Abstract
Objective
To describe the publication productivity of academic urologists in the United States by gender.
Materials and Methods
Gender inequality is prevalent in most surgical subspecialties, including urology. Despite small numbers of women in academic positions, differences in scholarly impact by gender are relatively unknown. We assembled a list of 1922 academic urologists (1686 male (87.7%), 236 female (12.3%)) at 124 academic institutions throughout the United States as of February 2016. Scopus and Google Scholar were queried for bibliometric data on each individual, including h-index and m-quotient. We analyzed these metrics for both genders by educational background, subspecialty, NIH funding, and academic rank.
Results
Men had higher median h-indices than women overall (p<0.05), and by successive academic ranks (p<0.05). Proportionally fewer women attained senior academic ranking (professor/chair), (p<0.05). There was no difference in research productivity by successive rank after controlling for career duration (m-quotient). Women were more likely to choose a practice that specialized in pediatric urology or female urology/pelvic reconstructive surgery than their male counterparts (p<0.05).
Conclusions and Relevance
Women represent a growing proportion of academic urology faculty, but despite the recent increase in number entering the field, relatively few women occupy senior leadership positions. Improving psychosocial barriers to advancement such as lack of mentorship or discriminatory policies may help pioneering female urologists as they progress in their careers.
Keywords: h-index, academic urology, bibliometrics, citation impact, Scopus, Google Scholar, gender differences, academic rank, publication productivity, career duration, NIH funding
Introduction
Women in surgery, and particularly in urology, remain a significant minority despite medicine’s closing gender gap.1, 2 According to 2015 American Urologic Association (AUA) census data, there are just 922 practicing female urologists nationwide, accounting for 7.7% of all practitioners.2 However, in recent years, women have been selecting careers in urology at an increasing rate. By 2050, it is predicted that approximately 28% of practicing urologists will be women.1 This increase in the number of women entering urology represents substantial progress toward equality, but we have yet to see equalization of academic rank.
For women that do enter surgical academic practice, relatively few ever attain senior leadership positions.3–5 Teaching duties, clinical productivity, and administrative functions contribute to faculty member evaluations, but scholarly output is heavily weighted in decisions regarding individual promotion in academic medicine. Female urologists over the course of their careers publish at a rate that exceeds their relative number in the field,6 suggesting that female academic rank is not reflective of their academic output. This discordance between academic rank and lifetime publication productivity for female urologists deserves more attention.
Several medical specialties have utilized bibliometric analysis to examine gender differences in publication output and other related factors, but this approach has not yet been applied to urology.7–9 This study seeks to investigate the gender imbalance in scholarly output in academic urology using bibliometrics. By highlighting any disparities, we hope to encourage discussion of barriers to a woman’s academic success and promote systematic change so that women with aspirations in urology have equal opportunity for prolific careers as leaders in the field.
Methods
Bibliometrics
The most commonly used objective indicator for research productivity is the Hirsch index (h-index), calculated using an author’s publications where N papers have at least N citations. For example, an author with 10 publications cited at least 10 times will have an h-index of 10. Because citation number is accounted for with this metric, the h-index represents both a quantitative and qualitative measure of a researcher’s output. One limitation of the h-index is its inherent temporal bias when using the metric to compare individuals. Investigators engaged in publication activities for a longer period of time will have more opportunities to publish, and publications that have been in circulation longer will have more opportunity to be cited. The m-quotient is a potential correction for the h-index’s inherent dependence on time by mitigating the effects of differing career lengths when comparing the h-indices of multiple authors (m=h/n, where h is the h-index, and n is the years since an author’s first publication). This study uses the h-index and m-quotient to examine gender differences in academic urology.
Data collection
We assembled a list of 128 accredited U.S. urology residency programs from the Accreditation Council for Graduate Medical Education (ACGME, 2015–2016). We then used institutional websites to compile a database of academic urologists. Information on academic rank, educational background, sub-specialty (if mentioned), and gender were recorded (websites accessed January to February 2016). We only included faculty members with an MD, DO, or MD/DO + PhD degree who held an appointment within the department/division of urology and completed a urology residency training program or trained in obstetrics/gynecology and now specialize in Female Urology/Pelvic Reconstructive Surgery. Four military programs were excluded from analysis because they lacked sufficient physician information. Academic rank was categorized as chair, professor, associate professor, assistant professor, and instructor (defined as clinical instructor, staff clinician, or unspecified faculty listing). Gender was imputed from extant data (names, photographs, and biographic descriptions).
Institutional review board approval was not required as the data is publicly available and subjects were not contacted. For each urologist listed in our database we performed a custom search string using author search functions in both Scopus Google Scholar to retrieve bibliometric data, including h-index, m-quotient, and date of first urology publication. In cases where an author’s name was common and yielded multiple results, we used information on educational background, institutional affiliations, and publication subject (urology-related) to assign individual publications to an author. Where possible, both the current surname and maiden name were used to determine metrics for female faculty. Year of first publication was used as a proxy for inception of career in our calculation of academic career length (calculated by subtracting year of first publication from current year, 2016). The h-index and m-quotient from Scopus and Google Scholar databases were averaged for a combined h-index and m-quotient, which we used for all analyses. Previous studies report reasonably good concordance rates in h-index values between the two databases.10, 11 Finally, we accessed the NIH Research Portfolio Online Reporting Tools Web site in order to procure data on research funding using the Principal Investigator (PI)/Project Leader function.
Statistical Analysis
Mann-Whitney U tests and Kruskal-Wallis tests were used for comparison of continuous variables and Pearson chi-square test was used for comparison of categorical variables. All statistical analyses were done using SAS (SAS Institute Inc., Cary, NC) with two-sided p<0.05 considered statistically significant.
Results
Overall, 1922 urology faculty members from 124 academic institutions were included for analysis. Of these, 236 (12%) were women and 1686 (88%) were men. The h-index, m-quotient, career duration as well as number of faculty with PhDs and NIH funding stratified by gender and academic rank are listed in Table 1. The h-index for urology faculty by academic rank is displayed in Figure 1. As expected, h-index increased with ascending academic rank (p<.0001). The difference in h-index between department chair and professor was not significant (p=0.18). The career duration for all faculty members was also calculated and stratified by academic rank.
Table 1.
Academic Productivity Metrics, Career Duration, and National Institutes of Health (NIH) Funding for Urology Faculty by Gender and Academic Position, 2016a
| Position and gender | No. (%) | h-index, median (range)a | Career duration in years, median (range)a | m-quotient, median (range)a | PhD, no. (%)a | NIH funded, no. (%)a |
|---|---|---|---|---|---|---|
| Chair/Chief | 129 | 26.3 (2–109) |
28 (8–46) |
0.97 (0.07–2.97) |
4 (3.1%) |
15 (11.6%) |
| Men | 126 (97.67%) |
26.3 (2–109) |
28 (10–46) |
0.97 (0.07–2.97) |
1 (3.1%) |
15 (11.6%) |
| Women | 3 (2.33%) |
37.7 (4–43) |
27 (8–32) |
1.19 (0.50–1.50) |
0 (0%) |
0 (0%) |
|
| ||||||
| Professor | 466 | 25.7 (0–112) |
30 (4–46) |
0.88 (0–6.38) |
19 (4.1%) |
37 (7.9%) |
| Men | 441 (94.64%) |
26.3 (0–112)b |
31 (4–46)b |
0.88 (0–6.38) |
18 (3.9%) |
34 (7.3%) |
| Women | 25 (5.36%) |
20.7 (4–45)b |
24 (9–45)b |
0.79 (0.26–1.69) |
1 (0.2%) |
3 (0.6%) |
|
| ||||||
| Associate Professor | 361 | 13.3 (0–56) |
19 (1–54) |
0.68 (0–2.82) |
17 (4.7%) |
22 (6.1%) |
| Men | 315 (87.26%) |
13.7 (0–56)b |
20 (1–54)b |
0.68 (0–2.82) |
15 (4.2%) |
19 (5.3%) |
| Women | 46 (12.74%) |
10.5 (0–28)b |
14 (7–42)b |
0.65 (0–1.46) |
2 (0.6%) |
1 (0.8%) |
|
| ||||||
| Assistant Professor | 744 | 5.7 (0–55) |
13 (1–62) |
0.44 (0–2.95) |
18 (2.4%) |
10 (1.3%) |
| Men | 603 (81.05%) |
6.0 (0–55)b |
14 (1–62)b |
0.43 (0–2.75) |
15 (2.0%) |
9 (1.2%) |
| Women | 141 (18.95%) |
4.7 (0–35)b |
11 (1–46)b |
0.46 (0–2.95) |
3 (0.4%) |
1 (0.1%) |
|
| ||||||
| Instructor | 222 | 3.0 (0–61) |
19 (2–52) |
0.18 (0–2.96) |
2 (0.9%) |
5 (2.3%) |
| Men | 201 (90.54%) |
3.0 (0–61) |
19 (2–52) |
0.19 (0–2.96) |
2 (0.9%) |
5 (2.3%) |
| Women | 21 (9.46%) |
2.7 (0–26) |
17 (4–45) |
0.14 (0–1.27) |
0 (0%) |
0 (0%) |
|
| ||||||
| Total | 1922 | 10.3 (0–112) |
20 (1–62) |
0.58 (0–6.38) |
60 (3.1%) |
89 (4.6%) |
| Men | 1686 (87.72%) |
11.7 (0–112)b |
22 (1–62)b |
0.60 (0–6.38)b |
54 (2.8%) |
82 (4.3%) |
| Women | 236 (12.28%) |
6.3 (0–45)b |
13 (1–46)b |
0.50 (0–2.95)b |
6 (0.3%) |
7 (0.4%) |
h-index for 1922 MD, MD/DO, or MD/DO + PhD faculty at 124 academic urology institutions as reported by Scopus (Elsevier BV, Amsterdam, The Netherlands). The career duration was calculated as the number of years from first reported publication to 2016. m-quotient was calculated by dividing the h-index by the career duration. Whether or not the faculty member had a PhD was determined from departmental and individual physician website. NIH funding was determined using the NIH research portfolio Online Reporting Tools (RePORTER) website.
p < 0.05 for comparison of men versus women for that same column.
Figure 1.
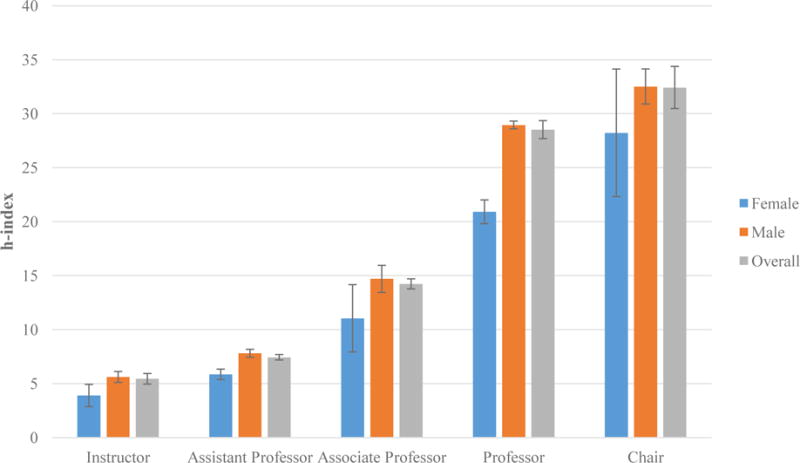
Mean h-index for 1922 academic urologists from 124 institutions according to academic rank. Error bars represent standard error of sample mean.
Gender comparison by category
Academic rank
The gender distribution by academic rank is displayed in Figure 2A. Men were more likely to occupy senior academic positions, i.e. professor and department chair (p<.0001). Women were not represented in higher academic positions proportional to their numbers in the field as a whole (Figure 2B). There were only 3 female chairs (1.3% of female urologists) versus 126 male chairs (7.5% of male urologists). There were 25 female professors (11% of female urologists) versus 441 male professors (26% of male urologists).
Figure 2.
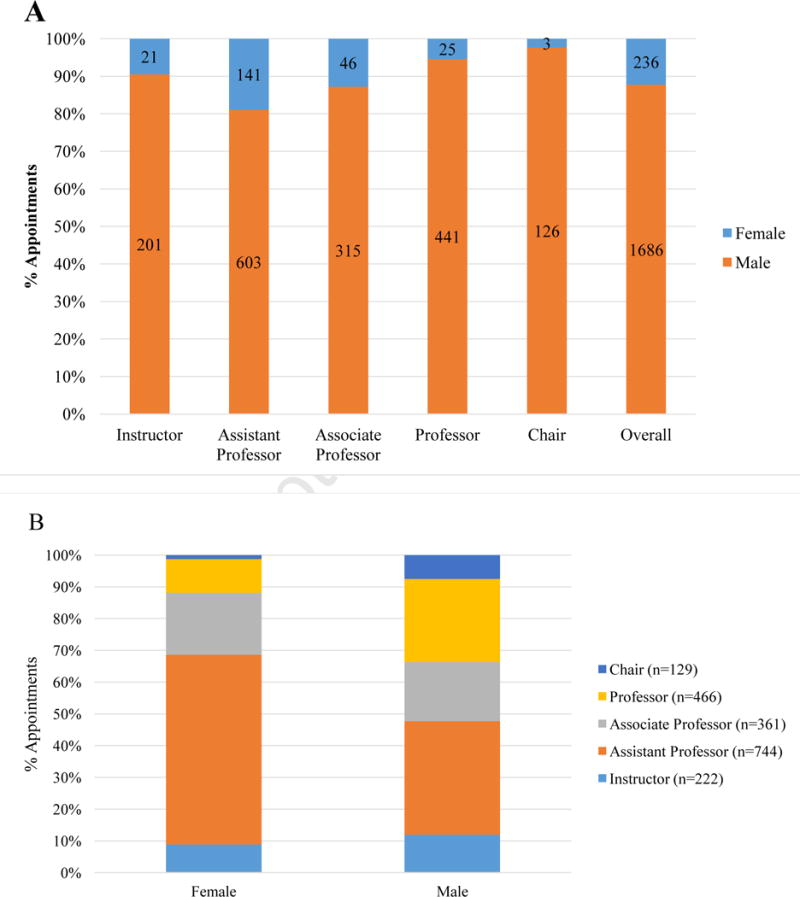
(A) Gender distribution of 1922 academic urologists from 124 institutions according to academic rank. Data labels represent number of faculty members for each gender respectively. (B) Academic rank representation by gender.
Specialty choice
Subspecialty choice was significantly different between genders (p <.0001). Men were more likely to choose General Urology (p= 0.0022) or Urologic Oncology (p<.0001) as their subspecialty. Women were more likely to choose Female Pelvic Medicine and Reconstructive Surgery (p <.0001) or Pediatric Urology (p <.0001). There was no gender difference in Andrology or Stone Disease and Advanced Endourology (p=0.0763 and p=0.0734, respectively). These patterns largely remained even after examining distributions over time where we compared subspecialty for those who had been in academia for over 10 years with those who had just begun their careers (career duration <10 years). The one exception was in in General Urology, there was no difference in gender for those with less than 10 years of experience (p=0.2453).
Publication productivity
The overall median h-index was 10.33, and men had a higher median h-index (11.67) than women (6.33), p<.0001. When organized by academic rank, there were also significant differences between gender for the same position (Figure 1). The h-indices for men were higher than those for women in every rank. The differences were statistically significant at the assistant (p= 0.02), associate (p=0.01), and professorship level (p=0.03). Because there were only 3 female chairs, statistical significance was not assessed. Similarly, the overall median m-quotient for men was higher at 0.60 than for women at 0.50 (p=0.0054). However, the differences in m-quotient between genders were not significant when stratified by academic rank.
NIH Funding and PhD status
Although more men (4.27%) received NIH funding than women (0.36%), the difference was not statistically significant (p= 0.2462). Similarly, there was not a significant difference in the number of faculty members who had obtained PhDs (p= 0.6930).
Career duration
Overall, men had a longer median career duration as measured by years since first research publication: 22.00 (range: 1–62) versus 13.00 (range: 1–46), (p <.0001). At every academic rank, men had a longer career duration (Table 1). h-indices were evaluated with regard to the length of research career (Figure 3). Gender differences were largest for individual in mid-career (21–30 years). Women in this range had a mean h-index of 14.59 and men had a mean h-index of 21.21 (p=0.0257). For urologists with less than 30 years of experience, men had a higher mean h-index than women (p<.0001). This difference in h-index by duration disappeared for faculty with greater than 30 years of active research activity (p= 0.5242) or less than 10 years (p=0.5242). There were only 16 women with more than 30 years of experience.
Figure 3.
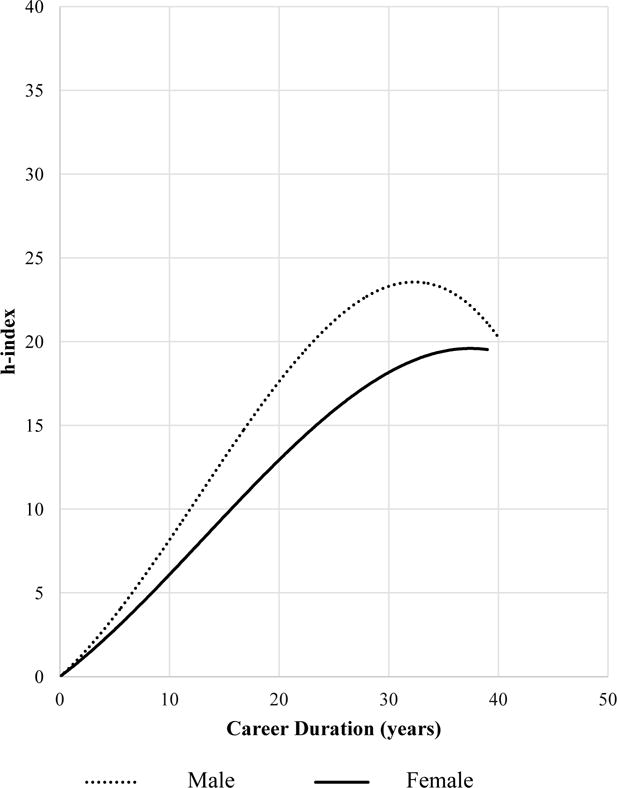
Chart of h-index plotted against career duration for 1922 academic urologists. Slope of the curve represents the rate of publication productivity. Note: The difference in h-index by gender at 10-year intervals is only significant for faculty with 11 to 20 years of experience (p=0.0019) and 21 to 30 years of experience (p=0.0257).
Discussion
Our study demonstrates that there are significant differences in academic ranking, subspecialty choice, and publication productivity by gender within academic urology. Women are disproportionately under-represented in senior leadership positions, more likely to subspecialize in certain fields, and have different publication profiles overall compared to men. However, there was no difference in research productivity by successive rank after controlling for career duration (m-quotient). So, when women achieve a certain academic rank, they are just as productive as their male counterparts, and differences in h-index are largely driven by longer careers of male urologists. The rapidly changing demographics within academic urology provide a unique opportunity for analysis of women’s barriers to academic advancement.
Gender Discrepancies in Medicine
Despite modest progress in recent years, women remain underrepresented in academic medicine as full-time faculty and in leadership positions.12, 13 This problem is magnified in surgical fields where women have traditionally made up a smaller portion of the workforce. Studies in gastroenterology, otolaryngology, ophthalmology, and radiation oncology have confirmed a systematic gender association with academic position.7–9, 14 Urology is no exception to these trends. Our results confirm previous findings where women tend to plateau at the rank of associate professor.15, 16 Only 12% of all female urologists in our study have advanced past this level to senior positions compared to 33% of male urologists.
Women’s underrepresentation in the upper echelons of academic medicine may simply be generational, as many years of significant research activity and clinical practice are required before senior promotion. In our analysis, men had a significantly longer career duration than women. This may be due to men’s higher likelihood to publish during residency training,16 which would increase their years of active research activity. There may also be a time-lag effect, where relatively few women now have careers of sufficient length to warrant senior positions due to the relatively recent rise in female urology trainees (1.9% in 1978 to 23.1% in 2013).17 AUA census data confirmed that high percentages of females are observed in younger age groups of practicing urologists: although only 7.7% of practicing urologists were women in 2015, they made up 17.2% of urologists < 45 years of age. The outlook is bright for these young, female urologists. As women mature in their careers, increasing numbers will be eligible for advancement, and publication productivity will likely continue to be a significant factor considered in hiring and promotion. In our study, men had a higher h-index than women, and the differences remained significant even when comparing gender of the same academic rank. However, h-index is related to the career duration and we employed the m-quotient to correct for these career length discrepencies. Overall, men had a higher m-quotient than women, but these differences were not significant on intra-rank comparison by gender, indicating that the overall m-quotient difference is due to a larger proportion of men in senior-level positions than women (a consequence of the time-lag effect for female trainees). Men and women are therefore publishing at similar rates in all ranks. There was no difference in h-index on subgroup analysis for faculty with less than 10 years of experience, suggesting that women entering the field of urology are equally contributing scientific knowledge. The differences beyond 10 years may represent a faster publication rate for men, which leads to a larger gap over time, or cohort differences in the accepted norms for men and women. For example, recent evidence suggests that women are more likely to enter a clinician-educator track than a traditional tenure track.18 This poses a considerable challenge to leadership parity for women, because faculty on the clinician-educator track typically lag behind their colleagues in academic promotion. It is essential that we retain productive cohorts of junior women faculty to help close the tenure gap and provide mentorship for the next generation.
In order to increase publication productivity and better prepare for chairships, this group of rising female urologists desperately need mentors that model senior-level leadership and/or head significant research groups. The approach should be two-fold: 1) more same gender mentors, and 2) better opposite gender ones. Inadequate mentorship, especially early on in career development, may hamper women’s opportunities for research output and advancement. A survey of medical students applying to the urology residency match cited mentorship in the field as one of the most important reasons for their decision to pursue urology.19 In fact, American medical schools with strong urology mentorship were much more likely to match applicants to urologic residency training programs.20 However, in a systemic review of mentoring in academic medicine less than half of all medical students claimed to have a mentor. The reviewers noted that women thought they had more difficulty obtaining a mentor than men, and many perceived that a mentor of the same gender would be more relatable. Several studies indicate that women have difficulty in finding same-sex mentors and role models,21–23 and this may lead women to choose mentors of lower rank than men.24 This difficulty may be compounded in urology where women are sparsely represented. Over one-third of current female urologists surveyed in one study reported dissatisfaction with the lack of mentoring.15 In a group of women who left academic urology, 25% claimed a lack of mentorship as a reason for leaving.15 Obtaining adequate mentorship may be difficult for early-career female urologists, especially for those seeking senior female faculty mentors. However, these alarming statistics should serve as a clarion call not only for more female mentors, but also for better mentorship from male colleagues. Female urology residents and junior faculty should not sacrifice relationships with productive male mentors, for less successful female mentors who may be less advanced in their careers.
Another reason for possible discrepancies in publication productivity for female urologist is pigeonholing, wherein women are relegated to practicing certain subspecialties. We found significant differences in the subspecialty based on gender in our cohort. Women were much more likely to describe their subspecialty practice as female or pediatric urology. Although we did not perform an analysis of publication productivity stratified by gender and subspecialty content, it may be that women have lower publication profiles because they publish within more niche specialties, where fewer articles are submitted and/or accepted for publication. Men, who are more likely to go into general urology and urologic oncology, will have broader readership and a higher citation rate for their work, although getting articles accepted may be more difficult with higher submission rates in these fields. Further work is needed to elucidate the effect of subspecialty choice on academic output.
The differences in research productivity and career trajectory may also be partially explained by greater obligation to family and parental responsibilities.4, 25–27 Men are more likely to have children during residency training than women, but largely rely on their spouse for childcare.28 Among residents and practicing surgeons who had children, more women take time off from work than men (67% versus 38% for residents and 64% versus 12% for post-training surgeons). Women considering pregnancy early in their careers face barriers trying to balance clinical/research activities with absence from work. As a result, nearly half of all women surgeons elect to delay childbearing until they have completed their training.29 Female urologists are no exception, as they tend to have children later in life, a small number of children, a higher induction rate, and a higher rate of pregnancy complications.30 Because surgical training spans the prime childbearing years for most women, concerns about the feasibility of starting a family may not only deter women from entering fields like urology, it may also pose a significant hurdle to early-career development and sustained productivity.
Our study has several limitations to consider. First, there is no quantification of non-NIH research funding. There may be gender differences in research funding that include institutional or private donor grants. Second, although we used the first urology-related publication as a proxy for initiation of an academic career, the duration of career is not necessarily defined by the year of first publication. However, this method has been used in other reported analyses of publication productivity within academic medicine.7, 11 Third, there are possible inaccuracies with identification of an institution’s complete faculty list and rank since departmental websites are not updated in real-time, but these measurement errors are not systematic as faculty member profiles are likely not updated preferentially by specific rankings. Finally, this study only reviews data pertinent to academic urologists as a group and cannot be applied to women seeking promotion in private practice or clinical-track faculty which might have different criteria for promotion.
Conclusions
While advancement in academic urology is based on a variety of achievements, our data show a gender disparity in senior leadership positions. This difference can partially be attributed to the difference in career length and its effect on publication productivity. Fortunately, when comparing the m-quotient (accounts for career duration) of men and women at the same academic rank, we observed no difference at any position. Since the most rigorous academic criteria are equivalent between the genders, perhaps psychosocial barriers such as a lack of mentorship and role-modeling are preventing women from attaining those highest leadership roles. As the percentage of women in urology increases, working toward a gender-neutral, merit-based work environment remains an optimal goal. Recognizing and identifying gender differences within urology is an important opportunity for leaders in the field.
Acknowledgments
The first author, Erik N. Mayer, had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. None of the authors have any conflicts of interest to disclose. This project was partially funded by NIH grant #1K12HD085852-01. This grant was used primarily to support the involvement of Heidi A. Hanson in all aspect of design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
References
- 1.Kim SJ, Hyun G. MP15-04 WOMEN IN UROLOGY: TIME TO LEAN IN. The Journal of urology. 191:e145. [Google Scholar]
- 2.Monga M. The State of the Urology Workforce and Practice in the United States 2015. In: Clemens Q, editor. American Urological Association Annual Meeting. San Diego, CA: American Urological Association (AUA); 2016. [Google Scholar]
- 3.Zhuge Y, Kaufman J, Simeone DM, Chen H, Velazquez OC. Is there still a glass ceiling for women in academic surgery? Annals of surgery. 2011;253:637–643. doi: 10.1097/SLA.0b013e3182111120. [DOI] [PubMed] [Google Scholar]
- 4.Reed DA, Enders F, Lindor R, McClees M, Lindor KD. Gender differences in academic productivity and leadership appointments of physicians throughout academic careers. Academic medicine : journal of the Association of American Medical Colleges. 2011;86:43–47. doi: 10.1097/ACM.0b013e3181ff9ff2. [DOI] [PubMed] [Google Scholar]
- 5.Nonnemaker L. Women Physicians in Academic Medicine — New Insights from Cohort Studies. New England Journal of Medicine. 2000;342:399–405. doi: 10.1056/NEJM200002103420606. [DOI] [PubMed] [Google Scholar]
- 6.Weiss DA, Kovshilovskaya B, Breyer BN. Gender trends of urology manuscript authors in the United States: a 35-year progression. The Journal of urology. 2012;187:253–258. doi: 10.1016/j.juro.2011.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Holliday EB, Jagsi R, Wilson LD, Choi M, Thomas CR, Jr, Fuller CD. Gender differences in publication productivity, academic position, career duration, and funding among U.S. academic radiation oncology faculty. Academic medicine : journal of the Association of American Medical Colleges. 2014;89:767–773. doi: 10.1097/ACM.0000000000000229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lopez SA, Svider PF, Misra P, Bhagat N, Langer PD, Eloy JA. Gender differences in promotion and scholarly impact: an analysis of 1460 academic ophthalmologists. Journal of surgical education. 2014;71:851–859. doi: 10.1016/j.jsurg.2014.03.015. [DOI] [PubMed] [Google Scholar]
- 9.Eloy JA, Svider P, Chandrasekhar SS, et al. Gender disparities in scholarly productivity within academic otolaryngology departments. Otolaryngology–head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2013;148:215–222. doi: 10.1177/0194599812466055. [DOI] [PubMed] [Google Scholar]
- 10.Lee J, Kraus KL, Couldwell WT. Use of the h index in neurosurgery. Clinical article. Journal of neurosurgery. 2009;111:387–392. doi: 10.3171/2008.10.JNS08978. [DOI] [PubMed] [Google Scholar]
- 11.Khan NR, Thompson CJ, Taylor DR, et al. An analysis of publication productivity for 1225 academic neurosurgeons and 99 departments in the United States. Journal of neurosurgery. 2014;120:746–755. doi: 10.3171/2013.11.JNS131708. [DOI] [PubMed] [Google Scholar]
- 12.Lautenberger DM, Dandar VM, Raezer CL, Sloane RA. The State of Women in Academic Medicine: The Pipeline and Pathways to Leadership, 2013–2014. 2014 [Google Scholar]
- 13.Eloy JA, Svider PF, Cherla DV, et al. Gender disparities in research productivity among 9952 academic physicians. The Laryngoscope. 2013;123:1865–1875. doi: 10.1002/lary.24039. [DOI] [PubMed] [Google Scholar]
- 14.Diamond SJ, Thomas CR, Jr, Desai S, et al. Gender Differences in Publication Productivity, Academic Rank, and Career Duration Among U.S. Academic Gastroenterology Faculty. Academic medicine : journal of the Association of American Medical Colleges. 2016 doi: 10.1097/ACM.0000000000001219. [DOI] [PubMed] [Google Scholar]
- 15.Lightner DJ, Terris MK, Tsao AK, Naughton CK, Lohse CM. Status of women in urology: based on a report to the Society of University Urologists. The Journal of urology. 2005;173:560–563. doi: 10.1097/01.ju.0000149739.51103.d3. [DOI] [PubMed] [Google Scholar]
- 16.Yang G, Villalta JD, Weiss DA, Carroll PR, Breyer BN. Gender differences in academic productivity and academic career choice among urology residents. The Journal of urology. 2012;188:1286–1290. doi: 10.1016/j.juro.2012.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Halpern JA, Lee UJ, Wolff EM, et al. Women in Urology Residency 1978–2013: a Critical Look at Gender Representation in Our Specialty. Urology. 2016 doi: 10.1016/j.urology.2015.12.092. [DOI] [PubMed] [Google Scholar]
- 18.Mayer AP, Blair JE, Ko MG, et al. Gender distribution of U.S. medical school faculty by academic track type. Academic medicine : journal of the Association of American Medical Colleges. 2014;89:312–317. doi: 10.1097/ACM.0000000000000089. [DOI] [PubMed] [Google Scholar]
- 19.Kerfoot BP, Nabha KS, Masser BA, McCullough DL. What makes a medical student avoid or enter a career in urology? Results of an international survey. The Journal of urology. 2005;174:1953–1957. doi: 10.1097/01.ju.0000177462.61257.4e. [DOI] [PubMed] [Google Scholar]
- 20.Kutikov A, Bonslaver J, Casey JT, et al. The gatekeeper disparity–why do some medical schools send more medical students into urology? The Journal of urology. 2011;185:647–652. doi: 10.1016/j.juro.2010.09.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McGinty KL, Martin CA, Demoss KL, Hill KK. Future career choices of women psychiatric residents : is research included? Academic psychiatry : the journal of the American Association of Directors of Psychiatric Residency Training and the Association for Academic Psychiatry. 1994;18:95–102. doi: 10.1007/BF03341527. [DOI] [PubMed] [Google Scholar]
- 22.Bright CM, Duefield CA, Stone VE. Perceived barriers and biases in the medical education experience by gender and race. Journal of the National Medical Association. 1998;90:681–688. [PMC free article] [PubMed] [Google Scholar]
- 23.Abu-Zaid A, Altinawi B. Perceived barriers to physician-scientist careers among female undergraduate medical students at the College of Medicine - Alfaisal University: a Saudi Arabian perspective. Medical teacher. 2014;36(Suppl 1):S3–7. doi: 10.3109/0142159X.2014.886006. [DOI] [PubMed] [Google Scholar]
- 24.Gordon MB, Osganian SK, Emans SJ, Lovejoy FH., Jr Gender differences in research grant applications for pediatric residents. Pediatrics. 2009;124:e355–361. doi: 10.1542/peds.2008-3626. [DOI] [PubMed] [Google Scholar]
- 25.Carr PL, Ash AS, Friedman RH, et al. Relation of family responsibilities and gender to the productivity and career satisfaction of medical faculty. Annals of internal medicine. 1998;129:532–538. doi: 10.7326/0003-4819-129-7-199810010-00004. [DOI] [PubMed] [Google Scholar]
- 26.Levinson W, Tolle SW, Lewis C. Women in academic medicine. Combining career and family. The New England journal of medicine. 1989;321:1511–1517. doi: 10.1056/NEJM198911303212205. [DOI] [PubMed] [Google Scholar]
- 27.Kuehn BM. More women choose careers in surgery: bias, work-life issues remain challenges. Jama. 2012;307:1899–1901. doi: 10.1001/jama.2012.3725. [DOI] [PubMed] [Google Scholar]
- 28.Mayer KL, Ho HS, Goodnight JE., Jr Childbearing and child care in surgery. Archives of surgery. 2001;136:649–655. doi: 10.1001/archsurg.136.6.649. [DOI] [PubMed] [Google Scholar]
- 29.Turner PL, Lumpkins K, Gabre J, Lin MJ, Liu X, Terrin M. Pregnancy among women surgeons: trends over time. Archives of surgery. 2012;147:474–479. doi: 10.1001/archsurg.2011.1693. [DOI] [PubMed] [Google Scholar]
- 30.Lerner LB, Stolzmann KL, Gulla VD. Birth trends and pregnancy complications among women urologists. Journal of the American College of Surgeons. 2009;208:293–297. doi: 10.1016/j.jamcollsurg.2008.10.012. [DOI] [PubMed] [Google Scholar]


