Abstract
Objective:
The objective of this study was to determine the safety and efficacy of sacral neuromodulation (SNM) in patients with idiopathic nonobstructive urinary retention.
Materials and Methods:
We retrospectively reviewed the files of patients who underwent staged neuromodulation for idiopathic nonobstructive urinary retention from 2004 to 2016 at our hospital. Patients who had a 50% improvement in symptoms after 1 week of stage 1 procedure were qualified for permanent device implantation. Patient data were assessed on efficacy and need for intermittent self-catheterization, complications, and operative revision rates.
Results:
Twenty-seven female patients who underwent SNM therapy were analyzed. The mean age of the patients was 32.5 ± 10.8 years. The mean duration of urinary retention was 3.2 ± 1.7 years. All patients were doing intermittent self-catheterization, but few were able to void <100 ml. Twenty-four (88.8%) of the 27 patients demonstrated a >50% improvement in symptoms and underwent permanent device placement. At a median follow-up of 5.7 ± 3.2 years, 20 (83.3%) of the 24 patients demonstrated sustained improvement rates of >50%. Seventeen (70.83%) of 24 patients could void spontaneously with a mean residual urine of 28.1 ± 24.4 ml (P < 0.001). Three (12.5%) were voiding with significant mean decreasing number of catheterizations from 5.6 ± 2.4 to 1.4 ± 2.1 (P < 0.001). Four (16.6%) had their device explanted. Ten (41.6%) of the 24 patients underwent surgical revision. Most of the adverse events were managed by device reprograming.
Conclusion:
SNM is a highly effective and safe procedure in this subset of the female population with idiopathic refractory nonobstructive urinary retention.
Keywords: Fowler's syndrome, idiopathic urinary retention, InterStim device, sacral neuromodulation, urodynamic study
INTRODUCTION
Lower urinary tract dysfunction is highly prevalent and affects millions of people worldwide. It may manifest as urinary urgency, frequency, incontinence, and urinary retention. Idiopathic urinary retention (IUR) represents one of the most challenging dilemmas in urological practice. Electromyography (EMG) of the external urethral sphincter divides these patients into two categories. Patients who present with burst and complex repetitive discharge on EMG are referred to as having Fowler's syndrome[1,2] and those who showed no activity on EMG are said to have idiopathic nonobstructive urinary retention.[3] These symptoms can be distressing and socially disruptive to patients, causing significant impairments to their health-related quality of life.[4]
Treatment in the form of urethral dilatation, intermittent catheterization, botulinum toxin injection of the urethral sphincter, and alpha blockers has been tried for women with urinary retention. Spontaneous recovery has been observed in 42% of patients, in which precipitating factors were present such as postpelvic surgery and postpartum.[5] Sacral neuromodulation (SNM), a minimally invasive therapy, has been shown to be a permissive and effective therapy in the restoration of spontaneous voiding and remains effective for several years in patients with urinary retention.[6,7] SNM was introduced as a revolutionary concept by Schmidt and Tanagho in the year 1979 to regain bladder control in patients with idiopathic nonobstructive urinary retention.[8] In 1997, SNM was approved by the United States FDA for refractory urinary urge incontinence, urinary frequency/urgency syndrome, and nonobstructive IUR.[9] SNM's mechanism of action is still unclear. It has been described in various studies that SNM inhibits bladder-afferent activities through its action on somatic-afferent pathways and thereby blocks abnormal sensory input to the spinal cord and brain and sends coordinated efferent impulses to the bladder.[10]
SNM has demonstrated high rates of clinical success, defined as a significant reduction in voiding-related symptoms, voided volume, and the number of pads used daily.[11]
De Ridder et al. demonstrated that the presence of Fowler's syndrome predicts successful long-term outcomes of sacral nerve stimulation in women with urinary retention. They observed a 5-year, 72% urinary symptom-free success rate in Fowler's syndrome and 46% in patients with idiopathic nonobstructive urinary retention treated with SNM.[12] Shaker and Hassouna found that SNM is highly successful in patients with nonobstructive urinary retention in their series.[3]
We wanted to see the overall results in terms of safety and efficacy of the SNM procedure in patients with nonobstructive urinary retention treated at King Faisal Specialist Hospital and Research Center in Riyadh.
MATERIALS AND METHODS
After receiving the Office of Research Administration (ORA) approval, a retrospective chart review was performed in all female patients with idiopathic refractory nonobstructive urinary retention treated with SNM at our institution from 2004 to 2016. Patient demographics including age, gender, and indication for SNM were obtained. All patients were evaluated for medical history, physical examination, voiding diaries, urodynamic studies, and cystoscopic examination. A urethral pressure profile and EMG were not done in urodynamic studies. All adult female patients with documented nonobstructive urinary retention who failed conservative or pharmacological therapy were included in our study. Patients who had overactive bladder symptoms, pelvic prolapse, bladder outflow obstruction, and interstitial cystitis were excluded from the study.
All patients were doing clean intermittent self-catheterization or were on a permanent catheter before the SNM procedure. IUR was defined as the inability to void without any obvious anatomical or neurological cause. The duration of urinary retention was calculated when patients started clean intermittent catheterization (CIC) or underwent permanent catheterization until the implantation of the InterStim device. After fulfilling preoperative criteria, all patients underwent Stage 1 SNM lead placement with the InterStim device in the sacral 3 foramen. Patients were observed for 1 week with voiding diaries. The detail of implantation has been described in literature.[13] Patients completed 1 week voiding diaries following Stage 1 SNM temporary lead insertion. Those who showed restoration of spontaneous voiding with a residual volume of <100 ml or who experienced a 50% reduction in catheterization frequency were offered permanent Stage 2 SNM device insertion. All our patients fulfilled the criteria for second stage InterStim device insertion. The InterStim device was placed deep within the subcutaneous fat of buttock ipsilateral to the electrode position. At day 1 after surgery, the stimulator was switched on and wavelength, amplitude, and frequency were adjusted to just below a comfortable perineal sensation.
Charts of patients were reviewed for length of follow-up, complications, device failure, number of reoperations, and the need for catheterization.
Descriptive statistics were analyzed as mean ± standard deviation, and duration of retention, pre- and post-operative residual urine, and age at permanent device implantation were analyzed using the independent samples t-test. Chi-squared test was also used to analyze voiding function before implantation. Statistical significance was considered as P ≤ 0.05.
RESULTS
From January 2004 to June 2016, 27 female patients with nonobstructive urinary retention refractory to standard medical and conservative therapy underwent a 2-stage SNM (InterStim) device implantation. The mean age of the patients was 32.5 ± 10.8 years (range: 20–63). All patients were doing intermittent self-catheterization, but few of them were able to void <100 ml. Preoperative urodynamic evaluation and flexible cystoscopy of these patients confirmed the absence of any obstructive factor for retention. The mean duration of urinary retention was 3.2 ± 1.7 years (range: 1–8). The average preoperative residual urine was 402.2 ± 107.4 ml. Patients' demographic data are shown in Table 1.
Table 1.
Patient demographic data
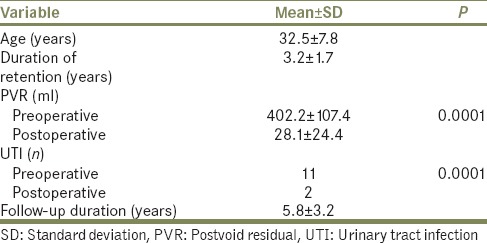
All patients underwent Stage 1 temporary lead insertion in sacral foramen 3. Of the 27 patients, 24 (88.8%) demonstrated a >50% reduction in catheterization and improvement in symptoms according to a 1-week follow-up diary; they subsequently underwent permanent SNM (InterStim) device implant. These patients were followed up postoperatively to determine efficacy, durability, and device-related complications. At a mean follow-up of 5.7 ± 3.2 years (range: 0.4–11.9), 20 (83.3%) of the 24 patients demonstrated sustained improvement of symptoms, reduction in significant postvoid residual (PVR) urine, and significant decrease in CIC. Seventeen (70.83%) of the 24 patients could void spontaneously and had a complete response with a mean PVR urine from 402.2 ± 107.4 to 28.1 ± 24.4 ml (P < 0.0001). The remaining three (12.5%) patients had a partial response and were voiding with a significant decrease in the number of self-catheterizations from mean 5.6 ± 2.4 to 1.4 ± 2.1 (P < 0.001). Four (16.6%) of the 24 patients were explanted during follow-up. The reasons for device explantation included loss of efficacy in two patients, box site infection in one patient, and stroke in one patient.
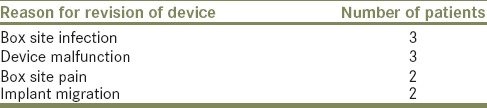
Moreover, 10 (41.6%) of the 24 patients required InterStim device revision during follow-up. The main reason for procedure revision was battery expiration or device malfunction in three, box site infection in three, implant migration in two, and box site pain in two patients as mentioned in Table 2 and Graph 1.
Table 2.
Reason for surgical revision procedure
Graph 1.
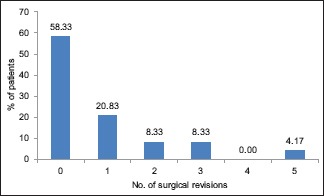
Total number of surgical revision procedures
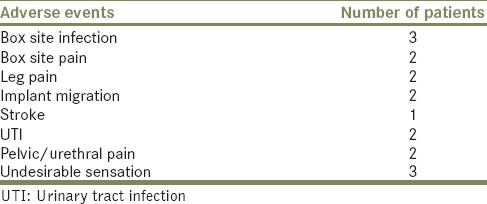
Two patients got pregnant during follow-up and the device remained off during that period. Most of the other adverse events such as back pain, perineal or urethral pain, leg pain, and abnormal or undesirable sensations were managed by reprograming the device in the outpatient clinic. With regard to urinary tract infection (UTI), there was a significant reduction in the UTI rate from the number of patients who developed preoperative UTI, 11 (45.83%), to postoperative patients who developed UTI, 2 (8.33%) (P < 0.0001). Adverse events are shown in Table 3.
Table 3.
Adverse events in patients during follow-up
The efficacy of the device was determined by obtaining objective data of patients from their follow-up diaries. Almost all patients could eliminate CIC completely. There was a significant reduction in PVR urine volume at a mean follow-up of 5.8 ± 3.2 years (P < 0.001).
DISCUSSION
SNM has been used successfully in patients with refractory IUR. Fowler's syndrome has remained a predictor of successful outcomes in young female patients treated with SNM therapy.[14] SNM's mechanism of action is still unclear. It is hypothesized that SNM inhibits the afferent limb of the voiding reflex and inhibits sacral interneuronal transmission. In patients with IUR, SNM inhibits somatic excitatory outflow to the external sphincter, preventing voiding reflex inhibition and therefore facilitating voiding.[15] Few studies contradict this mechanism of action of SNM in IUR. Dasgupta et al. found in their study that the electromyographic activity of the sphincter remained unchanged after SNM device implantation and there was a slight increase in detrusor activity. They postulated that this slight increase in detrusor contractility is sufficient to overcome sphincter activity and facilitate voiding.[16]
This long-term outcome study demonstrates our department's experience with SNM in patients with IUR over a 12-year period (2004–2016). This confirms the long-term efficacy of SNM therapy in patients with IUR. Nearly 70.83% of our patients had voiding restored with a sustained improvement over a mean follow-up of 67 months. Almost similar long-term data were obtained from Van Voskuilen et al.[17] that showed 76.2% efficacy of SNM over a period of 70.5 months. Elhilali et al.[18] demonstrated that SNM was effective in 78% of patients in restoring voiding over 77 months of follow-up. White et al.[19] in 2008 found that, at a mean follow-up of 40 months, 85.7% of patients with refractory, nonobstructive urinary retention demonstrated a >50% improvement in symptoms with SNM. Although the above-mentioned studies obviously cemented the definite role of SNM in the treatment of patients with refractory urinary retention, few data are currently available regarding the long-term efficacy and durability of SNM.
All our patients underwent the 2-stage technique of neuromodulation. We assume that the 2-stage technique is the standard technique rather than percutaneous nerve excitation (PNE) or the 1-stage implant as is evident in various studies.[20] In 2004, a prospective randomized trial was conducted comparing 1-stage with 2-stage implantation of a pulse generator in patients with pelvic floor dysfunction selected for SNM. Everaert et al.[21] found that 2-stage implantation for SNM has a higher success rate than 1-stage implantation. Datta et al. in 2007 found that the 2-stage technique is better than PNE in restoration of voiding.[22] They further elaborated that of the eight patients with negative PNE results, when they proceeded to the 2-stage procedure, five had voiding restored. All these studies described the effectiveness of the 2-stage procedure, as was reported by Janknegt et al. and Scheepens et al. in their studies.[23,24] SNM's success rate can be further improved with the use of tined lead as this helps anchor the lead and there is less chance of lead migration.[25]
The explantation rate in our study was 16.6%: two (8.33%) patients had lost efficacy site infections, one had his/her device explanted due to box site infection, and one developed a stroke and had to have the device removed. Although this explantation rate was higher than in previously reported studies, from 10% to 15%,[26,27] it was almost consistent with the rate found in a study by Al-zahrani et al.[28] that demonstrated a 20% explantation rate. The overall complication rate in our series is 41.66%, in which three patients had device failure or malfunction and three had box site infection. There were no differences measured in surgical techniques, age, and sterility. This rate of infection, although troubling, is consistent with other reported studies.[23,29] Most of the adverse events were managed with reprograming the device by a dedicated staff in our department.
The main limitation of our series was its retrospective nature and small number of study patients. Potential bias and reporting errors are the main risks of any retrospective study. Another limitation of our study was that subjective data in the form of voiding diaries were recorded sequentially during follow-up at the clinic. We assured that many of these ambiguities were mostly avoided during data collection. Urethral pressure profiles and EMG were not done during urodynamic studies of the patients. Therefore, we cannot say with certainty that the number of patients with Fowler's syndrome have high sphincter activity, which is one successful outcome predictor of SNM.
What is obvious from our study of the use of SNM therapy for treating patients with urinary retention is the necessity of continuous follow-up and a multidisciplinary team approach. We are fortunate to have a dedicated neurostimulator nurse, clinical psychologist, and pain physician in our institution to help patients during follow-up. We can suggest the long-term safety and efficacy of SNM in patients with IUR. We look forward to a prospective study in the future of patients with other indications for SNM and to include urodynamic studies before and after the procedure.
CONCLUSION
SNM gives a sustained prolonged benefit in a challenging group of patients with idiopathic nonobstructive urinary retention who are resistant to medical and conservative therapy. SNM is a safe, reversible, and minimally invasive therapy in appropriately selected patients with IUR to restore spontaneous voiding. Although much have been learned about SNM, there is still a need for ongoing research to know the exact mechanisms of action, proper patient selection, and to reduce adverse events and surgical revision rates to save costs.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Fowler CJ, Christmas TJ, Chapple CR, Parkhouse HF, Kirby RS, Jacobs HS. Abnormal electromyographic activity of the urethral sphincter, voiding dysfunction, and polycystic ovaries: A new syndrome? BMJ. 1988;297:1436–8. doi: 10.1136/bmj.297.6661.1436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jonas U, Fowler CJ, Chancellor MB, Elhilali MM, Fall M, Gajewski JB, et al. Efficacy of sacral nerve stimulation for urinary retention: Results 18 months after implantation. J Urol. 2001;165:15–9. doi: 10.1097/00005392-200101000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Shaker HS, Hassouna M. Sacral root neuromodulation in idiopathic nonobstructive chronic urinary retention. J Urol. 1998;159:1476–8. doi: 10.1097/00005392-199805000-00017. [DOI] [PubMed] [Google Scholar]
- 4.Coyne KS, Payne C, Bhattacharyya SK, Revicki DA, Thompson C, Corey R, et al. The impact of urinary urgency and frequency on health-related quality of life in overactive bladder: Results from a national community survey. Value Health. 2004;7:455–63. doi: 10.1111/j.1524-4733.2004.74008.x. [DOI] [PubMed] [Google Scholar]
- 5.Swinn MJ, Wiseman OJ, Lowe E, Fowler CJ. The cause and natural history of isolated urinary retention in young women. J Urol. 2002;167:151–6. [PubMed] [Google Scholar]
- 6.Dasgupta R, Wiseman OJ, Kitchen N, Fowler CJ. Long-term results of sacral neuromodulation for women with urinary retention. BJU Int. 2004;94:335–7. doi: 10.1111/j.1464-410X.2004.04979.x. [DOI] [PubMed] [Google Scholar]
- 7.Kavia RB, Datta SN, Dasgupta R, Elneil S, Fowler CJ. Urinary retention in women: Its causes and management. BJU Int. 2006;97:281–7. doi: 10.1111/j.1464-410X.2006.06009.x. [DOI] [PubMed] [Google Scholar]
- 8.Schmidt RA, Tanagho EA. Feasibility of controlled micturition through electric stimulation. Urol Int. 1979;34:199–230. doi: 10.1159/000280267. [DOI] [PubMed] [Google Scholar]
- 9.Oerlemans DJ, van Kerrebroeck PE. Sacral nerve stimulation for neuromodulation of the lower urinary tract. Neurourol Urodyn. 2008;27:28–33. doi: 10.1002/nau.20459. [DOI] [PubMed] [Google Scholar]
- 10.Elkelini MS, Abuzgaya A, Hassouna MM. Mechanisms of action of sacral neuromodulation. Int Urogynecol J. 2010;21(Suppl 2):S439–46. doi: 10.1007/s00192-010-1273-3. [DOI] [PubMed] [Google Scholar]
- 11.Cardarelli S, D'Elia C, Cerruto MA, Curti P, Ostardo E, Signorello D, et al. Efficacy of sacral neuromodulation on urological diseases: A multicentric research project. Urologia. 2012;79:90–6. doi: 10.5301/RU.2012.9278. [DOI] [PubMed] [Google Scholar]
- 12.De Ridder D, Ost D, Bruyninckx F. The presence of Fowler's syndrome predicts successful long-term outcome of sacral nerve stimulation in women with urinary retention. Eur Urol. 2007;51:229–33. doi: 10.1016/j.eururo.2006.06.031. [DOI] [PubMed] [Google Scholar]
- 13.Spinelli M, Sievert KD. Latest technologic and surgical development in using InterStim therapy for sacral neuromodulation: Impact on treatment success and safety. Eur Urol. 2008;54:1287–96. doi: 10.1016/j.eururo.2008.01.076. [DOI] [PubMed] [Google Scholar]
- 14.Swinn MJ, Kitchen ND, Goodwin RJ, Fowler CJ. Sacral neuromodulation for women with Fowler's syndrome. Eur Urol. 2000;38:439–43. doi: 10.1159/000020321. [DOI] [PubMed] [Google Scholar]
- 15.Leng WW, Chancellor MB. How sacral nerve stimulation neuromodulation works. Urol Clin North Am. 2005;32:11–8. doi: 10.1016/j.ucl.2004.09.004. [DOI] [PubMed] [Google Scholar]
- 16.DasGupta R, Fowler CJ. Urodynamic study of women in urinary retention treated with sacral neuromodulation. J Urol. 2004;171:1161–4. doi: 10.1097/01.ju.0000113201.26176.8f. [DOI] [PubMed] [Google Scholar]
- 17.van Voskuilen AC, Oerlemans DJ, Weil EH, de Bie RA, van Kerrebroeck PE. Long term results of neuromodulation by sacral nerve stimulation for lower urinary tract symptoms: A retrospective single center study. Eur Urol. 2006;49:366–72. doi: 10.1016/j.eururo.2005.11.009. [DOI] [PubMed] [Google Scholar]
- 18.Elhilali MM, Khaled SM, Kashiwabara T, Elzayat E, Corcos J. Sacral Neurobodulation: Long-term experience of one center. Urology. 2005;65:1114–17. doi: 10.1016/j.urology.2004.12.016. [DOI] [PubMed] [Google Scholar]
- 19.White WM, Dobmeyer-Dittrich C, Klein FA, Wallace LS. Sacral nerve stimulation for treatment of refractory urinary retention: Long-term efficacy and durability. Urology. 2008;71:71–4. doi: 10.1016/j.urology.2007.08.034. [DOI] [PubMed] [Google Scholar]
- 20.Bosch JL. Electrical neuromodulatory therapy in female voiding dysfunction. BJU Int. 2006;98(Suppl 1):43–8. doi: 10.1111/j.1464-410X.2006.06316.x. [DOI] [PubMed] [Google Scholar]
- 21.Everaert K, Kerckhaert W, Caluwaerts H, Audenaert M, Vereecke H, De Cuypere G, et al. A prospective randomized trial comparing the 1-stage with the 2-stage implantation of a pulse generator in patients with pelvic floor dysfunction selected for sacral nerve stimulation. Eur Urol. 2004;45:649–54. doi: 10.1016/j.eururo.2003.11.015. [DOI] [PubMed] [Google Scholar]
- 22.Datta SN, Chaliha C, Singh A, Gonzales G. Sacral neurostimulation for urinary retention: 10-year experience from one UK centre. BJU Int. 2007;101:192–6. doi: 10.1111/j.1464-410X.2007.07282.x. [DOI] [PubMed] [Google Scholar]
- 23.Janknegt RA, Weil EH, Eerdmans PH. Improving neuromodulation technique for refractory voiding dysfunctions: Two-stage implant. Urology. 1997;49:358–62. doi: 10.1016/S0090-4295(96)00506-7. [DOI] [PubMed] [Google Scholar]
- 24.Scheepens WA, Van Koeveringe GA, De Bie RA, Weil EH, Van Kerrebroeck PE. Long-term efficacy and safety results of the two-stage implantation technique in sacral neuromodulation. BJU Int. 2002;90:840–5. doi: 10.1046/j.1464-410x.2002.03028.x. [DOI] [PubMed] [Google Scholar]
- 25.Spinelli M, Giardiello G, Gerber M, Arduini A, van den Hombergh U, Malaguti S. New sacral modulation leads for percutaneous implantation using local anesthesia. Description and first experience. J Urol. 2003;170:1905–7. doi: 10.1097/01.ju.0000092634.64580.9a. [DOI] [PubMed] [Google Scholar]
- 26.Hijaz A, Vasavada SP, Daneshgari F, Frinjari H, Goldman H, Rackley R. Complications and troubleshooting of two-stage sacral neuromodulation therapy: A single-institution experience. Urology. 2006;68:533–7. doi: 10.1016/j.urology.2006.03.020. [DOI] [PubMed] [Google Scholar]
- 27.Blandon RE, Gebhart JB, Lightner DJ, Klingele CJ. Re-operation rates after permanent sacral nerve stimulation for refractory voiding dysfunction in women. BJU Int. 2008;101:1119–23. doi: 10.1111/j.1464-410X.2007.07426.x. [DOI] [PubMed] [Google Scholar]
- 28.Al-zahrani AA, Elzayat EA, Gajewski JB. Long-term outcome and surgical interventions after sacral neuromodulation implant for lower urinary tract symptoms: 14-year experience at 1 center. J Urol. 2011;185:981–6. doi: 10.1016/j.juro.2010.10.054. [DOI] [PubMed] [Google Scholar]
- 29.Weil EH, Ruiz-Cerdá JL, Eerdmans PH, Janknegt RA, Bemelmans BL, van Kerrebroeck PE. Sacral root neuromodulation in the treatment of refractory urinary urge incontinence: A prospective randomized clinical trial. Eur Urol. 2000;37:161–71. doi: 10.1159/000020134. [DOI] [PubMed] [Google Scholar]


