Abstract
Background
Although the association between coronary artery calcium (CAC) and future heart failure (HF) has been shown previously, the value of CAC progression in the prediction of HF has not been investigated. In this study, we investigated the association of CAC progression with subclinical left ventricular (LV) dysfunction and incident HF in the Multi‐Ethnic Study of Atherosclerosis.
Methods and Results
The Multi‐Ethnic Study of Atherosclerosis is a population‐based study consisting of 6814 men and women aged 45 to 84, free of overt cardiovascular disease at enrollment, who were recruited from 4 ethnicities. We included 5644 Multi‐Ethnic Study of Atherosclerosis participants who had baseline and follow‐up cardiac computed tomography and were free of HF and coronary heart disease before the second cardiac computed tomography. Mean (±SD) age was 61.7±10.2 years and 47.2% were male. The Cox proportional hazard models and multivariable linear regression models were deployed to determine the association of CAC progression with incident HF and subclinical LV dysfunction, respectively. Over a median follow‐up of 9.6 (interquartile range: 8.8–10.6) years, 182 participants developed incident HF. CAC progression of 10 units per year was associated with 3% of increased risk of HF independent of overt coronary heart disease (P=0.008). In 2818 participants with available cardiac magnetic resonance images, CAC progression was associated with increased LV end diastolic volume (β=0.16; P=0.03) and LV end systolic volume (β=0.12; P=0.006) after excluding participants with any coronary heart disease.
Conclusions
CAC progression was associated with incident HF and modestly increased LV end diastolic volume and LV end systolic volume at follow‐up exam independent of overt coronary heart disease.
Keywords: cardiac computed tomography, cardiac magnetic resonance imaging, coronary artery calcium, coronary artery calcium progression, heart failure
Subject Categories: Computerized Tomography (CT), Magnetic Resonance Imaging (MRI), Heart Failure
Introduction
Heart failure (HF) is a disabling disease with high burden on health care economy.1 It affects both men and women with a lifetime risk of 20%.2 Secondary to a combination of population aging and improvement in the managements of acute cardiovascular diseases, incidence and prevalence of HF have been increasing continuously in the past decades.3 Approximately 5.7 million Americans suffer from HF,1 and each year more than 550 000 new cases of HF are diagnosed.4 The most common cause of HF in the United States is coronary artery disease (CAD).5 CAD plays its role in the pathophysiology of HF through different mechanisms.6 In addition to clinically overt coronary heart disease (CHD), hypoperfusion and endothelial dysfunction may cause subclinical myocardial damage and dysfunction, which eventually will progress to symptomatic HF.7 Myocardial dysfunction in the subclinical phase is detectable by cardiac imaging, including echocardiography and cardiac magnetic resonance (CMR). Considering the progressive nature of HF and to implement effective risk modification strategies, it is imperative to detect asymptomatic individuals at risk to develop HF.8 Coronary artery calcium (CAC) measurement by noncontrast cardiac computed tomography is a reliable and accurate tool to detect subclinical atherosclerosis and has a strong correlation with atherosclerotic plaque burden.9 CAC score has incremental value over traditional risk scoring systems for cardiovascular risk stratification, especially in individuals who are classified as intermediate risk.10 Serial measurement of CAC score has been introduced as a tool to monitor the progression of subclinical atherosclerosis.11 CAC progression has a good predictive value for incident CHD and all‐cause mortality.12, 13 Although the association between CAC and incident HF has been demonstrated in a few studies independent of CHD,14, 15, 16, 17 the value of CAC progression in prediction of future HF has not been previously evaluated. In this study, we investigate CAC progression as a predictor of incident HF and subclinical left ventricular (LV) dysfunction measured by CMR in a population‐based cohort.
Materials and Methods
The Multi‐Ethnic Study of Atherosclerosis (MESA) is a prospective, population‐based cohort study including 4 racial/ethnic groups (whites, blacks, Hispanics, and Chinese).The design of MESA has been published in detail previously.18 Briefly, between July 2000 and August 2002 (Exam 1), 6814 men and women, aged 45 to 84 years and free of clinical cardiovascular disease at enrollment, were recruited from 6 US field centers (Baltimore, MD; Chicago, IL; Forsyth County, NC; Los Angeles County, CA; Northern Manhattan, NY; and St Paul, MN). All participants gave written informed consents and all study protocols were approved by the institutional review boards of each participating field center. Baseline examination (Exam 1) were followed by 4 more examinations with the following timeline: Exam 2 (September 2002–February 2004); Exam 3 (March 2004–September 2005); Exam 4 (September 2005–May 2007); and Exam 5 (April 2010–December 2011). In this study, we included all MESA participants who had CAC measured by cardiac computed tomography at baseline (Exam 1) and follow‐up (Exam 2 or 3). There were 142 participants who developed incident CHD, 58 who developed incident HF, and 35 who developed both incident CHD and HF before their second cardiac computed tomography and were excluded from this analysis.
At Exam 1, standard questionnaires were used to obtain demographic, medical, and family history, medication use, smoking status, household income, and highest education level. Smoking status was defined as never, former, or current smoker. BMI was calculated as weight (kg) divided by the square of height (m2). Resting blood pressure was measured 3 times using the Dinamap model Pro 100 automated oscillometric sphygmomanometer (Critiko, Tampa, FL) in the upright position and the mean of the last 2 measurements was recorded. Fasting blood glucose as well as total and high‐density lipoprotein (HDL) cholesterol were measured in serum. Participants were classified as normal and impaired fasting glucose if fasting blood glucose was <100 mg/dL and 100 to 125 mg/dL respectively. Diabetes mellitus was defined as fasting blood glucose ≥126 mg/dL or the use of insulin or any other hypoglycemic medication. An ElecSys 2010 analyzer (Roche Diagnostics, Indianapolis, IN) was used to measure N‐Terminal prohormone of brain natriuretic peptide (NT‐proBNP). Electrocardiogram was utilized to measure resting hear rate.
The details of the acquisition method of cardiac computed tomography in MESA has been published previously.12, 19 For each participant 2 consecutive scans were obtained over a standard calcium phantom at both baseline and follow‐up exams. All images were transferred to a central computed tomography reading center (Los Angeles Biomedical Research Institute, Torrance, CA) and interpreted by an experienced physician. CAC score was calculated using the method introduced by Agatston et al. The mean of 2 scans at each exam were used for data analysis after being adjusted according to the calcium phantom. The acquisition method of CMR images in MESA has been explained in detail in previous publications.20, 21 CMR was performed using 1.5 Tesla scanners. In Exam 5, the steady‐state free precession pulse sequence was used to measure the parameters of cardiac function and structure. All CMR images were analyzed by blinded readers in a central magnetic resonance imaging (MRI) reading center (Johns Hopkins Hospital, Baltimore, MD). CMR images in Exam 5 were quantified using CIM software (version 6.0; UniServices, Auckland, New Zealand). The following CMR variables were used in our study: LV mass (LVM); LV end diastolic volume (LVEDV); LV end systolic volume (LVESV); stroke volume (SV); ejection fraction (EF); and mass‐to‐volume ratio (MVR; MVR=LV mass/LVEDV). The first 4 variables were indexed to body surface area. In 3 participants, the indexed parameters were not calculated because of missing weight variable. In 1 participant, EF, SV, and LVESV were missing.
Every 9 to 12 months, a telephone interviewer called each participant to find about any interim hospital admissions, cardiovascular outpatient diagnoses, and deaths. Inpatient and outpatient medical records and information were received successfully in ≈98% and 95%, respectively. CHD was assessed as any of myocardial infarction, resuscitated cardiac arrest, definite angina, probable angina (if followed by revascularization), and CHD death. The end point for our study was a combination of probable and definite HF. Both types required clinical symptoms and signs of HF, such as shortness of breath or edema. HF was considered probable if a physician made the diagnosis and the patient was receiving medical treatment for HF. Definite HF required to meet at least 1 of the following criteria: (1) pulmonary edema/congestion in chest x‐ray; (2) dilated or dysfunctional LV by echocardiography or any ventriculography; or (3) any evidence of LV diastolic dysfunction.
Statistical Analysis
Baseline characteristics are presented using mean±SD or numbers (%). CAC progression (continuous variable) was calculated as follow‐up CAC minus baseline CAC divided by interscan period in years (annualized change in CAC). In addition, progressors versus nonprogressores (categorical variable) was defined using the method that was introduced by Berry et al.22 A participant is considered as a progressor if he or she has:
Baseline CAC=0 and follow‐up CAC more than zero, or
0 < baseline CAC ≤100 and annualized change in CAC ≥10, or
Baseline CAC >100 and annualized relative change in CAC ≥10% (annualized change in CAC divided by baseline CAC multiplied by 100).
The Cox proportional hazards (CPH) model was used to evaluate the association of CAC progression, either continuous CAC progression or categorical CAC progression, and time to incident HF in participants free of any CHD or HF before the follow‐up CAC measurement. Three separate models were used for the analysis:
Model 1: CPH regression without adjusting covariates other than CAC progression.
Model 2: CPH regression with covariate adjustment for demographics and known risk factors of HF (Exam 1), including age, sex, race, BMI, systolic blood pressure (SBP), diastolic blood pressure (DBP), use of antihypertensive medication, total cholesterol, HDL cholesterol, use of lipid‐lowering medication, diabetes mellitus, cigarette smoking status, heart rate, creatinine, highest education level, household income, and baseline CAC score. A sensitivity analysis was done by comparing the results with and without adjusting for baseline NT‐proBNP. Participants with any CHD and HF before second CAC measurement were excluded.
Model 3: model 2 after excluding the participants with any CHD before and after second CAC measurement. Subgroups analyses were done for participants with baseline CAC=0 and participants with baseline CAC >0.
For the analysis of LV dysfunction, multivariable linear regression models were used to assess the association of CAC progression, either continuous or categorical CAC progression, with each of the MRI parameters of LV function and structure at Exam 5. The same exclusion criteria were applied as in the CPH analysis. Two adjusted models were constructed with the covariates that were used for CPH analysis. Given that the distribution of CAC scores is skewed, the baseline CAC score in the models was transformed by the logarithmic transformation [ln (CAC+1)]. All statistical results were computed using Stata statistical software (version 14.1; StataCorp LP, College Station, TX). P value of less than 0.05 was considered significant.
Results
A total of 5644 MESA participants free of HF and CHD before the second CAC measurement were included in this study. The baseline characteristics of the study participants are shown in Table 1. The mean (±SD) interscan period (baseline and follow‐up) was 2.4±0.9 years. Baseline CAC was zero in more than half of the cohort population (51.8%), and the majority (84.1%) remained CAC free in the second measurement. Of those with baseline CAC >0 to 100 and >100, 43.3% and 66.9% showed progression based on the above‐defined basis for identifying progressors, respectively.
Table 1.
Baseline Characteristics of Participants
| Characteristics | Mean±SD or N (%) | Characteristics | Mean±SD or N (%) |
|---|---|---|---|
| All participants | 5644 | LDL cholesterol, mg/dL | 117.3±31 |
| Males | 2662 (47.2) | HDL cholesterol, mg/dL | 51±14.7 |
| Age, y | 61.7±10.2 | Lipid‐lowering medication | 909 (16.1) |
| Race | Diabetes mellitus | ||
| White | 2232 (39.5) | Normal | 4209 (74.8) |
| Black | 1529 (27.1) | Impaired fasting glucose | 764 (13.6) |
| Hispanic | 1207 (21.4) | Untreated diabetes mellitus | 146 (2.6) |
| Chinese | 676 (12) | Treated diabetes mellitus | 508 (9) |
| Highest education level | Smoking status | ||
| 25th percentile | Completed high school/GED | Never smoker | 2868 (51) |
| Median | Some college but no degree | Former smoker | 2068 (36.7) |
| 75th percentile | Bachelor's degree | Current smoker | 694 (12.3) |
| Household income | Creatinine, mg/dL | 0.95±0.25 | |
| 25th percentile | $20 000 to $24 999 | Heart rate (beats per minute) | 63±9.6 |
| Median | $40 000 to $49 999 | CAC score=0 | 2923 (51.8) |
| 75th percentile | $50 000 to $74 999 | CAC score >0 to 100 | 1481 (26.2) |
| BMI, kg/m2 | 28.3±5.4 | CAC score >100 | 1240 (22) |
| SBP, mm Hg | 125.7±21 | CAC score (Agatston Unit) in participants with CAC >0 | 270.6±506 |
| DBP, mm Hg | 71.8±10.2 | ||
| Blood pressure medication | 2023 (35.9%) | Interscan period, yr | 2.4±0.9 |
These figures are numbers (%) and mean±SD. CAC indicates coronary artery calcium; DBP, diastolic blood pressure; GED, general education development; HDL, high‐density lipoprotein; LDL, low‐density lipoprotein; SBP, systolic blood pressure.
Over a median 9.6 (interquartile range [IQR], 8.8–10.6) years of follow‐up from the second CAC measurement (12.2 [IQR, 11.7–12.7] years from Exam 1), 182 participants developed incident HF. Of those with HF, 83 participants developed concomitant CHD. Using CAC progression as a continuous variable, a longitudinal increase in CAC of 10 Agatston Units (AU) per year was associated with 2% (P=0.012) of increased risk of HF independent of known risk factors for HF and baseline CAC. This association remained statistically significant after excluding the participants with CHD (Table 2). The association between CAC progression as a categorical variable and HF was not statistically significant in adjusted models. Subgroups analysis were performed for participants with baseline CAC=0 and CAC >0 separately (Table 3). Any change in CAC from zero was associated with a hazard ratio (HR) of 2.52 (P=0.003) independent of traditional cardiovascular risk factors. In Figure, Kaplan–Meier curves of cumulative events show higher cumulative incident of HF in progressors compared to nonprogressors (Figure Panel A: full cohort; Figure Panel B: baseline CAC=0; and Figure Panel C: baseline CAC >0). A sensitivity analysis was done on a group of 4664 participants with available baseline NT‐proBNP to investigate the effect of adjusting the CPH models for NT‐proBNP (Table S1). The magnitude and significance of the associations remained largely unchanged.
Table 2.
Hazard Ratios (95% CIs) Showing the Association Between Changes in CAC and Incident Heart Failure in the Full Cohort
| Models (No. of Events/Analyzed) | Model 1a (182/5644) | Model 2b (168/5384) | Model 3c (90/5049) |
|---|---|---|---|
| Absolute changes in CAC per yeard | 1.05 (1.04–1.06)e | 1.02 (1.004–1.04)e | 1.03 (1.01–1.05)e |
| Progressors vs nonprogressors | 2.74 (2.05–3.68)e | 1.29 (0.93–1.81) | 1.25 (0.79–1.97) |
Model 1: unadjusted.
Model 2: adjusted for age, sex, race, BMI, systolic blood pressure (SBP), diastolic blood pressure (DBP), use of antihypertensive medication, total cholesterol, high‐density lipoprotein (HDL) cholesterol, use of lipid‐lowering medication, diabetes mellitus, cigarette smoking status, heart rate, creatinine, highest education level, household income, and baseline coronary artery calcium (CAC) score (Exam 1).
Model 3: Model 2 after excluding participants with any coronary heart diseases.
Hazard ratio (HR) per 10 Agatston Unit annual increase in CAC.
Statistically significant HRs (95% CIs).
Table 3.
Hazard Ratios (95% CIs) Showing the Association Between Changes in CAC and Incident Heart Failure in Participants With Baseline CAC=0 and Baseline CAC >0 Separately
| Models (No. of Events/Analyzed) | Baseline CAC=0 | Baseline CAC >0 | ||||
|---|---|---|---|---|---|---|
| Model 1a (49/2923) | Model 2b (46/2791) | Model 3c (33/2741) | Model 1a (133/2721) | Model 2b (122/2593) | Model 3c (57/2308) | |
| Absolute changes in CAC per yeard | 2.02 (1.47–2.78)e | 1.8 (1.21–2.69)e | 1.79 (1.08–2.95)e | 1.04 (1.03–1.05)e | 1.02 (0.999–1.03) | 1.02 (1.001–1.05)e |
| Progressors vs nonprogressors | 3.74 (2.12–6.62)e | 2.52 (1.36–4.67)e | 2.39 (1.15–4.95)e | 1.54 (1.08–2.19)e | 1.09 (0.74–1.59) | 0.98 (0.56–1.68) |
Model 1: unadjusted.
Model 2: adjusted for age, sex, race, BMI, systolic blood pressure (SBP), diastolic blood pressure (DBP), use of antihypertensive medication, total cholesterol, high‐density lipoprotein (HDL) cholesterol, use of lipid‐lowering medication, diabetes mellitus, cigarette smoking status, heart rate, creatinine, highest education level, household income, and baseline coronary artery calcium (CAC) score (Exam 1).
Model 3: Model 2 after excluding participants with any coronary heart diseases.
Hazard ratio (HR) per 10 Agatston Unit annual increase in CAC.
Statistically significant HRs (95% CIs).
Figure 1.
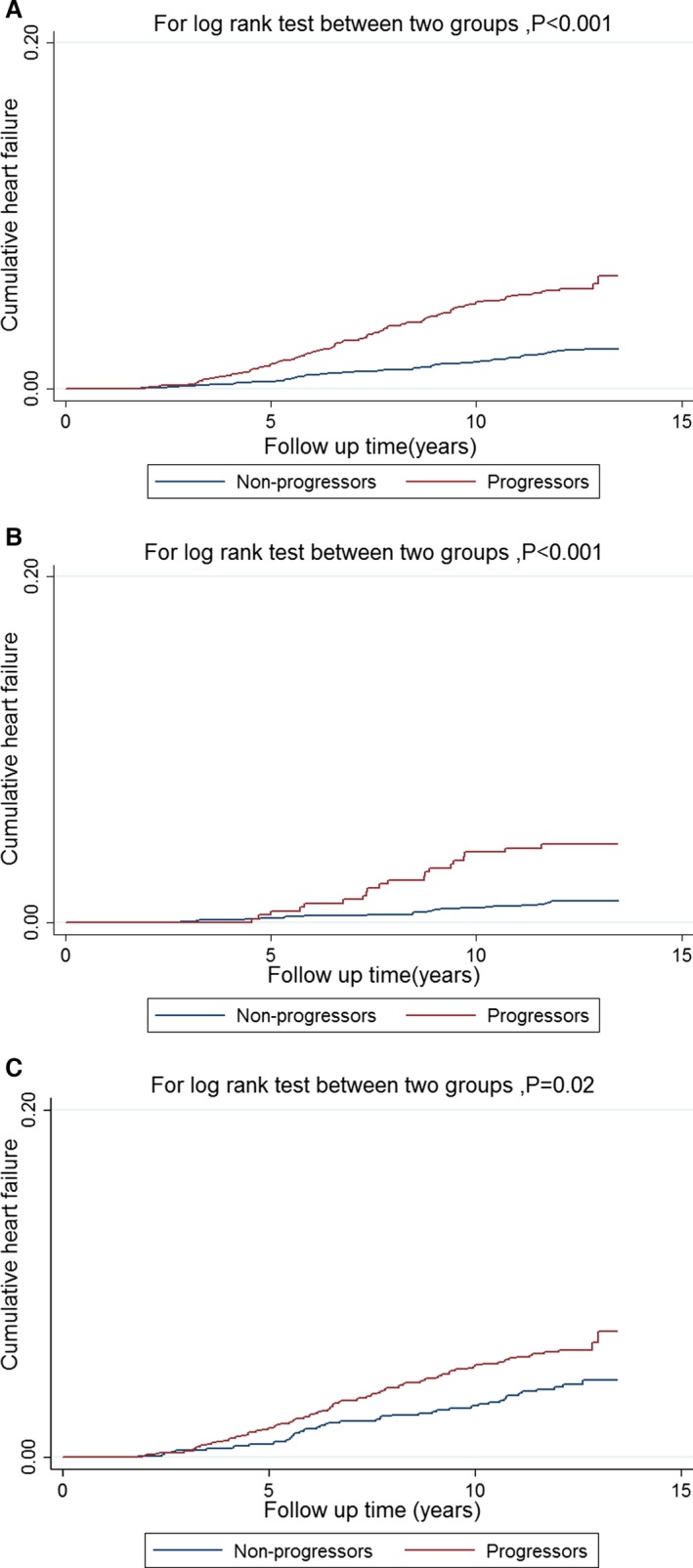
Kaplan–Meier curves of cumulative events show higher rate of incident heart failure in progressors versus nonprogressors in full cohort (A), in participants free of coronary artery calcium (CAC) at baseline (B), and in participants with baseline CAC >0 (C). The Kaplan–Meier curves for progressors and nonprogressors overlap for the first 3 years of follow‐up because we only included the heart failure events that occurred after second CAC measurement.
Follow‐up CMR images (Exam 5) were available for 2818 participants who were free of HF and CHD before the second CAC measurement. Mean±SD of the parameters of LV function and structure have been summarized in Table S2. Compared to participants with baseline CAC >0, participants with baseline CAC=0 showed higher EF and SV and lower LVM and MVR at the follow‐up exam.
Table 4 shows the association between CAC progression and LV function and structure measured by CMR at Exam 5. Longitudinal increase in CAC was associated with higher LVESV (β=0.09; P<0.05) independent of traditional cardiovascular risk factors. This association remained statistically significant after excluding the participants with any CHD. The association between CAC progression and LVEDV became statistically significant only after excluding participants with any CHD (β=0.16; P=0.03). Progressors showed statistically significant associations with increased LVESV (β=0.79; P=0.034) and LVEDV (β=1.21; P<0.05). These associations had reduced statistical significance level after excluding the participants with any CHD. Subgroup analyses were done for participants with baseline CAC=0 and CAC >0 (Tables S3 and S4). In participants with baseline CAC=0, CAC progression was associated with increased LVEDV, LVESV, and LVM in multivariate analysis. By excluding participants with any CHD, these associations were no longer significant.
Table 4.
Estimated Regression Coefficients and Their 95% Confidence Intervals Showing the Association Between CAC Progression and the Left Ventricular Function and Structure Measures by Cardiac Magnetic Resonance in Full Cohort
| Models (n) | Absolute Changes in CAC Per Yeara | Progressors vs Nonprogressors | |
|---|---|---|---|
| EF | Model 1b (2721) | −0.04 (−0.11 to 0.03) | −0.24 (−0.88 to 0.41) |
| Model 2c (2598) | −0.07 (−0.15 to 0.01) | −0.01 (−0.67 to 0.64) | |
| SV | Model 1 (2719) | 0.05 (−0.04 to 0.14) | 0.42 (−0.33 to 1.17) |
| Model 2 (2596) | 0.04 (−0.06 to 0.13) | 0.53 (−0.24 to 1.3) | |
| LVEDV | Model 1 (2720) | 0.14 (−0.01 to 0.28) | 1.21 (0.02–2.39)d |
| Model 2 (2597) | 0.16 (0.01–0.31)d | 0.98 (−0.21–2.18) | |
| LVESV | Model 1 (2719) | 0.09 (0.002–0.18)d | 0.79 (0.06–1.51)d |
| Model 2 (2596) | 0.12 (0.03–0.21)d | 0.44 (−0.26 to 1.15) | |
| LVM | Model 1 (2720) | 0.08 (−0.03 to 0.20) | 0.70 (−0.31 to 1.70) |
| Model 2 (2597) | 0.1 (−0.03 to 0.23) | 0.61 (−0.42 to 1.64) | |
| MVR | Model 1 (2722) | −0.001 (−0.003 to 0.001) | −0.01 (−0.02 to 0.01) |
| Model 2 (2599) | −0.001 (−0.003 to 0.001) | −0.01 (−0.02 to 0.01) |
CAC indicates coronary artery calcium; EF, ejection fraction; LVEDV, left ventricular end diastolic volume; LVESV, left ventricular end systolic volume; LVM, left ventricular mass; MVR, mass to volume ratio; SV, stroke volume.
Coefficient (95% CI) per 10 Agatston Unit annual increase in CAC.
Model 1: adjusted for age, sex, race, BMI, systolic blood pressure (SBP), diastolic blood pressure (DBP), use of antihypertensive medication, total cholesterol, high‐density lipoprotein (HDL) cholesterol, use of lipid‐lowering medication, diabetes mellitus, cigarette smoking status, heart rate, creatinine, highest education level, household income, and baseline CAC score (Exam 1).
Model 2: Model 1 after excluding participants with any coronary heart diseases.
Statistically significant coefficients (95% CIs).
Discussion
Serial CAC measurement has been suggested as a noninvasive method to monitor the progression of CAD.11 It has been proven, in previous studies, that CAC progression is associated with future CHD and all‐cause mortalities.12, 13 In this study, we found CAC progression as a predictor of incident HF independent of traditional risk factors for HF and baseline CAC. We also observed that longitudinal increase in CAC is associated with greater LVESV and LVEDV as measured by CMR independent of known risk factors for HF and overt CHD.
CAD is the most common underlying cause of HF especially in the elderly population.23 LV remodeling after myocardial infarction is a well‐described etiology of HF.24 The necrotic area will be replaced by fibrotic tissue, which is nonfunctional and less elastic than myocytes.5 Additionally, ischemia induces activation of neurohormonal cascade, which, in fact, has a negative impact on the remaining normal myocardium.6 In addition to this pathway, CAD and ischemia may play a crucial rule in the pathophysiology of HF without presenting as a clinically overt CHD.7 In other words, in many patients, HF is the first presentation of CAD.15 In our study, we showed that the association of CAC progression and HF remained statistically significant, even after excluding all participants with CHD. Our result is in agreement with a few previous studies that evaluated the association between baseline CAC and HF.14, 15, 17
Kalsch et al in the Heinz Nixdorf Recall Study has shown a significant association between CAC and history of HF in a univariate cross‐sectional analysis.14 This association became statistically insignificant after adjusting for traditional cardiovascular risk factors. The investigators explained this diminished association by the fact that cardiovascular risk factors like hypertension can lead to both CAC formation and HF. Sakuragi et al recently reported the result of a study on 487 Japanese participants free of CAD and HF at enrollment.17 During the mean follow‐up of 497±315 days, 9 participants developed incident HF without any overt CHD. Higher CAC was associated with higher incidence of HF and higher NT‐pro BNP level. The number of incident HFs in this study was limited and the investigators proposed a multicenter study to confirm the association of CAC and HF. In another study, Leening et al investigated the association between baseline CAC and HF in the Rotterdam study.15 In this population‐based study, 1897 participants free of any history of CHD and HF were followed for a median of 6.8 years for incident HF and CHD events. Baseline CAC was strongly associated with higher incidence of HF independent of traditional cardiovascular risk factors. This association remained statistically significant after excluding the participants with incident myocardial infarction or revascularization procedures. This study was done on a Dutch elderly population, and the result cannot be extrapolated to the middle‐age population and other ethnic groups.
There are some possible explanations for the association between CAD and HF in patients without overt CHD. Coronary artery endothelial dysfunction is an integral part of the cascade that eventually results in atherosclerotic plaque formation.25 Dysfunctional endothelium produces more vasoconstrictors like endothelin instead of vasodilator substances.26 These vasoconstrictor substances have a direct detrimental effect on the myocardium, which eventually lead to myocardial fibrosis and HF.27 In addition, in patients without clinically overt CHD, chronic ischemia/hypoperfusion may result in a hibernating myocardium.6 Consequently, in the affected area, apoptosis may occur, which, in turn, will result in myocardial dysfunction.28
In the second part of the study, we observed a direct association between CAC progression and follow‐up LVESV and LVEDV, independent of baseline CAC, traditional cardiovascular risk factors, and overt CHD. The result of our study is in line with a few previous studies that investigated the relationship between subclinical atherosclerosis and LV dysfunction.29, 30 Edvardsen et al studied the relation between regional CAC and regional LV systolic dysfunction in 509 MESA participants.29 High regional CAC were associated with regional myocardial dysfunction defined by LV circumferential strain and strain rate in the same perfusion territory. However, this study did not show any association between increased CAC and decrease in SV and EF. In another study, Colletti et al investigated the association between CAC and LV dysfunction measured by CMR.30 At enrollment, the participants of the South Bay Heart Watch (SBHW) were older than 45 years with various cardiovascular risk factors, but without any evidence of CHD. CAC was measured in a group of 1312 SBHW participants. After a mean of ≈11 years, 386 participants underwent CMR to measure LV function parameter, including EF, peak filling rate, and regional wall motion abnormalities (RWMAs). The association between baseline CAC and follow‐up RWMA remained statistically significant even after adjusting for cardiovascular risk factors.
The clinical importance of subclinical LV dilatation has been shown in previous studies.31, 32, 33 In a study on participants of the Framingham Heart Study and Framingham Offspring Study, 4744 individuals free of myocardial infarction and HF who underwent echocardiography at baseline were followed for incident HF.32 It was shown that increased LVED and LVES dimensions were associated with higher incidence of future HF. In another study, Yeboah et al demonstrated the association between LV dilatation measured by CMR at baseline with incident HF in 4974 MESA participants during over 9.4 years follow‐up.33
In our study, progressors failed to show any statistically significant increase in incidence of HF or subclinical decrease in EF and SV in adjusted models. There are some explanations for this finding. CAC and HF share many common risk factors like SBP, which behave as confounders in their relation. The association between CAC and HF is not as strong as the association between CAC and CHD, and by categorizing the participants, there is not enough power to detect this association. Finally, there are many different definitions in the literature for progressors. Utilizing different methods to define progressors will cause at least minor discrepancy in the results.
Strength and Limitations
MESA is a well‐designed, multiethnic, population‐based study with long‐term follow‐up. In addition to the general strength of MESA, our study is the first to investigate the association of CAC progression with HF and subclinical LV dysfunction. There are some limitations that need to be mentioned. MESA participants were free of any cardiovascular disease at study entry, and the number of events can be different from general population. The HF event ascertainment in MESA is based on the data collected from medical records at the time of diagnosis and therefore is subject to misclassification from accuracy and performance of the diagnostic tools, such as echocardiography and clinical data. Nevertheless, this is the standard method in most of the large‐scale, prospective cohort studies, where the event ascertainment and data collection on events are often performed after the events have already occurred.34, 35, 36 Additionally, given the unavailability of EF at the time of diagnosis of HF for all participants, we did not differentiate cases into HF with preserved EF and HF with reduced EF. For the subclinical assessment of LV, CMR was available for less than half of the participants. Although we found a statistically significant association between longitudinal increase in CAC and LVESV and LVEDV, the strength of the association is not strong enough to be meaningfully translated into clinical practice.
Conclusion
In a multiethnic, population‐based study, we have shown that CAC progression predicts incident HF and increased LVEDV and LVESV measured by CMR at follow‐up exam independent of traditional cardiovascular risk factor, baseline CAC, and overt CHD. Despite the presence of the statistically significant association between CAC progression and subclinical LV dilatation in participants free of any CHD, these weak associations may not be of any clinical significance. We recommend further research to identify the subgroup of individuals who will benefit from serial CAC measurement for cardiovascular risk stratification.
Sources of Funding
This research was supported by contracts HHSN268201500003I, N01‐HC‐95159, N01‐HC‐95160, N01‐HC‐95161, N01‐HC‐95162, N01‐HC‐95163, N01‐HC‐95164, N01‐HC‐95165, N01‐HC‐95166, N01‐HC‐95167, N01‐HC‐95168, and N01‐HC‐95169 from the National Heart, Lung, and Blood Institute and by grants UL1‐TR‐000040, UL1‐TR‐001079, and UL1‐TR‐001420 from the National Center for Advancing Translational Sciences.
Disclosures
Budoff reports grant support from NIH and General Electric. Lima reports grant support from Toshiba Medical Systems.
Supporting information
Table S1. Hazard Ratios (95% CIs) Showing the Association Between CAC Progression and Incident Heart Failure in Participants With Available Measurements of Baseline NT‐proBNP
Table S2. Comparing the Parameter of LV Function and Structure Measured by Cardiac Magnetic Resonance in Participants With Baseline CAC=0 and Participants With Baseline CAC >0
Table S3. Estimated Regression Coefficients and Their 95% Confidence Intervals Showing the Association Between CAC Progression and the Left Ventricular Function and Structure Measures by Cardiac MRI in Participants With Baseline CAC=0
Table S4. Estimated Regression Coefficients and Their 95% Confidence Intervals Showing the Association Between CAC Progression and the Left Ventricular Function and Structure Measures by Cardiac MRI in Participants With Baseline CAC >0
Acknowledgments
The authors thank the other investigators, the staff, and the participants of the MESA study for their valuable contributions. A full list of participating MESA investigators and institutions can be found at http://www.mesa-nhlbi.org. The views expressed in this article are those of the authors and do not necessarily represent the views of the National Heart, Lung, and Blood Institute; the National Institutes of Health; or the US Department of Health and Human Services.
(J Am Heart Assoc. 2017;6:e005253 DOI: 10.1161/JAHA.116.005253.)28428195
References
- 1. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, de Ferranti S, Despres JP, Fullerton HJ, Howard VJ, Huffman MD, Isasi CR, Jimenez MC, Judd SE, Kissela BM, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Magid DJ, McGuire DK, Mohler ER III, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Rosamond W, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Woo D, Yeh RW, Turner MB. Heart disease and stroke statistics—2016 update: a report from the American Heart Association. Circulation. 2016;133:e38–e360. [DOI] [PubMed] [Google Scholar]
- 2. Velagaleti RS, Vasan RS. Heart failure in the twenty‐first century: is it a coronary artery disease or hypertension problem? Cardiol Clin. 2007;25:487–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Liu L, Eisen HJ. Epidemiology of heart failure and scope of the problem. Cardiol Clin. 2014;32:1–8. [DOI] [PubMed] [Google Scholar]
- 4. Bui AL, Horwich TB, Fonarow GC. Epidemiology and risk profile of heart failure. Nat Rev Cardiol. 2011;8:30–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Johnson FL. Pathophysiology and etiology of heart failure. Cardiol Clin. 2014;32:9–19. [DOI] [PubMed] [Google Scholar]
- 6. Gheorghiade M, Sopko G, De Luca L, Velazquez EJ, Parker JD, Binkley PF, Sadowski Z, Golba KS, Prior DL, Rouleau JL, Bonow RO. Navigating the crossroads of coronary artery disease and heart failure. Circulation. 2006;114:1202–1213. [DOI] [PubMed] [Google Scholar]
- 7. Gheorghiade M, Bonow RO. Chronic heart failure in the United States: a manifestation of coronary artery disease. Circulation. 1998;97:282–289. [DOI] [PubMed] [Google Scholar]
- 8. Owens AT, Jessup M. What if we could prevent heart failure?. JACC Cardiovasc Imaging. 2012;5:881–883. DOI: 10.1016/j.jcmg.2012.06.005. [DOI] [PubMed] [Google Scholar]
- 9. Tota‐Maharaj R, Al‐Mallah MH, Nasir K, Qureshi WT, Blumenthal RS, Blaha MJ. Improving the relationship between coronary artery calcium score and coronary plaque burden: addition of regional measures of coronary artery calcium distribution. Atherosclerosis. 2015;238:126–131. [DOI] [PubMed] [Google Scholar]
- 10. Hecht HS. Coronary artery calcium scanning: past, present, and future. JACC Cardiovasc Imaging. 2015;8:579–596. [DOI] [PubMed] [Google Scholar]
- 11. Budoff MJ, Raggi P. Coronary artery disease progression assessed by electron‐beam computed tomography. Am J Cardiol. 2001;88:46E–50E. [DOI] [PubMed] [Google Scholar]
- 12. Budoff MJ, Young R, Lopez VA, Kronmal RA, Nasir K, Blumenthal RS, Detrano RC, Bild DE, Guerci AD, Liu K, Shea S, Szklo M, Post W, Lima J, Bertoni A, Wong ND. Progression of coronary calcium and incident coronary heart disease events: mesa (Multi‐Ethnic Study of Atherosclerosis). J Am Coll Cardiol. 2013;61:1231–1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Budoff MJ, Hokanson JE, Nasir K, Shaw LJ, Kinney GL, Chow D, Demoss D, Nuguri V, Nabavi V, Ratakonda R, Berman DS, Raggi P. Progression of coronary artery calcium predicts all‐cause mortality. JACC Cardiovasc Imaging. 2010;3:1229–1236. [DOI] [PubMed] [Google Scholar]
- 14. Kalsch H, Lehmann N, Mohlenkamp S, Neumann T, Slomiany U, Schmermund A, Stang A, Moebus S, Bauer M, Mann K, Jockel KH, Erbel R. Association of coronary artery calcium and congestive heart failure in the general population: results of the Heinz Nixdorf Recall study. Clin Res Cardiol. 2010;99:175–182. [DOI] [PubMed] [Google Scholar]
- 15. Leening MJ, Elias‐Smale SE, Kavousi M, Felix JF, Deckers JW, Vliegenthart R, Oudkerk M, Hofman A, Steyerberg EW, Stricker BH, Witteman JC. Coronary calcification and the risk of heart failure in the elderly: the Rotterdam Study. JACC Cardiovasc Imaging. 2012;5:874–880. [DOI] [PubMed] [Google Scholar]
- 16. Latif MA, Budoff MJ. Coronary artery calcium scanning: a useful tool for refining heart failure risk prediction? Future Cardiol. 2013;9:1–3. [DOI] [PubMed] [Google Scholar]
- 17. Sakuragi S, Ichikawa K, Yamada K, Tanimoto M, Miki T, Otsuka H, Yamamoto K, Kawamoto K, Katayama Y, Tanakaya M, Ito H. An increase in the coronary calcification score is associated with an increased risk of heart failure in patients without a history of coronary artery disease. J Cardiol. 2016;67:358–364. [DOI] [PubMed] [Google Scholar]
- 18. Bild DE, Bluemke DA, Burke GL, Detrano R, Diez Roux AV, Folsom AR, Greenland P, Jacob DR Jr, Kronmal R, Liu K, Nelson JC, O'Leary D, Saad MF, Shea S, Szklo M, Tracy RP. Multi‐Ethnic Study of Atherosclerosis: objectives and design. Am J Epidemiol. 2002;156:871–881. [DOI] [PubMed] [Google Scholar]
- 19. Carr JJ, Nelson JC, Wong ND, McNitt‐Gray M, Arad Y, Jacobs DR Jr, Sidney S, Bild DE, Williams OD, Detrano RC. Calcified coronary artery plaque measurement with cardiac CT in population‐based studies: standardized protocol of Multi‐Ethnic Study of Atherosclerosis (MESA) and Coronary Artery Risk Development in Young Adults (CARDIA) study. Radiology. 2005;234:35–43. [DOI] [PubMed] [Google Scholar]
- 20. Ambale Venkatesh B, Volpe GJ, Donekal S, Mewton N, Liu CY, Shea S, Liu K, Burke G, Wu C, Bluemke DA, Lima JA. Association of longitudinal changes in left ventricular structure and function with myocardial fibrosis: the Multi‐Ethnic Study of Atherosclerosis study. Hypertension. 2014;64:508–515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Natori S, Lai S, Finn JP, Gomes AS, Hundley WG, Jerosch‐Herold M, Pearson G, Sinha S, Arai A, Lima JA, Bluemke DA. Cardiovascular function in Multi‐Ethnic Study of Atherosclerosis: normal values by age, sex, and ethnicity. AJR Am J Roentgenol. 2006;186:S357–S365. [DOI] [PubMed] [Google Scholar]
- 22. Berry JD, Liu K, Folsom AR, Lewis CE, Carr JJ, Polak JF, Shea S, Sidney S, O'Leary DH, Chan C, Lloyd‐Jones DM. Prevalence and progression of subclinical atherosclerosis in younger adults with low short‐term but high lifetime estimated risk for cardiovascular disease: the coronary artery risk development in young adults study and Multi‐Ethnic Study of Atherosclerosis. Circulation. 2009;119:382–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Dei Cas L, Metra M, Nodari S, Dei Cas A, Gheorghiade M. Prevention and management of chronic heart failure in patients at risk. Am J Cardiol. 2003;91:10F–17F. [DOI] [PubMed] [Google Scholar]
- 24. Sutton MG, Sharpe N. Left ventricular remodeling after myocardial infarction: pathophysiology and therapy. Circulation. 2000;101:2981–2988. [DOI] [PubMed] [Google Scholar]
- 25. Gimbrone MA Jr, Garcia‐Cardena G. Endothelial cell dysfunction and the pathobiology of atherosclerosis. Circ Res. 2016;118:620–636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Luscher TF, Boulanger CM, Dohi Y, Yang ZH. Endothelium‐derived contracting factors. Hypertension. 1992;19:117–130. [DOI] [PubMed] [Google Scholar]
- 27. Colucci WS. Molecular and cellular mechanisms of myocardial failure. Am J Cardiol. 1997;80:15L–25L. [DOI] [PubMed] [Google Scholar]
- 28. Stephanou A, Brar BK, Scarabelli TM, Jonassen AK, Yellon DM, Marber MS, Knight RA, Latchman DS. Ischemia‐induced STAT‐1 expression and activation play a critical role in cardiomyocyte apoptosis. J Biol Chem. 2000;275:10002–10008. [DOI] [PubMed] [Google Scholar]
- 29. Edvardsen T, Detrano R, Rosen BD, Carr JJ, Liu K, Lai S, Shea S, Pan L, Bluemke DA, Lima JA. Coronary artery atherosclerosis is related to reduced regional left ventricular function in individuals without history of clinical cardiovascular disease: the Multiethnic Study of Atherosclerosis. Arterioscler Thromb Vasc Biol. 2006;26:206–211. [DOI] [PubMed] [Google Scholar]
- 30. Colletti PM, Dustin LD, Wong ND, Shriki JE, Kawakubo M, Azen SP, Detrano RC. Does coronary calcium score predict future cardiac function? Association of subclinical atherosclerosis with left ventricular systolic and diastolic dysfunction at MR imaging in an elderly cohort. Radiology. 2010;257:64–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Lauer MS, Evans JC, Levy D. Prognostic implications of subclinical left ventricular dilatation and systolic dysfunction in men free of overt cardiovascular disease (the Framingham Heart Study). Am J Cardiol. 1992;70:1180–1184. [DOI] [PubMed] [Google Scholar]
- 32. Vasan RS, Larson MG, Benjamin EJ, Evans JC, Levy D. Left ventricular dilatation and the risk of congestive heart failure in people without myocardial infarction. N Engl J Med. 1997;336:1350–1355. [DOI] [PubMed] [Google Scholar]
- 33. Yeboah J, Bluemke DA, Hundley WG, Rodriguez CJ, Lima JA, Herrington DM. Left ventricular dilation and incident congestive heart failure in asymptomatic adults without cardiovascular disease: Multi‐Ethnic Study of Atherosclerosis (MESA). J Card Fail. 2014;20:905–911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Bleumink GS, Knetsch AM, Sturkenboom MC, Straus SM, Hofman A, Deckers JW, Witteman JC, Stricker BH. Quantifying the heart failure epidemic: prevalence, incidence rate, lifetime risk and prognosis of heart failure the Rotterdam Study. Eur Heart J. 2004;25:1614–1619. [DOI] [PubMed] [Google Scholar]
- 35. Kucharska‐Newton AM, Heiss G, Ni H, Stearns SC, Puccinelli‐Ortega N, Wruck LM, Chambless L. Identification of heart failure events in Medicare claims: the Atherosclerosis Risk in Communities (ARIC) Study. J Card Fail. 2016;22:48–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Rosamond WD, Chang PP, Baggett C, Johnson A, Bertoni AG, Shahar E, Deswal A, Heiss G, Chambless LE. Classification of heart failure in the Atherosclerosis Risk in Communities (ARIC) Study: a comparison of diagnostic criteria. Circ Heart Fail. 2012;5:152–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Hazard Ratios (95% CIs) Showing the Association Between CAC Progression and Incident Heart Failure in Participants With Available Measurements of Baseline NT‐proBNP
Table S2. Comparing the Parameter of LV Function and Structure Measured by Cardiac Magnetic Resonance in Participants With Baseline CAC=0 and Participants With Baseline CAC >0
Table S3. Estimated Regression Coefficients and Their 95% Confidence Intervals Showing the Association Between CAC Progression and the Left Ventricular Function and Structure Measures by Cardiac MRI in Participants With Baseline CAC=0
Table S4. Estimated Regression Coefficients and Their 95% Confidence Intervals Showing the Association Between CAC Progression and the Left Ventricular Function and Structure Measures by Cardiac MRI in Participants With Baseline CAC >0


