Abstract
Shoulder pain from overuse of the arm is common after spinal cord injury (SCI). This pain can be difficult to eliminate. There are many other complications after SCI; therefore, shoulder pain is sometimes not the first priority. However, if neglected for too long, shoulder pain could mean that more serious problems are happening inside the shoulder joint. Here we present the options available when treatment for shoulder pain is needed.
One research survey has found that half of adults with SCI have pain in both shoulders, and often the pain will last longer than 1 year.1 Shoulder pain can develop any time after an SCI, but it is most common within the first 5 years after injury.2 Shoulder pain is most intense during activities of daily living, including wheelchair propulsion uphill, transfers, reaching overhead, and other tasks that require a lot of force through the hand.3–5 Patients with SCI and shoulder pain often have injured rotator cuff tendons.6
Rotator cuff tendons are the end sections of small muscles of the shoulder that attach to the bone of the arm. They provide support to the shoulder so that it moves properly. A shoulder that does not move properly may develop painful arthritis.
Another problem with shoulders that do not move properly is that the rotator cuff tendons can get overcrowded or pinched, which is called subacromial impingement or impingement syndrome. This pinching can be painful or it can cause tears to the tendons which can be painful. Once a tendon is torn, it may be more difficult to move the shoulder properly, which can lead to further damage. This cycle in which some tendon damage leads to more shoulder damage is common among people who use their arms a lot. This includes people with SCI. For all of these reasons, it is recommended that people treat shoulder pain rather than just live with it.
What options are available for treating shoulder pain in people with SCI?
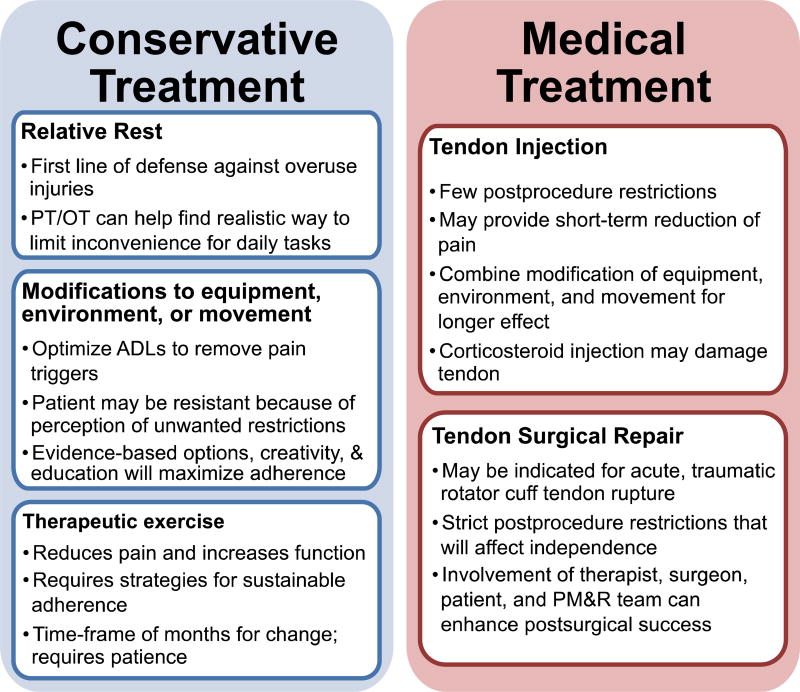
Many treatment options are available for shoulder pain in people with SCI. Treatments include conservative options (eg, physical therapy, occupational therapy) and more aggressive medical options (eg, injectable medications, surgery) (fig 1).
Fig 1.
Conservative and medical treatment options for patients with SCI with shoulder pain and injury. Abbreviations: ADLs, activities of daily living; OT, occupational therapy; PM&R, physical medicine and rehabilitation; PT, physical therapy; SCI, spinal cord injury.
What conservative treatment options exist for patients with SCI who have shoulder pain and injury?
The first treatment is often physical therapy or occupational therapy (or both). Studies have shown that a high-quality exercise program will reduce pain, even in patients with long-term pain. The quality of the exercise program depends on the specific exercises prescribed and on the technique used when performing the exercises.6–8 Therefore, it is important to see a therapist who is familiar with treating shoulder pain. A list of things to include in a good exercise program are subsequently listed. Many of the terms used in the following list may be confusing, but a therapist will know what they mean. If a therapist cannot explain the use of these terms in an exercise program, then a different therapist may be better. Shoulder programs should include exercises that:
Strengthen the muscles that stabilize the shoulder blade and the shoulder joint (rotator cuff muscles).
Rotate the shoulder out (external rotation of the shoulder).
Bring the shoulder blades down and back on the trunk (scapular depression and retraction).
Balance the strength of muscles used for pulling and pushing (exercise muscles located on the back and front of the shoulder).
Shorten and lengthen the muscle. After each repetition of an exercise is completed, you should return to the beginning position slowly before doing the next repetition. This slow return to the starting position strengthens the muscle while it lengthens.
-
Stretch muscles that are tight, with special attention to:
Front chest musculature
Back of the shoulder joint, which is often tight when the patient has limited inward rotation of the shoulder (they cannot reach behind and up their back very far)
Advance the difficulty of exercises as needed, followed by an easy-to-sustain maintenance program. Researchers have found that a program that progresses for approximately 12 weeks before beginning a maintenance program is effective.
- Focus on proper technique and posture when exercising, including the following:
- Center the arm in its socket before beginning an exercise (roll shoulders down and back into a good posture)
- Avoiding substitution of other muscle groups; a common mistake is shrugging the shoulders while exercising
- Provide modifications to make the exercise easier and allow the patient to maintain proper technique. This may require:
- Lying down (rather than sitting up) while performing the exercise
- Limiting the range of motion used in the exercise; in fact, isometric exercises (those with no movement when muscles are contracting) may be necessary in the beginning
- Limiting the resistance or force that is required to perform the exercise
- Building up to the desired number of repetitions for each exercise in the program
Encourage completion of the program. A properly designed program should fit naturally into your daily routine, use equipment that is readily available, and include activities that you will be able to perform throughout the duration of the program.
In addition to physical or occupational therapy, rest can be a very effective treatment. Finding new ways to perform daily tasks without causing pain is also important. It may take more time to complete a task (eg, transfer with a sliding board) while waiting for a shoulder to improve. Incorporating more rest periods during lengthy repetitive tasks (eg, propelling a wheelchair) may also be helpful. However, it is important to remember that a minor inconvenience now may prevent a major inconvenience later. Daily activities should not feel overly strenuous or cause pain to the shoulder. Physical and occupational therapists often provide realistic solutions for changing a task or movement so that is it more comfortable to perform.
What options exist if conservative treatment is not enough?
Other options are subsequently listed for the treatment of shoulder pain if conservative treatment is not enough. Like all treatments, the pros and cons should be considered (see fig 1).
Corticosteroid injection
An injection of a corticosteroid medication may provide short-term pain relief from shoulder pain because of rotator cuff tendon disease. If the underlying reason for the pain is not corrected, the pain will likely return. Therefore, patients receiving corticosteroid injections should also try exercise to assist in longer-term pain relief. Sometimes these injections help reduce the pain enough to allow the patient to begin an exercise program that was previously too painful. After an injection, the patient likely will be required to reduce arm use for a few days. Some doctors do not use corticosteroid medications with patients who have an SCI because the injection itself may weaken a tendon that is already working hard because of the high demands of living with an SCI.9
Surgical repair
Sometimes surgery is necessary. For example, surgery should be performed if a tendon in the shoulder was recently torn because of a fall and the patient consequently lost independence. For patients with shoulder symptoms that are worsening over time, there are no clear guidelines to determine if and when surgery is necessary. It is difficult to predict whether a partially torn tendon will develop into something that limits a patient’s function. Exercise therapy is almost always prescribed before surgery is considered. However, there is a risk that if the wait period before surgery is too long, muscles can break down and fat can develop in the muscle. Therefore, a delayed surgery may be less effective. Additionally, the surgeon should discuss with the patient whether the pain is likely to be reduced or eliminated with surgery.
The major drawback to surgery for patients with SCI is that typically the shoulder must not be used for 6 to 8 weeks after surgery. After that period, limited use may be allowed for the next 6 to 8 weeks. These restrictions mean the patient may not be allowed to do independent transfers and other activities of daily living for months. One study did report success with rotator cuff surgery in patients with SCI when a team of specialists (surgeon, therapists, rehabilitation doctors, social workers, and others) was involved in the decision-making and care before and after surgery.10
Summary
Shoulder pain in people with SCI is often caused by injury to the rotator cuff, the muscles that help stabilize the arm in the shoulder joint and control shoulder movement. Fortunately, conservative therapies that incorporate exercise can significantly reduce shoulder pain in people with SCI. However, pain can still persist after exercise therapy. Additional options (eg, injections of corticosteroid medication, surgery) are available, but the pros and cons of treatment should be discussed with a team of medical professionals before deciding on care plans.
Acknowledgments
This publication was made possible by funding from the Mayo Clinic Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery and by the National Institutes of Health (grant no. R01 HD84423-01).
Footnotes
Authorship
This product was developed by Meegan G. Van Straaten, PT, MSPH, Department of Physical Medicine and Rehabilitation, Mayo Clinic Rehabilitation Medicine Research Center; Beth A. Cloud, PT, DPT, PhD, Department of Physical Medicine and Rehabilitation, Mayo Clinic Rehabilitation Medicine Research Center; Kristin D. Zhao, PhD, Department of Physical Medicine and Rehabilitation, Mayo Clinic Rehabilitation Medicine Research Center; Emma Fortune, PhD, Mayo Clinic Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery, Department of Health Sciences Research; and Melissa M. B. Morrow, PhD, MSc, Mayo Clinic Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery, Department of Health Sciences Research.
Disclaimer
This information is not meant to replace the advice of a medical professional. You should consult your health care provider regarding specific medical concerns or treatment. This information/education page may be reproduced for noncommercial use for health care professionals to share with patients and their caregivers. Any other reproduction is subject to approval by the publisher.
Contributor Information
Meegan G. Van Straaten, Department of Physical Medicine and Rehabilitation, Mayo Clinic Rehabilitation Medicine Research Center.
Beth A. Cloud, Department of Physical Medicine and Rehabilitation, Mayo Clinic Rehabilitation Medicine Research Center.
Kristin D. Zhao, Department of Physical Medicine and Rehabilitation, Mayo Clinic Rehabilitation Medicine Research Center.
Emma Fortune, Mayo Clinic Robert D. and Patricia E. Kern Center for the Science of Health Care, Delivery, Department of Health Sciences Research.
Melissa M. B. Morrow, Mayo Clinic Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery, Department of Health Sciences Research, Mayo Clinic Rehabilitation Medicine Research Center.
References
- 1.Alm M, Saraste H, Norrbrink C. Shoulder pain in persons with thoracic spinal cord injury: prevalence and characteristics. J Rehabil Med. 2008;40:277–83. doi: 10.2340/16501977-0173. [DOI] [PubMed] [Google Scholar]
- 2.Sie IH, Waters RL, Adkins RH, Gellman H. Upper extremity pain in the postrehabilitation spinal cord injured patient. Arch Phys Med Rehabil. 1992;73:44–8. [PubMed] [Google Scholar]
- 3.Curtis KA, Drysdale GA, Lanza RD, Kolber M, Vitolo RS, West R. Shoulder pain in wheelchair users with tetraplegia and paraplegia. Arch Phys Med Rehabil. 1999;80:453–7. doi: 10.1016/s0003-9993(99)90285-x. [DOI] [PubMed] [Google Scholar]
- 4.Curtis KA, Roach KE, Applegate EB, et al. Development of the Wheelchair User’s Shoulder Pain Index (WUSPI) Paraplegia. 1995;33:290–3. doi: 10.1038/sc.1995.65. [DOI] [PubMed] [Google Scholar]
- 5.McCasland LD, Budiman-Mak E, Weaver FM, Adams E, Miskevics S. Shoulder pain in the traumatically injured spinal cord patient: evaluation of risk factors and function. J Clin Rheumatol. 2006;12:179–86. doi: 10.1097/01.rhu.0000230532.54403.25. [DOI] [PubMed] [Google Scholar]
- 6.Requejo PS, Furumasu J, Mulroy SJ. Evidence-based strategies for preserving mobility for elderly and aging manual wheelchair users. Top Geriatr Rehabil. 2015;31:26–41. doi: 10.1097/TGR.0000000000000042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Van Straaten MG, Cloud BA, Morrow MM, Ludewig PM, Zhao KD. Effectiveness of home exercise on pain, function, and strength of manual wheelchair users with spinal cord injury: a high-dose shoulder program with telerehabilitation. Arch Phys Med Rehabil. 2014;95:1810–7. doi: 10.1016/j.apmr.2014.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mulroy SJ, Thompson L, Kemp B, et al. Strengthening and optimal movements for painful shoulders (STOMPS) in chronic spinal cord injury: a randomized controlled trial. Phys Ther. 2011;91:305–24. doi: 10.2522/ptj.20100182. [DOI] [PubMed] [Google Scholar]
- 9.Coombes BK, Bisset L, Vicenzino B. Efficacy and safety of corticosteroid injections and other injections for management of tendinopathy: a systematic review of randomised controlled trials. Lancet. 2010;376:1751–67. doi: 10.1016/S0140-6736(10)61160-9. [DOI] [PubMed] [Google Scholar]
- 10.Fattal C, Coulet B, Gelis A, et al. Rotator cuff surgery in persons with spinal cord injury: relevance of a multidisciplinary approach. J Shoulder Elbow Surg. 2014;23:1263–71. doi: 10.1016/j.jse.2014.01.011. [DOI] [PubMed] [Google Scholar]