Abstract
What is the role of shared calendars for home health management? Utilizing a maximum variation sampling method, we interviewed 20 adult individuals with diabetes and 20 mothers of children with asthma to understand calendar use in the context of chronic disease home health management. In comparing the experiences of these two groups, we explore participants’ use of tools for organizing tasks and appointments, their strategies for capturing health and non-health events in the family calendar system, the ecology of artifacts that intersect with their scheduling tools, and the failures they experienced while managing their calendar systems. Through this work, we offer a context-specific perspective of schedule management strategies for individuals and families who must integrate their handling of chronic illnesses with everyday living.
Author Keywords: Medical and health support, Home/family/intimacy support, Empirical Methods, Qualitative, Workflow management
ACM Classification Keywords: H.5.3 Group and Organization Interfaces
INTRODUCTION
Calendars are crucial to managing daily life in the home [22]. Household calendars depict complex interactions among individual schedules of family members and can convey meaning and values behind the priorities of scheduling [14]. With the importance of the household calendar in mind, we investigate the use of calendars in the home among families who have one or more individuals living with a chronic illness (pediatric asthma or diabetes).
Individuals living with a chronic illness must perform a large number of daily self-care activities to ensure the best health outcomes [1, 2]. Management of diabetes can include regular activities such as home blood pressure measurements as well as clinical tests to assess blood glucose control [12, 19, 26]. For children with asthma, symptoms are monitored through clinic outpatient visits [10] and caregivers must monitor symptom control and often administer medications on a daily schedule [18]. For individuals with diabetes and asthma, these extra disease management activities take place in addition to the everyday schedule management typical of all families. Thus, we investigate calendar management in this context and explore the strategies that patients with diabetes and caregivers of children with asthma use to meet their health goals and coordinate with clinicians.
Given that our participants must make decisions about prioritizing regular self-care activities, and integrate medical care with their schedule management practices, we explore complicated behaviors in interactions with healthcare information systems and personal calendar tools. Through a user-centered approach we consider the unique context of chronic disease management and build upon previous work in the design space for shared calendar systems in the home. In this paper, we focus on describing the day-to-day routines of patients and caregivers, as well as current patient engagement with provider healthcare information systems. The descriptive work reported here is an initial investigation that provides contextual information to inform future design of user-centered reminder systems in the healthcare and home health management settings.
RELATED WORK
Research in the shared calendar space—of which family calendars are one example—started in the domain of workplace groupware, where electronic calendars were used initially in the workplace context [23]. As adoption in the workplace increased, usage of personal digital assistants and mobile phones blurred the boundaries of calendar management between work and home [9] and led to in-creased research in personal life and family unit domains. We review the history of investigation of the shared calendar space as well as the limited work on the use of calendars in home health management to build upon and update research in this area.
Groupware calendar use in the workplace context
Payne’s [24] investigation of electronic calendar use among professionals revealed that, despite access to a range of software tools for schedule and to-do list management, interviewees continued to use supplementary paper calendars. Calendar tools of any type were critical to “prospective remembering”—that is, remembering to do things and forming intentions for future actions. Payne also found that calendars were valuable for eliciting information about users’ intentions and priorities in their lives.
More recent investigations of groupware calendars in the workplace have incorporated the shifting boundaries of work and home calendars, particularly with the adoption of personal digital assistants and mobile phones. Sellen et al. [27]deployed a short survey to working parents and found one highly-ranked concern about the ability to coordinate tasks in real time among family members. Grimes and Brush [9] researched parents who used Microsoft Outlook professionally to explore the overlap between work and personal schedule management through calendar tool use. Parents described failures in being able to share Outlook calendars and coordinate with spouses working in other organizations, but parents also feared judgment from coworkers for entering personal appointments on the shared work calendar. As a result of this study, Grimes and Brush argued for more finely tuned controls over calendar information, with the ability to share or not share event information at the appointment level, rather than the calendar preference level. Mariani et al. [15] also identified user privacy through access controls of event information as an important design feature in electronic calendars.
Sell and Walden [28] found that mobile calendars used among knowledge workers were valuable for managing self-described “hectic” and “volatile” personal schedules. Participants in the study valued certain design features of digital calendars over those of paper calendars, including: the inability to inadvertently double-book time slots; reminder functions that “free up” the brain from remembering upcoming commitments; the backward archive of previous commitments for personal records; and the always-available nature of electronic calendars.
Shared calendar use in personal and intrafamily context
Investigating calendar use in the family context introduces different challenges to the coordination of schedules. The adoption of electronic calendars, personal digital assistants, and mobile phones in the workplace and then in the home has encouraged greater exploration of personal schedule management integrated within the family environment.
Crabtree and Rodden [7] observed that the domestic unit (its inhabited structure, individual actors, and involved technology and coordinating habits) is not strictly analogous to an organizational unit of work, but treating the domestic unit as a discrete subject of interest has thus far yielded valuable ethnographic insights to the “routines” of everyday life therein. Through direct observation of home life, Crabtree and Rodden used physical and locational mapping of family homes to highlight ecologies, activity centers, and coordinating displays of domestic habitat. Further research into calendar management in the home context has identified more complex calendar use among working parents [6], as well as the importance of informal information management practices that supplement calendar management. Informal management of schedules in families identified in Brush and Turner’s [6] survey included face to face or email interactions, which enabled coordination between partner parents.
To gather descriptive information around tool use, Brush and Inkpen [5] interviewed 15 families and found linkages between device type and ownership types. For example, mobile phones and iPods were generally individually owned, whereas shared computers in shared areas did not have such individual ownership ties. Ownership of calendar content was explored by Neustaeder et al. [22], who articulated a taxonomy of three calendar content ownership types: monocentric families relied on a sole primary scheduler to maintain the calendar, pericentric families had a primary scheduler, with an occasional secondary scheduler assisting in recording or maintaining calendar content, and polycentric families maintained calendars among multiple schedulers, who would add and edit content as needed. The concepts of device or content ownership in these two studies are valuable in articulating the access and control needs for managing a calendar across family members.
Design-based research into family calendar management includes participatory design with mothers [20] and a pilot field test of the resulting tablet PC-based system, LINC, in four family homes [21]. Using existing knowledge about high-traffic areas in the family home and opportunities for family calendar collaboration, families were encouraged to place the calendar where it could be accessed by all members. In both studies, along with Tungare and Perez-Quinones [31], researchers found a preference for always-on access to shared family calendars among interviewees, meaning that the family members could walk up and immediately access calendar information with minimal start-up time when a digital device tool was used.
Importantly, Bødker and Grönvall [3] moved their scope of family calendar investigation to that of shared goal spaces, which may involve people or organizations outside of the family. The authors presented two case studies of shared-work space calendars designed to aid 1) elder care tasks involving family members, paid caregivers, and clinicians, and 2) parental leave scheduling in a Danish municipality. This work is unique in its support of family-based goals, with an application of a calendar tool as an artifact of negotiation and coordination among family members and people outside of the family. In this sense, Bødker and Grönvall’s research resembles our exploration into current use of calendar artifacts in families to coordinate the “work” of chronic disease management with outside organizations (e.g., the healthcare system) and people (e.g., individual clinicians or specialists involved in family care).
Calendar use in home health management
Other researchers have investigated personal health information management practices in the home and identified calendars as a component of patients’ health information management strategy. In one of the first studies of personal health information management in the home, Moen and Brennan identified a variety of strategies—just in time, just because, just at hand, just in case—that people used to remind themselves of health tasks [17]. Although they note calendars as one of many tools used to support those strategies, they did not describe any details for how or why calendars were used. In Klasnja et al.’s [13] study of breast cancer patients, they also noted calendars as an artifact that patients frequently used to help them manage health information while they were out and about. Based on their fieldwork, they also used calendars as a core component in the design of their personal health information management system—HealthWeaver—in linking information to their mobile calendar [14] as well as in coordinating help among patients’ social network [29]. Based on their fieldwork of elderly home health management, Bossen et al. also chose to use a calendar system as the main artifact to support care coordination for elderly patients [4]. Thus, several re-searchers have noted use of calendars in personal health information management, but none have thoroughly documented its role of the calendar in personal or home health information management.
Current study contributions
Previous work in the shared calendar area has investigated calendar groupware use in organizations, user-designated ownership of calendars and content, management of tools between home and work (particularly among working parents), and calendar features that enhance sharing opportunities and user coordination. In this study, we explore calendar use in a specific context: among families who manage chronic health conditions in the home, and face complexities in schedule management related to daily health management activities. By focusing on calendar tool use within a maximum variation sample, we are able to reflect on a range of schedule management behaviors in support of goals for health outcomes and describe perceptions about multiple modalities of calendar control (e.g., paper and electronic calendars) from a holistic, user-centered point of view. We probed successful and unsuccessful strategies for calendar management in this context, with the goal of updating work on taxonomies of shared calendar management, as well as identifying design opportunities for shared calendar and reminder systems that will assist patients and clinicians in managing chronic diseases.
METHODS
Participants were recruited from 18 clinics within an integrated healthcare delivery system in the northwestern United States. Over 300,000 members receive care from these facilities from over 1,000 physicians. This healthcare system has offered patient access to online health services since 2003, including: secure messaging with primary and specialty healthcare providers; ordering medication refills; scheduling in person appointments; viewing summaries of care; viewing results of medical tests; and viewing lists of immunizations, allergies and health conditions. As of May 2014, 74% of those enrolled in the integrated delivery system were registered for these online services [25].
Sample
Adults with Type 2 diabetes (n=20) and mothers of children with asthma (n=20) were recruited using a purposeful sampling framework. Inclusion of these two distinct groups, each managing different aspects of chronic illness, allowed us to maximize the variation in the elicited responses regarding home health care and calendar management. Since both asthma and diabetes require ongoing self-management as well as communication with healthcare providers, we also anticipated that some calendaring and other reminding strategies may be shared across the groups. Our intention was not to compare asthma and diabetes cohort responses, but to gather the widest range of calendar management behaviors for chronic disease management. By collecting the perspectives and needs of a diverse population of chronic disease users we can improve our approach to future design work that incorporates user strategies around both paper and electronic calendars.
All participants were recruited by telephone. Interviews were conducted in the home and ranged from 45 to 90 minutes, including a supplemental home tour during which participants demonstrated where and how they manage their calendars and other relevant home health care. Participants were asked to share information about their health care priorities, day-to-day health care routines, calendar management, frequency and modality of clinical contact, and perceptions about interactions with their healthcare system, specifically how they schedule medical appointments, manage appointment reminders, and utilize patient information artifacts such as after-visit summaries. Each participant was paid $50 for his or her participation.
Interviewees included 10 men (patients with diabetes) and 30 women (10 patients with diabetes and 20 mothers of children with asthma). The median sample age was 54.5, but varied within each sub-sample, with mothers being younger on average than the patients with diabetes. We intentionally over sampled racial and ethnic minorities and sought to recruit a sample with an educational level representative of the United States population. Finally, we sought a mixture of those using and not using the online patient portal services, to reflect growing patient engagement in the electronic health record. Sample characteristics are presented in Table 1.
Table 1.
Sample Cohort Demographics
| Total | Asthma | Diabetes | |||
|---|---|---|---|---|---|
| N | N | % | N | % | |
| 40 | 20 | 100 | 20 | 100 | |
| Median Age (Years) | 54.5 | 37.0 | 64.0 | ||
| Mean Age (Years) | 54.4 | 37.5 | 64.5 | ||
|
| |||||
| Race & ethnicity | |||||
|
| |||||
| Asian | 2 | 0 | 0 | 2 | 10 |
| Black | 12 | 6 | 30 | 6 | 30 |
| Hawaiian | 1 | 1 | 5 | 0 | 0 |
| Indian | 0 | 0 | 0 | 0 | 0 |
| Mixed | 1 | 0 | 0 | 1 | 5 |
| Other | 2 | 1 | 5 | 1 | 5 |
| Unknown | 2 | 2 | 10 | 0 | 0 |
| White | 20 | 10 | 50 | 10 | 50 |
|
| |||||
| Hispanic* | 2 | 1 | 5 | 1 | 5 |
|
| |||||
| Online health portal use | |||||
|
| |||||
| User | 27 | 17 | 85 | 10 | 50 |
| Non-user | 13 | 3 | 15 | 10 | 50 |
|
| |||||
| Education | |||||
|
| |||||
| >High school | 28 | 16 | 80 | 12 | 60 |
| High school or less | 12 | 4 | 20 | 8 | 40 |
Hispanic ethnicity designation overlapped with other designations of race; total is > 100%
ANALYSIS
All 40 interviews were transcribed and then imported into qualitative analysis software (Atlas.ti). Four independent coders worked on three coding schema iterations to identify significant themes related to schedule management behaviors, calendaring strategies and artifacts, and home health management. The group of coders used “brainstorming the data” [30] individually as an approach to identify themes during the open coding period. The group then met periodically to review and revise codes to develop consensus around code definitions and their use within the transcripts. To organize the emerging codes and consolidate similar themes, we then used affinity grouping and refinement of code definitions to agree on a final set of codes [16].
Descriptive overview
Twenty-eight of the 40 total participants indicated that they used a calendar (N=15) or a mobile phone (N=13) as their primary tool to manage the household schedule. However, each cohort demonstrated different primary calendar tool use; participants were asked to indicate which calendar tool they used daily or considered to be the go-to information source for schedule management. Diabetes cohort participants reported wall calendars as a primary tool (N=11, or 55%) more often than mothers (N=4, or 20%), while a greater proportion of mothers used mobile phones (N=11) as a primary tool than diabetes cohort interviewees (N=2).
In addition to the differences in primary tool use, the behavior around sharing calendar information related to tools differed. Shared tools were those that were displayed intentionally in the household (in the case of paper tools) or opened access controls for multiple users (in the case of electronic tools, such as a Google calendar). Tools were shared for the benefit of multiple individuals or for frequent reference. Unshared tools were intentionally private, due to concerns about privacy, preferences for information sharing, or perceived difficulty in managing technology features, such as with mobile calendars. Wall calendars were generally indicated as shared primary tools, whereas mobile phone calendars were largely used as private calendar aids. In Table 2, we summarize the primary schedule management tools used by the study participants. A more detailed overview of tool use is available in Appendix A.
Table 2.
Primary tool use reported by each study participant, by cohort
| # reporting unshared primary tool | # reporting shared primary tool | |
|---|---|---|
| Asthma moms cohort (N=20) | ||
| paper reference* | 1 | |
| phone | 9 | 2 |
| tablet | 1 | |
| wall calendar (paper) | 4 | |
| whiteboard | 2 | |
| e-calendar | 1 | |
| Diabetes cohort (N=20) | ||
| desk calendar | 1 | 1 |
| phone | 2 | |
| planner | 1 | |
| tablet | 1 | |
| wall calendar (paper) | 1 | 10 |
| whiteboard | 1 | |
| e-calendar | 1 | 1 |
Participant primarily used a basket of mail to manage her schedule
RESULTS
Given the differences in calendar tool use profiles between the participant cohorts, we were interested in investigating themes that reflected the diverse strategies participants used to integrate their health management needs within their regular daily schedules. Using affinity diagramming and iterative coding practices, we identified four major thematic groups: (1) the participant’s rationale for particular scheduling tool use; (2) their strategies for capturing events in the family calendar system; (3) their integration of reminder systems into their calendar tools; and (4) the challenges and failure points that they experienced in family calendar and schedule-keeping strategies.
Rationale for particular tool use
Throughout the interviews, participants described their reasoning for using a particular calendar tool based on the tool’s visibility, accessibility, trust, and ease of use. These qualities strongly influenced whether a participant used a paper-based or electronic system in different situations. When coordination with other family members was paramount, often a simple wall calendar system was used to keep family members informed about the schedule. The paper wall calendars were one of the most widely used tools across our participants and often placed in prominent, high traffic areas to maximize schedule visibility and sharing.
[The calendar is] probably more for [my husband] so that he knows that I have a doctor’s appointment that day or something. It’s that communication between the two of us more than anything. I probably wouldn’t - I might, but I probably wouldn’t be as tempted to do it if it were just me alone. (D20)
The participants valued the highly visible tool because it encouraged regular dialogue about upcoming activities and helped avoid last minute coordination. However, although the wall calendars were easily accessible in the home, some participants favored a shared e-calendar for making it easier for multiple family members to manage content regardless of their location. A13 and her family describe how, “We just couldn’t keep [our family wall calendar] up to date because we’re in so many different places…so we do it online now.” The family’s polycentric scheduling model was supported best through shared input online by multiple members of the family. In this type of environment, electronic calendars helped to organize and streamline information by reducing the amount of paper clutter (A20).
Despite the growing use of electronic tools, some study participants disliked maintaining schedules in a virtual environment. They highlighted the issue of already spending too much time in front of a mobile phone or other computing device. In addition, the participants who resisted adoption of electronic calendars expressed anxiety about losing data, running out of battery, or lacking technical skills to troubleshoot the tool.
[I]write it on a piece of paper and then I usually put it on the planner because that’s what I look at really, that’s what I depend on. I don’t depend on my phone to have everything in it. Until I get to that point, I just don’t see how, I mean what if you need to look at it and there’s no more juice in it? (D01)
Regardless of which primary tool a participant used, they often incorporated additional artifacts that supported their schedule management. These artifacts included pre-printed school calendars, appointment cards from a dentist or doctor, letters in the mail, temporary post-it notes, and secondary calendar tools. In most cases, the artifacts served as workarounds to compensate for periodic shortcomings in accessibility to the primary calendar system (e.g. being outside the home). One mother described using the “notes” feature of her mobile phone calendar to temporarily record data when out of cellular range in the workplace (A15). Others found it easier to place a temporary artifact such as an appointment card or soccer schedule in a visible location rather than enter it into the calendar.
I don’t know, I feel like I still appreciate both [written and electronic]. Like the dentist office, they’ll still hand out the little, it looks like a business card and it shows the date and time. I just throw it in my wallet and I feel like whenever I’m reaching for other stuff in my own wallet, basically it lives there for about six months and I see it once in a while and it just reminds me. (A06)
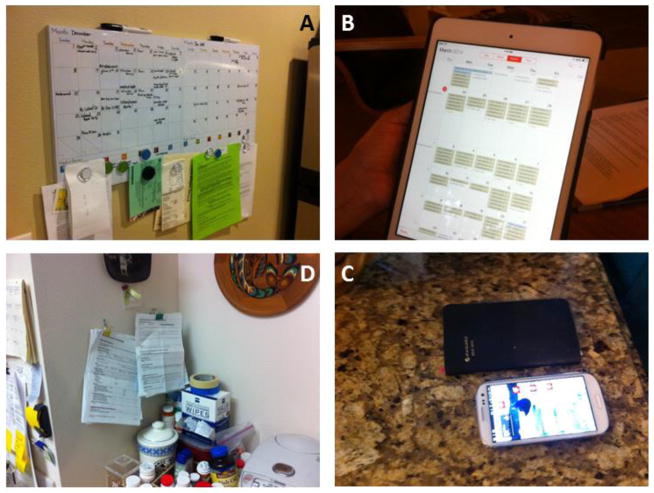
Some participants that had a secondary calendar system appreciated having different aspects of their lives (work, home, health) segmented into different systems, felt more secure with a backup system of upcoming events, or did not want to deal with the burden of transferring everything over into their primary tool. Overall, interviewees characterized their use of additional scheduling artifacts based on the accessibility of their primary tool, enhanced schedule awareness created through redundant streams of information, and the ease of integrating the event information from multiple sources. Examples of tools used by participants are shown in Figure 1.
Figure 1.
Example of home calendar systems. Clockwise from top left: A) Whiteboard calendar with paper artifacts attached; B) Shared electronic calendar accessed through table computer; C) Dual paper planner and mobile phone calendar system that requires manual information transfer; D) Paper-based system using artifacts from healthcare system and “basket” of related health care items
Strategies for capturing events
The bulk of calendar information participants reported was manually input; this information included both health and personal events. Transferring information from artifacts such as external calendars (e.g., those provided by the school district for mothers) or appointment cards (e.g., from hair salons, doctors, or dentists) often helped participants remember upcoming events more effectively: as one participant stated, “When you write it down, it tends to stay in my memory a lot better” (D10).
Behavior in manually entering calendar content changed depending on whether planning for events was taking place in the short or long term time horizon. Participants were more likely to skip entering an event on the calendar if it was to take place the same day, such as an urgent care appointment for a child, since the engagement occurs relatively quickly thereafter and is likely a priority. The exception to this theme included situations of sharing information about a same-day appointment with a partner or spouse; one mother stated, “I’ll put it in the calendar so my husband knows where we’re at” (A19).
Participants recorded more information about their upcoming appointments, such as the clinic location, when they had a greater number of clinicians involved in their own or their child’s care. Other purposes for recording information outside of the doctor’s name and the time of the appointment included visiting a new location for the first time (A03, A09), preparing transportation for future appointments (D15, D18), or adding geolocation data through an electronic calendar application for future navigation in the car on the way to the appointment (A06, A12).
The act of adding content to calendars was described as highly situational by the majority of participants. Participants noted that it was important to capture details about a new event as soon as possible to make sure the content was captured successfully. Event details were most likely to end up on the desired calendar tool if the participant was physically near the tool while discussing the event or making appointments. In one case, a participant described putting off making follow-up doctor’s appointments until she could go home and look at her paper calendar: “I don’t think I’ve ever made an appointment at the [doctor’s] office. I think I always come home and call them back” (D13).
Capturing content in a timely manner was not only reported as an issue with paper calendars, however. Mobile phone calendar users reported problems with making appointments while using their mobile phones and the calendar application at the same time. One mother described her necessary, but seemingly impolite, work-around:
If I’m on the phone with someone, I will put them on speaker and change modes so I’ll look at the calendar while I’m talking to them, because often if I rely on my brain, even if we just hung up three minutes later, I might not remember what day it is, especially if we go over multiple dates for an appointment. It can feel rude to someone to be put on speaker, but if we want this on my calendar, I have to do that. (A09)
Both mothers of children with asthma and adults with diabetes had strong personal preferences for calendar content. Some participants preferred to maintain separate calendars for specific purposes; diabetes cohort participants described keeping one calendar specifically for medical appointments, avoiding extra clutter from personal engagements (D15, D12). Separate calendars were also used for synchronizing appointment information, a different strategy by which the act of transferring information from one calendar to another was itself a memory aid:
If I get an appointment, then I write it down…I go in [the patient website], because it shows upcoming appointments so then I’ll print off the deal and go in there and check my calendar, so it’s a backup type, so I got a system, my checks and balances. (D05)
In addition to adding content to calendars manually, participants provided a number of examples in their personal lives where electronic calendar invites simplified schedule management. Participants were generally receptive toward receiving calendar invitations for special events, which saved them the trouble of manually updating the calendar:
My older son’s soccer team, his coach was a Microsoft guy so he was very tech savvy. He sent out basically like a Google calendar invite so he had all our games and all our practices basically preloaded for us. All we had to do was accept the invite and then automatically it showed up on my calendar. It’s like magic. (A06)
Helpful external aids for calendaring events were not limited to electronic users; paper calendar users also pointed to helpful tools, as one mom explained:
This is kind of a neat thing the school does. The school does these preprinted stickers so that we get all the events for the whole year on [the wall calendar]. (A18)
For participants who used mobile phone calendar applications, several also reported automatic syncing between social media applications and their personal calendars, such as for birthdays from Facebook.
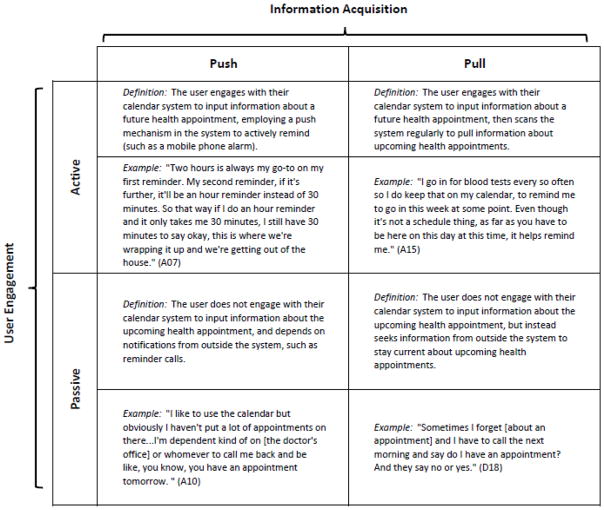
Integration of reminder systems
Another important theme was habits of engagement with calendar tools that users developed to help them remember activities that they had captured in their calendars. We refer to these habits of engagement as reminder systems. Reminder systems were important behaviors associated with calendar use, because as one interviewee explained, “It’s not the system failing me, it’s me not engaging with the system sometimes, if I think I know something” (A09). Examples of reminder systems include alarms that participants set on their phones or e-calendars to remember an appointment, actively scanning paper calendars to review the day’s activities at a routine time in the morning, or even having informal discussions with family members to coordinate on details of upcoming events.
Based on our participants’ reports of using reminder systems, we identified two facets of preferred reminder characteristics: active vs. passive and push vs. pull. In the first facet of reminder systems, we found that reminders could be active or passive. Active reminders were those that the participant had to initiate, where the individual described interacting with the system to record the reminder and determine its characteristics (such as an alarm on the phone, or a post-it note on the front door). Passive reminders were those in which the individual did not explicitly interact with their system to create a reminder, and rather relied on receiving an outside prompt—such as a reminder phone call from their clinic—to remember about an upcoming obligation or event.
The second facet of reminder systems was push versus pull information acquisition. In a push information acquisition, the participant expressed a need to have her attention drawn to an upcoming obligation or event—essentially, an interruption helped the individual to remember. This strategy could incorporate reminders set on a mobile phone, for instance, and make a particular sound to alert the participant to look at the event details.
Alternatively, a pull information acquisition involved encountering or scanning information—although an individual could choose to stop and read a dentist’s appointment card found at the bottom of a purse, it could also be ignored, and lacked the same disruptive quality of a push reminder. By using the two facets of reminder management associated with calendar tool use, we are able to discern a structure in participant preferences for how they maintained awareness about their health appointments (see Figure 2).
Figure 2.
Reminder systems can be classified by facets such as push or pull information acquisition, and the type of user engagement (passive, active): examples of each classification are shown here
Finally, patterns in preferences and behavior around reminders were found to be tool agnostic. Participants using mobile phone calendars described using pull-type reminders in the same way as wall calendar users did, particularly when push reminders were troublesome to set or inappropriately disruptive at the participant’s place of work.
Challenges and failure points in schedule management
In addition to probing strategies and habits related to calendar management and sharing, we also inquired about negative events in scheduling behaviors that led to participant-perceived failures. Participants discussed failures related to tool access, user entry errors, and missed appointments or events due to scheduling mistakes or forgetfulness. Using the body of narratives we collected about failures in calendar management, we identified multiple points of potential failure in the processes for setting an appointment or scheduling an event and remembering to attend the appointment as scheduled.
Initial opportunities for failure in calendar management can occur at the time event details are added. Sufficient details of the event must be added to the calendar to remind the user of the upcoming events successfully. For this evententry stage, we identified three distinct types of failures: uncaptured events, events captured incorrectly, or events not synchronized to multiple tools. In all types of failures, participants described experiencing a negative event that was unavoidable without outside intervention or unless the calendar owner reviewed the tool or tools to verify information
Subsequent to capturing an event or appointment, the next major point of potential failure in calendar management occurs at the reminder stage. Both paper and electronic calendar users reported failures in scanning calendar content as a cue for reminding about upcoming events. As one participant stated, “If I don’t look at the calendar, I may forget” (D04).
Participants who used electronic calendars as their primary tool also reported failures in push reminders associated with events, a problem paper calendar users did not encounter. Failures at the reminder stage could be caused by ineffective reminder settings, or by dismissal of or distraction from the reminder that reduces its effectiveness.
[Microsoft] Outlook for sure can be really frustrating if you don’t set it for enough notification time. I’m really good at setting it, it’s got a default for 15 minutes. Well, 15 minutes is not enough time if you forget…That’s probably the biggest one is Outlook for me, because if I don’t reset that default, then I miss things or forget about things at the last minute. (A04)
I guess the one thing I changed after [the missed doctor’s appointment] is I’ve set reminders on my phone - or thought I set reminders on my phone and I never actually activated the alarm and that has made me miss appointments. (A03)
Incorporating participant narratives about failures in our analysis helped us to understand vulnerabilities in the different stages of schedule management and provided a richer understanding of the challenges patients can face in attempting to achieve their health goals.
DISCUSSION
Participants spoke about knowing which tactics could successfully engage their prospective memory as often as they discussed the devices and artifacts of calendars and reminders. Discussing calendars and schedules revealed participants’ priorities for their lives, as described previously by Payne [24] and Mariani et al. [15]. Participants’ accounts of intentions and priorities in managing daily schedules led to more in-depth discussions about personal importance of activities such as doctor’s visits and self-care routines. One mother described the events that migrated to her calendar as things that “make me money and keep [my daughter] healthy.” A caregiver for an adult with advanced diabetes referred to the act of keeping the household schedule as “what’s keeping [her partner] alive.” The importance of the calendar systems, and the involvement of calendar and scheduling activities in health-related activities, proved to offer rich interrelated themes.
Our investigation also revealed that the majority of the households we visited employed an “ecology” of calendar, scheduling, and reminder tools. The interaction between multiple tools created an even more complicated meta-system of information fragmentation, information transfer, redundancies, and information dissemination among family members, and is supported by previous work examining home health management strategies [17]. This complexity of home information management observed in this study underlines the importance of considering the wide range of preferences and needs of users and how they rely on and integrate healthcare information systems as part of their schedule management ecologies.
As previous studies have found through the years [6, 24], paper systems in these ecologies have not disappeared, and are often a critical part of the calendar and schedule system in the household, even when the primary calendar tool is a mobile phone—9 (69%) of 13 participants who used mobile phone calendars primarily used at least one secondary paper system. Participants in the diabetes cohort were more likely to use paper-based primary tools, whereas the asthma cohort reported using mostly digital calendars as their main tool; each cohort contained notable exceptions (e.g., enthusiastic technophiles in the diabetes cohort and reluctant technology users in the asthma cohort), but the preference for paper versus digital appeared to adhere to generational preferences, with the younger asthma moms using digital tools and diabetes patients preferring paper calendars. Although each participant had a primary calendar tool, it was unusual for an individual (diabetes patient or mother-caregiver) to rely on just one tool; diabetes participants reported an average of two calendar tools in use, and asthma mothers used an average of 3.4 tools each. This is consistent with the finding from Brush and Turner [6] that people who have children in the household use more tools than people without children. Additionally, participants in the diabetes cohort reported fewer needs to display shared information, and often consolidated calendar information to one artifact, resulting in fewer paper systems per household.
Redundancy in the ecosystem of household calendar management was often cited as a mechanism that helped participants avoid failure. Participants cited a variety of backup tools – including those outside of their own systems or generated by users who shared the systems – that reduced the effects of calendar failures. Backup mechanisms outside of the internal family system tended to include reminder calls, emails and texts from medical or service providers. Participants also confirmed calendar information by checking in with other sources, such as by calling the doctor’s office or checking the patient portal for appointment information. We described such strategies as methods for increasing reliability of calendar systems in a previous analysis of calendar system failures [11], categorizing such adaptations by calendar users as redundancy, diversity of systems used, and active monitoring behavior.
Informal reminders from partners or spouses who shared a calendar tool served to reduce failures in schedule management; these informal methods were also identified as a major element of schedule management in previous studies [6, 21]. Participants reported that keeping external artifacts, such as appointment cards from doctors or dentists, also served as a dual, backup reminder system. Paper proved to be an essential part of the ecosystem and its redundancy surrounding primary calendar tools. In particular, participants in the asthma cohort often reported multiple paper supplementary systems in their system used to share information with others, such as tacked up paper reminders to notify partners or children who could read about upcoming events (please see Appendix A).
We also elicited information from participants about their use of external systems that interacted with participants’ calendar management strategies, such as electronic calendar invites and preprinted stickers sent home from school, which aided paper calendar users in transferring important information to the home system. As we move forward in seeking design opportunities for individual calendar and reminder systems and healthcare information systems, we will be able to address approaches for integrating external healthcare information systems with patients’ home calendar ecologies and better support home health management.
Finally, we observed how the heath-care system touched the day-to-day routines and calendar management of chronically ill patients and their caregivers through multiple modalities. Our participants still relied on paper-based artifacts, such as appointment cards and letters, but increasingly used the patient portal for activities such as referring to appointment calendars and communicating with providers. Patient perceptions of the timeliness and effectiveness of different types of healthcare reminders also highlighted the importance of tailoring these reminders to the home calendaring practices and capabilities of patients and caregivers.
For designers, this work sheds light on the importance of user engagement as a feature of calendar systems that support home health management. We found that the highly situational and time-sensitive nature of health information influenced user’s habits of engagement in ways not anticipated by current information system designs, despite the different affordances digital and paper tools have for push/pull and active/passive engagement. Future work will explore opportunities for enhancing user engagement, especially with redundant and external systems that reduce failure opportunities and reinforce user discretion and competence in managing health information.
LIMITATIONS
This study is limited in its generalizability due to its qualitative nature and purposive sampling, meant to mimic the demographics of the United States. However, the inquiry is intended to give a broad set of information about calendar use in the home in the chronic disease management context through maximum variation between the two sample cohorts. By gathering participant experience that is both typical and divergent, we construct a rich set of findings about participant context and use of calendar tools. In this study, we are more concerned with “a full array of multiple realities” than statistical significance [8], and we hope to build upon the rich contextual descriptions with further design work (see below), but we cannot claim to make generalizable findings to a wider population.
CONCLUSIONS
This paper describes our exploration of calendar management strategies among patients, caregivers, and families coping with chronic disease. We approached the topic of calendar management in the context of chronic disease management to update and enrich the knowledge around shared calendars among users whose day-to-day routines often are complicated by home health care activities. Information about calendar management was elicited from a holistic point of view, allowing us to discuss calendar ecosystems – including interactions among users of shared tools, multiple tool modalities, and system failures – rather than focus on individual tools. We found that calendar ecosystems overwhelmingly included multiple tools in each household, and paper systems continue to back up electronic device use. Integration of reminder systems into their calendar tools included both active and passive reminders as well as those that relied on push and pull approaches.
By studying shared calendar use and the range of behaviors described by our participants, we are able to show diverse user needs and a complex ecosystem of paper and electronic tools. Improvements to healthcare information systems must consider this complexity to integrate and support home health management successfully. This work provides valuable contextual information for design opportunities in calendar management systems for supporting individuals and families living day-to-day with chronic illness.
Acknowledgments
This work was supported in part by the AHRQ grant (R01HS 021590).
Appendix A: Shared and Unshared Calendar Tool (Detailed)
| Private Tools | Shared/Public Tools | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| <---analog-----------------------------------------------------------------------------------digital---> | <---analog-----------------------------------------------------------------------------------digital---> | |||||||||||||||||
| Participant ID | wall calendar (paper) | paper reference | white board | desk calendar | planner | tablet | e-calendar | phone | wall calendar (paper) | paper reference | white board | desk calendar | planner | tablet | e-calendar | phone | Total tools used | |
| Asthma cohort | 01 | ■ | ■■ | ■ | 4 | |||||||||||||
| 02 | ■ | ■ | 2 | |||||||||||||||
| 03 | ■ | ■ | ■■ | ■ | 5 | |||||||||||||
| 04 | ■ | ■ | ■ | ■ | 4 | |||||||||||||
| 05 | ■ | ■ | ■■ | 4 | ||||||||||||||
| 06 | ■ | ■■ | 3 | |||||||||||||||
| 07 | ■ | ■ | ■■ | 4 | ||||||||||||||
| 08 | ■ | ■ | 2 | |||||||||||||||
| 09 | ■■ | ■ | 3 | |||||||||||||||
| 10 | ■ | ■ | ■ | 3 | ||||||||||||||
| 11 | ■ | ■ | ■ | 3 | ||||||||||||||
| 12 | ■ | ■ | ■■■ | ■ | 6 | |||||||||||||
| 13 | ■ | ■ | ■ | 3 | ||||||||||||||
| 14 | ■ | ■ | ■ | 3 | ||||||||||||||
| 15 | ■ | 1 | ||||||||||||||||
| 16 | ■ | ■ | ■■ | 4 | ||||||||||||||
| 17 | ■ | ■ | ■ | ■ | ■ | 5 | ||||||||||||
| 18 | ■ | ■ | ■ | 3 | ||||||||||||||
| 19 | ■■ | 2 | ||||||||||||||||
| 20 | ■ | ■ | ■ | 3 | ||||||||||||||
| Diabetes Cohort | 01 | ■ | ■ | ■ | 3 | |||||||||||||
| 02 | ■ | ■ | ■ | ■ | 4 | |||||||||||||
| 03 | ■ | ■ | 2 | |||||||||||||||
| 04 | ■ | 1 | ||||||||||||||||
| 05 | ■ | ■ | ■ | 3 | ||||||||||||||
| 06 | ■ | ■ | 2 | |||||||||||||||
| 07 | ■ | ■ | 2 | |||||||||||||||
| 08 | ■ | ■ | 2 | |||||||||||||||
| 09 | ■ | ■ | 2 | |||||||||||||||
| 10 | ■ | 1 | ||||||||||||||||
| 11 | ■ | ■ | 2 | |||||||||||||||
| 12 | ■ | ■ | ■ | 3 | ||||||||||||||
| 13 | ■ | ■ | 2 | |||||||||||||||
| 14 | ■ | 1 | ||||||||||||||||
| 15 | ■ | 1 | ||||||||||||||||
| 16 | ■ | ■ | ■ | 3 | ||||||||||||||
| 17 | ■ | ■ | 2 | |||||||||||||||
| 18 | ■ | 1 | ||||||||||||||||
| 19 | ■ | 1 | ||||||||||||||||
| 20 | ■ | ■ | 2 | |||||||||||||||
 = 1 tool observed
= 1 tool observed
References and Citations
- 1.Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary care. JAMA. 2002a;288(19):2469–2475. doi: 10.1001/jama.288.19.2469. [DOI] [PubMed] [Google Scholar]
- 2.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: the chronic care model, Part 2. JAMA. 2002b;288(15):1909–1914. doi: 10.1001/jama.288.15.1909. [DOI] [PubMed] [Google Scholar]
- 3.Bødker S, Grönvall E. Calendars: time coordination and overview in families and beyond. ECSCW 2013: Proceedings of the 13th European Conference on Computer Supported Cooperative Work; 2013. pp. 63–81. [Google Scholar]
- 4.Bossen Claus, et al. CareCoor: Augmenting the coordination of cooperative home care work. International journal of medical informatics. 2013;82(5):e189–e199. doi: 10.1016/j.ijmedinf.2012.10.005. [DOI] [PubMed] [Google Scholar]
- 5.Brush AJ, Inkpen KM. Yours, Mine and Ours? Sharing and Use of Technology in Domestic Environments. UbiComp 2007: Ubiquitous Computing. 2007:109–126. [Google Scholar]
- 6.Brush AJ, Turner TC. A Survey of Personal and Household Scheduling Practices: Implications for Digital Family Calendars. 2007 MSR-TR-2007-23 (2007). http://research.microsoft.com/pubs/70417/tr-2007-28.pdf.
- 7.Crabtree A, Rodden T. Domestic routines and design for the home. Computer Supported Cooperative Work (CSCW) 2004;13(2):191–220. [Google Scholar]
- 8.Erlandson DA, editor. Doing naturalistic inquiry: Aguide to methods. Sage; 1993. [Google Scholar]
- 9.Grimes A, Brush AJ. Life scheduling to support multiple social roles. Proceedings of the SIGCHI Conference on Human Factors in Computing Systems; 2008. pp. 821–824. [Google Scholar]
- 10.Halterman JS, Yoos HL, Sidora K, Kitzman H, McMullen A. Medication use and health care contacts among symptomatic children with asthma. Ambulatory Pediatrics. 2001;1(5):275–279. doi: 10.1367/1539-4409(2001)001<0275:muahcc>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 11.[redacted for anonymity]
- 12.Kirkman MS, Briscoe VJ, Clark N, Florez H, Haas LB, Halter JB, Huang ES, et al. Diabetes in older adults: a consensus report. Journal of the American Geriatrics Society. 2012;60(12):2342–2356. doi: 10.1111/jgs.12035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Klasnja P, Civan Hartzler A, Unruh KT, Pratt W. Blowing in the wind: unanchored patient information work during cancer care. Proceedings of the SIGCHI Conference on Human Factors in Computing Systems; 2010. pp. 193–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Klasnja P, Hartzler A, Powell C, Pratt W. Supporting cancer patients’ unanchored health information management with mobile technology. AMIA Annual Symposium Proceedings; 2011. p. 732. [PMC free article] [PubMed] [Google Scholar]
- 15.Mariani JA, Crabtree A, Hemmings T, Rodden T. Informing the design of calendar systems for domestic use. Proc of the Eighth European Conference on Computer-Supported Cooperative Work; 2003. [Google Scholar]
- 16.Miles MB, Huberman AM. Qualitative data analysis: An expanded sourcebook. Chicago: Sage; 1994. [Google Scholar]
- 17.Moen A, Brennan PF. Health@ Home: the work of health information management in the household (HIMH): implications for consumer health informatics (CHI) innovations. Journal of the American Medical Informatics Association. 2005;12(6):648–656. doi: 10.1197/jamia.M1758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.National Heart, Lung and Blood Institute. Expert Panel Report III: Guidelines for the diagnosis and management of asthma. Bethesda: NIH; 2007. [Google Scholar]
- 19.Neumiller JJ, Setter SM. Pharmacologic management of the older patient with type 2 diabetes mellitus. The American journal of geriatric pharmacotherapy. 2009;7(6):324–342. doi: 10.1016/j.amjopharm.2009.12.002. [DOI] [PubMed] [Google Scholar]
- 20.Neustaedter C, Brush AJ. “LINC-ing” the family: the participatory design of an inkable family calendar. Proceedings of the SIGCHI Conference on Human Factors in Computing Systems; 2006. pp. 141–150. [Google Scholar]
- 21.Neustaedter C, Brush AJ, Greenberg S. A digital family calendar in the home: lessons from field trials of LINC. Proceedings of Graphics Interface; 2007. pp. 199–20. [Google Scholar]
- 22.Neustaedter C, Brush AJ, Greenberg S. The calendar is crucial: Coordination and awareness through the family calendar. ACM Transactions on Computer-Human Interaction (TOCHI) 2009;16(1):1–48. [Google Scholar]
- 23.Palen L, Grudin J. Implementing collaboration technologies in industry. London: Springer; 2003. Discretionary adoption of group support software: Lessons from calendar applications; pp. 159–180. [Google Scholar]
- 24.Payne SJ. Understanding calendar use. Human-Computer Interaction. 1993;8(2):83–100. [Google Scholar]
- 25.Ralston JD, Carrell D, Reid R, Anderson M, Moran M, Hereford J. Patient web services integrated with a shared medical record: patient use and satisfaction. Journal of the American Medical Informatics Association. 2007;14(6):798–806. doi: 10.1197/jamia.M2302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Saudek CD, Derr RL, Kalyani RR. Assessing glycemia in diabetes using self-monitoring blood glucose and hemoglobin A1c. JAMA. 2006;295(14):1688–1697. doi: 10.1001/jama.295.14.1688. [DOI] [PubMed] [Google Scholar]
- 27.Sellen AJ, Hyams J, Eardley R. The everyday problems of working parents: Implications for new technologies. Hewlett-Packard Labs Technical Report HPL-2004-37. 2004 [Google Scholar]
- 28.Sell A, Walden P. Mobile digital calendars: an interview study. System Sciences, 2006. HICSS’06. Proceedings of the 39th Annual Hawaii International Conference on System Sciences; 2006. [Google Scholar]
- 29.Skeels MM, Unruh KT, Powell C, Pratt W. Catalyzing social support for breast cancer patients. Proceedings of the SIGCHI Conference on Human Factors in Computing Systems; 2010. pp. 173–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Strauss AL, Corbin J. Basics of qualitative research. Vol. 15. Newbury Park, CA: Sage; 1990. [Google Scholar]
- 31.Tungare M, Pérez-Quiñones M. Technical report. Computing Research Repository (CoRR); 2008. An exploratory study of personal calendar use. [Google Scholar]