Abstract
Objective:
Anti-tuberculosis (TB) treatment remains the mainstay of treatment of spinal TB. There is a lack of consensus regarding the timing of interventional procedures and surgery in the patients with spinal TB. This study aims to prospectively study the clinical outcome and management in patients presenting with spinal TB at our tertiary referral center and teaching hospital.
Methods:
Data were collected prospectively from 48 patients treated for spinal TB presenting to us from August 2011 to December 2012. All the patients were followed-up for the duration of anti-TB treatment.
Results:
The categorization of patients into different management groups was based on the clinical and radiological findings at the time of diagnosis. The patients with mild disease (n = 23) were successfully managed with anti-TB treatment alone. The other 25 patients needed an intervention either in the form of pigtail catheter drainage of the paravertebral collection (n = 18) or an extensive surgical debridement followed by the fusion techniques (n = 7). All the patients responded well to the treatment, and there were no significant complications in any of the patients. It had been observed that various stages of spinal TB demand different approaches for the treatment in the form of either chemotherapy alone, chemotherapy with pigtail drainage of the paravertebral collection, or surgery in conjunction with chemotherapy.
Conclusions:
Judicious use of pigtail drainage and surgical intervention in addition to anti TB treatment can be rewarding in the patients with spinal TB.
Keywords: Paravertebral collection, pigtail drainage, spinal tuberculosis, surgery for spinal tuberculosis
Introduction
Spinal tuberculosis (TB) is the most common form of skeletal involvement by TB amounting to about half the cases of skeletal TB. It is a serious form of extra pulmonary TB which if left untreated can be fatal.[1] The treatment for spinal TB is either chemotherapy alone or surgery in addition to chemotherapy. A “middle path” regime of treatment for spinal TB has also been described which includes percutaneous drainage of the paravertebral abscess along with conventional chemotherapy,[2] although many studies describe surgery as the only therapeutic option for such patients.[3] Thus, a significant dilemma exists as to which line of management a person needs to be subjected once diagnosed to have spinal TB. The present study aims to study the clinical outcome and management according to severity in the patients with spinal TB at our tertiary referral center and teaching hospital.
Methods
Data was collected prospectively from 48 patients treated for spinal TB presenting to Sri Venkateswara Institute of Medical Sciences, Tirupati, Andhra Pradesh, India from August 2011 to December 2012. A total number of 48 patients were thoroughly evaluated clinico-radiologically and placed into various groups depending on the line of management opted for that particular patient. Daily basis, self-supervised anti-TB treatment was administered scheduled according to the recent World Health Organization guidelines.[4,5,6] A Milder form of the disease in the form of vertebral body destruction and the minimal paravertebral collection was observed in 23 of them, who were placed in the conservative group and managed with anti-TB treatment alone. The patients having mild to moderate vertebral body destruction with a significant paravertebral collection (n = 18) were managed by pigtail catheter drainage of the paraspinal collection along with anti-TB treatment. Severe neurological deficits were observed in 7 patients who needed surgical intervention in the form of debridement and fusion in addition to anti-TB treatment. Pathological confirmation of the disease was established if either computed tomography guided fine-needle aspiration cytology or biopsy of the diseased tissue confirmed positive for TB. Follow-up assessment was carried out at 3rd and 6th month after the commencement of treatment for all the patients. All patients were assessed for their functional status with the help of Modified McCormicks’ scale.[7] Patients who underwent surgery were assessed radiologically during the follow-up visits with the help of Bridwell fusion scale.[8,9] This study was approved by the institutional ethical committee and did not have any ethical issues.
Results
In this study, 23 patients with a milder form of the disease were successfully managed with anti-TB treatment alone. The other 25 patients needed some kind of intervention either in the form of pigtail drainage of the paravertebral collection or an extensive surgical debridement and fusion technique in addition to conventional anti-TB treatment [Figure 1]. Among a total of 48 patients, 25 were males and 23 were females with an overall ratio of 1.08:1. Males dominated the conservative group (n = 13) and females dominated the surgical group (n = 4), but the pigtail group consisted equal number of males and females ([n = 9 each]; ratio 1:1). The duration of symptoms ranged from 10 days to 3 years. Patients who were treated conservatively were the ones who presented early during their illness accounting to a mean duration of 2.9 months, whereas the ones in the pigtail group had a relatively late presentation with a mean of 7.8 months. The patients who required surgery had an intermediate presentation with a mean duration of illness amounting to 5.28 months [Figure 2].
Figure 1.
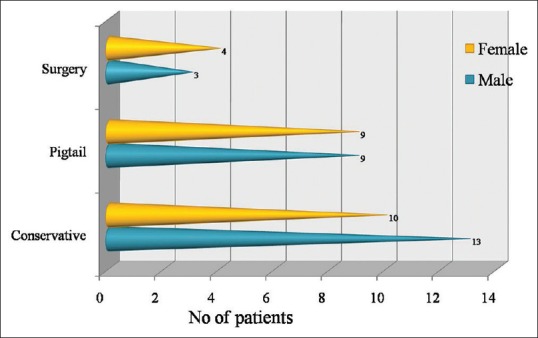
Distribution of patients among 48 patients with spinal tuberculosis
Figure 2.
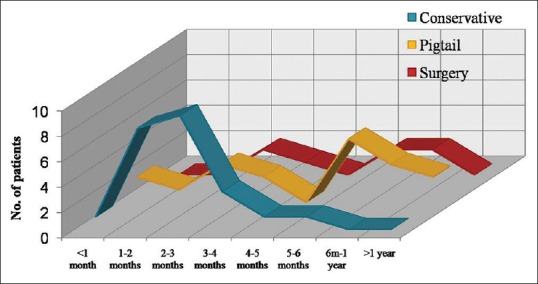
Duration of symptoms among 48 patients with spinal tuberculosis
The pain was the predominant presenting symptom in all the patients. The next commonest presenting symptom observed were paresthesias which were seen in 20 patients in the conservative group, 11 patients in the pigtail group and 6 patients in the surgical group. This was followed by the weakness in the limbs which was seen in 3 patients in the conservative group, 8 patients from the pigtail group and 6 patients in the surgical group. All the patients included in the conservative had minimal neurological signs in the form of motor and sensory deficits, as seen in 4 patients and 2 patients, respectively. Motor deficits predominated in the pigtail group and the surgical group amounting to 10 patients and 7 patients, respectively. Autonomic involvement in the form of bladder/bowel disturbances was observed mostly in the surgical group amounting to 4 patients, and only one patient in the pigtail group had autonomic disturbances which gradually improved with the treatment. Kyphosis, which is an absolute indication for surgery, was observed in 4 patients in the surgical group. The commonest levels of involvement in spinal TB were the lumbar and dorsal regions which were seen in 26 patients and 14 patients, respectively. TB of the cervical spine was observed in only one patient who was treated surgically. Dorsolumbar TB was found in 4 patients out of which 1 patient was needed surgery, and 3 were treated by pigtail aspiration. The multilevel disease was observed in 3 patients out of which 2 were managed conservatively and one required pigtail aspiration.
Out of 48 patients, most of the patients had the involvement of two contiguous vertebrae (25 patients). Three level diseases were observed in 12 patients whereas the single level, and multilevel disease was observed in 5 patients. Vertebral body destruction was observed in all the patients, irrespective of the group. The paravertebral collection was observed in all the patients included in the pigtail group, out of which 11 patients had some amount of cord compression. All the patients in the surgical group had a variable degree of cord compression. Out of these, 3 patients each had kyphosis and paravertebral collection in addition to cord compression. Of the patients in the conservative group, two patients each had a paravertebral collection and cord compromise. The pathological confirmation of TB could be established only in the patients of the surgical group where an adequate sample size for analysis was available. A definitive pathological diagnosis could not be established in the conservative and the pigtail groups.
The functional outcome assessment was carried out with the help of Modified McCormick's functional outcome scale[7] recorded at the time of initiation of treatment, at 3rd month and 6th month follow-up period. All the patients showed a good functional improvement in their neurological status during their follow-up at a 3rd month and 6th month, irrespective of the treatment they were subjected to. The radiological outcome assessed with the help of Bridwell fusion scale,[8,9] done for the patients in the surgical group showed that all patients during their first follow-up had minimal fusion amounting to a Bridwell fusion scale of III. At the end of 6 months during their second follow-up, 6 patients exhibited a grade II fusion whereas one patient remained to have a grade III fusion at the operated site. It had been observed that the various stages of spinal TB demanded different approaches for treatment in the form of either anti-TB treatment alone, anti-TB treatment with pigtail drainage of the paravertebral collection or surgery in conjunction with anti-TB treatment [Tables 1 and 2]. Comparison of different variables in previous studies[10,11,12] on management of spinal TB with the observations in the present study is shown in Table 3. A few of the treated cases are illustrated in Figures 3–6.
Table 1.
Functional outcome in 48 patients with spinal TB
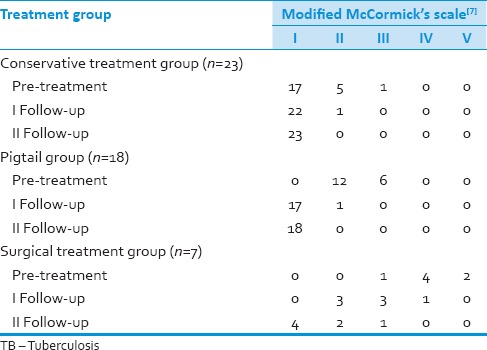
Table 2.
Radiological outcome in 7 patients with spinal TB managed surgically along with antituberculosis treatment
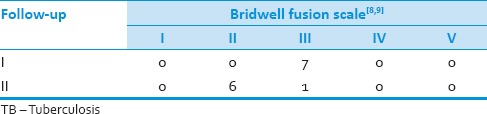
Table 3.
Comparison of different variables in previous studies[10,11,12] on management of spinal TB with the observations in the present study
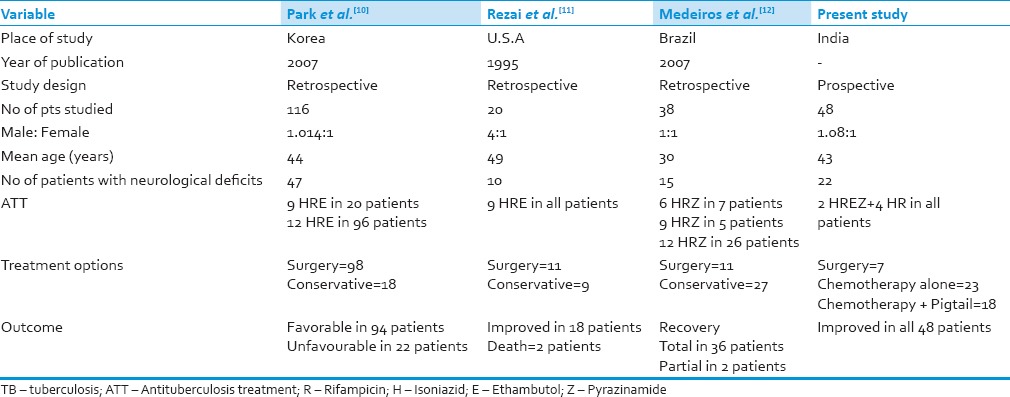
Figure 3.
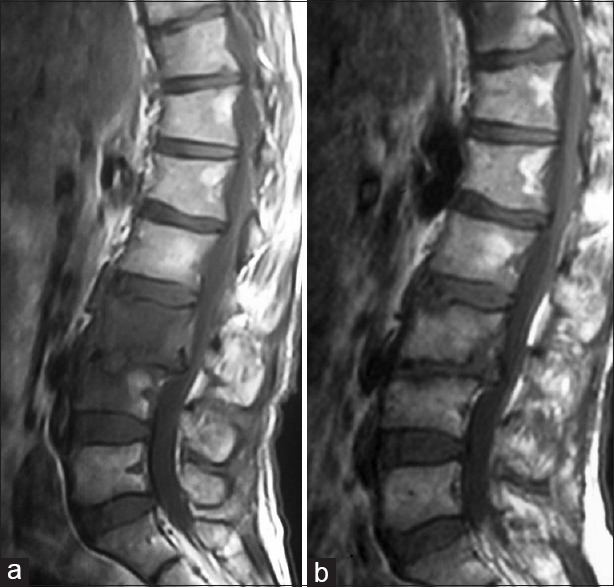
(a) Pretreatment sagittal T1-weighted magnetic resonance imaging of a patient who received anti-tuberculosis treatment alone showing involvement of contiguous vertebral bodies. (b) Posttreatment sagittal T1-weighted axial magnetic resonance imaging of the same patient showing near total resolution of disease with anti-tuberculosis treatment alone
Figure 6.

(a) Preoperative sagittal computed tomography of the same patient managed surgically showing destruction of vertebral bodies with kyphotic deformity. (b) Postoperative sagittal computed tomography of the same patient showing implants in place following anterior fusion
Figure 4.
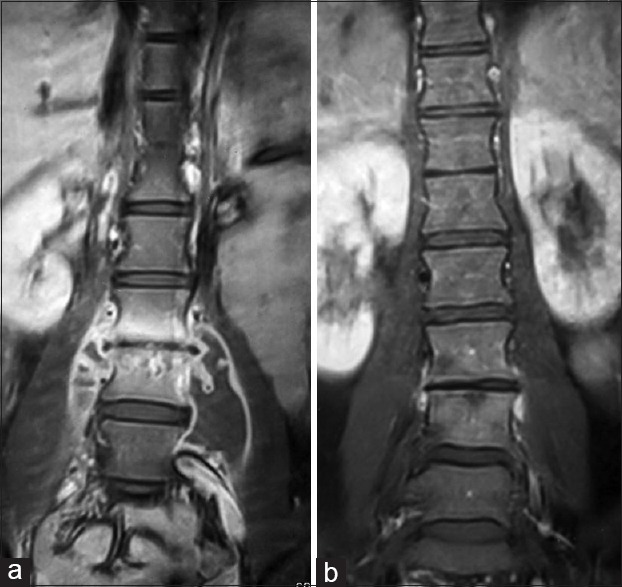
(a) Pretreatment coronal contrast T1-weighted magnetic resonance imaging of a patient managed by pigtail drainage showing vertebral body destruction with bilateral psoas abscesses. (b) Posttreatment coronal contrast T1-weighted magnetic resonance imaging of the same patient showing near total healing of the vertebral lesion with resolution of psoas abscess following pigtail drainage
Figure 5.
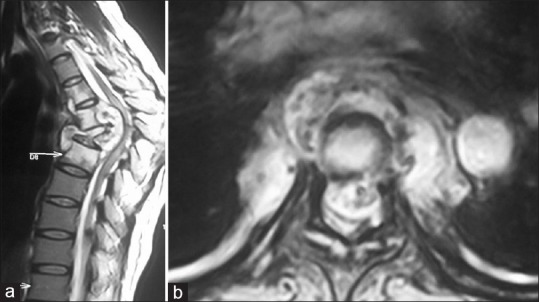
(a) Preoperative sagittal T2-weighted magnetic resonance imaging of a patient managed surgically showing gross vertebral body destruction with associated with severe cord compression, paravertebral collection and kyphotic deformity. (b) Preoperative axial T2-weighted magnetic resonance imaging of the same patient managed surgically showing vertebral body destruction and paravertebral collection
Discussion
Spinal TB is a serious form of extra pulmonary TB associated with high morbidity and if left untreated can be fatal. A significant controversy exists regarding what constitutes the optimal treatment for the patients with spinal TB. Anti-TB treatment for spinal TB follows a model of short term anti-TB treatment and includes an intensive phase of treatment followed by a continuation phase. Although anti-TB treatment is now the mainstay of management for spinal TB, it may not be adequate in all situations, especially in the patients with risk of deformity, instability, and progression of neurologic deficit. Numerous studies conducted previously have described the surgery as the treatment modality for such cases,[13,14] though very few studies describe pigtail aspiration of the paraspinal abscess as an option for selected patients.
In this prospective study, we analyzed the factors influencing the clinical outcome in the patients treated for spinal TB, focusing on the modality of treatment adopted. The good functional improvement was observed in all the patients at the end of treatment, irrespective of whether they were treated conservatively, by pigtail drainage or by surgery. Younger age group and early treatment were related to a favorable outcome in the present study, but sex distribution and chemotherapy given were not.
In this study, there was mild male preponderance which is comparable with a Korean study[10] where a ratio of 1.014:1 was observed. These results were in contrast to the study carried out in the USA, which showed an M: F ratio of 4:1.[11] In the present study, the mean age was 43 years which was comparable to the Korean and American studies who had patients with a mean age of 44 years and 49 years, respectively. However, the mean age in a Brazilian study[12] was 30 years.
Approximately, half of all forms of skeletal TB affect the spinal column and the lumbar, and dorsal vertebrae are the usual sites of infection affecting the cervical spine in rare cases. In our study, most of the patients (54.1%) had the disease of the lumbar spine followed by that of the dorsal spine. TB of the cervical spine was relatively rare and was seen only in one patient. This was comparable with the Korean study[10] in which 44.8% of patients had the disease of the lumbar spine, 31.3% had that of the dorsal spine, and none with cervical spine disease.
In the present study, pain is the commonest presenting symptom. Less than half of the patients with TB spine have neurological deficits in one form of the other at the time of presentation, a fact that is consistent with studies done in Korea[10] and Brazil.[12] The American study conducted in 1995, though, had equal patients with and without neurological deficits.
The time of presentation reflects the severity of the condition and is directly proportional to the aggressiveness of the treatment. Individuals with a milder form of the disease with minimal symptoms and no neurological deficits recover well with conventional medical treatment. Spinal TB associated with a paraspinal collection with minimal neurological deficits can be managed by catheter drainage of the abscess cavity in conjunction with the conventional therapy. The patients with more severe disease of spinal TB in the form of severe disability, gross neurological deficits, spinal deformities, and autonomic involvement demands more aggressive treatment in the form of the surgical debridement and fusion procedures in addition to conventional anti-TB treatment. In our study, out of 48 patients, 47.9% of patients were managed conservatively with anti-TB treatment alone, which was comparable with the study conducted in the USA who managed 55% of patients with anti-TB treatment alone.
A study conducted in Chandigarh, India[15] reported bilateral psoas abscesses as an atypical presentation of spinal TB, who successfully managed 3 such cases with pigtail aspiration along with the conventional anti-TB treatment. Another study conducted in Spain[16] treated 7 patients having spinal TB with psoas abscesses in a similar manner and had favorable results. The outcome in the present study for the management of spinal TB by anti-TB treatment with pigtail drainage of the paraspinal abscesses were comparable to the above two studies who achieved a complete recovery from disease [Table 3]. Patients with neurological deficits who are medically unfit to undergo surgical therapy can be given a trial by percutaneous drainage of the paravertebral collection if present by a pigtail catheter. Surgery can be planned at a later date in the patients whose general condition improves, develop a recurrent abscess, and if there is progressive neurological deterioration despite rest and anti-TB treatment.
Clinical and neurological improvement was good in all the groups depending on their condition at the time of initiation of therapy, indicating no difference irrespective of the treatment option employed, a finding which is consistent with the studies conducted previously.[8,10,11,12,13,14,15,16,17] The variables in the present study are compared with those of the previous studies in Table 3.
In the present study, the variation in the presenting symptoms of spinal TB in different study groups is a limitation that may have caused an outcome bias. The present study is not a randomized trial, and hence a statistical significance cannot be drawn from it. In addition, the degree of preoperative and postoperative kyphotic deformity and the advantages and disadvantages related to the anterior and posterior fusion in surgical patients could not be studied in the current study due to inadequate sample size in the surgical group.
Conclusions
Various stages of spinal TB, if managed by the correct modality of treatment, is associated with a high cure rate. However, a careful and meticulous selection of patients based on the clinical and radiological findings is necessary for deciding the optimum treatment plan for a particular patient suffering from spinal TB.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors wish to thank the Departments of Radiodiagnosis, Pathology and Cardiothoracic and Vascular Surgery at Sri Venkateswara Institute of Medical Sciences, Tirupati, Andhra Pradesh, India for their help in managing the patients.
References
- 1.Tuli SM. Tuberculosis of the Skeletal System: Bones, Joints, Spine and Bursal Sheaths. Rev reprint. New Delhi: Jaypee Brothers Medical Publishers; 1993. p. 268. [Google Scholar]
- 2.Tuli SM. Results of treatment of spinal tuberculosis by “middle-path” regime. J Bone Joint Surg Br. 1975;57:13–23. [PubMed] [Google Scholar]
- 3.Goregaonkar AB. Posterior stabilisation for Kochs spine. In: Ramani PS, editor. Textbook of Spinal Surgery. 1st ed. Mumbai: India Printing House; 1996. p. 251. [Google Scholar]
- 4.Sharma SK, Mohan A. Tuberculosis: From an incurable scourge to a curable disease – Journey over a millennium. Indian J Med Res. 2013;137:455–93. [PMC free article] [PubMed] [Google Scholar]
- 5.Sharma SK, Mohan A. Extrapulmonary tuberculosis. Indian J Med Res. 2004;120:316–53. [PubMed] [Google Scholar]
- 6.World Health Organization. Treatment of Tuberculosis: Guidelines for National Programmes. WHO/CDS/TB/2003. 3rd ed. Geneva: World Health Organization; 2003. [Google Scholar]
- 7.Manzano G, Green BA, Vanni S, Levi AD. Contemporary management of adult intramedullary spinal tumors-pathology and neurological outcomes related to surgical resection. Spinal Cord. 2008;46:540–6. doi: 10.1038/sc.2008.51. [DOI] [PubMed] [Google Scholar]
- 8.Bridwell KH, Lenke LG, McEnery KW, Baldus C, Blanke K. Anterior fresh frozen structural allografts in the thoracic and lumbar spine. Do they work if combined with posterior fusion and instrumentation in adult patients with kyphosis or anterior column defects? Spine (Phila Pa 1976) 1995;20:1410–8. [PubMed] [Google Scholar]
- 9.Matsumoto Y, Harimaya K, Doi T, Maeda T, Iwamoto Y. Outcome of osteoplastic laminotomy for excision of spinal cord tumours. J Orthop Surg (Hong Kong) 2009;17:275–9. doi: 10.1177/230949900901700305. [DOI] [PubMed] [Google Scholar]
- 10.Park DW, Sohn JW, Kim EH, Cho DI, Lee JH, Kim KT, et al. Outcome and management of spinal tuberculosis according to the severity of disease: A retrospective study of 137 adult patients at Korean teaching hospitals. Spine (Phila Pa 1976) 2007;32:E130–5. doi: 10.1097/01.brs.0000255216.54085.21. [DOI] [PubMed] [Google Scholar]
- 11.Rezai AR, Lee M, Cooper PR, Errico TJ, Koslow M. Modern management of spinal tuberculosis. Neurosurgery. 1995;36:87–97. doi: 10.1227/00006123-199501000-00011. [DOI] [PubMed] [Google Scholar]
- 12.Medeiros RS, Abdo RC, de Paula FC, Narazaki DK, Correia LS, Araújo MP, et al. Treatment of spinal tuberculosis: Conservative or surgical? Acta Ortop Bras. 2007;15:128–31. [Google Scholar]
- 13.Parthasarathy R, Sriram K, Santha T, Prabhakar R, Somasundaram PR, Sivasubramanian S. Short-course chemotherapy for tuberculosis of the spine. A comparison between ambulant treatment and radical surgery – Ten-year report. J Bone Joint Surg Br. 1999;81:464–71. doi: 10.1302/0301-620x.81b3.9043. [DOI] [PubMed] [Google Scholar]
- 14.Vidyasagar C, Murthy HK. Management of tuberculosis of the spine with neurological complications. Ann R Coll Surg Engl. 1994;76:80–4. [PMC free article] [PubMed] [Google Scholar]
- 15.Goni V, Thapa BR, Vyas S, Gopinathan NR, Rajan Manoharan S, Krishnan V. Bilateral psoas abscess: Atypical presentation of spinal tuberculosis. Arch Iran Med. 2012;15:253–6. [PubMed] [Google Scholar]
- 16.Pombo F, Martín-Egaña R, Cela A, Díaz JL, Linares-Mondéjar P, Freire M. Percutaneous catheter drainage of tuberculous psoas abscesses. Acta Radiol. 1993;34:366–8. [PubMed] [Google Scholar]
- 17.Enam SA, Shah AA. Treatment of spinal tuberculosis: Role of surgical intervention. Pak J Neurol Sci. 2006;1:145–51. [Google Scholar]


