence in different countries indicates more or less similar pattern, though in one work [1] it is more than others.
Strictly speaking the incidence recorded is only of those tackled by one centre of pathology and not necessarily the occurrence in the population at large; however the figures certainly give an idea of their frequency of occurrence.
Regarding occurrence of different types of histological patterns, there are variations, as expected; However preponderance of some types viz. pleomorphic adenoma, mucoepidermoid carcinoma and adenoid cystic carcinoma is universal. One of the reasons of variation is authors outlook at classification. Present work was based on WHO system, which is authentic and agreed upon by most centres. Table 4 gives an overview of the different types of salivary tumours in different works. [18, 19, 20, 21].
TABLE 4.
Histological varieties of salivary tumours in various series (in percent)
| Type of tumour | Sirsat (1953) | Davies (1964) | Singh (1968) | Banerjee (1973) | Khazanchi (1988) | Panda et al (1969) | Agarwal et al (1967) | Bhargawa, et al (1982) | Present 1992 |
|---|---|---|---|---|---|---|---|---|---|
| Pleomorphic adenomas | 56.20 | 62.00 | 58.50 | 64.00 | 56.50 | 61.20 | 66.00 | 52.00 | 47.60 |
| Monomorphic adenoma | − | − | 1.06 | 4.00 | − | − | − | 2.30 | 6.03 |
| Adenolymphoma | 2.40 | − | − | 2.00 | 7.80 | − | − | 1.30 | 4.40 |
| Oncocytoma | − | − | − | 4.00 | − | 1.20 | − | 1.30 | 0.30 |
| Haemangioma | − | − | − | − | − | − | − | 3.00 | 2.40 |
| Acinic cell CA | − | − | − | 2.00 | 3.00 | 1.20 | − | 1.30 | 1.80 |
| Mucoepidermoid CA | 10.70 | 21.70 | 9.00 | 5.00 | 11.30 | 10.60 | 9.50 | 3.00 | 8.20 |
| Adenocarcinoma | − | 14.70 | 15.90 | − | 3.40 | 2.30 | 7.50 | 12.60 | 3.60 |
| Adenoidcystic CA | 12.40 | − | 2.12 | 6.00 | 5.60 | 10.60 | 7.50 | 14.00 | 13.30 |
| CA in pleomorphic adenoma | − | 1.60 | 9.00 | 4.00 | 5.60 | 3.50 | 6.00 | 1.30 | 4.60 |
| Undifferentiated CA | − | − | 11.10 | − | 3.40 | 3.60 | 3.40 | 5.80 | 1.30 |
| Squamous cell CA | − | 14.70 | 3.90 | − | 3.40 | 4.70 | 3.50 | 4.00 | 6.10 |
| Carcinomas | 19.00 | − | − | 7.00 | − | − | − | − | − |
Since there were 42 cases of tumours of minor salivary glands in the present series, a comparison of the sites involved with other significant works will be quite appropriate, for which Table 5 is given [21].
TABLE 5.
Comparison of site involvement in minor salivary glands
| Author | Year | Alveolar Margin | Palate | Cheek | Tongue | Floor of mouth | Lip | Nose | Max antrum | Tonsils | Larynx |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Bhargava and Sant (Total cases 85) | (1982) | − | 19 | 6 | 15 | 4 | 4 | 6 | 23 | 3 | 5 |
| Present series (Total cases 42) | (1992) | 2 | 7 | 16 | 3 | 1 | 1 | 2 | 4 | 4 | 2 |
Comparison of age of occurrence of salivary gland tumours between present work and earlier series does not show gross difference. In benign cases the age of occurrence was slightly lower.
Regarding sex incidence, present work figures are comparable with western authors where females had slight preponderance (54.38%) over males for benign growth, while males were slightly more (52.8%) in malignant series.
Present series of 315 cases studied over a period of 23 years is one of the largest work on the subject and possibly the latest incorporating the WHO classification. A look at the different Indian workers will be justified. (Table-6).
TABLE 6.
Comparison of other Indian works
| Authors | Year | Total sample |
|---|---|---|
| Sirsat | 1953 | 121 |
| Deshpandey | 1955 | 109 |
| Agrawal | 1967 | 147 |
| Panda | 1969 | 085 |
| Budhraja | 1974 | 056 |
| Banerjee | 1974 | 111 |
| Sinha | 1975 | 154 |
| Bhargava | 1982 | 300 |
| Khazanchi | 1988 | 088 |
| Present | 1992 | 315 |
Salivary gland tumour is a subject of considerable interest because of its not very uncommon occurrence, varied histology and its characteristic clinical features. Present work is possibly the largest collection published so far in India and hence will be a useful addition to the present knowledge on the subject. Unlike different norms of classification adopted by earlier workers, in this series the tumours have been classified on the lines recommended by WHO (1972).
References
- 1.Marsden ATH. Distinctive features of tumours of salivary glands in Malaya. Br J Cancer. 1951;5:375. doi: 10.1038/bjc.1951.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Davies JP. Salivary gland tumours in Uganda. Cancer. 1964;17:1310–1322. doi: 10.1002/1097-0142(196410)17:10<1310::aid-cncr2820171014>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 3.Frazell EL. Clinical aspects of tumours of major salivary glands. Cancer. 1954;7:637. doi: 10.1002/1097-0142(195407)7:4<637::aid-cncr2820070403>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 4.AC. Thackray 1968; Quoted by Evans and Cruickshank
- 5.Willis RA. Pathology of Tumours. Butter Worths. 1960 [Google Scholar]
- 6.Wallace AC. Salivary gland tumours in Canadian Eskimos. Cancer. 1963;16:1338–1353. doi: 10.1002/1097-0142(196310)16:10<1338::aid-cncr2820161015>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 7.Gore DO, Harland A. Tumours of salivary gland origin. Surg Gynae Obst. 1964;119:1290. [PubMed] [Google Scholar]
- 8.Kalra VB, Lodha SK, Sareen PM, Utreja SR. Benign mixed salivary tumours. Ind J Surg. 1982;44:498. [Google Scholar]
- 10.Panda PK, Agarwal S. Tumours of salivary glands. Ind J Cancer. 1962;6:82. [PubMed] [Google Scholar]
- 11.Ackermann LV. Epithelial tumours of lachrymal glands. Am J Surg. 1962;104:657. doi: 10.1016/0002-9610(62)90414-2. [DOI] [PubMed] [Google Scholar]
- 12.Zimmermann LE. Epithelial tumours of lachrymal glands. Am J Surg. 1962;104:667. doi: 10.1016/0002-9610(62)90414-2. [DOI] [PubMed] [Google Scholar]
- 13.Ewing J. Diseases Neoplastic 4th ed. WB Saunders; Philadelphia: 1940. [Google Scholar]
- 14.Thackray AC, Sobin LH. Histological typing of salivary gland tumours. International histological classification of tumours (WHO Geneva) 1972;7 [Google Scholar]
- 15.Ellis GL, Gnepp DR. Pathology Head and Neck 1988. Churchill Livingston; New York: 1988. [Google Scholar]
- 16.Thackray AC, Lucos RB. Atlas of Tumour pathology. Washington Armed Forces Institute of Pathology: Fascicle 10. 1974 [Google Scholar]
- 17.Crumpler C, Scharrenberrg C, Reed J. Monomorphic adenoma of salivary glands. Cancer. 1976;38:193–200. doi: 10.1002/1097-0142(197607)38:1<193::aid-cncr2820380130>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 18.Sirsat MV. Salivary gland tumours. Ind Surg. 1953;15:123. [Google Scholar]
- 19.Khazanchi RK, Saha SS, Mittal D, Dhawan IK. Tumours of Parotid glands-A review of 86 patients and current methods of treatment. Ind J Cancer. 1988;25:1. [PubMed] [Google Scholar]
- 20.Agarwal RV, Solanki BR. Salivary gland tumours. Ind J Cancer. 1967;4:209–214. [PubMed] [Google Scholar]
- 21.Bhargava S, Sant MS, Arora MM. Histomorphological spectrum of minor salivary gland tumours. Ind J Cancer. 1982;19:134–140. [PubMed] [Google Scholar]
UNCITED REFERENCE
- 9.Singh S, Mehdiratta KS, Satyanand D. A study of salivary gland tumours. Ind J Surg. 1968;30:193. [Google Scholar]


