Abstract
Background
The impact of the 2013 American College of Cardiology/American Heart Association cholesterol guidelines on statin eligibility in individuals otherwise destined to experience cardiovascular disease (CVD) events is unclear.
Methods and Results
We analyzed a prospective cohort of consecutive ST‐segment elevation myocardial infarction (STEMI) patients from a regional STEMI system with data on patient demographics, low‐density lipoprotein cholesterol levels, CVD risk factors, medication use, and outpatient visits over the 2 years prior to STEMI. We determined pre‐STEMI eligibility according to American College of Cardiology/American Heart Association guidelines and the prior Third Report of the Adult Treatment Panel guidelines. Our sample included 1062 patients with a mean age of 63.7 (13.0) years (72.5% male), and 761 (71.7%) did not have known CVD prior to STEMI. Only 62.5% and 19.3% of individuals with and without prior CVD were taking a statin before STEMI, respectively. In individuals not taking a statin, median (interquartile range) low‐density lipoprotein cholesterol levels in those with and without known CVD were low (108 [83, 138] mg/dL and 110 [87, 133] mg/dL). For individuals not taking a statin, only 38.7% were statin eligible by ATP III guidelines. Conversely, 79.0% would have been statin eligible according to American College of Cardiology/American Heart Association guidelines. Less than half of individuals with (49.2%) and without (41.1%) prior CVD had seen a primary care provider during the 2 years prior to STEMI.
Conclusions
In a large cohort of STEMI patients, application of American College of Cardiology/American Heart Association guidelines more than doubled pre‐STEMI statin eligibility compared with Third Report of the Adult Treatment Panel guidelines. However, access to and utilization of health care, a necessity for guideline implementation, was suboptimal prior to STEMI.
Keywords: cholesterol, prevention, statin, ST‐segment elevation myocardial infarction
Subject Categories: Epidemiology, Statements and Guidelines, Lipids and Cholesterol, Acute Coronary Syndromes
Introduction
Approximately one third of myocardial infarctions (MIs) present as ST‐segment elevation MI (STEMI).1 STEMI is a cardiovascular emergency, frequently complicated by cardiogenic shock or cardiac arrest, and thus emergent percutaneous coronary intervention is the standard of care. It remains one of the most costly and morbid presentations of cardiovascular disease (CVD) and therefore prevention of STEMI is of utmost importance. Although the incidence of STEMI in the United States has been declining over the past 3 decades, it remains a common CVD event.1, 2 This decline has largely been attributed to declining rates of tobacco use and improved control of traditional cardiovascular risk factors, including low‐density lipoprotein cholesterol (LDL‐C).3, 4, 5
Total cholesterol and LDL‐C levels declined in the United States from 1988 to 2010 in individuals both taking and not taking lipid‐lowering medications.6 Statin therapy remains the mainstay of the treatment of elevated cholesterol and has been shown to substantially lower the risk of MI in both primary and secondary prevention.7, 8, 9, 10 This benefit has been largely independent of baseline LDL‐C, including in individuals with a baseline LDL‐C <100 mg/dL.10 Additionally, prior data have shown that LDL‐C, although a clear CVD risk factor, does not improve discrimination for future CVD events when added to age and other traditional risk factors.11 Therefore, relying on absolute risk to determine statin eligibility may substantially increase eligibility in patients otherwise destined to develop STEMI. In contrast to the prior Third Report of the Adult Treatment Panel (ATP III) guidelines for the treatment of cholesterol that relied heavily on LDL‐C levels,12 the 2013 American College of Cardiology (ACC)/American Heart Association (AHA) cholesterol guidelines have endorsed a strategy recommending statin allocation largely based on absolute CVD risk.13
We previously reported that use of preventive CVD medications prior to STEMI was low, with only 7.8% of individuals taking aspirin and a statin before their event.14 In this analysis, our aim was to contrast the rates of pre‐STEMI statin eligibility according to ACC/AHA guidelines compared with the prior ATP III guidelines in a contemporary, prospective cohort of STEMI patients. Implementation of either guideline to a given population requires access to and utilization of preventive health care, so we also analyzed the frequency of visits to both primary care providers as well as cardiovascular medicine providers in the 2 years prior to STEMI.
Methods
Study Design and Patients
The Minneapolis Heart Institute Level 1 MI program is a regional transfer system using a standardized protocol designed to improve time to treatment and clinical outcomes in patients with STEMI presenting directly to the percutaneous coronary intervention center as well as community hospitals without percutaneous coronary intervention capability. The system was established in 2003, and its design and results have been previously published.15, 16, 17 Standardized protocols and predetermined transfer plans are implemented for each site. Patients are enrolled in a comprehensive, prospective database and followed for 5 years. Inclusion criteria for the prospective registry are ECG findings consistent with STEMI or new left bundle branch block in patients with chest pain of <24 hours' duration. There are no exclusions; thus, the registry includes patients of all ages as well as those with out‐of‐hospital cardiac arrest and cardiogenic shock. The study was funded by the Minneapolis Heart Institute Research Foundation, Minneapolis, Minnesota. No extramural funding was used to support this work. Institutional review board approval was obtained for data collection, follow‐up, and data analysis.
From January 1, 2011, until December 31, 2014, there were 1476 consecutive patients with STEMI enrolled in the database. We excluded 226 without a clear culprit artery, 116 who did not have a lipid panel on admission, 69 who did not have percutaneous coronary intervention performed, 2 who we could not identify whether a history of CVD was present, and 1 patient who was missing admission medication data, leaving 1062 STEMI patients in the final sample.
Patient Demographics, Pre–ST‐Segment Elevation Myocardial Infarction Medication Use, and Utilization of Care
The Level 1 MI program occurs within the parameters of a healthcare system (Allina Health) with a unified electronic health record (EHR). Age, sex, race, height, weight, systolic blood pressure (SBP), family history of CVD, and history of tobacco use were recorded using data from the patient's EHR. BMI was calculated as the weight in kilometers divided by the height in meters squared. Total cholesterol, high‐density lipoprotein cholesterol, triglycerides, and a calculated LDL‐C were obtained from a fasting lipid panel drawn the day of or morning after admission, which is part of the standardized STEMI admission order set.
A prior diagnosis of CVD; diagnoses of hypertension, dyslipidemia, or diabetes mellitus; and a family history of CVD were recorded from the patient's active medical problems listed in the EHR as well as by reviewing the history and physical examination by the admitting physician at the time of the STEMI. Preadmission medications were recorded from the EHR and confirmed by review of the medication reconciliation note recorded by the registered nurse at the time of admission. For the medication reconciliation note documented by the admitting registered nurse, each nurse is expected to verify the medication list in the EHR with the patient or the patient's outpatient medication list. If the medication list cannot be verified by those means, the patient's primary care physician or pharmacy is contacted to verify the patient's medications. We specifically recorded the preadmission use of aspirin (any dose), antiplatelet medications (clopidogrel, prasugrel, ticagrelor), statin medications (20–40 mg/d of rosuvastatin and 40–80 mg/d of atorvastatin were considered high‐intensity statins), and antihypertensive medications (calcium channel blockers, angiotensin‐converting enzyme inhibitors/angiotensin receptor blockers, β‐blockers, and diuretics).
We also recorded the presence of any documented clinical encounters in the 2 years before the individual's STEMI. Encounters were classified as primary care if the visit was to a provider in the field of internal medicine, family practice, or obstetrics/gynecology. Encounters with cardiovascular medicine providers were also recorded. Encounters with other subspecialists (eg, urologists and dermatologists) were not included. When available, blood pressure recordings from outpatient clinic visits were documented for use in risk calculation.
Indications for Statin Therapy and Calculation of 10‐Year Cardiovascular Disease Risk
Indications for statin therapy pre‐STEMI were analyzed according to ATP III guidelines,12 which were the relevant cholesterol guidelines in the United States for the majority of our analysis period, and 2013 ACC/AHA guidelines.13 ATP III guidelines defined thresholds for control of hyperlipidemia, with an LDL‐C goal of <100 mg/dL for individuals with known coronary heart disease, other CVD, diabetes mellitus, or a 10‐year coronary heart disease risk of >20% according to the Framingham Risk Score; an LDL‐C goal of <130 mg/dL for individuals with 2 or more major CVD risk factors; and an LDL‐C goal of <160 mg/dL in individuals with 0 or 1 risk factor. LDL‐C levels were used from fasting lipid levels obtained on admission at the time of STEMI.
The ACC/AHA guidelines include 4 major indications for statin therapy: (1) a diagnosis of clinical CVD (acute coronary syndromes, history of MI, stable angina, coronary or other arterial revascularization, stroke, transient ischemic attack, or peripheral arterial disease of atherosclerotic origin); (2) a diagnosis of diabetes mellitus; (3) an LDL‐C >190 mg/dL; and (4) an estimated 10‐year CVD risk >7.5% according to the Pooled Cohort Equations calculator. For individuals meeting 1 of these 4 criteria, a moderate‐ to high‐intensity statin is a class I recommendation for individuals younger than 75 years. For individuals with a 10‐year CVD risk 5% to 7.5%, a moderate‐intensity statin can be considered (class IIa recommendation). Individuals with a 10‐year CVD risk <5% are recommended to not receive pharmacological treatment to lower their cholesterol.
For individuals without known CVD, diabetes mellitus, or an LDL‐C >190 mg/dL, we calculated the 10‐year CVD risk according to the Pooled Equations calculator.13 We used EHR data at the time of STEMI for age, sex, race, total cholesterol, high‐density lipoprotein cholesterol, history of antihypertensive treatment, and diabetes mellitus. Given the instability of blood pressure in the setting of STEMI, we did not use the SBP at the time of admission. Instead, we used the SBP from the most recent ambulatory visit to a primary care provider or cardiovascular medicine provider in the prior 2 years. For individuals missing data on SBP (n=354), we imputed SBP using the median SBP from individuals with known data on SBP stratified into 3 categories, no history of hypertension, treated hypertension, and untreated hypertension.
Statistical Analysis and Assessment of Pre–ST‐Segment Elevation Myocardial Infarction Statin Eligibility
Baseline characteristics were analyzed after stratification by CVD status prior to STEMI. Descriptive statistics are displayed as mean (SD) for continuous variables, and as number (percentage) for categorical variables. When continuous variables had a skewed distribution, median (25th, 75th percentiles) were reported. Categorical variables were analyzed using Pearson's chi‐square or Fisher's exact tests. Continuous variables were analyzed using Student t test for normally distributed variables or Kruskal–Wallis tests for continuous variables with a non‐normal distribution. Preadmission medication use and lipid levels were also analyzed stratified by CVD status. We then assessed pre‐STEMI statin eligibility in 2 ways. First, we analyzed eligibility by both ATP III and ACC/AHA guidelines in individuals who were not taking statin therapy before their event (the majority of the sample). Second, we calculated pre‐STEMI statin eligibility for the entire sample with estimation of off‐treatment lipid values in those taking statin therapy by assuming a 30% increase in LDL‐C for the ATP III guidelines and a 20% increase in total cholesterol and no change in high‐density lipoprotein cholesterol for the ACC/AHA guidelines.
We also performed a prespecified sex analysis comparing pre‐STEMI statin eligibility according to sex in individuals not taking statin therapy prior to STEMI. Additionally, a sensitivity analysis was performed assuming a low (115/60 mm Hg) and elevated (150/90 mm Hg) SBP for individuals with missing blood pressure data. Finally, we calculated the prevalence of access to and utilization of both primary care and cardiovascular medicine in the 2 years prior to STEMI in those with and without known CVD. All statistical calculations were performed in Stata 14.1 (StataCorp LP, College Station, TX).
Results
Baseline Demographics and Pre–ST‐Segment Elevation Myocardial Infarction Cardiovascular Disease Medication Use
The baseline characteristics of the 1062 STEMI patients are shown in Table 1 stratified by a diagnosis of CVD prior to STEMI. The majority (71.7%) of STEMI patients did not have known CVD prior to STEMI. Rates of current smoking were high in those without and with prior CVD (36.8% and 25.6%, respectively). Compared with those without known CVD, STEMI patients with prior CVD were more likely to have a diagnosis of hypertension (79.7% versus 49.7%) and dyslipidemia (87.3% versus 41.0%) prior to STEMI (P<0.001 of both).
Table 1.
Baseline Characteristics, Prescribed Preadmission Medications, and Lipid Levels of 1062 STEMI Patients Stratified by the Presence of Previously Diagnosed CVD
| Characteristic | No Prior CVD (n=761) | Prior CVD (n=301) | P Value |
|---|---|---|---|
| Age, y | 62.5±13.0 | 66.8±12.6 | <0.001 |
| Men, No. (%) | 541 (71.1) | 229 (76.1) | 0.10 |
| Race, No. (%) | |||
| White | 699 (91.9) | 285 (94.7) | 0.61 |
| Black | 18 (2.4) | 4 (1.3) | |
| Asian | 6 (0.8) | 2 (0.7) | |
| Hispanic | 7 (0.9) | 2 (0.7) | |
| Other/not listed | 31 (4.1) | 8 (2.7) | |
| BMI, kg/m2 | 29.6±6.1 | 29.2±5.7 | 0.28 |
| Smoking, % | |||
| Current smoker | 280 (36.8) | 77 (25.6) | <0.001 |
| Former smoker | 188 (24.7) | 120 (39.9) | |
| Never smoker | 293 (38.5) | 120 (39.9) | |
| Hypertension, No. (%) | 378 (49.7) | 239 (79.4) | <0.001 |
| Dyslipidemia, No. (%) | 311 (40.9) | 262 (87.0) | <0.001 |
| Diabetes mellitus, No. (%) | 127 (16.7) | 82 (27.2) | <0.001 |
| Family history of CHD, No. (%) | 276 (36.3) | 108 (35.9) | 0.99 |
| Medication, No. (%) | |||
| Aspirin | 210 (27.6) | 224 (74.4) | <0.001 |
| Other antiplatelet* | 2 (0.3) | 69 (22.9) | <0.001 |
| Dual antiplatelet | 0 (0) | 59 (19.6) | <0.001 |
| Any antihypertensive | 276 (36.3) | 227 (75.4) | <0.001 |
| ACEI/ARB | 154 (20.2) | 136 (45.2) | <0.001 |
| β‐Blocker | 110 (14.5) | 176 (58.5) | <0.001 |
| CCB | 65 (8.5) | 39 (13.0) | 0.026 |
| Diuretic | 111 (14.6) | 33 (11.0) | 0.13 |
| Statin | 147 (19.3) | 188 (62.5) | <0.001 |
| High‐intensity statin | 17 (2.2) | 55 (18.3) | <0.001 |
| Lipid Levels | No Statin (n=614) | Taking Statin (n=147) | No Statin (n=113) | Taking Statin (n=188) |
|---|---|---|---|---|
| Total cholesterol, mg/dL | 175 (147, 200) | 150 (130, 177) | 173 (142, 201) | 140 (121, 164) |
| HDL‐C, mg/dL | 36 (31, 43) | 37 (32, 43) | 34 (29, 41) | 36 (30, 42) |
| Triglycerides, mg/dL | 122 (88, 166) | 114 (83, 148) | 127 (91, 170) | 118 (88, 163) |
| LDL‐C, mg/dL | 110 (87, 133) | 83 (67, 111) | 108 (83, 138) | 77 (59, 98) |
wACEI indicates angiotensin‐converting enzyme inhibitor; ARB, angiotensin receptor blocker; CCB, calcium channel blocker; CHD, coronary heart disease; CVD, cardiovascular disease; HDL‐C, high‐density lipoprotein cholesterol; LDL‐C, low‐density lipoprotein cholesterol; STEMI, ST‐segment elevation myocardial infarction. Lipid Values are presented as median (interquartile range). *Other antiplatelet agents include clopidogrel, prasugrel, and ticagrelor.
The prevalence of preventive medication utilization prior to STEMI in those without known CVD was low, with 27.9% prescribed aspirin and only 19.3% a statin. On average, LDL‐C levels in STEMI patients without prior CVD were not significantly elevated regardless of the use of statin therapy (median LDL‐C 83 [67, 111] mg/dL in those taking statin therapy and 110 [87, 133] mg/dL in those not taking statin therapy). In individuals with known CVD prior to STEMI, the utilization of preventive medications was higher but suboptimal (75.9% reporting use of aspirin, 75.4% an antihypertensive, and 62.5% a statin). In individuals with prior CVD, the median LDL‐C was 108 [83, 138] mg/dL in those not taking a statin and 77 [59, 98] mg/dL in those taking a statin.
Pre–ST‐Segment Elevation Myocardial Infarction Statin Eligibility
The prevalence of statin eligibility prior to STEMI according to ATP III guidelines in our sample is shown in Table 2. In individuals who were not taking statin therapy prior to STEMI, 38.7% had LDL‐C levels that were not at goal by ATP III guidelines and were therefore statin eligible. Estimating off‐treatment lipids levels (assuming a 30% increase in LDL‐C) for those taking statin therapy and including them in the analysis resulted in minimal change in the prevalence of statin eligibility by ATP III guidelines (42.0% were statin eligible).
Table 2.
Pre‐STEMI Statin Eligibility According to ATP III Cholesterol Guidelines
| APT III CHD Risk Categories | ||||||
|---|---|---|---|---|---|---|
| 0 or 1 Risk Factor | 2 Risk Factors | CHD Risk >20% | Diabetes Mellitus | Prevalent CHD | Total | |
| 727 STEMI patients not taking statin therapy prior to STEMI | ||||||
| LDL‐C goal | <160 mg/dL | <130 mg/dL | <100 mg/dL | <100 mg/dL | <100 mg/dL | |
| No. | 65 | 380 | 90 | 79 | 113 | 727 |
| Age, y | 56.9±13.8 | 60.3±12.6 | 68.1±10.8 | 68.0±12.9 | 65.7±13.4 | 62.6±13.2 |
| Women, No. (%) | 29 (44.6) | 103 (27.1) | 4 (4.4) | 34 (43.0) | 25 (22.1) | 195 (26.8) |
| LDL‐C, mg/dL | 109 (86, 137) | 108 (87, 130) | 124 (106, 145) | 95 (72, 118) | 108 (83, 138) | 109 (86, 134) |
| Statin eligible, No. (%) | 5 (7.7) | 96 (25.3) | 75 (83.3) | 37 (46.8) | 68 (60.2) | 281 (38.7) |
| 1062 STEMI patients—estimating off‐treatment LDL‐C levels for those taking statins* | ||||||
| LDL‐C goal | <160 mg/dL | <130 mg/dL | <100 mg/dL | <100 mg/dL | <100 mg/dL | |
| No. | 69 | 454 | 111 | 127 | 301 | 1062 |
| Age, y | 58.0±14.1 | 60.7±12.6 | 67.7±10.9 | 67.0±12.9 | 66.8±12.5 | 63.7±13.0 |
| Women, No. (%) | 30 (43.5) | 132 (29.1) | 4 (3.6) | 54 (42.5) | 72 (23.9) | 292 (27.5) |
| LDL‐C, mg/dL | 107 (86, 136) | 109 (87, 133) | 126 (106, 149) | 99 (74, 121) | 104 (78, 130) | 108 (85, 134) |
| Statin eligible, % | 5 (7.3) | 124 (27.3) | 91 (82.0) | 63 (49.6) | 163 (54.2) | 446 (42.0) |
ATP III indicates Third Report of the Adult Treatment Panel; CHD, coronary heart disease.
*For patients taking statin therapy prior to ST‐segment elevation myocardial infarction (STEMI), a 30% increase in low‐density lipoprotein cholesterol (LDL‐C) was assumed. LDL‐C levels are presented as median (interquartile range).
The prevalence of statin eligibility by ACC/AHA guidelines prior to STEMI is shown in Table 3. Application of ACC/AHA guidelines to those not taking statin therapy resulted in 79.0% being statin eligible prior to STEMI. Including those taking statin therapy and estimating off‐treatment cholesterol levels (assuming a 20% increase in total cholesterol and no change in high‐density lipoprotein cholesterol) resulted in 84.0% being statin eligible.
Table 3.
Pre‐STEMI Statin Eligibility According to ACC/AHA Cholesterol Guidelines
| ACC/AHA Statin Eligibility Categories | |||||||
|---|---|---|---|---|---|---|---|
| Clinical CVD | Diabetes Mellitus | LDL‐C >190 mg/dL | CVD Risk >7.5% | All 4 Statin‐Eligible Groups | CVD Risk 5% to 7.5% | CVD Risk <5% | |
| 727 STEMI patients not taking statin therapy | |||||||
| No. | 124 | 74 | 6 | 370 | 574 (79.0%) | 69 | 84 |
| Age, y | 66.1±13.3 | 67.7±13.1 | 61.0±14.5 | 65.7±11.6 | 66.0±12.2 | 53.2±6.7 | 47.2±7.7 |
| Women, No. (%) | 29 (23.4) | 32 (43.2) | 2 (33.3) | 80 (21.6) | 143 (24.9) | 15 (21.7) | 37 (44.1) |
| LDL‐C, mg/dL | 106 (83, 134) | 96 (72, 118) | 202 (196, 206) | 112 (89, 134) | 110 (86, 133) | 111 (90, 135) | 108 (86, 128) |
| 1062 STEMI patients—estimating off‐treatment lipid levels for those taking statins* | |||||||
| N | 320 | 119 | 11 | 442 | 892 (84.0%) | 79 | 91 |
| Age, y | 67.0±12.6 | 66.8±12.9 | 57.1±13.0 | 65.9±11.6 | 66.3±12.2 | 53.5±6.6 | 47.4±7.5 |
| Women, No. (%) | 80 (25.0) | 51 (42.9) | 2 (18.2) | 101 (22.9) | 234 (26.2) | 17 (21.5) | 41 (45.1) |
| LDL‐C, mg/dL | 104 (78, 130) | 99 (75, 121) | 200 (196, 211) | 111 (90, 134) | 108 (84, 133) | 108 (88, 135) | 109 (86, 140) |
The numbers in the categories of clinical cardiovascular disease (CVD), diabetes mellitus, low‐density lipoprotein cholesterol (LDL‐C) >190 mg/dL, and 10‐year CVD risk >7.5% were considered successively from left to right. These categories are class 1 indications for statin therapy. Individuals with a 10‐year CVD risk of 5% to 7.5% can consider moderate‐intensity statin therapy. Individuals with a 10‐year CVD risk <5% are not recommended to take a statin. To estimate the off‐treatment total cholesterol used to determine CVD risk, we assumed a 20% increase in total cholesterol for individuals taking statin therapy. ACC/AHA indicates American College of Cardiology/American Heart Association. LDL‐C levels are presented as median (interquartile range).
*For patients taking statin therapy prior to ST‐segment elevation myocardial infarction (STEMI), a 30% increase in LDL‐C was assumed.
In an analysis by sex, there was no statistically significant difference in the prevalence of pre‐STEMI statin eligibility according to ATP III guidelines. Of the 727 patients not taking statin therapy prior to STEMI, 195 were women, of which 67 (34.4%) would have been eligible pre‐STEMI compared with 214 (40.2%) of the 532 men (P=0.15). In contrast, the prevalence of statin eligibility was higher in men according to the ACC/AHA guidelines, with 143 (73.3%) of the 195 women statin eligible prior to STEMI compared with 431 (81.0%) of the 532 men (P=0.02).
Sensitivity analysis assuming a range of SBPs for STEMI patients without SBP data did not significantly alter the rate of statin eligibility. Compared with 84.0% being eligible based on imputed SPB, assuming an SBP of 115 mm Hg for all patients with missing data resulted in 82.6% being statin eligible according to ACC/AHA guidelines while assuming an SBP of 150 mm Hg resulted in 88.0% being statin eligible.
Table 4 shows the characteristics of the 8.6% of patients in our sample at low 10‐year CVD risk (<5%) who were not statin eligible prior to STEMI compared with patients with a CVD risk >7.5%. Individuals presumed to be at low CVD risk who experienced STEMI were significantly younger and more likely to be female and were less likely to smoke or have previously diagnosed hypertension. Lipid levels were similar between the 2 groups.
Table 4.
Characteristics of the 91 Patients Without CVD, Diabetes Mellitus, or LDL‐C >190 mg/dL Who Were at Low CVD Risk and Therefore Not Statin Eligible Compared With the 442 Who Were Eligible for Statin Therapy According to ACC/AHA Guidelines Prior to STEMI
| Characteristic | CVD Risk <5% | CVD Risk >7.5% | P Value |
|---|---|---|---|
| Patients, No. | 91 | 442 | ··· |
| Age, y | 47.4±7.5 | 65.9±11.6 | <0.001 |
| Women, No. (%) | 41 (45.1) | 101 (22.9) | <0.001 |
| BMI, kg/m2 | 30.8±7.3 | 29.1±5.6 | 0.016 |
| Smoking, No. (%) | 0.007 | ||
| Current smoker | 23 (25.3) | 187 (42.3) | |
| Former smoker | 25 (27.5) | 107 (24.2) | |
| Never smoker | 43 (47.3) | 148 (33.5) | |
| Hypertension | 23 (25.6) | 232 (52.5) | <0.001 |
| Dyslipidemia | 23 (25.8) | 174 (39.4) | 0.016 |
| Family history of CHD, No. (%) | 36 (42.4) | 163 (42.6) | 0.97 |
| Total cholesterol, mg/dL | 174 (145, 206) | 176 (151, 200) | 0.91 |
| HDL‐C, mg/dL | 38 (33, 43) | 36 (31, 42) | 0.030 |
| Triglycerides, mg/dL | 111 (81, 145) | 117 (87, 162) | 0.33 |
| LDL‐C, mg/dL | 109 (86, 140) | 111 (90, 134) | 0.81 |
ACC/AHA indicates American College of Cardiology/American Heart Association; CHD, coronary heart disease; CVD, cardiovascular disease; HDL‐C, high‐density lipoprotein cholesterol; LDL‐C, low‐density lipoprotein cholesterol; STEMI, ST‐segment elevation myocardial infarction. Lipid values are presented as median (interquartile range).
Access to and Utilization of Outpatient Care Prior to ST‐Segment Elevation Myocardial Infarction
Of the 761 patients without known CVD, 265 (34.8%) had seen a primary care provider in the 2 years prior to their STEMI and only 24 (3.2%) had seen a cardiovascular provider. Of the 301 patients with known CVD prior to STEMI, 146 (48.5%) had seen a primary care provider and 114 (37.9%) had seen a cardiovascular provider. The median lipid levels, prevalence of utilization of health care in the 2 years prior to STEMI, and prevalence of statin eligibility according to ATP III guidelines and ACC/AHA guidelines is shown in the Figure.
Figure 1.
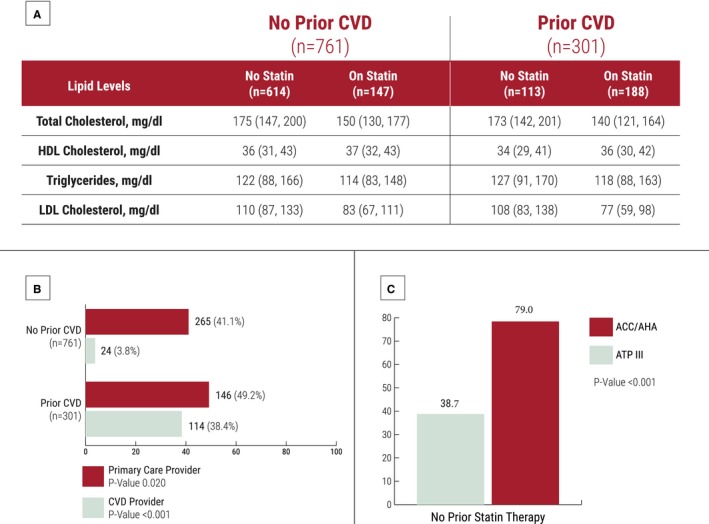
Lipid values (A), the prevalence of access to and utilization of primary and cardiovascular disease (CVD) outpatient care in the 2 years prior to ST‐segment elevation myocardial infarction (STEMI) in 1064 STEMI patients (B), and pre‐STEMI statin eligibility (C) according to the prior Third Report of the Adult Treatment Panel (ATP III) cholesterol guidelines and the current American College of Cardiology/American Heart Association (ACC/AHA) cholesterol guidelines in 727 patients not taking statin therapy prior to STEMI. HDL indicates high‐density lipoprotein; LDL, low‐density lipoprotein.
Discussion
In a large prospective cohort of STEMI patients, we found that LDL‐C levels were not significantly elevated prior to STEMI in the majority of individuals, with a median LDL‐C of 110 mg/dL in individuals not taking statin therapy without known prior CVD prior to STEMI. Compared with the ATP III guidelines, application of the ACC/AHA guidelines more than doubled statin eligibility prior to STEMI (38.7% versus 79.0%). Our results suggest that implementation of the ACC/AHA guidelines may result in a substantial increase in statin usage in individuals otherwise destined to experience STEMI. However, we also found that access to and utilization of health care, a necessity for guideline implementation, was suboptimal prior to STEMI, with less than half of those with and without prior CVD seeing a primary care provider over the 2 years prior to STEMI.
Impact of ACC/AHA Cholesterol Guidelines on Statin Eligibility
The ACC/AHA guidelines for the treatment of blood cholesterol represent a significant paradigm shift from the prior ATP III guidelines, focusing on absolute CVD risk as the main determinant of eligibility as opposed to LDL‐C levels. One of the main goals of the ACC/AHA guidelines was to allocate statin therapy to those most likely to benefit, and our data provide support for that concept. Initial research on the ACC/AHA guidelines has largely focused on its impact on statin eligibility for the general US adult population.18, 19, 20 An analysis of US National Health and Nutrition Examination Survey data evaluated statin eligibility in the estimated 115.4 million US adults aged 40 to 75 years. The study concluded that implementation of the ACC/AHA guidelines would lead to an ≈30% increase in statin eligibility in the general adult population (an additional 12.8 million US adults), largely due to an increase in eligible adults older than 60 years without CVD.18 While the ACC/AHA guidelines result in an increase in statin eligibility in the general population, our results suggest that they result in a much greater increase in eligibility in individuals most likely to benefit, as eligibility in our STEMI population increased 100% with application of the ACC/AHA guidelines.
Absolute Cardiovascular Disease Risk is a Better Predictor of Benefit From Statin Therapy Than Low‐Density Lipoprotein Cholesterol
The release of the ACC/AHA guidelines has been accompanied by some controversy, mostly related to the near‐universal eligibility of older individuals (65 to 75 years) and the accuracy of the Pooled Cohort Equations Calculator.19, 21 However, this controversy should not draw attention away from the significant limitations associated with determining statin eligibility largely based on LDL‐C levels. For individuals in our study with known CVD who were not taking statin therapy prior to STEMI, over half had LDL‐C levels <100 mg/dL. Given their known CVD, this group is clearly at elevated risk and therefore likely to benefit from statin therapy despite low LDL‐C levels. Data from randomized trials of statin therapy have been consistent in showing that the relative risk reduction with statin therapy is independent of baseline LDL‐C levels. Additionally, for STEMI patients without known CVD (>70% of our sample), LDL‐C levels were not significantly elevated, although these individuals were often at elevated absolute risk due to age and other CVD risk factors.
Guidelines Cannot be Implemented Without Access to and Utilization of Preventive Health Care
Implementation of any guideline requires a patient‐provider interaction. Our data suggest that access to and utilization of outpatient care prior to STEMI is suboptimal, with less than half of individuals without prior CVD (41.1%) and with known CVD (49.2%) seeing a primary care provider in the 2 years before their STEMI. Lack of access to health care has been shown to correlate with poorer control of CVD risk factors as well as total mortality.22, 23 Additionally, a source of usual care (a provider, clinic, or hospital that patients identify as their usual source of health care) is associated with improved control of blood pressure and cholesterol, regardless of health insurance status.24 Whether individuals in our study who did not see a primary care provider lacked health insurance or simply chose not to utilize preventive care is unclear. Regardless, in addition to efforts to increase compliance with CVD prevention guidelines, initiatives aimed at increasing access to and utilization of primary care will be needed to optimize CVD prevention in the United States.
Strengths and Limitations
Our study has strengths and limitations. Its strengths include a large prospective cohort of STEMI patients from a large regional STEMI system and detailed chart review and utilization of EHR data to provide accurate information on demographics, CVD risk factors, and lipid values. A possible concern that could be raised is that lipid values may not be accurate in the setting of STEMI. However, recent data from the Limiting Undertreatment of Lipids in Acute Coronary Syndrome with Rosuvastatin (LUNAR) trial25 demonstrated that lipid values are stable and unchanged from baseline in the first 72 to 96 hours after an acute coronary syndrome, and fasting lipid panels were drawn within 24 hours of admission for our cohort. Additionally, a recent analysis from the National Registry of Myocardial Infarction (NRMI) database evaluating the association of LDL‐C level with mortality found similar levels of LDL‐C in individuals experiencing myocardial infarction with a mean LDL‐C of 104 (38) mg/dL.26
Our data were taken from a single regional STEMI system and therefore the prevalence of CVD, diabetes mellitus, and other determinants of statin eligibility may not be generalizable to other populations. Over half of the individuals in our cohort did not have a primary care visit in the 2 years prior to STEMI and therefore we had to estimate SBP in individuals without CVD, diabetes mellitus, or an LDL‐C >190 mg/dL for use in CVD risk estimation. However, sensitivity analysis using a wide range of SBP showed minimal change in statin eligibility for the total sample. We were not able to measure compliance or adherence to preventive medications prior to STEMI and a history of statin intolerance or adverse reaction to preventive medications was not evaluated. The presence of CVD risk factors was determined from the active medical problems list from EHR data on admission as opposed to direct measurement. Finally, access to and utilization of health care prior to STEMI was only assessed for the single healthcare system. Despite a healthcare system with multiple hospitals and clinics and a unified EHR, patients may have been receiving health care from outside the system prior to STEMI. However, as movement continues towards value‐based, accountable health care, the prevalence of prior care within a given system is very relevant as future systems of care aimed at prevention of CVD are designed.
Conclusions
In a contemporary cohort of STEMI patients, we found that the 2013 ACC/AHA guidelines, compared with the prior ATP III cholesterol guidelines, substantially increase statin eligibility in individuals otherwise destined to experience STEMI. However, improvements in access to and utilization of preventive health care will be required to realize the full potential of these guidelines.
Disclosures
None.
Acknowledgments
The authors would like to thank the patients of the Level 1 MI database for providing consent to be followed for this study. Miedema and Garberich had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
(J Am Heart Assoc. 2017;6:e005333 DOI: 10.1161/JAHA.116.005333.)28404560
References
- 1. Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS. Population trends in incidence and outcomes of acute myocardial infarction. N Engl J Med. 2010;362:2155–2165. [DOI] [PubMed] [Google Scholar]
- 2. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, de Ferranti S, Després JP, Fullerton HJ, Howard VJ, Huffman MD, Isasi CR, Jiménez MC, Judd SE, Kissela BM, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Magid DJ, McGuire DK, Mohler ER III, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Rosamond W, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Woo D, Yeh RW, Turner MB. Heart disease and stroke statistics—2015 update: a report from the American Heart Association. Circulation. 2016;133:447–454. [DOI] [PubMed] [Google Scholar]
- 3. Cutler JA, Sorlie PD, Wolz M, Thom T, Fields LE, Roccella EJ. Trends in hypertension prevalence, awareness, treatment, and control rates in United States adults between 1988–1994 and 1999–2004. Hypertension. 2008;52:818–827. [DOI] [PubMed] [Google Scholar]
- 4. Mann D, Reynolds K, Smith D, Muntner P. Trends in statin use and low density lipoprotein cholesterol levels among US adults: impact of the 2001 National Cholesterol Education Program guidelines. Ann Pharmacother. 2008;42:1208–1215. [DOI] [PubMed] [Google Scholar]
- 5. Ford ES, Ajani UA, Croft JB, Critchley JA, Labarthe DR, Kottke TE, Giles WH, Capewell S. Explaining the decrease in U.S. deaths from coronary disease, 1980–2000. N Engl J Med. 2007;356:2388–2398. [DOI] [PubMed] [Google Scholar]
- 6. Carroll MD, Kit BK, Lacher DA, Shero ST, Mussolino ME. Trends in lipids and lipoproteins in US adults, 1988–2010. JAMA. 2012;308:1545–1554. [DOI] [PubMed] [Google Scholar]
- 7. Shepherd J, Cobbe SM, Ford I, Isles CG, Lorimer AR, MacFarlane PW, McKillop JH, Packard CJ. Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. N Engl J Med. 1995;333:1301–1307. [DOI] [PubMed] [Google Scholar]
- 8. Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. The Long‐Term Intervention with Pravastatin in Ischaemic Disease (LIPID) Study Group. N Engl J Med. 1998;339:1349–1357. [DOI] [PubMed] [Google Scholar]
- 9. Sever PS, Dahlof B, Poulter NR, Wedel H, Beevers G, Caulfield M, Collins R, Kjeldsen SE, Kristinsson A, McInnes GT, Mehlsen J, Nieminen M, O'Brien E, Ostergren J; ASCOT investigators . Prevention of coronary artery and stroke events with atorvastatin in hypertensive patients who have average or lower‐than‐average cholesterol concentrations, in the Anglo‐Scandinavian Cardiac Outcomes Trial‐Lipid Lowering Arm (ASCOT‐LLA): a multicenter randomized controlled trial. Lancet. 2003;361:1149–1158. [DOI] [PubMed] [Google Scholar]
- 10. Ridker PM, Danielson E, Fonseca FA, Genest J, Gotto AM Jr, Kastelein JJ, Koenig W, Libby P, Lorenzatti AJ, MacFadyen JG, Nordestgaard BG, Shepherd J, Willerson JT, Glynn RJ; JUPITER Study Group . Rosuvastatin to prevent vascular events in men and women with elevated C‐reactive protein. N Engl J Med. 2008;359:2195–2207. [DOI] [PubMed] [Google Scholar]
- 11. Gaziano TA, Young CR, Fitzmaurice G, Atwood S, Gaziano JM. Laboratory‐based versus non‐laboratory‐based method for assessment of cardiovascular disease risk: the NHANES I Follow‐up Study cohort. Lancet. 2008;371:923–931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) . Third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–3421. [PubMed] [Google Scholar]
- 13. Stone NJ, Robinson J, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, Goldberg AC, Gordon D, Levy D, Lloyd‐Jones DM, McBride P, Schwartz JS, Shero ST, Smith SC Jr, Watson K, Wilson PW, Eddleman KM, Jarrett NM, LaBresh K, Nevo L, Wnek J, Anderson JL, Halperin JL, Albert NM, Bozkurt B, Brindis RG, Curtis LH, DeMets D, Hochman JS, Kovacs RJ, Ohman EM, Pressler SJ, Sellke FW, Shen WK, Smith SC Jr, Tomaselli GF; American College of Cardiology/American Heart Association Task Force on Practice Guidelines . 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults. J Am Coll Cardiol. 2014;63:3024–3025. [DOI] [PubMed] [Google Scholar]
- 14. Miedema MD, Cohn JN, Garberich RF, Knickelbine T, Graham K, Henry TD. Underuse of cardiovascular preventive pharmacotherapy in patients presenting with ST‐elevation myocardial infarction. Am Heart J. 2012;164:259–267. [DOI] [PubMed] [Google Scholar]
- 15. Henry TD, Unger BT, Sharkey SW, Lips DL, Pedersen WR, Madison JD, Mooney MR, Flygenring BP, Larson DM. Design of a standardized system for transfer of patients with ST‐elevation myocardial infarction for percutaneous coronary intervention. Am Heart J. 2005;150:373–384. [DOI] [PubMed] [Google Scholar]
- 16. Henry TD, Sharkey SW, Burke MN, Lips DL, Pedersen WR, Madison JD, Mooney MR, Flygenring BP, Larson DM. A regional system to provide timely access to percutaneous coronary intervention for ST‐elevation myocardial infarction. Circulation. 2007;116:721–728. [DOI] [PubMed] [Google Scholar]
- 17. Miedema MD, Newell MC, Duval S, Garberich RF, Handran CB, Larson DM, Mulder S, Wang YL, Lips DL, Henry TD. Circulation. 2011;124:1636–1644. [DOI] [PubMed] [Google Scholar]
- 18. Pencina MJ, Navar‐Boggan AM, D'Agostino RB Sr, Williams K, Neely B, Sniderman AD, Peterson ED. Application of new cholesterol guidelines to a population‐based sample. N Engl J Med. 2014;370:1422–1431. [DOI] [PubMed] [Google Scholar]
- 19. Miedema MD, Lopez FL, Blaha MJ, Virani SS, Coresh J, Ballantyne CM, Folsom AR. Eligibility for statin therapy according to new cholesterol guidelines and prevalent use of medication to lower lipid levels in an older US cohort: the Atherosclerosis Risk in Communities Study Cohort. JAMA Intern Med. 2015;175:138–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Maddox TM, Borden WB, Tang F, Virani SS, Oetgen WJ, Mullen JB, Chan PS, Casale PN, Douglas PS, Masoudi FA, Farmer SA, Rumsfeld JS. Implications of the 2013 ACC/AHA cholesterol guidelines for adults in contemporary cardiovascular practice: insights from the NCDR PINNACLE registry. J Am Coll Cardiol. 2014;64:2183–2192. [DOI] [PubMed] [Google Scholar]
- 21. Ridker PM, Cook NR. Statins: new American guidelines for prevention of cardiovascular disease. Lancet. 2013;382:1762–1765. [DOI] [PubMed] [Google Scholar]
- 22. Brooks EL, Preis SR, Hwang SJ, Murabito JM, Benjamin EJ, Kelly‐Hayes M, Sorlie P, Levy D. Health insurance and cardiovascular disease risk factors. Am J Prev Med. 2010;123:741–747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wilper AP, Woolhandler S, Lasser KE, McCormick D, Bor DH, Himmelstein DU. A national study of chronic disease prevalence and access to care in uninsured US adults. Ann Intern Med. 2008;149:170–176. [DOI] [PubMed] [Google Scholar]
- 24. Spatz ES, Ross JS, Desai MM, Canavan ME, Krumholz HM. Beyond insurance coverage: usual source of care in the treatment of hypertension and hypercholesterolemia. Data from the 2003–2006 National Health and Nutrition Examination Survey. Am Heart J. 2010;160:115–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Pitt B, Loscalzo J, Ycas J, Raichlen JS. Lipid levels after acute coronary syndromes. J Am Coll Cardiol. 2008;51:1440–1445. [DOI] [PubMed] [Google Scholar]
- 26. Reddy VS, Bui QT, Jacobs JR, Begelman SM, Miller DP, French WJ; Investigators of National Registry of Myocardial Infarction (NRMI) 4b–5 . Relationship between serum low‐density lipoprotein cholesterol and in‐hospital mortality following acute myocardial infarction (the lipid paradox). Am J Cardiol. 2015;115:557–562. [DOI] [PubMed] [Google Scholar]


