Abstract
Radiation therapy is widely used as adjuvant or primary treatment modality of neoplastic lesions. Radiation therapy may cause an acute adverse effect such as brain edema, radiation necrosis, or delayed, for example, panhypopituitarism, vasculitis, and rare de-novo neoplasm development. However, radiation-induced meningioma (RIM) occurrence is extremely rare. A detailed PubMed and Medline search yielded only three isolated Case-reports of RIM development in craniopharyngioma cases receiving radiotherapy after surgery. All cases occurred in patients < 13-year age, with male preponderance, detected after a mean interval of 23-year, the range being 2–44 years. Two had solitary while the third had multiple meningiomas. Authors report an 8-year-old female, who was operated for craniopharyngioma and received adjuvant therapy, was asymptomatic for next 30 years, met a road traffic accident and magnetic resonance imaging brain revealed incidental right sphenoid wing en plaque meningioma. She was planned for gamma-knife therapy as unwilling for surgical intervention. Management of RIM development after radiotherapy of craniopharyngioma along with pertinent literature is reviewed briefly.
Keywords: 30 years free survival, asymptomatic en plaque meningioma, craniopharyngioma, radiation-induced meningioma
Introduction
Cranial radiation therapy is widely used as either adjuvant or primary treatment of central nervous system neoplasm including glioma, ependymoma, medulloblastoma, and benign meningioma, pituitary adenoma and metastatic tumor. Previously, cranial radiation was also commonly used for management of tinea capitis and chronic myeloid leukemia.[1,2,3] Radiation therapy of head can produce acute or long-term adverse effects. Radiation-induced meningioma (RIM) was first described by Mann et al. 1953, and it constitutes a separate entity comparing to the sporadic occurrence.[3] Sporadic meningioma is usually considered as a benign tumor, accounting for approximately 20% of intracranial tumors and tends to affect middle-aged females. Sporadic meningioma constitutes about 90% of benign meningioma while atypical and anaplastic type accounts for 5% and 3%, respectively. However, RIM, are considered rare and about total 750 odd cases are reported till date.[4,5,6,7]
The latency period of tumor development in the RIM depends on initial total radiation dosage and timing.[8,9] On the basis of the initial dose of radiotherapy prescribed, Harrison et al.[4] categorized cases into three groups, low-dose group receiving (<10 Gy), intermediate (10–20 Gy), and high (more than 20 Gy) and the time period of latency is about 35, 26, and 19–24 years, respectively for low-, medium-, and high-radiation dosage groups, showing an inverse dose-response relation curve.[4,5] Authors report a unique, interesting case, an 8-year-old girl received high-dose fractionated external beam radiotherapy for residual craniopharyngioma, after 30 years had met an accident presented and imaging picked up incidentally on RMI.
Case Report
An 8-year-old girl presented with a complaint of visual deterioration; imaging revealed suprasellar supradiaphragmatic cystic craniopharyngioma underwent stereotactic aspiration of cystic lesion and received 60 Gy external beam radiotherapy in the postoperative for residual 30-year back at our institute. She lost follow-up as she was asymptomatic. After 30-year following radiotherapy, she reported with a complaint of retro-orbital pain over the right eye and headache for last 6 months following minor head injury. On evaluation at current follow-up, visual acuity was 6/9 bilaterally; rest of the neurological examination was essentially within normal limits.
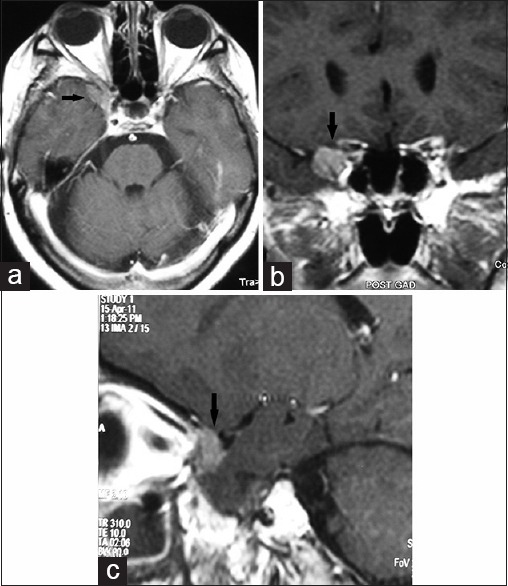
Noncontrast computed tomography scan head revealed a mass lesion at the right orbital apex with intracranial extension. Magnetic resonance imaging brain contrast enhancement, axial, coronal section images revealed presence of heterogeneous mass lesion in the sella with suprasellar extension [Figure 1a–c]. In addition, it also revealed en plaque meningioma involving the right medial sphenoid wing [Figure 2] with right intraorbital extension in the axial image. Compared to previous follow-up scans carried at 3 years before the current visit, a diagnosis of RIM was based on neuroimaging. She was given the option of surgery or gamma knife, she preferred and planned for gamma knife radiosurgery, in view of good visual acuity. She is clinically stable for past 6 months.
Figure 1.

Magnetic resonance imaging study of brain after gadolinium administration axial (a), coronal (b), and sagittal (c) sections images showing presence of small residual craniopharyngioma in suprasellar supradiaphragmatic region, 30 years following surgery and adjuvant therapy (arrows)
Figure 2.
Gadolinium-enhanced magnetic resonance imaging of brain with axial (a), coronal (b), and sagittal (c) sections demonstrating en plaque right sphenoid wing meningioma with extension into the right orbit (small arrows)
Discussion
Cranial irradiation has been utilized as therapeutic modalities of neoplastic as well as tinea capitis.[1,7,10,11,12,13] Radiation therapy can be associated with adverse effect occurring immediately, for example, brain edema, radiation necrosis, however, rarely can also happen after a relatively long period of interval such as vasculitis, panhypopituitarism, and rarely new neoplasm development.[14,15,16] The oncogenic potential of radiation is well-known hazard commonly encountered in atomic bomb survivors, work place-related exposure, or therapeutic intervention.
Development of a radiation-induced neoplasm is considered as relatively rare, and these includes relatively more common developing intracranial meningioma, sarcoma, and glioma comparing to the rarer ependymoma, schwannoma, primitive neuroectodermal tumor, and pituitary adenoma can also develop.[17,18,19]
Usually, RIM occurs in association with the primary radiation therapy of acute lymphoblastic leukemia, tinea capitis[6] and intracranial malignancy, for example, medulloblastoma, primitive neuroectodermal epithelial tumors, and ependymoma.[7] However, RIM occurrence is much rarer following radiation therapy of benign lesions such as pituitary adenoma,[13,20] and extremely rare in cases of craniopharyngioma.[9]
The diagnosis of RIM is based on generalized Cahan's criteria,[1] which was modified by Schrantz and Araoz in 1972.[21] The radiation-induced lesions should be located within the field of previous radiation therapy and also these should not exit before radiation therapy and usually occur after a gap of reasonable long-time interval usually more than 5 years of the previous radiation therapy. Other criteria are the development of histologically distinct neoplasm, and final criteria include the absence of any known familial or genetic predisposing factors promoting the development of the multiple or secondary malignancies.[1,2]
RIM is characterized by distinct clinical and radiobiologic features compared to the sporadic meningioma.[6] RIM tends to occur in the relatively younger age, characterized by the occurrence of multiple meningiomas located within the field of radiotherapy, possessing more aggressive clinically, course and higher recurrence rate following surgical resection and calvarial location compared with sporadic meningiomas, histopathologically more malignant features.[6] Radio-biologic aggressiveness of RIM is can be assessed with positron emission tomography scan with fluorodeoxyglucose and result outcome positively correlates with aggressive pattern glucose uptake utilization.[10] Cytogenetic abnormalities linked to RIM are deletions of 6p or 7p, loss of 1p chromosome, and less more common being a loss of chromosome 22.[11,12,13,14]
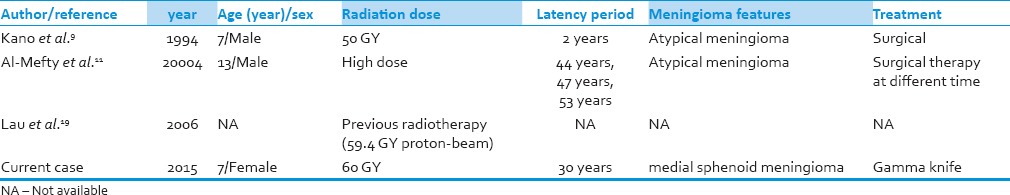
In the PubMed literature search of RIM following craniopharyngioma treatment, authors found only three isolated cases reports. There were two males, and one case had no mention of sex, our case was female. All case received radiotherapy when patients were in their first decade of life, regarding dosage, all received high dosage in addition case reported by Luu et al. had also received additional 59.8 Gy proton beam therapy. Latency period varied from 2 years to 53 years. RIM can be focal or multiple; it was focal in two cases and multiple in one case with a series of successive occurrence meningiomas occurred at 44, 47, and 53 years, respectively after initial radiotherapy [Table 1]. RIM can develop even after a very long period of latency up to six decades after radiation therapy.[18,19,20]
Table 1.
Summary of previously reported of craniopharyngioma cases developing radiation induced meningioma
Authors also previously reported an interesting case of occurrence of radiation-induced pituitary adenoma in survivor of brainstem glioma, who first underwent surgery and radiation therapy of brain stem glioma, later he developed pituitary adenoma and underwent successful transsphenoidal surgery.[13]
Management of RIM possesses a special challenge. Surgical resection of the meningioma remains the mainstay of treatment. Surgical management is favored in cases with easily accessible area, limited number of meningioma, availability of an easy and safe corridor. However, surgery may not be safer and complete resection may not be feasible in cases with multiple lesions, the involvement of adjacent bone and dural sinuses, encasement of vessels, nerves or aggressive behavior.[7] In selected groups of RIMs, where surgery is contraindicated, or recurrence of RIM, the primary or secondary gamma-knife therapy can be a suitable alternative option of management. Gamma knife can provide about 94.1% and 80.7% overall survival at 3 and 5 years, respectively with limited side effect and reasonable control of the size of RIM.[15] Kuhn et al. reported 100% local control of RIM in their study involving 12 patients, who received gamma knife radiosurgery, with a mean follow-up of 35 months.[16] However, fractionated radiotherapy can be another modality option available.[17]
The current reported case is unique, fourth case of craniopharyngioma, with 30-year of latency period as well as disease free craniopharyngioma survival, detected incidentally with imaging study is extremely unusual occurrence. Considering the possibility of delayed occurrence of RIM in such patients, long-term surveillance is necessity for early diagnosis and optimum management.[17,18,19,20] Significant progress in the field of radiation oncology led to more targeted and conformal therapy, however, long-term follow-up is required to assess the impact on the development of RIM.[18,19]
Conclusion
RIM is one of the important long-term sequelae of high-dose cranial radiotherapy prescribed especially in younger age group. A high degree of suspicion and regular life-long follow-up supplemented with periodic neuroimaging study is advised for early detection. The possibility of RIM or other neoplasm should be kept as a possibility in patients presenting with recurrent or new onset symptoms, seizure or mass effect in long-term survivor of intracranial lesion, who received radiation therapy in the past. Early diagnosis and prompt management may provide optimal neurological outcome.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Cahan WG, Woodard HQ, Higinbotham NL, Stewart FW, Coley BL. Sarcoma arising in irradiated bone: Report of eleven cases 1948. Cancer. 1998;82:8–34. doi: 10.1002/(sici)1097-0142(19980101)82:1<8::aid-cncr3>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 2.Jensen AW, Brown PD, Pollock BE, Stafford SL, Link MJ, Garces YI, et al. Gamma knife radiosurgery of radiation-induced intracranial tumors: Local control, outcomes, and complications. Int J Radiat Oncol Biol Phys. 2005;62:32–7. doi: 10.1016/j.ijrobp.2004.09.033. [DOI] [PubMed] [Google Scholar]
- 3.Mann I, Yates PC, Ainslie JP. Unusual case of double primary orbital tumour. Br J Ophthalmol. 1953;37:758–62. doi: 10.1136/bjo.37.12.758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Harrison MJ, Wolfe DE, Lau TS, Mitnick RJ, Sachdev VP. Radiation-induced meningiomas: Experience at the Mount Sinai Hospital and review of the literature. J Neurosurg. 1991;75(4):564–74. doi: 10.3171/jns.1991.75.4.0564. [DOI] [PubMed] [Google Scholar]
- 5.Salvati M, Cervoni L, Puzzilli F, Bristot R, Delfini R, Gagliardi FM. High-dose radiation-induced meningiomas. Surg Neurol. 1997;47:435–41. doi: 10.1016/s0090-3019(96)00360-6. [DOI] [PubMed] [Google Scholar]
- 6.Sadetzki S, Flint-Richter P, Ben-Tal T, Nass D. Radiation-induced meningioma: A descriptive study of 253 cases. J Neurosurg. 2002;97:1078–82. doi: 10.3171/jns.2002.97.5.1078. [DOI] [PubMed] [Google Scholar]
- 7.Umansky F, Shoshan Y, Rosenthal G, Fraifeld S, Spektor S. Radiation-induced meningioma. Neurosurg Focus. 2008;24:E7. doi: 10.3171/FOC/2008/24/5/E7. [DOI] [PubMed] [Google Scholar]
- 8.Partington MD, Davis DH. Radiation-induced meningioma after treatment for pituitary adenoma: Case report and literature review. Neurosurgery. 1990;26:329–31. doi: 10.1097/00006123-199002000-00025. [DOI] [PubMed] [Google Scholar]
- 9.Kano T, Zama A, Ono N, Nakamura T, Tamura M, Ohe T, et al. A juvenile case of radiation-induced meningioma two years after radiation for craniopharyngioma. No Shinkei Geka. 1994;22:367–70. [PubMed] [Google Scholar]
- 10.Kado H, Ogawa T, Hatazawa J, Iwase M, Kanno I, Okudera T, et al. Radiation-induced meningioma evaluated with positron emission tomography with fludeoxyglucose F 18. AJNR Am J Neuroradiol. 1996;17:937–8. [PMC free article] [PubMed] [Google Scholar]
- 11.Al-Mefty O, Topsakal C, Pravdenkova S, Sawyer JR, Harrison MJ. Radiation-induced meningiomas: Clinical, pathological, cytokinetic, and cytogenetic characteristics. J Neurosurg. 2004;100:1002–13. doi: 10.3171/jns.2004.100.6.1002. [DOI] [PubMed] [Google Scholar]
- 12.Brassesco MS, Valera ET, Neder L, Castro-Gamero AM, de Oliveira FM, Santos AC, et al. Childhood radiation-associated atypical meningioma with novel complex rearrangements involving chromosomes 1 and 12. Neuropathology. 2009;29:585–90. doi: 10.1111/j.1440-1789.2008.00991.x. [DOI] [PubMed] [Google Scholar]
- 13.Kurwale NS, Ahmad FU, Satyarthi G, Suri A, Mahapatra AK. Can radiation induce pituitary tumors? Giant prolactinoma after radiation exposure. J Clin Neurosci. 2008;15:1287–8. doi: 10.1016/j.jocn.2007.08.029. [DOI] [PubMed] [Google Scholar]
- 14.Shoshan Y, Chernova O, Juen SS, Somerville RP, Israel Z, Barnett GH, et al. Radiation-induced meningioma: A distinct molecular genetic pattern? J Neuropathol Exp Neurol. 2000;59:614–20. doi: 10.1093/jnen/59.7.614. [DOI] [PubMed] [Google Scholar]
- 15.Kondziolka D, Kano H, Kanaan H, Madhok R, Mathieu D, Flickinger JC, et al. Stereotactic radiosurgery for radiation-induced meningiomas. Neurosurgery. 2009;64:463–9. doi: 10.1227/01.NEU.0000336765.85922.D9. [DOI] [PubMed] [Google Scholar]
- 16.Kuhn EN, Chan MD, Tatter SB, Ellis TL. Gamma knife stereotactic radiosurgery for radiation-induced meningiomas. Stereotact Funct Neurosurg. 2012;90:365–9. doi: 10.1159/000339636. [DOI] [PubMed] [Google Scholar]
- 17.Galloway TJ, Indelicato DJ, Amdur RJ, Swanson EL, Morris CG, Marcus RB. Favorable outcomes of pediatric patients treated with radiotherapy to the central nervous system who develop radiation-induced meningiomas. Int J Radiat Oncol Biol Phys. 2011;79:117–20. doi: 10.1016/j.ijrobp.2009.10.045. [DOI] [PubMed] [Google Scholar]
- 18.Kleinschmidt-DeMasters BK, Lillehei KO. Radiation-induced meningioma with a 63-year latency period. Case report. J Neurosurg. 1995;82:487–8. doi: 10.3171/jns.1995.82.3.0487. [DOI] [PubMed] [Google Scholar]
- 19.Luu QT, Loredo LN, Archambeau JO, Yonemoto LT, Slater JM, Slater JD. Fractionated proton radiation treatment for pediatric craniopharyngioma: Preliminary report. Cancer J. 2006;12:155–9. [PubMed] [Google Scholar]
- 20.Ron E, Modan B, Boice JD, Jr, Alfandary E, Stovall M, Chetrit A, et al. Tumors of the brain and nervous system after radiotherapy in childhood. N Engl J Med. 1988;319:1033–9. doi: 10.1056/NEJM198810203191601. [DOI] [PubMed] [Google Scholar]
- 21.Schrantz JL, Araoz CA. Radiation induced meningeal fibrosarcoma. Arch Pathol. 1972;93:26–31. [PubMed] [Google Scholar]


