Abstract
Sustained fluid overload (FO) is considered a major cause of hypertension, heart failure, and mortality in patients with ESRD on maintenance hemodialysis. However, there has not been a cohort study investigating the relationship between chronic exposure to FO and mortality in this population. We studied the relationship of baseline and cumulative FO exposure over 1 year with mortality in 39,566 patients with incident ESRD in a large dialysis network in 26 countries using whole-body bioimpedance spectroscopy to assess fluid status. Analyses were applied across three discrete systolic BP (syst-BP) categories (<130, 130–160, and >160 mmHg), with nonoverhydrated patients with syst-BP=130–160 mmHg as the reference category; >200,000 FO measurements were performed over follow-up. Baseline FO value predicted excess risk of mortality across syst-BP categories (<130 mmHg: hazard ratio [HR], 1.51; 95% confidence interval [95% CI], 1.38 to 1.65; 130–160 mmHg: HR, 1.25; 95% CI, 1.16 to 1.36; >160 mmHg: HR, 1.30; 95% CI, 1.19 to 1.42; all P<0.001). However, cumulative 1-year FO exposure predicted a higher death risk (P<0.001) across all syst-BP categories (<130 mmHg: HR, 1.94; 95% CI, 1.68 to 2.23; 130–160 mmHg: HR, 1.51; 95% CI, 1.35 to 1.69; >160 mmHg: HR, 1.62; 95% CI, 1.39 to 1.90). In conclusion, chronic exposure to FO in ESRD is a strong risk factor for death across discrete BP categories. Whether treatment policies that account for fluid status monitoring are preferable to policies that account solely for predialysis BP measurements remains to be tested in a clinical trial.
Keywords: Epidemiology and outcomes, blood pressure, VOLUME EXPANSION, ESRD, hemodialysis, mortality risk
Life expectancy in patients with ESRD is notoriously very limited.1 Progress in technology notwithstanding, the prognosis in ESRD has shown only modest improvement over the last decades.2 Controlling the high prevalence of fluid overload (FO) in this population is considered an unmet clinical need, and there is a quest for clinical policies specifically aimed at optimizing the control of FO to improve the dim prognosis of patients with ESRD.3 However, until now, the relationship between objectively measured FO and mortality has been investigated in just three small studies in prevalent patients,4–6 and FO in these studies was quantified only at baseline.
In the Fresenius Medical Care (FMC) dialysis network, systematic measurements of FO over time were implemented in 2009 and 2010. We have, therefore, used the extensive clinical database from this large international dialysis network to estimate the risk of death by chronic fluid volume excess in a large cohort of patients on incident hemodialysis treated in FMC centers in 26 countries in Europe, Africa, the Middle East, and Latin America. Overall, analyses in this study are on the basis of >200,000 measurements of fluid status in approximately 40,000 patients using the body composition monitor (BCM), an instrument allowing accurate and precise estimates of body fluids.
Results
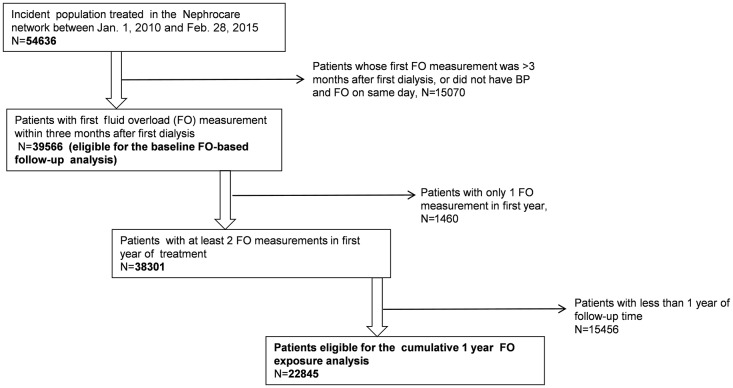
The flow diagram of patients enrolled in the study is presented in Figure 1. Of 54,636 incident patients in the European Clinical Database version 5 (EuCliD5) database (from January 1, 2010 to February 28, 2015), 39,761 had their first BCM measurement performed within 3 months of the first dialysis treatment. Of these, 195 were excluded due to lack of predialysis systolic BP measurement on the day when FO was measured. Therefore, 39,566 patients could be enrolled into this study.
Figure 1.
Flow diagram of the study cohort.
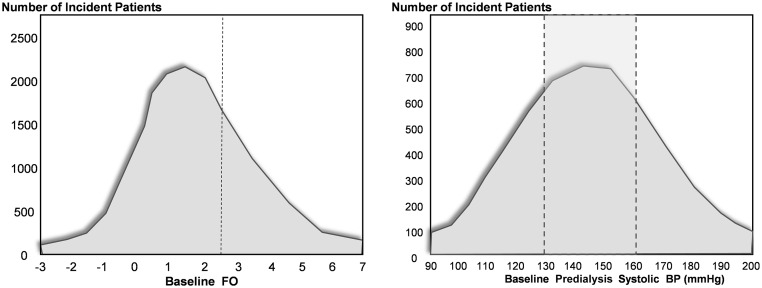
The average age of the study cohort at baseline was 60.9±15.7 years old (59.6% men). The distribution of FO at baseline in the whole population is shown in Figure 2. Predialysis baseline FO had a Gaussian distribution with an average value of 2.7 L and encompassed a wide range (from −0.1 L [10th percentile] to 6.1 L [90th percentile]). A total of 18,371 (46%) patients were overhydrated at baseline, and 21,195 (54%) were not. Figure 2 also shows the distribution of predialysis systolic BP measured on the same day as FO. In total, 20,013 (50.6%) patients had predialysis systolic BP in the range of 130–160 mmHg, 7797 (19.7%) had values >160 mmHg, and 11,756 (29.7%) had values <130 mmHg.
Figure 2.
Distribution of FO and systolic BP in the study population at baseline. The vertical lines identify (left panel) the upper limit of the normal range of FO and (right panel) the reference population for systolic BP (130–160 mmHg).
The characteristics of patients categorized on the basis of baseline FO (overhydrated versus nonoverhydrated) are presented in Table 1. Overhydrated patients had, on average, a substantially lower body mass index (−1.9 kg/m2), which coincided with lower serum albumin, LDL cholesterol, and hemoglobin, pointing to coexisting malnutrition. As expected, predialysis BP in overhydrated patients was +7.8 mmHg higher than in nonoverhydrated patients. The proportion of patients with diabetes was substantially higher in the overhydrated group, and chronic heart failure and peripheral vascular disease were also much more common in overhydrated patients. Coronary heart disease, dementia, bronchopulmonary disease, neoplasia, liver disease, and connective tissue disorders all coincided with FO (Table 1). Similar differences were found when patients were categorized on the basis of the cumulative FO exposure over 1 year (Supplemental Table 1).
Table 1.
Baseline characteristics in incident patients as categorized on the basis of the baseline FO measurement
| Variables | Overhydrated (Men: FO≥15%, Women: FO≥13%) | Nonoverhydrated (Men: FO<15%, Women: FO<13%) | P Value | All Subjects |
|---|---|---|---|---|
| Patients, N | 18,371 | 21,195 | 39,566 | |
| Follow-up, d | 474±351 | 518±362 | <0.001 | 497±358 |
| Women/men, N (%) | 7144/11,227 (38.9/61.1) | 8829/12,366 (41.7/58.3) | <0.001 | 15,973/23,593 (40.4/59.6) |
| Age, yr | 61.0±15.5 | 60.8±15.9 | 0.32 | 60.9±15.7 |
| Height, cm | 165.4±9.8 | 164.5±10.0 | <0.001 | 164.9±9.9 |
| Weight predialysis, kg | 70.6±16.4 | 74.2±16.7 | <0.001 | 72.5±16.7 |
| Preweight − postweight, kg | 1.9±1.3 | 1.4±1.6 | <0.001 | 1.6±1.5 |
| BMI predialysis, kg/m2 | 26.1±16.3 | 27.9±20.2 | <0.001 | 27.1±18.5 |
| BP predialysis, mmHg | 146±26/75±15 | 138±24/73±14 | <0.001 | 142±25/74±15 |
| Treatment time, min | 233±34 | 232±38 | 0.03 | 232±36 |
| Patients on antihypertensive drugs, % | 54.8 | 51.4 | <0.001 | 53.0 |
| Patients with catheter, N (%) | 10,930 (59.5) | 10,168 (48.0) | <0.001 | 21,098 (53.3) |
| Patient smoking, N (%) | 3881 (21.1) | 4305 (20.3) | 0.05 | 8186 (20.7) |
| Ethnicity: white, N (%) | 15,103 (82.2) | 18,253 (86.1) | <0.001 | 33,356 (84.3) |
| Comorbidities | ||||
| Diabetes, % | 31.6 | 20.9 | <0.001 | 25.9 |
| Coronary artery disease, N (%) | 1258 (6.8) | 1183 (5.6) | <0.001 | 2441 (6.2) |
| Congestive heart failure, N (%) | 3555 (19.4) | 3051 (14.4) | <0.001 | 6606 (16.7) |
| Cerebrovascular disease (stroke), N (%) | 1987 (10.8) | 2246 (10.6) | 0.48 | 4233 (10.7) |
| Peripheral vascular disease, N (%) | 2232 (12.1) | 2096 (9.9) | <0.001 | 4328 (10.9) |
| Dementia, N (%) | 157 (0.9) | 130 (0.6) | <0.01 | 287 (0.7) |
| Chronic bronchopulmonary disease, N (%) | 1304 (7.1) | 1338 (6.3) | 0.002 | 2642 (6.7) |
| Paraplegia, N (%) | 51 (0.3) | 56 (0.3) | 0.80 | 107 (0.3) |
| Liver disease, N (%) | 1393 (7.6) | 1384 (6.5) | <0.001 | 2777 (7.0) |
| Connective tissue disorder, N (%) | 301 (1.6) | 263 (1.2) | <0.001 | 564 (1.4) |
| Biochemical measurements | ||||
| Hb, g/dl | 9.5±1.7 | 10.3±1.7 | <0.001 | 9.9±1.7 |
| Albumin, g/dl | 3.5±0.6 | 3.8±0.5 | <0.001 | 3.7±0.5 |
| Na, mmol/L | 137.8±4.6 | 137.7±4.2 | 0.65 | 137.8±4.4 |
| Phosphate, mg/dl | 4.6±1.7 | 4.8±1.7 | <0.001 | 4.7±1.7 |
| LDL cholesterol, mg/dl | 97.8±55.1 | 100.9±155.7 | 0.02 | 99.5±120.0 |
| HDL cholesterol, mg/dl | 42.8±16.7 | 40.8±15.4 | <0.001 | 41.7±16.1 |
| CRP, mg/L | 20.2±38.8 | 15.8±31.1 | <0.001 | 17.8±34.9 |
| Kt/V | 1.38±1.94 | 1.37±1.93 | 0.80 | 1.37±1.93 |
| PCRn, g/kg per d | 0.9±0.8 | 1.0±0.6 | <0.001 | 1.0±0.7 |
| FO predialysis, L | 4.8±2.8 | 0.9±1.5 | <0.001 | 2.7±2.9 |
BMI, body mass index; Hb, hemoglobin; Na, sodium; CRP, C-reactive protein; PCRn, normalized protein catabolic rate.
Survival Analyses on the Basis of Baseline FO
Of the 39,566 patients eligible for baseline analysis, 5866 (14.8%) patients died during the 497±358 days of follow-up: 3290 (17.9%) in the overhydrated group and 2576 (12.1%) in the nonoverhydrated group. In unadjusted analyses, overhydrated patients had a 62% excess risk for mortality (hazard ratio [HR], 1.62; 95% confidence interval [95% CI], 1.54 to 1.70) compared with nonoverhydrated patients. The excess risk was maintained (HR, 1.26; 95% CI, 1.19 to 1.33) in analyses adjusting for demographic and anthropometric variables (the full list of variables is in Table 1), and excluding BP from the model did not materially change the HR for death of FO.
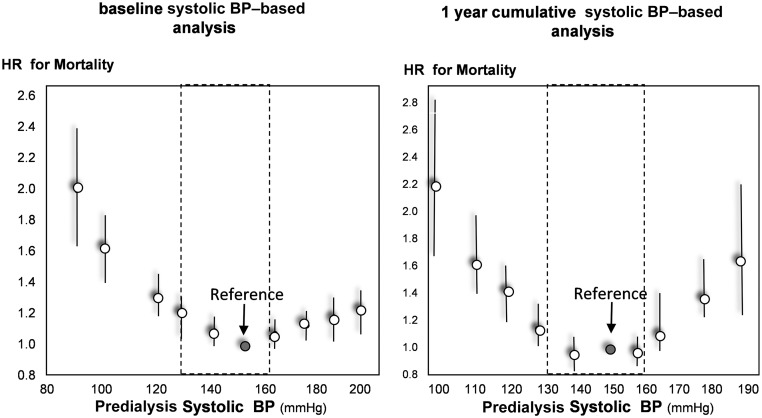
The relationship between baseline predialysis systolic BP and mortality is shown in Figure 3, left panel. The relationship was J shaped, and the risk of death was minimal in patients with predialysis BP in the range of 130–160 mmHg. Compared with normal predialysis BP (130–160 mmHg), patients with low (<130 mmHg) and high (>160 mmHg) predialysis BP exhibited a higher risk for all-cause death in both unadjusted (low BP: HR, 1.28; 95% CI, 1.21 to 1.36; high BP: HR, 1.07; 95% CI, 1.00 to 1.14) and fully adjusted analyses (low BP: HR, 1.14; 95% CI, 1.08 to 1.21; high BP: HR, 1.06; 95% CI, 0.99 to 1.13).
Figure 3.
Relationship between (left panel) baseline and (right panel) 1-year cumulative systolic BP and mortality. Data are adjusted for the full list of variables in Table 1.
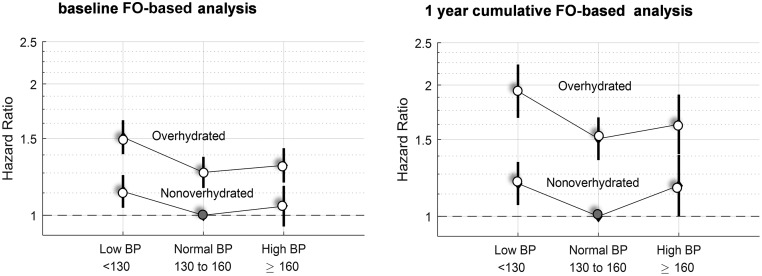
In Figure 4, left panel, the fully adjusted risk (Table 2) for adverse clinical outcomes is presented in patients stratified according to fluid status (i.e., being fluid overloaded or not) and predialysis systolic BP. FO in patients with high systolic BP (>160 mmHg; HR, 1.30; 95% CI, 1.19 to 1.42) or low BP (<130 mmHg; HR, 1.51; 95% CI, 1.38 to 1.65) associated with the highest risk of death, whereas the mortality risk was intermediate in overhydrated patients with normal BP (130–160 mmHg; HR, 1.25; 95% CI, 1.16 to 1.36). The death risk was substantially lower in nonoverhydrated patients. Indeed, such risk was just 13% higher than that in the reference category (BP=130–160 mmHg) in patients with low BP (HR, 1.13; 95% CI, 1.04 to 1.24) and 5% higher than the reference risk in those with high BP (HR, 1.05; 95% CI, 0.94 to 1.17). The independent relationship between FO and mortality was similar across sex; age strata; body mass index; diabetes; and other comorbidities, including coronary heart disease, heart failure, stroke, peripheral vascular disease, and antihypertensive treatment; and in those on hemodialysis and hemodiafiltration. Furthermore, no effect modification by country was registered for the same relationship.
Figure 4.
(Left panel) Baseline and (right panel) 1-year cumulative FO and mortality in patients stratified by predialysis systolic BP. Data are adjusted for the full list of variables in Table 1. Data are HR and 95% CIs. Fluid-overloaded patients had a significantly higher risk of death compared with nonoverloaded patients across all BP strata (all P<0.001).
Table 2.
Multivariate Cox regression model of the risk of death associated with FO measured at baseline across systolic BP categories
| Variables | HR (95% CI) |
|---|---|
| BP<130 FO normal | 1.13 (1.04 to 1.24) |
| BP<130 FO high | 1.51 (1.38 to 1.65) |
| BP=130–160, FO normal | 1.00 (Reference) |
| BP=130–160, FO high | 1.25 (1.16 to 1.36) |
| BP>160, FO normal | 1.05 (0.94 to 1.17) |
| BP>160, FO high | 1.30 (1.19 to 1.42) |
| Sex (1= man) | 0.99 (0.93 to 1.06) |
| Age, per yr | 1.04 (1.03 to 1.04) |
| Height, per cm | 1.00 (1.00 to 1.01) |
| Weight predialysis, per kg | 0.99 (0.99 to 0.99) |
| Preweight − postweight, per kg | 1.04 (1.03 to 1.05) |
| BMI, per kg/m2 | 1.00 (1.00 to 1.00) |
| Treatment time, per min | 1.00 (1.00 to 1.00) |
| Smoking (1= yes) | 1.00 (0.94 to 1.07) |
| Ethnicity (1= white) | 0.75 (0.70 to 0.81) |
| Diabetes | 1.01 (0.95 to 1.07) |
| Coronary artery disease | 1.75 (1.62 to 1.88) |
| Congestive heart failure | 1.70 (1.61 to 1.81) |
| Peripheral vascular disease | 0.86 (0.80 to 0.92) |
| Dementia | 1.28 (1.07 to 1.54) |
| Chronic bronchopulmonary disease | 1.03 (0.94 to 1.12) |
| Paraplegia | 1.03 (0.69 to 1.52) |
| Liver disease | 0.99 (0.90 to 1.10) |
| Connective tissue disorder | 1.23 (0.99 to 1.53) |
| Cerebrovascular disease | 1.13 (1.05 to 1.23) |
| Hb, per g/L | 1.00 (1.00 to 1.00) |
| Albumin, per g/L | 0.94 (0.94 to 0.95) |
| Na, per mmol/L | 0.99 (0.98 to 0.99) |
| Phosphate, per mg/dl | 1.00 (0.99 to 1.02) |
| LDL, per mg/dl | 1.00 (1.00 to 1.00) |
| HDL, per mg/dl | 0.99 (0.99 to 1.00) |
| CRP, per mg/L | 1.03 (1.02 to 1.03) |
| PCRn, per g/kg per day | 0.99 (0.97 to 1.00) |
| Kt/V | 1.00 (1.00 to 1.00) |
| Use of AHT medication (1= yes) | 0.94 (0.89 to 0.99) |
Patients were classified as overhydrated or nonoverhydrated after dividing the cumulative FO by the days of exposure. Such calculation takes back the cumulative estimate to the original scale (single measurement). All comorbidities: 1= yes. BMI, body mass index; Hb, hemoglobin; Na, sodium; CRP, C-reactive protein; PCRn, normalized protein catabolic rate; AHT, antihypertensive treatment.
Survival Analyses on the Basis of Cumulative FO Exposure over 1 Year
The duration of follow-up in the 22,845 patients in whom we analyzed the effect of 1-year cumulative exposure to FO on survival after the first year of dialysis treatment was 385±291 days. The average numbers of FO measurements in overhydrated and nonoverhydrated patients during the first year were 10.0±5.5 and 9.8±4.6, respectively. Overall, 2589 (11.3%) patients died during follow-up, 1121 (16.6%) patients died in the overhydrated group, and 1468 (9.1%) patients died in the nonoverhydrated group. As presented in detail in Figure 4, right panel and Table 3 (detailed description of the full model), the independent risk attributable to chronic FO in patients with BP<130 or >160 mmHg was comparable in magnitude or higher than that of coronary artery disease (HR, 1.63; 95% CI, 1.46 to 1.82), congestive heart failure (HR, 1.65; 95% CI, 1.52 to 1.81), or an increase in age of ≥12 years (HR, 1.48; 95% CI, 1.39 to 1.56), and excluding BP from the multivariate model did not materially change the HR associated with FO (HR, 1.50; 95% CI, 1.38 to 1.64).
Table 3.
Multivariate Cox regression model of the risk of death associated with cumulative (1 year) exposure to FO across systolic BP categories
| Variables | HR (95% CI) |
|---|---|
| BP<130 FO normal | 1.19 (1.06 to 1.33) |
| BP<130 FO high | 1.94 (1.68 to 2.23) |
| BP=130–160, FO normal | 1.00 (Reference) |
| BP=130–160, FO high | 1.51 (1.35 to 1.69) |
| BP>160, FO normal | 1.18 (1.00 to 1.38) |
| BP>160, FO high | 1.62 (1.39 to 1.90) |
| Sex (1= man) | 1.09 (0.98 to 1.21) |
| Age, per yr | 1.03 (1.03 to 1.04) |
| Height, per cm | 1.00 (0.99 to 1.00) |
| Weight predialysis, per kg | 0.99 (0.99 to 1.00) |
| Preweight − postweight, per kg | 1.05 (0.98 to 1.12) |
| BMI, per kg/m2 | 1.00 (0.99 to 1.01) |
| Treatment time, per min | 1.00 (1.00 to 1.00) |
| Smoking (1= yes) | 1.09 (0.99 to 1.20) |
| Ethnicity (1= white) | 0.82 (0.72 to 0.94) |
| Diabetes | 1.13 (1.03 to 1.23) |
| Coronary artery disease | 1.63 (1.46 to 1.82) |
| Congestive heart failure | 1.66 (1.52 to 1.81) |
| Peripheral vascular disease | 0.99 (0.90 to 1.09) |
| Dementia | 1.26 (0.96 to 1.65) |
| Chronic bronchopulmonary disease | 1.16 (1.03 to 1.31) |
| Paraplegia | 0.83 (0.46 to 1.50) |
| Liver disease | 1.01 (0.88 to 1.16) |
| Connective tissue disorder | 1.16 (0.82 to 1.63) |
| Cerebrovascular disease | 1.11 (0.98 to 1.25) |
| Hb, per g/L | 0.98 (0.98 to 0.99) |
| Albumin, per g/L | 0.93 (0.92 to 0.94) |
| Na, per mmol/L | 0.97 (0.95 to 0.98) |
| Phosphate, per mg/dl | 1.03 (0.99 to 1.07) |
| LDL, per mg/dl | 1.00 (1.00 to 1.00) |
| HDL, per mg/dl | 1.00 (1.00 to 1.00) |
| CRP, per mg/L | 1.04 (1.03 to 1.06) |
| PCRn, per g/kg per d | 0.81 (0.73 to 0.89) |
| Kt/V | 0.97 (0.96 to 0.98) |
| Use of AHT medication (1= yes) | 1.13 (1.03 to 1.23) |
In this analysis, systolic BP, predialysis weight, and postdialysis weight (and the difference between predialysis weight and postdialysis weight) of the days on which fluid volume (BMC) was measured were averaged and taken as study variables for the multivariate Cox regression. All comorbidities: 1= yes. BMI, body mass index; Hb, hemoglobin; Na, sodium; CRP, C-reactive protein; PCRn, normalized protein catabolic rate; AHT, antihypertensive treatment.
In this subcohort of patients who survived at least 1 year, the relationship between systolic BP and mortality was U shaped, and the risk of death was minimal in the 130- to 160-mmHg category (Figure 3). Of note, the fully adjusted risk associated with cumulative exposure to FO was substantially higher than that estimated for baseline FO across all BP strata (Figure 4). Fluid-overloaded patients with either high BP (>160 mmHg; HR, 1.62; 95% CI, 1.39 to 1.90) or low BP (<130 mmHg; HR, 1.94; 95% CI, 1.68 to 2.23) exhibited the highest risk of death, whereas the mortality risk was intermediate in overhydrated patients with normal BP (130–160 mmHg; HR, 1.51; 95% CI, 1.35 to 1.69); such as in the analysis on the basis of the baseline FO, the death risk was substantially lower in nonoverhydrated patients. Indeed, the risk was just 19% higher than that in the reference category (BP=130–160 mmHg) in patients with low BP (HR, 1.19; 95% CI, 1.06 to 1.33) and 18% higher in patients with high BP (HR, 1.18; 95% CI, 1.00 to 1.38). No effect modification by type of treatment (hemodialysis versus hemodiafiltration) or country was registered (P>0.20).
In a sensitivity analysis with face to face comparison of the fully adjusted HR of 1-year cumulative exposure to FO (in the 22,845 patients who survived at least 1 year) with the HR of the baseline FO in the same patients, the risk of cumulative FO exposure (see above) was again more pronounced than the corresponding risk estimated by the baseline FO measurement across all systolic BP categories (<130 mmHg: HR, 1.32; 95% CI, 1.15 to 1.51 versus 130–160 mmHg: HR, 1.13; 95% CI, 1.00 to 1.27 and >160 mmHg: HR, 1.21; 95% CI, 1.06 to 1.38; all P<0.001).
Discussion
Chronic exposure to FO as quantified by repeated measurements of body fluids by bioimpedance spectroscopy substantially increased the risk of death across discrete BP categories in a large cohort of patients on incident hemodialysis. The magnitude of death risk attributable to chronic FO was comparable with that of coronary artery disease or congestive heart failure per se or an increase in age of ≥12 years.
Only three studies have tested the relationship between directly measured FO and the risk of death in the ESRD population.4–6 In these studies—all on the basis of prevalent patients and collectively including just 667 patients—FO was measured only at baseline. We tested the relationship between exposure to FO and mortality by two approaches. By the first approach, we estimated the risk of death associated with baseline FO in incident patients, which is a survival bias–free approach. By the second approach, we investigated the relationship between cumulative exposure to FO over 1 year and death beyond the first year, an approach surmising that, like for traditional risk factors,7–10 the effects of FO are cumulative in nature. In both analyses, the link between FO and mortality was robust and resisted adjustment for a large series of potential confounders, including heart failure and major comorbidities. The risk of death portended by cumulative FO was higher than the risk estimated solely on the basis of the baseline FO measurement, suggesting that, in patients on incident hemodialysis, persistent FO is a much stronger risk predictor than FO as measured at only one time point. The initial (baseline) FO measurement in patients with incident ESRD may be an imprecise marker of the chronic fluid status in this population, because detection of a high FO value may prompt the prescription of an intensification of ultrafiltration to correct overhydration, an intervention that eventually dissociates the baseline FO assessment from the actual chronic exposure to FO. The risk of FO was almost equally strong in hypertensive and hypotensive patients, and such risk also remained substantial in normotensive patients as defined by predialysis BP, which is the BP metric most commonly applied to guide the ultrafiltration regimen and antihypertensive therapy in the dialysis population. This was true across the 26 countries and the types of extracorporeal treatment (hemodialysis and hemofiltration), suggesting that our findings are generalizable to a vast population of patients. The risk of death dictated by systolic BP categories per se was modest and of the same order of that registered in the Dialysis Outcomes and Practice Patterns Study,11 ranging from 6% in patients with low BP to 26% in those with high BP. Predialysis systolic BP is a measurement performed at peak FO, and therefore, it is a proxy of left ventricular function rather than a metric of long-term BP burden.12 In patients in the Chronic Renal Insufficiency Cohort who progressed to ESRD, the relationship of predialysis BP with mortality was U shaped. However, standardized BP measurements outside the hemodialysis environment were linearly related with mortality in the same patients.13 Therefore, more reliable metrics of the actual BP burden, such as 24-hour ambulatory blood pressure monitoring,14 standardized BP,13 or home BP,14 may show stronger links between BP and mortality than predialysis BP. Notwithstanding this limitation, this BP metric remains the method whereupon most renal physicians base their decisions about BP treatment, including decisions about the ultrafiltration regimen. Recently, a comprehensive survey including 172 centers serving 62% of the hemodialysis population in Great Britain3 showed that 78% of the centers have no concurring policy for managing fluid balance. Most centers relied on clinical assessment, including predialysis BP, and only 27% of the centers applied bioimpedance to measure body fluids. Given the strong association between chronic FO and mortality, which far exceeds that of low and high predialysis BP, our study suggests that treatment policies guided by fluid status monitoring might be preferable to policies guided solely by predialysis BP measurement. Pilot studies on the basis of surrogates, such as left ventricular mass index and/or pulse wave velocity,15,16 support the contention that systematic body fluids measurements may produce favorable effects.
Our study has limitations. The first limitation is the purely observational nature of our observations. Although we adjusted for a large series of potential confounders, residual confounding by imprecisely measured concomitant risk factors and/or other risk factors that we did not measure might have altered the precision of the estimate of the mortality risk of FO. Also, the study of the cumulative exposure to FO over 1 year is open to survival bias. However, although restricted to the ESRD population with survival of at least 1 year, which is about 80%–85% of the hemodialysis population in European countries1 and the United States,2 these data clearly indicate that sustained FO is an independent risk factor of the same magnitude as heart failure per se or an increase in age of ≥12 years. The incident nature of our cohort and the very large sample size including diverse populations across 26 countries are important strengths.
In conclusion, chronic exposure to FO (as quantified by >200,000 measurements of body fluids by bioimpedance spectroscopy in about 35,000 patients on incident hemodialysis) is a strong risk factor for death across discrete BP categories. These findings support a strong call for a randomized trial on the basis of clinical end points comparing a clinical policy on the basis of FO measurements by BCM with the standard clinical policy guided by BP, symptoms, and clinical signs, which is the standard currently adopted by the majority of centers worldwide.
Concise Methods
All patients included in the cohort of this study were treated in the NephroCare–FMC dialysis center network operating in 26 countries in Europe, the Middle East, Africa, and Latin America. Data were retrieved from the central EuCliD5 database, which integrates patient characteristics as well as day by day treatment data, laboratory parameters, and medications. This study was approved by the institutional review committee of NephroCare–FMC.
Clinical and Demographic Measures and Comorbid States
The first (baseline) data for each patient were those coinciding with the first available BCM measurement, which had to be within the first 3 months of dialysis treatment. Demographic and clinical variables considered in this study are listed in Table 1.
BCM Index of FO
Body composition and fluid status were assessed by whole-body bioimpedance spectroscopy (BCM; FMC) as described by Moissl et al.17 and Machek et al.18 BCM determines FO in absolute liters independent of body composition by use of a physiologic model on the basis of normal tissue hydration.19 BCM was validated against gold standard references (bromide and deuterium dilution in a wide range of healthy subjects and patients ranging in age from 2 to 95 years old).20 FO is estimated in proportional terms relative to extracellular water (FO percentage). Patients are considered to be overhydrated when their relative FO (=FO/extracellular volume) is ≥15% in men and ≥13% in women, which coincides with an absolute FO of about 2.5 L.4
Statistical Analyses
We performed two analyses. First, a standard Cox regression analysis was performed to predict all-cause mortality on the basis of baseline FO and other variables over the 497±358 days of follow-up. Second, an analysis was performed on the basis of the cumulative exposure to FO over the first year of dialysis treatment to predict mortality after the first year. This analysis surmises that the effects of volume overload are cumulative and takes full advantage of estimates on the basis of repeated measurements of the exposure variable.21 The rationale of this method is that estimates of the long-term exposure to risk factors, including hyperlipidemia,7,22 hypertension,8,23 hyperglycemia,24 and other risk factors,9 provide better estimates of the health hazards of the same risk factors measured at just one time point.9 Cumulative exposure to FO was calculated by the area under the curve of FO measurements over 1 year.21 Both survival analyses were adjusted for the full list of variables reported in Table 1. Missing values other than the BCM, the fundamental variable guiding patient selection for which no missing values could exist, were imputed by the median of existing values. The list of missing values in variables other than FO is presented in detail in Supplemental Table 2.
Groups were compared by Wilcoxon rank sum tests in the case of non-normal distributions, t tests were used for continuous variables, and chi-squared tests were used for categorical variables. A P value of <0.05 was considered to indicate significant difference between groups.
Disclosures
C.Z., F.M., and G.T. declare no conflict of interest with the content of this manuscript. The remaining authors are all employees of Fresenius Medical Care.
Supplementary Material
Acknowledgments
The National Medical Directors of the NephroCare–Fresenius Medical Care oversaw data collection and were responsible for checking data quality at the country level. These contributors are Goran Imamovic (Bosnia and Herzegovina), Zarko Belavic (Croatia), Daniela Voiculescu (Romania), Konstantin Gurevich (Russia), Reina Dovc-Dimec (Slovenia), Zoran Paunic (Serbia), Charles Swanepoel (South Africa), Fatih Kircelli (Turkey), Nick Richards (United Arab Emirates), Tomas Jirka, Michaela Sagova (Czech Republic), Martin Lepiksoo (Estonia), Erzsebet Ladanyi (Hungary), Miroslaw Kroczak (Poland), Jaroslav Rosenberger (Slovakia), Dariusz Zarczynski (Sweden), Charles Chazot (France), Alex Heaton (Ireland), Attilio Di Benedetto (Italy), Pedro Ponce (Portugal), Jose Ignacio Merello and Rosa Ramos (Spain), Alex Heaton (United Kingdom), Cristina Marelli (Argentina), Eufronio Dalmeida (Brasil), Eduardo Machuca (Chile), Victor Delgado (Colombia), Leonor Briones (Ecuador).
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
See related editorial, “Turning the Tide: Improving Fluid Management in Dialysis through Technology,” on pages 2260–2262.
This article contains supplemental material online at http://jasn.asnjournals.org/lookup/suppl/doi:10.1681/ASN.2016121341/-/DCSupplemental.
References
- 1.USRDS : 2015 USRDS Annual Data Report Volume 2: ESRD in the United States. Bethesda, MD, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2015
- 2.Pippias M, Jager KJ, Kramer A, Leivestad T, Sánchez MB, Caskey FJ, Collart F, Couchoud C, Dekker FW, Finne P, Fouque D, Heaf JG, Hemmelder MH, Kramar R, De Meester J, Noordzij M, Palsson R, Pascual J, Zurriaga O, Wanner C, Stel VS: The changing trends and outcomes in renal replacement therapy: Data from the ERA-EDTA registry. Nephrol Dial Transplant 31: 831–841, 2016 [DOI] [PubMed] [Google Scholar]
- 3.Dasgupta I, Farrington K, Davies SJ, Davenport A, Mitra S: UK national survey of practice patterns of fluid volume management in haemodialysis patients: A need for evidence. Blood Purif 41: 324–331, 2016 [DOI] [PubMed] [Google Scholar]
- 4.Wizemann V, Wabel P, Chamney P, Zaluska W, Moissl U, Rode C, Malecka-Masalska T, Marcelli D: The mortality risk of overhydration in haemodialysis patients. Nephrol Dial Transplant 24: 1574–1579, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chazot C, Wabel P, Chamney P, Moissl U, Wieskotten S, Wizemann V: Importance of normohydration for the long-term survival of haemodialysis patients. Nephrol Dial Transplant 27: 2404–2410, 2012 [DOI] [PubMed] [Google Scholar]
- 6.Kim YJ, Jeon HJ, Kim YH, Jeon J, Ham YR, Chung S, Choi DE, Na KR, Lee KW: Overhydration measured by bioimpedance analysis and the survival of patients on maintenance hemodialysis: A single-center study. Kidney Res Clin Pract 34: 212–218, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Navar-Boggan AM, Peterson ED, D’Agostino RB Sr., Neely B, Sniderman AD, Pencina MJ: Hyperlipidemia in early adulthood increases long-term risk of coronary heart disease. Circulation 131: 451–458, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kishi S, Teixido-Tura G, Ning H, Venkatesh BA, Wu C, Almeida A, Choi E-Y, Gjesdal O, Jacobs DR Jr., Schreiner PJ, Gidding SS, Liu K, Lima JAC: Cumulative blood pressure in early adulthood and cardiac dysfunction in middle age: The CARDIA study. J Am Coll Cardiol 65: 2679–2687, 2015 [DOI] [PubMed] [Google Scholar]
- 9.Liu X, Cui L, Wang A, Wang X, Song Q, Li S, Shi J, Zhao X, Chen S, Du X, Ji C, Huxley R, Guo Y, Wu S: Cumulative exposure to ideal cardiovascular health and incident diabetes in a Chinese population: The Kailuan study. J Am Heart Assoc 5: e004132, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kriebel D, Checkoway H, Pearce N: Exposure and dose modelling in occupational epidemiology. Occup Environ Med 64: 492–498, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Robinson BM, Tong L, Zhang J, Wolfe RA, Goodkin DA, Greenwood RN, Kerr PG, Morgenstern H, Li Y, Pisoni RL, Saran R, Tentori F, Akizawa T, Fukuhara S, Port FK: Blood pressure levels and mortality risk among hemodialysis patients in the dialysis outcomes and practice patterns study. Kidney Int 82: 570–580, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zoccali C, Tripepi R, Torino C, Tripepi G, Mallamaci F: Moderator’s view: Ambulatory blood pressure monitoring and home blood pressure for the prognosis, diagnosis and treatment of hypertension in dialysis patients. Nephrol Dial Transplant 30: 1443–1448, 2015 [DOI] [PubMed] [Google Scholar]
- 13.Bansal N, McCulloch CE, Rahman M, Kusek JW, Anderson AH, Xie D, Townsend RR, Lora CM, Wright J, Go AS, Ojo A, Alper A, Lustigova E, Cuevas M, Kallem R, Hsu C-YY; CRIC Study Investigators : Blood pressure and risk of all-cause mortality in advanced chronic kidney disease and hemodialysis: The chronic renal insufficiency cohort study. Hypertension 65: 93–100, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Agarwal R: Blood pressure and mortality among hemodialysis patients. Hypertension 55: 762–768, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hur E, Usta M, Toz H, Asci G, Wabel P, Kahvecioglu S, Kayikcioglu M, Demirci MS, Ozkahya M, Duman S, Ok E: Effect of fluid management guided by bioimpedance spectroscopy on cardiovascular parameters in hemodialysis patients: A randomized controlled trial. Am J Kidney Dis 61: 957–965, 2013 [DOI] [PubMed] [Google Scholar]
- 16.Onofriescu M, Hogas S, Voroneanu L, Apetrii M, Nistor I, Kanbay M, Covic AC: Bioimpedance-guided fluid management in maintenance hemodialysis: A pilot randomized controlled trial. Am J Kidney Dis 64: 111–118, 2014 [DOI] [PubMed] [Google Scholar]
- 17.Moissl UM, Wabel P, Chamney PW, Bosaeus I, Levin NW, Bosy-Westphal A, Korth O, Müller MJ, Ellegård L, Malmros V, Kaitwatcharachai C, Kuhlmann MK, Zhu F, Fuller NJ: Body fluid volume determination via body composition spectroscopy in health and disease. Physiol Meas 27: 921–933, 2006 [DOI] [PubMed] [Google Scholar]
- 18.Machek P, Jirka T, Moissl U, Chamney P, Wabel P: Guided optimization of fluid status in haemodialysis patients. Nephrol Dial Transplant 25: 538–544, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chamney PW, Wabel P, Moissl UM, Müller MJ, Bosy-Westphal A, Korth O, Fuller NJ: A whole-body model to distinguish excess fluid from the hydration of major body tissues. Am J Clin Nutr 85: 80–89, 2007 [DOI] [PubMed] [Google Scholar]
- 20.Wabel P, Chamney P, Moissl U, Jirka T: Importance of whole-body bioimpedance spectroscopy for the management of fluid balance. Blood Purif 27: 75–80, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Matthews JN, Altman DG, Campbell MJ, Royston P: Analysis of serial measurements in medical research. BMJ 300: 230–235, 1990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Martin SS, Michos ED: Mapping hyperlipidemia in young adulthood to coronary risk: Importance of cumulative exposure and how to stay young. Circulation 131: 445–447, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zemaitis P, Liu K, Jacobs DR Jr., Cushman M, Durazo-Arvizu R, Shoham D, Palmas W, Cooper R, Kramer H: Cumulative systolic BP and changes in urine albumin-to-creatinine ratios in nondiabetic participants of the multi-ethnic study of atherosclerosis. Clin J Am Soc Nephrol 9: 1922–1929, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.The Diabetes Control and Complications Trial Research Group : The relationship of glycemic exposure (HbA1c) to the risk of development and progression of retinopathy in the diabetes control and complications trial. Diabetes 44: 968–983, 1995 [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.