Abstract
Recent studies suggest both normal and cancerous cells secret vesicles into the extracellular space. These extracellular vesicles (EVs) contain materials that mirror the genetic and proteomic content of the secreting cell. The identification of cancer-specific material in EVs isolated from the biofluids (e.g. serum, cerebrospinal fluid, urine) of cancer patients suggests EVs as an attractive platform for biomarker development. It is important to recognize that the EV derived from clinical samples are likely highly heterogeneous in make-up and arose from diverse sets of biologic processes. This article aims to review the biologic processes that give rise to various types of EVs, including exosomes, microvesicles, retrovirus like particles (RLPs), and apoptotic bodies. Clinical pertinence of these EVs to neuro-oncology will also be discussed.
Introduction
A platform that has emerged as a promising avenue for biomarker development involves the isolation of extracellular vesicles (EV) [1]. These vesicles are secreted by both normal cells and cancerous cells as means of cell-to-cell communication [2-5]. Signals are transmitted by either direct interaction between the vesicle membrane protein and the recipient membrane protein [2, 6] or by internalization of the vesicle content by the recipient cell [7-9]. Recent studies suggest that the rate of vesicle release is enhanced by oncogenic processes [10, 11] and that the contents of the vesicles released mirror aspects of the secreting cell. [1]. For instance, mRNA transcripts of a glioblastoma specific variant of the Epidermal Growth Factor Receptor (EGFR variant III) can be detected in vesicles isolated from the blood of patients harboring such tumors [1]. The encapsulation of the tumor specific mRNAs within the EVs appears to protect them from the degradative enzymes that are replete within the serum.
While these EVs constitute a promising platform for biomarker development, the terminology used to describe these vesicles has not been standardized. When EVs are isolated from biofluids such as blood, cerebrospinal fluid, or urine, one convention adopted is to name the vesicles based on the source of isolation rather than the mechanism of biogenesis. In this way, terms including epididimosomes, argosomes, exosome-like vesicles, microvesicles, promininosomes, prostasomes, dexosomes, texosomes, archaeosomes and oncosomes have all been used [12]. Other terminology reflects both varying methods of isolation and differing mechanism of biogenesis. For instance, vesicles isolated from biofluids using the same methods can be referred to as exosomes by some [9, 10], microvesicles by others [1, 13], and still others blur the difference with the term “exosomes/microvesicles” [14]. The underlying source of confusion is that “exosome” and “microvesicle” are terms defined by cell biologists to denote EVs that arise through specific biological mechanisms [15, 16]. However, when considering the use of EV as biomarkers, it is important to recognize and understand that multiple types of EV may be present in a given biofluid. The goal of this article is to review the various types of EVs that have been reported in clinical samples as well as describe the potential mechanisms of their biogenesis. The EVs reviewed here will include: exosomes, microvesicles, retrovirus like particles (RLPs), and apoptotic bodies. Potential cell surface markers for these EVs will be reviewed (Figure 1).
Fig 1.
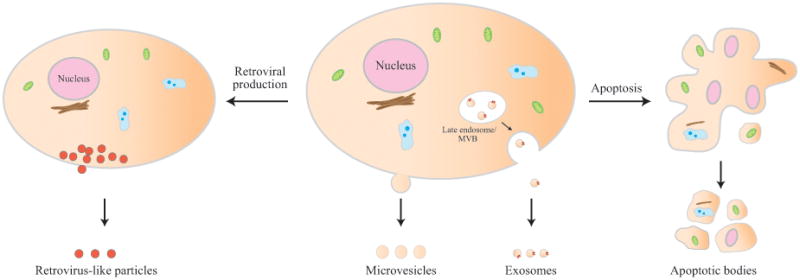
Biogenesis of the various types of extracellular vesicles: exosomes, microvesicles, retrovirus-like vesicles, and apoptotic bodies.
Isolation of Extracellular Vesicles
EVs have been isolated from a variety of biofluids including blood, urine, cerebrospinal fluid, lymphatics, tears, saliva and nasal secretions, ascites, and semen. There is no general consensus as to the best method for isolation. Described methods for isolation include step-wise centrifugation to remove large cellular debris followed by ultracentrifugation (at 100,000g) to pellet the nano-sized vesicles [2]. Purification by density gradient using sucrose gradients has also been reported [17]. Other methods of isolation include: 1) the use of serial filtration [18], and 2) immune-isolation employing magnetic beads conjugated with anti-bodies directed specifically at proteins that are overrepresented on EVs [19, 20]. In general, the isolated particles are too small to be visualized by light microscopy. The purity of the preparation is typically confirmed using electron microscopy [19] or laser scatter tracking [21]. Western blotting of proteins overrepresented in EVs are frequently performed to ensure the integrity of the particle proteins [22, 23].
Exosomes
The recognition of exosomes as an entity emerged during the golden era of electron microscopy (EM). The term exosome was coined by Dr. Rose Johnstone in a quest to understanding the biologic process that underlie the transformation from a reticulocyte to a mature erythrocyte [24].
Dr. Johnstone observed that maturing reticulocytes contained large sacs filled with small membrane enclosed vesicles of nearly uniform size (30-100 nm) within their cytoplasms. She subsequently identified transferrin as an abundant membrane protein on these sacs [25]. Immunogold labeling with a monoclonal antibody against transferrin receptor revealed that the larger sacs eventually fuse with the cell's plasma membrane, releasing the small membrane enclosed structures (Figure 2). Subsequent studies confirmed the secretion of these vesicles as the mechanism by which membranes and proteins (such as transferrin) are removed during reticulocyte maturation. Because the process of vesicular secretion was akin to “reverse endocytosis”, the small extruded vesicles were termed “exosomes”. It should be noted that, in another context, the term “exosome” is also used to denote a multi-subunit RNA degrading complex [26].
Fig 2.
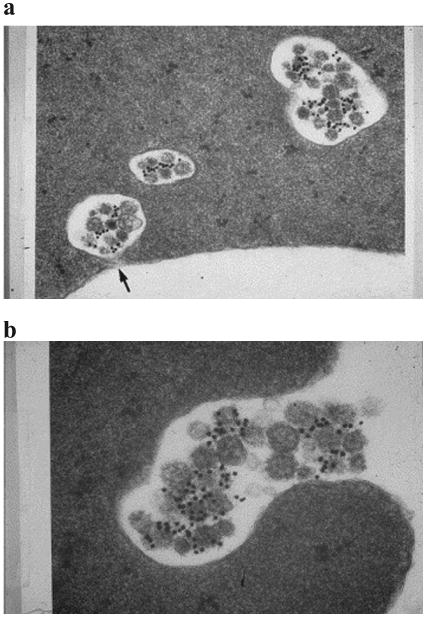
Electron micrograph of exosomes in maturing sheep reticulocytes. (a) Immunogold labeling with a monoclonal antibody against transferrin receptor. After eighteen hours of incubation, the gold label is found in the MVB but associated with the surface of the internal exosomes. The black arrow shows a sac beginning to fuse with the plasma membrane. (b) After 36 h of incubation, fusion is complete, and exosomes are released. Reprinted with permission from Blood Cells, Molecules, and Diseases [127].
Since their initial discovery, much has been learned about the biogenesis of exosomes. Exosomes are formed within the endosomal network, a membranous compartment that sorts the various intraluminal vesicles and directs them to their appropriate destinations, including lysosomes and cell surface membranes. In doing so, endosomes target some proteins/lipids for lysosomal degradation while targeting others for recycling or exocytosis.
Endosomes can be further sub-divided into three distinct compartments: early endosomes, late endosomes, and recycling endosomes (Figure 3). Early endosomes fuse with endocytic vesicles and incorporate their content into those destined for recycling, degradation, or exocytosis. The contents destined for recycling are sorted into recycling endosomes. The remainder of the early endosome then undergoes a series of transformations to become late endosomes. During this transformation, contents fated to be degraded or exported are preferentially sorted into 30-100 nm vesicles that bud into the lumen of late endosome. Given the presence of multiple small vesicles (the small vesicles are sometimes referred to as intraluminal vesicles or ILVs) in these late endosomes. They are also known as multi-vesicular bodies (MVBs) [27]. The late endosomes are targeted to either fuse with lysosomes or the plasma membrane. Fusion with a lysosome will result in destruction of the content of the late endosome. On the other hand, fusion with the plasma membrane results in the secretion of the 30-100 nm vesicles into the extra-cellular space. These excreted vesicles are exosomes.
Fig 3.
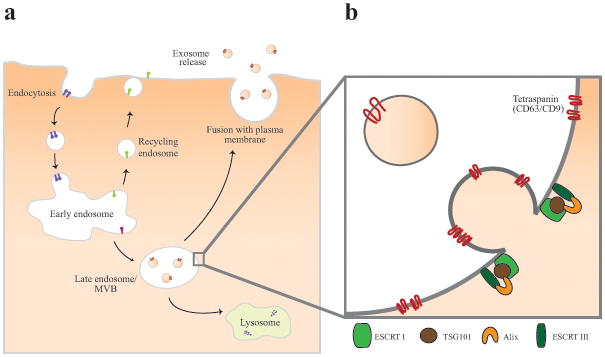
Biogenesis and release of exosomes. (a) Exosomes are formed within the endosomal network. Early endosomes fuses with endocytic vesicles and incorporate their content into those destined for recycling, degradation, or exocytosis. Late endosomes, or multi-vesicular bodies (MVBs), develop from early endosomes, and are characterized by the presence of multiple small interluminal vesicles (ILVs). Exosomes are released from late endosomal compartment through the fusion of MVBs to the plasma membrane. (b) A key step in ILV formation is the reorganization of endosomal membrane protein such as CD9 and CD63 into tetraspanin enriched microdomains. Next, a series of Endosomal Sorting Complex Required for Transport, or ESCRTs are recruited to the site of budding. ESCRTI and II drive membrane budding and ESCRT III is required for completion of budding. ESCRTIII is recruited to the site of ESCRTI and II via Alix.
Here, a brief discussion of the predominant process by which the ILVs are formed is needed since many of the involved proteins are proposed as markers that define exosomes. Work in yeast [28-31] and other tissue culture models [32-34] suggests that ILV formation requires two distinct processes. The first involves the organization of the endosome membrane into specialized units highly enriched for a class of membrane proteins called tetraspanins [35]. These specialized regions of membrane proteins are termed Tetraspanin Enriched Microdomains or TEMs. Tetraspanins are so termed because they consist of four transmembrane domains that form a stereotypical tertiary structure [36]. The sequences that connect the four transmembrane domains are variable and define specific protein-protein interactions. The TEMs are thought to cluster proteins required for ILV formation through these protein-protein interactions. Two tetraspanins that are thought to be play roles in exosome formation include CD9 and CD63. CD9 and CD63 serve as the most commonly used identifiers of exosomes and have been targeted for selective isolation [37, 38].
The second step in ILV/exosome formation involves a series of complexes called Endosomal Sorting Complex Required for Transport, or ESCRTs for short. There are four multi-protein complexes required for ILV formation and they are termed ESCRT 0, I, II, and III [39-41]. The membranes of early endosomes are marked by an abundance of phosphatidylinositol 3-phosphate (PIP3). The presence of PIP3, ubiquitinated cargos, and the curved membrane topology induces the recruitment of ESCRT-I and ESCRT-II [42]. In vitro reconstitution experiments suggest that recruitment of ESCRT-I and II drive membrane budding and that ESCRT-III is required for completion of budding. ESCRT-III is recruited to the site of ESCRT-I and II via Alix, a protein that simultaneously binds to the TSG101 component of the ESCRT-I complex and CHMP4 [43-45], a component of ESCRT-III. TSG101 and Alix are two other proteins sometimes used as exosome markers [38, 46, 47].
Available data suggest that both TSG101 and Alix, in addition to CD63 and CD9, are highly enriched in vesicle preparation thought to be related to exosomes. However, there has not been a careful assessment in terms of the specificity or sensitivity by which these biomarkers define exosomes. It is unlikely that any surface marker will single-handedly define EVs as exosomes. For example, ESCRT independent mechanisms of exosome formation have been reported in some experimental systems [48, 49]. Exosomes formed outside of the ESCRT pathway would presumably be absent Alix and TSG101. And while CD63 is thought to serve as a reliable membrane marker for exosomes, it is also prevalent in many other processes [50] including neutrophils undergoing apoptosis [51], platelets [52], vascular endothelium Weibel-palade bodies [53], and lysosome-related vesicles of leukocytes including the granules of megakaryocytes [54], T lymphocytes [55], eosinophils [56], mast cells [57], and basophils [58]. Future testing is warranted to validate existing exosomal markers for their sensitivity and specificity for exosomes and also for the discovery of new markers.
Microvesicles
The mode of biogenesis of exosomes is distinct from vesicles that arise through direct outward budding and fission of the plasma membrane (Figure 4). To distinguish these vesicles by their mode of biogenesis, the latter class of vesicles is frequently referred to as microvesicles [59]. The term “ectosomes” have also been coined to describe these vesicles [60, 61]. Microvesicles tend to be larger in size (50-2000 nm) relative to exosomes, though the size ranges overlap between these two types of vesicles. It is important to note that the mechanism of biogenesis remains the primary distinction between them.
Fig 4.
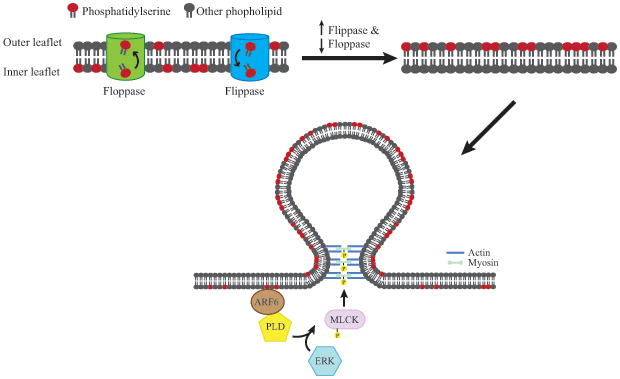
Microvesicle arises through outward budding and fission of plasma membrane and is the result of dynamic interplay between phospholipid redistribution and cytoskeletal protein contraction. Membrane budding/vesicle formation is induced by translocation of phosphatidylserine to the outer-membrane leaflet through the activity of aminophospholipid translocases. To enable microvesicle budding, ADP-ribosylation factor 6 (ARF6) initiates a signaling cascade that starts with the activation of phospholipase D (PLD), which recruits the extracellular signal-regulated kinase (ERK) to the plasma membrane. ERK phosphorylates and activates myosin light-chain kinase (MLCK). Phosphorylation and activation of the myosin light chain by MLCK triggers the release of microvesicles.
Microvesicular formation is the result of dynamic interplay between phospholipid redistribution and cytoskeletal protein contraction. The protein and phospholipid distribution within the plasma membrane is far from uniform and forms micro-domains. The asymmetric distribution is tightly regulated by aminophospholipid translocases [62-64], proteins that transfer phospholipids from one leaflet of the plasma membrane to the other. Flippases are translocases that transfer phospholipids from the outer leaflet to the inner leaflet while floppases transfer phospholipids from the inner leaflet to the outer leaflet. Membrane budding/vesicle formation is induced by translocation of phosphatidylserine to the outer-membrane leaflet [62, 65]. The budding process is completed through contraction of cytoskeletal structures by actin-myosin interactions [66, 67].
In a melanoma model, overexpression of a rho family member, GTP-binding protein ADP-ribosylation factor 6 (ARF6), results in increased microvesicle secretion. The activated form of ARF6 initiates a signaling cascade that starts with the activation of phospholipase D and terminates in the phosphorylation and activation of the myosin light chain, culminating in microvesicle release. Interestingly, this signaling cascade does not significantly alter the secretion of vesicles in the size range classically associated with exosomes (50-70 nm vesicles) [66]. These observations provide further support that the biogenesis of microvesicles and exosomes are distinct.
Like exosomes, the content of microvesicles appears highly enriched for a subset of proteins. For instance, microvesicles derived from melanoma cells are enriched for B1 integrin receptors and other membrane associated proteins, such as vesicle-associated membrane protein 3 (VAMP3) [66]. On the other hand, transferrin receptors, highly enriched in exosomes, appear notably to be missing in microvesicles [68].
Retrovirus-Like Particles (RLPs)
Retrovirus-like Particles (RLPs) are those that resemble retroviral vesicles on EM but are non-infectious because they do not contain the full complement of genes required for cellular entry or viral propagation. These vesicles are typically defined by their size (90-100 nm) and the presence of a subset of retroviral proteins [69-72].
The origins of RLPs remain an active area of investigation. There are some speculations that RLPs arise from transcription of Human Endogenous Retrovirus Sequences (or HERV). Approximately 8% of the human genome is made up of endogenous retroviral sequences. The HERVs are grouped into families annotated by letters (i.e. HERV-A, B, C…). Of these, the HERV-K family is the only one that contains open reading frames for functional retroviral proteins, gag, env, rec, and pol [73, 74]. Though the expression of the HERV-K genes is generally repressed [75-77], de-repression occurs during cellular stress, including radiation, chemical treatment, cytokine/hormone stimulation, or oncogenic transformation [78-82].
RLPs arise by directly budding from the plasma membrane [83] (Figure 5). However, the mechanism of biogenesis is thought to be distinct from the plasma membrane dynamics related to microvesicle or exosome formation. The most widely accepted mechanism for RLP formation involves interaction of retroviral proteins, such as Gag, with components of the plasma membrane [84] and cytoskeletal proteins [85]. As such, the Gag protein may serve a marker for RLPs.
Fig 5.
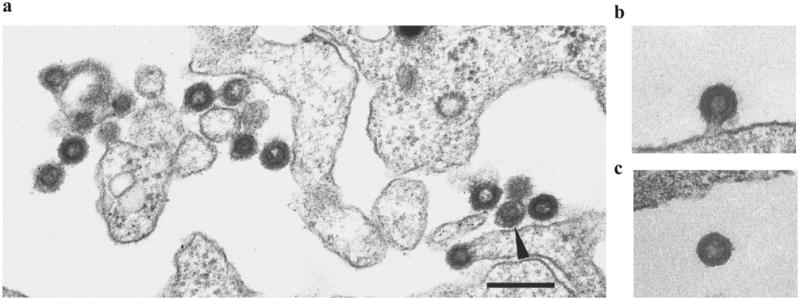
Electron micrograph of retrovirus-like particles budding from teratocarcinoma cell lines, GH (a) and Tera-1 (b, c). Scale bar = 250 nm. Reprinted with permission from Journal of General Virology [83].
RLPs have been isolated from the media of melanoma cell lines [86, 87], breast cancer cell lines [88], the serum of psoriatic patients [89], and monocytes from breast cancer patients [90]. Additionally, HERV-K sequences have been detected in EVs isolated from glioblastoma primary cell lines [13] and the plasma of lymphoma patients [91]. These results suggest that RLPs may be a constituent of the EVs isolated from patient biofluids. The size overlap between RLPs and exosomes renders it difficult to define their relative contribution to the EVs. Importantly, peptides of Gag proteins have been identified in preparations of EVs that some investigators have referred to as exosomes or microvesicles [23, 92], suggesting the presence of RLPs in these preparations.
Apoptotic Bodies
Apoptosis is a major mechanism of cell death for both normal and cancerous cells [93, 94]. A cell dying by apoptosis progresses through several stages, initiating with condensation of the nuclear chromatin, followed by membrane blebbing, progressing to disintegration of the cellular content into distinct membrane enclosed vesicles termed apoptotic bodies or apoptosomes [93]. Whereas exosomes, microvesicles, and RLPs are secreted during normal cellular processes, apoptotic bodies are formed only during programmed cell death. While apoptotic bodies are generally larger in size (500-4000 nm) [95, 96], and are characterized by the presence of organelles within the vesicles [94, 97], smaller vesicles (50-500 nm) are also released during this process [98]. It remains unclear whether these smaller vesicles resulted from membrane blebbing that occurs during apoptosis. The available data suggest that membrane blebbing is, in part, mediated, by actin-myosin interaction [99, 100] (Figure 6).
Fig 6.
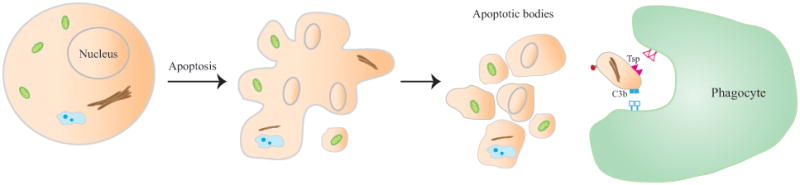
Formation of apoptotic bodies during apoptosis. A cell dying by apoptosis progress through several stages, initiating with condensation of the nuclear chromatin, followed by membrane blebbing, progressing to disintegration of the cellular content into distinct membrane enclosed vesicles termed apoptotic bodies or apoptosomes. The clearance of apoptotic bodies by macrophages via phagocytosis is mediated by specific interactions between recognition receptors on the phagocytes and the specific changes in the composition of the apoptotic cell membrane. Theses changes include the oxidation of surface molecules, which create sites for binding of Thrombospondin (Tsp) or the complement protein C3b.
During normal development, most apoptotic bodies are phagocytosed by macrophages [94, 97, 101] and are cleared locally. This clearance is mediated by specific interactions between recognition receptors on the phagocytes and the specific changes in the composition of the apoptotic cell's membrane [102-105]. Among these changes, the best characterized involves the translocation of phosphatidylserine to the outer leaflet of the lipid layer. These translocated phosphatidylserines bind to Annexin V, which is recognized by phagocytes [106]. Another well-characterized membrane alteration involves oxidation of surface molecules. These changes create sites for binding of thrombospondin [107, 108] or the complement protein C3b [102]. Thrombospondin and C3b are, in turn, recognized by phagocyte receptors [101, 109, 110]. Annexin V, thrombospondin, and C3b thus, serve as three well-accepted markers of apoptotic bodies [111].
The discovery that exosomes and microvesicles may mediate intercellular communication via the delivery of genetic materials from one cell to another served as an impetus for renewed interest in extracellular vesicles as potential cancer biomarkers [1, 112]. But the ability to transfer genetic content intercellularly does not appear to be unique to one class of extracellular vesicles. In mice bearing tumor xenografts, apoptotic bodies can also be detected in the blood of the organism [113]. Importantly, uptake of apoptosomes derived from H-rasV12- or human c-myc-transfected cells by murine fibroblast resulted in loss of contact inhibition in vitro and a tumorigenic phenotype in vivo [114]. These results suggest that genetic information can also be transferred by uptake of apoptotic bodies.
Potential Surface Markers for Defining Clinically Isolated EVs
While each of the four types of EVs presented here arose from distinct mechanisms, it should be noted that certain aspects of these mechanisms overlap. For instance, actin-myosin interactions appear critical to the formation of all four types of EVs [66, 85, 100, 115]. The available data suggest that vesicle formation occurs through mechanisms similar to those observed during cytokinesis. In this regard, it is not surprising that certain proteins involved in EV formation also participate in cytokinesis [40]. As another example, the translocation of phosphatidylserine to the outer membrane appeared a common feature during the formation of both apoptotic bodies and microvesicles [65, 106]. Such translocation may also occur during exosome formation [116]. In this context, Annexin V binding alone may not be sufficient as a distinguishing marker. Certain combinations of markers are generally used for defining exosomes, microvesicles, and apoptotic bodies (Table 1). CD63 and CD9 are potential markers of exosomes [22, 117]. Markers of microvesicles are less well established though ARF6 and VCAMP3 are recently proposed [66]. TSP and C3b are generally accepted markers of apoptotic bodies. The RLPs are less well studied though Gag protein may be a marker for this group of EVs (Table 1).
Table I. Potential surface markers for the various EVs.
| EV Type | Cell Surface Markers |
|---|---|
| Exosomes | CD63, CD9 |
| Microvesicles | ARF6, VCAMP3 |
| RLPs | Gag |
| Apoptotic bodies | TSP, C3b |
It is important to recognize that these markers are established using non-neoplastic cell lines. To what extent these processes are altered in neoplastic cells remains an open question. It is not unusual to observe processes that are clearly defined in normal development which become dysregulated or dysfunctional in cancer cells. Another caveat is that, even in the more normal cells, the cellular processes leading to the formation of the various types of vesicles remain incompletely understood. For instance, an ESCRT independent mechanism for exosome formation has been described [48, 49]. Such exosomes may be devoid of biomarkers associated with the ESCRT complex, such as CD63 or CD9. In this context, careful deliberation and judicious interpretation is required in terms of adapting the schema proposed in this article.
Clinical Applications
The ability of EVs to shelter proteins and genomic material from the harsh destructive environment of the extracellular space makes them a promising source of potential biomarkers. Their varied contents make them amenable to several fields of biomarker testing including protein typing assays, microarray assays, and DNA sequencing studies. Several of these assays have already reached the threshold of potential clinical utility. For example, mRNA profiling of serum derived EV contents can discriminate between healthy and glioblastoma bearing patients [118]. IDH-1 (isocitrate dehydrogenase 1) transcripts have been detected from EVs isolated from the blood of glioblastoma bearing patients using immunoisolations of EVs targeting CD63 [119]. Genetic mutations of mRNA such as EGFRvIII has been detected by nested PCR of EVs isolated from the serum of glioblastoma patients [1], and c-myc amplification has been effectively identified in the serum of medulloblastoma xenograft bearing mice [120]. A full discussion of these and other recent advances in EV based biomarker discovery can be found in a review by Gonda et al. [121].
Of the recent EV biomarker discovery reports, one study stood out in terms of potential for clinical translation in the immediate future. In this study, Shao et al. report the fabrication of a microfluidic chip that quantifies presence of glioblastoma specific proteins, including EGFR, EGFRvIII, podoplanin (PDPN), and IDH1 R132H proteins by a micro-nuclear magnetic resonance (μNMR) [122]. This technology allows detection of EV harboring glioblastoma-specific proteins with a sensitivity that is orders of magnitude above existing proteomic methods including, Western blotting and enzyme-linked immunosorbent assays (ELISA). Importantly, Using this μNMR device, the authors were able to differentiate EVs collected from the serum of gliobastoma patients as opposed to EV from the serum of non-tumor donors. Furthermore, changes in EV protein profiles in serial serum sampling of glioblastoma patients appeared to closely track eventual clinical response [122]. Validation of these results may yield a platform for diagnostic, prognostic, and predictive tracking.
Therapeutic strategies for EVs are also being investigated. One therapeutic strategy is to use EVs as delivery vehicles for targeted drug or gene delivery. For intance, EVs derived from dendritic cells engineered to express rabies viral glycoprotein have been successfully used to deliver siRNA across the blood brain barrier in murine models providing proof-of-principle of their delivery potential for drugs and genes [123]. Drugs targeting EV secretion has been shown to increase chemotherapeutic sensitivities of tumors [124, 125]. Strategies involving inhibition of EV production as means to disrupt chemotherapeutic escape mechanisms are also currently under testing.
Though EVs hold tremendous promise as a platform for new therapeutic strategies and biomarker development, a number of challenges persist. Serum and plasma samples contain EVs of platelet, neutrophil and macrophage origin whose release likely is influenced by age, infection, and inflammation. Relative to this population, EVs derived from tumors remain a small minority of total EVs isolated in a given biofluid sample [118]. Thus, the sensitivity of detection remains a major challenge in tumor-specific biomarker development. Current isolation methods rely largely on size and density variations of vesicles and/or markers such as CD63 [126] which may or may not be specific to a single type of EV. Understanding exactly which EVs are being isolated and targeting specific EV populations may improve our ability to achieve desired diagnostic or therapeutic goals.
Concluding Remarks
While tumor specific genetic and proteomic materials have been described in EVs derived from clinical biofluids, the biogenesis and constitution of these vesicles remain poorly understood. Current understanding of EVs suggests that the vesicles are a mixed population of exosomes, microvesicles, RLPs, and apoptotic bodies. Each of these populations likely harbor distinct vesicular contents. There remains a critical need to identify the vesicle compartment most enriched for tumor specific material of interest.
References
- 1.Skog J, et al. Glioblastoma microvesicles transport RNA and proteins that promote tumour growth and provide diagnostic biomarkers. Nat Cell Biol. 2008;10(12):1470–6. doi: 10.1038/ncb1800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Raposo G, et al. B lymphocytes secrete antigen-presenting vesicles. J Exp Med. 1996;183(3):1161–72. doi: 10.1084/jem.183.3.1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Blanchard N, et al. TCR activation of human T cells induces the production of exosomes bearing the TCR/CD3/zeta complex. J Immunol. 2002;168(7):3235–41. doi: 10.4049/jimmunol.168.7.3235. [DOI] [PubMed] [Google Scholar]
- 4.Andre F, et al. Exosomes as Potent Cell-Free Peptide-Based Vaccine. I. Dendritic Cell-Derived Exosomes Transfer Functional MHC Class I/Peptide Complexes to Dendritic Cells. The Journal of Immunology. 2004;172(4):2126–2136. doi: 10.4049/jimmunol.172.4.2126. [DOI] [PubMed] [Google Scholar]
- 5.Taylor DD, Akyol S, Gercel-Taylor C. Pregnancy-Associated Exosomes and Their Modulation of T Cell Signaling. The Journal of Immunology. 2006;176(3):1534–1542. doi: 10.4049/jimmunol.176.3.1534. [DOI] [PubMed] [Google Scholar]
- 6.Miyanishi M, et al. Identification of Tim4 as a phosphatidylserine receptor. Nature. 2007;450(7168):435–439. doi: 10.1038/nature06307. [DOI] [PubMed] [Google Scholar]
- 7.Denzer K, et al. Follicular dendritic cells carry MHC class II-expressing microvesicles at their surface. J Immunol. 2000;165(3):1259–65. doi: 10.4049/jimmunol.165.3.1259. [DOI] [PubMed] [Google Scholar]
- 8.Clayton A, et al. Adhesion and signaling by B cell-derived exosomes: the role of integrins. FASEB J. 2004;18(9):977–9. doi: 10.1096/fj.03-1094fje. [DOI] [PubMed] [Google Scholar]
- 9.Valadi H, et al. Exosome-mediated transfer of mRNAs and microRNAs is a novel mechanism of genetic exchange between cells. Nat Cell Biol. 2007;9(6):654–9. doi: 10.1038/ncb1596. [DOI] [PubMed] [Google Scholar]
- 10.Taylor DD, Gercel-Taylor C. MicroRNA signatures of tumor-derived exosomes as diagnostic biomarkers of ovarian cancer. Gynecol Oncol. 2008;110(1):13–21. doi: 10.1016/j.ygyno.2008.04.033. [DOI] [PubMed] [Google Scholar]
- 11.Rabinowits G, et al. Exosomal microRNA: a diagnostic marker for lung cancer. Clin Lung Cancer. 2009;10(1):42–6. doi: 10.3816/CLC.2009.n.006. [DOI] [PubMed] [Google Scholar]
- 12.Al-Nedawi K, Meehan B, Rak J. Microvesicles: messengers and mediators of tumor progression. Cell Cycle. 2009;8(13):2014–8. doi: 10.4161/cc.8.13.8988. [DOI] [PubMed] [Google Scholar]
- 13.Balaj L, et al. Tumour microvesicles contain retrotransposon elements and amplified oncogene sequences. Nat Commun. 2011;2:180. doi: 10.1038/ncomms1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shen B, et al. Protein targeting to exosomes/microvesicles by plasma membrane anchors. J Biol Chem. 2011;286(16):14383–95. doi: 10.1074/jbc.M110.208660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Heijnen HF, et al. Activated platelets release two types of membrane vesicles: microvesicles by surface shedding and exosomes derived from exocytosis of multivesicular bodies and alpha-granules. Blood. 1999;94(11):3791–9. [PubMed] [Google Scholar]
- 16.Denzer K, et al. Exosome: from internal vesicle of the multivesicular body to intercellular signaling device. J Cell Sci. 2000;113 Pt 19:3365–74. doi: 10.1242/jcs.113.19.3365. [DOI] [PubMed] [Google Scholar]
- 17.Thery C, et al. Isolation and characterization of exosomes from cell culture supernatants and biological fluids. Curr Protoc Cell Biol. 2006;Chapter 3(Unit 3):22. doi: 10.1002/0471143030.cb0322s30. [DOI] [PubMed] [Google Scholar]
- 18.Lamparski HG, et al. Production and characterization of clinical grade exosomes derived from dendritic cells. J Immunol Methods. 2002;270(2):211–26. doi: 10.1016/s0022-1759(02)00330-7. [DOI] [PubMed] [Google Scholar]
- 19.Clayton A, et al. Analysis of antigen presenting cell derived exosomes, based on immuno-magnetic isolation and flow cytometry. J Immunol Methods. 2001;247(1-2):163–74. doi: 10.1016/s0022-1759(00)00321-5. [DOI] [PubMed] [Google Scholar]
- 20.Koga K, et al. Purification, characterization and biological significance of tumor-derived exosomes. Anticancer Res. 2005;25(6A):3703–7. [PubMed] [Google Scholar]
- 21.Dragovic RA, et al. Sizing and phenotyping of cellular vesicles using Nanoparticle Tracking Analysis. Nanomedicine. 2011;7(6):780–8. doi: 10.1016/j.nano.2011.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Escola JM, et al. Selective enrichment of tetraspan proteins on the internal vesicles of multivesicular endosomes and on exosomes secreted by human B-lymphocytes. J Biol Chem. 1998;273(32):20121–7. doi: 10.1074/jbc.273.32.20121. [DOI] [PubMed] [Google Scholar]
- 23.Thery C, et al. Molecular characterization of dendritic cell-derived exosomes. Selective accumulation of the heat shock protein hsc73. J Cell Biol. 1999;147(3):599–610. doi: 10.1083/jcb.147.3.599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Johnstone RM, et al. Vesicle formation during reticulocyte maturation. Association of plasma membrane activities with released vesicles (exosomes) J Biol Chem. 1987;262(19):9412–20. [PubMed] [Google Scholar]
- 25.Pan BT, et al. Electron microscopic evidence for externalization of the transferrin receptor in vesicular form in sheep reticulocytes. J Cell Biol. 1985;101(3):942–8. doi: 10.1083/jcb.101.3.942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mitchell P, et al. The exosome: a conserved eukaryotic RNA processing complex containing multiple 3′-->5′ exoribonucleases. Cell. 1997;91(4):457–66. doi: 10.1016/s0092-8674(00)80432-8. [DOI] [PubMed] [Google Scholar]
- 27.Sotelo JR, Porter KR. An electron microscope study of the rat ovum. J Biophys Biochem Cytol. 1959;5(2):327–42. doi: 10.1083/jcb.5.2.327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Odorizzi G, Babst M, Emr SD. Fab1p PtdIns(3)P 5-kinase function essential for protein sorting in the multivesicular body. Cell. 1998;95(6):847–58. doi: 10.1016/s0092-8674(00)81707-9. [DOI] [PubMed] [Google Scholar]
- 29.Reggiori F, Pelham HRB. Sorting of proteins into multivesicular bodies: ubiquitin-dependent and -independent targeting. EMBO J. 2001;20(18):5176–5186. doi: 10.1093/emboj/20.18.5176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nickerson DP, et al. Regulators of Vps4 ATPase activity at endosomes differentially influence the size and rate of formation of intralumenal vesicles. Mol Biol Cell. 2010;21(6):1023–32. doi: 10.1091/mbc.E09-09-0776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Babst M. A protein's final ESCRT. Traffic. 2005;6(1):2–9. doi: 10.1111/j.1600-0854.2004.00246.x. [DOI] [PubMed] [Google Scholar]
- 32.Hurley JH, Emr SD. The ESCRT complexes: structure and mechanism of a membrane-trafficking network. Annu Rev Biophys Biomol Struct. 2006;35:277–98. doi: 10.1146/annurev.biophys.35.040405.102126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Katzmann DJ, Odorizzi G, Emr SD. Receptor downregulation and multivesicular-body sorting. Nat Rev Mol Cell Biol. 2002;3(12):893–905. doi: 10.1038/nrm973. [DOI] [PubMed] [Google Scholar]
- 34.Slagsvold T, et al. Endosomal and non-endosomal functions of ESCRT proteins. Trends Cell Biol. 2006;16(6):317–26. doi: 10.1016/j.tcb.2006.04.004. [DOI] [PubMed] [Google Scholar]
- 35.Pols MS, Klumperman J. Trafficking and function of the tetraspanin CD63. Exp Cell Res. 2009;315(9):1584–92. doi: 10.1016/j.yexcr.2008.09.020. [DOI] [PubMed] [Google Scholar]
- 36.Hemler ME. Tetraspanin functions and associated microdomains. Nat Rev Mol Cell Biol. 2005;6(10):801–11. doi: 10.1038/nrm1736. [DOI] [PubMed] [Google Scholar]
- 37.Jansen FH, et al. Exosomal secretion of cytoplasmic prostate cancer xenograft-derived proteins. Mol Cell Proteomics. 2009;8(6):1192–205. doi: 10.1074/mcp.M800443-MCP200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kosaka N, et al. Secretory mechanisms and intercellular transfer of microRNAs in living cells. J Biol Chem. 2010;285(23):17442–52. doi: 10.1074/jbc.M110.107821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wollert T, Hurley JH. Molecular mechanism of multivesicular body biogenesis by ESCRT complexes. Nature. 2010;464(7290):864–9. doi: 10.1038/nature08849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hurley JH, Hanson PI. Membrane budding and scission by the ESCRT machinery: it's all in the neck. Nat Rev Mol Cell Biol. 2010;11(8):556–566. doi: 10.1038/nrm2937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Babst M, et al. Escrt-III: an endosome-associated heterooligomeric protein complex required for mvb sorting. Dev Cell. 2002;3(2):271–82. doi: 10.1016/s1534-5807(02)00220-4. [DOI] [PubMed] [Google Scholar]
- 42.Babst M. MVB vesicle formation: ESCRT-dependent, ESCRT-independent and everything in between. Curr Opin Cell Biol. 2011;23(4):452–7. doi: 10.1016/j.ceb.2011.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.McCullough J, et al. ALIX-CHMP4 interactions in the human ESCRT pathway. Proc Natl Acad Sci U S A. 2008;105(22):7687–91. doi: 10.1073/pnas.0801567105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Katoh K, et al. The ALG-2-interacting protein Alix associates with CHMP4b, a human homologue of yeast Snf7 that is involved in multivesicular body sorting. J Biol Chem. 2003;278(40):39104–13. doi: 10.1074/jbc.M301604200. [DOI] [PubMed] [Google Scholar]
- 45.Strack B, et al. AIP1/ALIX Is a Binding Partner for HIV-1 p6 and EIAV p9 Functioning in Virus Budding. Cell. 2003;114(6):689–699. doi: 10.1016/s0092-8674(03)00653-6. [DOI] [PubMed] [Google Scholar]
- 46.Lasser C, Eldh M, Lotvall J. Isolation and characterization of RNA-containing exosomes. J Vis Exp. 2012;(59):e3037. doi: 10.3791/3037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fernandez-Llama P, et al. Tamm-Horsfall protein and urinary exosome isolation. Kidney Int. 2012;77(8):736–42. doi: 10.1038/ki.2009.550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Trajkovic K, et al. Ceramide Triggers Budding of Exosome Vesicles into Multivesicular Endosomes. Science. 2008;319(5867):1244–1247. doi: 10.1126/science.1153124. [DOI] [PubMed] [Google Scholar]
- 49.Fang Y, et al. Higher-order oligomerization targets plasma membrane proteins and HIV gag to exosomes. PLoS Biol. 2007;5(6):e158. doi: 10.1371/journal.pbio.0050158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Schroder J, et al. Deficiency of the tetraspanin CD63 associated with kidney pathology but normal lysosomal function. Molecular and cellular biology. 2009;29(4):1083–94. doi: 10.1128/MCB.01163-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Beinert T, et al. Increased expression of the tetraspanins CD53 and CD63 on apoptotic human neutrophils. Journal of leukocyte biology. 2000;67(3):369–73. doi: 10.1002/jlb.67.3.369. [DOI] [PubMed] [Google Scholar]
- 52.Nishibori M, et al. The protein CD63 is in platelet dense granules, is deficient in a patient with Hermansky-Pudlak syndrome, and appears identical to granulophysin. The Journal of clinical investigation. 1993;91(4):1775–82. doi: 10.1172/JCI116388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kobayashi T, et al. The tetraspanin CD63/lamp3 cycles between endocytic and secretory compartments in human endothelial cells. Molecular biology of the cell. 2000;11(5):1829–43. doi: 10.1091/mbc.11.5.1829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Heijnen HF, et al. Multivesicular bodies are an intermediate stage in the formation of platelet alpha-granules. Blood. 1998;91(7):2313–25. [PubMed] [Google Scholar]
- 55.Peters PJ, et al. Cytotoxic T lymphocyte granules are secretory lysosomes, containing both perforin and granzymes. The Journal of experimental medicine. 1991;173(5):1099–109. doi: 10.1084/jem.173.5.1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mahmudi-Azer S, Downey GP, Moqbel R. Translocation of the tetraspanin CD63 in association with human eosinophil mediator release. Blood. 2002;99(11):4039–47. doi: 10.1182/blood.v99.11.4039. [DOI] [PubMed] [Google Scholar]
- 57.Escribano L, et al. Human bone marrow mast cells from indolent systemic mast cell disease constitutively express increased amounts of the CD63 protein on their surface. Cytometry. 1998;34(5):223–8. doi: 10.1002/(sici)1097-0320(19981015)34:5<223::aid-cyto3>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 58.Nishikata H, et al. The rat mast cell antigen AD1 (homologue to human CD63 or melanoma antigen ME491) is expressed in other cells in culture. Journal of immunology. 1992;149(3):862–70. [PubMed] [Google Scholar]
- 59.Cocucci E, Racchetti G, Meldolesi J. Shedding microvesicles: artefacts no more. Trends Cell Biol. 2009;19(2):43–51. doi: 10.1016/j.tcb.2008.11.003. [DOI] [PubMed] [Google Scholar]
- 60.Hess C, et al. Ectosomes released by human neutrophils are specialized functional units. J Immunol. 1999;163(8):4564–73. [PubMed] [Google Scholar]
- 61.Stein JM, Luzio JP. Ectocytosis caused by sublytic autologous complement attack on human neutrophils. The sorting of endogenous plasma-membrane proteins and lipids into shed vesicles. Biochem J. 1991;274(Pt 2):381–6. doi: 10.1042/bj2740381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zwaal RF, Schroit AJ. Pathophysiologic implications of membrane phospholipid asymmetry in blood cells. Blood. 1997;89(4):1121–32. [PubMed] [Google Scholar]
- 63.Bevers EM, et al. Lipid translocation across the plasma membrane of mammalian cells. Biochim Biophys Acta. 1999;1439(3):317–30. doi: 10.1016/s1388-1981(99)00110-9. [DOI] [PubMed] [Google Scholar]
- 64.Leventis PA, Grinstein S. The distribution and function of phosphatidylserine in cellular membranes. Annu Rev Biophys. 2010;39:407–27. doi: 10.1146/annurev.biophys.093008.131234. [DOI] [PubMed] [Google Scholar]
- 65.Hugel B, et al. Membrane microparticles: two sides of the coin. Physiology (Bethesda) 2005;20:22–7. doi: 10.1152/physiol.00029.2004. [DOI] [PubMed] [Google Scholar]
- 66.Muralidharan-Chari V, et al. ARF6-regulated shedding of tumor cell-derived plasma membrane microvesicles. Curr Biol. 2009;19(22):1875–85. doi: 10.1016/j.cub.2009.09.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.McConnell RE, et al. The enterocyte microvillus is a vesicle-generating organelle. The Journal of Cell Biology. 2009;185(7):1285–1298. doi: 10.1083/jcb.200902147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Muralidharan-Chari V, et al. Microvesicles: mediators of extracellular communication during cancer progression. J Cell Sci. 2010;123(Pt 10):1603–11. doi: 10.1242/jcs.064386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bronson DL, et al. Induction of retrovirus particles in human testicular tumor (Tera-1) cell cultures: an electron microscopic study. J Natl Cancer Inst. 1979;63(2):337–9. [PubMed] [Google Scholar]
- 70.Boller K, et al. Evidence That HERV-K Is the Endogenous Retrovirus Sequence That Codes for the Human Teratocarcinoma-Derived Retrovirus HTDV. Virology. 1993;196(1):349–353. doi: 10.1006/viro.1993.1487. [DOI] [PubMed] [Google Scholar]
- 71.Mueller-Lantzsch N, et al. Human endogenous retroviral element K10 (HERV-K10) encodes a full-length gag homologous 73-kDa protein and a functional protease. AIDS Res Hum Retroviruses. 1993;9(4):343–50. doi: 10.1089/aid.1993.9.343. [DOI] [PubMed] [Google Scholar]
- 72.Dewannieux M, Blaise S, Heidmann T. Identification of a functional envelope protein from the HERV-K family of human endogenous retroviruses. J Virol. 2005;79(24):15573–7. doi: 10.1128/JVI.79.24.15573-15577.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Barbulescu M, et al. Many human endogenous retrovirus K (HERV-K) proviruses are unique to humans. Curr Biol. 1999;9(16):861–8. doi: 10.1016/s0960-9822(99)80390-x. [DOI] [PubMed] [Google Scholar]
- 74.Bock M, Stoye JP. Endogenous retroviruses and the human germline. Curr Opin Genet Dev. 2000;10(6):651–5. doi: 10.1016/s0959-437x(00)00138-6. [DOI] [PubMed] [Google Scholar]
- 75.Florl AR, et al. DNA methylation and expression of LINE-1 and HERV-K provirus sequences in urothelial and renal cell carcinomas. Br J Cancer. 1999;80(9):1312–21. doi: 10.1038/sj.bjc.6690524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Gotzinger N, et al. Regulation of human endogenous retrovirus-K Gag expression in teratocarcinoma cell lines and human tumours. J Gen Virol. 1996;77(Pt 12):2983–90. doi: 10.1099/0022-1317-77-12-2983. [DOI] [PubMed] [Google Scholar]
- 77.Yoder JA, Walsh CP, Bestor TH. Cytosine methylation and the ecology of intragenomic parasites. Trends Genet. 1997;13(8):335–40. doi: 10.1016/s0168-9525(97)01181-5. [DOI] [PubMed] [Google Scholar]
- 78.Depil S, et al. Expression of a human endogenous retrovirus, HERV-K, in the blood cells of leukemia patients. Leukemia. 2002;16(2):254–9. doi: 10.1038/sj.leu.2402355. [DOI] [PubMed] [Google Scholar]
- 79.Reiche J, Pauli G, Ellerbrok H. Differential expression of human endogenous retrovirus K transcripts in primary human melanocytes and melanoma cell lines after UV irradiation. Melanoma Res. 2010;20(5):435–40. doi: 10.1097/CMR.0b013e32833c1b5d. [DOI] [PubMed] [Google Scholar]
- 80.Golan M, et al. Human endogenous retrovirus (HERV-K) reverse transcriptase as a breast cancer prognostic marker. Neoplasia. 2008;10(6):521–33. doi: 10.1593/neo.07986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Wang-Johanning F, et al. Quantitation of HERV-K env gene expression and splicing in human breast cancer. Oncogene. 2003;22(10):1528–35. doi: 10.1038/sj.onc.1206241. [DOI] [PubMed] [Google Scholar]
- 82.Taruscio D, Mantovani A. Factors regulating endogenous retroviral sequences in human and mouse. Cytogenet Genome Res. 2004;105(2-4):351–62. doi: 10.1159/000078208. [DOI] [PubMed] [Google Scholar]
- 83.Bieda K, Hoffmann A, Boller K. Phenotypic heterogeneity of human endogenous retrovirus particles produced by teratocarcinoma cell lines. J Gen Virol. 2001;82(Pt 3):591–6. doi: 10.1099/0022-1317-82-3-591. [DOI] [PubMed] [Google Scholar]
- 84.Pincetic A, Leis J. The Mechanism of Budding of Retroviruses From Cell Membranes. Adv Virol. 2009;2009:6239691–6239699. doi: 10.1155/2009/623969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Gladnikoff M, et al. Retroviral Assembly and Budding Occur through an Actin-Driven Mechanism. Biophysical Journal. 2009;97(9):2419–2428. doi: 10.1016/j.bpj.2009.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Muster T, et al. An endogenous retrovirus derived from human melanoma cells. Cancer Res. 2003;63(24):8735–41. [PubMed] [Google Scholar]
- 87.Buscher K, et al. Expression of the human endogenous retrovirus-K transmembrane envelope, Rec and Np9 proteins in melanomas and melanoma cell lines. Melanoma Res. 2006;16(3):223–34. doi: 10.1097/01.cmr.0000215031.07941.ca. [DOI] [PubMed] [Google Scholar]
- 88.Seifarth W, et al. Retrovirus-like particles released from the human breast cancer cell line T47-D display type B- and C-related endogenous retroviral sequences. J Virol. 1995;69(10):6408–16. doi: 10.1128/jvi.69.10.6408-6416.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Lai OY, et al. Protective Effect of Human Endogenous Retrovirus K dUTPase Variants on Psoriasis Susceptibility. J Invest Dermatol. 2012 doi: 10.1038/jid.2012.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Al-Sumidaie AM, et al. Particles with properties of retroviruses in monocytes from patients with breast cancer. Lancet. 1988;1(8575-6):5–9. doi: 10.1016/s0140-6736(88)90998-1. [DOI] [PubMed] [Google Scholar]
- 91.Contreras-Galindo R, et al. Human endogenous retrovirus K (HML-2) elements in the plasma of people with lymphoma and breast cancer. Journal of virology. 2008;82(19):9329–36. doi: 10.1128/JVI.00646-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Graner MW, et al. Proteomic and immunologic analyses of brain tumor exosomes. FASEB J. 2009;23(5):1541–57. doi: 10.1096/fj.08-122184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Kerr JF, Wyllie AH, Currie AR. Apoptosis: a basic biological phenomenon with wide-ranging implications in tissue kinetics. Br J Cancer. 1972;26(4):239–57. doi: 10.1038/bjc.1972.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Elmore S. Apoptosis: a review of programmed cell death. Toxicol Pathol. 2007;35(4):495–516. doi: 10.1080/01926230701320337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Ihara T, et al. The process of ultrastructural changes from nuclei to apoptotic body. Virchows Arch. 1998;433(5):443–7. doi: 10.1007/s004280050272. [DOI] [PubMed] [Google Scholar]
- 96.Hristov M, et al. Apoptotic bodies from endothelial cells enhance the number and initiate the differentiation of human endothelial progenitor cells in vitro. Blood. 2004;104(9):2761–6. doi: 10.1182/blood-2003-10-3614. [DOI] [PubMed] [Google Scholar]
- 97.Taylor RC, Cullen SP, Martin SJ. Apoptosis: controlled demolition at the cellular level. Nat Rev Mol Cell Biol. 2008;9(3):231–241. doi: 10.1038/nrm2312. [DOI] [PubMed] [Google Scholar]
- 98.Simpson RJ, Mathivanan S. Extracellular Microvesicles: The Need for Internationally Recognised Nomenclature and Stringent Purification Criteria. J Proteomics Bioinform. 2012;5(ii-ii) [Google Scholar]
- 99.Coleman ML, et al. Membrane blebbing during apoptosis results from caspase-mediated activation of ROCK I. Nat Cell Biol. 2001;3(4):339–45. doi: 10.1038/35070009. [DOI] [PubMed] [Google Scholar]
- 100.Sebbagh M, et al. Caspase-3-mediated cleavage of ROCK I induces MLC phosphorylation and apoptotic membrane blebbing. Nat Cell Biol. 2001;3(4):346–52. doi: 10.1038/35070019. [DOI] [PubMed] [Google Scholar]
- 101.Erwig LP, Henson PM. Clearance of apoptotic cells by phagocytes. Cell Death Differ. 2008;15(2):243–50. doi: 10.1038/sj.cdd.4402184. [DOI] [PubMed] [Google Scholar]
- 102.Takizawa F, Tsuji S, Nagasawa S. Enhancement of macrophage phagocytosis upon iC3b deposition on apoptotic cells. FEBS Letters. 1996;397(2,Äì3):269–272. doi: 10.1016/s0014-5793(96)01197-0. [DOI] [PubMed] [Google Scholar]
- 103.Fadok VA, et al. Exposure of phosphatidylserine on the surface of apoptotic lymphocytes triggers specific recognition and removal by macrophages. J Immunol. 1992;148(7):2207–16. [PubMed] [Google Scholar]
- 104.Martin SJ, et al. Early redistribution of plasma membrane phosphatidylserine is a general feature of apoptosis regardless of the initiating stimulus: inhibition by overexpression of Bcl-2 and Abl. J Exp Med. 1995;182(5):1545–56. doi: 10.1084/jem.182.5.1545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Vandivier RW, et al. Role of Surfactant Proteins A, D, and C1q in the Clearance of Apoptotic Cells In Vivo and In Vitro: Calreticulin and CD91 as a Common Collectin Receptor Complex. The Journal of Immunology. 2002;169(7):3978–3986. doi: 10.4049/jimmunol.169.7.3978. [DOI] [PubMed] [Google Scholar]
- 106.Martinez MC, Freyssinet JM. Deciphering the plasma membrane hallmarks of apoptotic cells: phosphatidylserine transverse redistribution and calcium entry. BMC Cell Biol. 2001;2:20. doi: 10.1186/1471-2121-2-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Friedl P, Vischer P, Freyberg MA. The role of thrombospondin-1 in apoptosis. Cell Mol Life Sci. 2002;59(8):1347–57. doi: 10.1007/s00018-002-8512-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Savill J. Recognition and phagocytosis of cells undergoing apoptosis. Br Med Bull. 1997;53(3):491–508. doi: 10.1093/oxfordjournals.bmb.a011626. [DOI] [PubMed] [Google Scholar]
- 109.Savill J, et al. Thrombospondin cooperates with CD36 and the vitronectin receptor in macrophage recognition of neutrophils undergoing apoptosis. J Clin Invest. 1992;90(4):1513–22. doi: 10.1172/JCI116019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Mevorach D, et al. Complement-dependent clearance of apoptotic cells by human macrophages. J Exp Med. 1998;188(12):2313–20. doi: 10.1084/jem.188.12.2313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.van Engeland M, et al. Annexin V-affinity assay: a review on an apoptosis detection system based on phosphatidylserine exposure. Cytometry. 1998;31(1):1–9. doi: 10.1002/(sici)1097-0320(19980101)31:1<1::aid-cyto1>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 112.Miranda KC, et al. Nucleic acids within urinary exosomes/microvesicles are potential biomarkers for renal disease. Kidney Int. 2010;78(2):191–9. doi: 10.1038/ki.2010.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Samos J, et al. Circulating nucleic acids in plasma/serum and tumor progression: are apoptotic bodies involved? An experimental study in a rat cancer model. Ann N Y Acad Sci. 2006;1075:165–73. doi: 10.1196/annals.1368.022. [DOI] [PubMed] [Google Scholar]
- 114.Bergsmedh A, et al. Horizontal transfer of oncogenes by uptake of apoptotic bodies. Proc Natl Acad Sci U S A. 2001;98(11):6407–11. doi: 10.1073/pnas.101129998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Piper RC, Katzmann DJ. Biogenesis and function of multivesicular bodies. Annu Rev Cell Dev Biol. 2007;23:519–47. doi: 10.1146/annurev.cellbio.23.090506.123319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Thery C, Zitvogel L, Amigorena S. Exosomes: composition, biogenesis and function. Nat Rev Immunol. 2002;2(8):569–79. doi: 10.1038/nri855. [DOI] [PubMed] [Google Scholar]
- 117.Bard MP, et al. Proteomic analysis of exosomes isolated from human malignant pleural effusions. Am J Respir Cell Mol Biol. 2004;31(1):114–21. doi: 10.1165/rcmb.2003-0238OC. [DOI] [PubMed] [Google Scholar]
- 118.Noerholm M, et al. RNA expression patterns in serum microvesicles from patients with glioblastoma multiforme and controls. BMC cancer. 2012;12(1):22. doi: 10.1186/1471-2407-12-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Chen C, et al. Microfluidic isolation and transcriptome analysis of serum microvesicles. Lab Chip. 2010;10(4):505–11. doi: 10.1039/b916199f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Balaj L, et al. Tumour microvesicles contain retrotransposon elements and amplified oncogene sequences. Nature communications. 2011;2:180. doi: 10.1038/ncomms1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Gonda DD, et al. Neuro-Oncologic Applications of Exosomes, Microvesicles, and Other Nano-sized Extra-cellular Particles. Neurosurgery. 2013 doi: 10.1227/NEU.0b013e3182846e63. In press. Publish Ahead of Print: p. 10.1227/NEU.0b013e3182846e63. [DOI] [PubMed] [Google Scholar]
- 122.Shao H, et al. Protein typing of circulating microvesicles allows real-time monitoring of glioblastoma therapy. Nat Med. 2012;18(12):1835–40. doi: 10.1038/nm.2994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Alvarez-Erviti L, et al. Delivery of siRNA to the mouse brain by systemic injection of targeted exosomes. Nature biotechnology. 2011;29(4):341–5. doi: 10.1038/nbt.1807. [DOI] [PubMed] [Google Scholar]
- 124.Chalmin F, et al. Membrane-associated Hsp72 from tumor-derived exosomes mediates STAT3-dependent immunosuppressive function of mouse and human myeloid-derived suppressor cells. The Journal of clinical investigation. 2010;120(2):457–71. doi: 10.1172/JCI40483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Luciani F, et al. Effect of proton pump inhibitor pretreatment on resistance of solid tumors to cytotoxic drugs. Journal of the National Cancer Institute. 2004;96(22):1702–13. doi: 10.1093/jnci/djh305. [DOI] [PubMed] [Google Scholar]
- 126.Chen C, et al. Microfluidic isolation and transcriptome analysis of serum microvesicles. Lab on a chip. 2010;10(4):505–11. doi: 10.1039/b916199f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Johnstone RM. Revisiting the road to the discovery of exosomes. Blood Cells Mol Dis. 2005;34(3):214–9. doi: 10.1016/j.bcmd.2005.03.002. [DOI] [PubMed] [Google Scholar]


