Abstract
This systematic review wasdesigned to compare the complications of acoustic neuroma surgery via the suboccipital retrosigmoid approach in the sitting versus lateral positions. Searches for randomized trials and observational studies about the complications of acoustic neuroma surgery were performed in five medical databases (though October 2015) including PubMed, MEDLINE (In-Process and Other Non-Indexed Citations), EMBASE, Cochrane Central Register of Controlled Trials (CENTRAL) and PsycINFO. Primary outcomes in this study were venous air emboli, neuropsychological defects, CSF leak, facial and abducens nerves palsy, postoperative deafness, hydrocephalus and mortality. Secondary outcomes were total tumor removal, facial and cochlear nerves preservation and ataxia. 843 abstracts and titles were reviewed and 10 studies (two non-randomized comparative studies and 8 non-comparative case series) were included for data extraction. Because of the heterogeneity of the studies, small number of participants and methodological shortcomings, findings were evaluated qualitatively. No impressive advantage was found in surgical or neurological outcomes for use of the sitting or lateral positions in patients with acoustic neuroma surgery. According to the available evidence, it seems that both sitting and lateral positions can be used with an equivalent safety for acoustic neuroma surgery via the retrosigmoid suboccipital approach. There seems a clear need for comparative studies to compare harms and other outcomes for these two positions.
Keywords: Acoustic neuroma, complications, retrosigmoid approach, vestibular schwannoma
Introduction
Acoustic neuroma or vestibular schwannoma is a cerebellopontine angle (CPA) tumor that accounts for 6–8% of all intracranial tumors.[1] About 78% of all CPA tumors are reported to be an acoustic neuroma. In the last two decades, improvements have been achieved in the results of skull base surgeries presumably due to advances in diagnostic methods, anesthesia, microsurgery techniques, and cranial nerve monitoring during surgery.[2] However, there remains controversy about optimal surgical techniques, including the position (sitting, supine, lateral) and the approach (suboccipital retromastoid, translabyrinthine, middle fossa) of the surgery.
The suboccipital retrosigmoid approach is the most commonly used surgical approach used for acoustic neuroma tumor surgery and other CPA tumors.[3] This approach enables rapid and accurate identification of the tumor and wide exposure to the posterior fossa.[4] The main indication for the suboccipital retrosigmoid approach is an acceptable preoperative hearing and extracanalicular tumors < 15 mm. However, this approach is commonly used for a broad range of acoustic neuromas from intracanalicular to tumors larger than 4 cm.[4] The surgery is commonly performed with the patient either in the sitting or lateral position. Posterior fossa surgery in the sitting position has some potential advantages over the lateral position, such as easier access to the operative field, better venous drainage, and easier monitoring of the cranial nerves. However, there are potential disadvantages including postural hypotension and cardiac arrhythmias.[5] In addition, there are some reports of venous air emboli in patients who have undergone surgeries in the sitting position.[6]
Because of the potential risks, only 40% of surgeons in Germany prefer to do posterior fossa surgeries in the sitting position[7] and the presence of a patent foramen ovale is considered as a contraindication to neurosurgery in the sitting position.[6]
The purpose of this study was to review the comparative risks of acoustic neuroma surgery via the suboccipital retrosigmoid approach in the sitting versus lateral positions systematically.
Methods
Literature searches were performed in February 2013 and then updated in October 2015 on five electronic databases including PubMed, MEDLINE (In-Process and Other Non-Indexed Citations), EMBASE, Cochrane Central Register of Controlled Trials, and PsycINFO. A medical librarian designed our search strategies with the assistance of a neurosurgeon and a medical doctor. There were 843 abstracts after removal of duplicates. Electronic searches were supplemented by reviews of reference lists and suggestions from experts.
We included studies about acoustic neuroma/vestibular schwannoma surgery performed via the suboccipital retrosigmoid approach that reported complications in the sitting or lateral positions. Primary outcomes of our study were venous air emboli, neuropsychological defects, cerebrospinal fluid (CSF) leak, facial and abducens nerves palsy, postoperative deafness, hydrocephalus, and mortality. Secondary outcomes were total tumor removal, facial, and cochlear nerves preservation and ataxia. We included randomized and nonrandomized clinical trials, cohort studies (retro- or prospective), and uncontrolled surgical series. We excluded case reports and case series with sample sizes less than ten patients in addition to studies that did not report data for acoustic neuroma surgery performed via the suboccipital retrosigmoid or did not describe the surgical approach or position.
We classified surgeries performed with patients in the sitting or semi-sitting positions as sitting surgery group, and surgeries performed with patients in the supine, horizontal, or lateral decubitus positions as lateral surgery group.
Critical appraisal (quality assessment) and evidence synthesis
Because of the heterogeneity of the studies, small number of participants and methodological shortcomings (no randomized trials and only two comparative observational studies), we decided not to pool the studies. Rather, we synthesized data qualitatively based on the GRADE approach as described in guidelines from the Cochrane Back Review Group.[8] We assessed the level of evidence (LoE) based on study limitations (quality), consistency, precision, and directness to determine an overall grade (very low, low, moderate, or high). Since the quality of the studies have not been adjusted for confounders, we would have to rate them as high risk of bias on that basis.
Results
Searches identified 843 abstracts after de-duplication. All 843 abstracts were reviewed for inclusion by two investigators [Figure 1]. After full-text review, ten studies met inclusion criteria. The characteristics of the ten included studies including sample sizes, type of positions, countries where the surgeries performed in, variation in the general approaches and any relevant patient or tumor characteristics (age, sex, tumor size, etc.) are shown in Table 1. We identified no randomized trials and two nonrandomized retrospective comparative studies by Duke et al. (n = 432) and Spektor et al. (n = 130). Eight noncomparative surgical series (n = 22–962) reported complication rates following surgery performed in either the sitting or lateral positions. Table 2 shows a summary of the results from the ten included studies.
Figure 1.

Flow diagram of studies based on the PRISMA statement. *Supplemental content 2. **Including studies on cadavers, studies about auditory brainstem implant or irrelevant methods of surgery. ***Supplemental content 3
Table 1.
Characteristic of the final original included studies
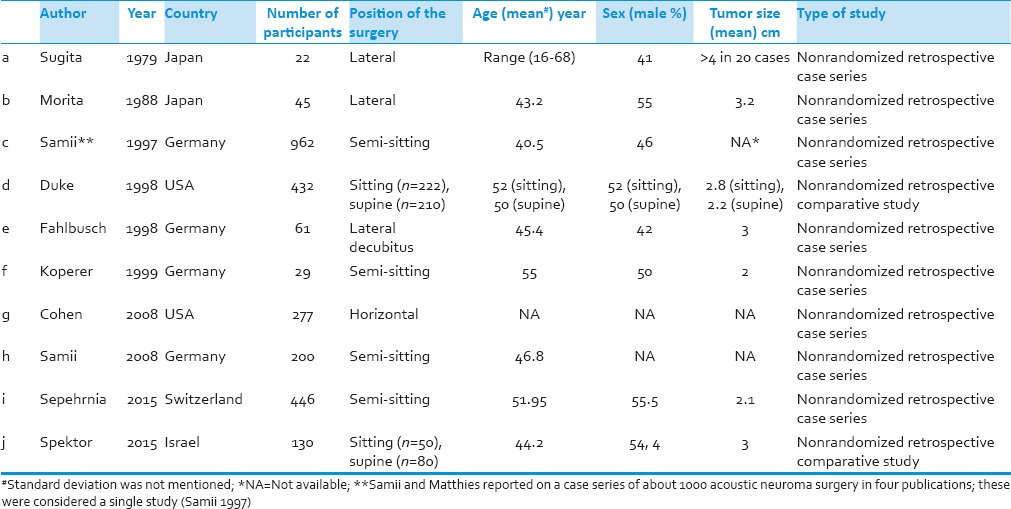
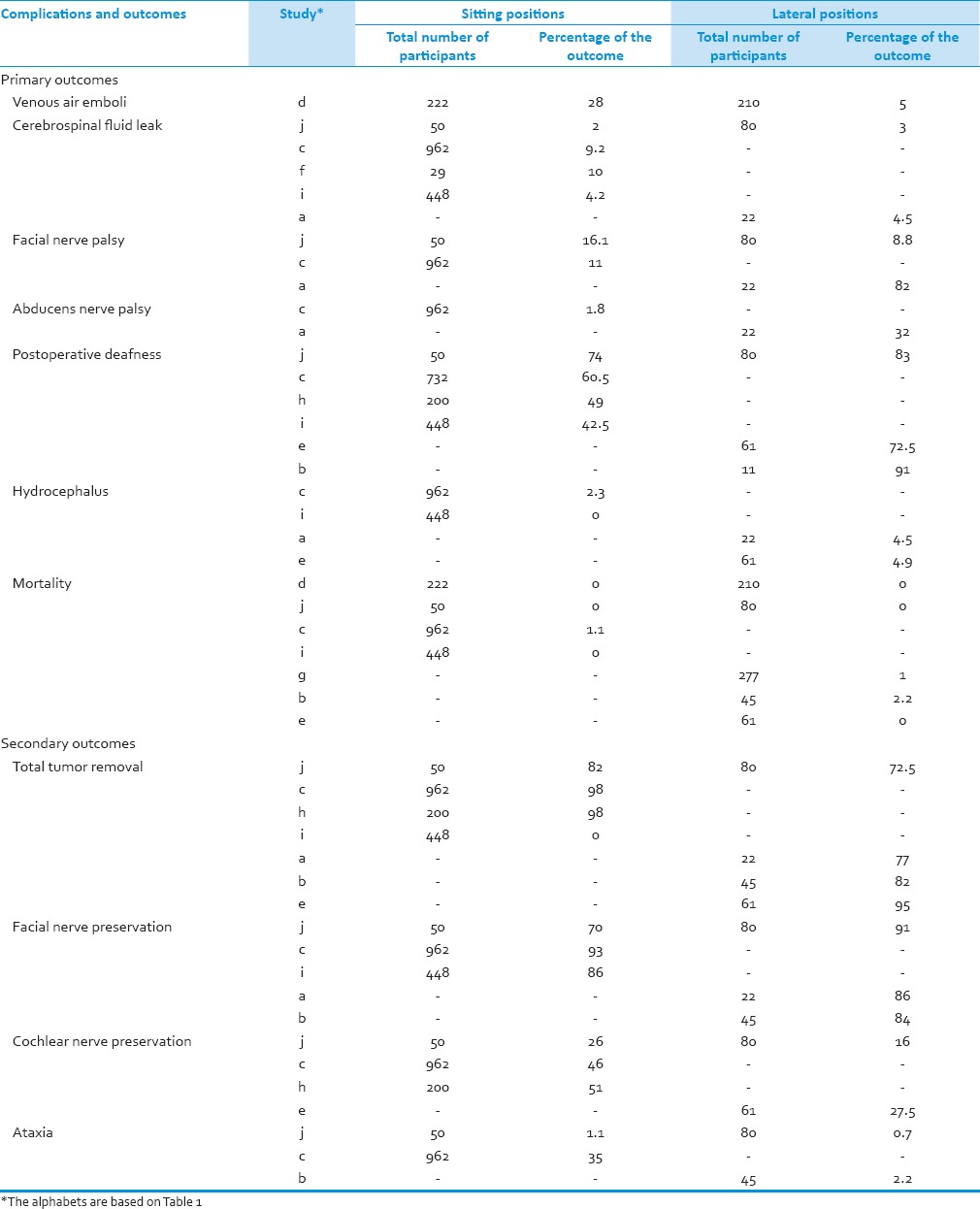
Table 2.
Complications and outcomes of acoustic neuroma surgery with the suboccipital retrosigmoid approach based on the position of the surgery
Primary outcomes
Primary outcome (PO) 1: Venous air emboli
One nonrandomized comparative study (Duke 1998) (n = 432) found acoustic neuroma surgery associated with higher risk of venous air emboli in the sitting position (28%) versus the lateral position (5%) (risk ratio 5.86, 95% confidence interval 3.09–11.13). The LoE was graded very low due to high risk of bias and imprecision, with results based on only one study.
PO2: Neuropsychological assessments
No study reported complications as determined by neuropsychological assessments (LoE: Insufficient).
PO3: Cerebrospinal fluid leak
One nonrandomized comparative study (Spektor et al.) (n = 130) reported 3.1% CSF leak in the sitting (2%) and lateral (3%) positions. The difference was not statistically significant (P = 1.00). Three noncomparative studies (Samii 1997; Sepehrnia 2015 and Koperer 1999) (n = 962,448 and 29) reported CSF leak rates of 9.2%, 4.2%, and 10% following surgery performed in the sitting position, respectively. One study (Sugita 1979) (n = 22) reported a rate of 4.5% following surgery performed in the lateral position. The LoE for this and all other outcomes was graded insufficient since all findings were based on cross-study comparisons.
PO4: Facial nerve palsy
One nonrandomized comparative study (Spektor 2015) (n = 130) found acoustic neuroma surgery associated with a higher facial nerve palsy (House–Brackmann score ≥III) in the sitting position (16.1%) versus the lateral position (8.8%) (P = 0.002). The LoE was graded very low due to high risk of bias and imprecision, with results based on only one study. One noncomparative study (Samii 1997) (n = 962) reported a rate of 11% for facial nerve palsy (7% due to facial nerve discontinuity and 4% despite nerve continuity) following surgery performed in the sitting position and one study (Sugita 1979) (n = 22) reported a rate of 82% facial nerve palsy following surgery performed in the lateral position.
PO5: Abducens nerve palsy
No comparative study reported rates of abducens nerve palsy. One noncomparative study (Samii 1997) (n = 962) reported a rate of 1.8% abducens nerve palsy following surgery performed in the sitting position and one study (Sugita 1979) (n = 22) reported a rate of 32% following surgery performed in the lateral position.
PO6: Postoperative deafness
One nonrandomized comparative study (Spektor et al.) (n = 130) reported acoustic neuroma surgery associated with 80% postoperative deafness either in sitting (74%) or lateral (83%) positions. The difference was not statistically significant (P = 0.27). Three noncomparative studies (Samii 1997; Sepehrnia 2015, and Samii 2008) (n = 200, 448, and 732) reported that 49%, 42.5%, and 60% of patients did not have functional hearing preservation following surgery performed in the sitting position, respectively. Two studies (Fahlbusch 1998; Morita 1988) (n = 61 and n = 11) reported rates of postoperative deafness 72% and 91% following surgery in the lateral position.
PO7: Hydrocephalus
No comparative study reported rates of hydrocephalus. Two noncomparative studies (Samii 1997; Sepehrnia 2015) (n = 962, 448) reported hydrocephalus in 2.3% and 0% of patients following surgery in the sitting position and two studies (Sugita 1979; Fahlbusch 1998) (n = 22 and 61) reported rates of hydrocephalus 4.5% and 4.9% following surgery in the lateral position.
PO8: Mortality
Two nonrandomized comparative studies (Duke 1998, Spektor 2015) (n = 432 and 130) reported no surgical mortalities in patients following surgery in the sitting or lateral positions. The LoE was graded low, due to high risk of bias and imprecision, with results based on two studies. Three noncomparative studies (Samii 1997; Sepehrnia 2015; Cohen 2008) (n = 962, 448, and 277) reported mortality of 1.1%, 0%, and 1% following surgery in the sitting position and two studies (Fahlbusch 1998; Morita 1988) (n = 61 and 45) reported mortality of 0% and 2.2% following surgery in the lateral position.
Secondary outcomes
Secondary outcome (SO)1: Total tumor removal
One nonrandomized comparative study (Spektor et al.) (n = 130) reported acoustic neuroma surgery associated with 76.2% total tumor removal (82% in sitting and 72.5% in lateral position). The difference was not statistically significant (P = 0.29). Three noncomparative studies (Samii 1997; Sepehrnia 2015; and Samii 2008) (n = 962, 448, and 200) reported the rate of total tumor removal 98%, 100%, and 98% in sitting position and three studies (Fahlbusch 1998, Morita 1988, Sugita 1979) (n = 61, 45, and 22) reported rates of total tumor removal of 95%, 82%, and 77% in lateral position, respectively.
SO2: Facial nerve preservation
One nonrandomized comparative study (Spektor 2015) (n = 130) found acoustic neuroma surgery associated with a better facial nerve preservation (House–Brackmann score I and II) in the lateral position (91%) versus the sitting position (70%) (P = 0.002). The LoE was graded to very low due to high risk of bias and imprecision, with results based on only one study. In uncontrolled studies, two noncomparative study (Samii 1997; Sepehrnia 2015) (n = 962, 448) reported a rate of 93% and 86% facial nerve preservation in the sitting position and two studies (Morita 1988; Sugita 1979) (n = 45 and 22) reported a rate of 84% and 86% facial nerve preservation in the lateral position.
SO3: Cochlear nerve preservation
One nonrandomized comparative study (Spektor et al.) (n = 130) reported 19% of cochlear nerve preservation (26% in sitting and 16% in lateral position). The difference was not statistically significant (P = 0.27). Two noncomparative studies (Samii 1997 and Samii 2008) (n = 962 and 200) reported rates of 68% and 76% for anatomical cochlear nerve preservation and 46% and 51% for functional cochlear nerve preservation the following surgery in the sitting position. While the study by Fahlbusch et al. (n = 61) reported cochlear nerve presentation 27.5% in the lateral position
SO4: Ataxia
One nonrandomized comparative study (Spektor et al.) (n = 130) reported 0.8% ataxia (1.1% in sitting and 0.7% in lateral position). This difference was not statistically significant (P = 0.1). One noncomparative study (Samii 1997) (n = 962) reported a rate of 35% for ataxia (imbalance while walking) following surgery in the sitting position and one study (Morita 1988) (n = 45) reported a rate of 2.2% for this complication in the lateral position.
Other complications and outcomes
One noncomparative study (Samii 1997) (n = 962) reported disturbances of the cochlear (95%), vestibular (61%), trigeminal (9%), facial (6%), and caudal cranial nerves (2.7%) as the most frequent clinical symptoms following surgery in the sitting position. This study also reported one case of tetraparesis, 1% hemiparesis, and 5.5% caudal cranial nerve palsy and 2.2% hematomas, 1.2% bacterial meningitis, and 1.1% wound revisions. The most frequent complaint during the first 2–8 postsurgical weeks were a headache in 9%, swallowing difficulties in 4.5%, tinnitus in 35%, and dizziness or unsteadiness in 56% of patients.
One nonrandomized comparative study (Duke 1998) (n = 232) reported intraoperative hypotension in 1.8% of patients who underwent surgery in the sitting position and 1.4% of those who underwent surgery in the lateral position.
Discussion
No randomized clinical trial compared complications of acoustic neuroma surgery via the suboccipital retrosigmoid approach performed with patients in the sitting versus lateral position. In the only available nonrandomized comparative study, Duke et al. reported venous air emboli as a complication of the acoustic neuroma surgery with suboccipital retrosigmoid approach 28% in the sitting position and 5% in the lateral position (P < 0.0001). We downgraded the LoE to very low due to the retrospective design, high risk of bias and imprecision in estimates. Moreover, no adjustment for confounders was performed. The only other data are from noncomparative series of patients who underwent surgery either in the sitting of lateral position. Evidence from such cross-study comparisons is very weak and insufficient to determine if one position was associated with more harms than the other.
The incidence of venous air emboli in neurological surgeries in the sitting position is estimated between 10% and 80% and can lead to 1% mortality of the patients.[9,10] A systematic review reported an overall incidence rate of venous air emboli 39% for posterior fossa and 12% for cervical surgery in 4806 neurosurgeries in the sitting position. The rate of venous air emboli from the study comparing two positions was significantly higher in the sitting versus horizontal position (28.4% vs. 5.5%).[6]
We found no paper reporting neuropsychological assessments after acoustic neuroma surgery with the suboccipital retrosigmoid approach. Minovi et al.[11] and Schick et al.[12] reported neuropsychological assessment after acoustic neuroma surgery but with other approaches (transtemporal and middle fossa).
The CSF fluid leak after acoustic neuroma surgery via the retrosigmoid approach may be fairly common, with estimates of between 0% and 27%.[13,14] A meta-analysis by Selesnick et al. estimated CSF leak in 10% of patients following vestibular schwannoma surgery.[15] However, there was insufficient evidence to determine whether the surgical position affects the risk of CSF fluid leak. Mortality rate in acoustic neuroma surgeries is not expected to be more than 1–2%.[4] Standefer reported 30-day mortality rate 2.5% in 488 neurosurgeries in sitting position.[16] In our study, data on mortality was very sparse but appeared consistent with a low mortality rate.
Preservation of hearing is an important goal of acoustic neuroma surgery,[17] but we found insufficient evidence with which to determine effects of position on the likelihood of hearing preservation. Although some studies found smaller tumors associated with higher likelihood of hearing preservation (Samii et al. 2008; Fahlbusch), other studies reported no clear association between tumor size and likelihood of hearing preservation.[18] In addition to tumor size, the location of the tumor may also impact the possibility of hearing preservation. Other serious harms reported in case reports were five quadriplegia,[19] one sciatic neuropathy[20] and one tension pneumocephalous[21] in the sitting position. However, it is not possible to determine the rates of such events from case reports.
Spektor et al. reported all surgical complications associated with acoustic neuroma surgery to be significantly more in lateral position in comparison to sitting.[22] They also emphasized that facial nerve preservation is related to the extent of resection but not to a surgical position. The time required for anesthesiological induction and patient positioning and duration of surgery were significantly shorter in the lateral position.[22] A large meta-analysis by Ansari et al. including 35 studies with 5064 patients, analyzed the incidence of complications depending on the three basic surgical approaches for exposure of vestibular schwannomas: Translabyrinthine, middle fossa, and retrosigmoid. No statistically significant difference was observed in their study for residual tumor, tumor recurrence, mortality, noncranial nerve neurological complications and dysfunction of cranial nerves other than cranial nerves VII and VIII. Based on this data, the retrosigmoid approach seems to be the most effective approach for facial nerve preservation for most tumor sizes but it was associated with a higher risk of postoperative pain and CSF fistula.[23] In summary, the surgical position for this kind of surgery seems to be very subjective to the surgeon preference and we think that it would be hard to plan a randomized control study. The choice of operative position should be based on lesion characteristics and the patient's preoperative medical status as well as the experience and preferences of the surgeons.
Limitations of the study and potential biases
The data are collected from different studies, different surgeons with different methods of surgeries. Therefore, the comparison of the data and pooling them seems not to be reasonable and possible. Because of the heterogeneity of the studies, a small number of participants and not adequate randomization we decided not to pool the results together and we preferred to show them separately [Figures 2 and 3].
Figure 2.
Primary outcome measures
Figure 3.
Secondary outcome measures
We tried our best to cover all possible related data by designing accurate search strategies and screening, but there may be some studies that the exact position or approach of the surgery was not mentioned in the title/abstract of the paper, and we could not include them by our search. For instance, the important case series of Samii et al. in 1997 which was included of about 1000 cases of vestibular schwannoma was not included in our first search results because of not mentioning the position of the surgery and we included them after consulting experts.
The majority of the outcome measures do not seem to be significantly different between the two conditions being tested, and surgeon preference may override the small effect size seen in higher rate of venous air emboli in the sitting position. The overall sparseness of the available data prevents us to make firm conclusions regarding this topic. A potential source of bias is the fact that there are studies that were sometimes performed several decades apart with potential changes or differences in surgical technique and/or perioperative management (e.g. Sugita 1979 and Spektor 2015). There were only two studies in which two conditions were directly tested against each other, albeit in a retrospective fashion, from which some viable yet low confidence conclusions can be drawn. In another word, using a published literature search method to give insight into the important question of whether the operative positioning of the patient has an impact on outcomes of vestibular schwannomas surgical management may not be very feasible currently.
Conclusion
In conclusion, no impressive advantage was found in surgical or neurological outcomes for the use of the sitting or lateral positions in patients with acoustic neuroma surgery. According to the current evidence, it seems both sitting and lateral positions can be used with the same safety for acoustic neuroma surgery via retrosigmoid suboccipital approach. There is a clear need for comparative studies to compare harms and other outcomes with these two positions. If there are differences in risk of complications, research is also needed to identify groups of patients who are likely to do better with one position than the other.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors wish to thank Mr. Farhad Shokraneh for his help in writing search strategies and Dr. Soheil Saadat for his kind help in showing the results.
References
- 1.Jung S, Kang SS, Kim TS, Kim HJ, Jeong SK, Kim SC, et al. Current surgical results of retrosigmoid approach in extralarge vestibular schwannomas. Surg Neurol. 2000;53:370–7. doi: 10.1016/s0090-3019(00)00196-8. [DOI] [PubMed] [Google Scholar]
- 2.Cunningham CD, 3rd, Friedman RA, Brackmann DE, Hitselberger WE, Lin HW. Neurotologic skull base surgery in pediatric patients. Otol Neurotol. 2005;26:231–6. doi: 10.1097/00129492-200503000-00017. [DOI] [PubMed] [Google Scholar]
- 3.da Silva EB, Jr, Leal AG, Milano JB, da Silva LF, Jr, Clemente RS, Ramina R. Image-guided surgical planning using anatomical landmarks in the retrosigmoid approach. Acta Neurochir (Wien) 2010;152:905–10. doi: 10.1007/s00701-009-0553-5. [DOI] [PubMed] [Google Scholar]
- 4.Cohen NL. Retrosigmoid approach for acoustic tumor removal 1992. Neurosurg Clin N Am. 2008;19:239–50, vi. doi: 10.1016/j.nec.2008.02.006. [DOI] [PubMed] [Google Scholar]
- 5.Slbin MS, Babinski M, Maroon JC, Jannetta PJ. Anesthetic management of posterior fossa surgery in the sitting position. Acta Anaesthesiol Scand. 1976;20:117–28. doi: 10.1111/j.1399-6576.1976.tb05018.x. [DOI] [PubMed] [Google Scholar]
- 6.Fathi AR, Eshtehardi P, Meier B. Patent foramen ovale and neurosurgery in sitting position: A systematic review. Br J Anaesth. 2009;102:588–96. doi: 10.1093/bja/aep063. [DOI] [PubMed] [Google Scholar]
- 7.Ramsbacher J, Vesper J, Brock M. Permanent postoperative anosmia: A serious complication of neurovascular decompression in the sitting position. Acta Neurochir (Wien) 2000;142:1259–61. doi: 10.1007/s007010070023. [DOI] [PubMed] [Google Scholar]
- 8.Furlan AD, Pennick V, Bombardier C, van Tulder M. Editorial Board, Cochrane Back Review Group. 2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine (Phila Pa 1976) 2009;34:1929–41. doi: 10.1097/BRS.0b013e3181b1c99f. [DOI] [PubMed] [Google Scholar]
- 9.Matjasko J, Petrozza P, Cohen M, Steinberg P. Anesthesia and surgery in the seated position: Analysis of 554 cases. Neurosurgery. 1985;17:695–702. doi: 10.1227/00006123-198511000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Palmon SC, Moore LE, Lundberg J, Toung T. Venous air embolism: A review. J Clin Anesth. 1997;9:251–7. doi: 10.1016/s0952-8180(97)00024-x. [DOI] [PubMed] [Google Scholar]
- 11.Minovi A, Mangold R, Kollert M, Hofmann E, Draf W, Bockmühl U. Functional results, cognitive and effective quality of life disturbances after trans-temporal resection of acoustic neuroma. Laryngorhinootologie. 2005;84:915–20. doi: 10.1055/s-2005-870573. [DOI] [PubMed] [Google Scholar]
- 12.Schick B, Greess H, Gill S, Pauli E, Iro H. Magnetic resonance imaging and neuropsychological testing after middle fossa vestibular schwannoma surgery. Otol Neurotol. 2008;29:39–45. doi: 10.1097/mao.0b013e31815c2ad7. [DOI] [PubMed] [Google Scholar]
- 13.Hoffman RA. Cerebrospinal fluid leak following acoustic neuroma removal. Laryngoscope. 1994;104(1 Pt 1):40–58. doi: 10.1288/00005537-199401000-00009. [DOI] [PubMed] [Google Scholar]
- 14.Bentivoglio P, Cheeseman AD, Symon L. Surgical management of acoustic neuromas during the last five years. Part I. Surg Neurol. 1988;29:197–204. doi: 10.1016/0090-3019(88)90006-7. [DOI] [PubMed] [Google Scholar]
- 15.Selesnick SH, Liu JC, Jen A, Newman J. The incidence of cerebrospinal fluid leak after vestibular schwannoma surgery. Otol Neurotol. 2004;25:387–93. doi: 10.1097/00129492-200405000-00030. [DOI] [PubMed] [Google Scholar]
- 16.Standefer M, Bay JW, Trusso R. The sitting position in neurosurgery: A retrospective analysis of 488 cases. Neurosurgery. 1984;14:649–58. doi: 10.1227/00006123-198406000-00001. [DOI] [PubMed] [Google Scholar]
- 17.Samii M, Gerganov V, Samii A. Hearing preservation after complete microsurgical removal in vestibular schwannomas. Prog Neurol Surg. 2008;21:136–41. doi: 10.1159/000156900. [DOI] [PubMed] [Google Scholar]
- 18.Somers T, Casselman J, de Ceulaer G, Govaerts P, Offeciers E. Prognostic value of magnetic resonance imaging findings in hearing preservation surgery for vestibular schwannoma. Otol Neurotol. 2001;22:87–94. doi: 10.1097/00129492-200101000-00017. [DOI] [PubMed] [Google Scholar]
- 19.Hitselberger WE, House WF. A warning regarding the sitting position for acoustic tumor surgery. Arch Otolaryngol. 1980;106:69. doi: 10.1001/archotol.1980.00790260001001. [DOI] [PubMed] [Google Scholar]
- 20.El-Rubaidi OA, Horcajadas-Almansa A, Rodríguez-Rubio D, Galicia-Bulnes JM. Sciatic nerve compression as a complication of the sitting position. Neurocirugia (Astur) 2003;14:426–30. doi: 10.1016/s1130-1473(03)70524-7. [DOI] [PubMed] [Google Scholar]
- 21.Toung T, Donham RT, Lehner A, Alano J, Campbell J. Tension pneumocephalus after posterior fossa craniotomy: Report of four additional cases and review of postoperative pneumocephalus. Neurosurgery. 1983;12:164–8. doi: 10.1227/00006123-198302000-00005. [DOI] [PubMed] [Google Scholar]
- 22.Spektor S, Fraifeld S, Margolin E, Saseedharan S, Eimerl D, Umansky F. Comparison of outcomes following complex posterior fossa surgery performed in the sitting versus lateral position. J Clin Neurosci. 2015;22:705–12. doi: 10.1016/j.jocn.2014.12.005. [DOI] [PubMed] [Google Scholar]
- 23.Ansari SF, Terry C, Cohen-Gadol AA. Surgery for vestibular schwannomas: A systematic review of complications by approach. Neurosurg Focus. 2012;33:E14. doi: 10.3171/2012.6.FOCUS12163. [DOI] [PubMed] [Google Scholar]




