Dear Editor,
Propriospinal myoclonus (PSM) is characterized by jerks arising in axial muscles that spread to more caudal and rostral segments along propriospinal pathways. PSM at sleep onset is a subtype of PSM that occurs during the sleep-awake transition and causes severe sleep-onset insomnia.1 Previous case reports have focused on the etiology and mechanism of PSM, but have not evaluated treatment responses objectively. Moreover, most treatments have only employed clonazepam.1 We present a patient with PSM at sleep onset who improved after treatment with clonazepam and add-on levetiracetam. The improvement was confirmed by serial video polysomnography (VPSG).
Case presentation
A 52-year-old woman presented with a 10-year history of repetitive, involuntary flexor jerks of the trunk, neck, and limbs before falling sleep, which were enhanced in a supine position. These jerks resulted in the patient experiencing difficulty falling asleep and complaining of excessive daytime sleepiness. The findings of a neurologic examination were normal, and laboratory test results were within normal limits. An electrophysiological evaluation consisting of an electroencephalogram and evoked-potential studies and spinal magnetic resonance imaging also did not reveal any significant abnormalities.
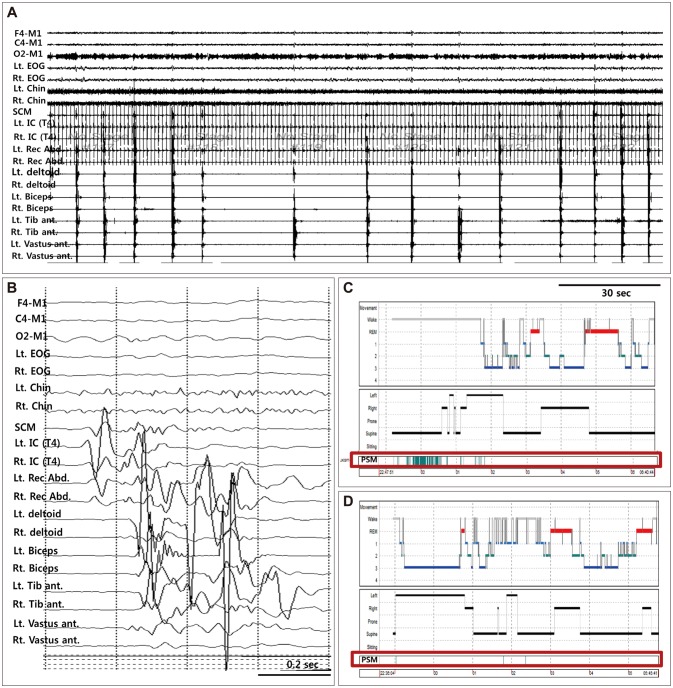
The patient underwent overnight VPSG with multiple surface electromyography (EMG). Initial VPSG showed spontaneous jerks starting in the left intercostalis muscle and spreading to the rectus abdominis, deltoid, and biceps, lasting for 400–600 ms (Fig. 1A and B) and with propagation velocities of 6–10 m/s. In total, 109 myoclonic events were observed during a drowsy state and light sleep, which prevented the patient from falling asleep. The movement was diminished in the lateral position and disappeared during N2, N3, and REM sleep (Fig. 1C). Sleep latency was prolonged to 152 minutes and sleep efficacy was decreased to 59.2%.
Fig. 1. Polysomnographic recordings and hypnograms. A: Polysomnographic recording with polymyography. B: Recording of a single jerk. C: Hypnogram of initial video polysomnography (VPSG). D: Hypnogram of follow-up VPSG performed 1 month after initiating levetiracetam. The red box indicates a propriospinal myoclonus (PSM) event.
Clonazepam was initiated at 0.25 mg/day and later increased to 0.5 mg/day, which reduced the frequency of the jerks. However, even with clonazepam use, the patient still complained of myoclonic activity preceding sleep. Levetiracetam (500 mg/day) was therefore added 4 months later, which nearly abolished the jerks. Follow-up VPSG was performed 1 month after the initiation of levetiracetam therapy using surface EMG electrodes. Only three myoclonic events were observed throughout the study (Fig. 1D). The sleep latency was normalized (10.5 minutes) and sleep efficacy was improved to 82.6%.
Discussion
The patient exhibited myoclonic jerks of axial muscles that slowly propagated from the thoracic level, consistent with PSM.2 Treatment of PSM with clonazepam and levetiracetam significantly reduced the number of myoclonic events and improved sleep efficacy.
Clonazepam enhances GABAergic neurotransmission by modulating benzodiazepine receptors and is most commonly used in patients with spinal myoclonus.3 It is considered a first-line therapy for PSM at sleep onset, but it has been found to be effective in only half of the published case reports.2 Our patient also showed only partial improvement after using clonazepam. Levetiracetam is mostly used to control cortical myoclonus, but it has also been reported to be effective in several patients with segmental spinal myoclonus.4 Its mechanism of action is thought to be related to modulation of glycine inhibitory neurotransmitters. It does not affect GABAergic neurotransmission, but it may modulate the release of several neurotransmitters by binding synaptic vesicle protein 2A.3 In addition, levetiracetam may reduce excitation of the spinal generator by modulating Ca and K currents.
The present case is the first to suggest that a combination of clonazepam and levetiracetam exerts synergistic effects in treating PSM at sleep onset.
Footnotes
Conflicts of Interest: The authors have no financial conflicts of interest.
References
- 1.Vetrugno R, Provini F, Meletti S, Plazzi G, Liguori R, Cortelli P, et al. Propriospinal myoclonus at the sleep-wake transition: a new type of parasomnia. Sleep. 2001;24:835–843. [PubMed] [Google Scholar]
- 2.van der Salm SM, Erro R, Cordivari C, Edwards MJ, Koelman JH, van den Ende T, et al. Propriospinal myoclonus: clinical reappraisal and review of literature. Neurology. 2014;83:1862–1870. doi: 10.1212/WNL.0000000000000982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Caviness JN. Treatment of myoclonus. Neurotherapeutics. 2014;11:188–200. doi: 10.1007/s13311-013-0216-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Keswani SC, Kossoff EH, Krauss GL, Hagerty C. Amelioration of spinal myoclonus with levetiracetam. J Neurol Neurosurg Psychiatry. 2002;73:457–458. doi: 10.1136/jnnp.73.4.457. [DOI] [PMC free article] [PubMed] [Google Scholar]